Abstract
Objective
To identify if functional treatment is the best available treatment for simple elbow dislocations.
Search strategy
Electronic databases MEDLINE, EMBASE, LILACS, and the Cochrane Central Register of Controlled Trials.
Selection criteria
Studies were eligible for inclusion if they were trials comparing different techniques for the treatment of simple elbow dislocations.
Data analysis
Results were expressed as relative risk for dichotomous outcomes and weighted mean difference for continuous outcomes with 95% confidence intervals.
Main results
This review has included data from two trials and three observational comparative studies. Important data were missing from three observational comparative studies and the results from these studies were extracted for this review. No difference was found between surgical treatment of the collateral ligaments and plaster immobilisation of the elbow joint. Better range of movement, less pain, better functional scores, shorter disability and shorter treatment time were seen after functional treatment versus plaster immobilisation.
Keywords: Elbow, Elbow joint, Dislocation, Review, Therapy
Introduction
The elbow joint is the second most commonly dislocated joint in adults. The annual incidence of simple and complex elbow dislocations in children and adults is 6.1 per 100,000 [1]. Elbow dislocations are classified as simple or complex types [2]. The simple dislocation is characterised by the absence of fractures, while the complex dislocation is associated with fractures. The terrible triad is an example of a complex posterior dislocation with intra-articular fractures of the radial head and coronoid process. The annual incidence of complex elbow dislocations in children and adults is 1.6 per 100,000, or 26% percent of all elbow dislocations [1]. Conn et al. [3] found 414 injuries of the elbow in their fracture service, including 58 elbow dislocations in children and adults. Elbow injuries accounted for 6.8% of all treated fractures. Seventy-six percent of the patients with elbow dislocations were older than 20 years. In 51% of these adults, the dislocations were simple, a lower percentage than the 74% found in Josefsson’s study [1]. Elbow dislocations can also be classified by the direction of their displacement. Nearly all the dislocations are of the posterior or posterolateral types. In Conn’s study, 96% of the dislocations were posterior or lateral [3] and Joseffson reported no anterior dislocations in his study of 52 patients [4]. In 58% of patients, the simple elbow dislocations were on the non-dominant side [4]. Following reposition and treatment in plaster of simple dislocations, recurrent dislocations and chronic instability are not or only rarely seen [2]. For instance in Joseffson’s study an obviously unstable joint was seen in his study of 52 patients after a mean follow-up of 24 years [4]. After reposition of the simple dislocation, treatment options include immobilisation in a static plaster for different periods, surgical treatment of the ruptured medial and lateral collateral ligaments or so-called functional treatment, which is characterised by early active movements within the limits of pain with or without the use of a sling, hinged brace or functional plaster. In theory, after repositioning of a simple dislocated elbow, the joint retains an inherent stability caused by the contour of the intact joint surfaces. This stability may allow the patient to exercise the joint shortly after the reposition. This functional treatment should prevent stiffness or restricted range of motion without risking increased joint instability.
The primary objective of this systematic review of the literature was to identify if functional treatment is the best available treatment for simple elbow dislocations after closed reduction.
Materials and methods
We conducted an electronic search including MEDLINE, EMBASE, LILACS and the Cochrane Central Register of Controlled Trials (CENTRAL). We did not limit the search by language or publication date. We used the following search terms in different combinations as MeSH (Medical Subject Heading) terms and as text words: elbow joint, dislocation, treatment outcome, surgery, controlled clinical trial, comparative study. Manual searches including reference lists of all included studies were used to identify trials that the electronic search may have failed to identify.
Two reviewers independently assessed the titles and abstracts of all reports identified by electronic and manual searches. Each report was labelled as (a) definitely exclude, (b) unsure or (c) definitely include. Full text articles of abstracts labelled as “unsure” were reassessed according to the inclusion criteria for this review. Any differences were resolved through discussion. Studies labelled as “definitely exclude” were excluded from the review, while studies labelled as “definitely include” were further assessed for methodological quality.
Two reviewers independently extracted the data for the primary and secondary outcomes and entered the data into data collection forms developed for this purpose. Discrepancies were resolved by discussion. All data were entered into Review Manager [RevMan, (Computer program. Version 5.0. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2008)].
Two reviewers independently assessed the included studies for sources of systematic bias in trials. The studies were evaluated with the following criteria: allocation concealment (selection bias), rates of follow-up and intention to treat analysis (attrition bias). Allocation concealment was graded as (a) adequate, (b) inadequate or (c) unsure. Differences between the two reviewers were resolved by discussion. Masking of outcome assessors in the included studies was assessed.
Dichotomous outcomes (e.g., presence/absence of normal extension) were reported as proportions and were directly compared (difference in proportions). We used these proportions to calculate risk ratios (RRs) and absolute risk reductions (risk differences) with 95% confidence intervals (CIs). For continuous data (e.g., range of motions, function scores) results are presented as weighted mean differences (WMD). We used Review Manager 5.0 software (RevMan 5.0, Cochrane software) for generating the figures and statistical analyses. We explored heterogeneity using the chi-squared test with significance set at a P value less than 0.10. The quantity of heterogeneity was estimated by the I-squared statistic.
Because prior statistical evidence existed for homogeneity of effect sizes, the planned analysis used a fixed effect model.
Results
A total of two randomised controlled trials (RCTs) and six observational comparative studies comparing different treatments for elbow dislocations were included with a total enrolment of 342 patients with available follow-up (see Tables 1, 2, 3, 4, 5, 6, 7 and 8 for characteristics of the included studies). The full text of every study was retrieved.
Table 1.
Characteristics of the study of Josefsson et al. [6]
| Methods | Randomised controlled trial |
| Participants | 30 consecutive patients included, acute dislocation of the elbow, age ≥16 years, mean age 34.5 years, free from elbow symptoms before injury. Dislocation with fracture excluded except small avulsed fragments <2 × 3 mm, 10 males, 20 females, 18 dislocations left, 12 dislocations right side, 28 posterior or posterolateral and 2 lateral dislocations. Reduction in emergency room. Examination under general anaesthesia after mean of 4 days for examination stability: all elbows medial instability and 16 lateral instability. N = 11 re-dislocated easily, most often in 45° of flexion |
| Interventions | Surgical treatment: N = 15, exploration medial and lateral side joint through separate incisions. Medial and lateral collateral ligaments found to be totally ruptured, although only 8 showed lateral instability. Suturing and re-fixation of ligaments. 6 of the 11 easily re-dislocated elbows treated surgically. Immobilisation in plaster, 90°, 19 days (SD = 3). 1 patient in this group lost to follow-up |
| Non-surgical treatment: N = 15, 5 of the 11 easily re-dislocated elbows treated non-surgically. Immobilisation 17 days (SD = 2). 1 patient in this group lost to follow-up | |
| Outcomes | Follow-up surgical group 31 months (SD = 15), non surgical 24 months (SD = 11). Range of motions at 5, 10 weeks and final examination >1 year: no difference in motion, grip strength, pain, instability |
| Loss of extension >1 year: surgical group 18° (SD = 15) and non-surgical group 10° (SD = 14) | |
| Loss of flexion >1 year: surgical group 1° (SD = 2) and non-surgical group 1° (SD = 2) | |
| For unstable elbows (N = 11 of which 6 were treated surgically) the loss of extension >1 year was 20° (SD = 19), and loss of flexion was 2° (SD = 3) | |
| No recurrent dislocations or episodes of instability in both groups | |
| Allocation concealment | Random selection by 30 sealed envelopes, 15 envelopes for surgical treatment and 15 for non-surgical treatment |
Table 2.
Characteristics of the study of Rafai et al. [7]
| Methods | Randomised controlled trial |
| Participants | 50 pure posterior luxations, adults, normal psychological profile, stable after reposition and tested under general anaesthesia, no previous elbow injury. Mean age 25 years (range 16–67 years), 43 males, 7 females, 30 right arm, 20 left arm |
| Interventions | Group I: N = 26, reduction in general anaesthesia and testing stability. Immobilisation for 3 weeks |
| Group II: N = 24, reduction in general anaesthesia and testing stability. Mobilisation after 3 days. Functional treatment | |
| Outcomes | Normal extension: group I 81% and group II 96% (statistically significant difference concluded by authors) |
| Stiffness (=loss of flexion): group I = 19% and group II = 4% (statistically significant difference concluded by authors) | |
| No difference in pain and ossifications | |
| No recurrent dislocations or episodes of instability in both groups | |
| Notes | No P values are given, but only remarks declaring significant results |
| Allocation concealment | No details about randomisation |
Table 3.
Characteristics of the study of Royle [5]
| Methods | Retrospective, observational study with 2 comparative groups with mean follow-up of 31 months |
| Participants | N = 38, follow-up of N = 32, period 1982–1987, mean age 35.8 years, 17 males (53%), 15 females (47%), N = 23 (72%) posterolateral dislocation, N = 9 (28%) posterior, N = 20 (62%) associated fractures: N = 12 radial head, N = 6 coronoid, N = 4 olecranon avulsion fracture, N = 4 medial epicondyle, N = 1 lateral condyle, N = 1 capitellum, average time for reduction 3.8 h, general anaesthesia N = 27 (84%), N = 1 internal fixation radial head fracture, instability after reduction N = 8 (tested in extension with valgus stress) |
| Interventions | Group I: N = 9, closed reduction and plaster, mean duration 24.7 days |
| Group II: N = 23, reduction and sling, mean 17.5 days | |
| Outcomes | Group I excellent (no pain and full extension) or good (minimal pain and extension loss <15°) in 33.3 versus 83% in group II. Results were graded according to Lindscheid and Wheeler |
| No recurrent dislocations | |
| Notes | Age range 11–75 years; thus included children, also associated fractures N = 20 (62%) |
| Posterior dislocation 100% good/excellent result versus N = 18 (56%) posterolateral dislocation | |
| Better outcome if reduction <3 h, 87 versus 53% good/excellent result | |
| Associated fractures N = 8 (40%) fair (exertional pain and 15–30° extension loss) or poor (constant pain and >30° extension loss) versus N = 2 (17%) without fractures | |
| The results of group I versus group II could be confounded by associated fractures, time of reduction and direction of dislocation | |
| Bias | Heterogeneity of groups, children included, confounded by associated fractures, time of reduction and direction of dislocation |
Table 4.
Characteristics of the study of Maripuri et al. [8]
| Methods | Observational retrospective comparative study |
| Participants | 47 simple elbow dislocations in period 2000–2004, mean age 42.5 years, follow-up >2 years, N = 42 available for review. Inclusion criteria: age ≥16 years, simple dislocation, closed reduction, concentric relocation confirmed by radiography, follow-up >2 years, no associated fractures, no neurovascular deficit. Posterolateral dislocation 60%, direct posterior 30%, posteromedial 10% |
| Interventions | Group I: N = 20, plaster immobilisation, mean 14 days followed by physiotherapy until range of motions (ROM) 100° |
| Group II: N = 22, sling application and early mobilisation within pain limits | |
| Outcomes | Group I: mean score Mayo Elbow Performance Index (MEPI) 83.8 (SEM = 4.2, SD = 18.8). Group II: mean score MEPI 96.5 (SEM = 8.9, SD = 8.9), P < 0.05. MEPI score components are pain, ROM, stability, daily function, which are graded as excellent 90–100, good 75–89, fair 60–74, poor <60 |
| Group I: mean score Quick Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire 12.8 (SEM = 3.5, SD = 15.7). Group II: mean score DASH 2.7 (SEM = 1.5, SD = 7.0), P < 0.05. Of the DASH the disability and symptom section was used | |
| Weeks off work: group I mean 6.6 weeks (SEM = 0.64, SD = 2.86); group II 3.2 weeks (SEM = 0.29, SD = 1.36), P < 0.001 | |
| 20 patients (of 22) with excellent or good result in group II (depends on MEPI score). 12 patients (of 20) with excellent or good result in group I (depends on MEPI score) | |
| One recurrent dislocation in group I, treated surgically | |
| Notes | Period of immobilisation depended on preference of the treating doctor |
| Allocation concealment | Retrospective study |
| Bias | Selection bias for therapy, attending physician decides, instability, time period, for co-interventions: only 50% of group 1 received physiotherapy at 2 weeks versus 100% of group II |
Table 5.
Characteristics of the study of Riel et al. [9]
| Methods | Observational retrospective comparative study with a historical control group. Mean follow-up 8.2 (SD = 4.5) years |
| Participants | In period 1976–1992 50 simple elbow dislocations, N = 6 treated surgically, N = 44 conservatively, last group re-examined. Reduction without anaesthesia (N = 31) or in local anaesthesia |
| Interventions | Group I: period 1976–1985, N = 20, reduction and immobilisation in plaster for 3–4 weeks, N = 17 patients re-examined, N = 1 telephone enquiry, follow-up 11 (SD = 2.6) years, mean plaster period 24 (SD = 3) days plus data from medical records, last examination after a mean of 6 months |
| Group II: period 1985–1992, N = 24, reduction and functional treatment day after reposition, N = 18 patients re-examined, N = 3 telephone enquiry, follow-up 4 (SD = 1.8) years, mean plaster period 2 (SD = 1) days plus data from medical records, last examination after a mean of 4 months | |
| Outcomes | Range of motions, stability and power not different between groups |
| After-treatment period group I 12 (SD = 3) weeks, group II 8 (SD = 3) weeks, disability period group I 16 (SD = 8) weeks, group II 8 (SD = 3) weeks, physical rehabilitation period group I 6 (SD = 3) months, group II 4 (SD = 3) months | |
| Notes | Sex had no influence on result. No recurrent dislocations |
| Allocation concealment | No RCT, observational comparative study with a historical control group |
Table 6.
Characteristics of the study of Protzmann [11]
| Methods | Retrospective observational study with 3 comparative groups, mean follow-up 24.5 months |
| Participants | 49 consecutive patients, military service, 1971–1976, from N = 47 follow-up, range age 17–44 years, N = 15 associated fractures of which 1 radial head fracture and one coronoid process (=only one which could influence stability). From N = 25 X-ray: 19 posterolateral, 5 posterior, 1 posteromedial, no anterior dislocation |
| Interventions | Closed reduction without anaesthesia and group I immobilisation <5 days, N = 27; group II immobilisation 10–15 days, N = 13; group III immobilisation >20 days, N = 7 |
| Outcomes | Mean extension loss group I = 3°, group II = 11°, group III = 21°. Mean duration disability group I = 6 weeks, group II = 19 weeks, group III = 24 weeks. No SD given |
| Notes | No standard deviations given for outcome measures. No recurrent dislocations and no subjective complaints of instability. 28 patients of the 47 with follow-up had periarticular or ligamentous calcifications |
| Allocation concealment | No RCT, observational study, probably retrospective, comparative study, comparison = post-hoc, immobilisation period was decision of orthopaedic surgeon |
| Bias | Selection bias for therapy, treating doctor decided |
Table 7.
Characteristics of the study of Mehlhoff et al. [10]
| Methods | Observational retrospective comparative study with 3 comparative groups, mean follow-up 34.3 months |
| Participants | 90 consecutive patients, adults, simple dislocations, follow-up >12 months, age >18 years, no associated fractures. Stable after reduction. Period 1978–1985, follow-up from N = 52 (56% follow-up), N = 34 males, N = 18 females. Dislocations: 90% posterolateral + posterior, 10% posteromedial + medial |
| Interventions | Closed reduction, after reduction stability and ROM were tested and gravity stress photos were taken. Group I immobilisation 0–13 days; group II immobilisation 14–24 days; group III immobilisation ≥25 days |
| Outcomes | Ratings extension loss: <5° excellent, <15° good, <30° fair, ≥30° poor |
| Groups divided according to immobilisation period: Group I 0–13 days. Group II 14–24 days, Group III >24 days | |
| Mean flexion contracture = loss of extension: group I: 5.1°; group III 30.1°; loss of flexion: group I 2.7°, group II 5.6°, group III 18.6°. Pain (McGill Pain Questionnaire): group I 80% no pain, group II 45% no pain, group III 10% no pain | |
| Instability non significant. No sample sizes of the groups and no SDs for the outcome measures are presented | |
| No gross instability of the elbow or recurrent dislocation | |
| Notes | No correlation between age, sex or length of follow-up and flexion contracture, pain or instability (Chi-square test, multiple testing) |
| Heterotopic ossification was seen in 55% of the radiographs, but there was no correlation with impairment of motion | |
| Allocation concealment | No RCT, observational study, probably not prospective, comparative study, groups were formed post-hoc |
| Bias | Selection bias, 31 of 84 patients did not participate, selection bias for therapy, treating doctor decided |
Table 8.
Characteristics of the study of Schippinger et al. [12]
| Methods | Retrospective observational study with comparative groups (post hoc). Mean follow-up 61.5 (SD = 22.2) months |
| Participants | 45 simple elbow dislocations, no or minor fractures (<2 × 3 mm), 2 trauma centres, period 1989–1995, N = 27 posterior, N = 12 posterolateral, N = 2 bilateral posterior, N = 1 medial, N = 1 anterior, N = 1 divergent, N = 1 anterolateral dislocation, age 44.5 years (SD = 15.9) |
| Interventions | Closed reduction without general anaesthesia. Check for re-dislocation in various flexion positions. Group I immobilisation <2 weeks; group II immobilisation 2–3 weeks; group III immobilisation >3 weeks |
| Outcomes | Morrey scores and pain group I and II better than group III, but nonsignificant. Number of groups and scores of groups not given |
| N = 28 periarticular ossifications and N = 11 heterotopic calcifications, but no correlation of ossifications with impairment of motion | |
| No recurrent dislocations | |
| Notes | Period of immobilisation was dependent on preference of the orthopaedic surgeon |
| Allocation concealment | No RCT, observational study, retrospective, comparative study, groups were formed post hoc, immobilisation period was decision of orthopaedic surgeon |
Because only two RCTs were retrieved we expanded the review with observational comparative studies. Non-comparative observational studies were excluded. All studies included simple elbow dislocations. One study consisted of patients with simple and complex elbow dislocations [5]. No RCTs or comparative studies of complex elbow dislocations were retrieved.
One RCT comparing surgical and non-surgical treatment of simple elbow dislocation was included [6]. The other RCT compared functional treatment with immobilisation in plaster during 3 weeks [7]. The observational comparative studies compared functional treatment with immobilisation in plaster [5, 8, 9] or compared different periods of immobilisation [10–12].
Observational studies that did not compare different treatments were excluded because they provide a low level of evidence (level IV evidence, no control group).
In Josefsson’s study [6] random selection was by the use of sealed envelopes, but in Rafai’s study [7] no information on randomisation was published. In the observational studies from Schippinger [12] and Maripuri [8] the period of immobilisation, and thus the treatment allocation, was dependent on the preference of the treating doctor.
Since blinding of treatment is difficult or impossible in surgical treatments, the RCTs did not blind doctors or patients to treatment. No information is provided about blinding of the evaluators of the outcomes.
In the observational studies of Protzman [11] and Mehlhoff [10] no standard deviations of the outcome measures are given and in the study of Mehlhoff [10] the sample sizes of the treatment groups are also not provided. In Schippinger’s study [12] the sample sizes and outcome scores of the three groups with different immobilisation periods are not provided.
In the observational studies of Schippinger [12] and Maripuri [8] the period of immobilisation was dependent on the treating doctor and was most likely biased by the severity of the trauma so that the patients with the most severe trauma received the longest period of immobilisation.
The results were expressed as relative risk (RR) for dichotomous outcomes and weighted mean difference (WMD) for continuous outcomes with 95% confidence intervals (CI).
Only data from two observational studies comparing functional treatment with plaster immobilisation could be pooled [5, 8]. The percentages of excellent or good results were pooled with the Mantel-Haenszel statistical method. For this pooling, the fixed effects model was used since we assumed that all variation between the two studies was caused by chance and that the studies measured the same overall effect. Even if a random-effects model was used, our conclusions remained the same. Data from the other studies that compared different types of treatment and used different outcome measures could not be pooled due to clinical and methodological heterogeneity, and thus are described individually.
Surgical versus non-surgical treatment of simple elbow dislocations
Only one RCT was found that compared surgical with non-surgical treatment [6] (Table 9). At more than 1 year the loss of extension (Comparison 1.1: WMD 8.00, 95% CI −2.75 to 18.75; P = 0.14) and loss of flexion (Comparison 1.2: WMD 0.00, 95% CI −1.48 to 1.48; P = 1.00) were not statistically different between the two groups. Furthermore, at 10 weeks the loss of extension (Comparison 1.3: WMD 11.00, 95% CI −4.19 to 26.19; P = 0.16) and loss of flexion (Comparison 1.4: WMD 6.00, 95% CI −0.11 to 12.11; P = 0.05) were not statistically different. Moreover, at 5 weeks the loss of extension (Comparison 1.5: WMD 11.00, 95% CI −4.93 to 26.93; P = 0.18) and loss of flexion (Comparison 1.6: WMD 9.00, 95% CI −0.88 to 18.88; P = 0.07) were not statistically different. A post hoc power calculation on the mean loss of extension after 1 year with G*Power software (version 3.03, Kiel, Germany) showed a power of 29%.
Table 9.
Surgical versus non-surgical treatment of simple elbow dislocation
| Outcome | Studies | Participants | Statistical method | Effect estimate |
|---|---|---|---|---|
| 1.1 Loss of extension at more than 1 year | 1 | 28 | Mean difference (IV, fixed, 95% CI) | 8.00 [−2.75, 18.75] |
| 1.2 Loss of flexion at more than 1 year | 1 | 28 | Mean difference (IV, fixed, 95% CI) | 0.00 [−1.48, 1.48] |
| 1.3 Loss of extension at 10 weeks | 1 | 28 | Mean difference (IV, fixed, 95% CI) | 11.00 [−4.19, 26.19] |
| 1.4 Loss of flexion at 10 weeks | 1 | 28 | Mean difference (IV, fixed, 95% CI) | 6.00 [−0.11, 12.11] |
| 1.5 Loss of extension at 5 weeks | 1 | 28 | Mean difference (IV, fixed, 95% CI) | 11.00 [−4.93, 26.93] |
| 1.6 Loss of flexion at 5 weeks | 1 | 28 | Mean difference (IV, fixed, 95% CI) | 9.00 [−0.88, 18.88] |
IV inverse variance; CI confidence interval
Functional treatment versus plaster treatment
One RCT and three observational studies are described (Table 10). The results of the RCT are described individually [7]. The percentages of normal extension (Comparison 2.1: RR 1.19, 95% CI 0.97–1.46; P = 0.10) and flexion (Comparison 2.3: RR 1.19, 95% CI 0.97–1.46; P = 0.10) and pronation and supination (Comparison 2.5: RR 1.25, 95% CI 0.99–1.56; P = 0.06) at 1 year and normal flexion (Comparison 2.4: RR 1.25, 95% CI 0.99–1.56; P = 0.06) at 3 months were not statistically different. The percentage of normal extension (Comparison 2.2: RR 1.78, 95% CI 1.23–2.57; P = 0.002) at 3 months was statistically higher in the functional treatment group. A post hoc power calculation on the percentages of normal extension and flexion at 1 year with G*Power software (version 3.03, Kiel, Germany) showed a power of 19%.
Table 10.
Functional treatment versus plaster immobilisation
| Outcome | Studies | Participants | Statistical method | Effect estimate |
|---|---|---|---|---|
| 2.1 Percentage of patients with normal extension at 1 year | 1 | 50 | Risk ratio (M-H, fixed, 95% CI) | 1.19 [0.97, 1.46] |
| 2.2 Percentage of patients with normal extension at 3 months | 1 | 50 | Risk ratio (M-H, fixed, 95% CI) | 1.78 [1.23, 2.57] |
| 2.3 Percentage of patients with normal flexion at 1 year | 1 | 50 | Risk ratio (M-H, fixed, 95% CI) | 1.19 [0.97, 1.46] |
| 2.4 Percentage of patients with normal flexion at 3 months | 1 | 50 | Risk ratio (M-H, fixed, 95% CI) | 1.25 [0.99, 1.56] |
| 2.5 Percentage of patients with normal pro- and supination at 1 year | 1 | 50 | Risk ratio (M-H, fixed, 95% CI) | 1.25 [0.99, 1.56] |
| 2.6 Percentage patients with excellent or good results at >2 years | 2 | 74 | Risk ratio (M-H, fixed, 95% CI) | 1.76 [1.19, 2.60] |
| 2.7 Mayo Elbow Performance Index (MEPI) | 1 | 42 | Mean difference (IV, fixed, 95% CI) | 12.70 [3.66, 21.74] |
| 2.8 Quick Disabilities of the Arm, Shoulder and Hand (DASH) | 1 | 42 | Mean difference (IV, fixed, 95% CI) | −10.10 [−17.58, −2.62] |
| 2.9 Weeks off work | 1 | 42 | Mean difference (IV, fixed, 95% CI) | −3.40 [−4.78, −2.02] |
| 2.10 Physiotherapy time (weeks) | 1 | 44 | Mean difference (IV, fixed, 95% CI) | −4.00 [−5.78, −2.22] |
| 2.11 Period disability (weeks) | 1 | 44 | Mean difference (IV, fixed, 95% CI) | −8.00 [−11.71, −4.29] |
| 2.12 After-treatment time (months) | 1 | 44 | Mean difference (IV, fixed, 95% CI) | −2.00 [−3.78, −0.22] |
M-H Mantel-Haenszel statistical method; CI confidence interval; IV inverse variance
Data from two studies could be pooled to analyse the percentage of excellent and good outcomes (Fig. 1) [5, 8]. At a follow-up time greater than 2 years, there was a significant difference between functional and plaster treatment for the outcome excellent and good results (Comparison 2.6: RR 1.76, 95% CI 1.19–2.60; P = 0.004). The other outcome measures of Maripuri [8] study are described individually. Several other measures were statistically different: the mean differences of the Mayo Elbow Performance Index (MEPI) (Comparison 2.7: WMD 12.70, 95% CI 3.66–21.74; P = 0.006), short Quick Disabilities of the Arm, Shoulder and Hand (Comparison 2.8: WMD −10.10, 95% CI −17.58 to −2.62; P = 0.008) and weeks off work (Comparison 2.9: WMD −3.40, 95% CI −4.78 to −2.02; P < 0.0001) all suggested better results following functional treatment. MEPI is one of the most commonly used physician-based elbow rating systems. This index consists of four parts: pain (with a maximum score of 45 points), ulnohumeral motion (20 points), stability (10 points) and the ability to perform five functional tasks (25 points). The DASH disability/symptom score is a summation of the responses to 11 questions on a scale of 1–5, with 0 (no disability) to 100 (severe disability).
Fig. 1.
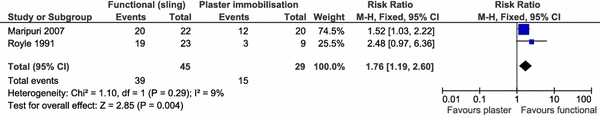
Forest plot comparing functional treatment (sling) and plaster immobilisation for the percentage of excellent or good results
The results of the observational study of Riel [9] are described individually. The physiotherapy time in weeks (Comparison 2.10: WMD −4.00, 95% CI −5.78 to −2.22; P < 0.0001), disability period in weeks (Comparison 2.11: WMD −8.00, 95% CI −11.71 to −4.29; P < 0.0001) and after-treatment time in months (Comparison 2.12: WMD −2.00, 95% CI −3.78 to −0.22; P = 0.03) were statistically significant shorter in the functional group.
Different periods of plaster immobilisation
The results of the observational studies [10–12] comparing different periods of plaster immobilisation could not be expressed as RR or WMD because data (sample sizes of the groups or scores and/or standard deviations) were missing. Thus, we could not judge the following conclusions made by the authors of the studies. Without making statistical inferences, Protzman [11] describes less extension loss and shorter mean disability in weeks for the shorter immobilisation group. Mehlhoff [10] describes less extension loss for the two shorter immobilisation groups (group I 0–13 days, group II 14–24 days), with a significant correlation between extension loss and duration of follow-up (P = 0.001). He also reported less flexion loss and less prevalence and severity of pain for the shorter immobilisation groups but did not analyse this data statistically. The number of patients with symptoms of instability of the elbow joints increased from the shorter immobilisation group to the longer immobilisation groups without reaching statistical significance at the 5% level. Schippinger [12] saw better Morrey scores, which are composed of the items pain, movement, strength, instability and function (activities of daily living), and better separate pain scores in the shorter immobilisation groups, though without statistical significance.
Stability testing of the elbow joint after reposition
Do the above results differ for stable or instable elbow joints after reduction? Nearly all cited studies only included stable joints after reduction. An exception is the study of Josefsson et al. [6]. In this study, the elbows were tested for instability after reduction in general anaesthesia and compared with the other elbow in full but unforced extension. All the elbows showed medial instability and 16 of 30 elbows showed lateral instability. Eleven elbows re-dislocated easily. Royle’s [5] study also included unstable elbow joints. The elbows were tested mainly in general anaesthesia in extension with valgus stress and eight of the 38 elbows showed instability. Mehlhoff et al. [10] and Schippinger et al. [12] tested for instability and did not include unstable elbows. Maripuri et al. [8], Riel et al. [9] and Protzman et al. [11] did not test the elbows for instability. We carefully conclude that the majority of the patients, included in these studies, had simple dislocations, which remained stable after reposition.
Discussion
This review has included data from two trials and three observational comparative studies. Important data were missing from three observational comparative studies and the results from these studies were extracted for this review.
Only one RCT assessed suture repair of the collateral ligaments of the elbow joint versus conservative treatment with plaster [6]. No statistically significant differences were found either for loss of extension at 5 weeks, 10 weeks or after more than 1 year, or for loss of flexion after more than 1 year. A trend was found for less loss of flexion at 5 and 10 weeks for the conservative group. This study lacked the power to find a significant difference because of its small sample size.
Only one RCT compared functional treatment and plaster [7]. The percentages of patients with normal extension and flexion at 1 year were not statistically different. A significantly higher percentage of patients with normal extension at 3 months was found for the group with functional treatment. A trend was found for a higher percentage of patients with normal flexion at 3 months and normal pro- and supination at 1 year for the functional treatment group. This study also lacked the power to find a significant difference because of its small sample size. An important shortcoming of this study is that it did not describe the randomisation process, so allocation bias cannot be excluded.
To analyse the percentage of patients with excellent or good results at more than 2 years following either functional treatment or plaster immobilisation, two observational comparative studies were pooled [5, 8]. This classification of excellent or good depends on the amount of pain and range of movement. The results favoured the functional group. This functional treatment after the reposition consisted of early mobilisation in a sling without a plaster or brace.
For the outcome measures MEPI score, quick DASH score and weeks of work we used an individual observational study. Functional treatment resulted in significantly better outcomes. In addition, an individual observational study showed that patients in the functional group needed less time for physiotherapy and after-treatment and had a shorter disability period. Importantly, since treatment allocation was determined by the attending physician in these observational studies, it is likely that severe cases were prescribed longer immobilisation. In one study, outcome was in fact correlated with the presence of fractures, delay to reduction, and direction of dislocation [5]. Any of these variables could be a confounding factor in analysing the effect of treatment in study, as the heterogeneity could be introduced by combining patients with simple and complex dislocations.
Data from the studies comparing different periods of plaster immobilisation could not be extracted, while the authors of all three observational studies observed less movement loss after shorter immobilisations, but this finding was only statistically significant in one study. These studies could also be confounded by the severance of the injury, as worse cases probably underwent longer immobilisation periods.
In the eight included studies only one recurrent dislocation after treatment was mentioned [8] i.e., one recurrence on 342 patients (0.3%). No subjective or gross objective signs of instability were found after treatment, indicating that recurrent dislocations and instability are not a problem after simple posterior dislocations. The majority of the patients (323 out of 342 patients) probably had a stable elbow joint after reduction of the dislocation, although it was not clear in three studies if the patients were tested for instability.
Summary of main results
No difference was found between surgical treatment of the collateral ligaments and plaster immobilisation of the elbow joint. Better range of movement, less pain, better functional scores, shorter disability and shorter treatment time were seen after functional treatment versus plaster immobilisation. Since we did not find any RCTs or comparative studies that studied complex elbow dislocations, our conclusions can only address simple elbow dislocations. Our conclusions only apply to stable elbow joints after reduction.
The quality of the evidence is very low because of the lack of high-quality RCTs. Moreover, the available RCTs lack power due to their small sample sizes. The observational studies could be biased by confounding due to the use of a historical control group or treatment allocation by the treating physician rather than by randomisation. In addition, the treatment groups were not balanced for important potential confounders, and some observational studies did not provide important data as sample size and/or standard deviations.
Since we did not find any RCTs or comparative studies that studied complex elbow dislocations, our conclusions can only address simple elbow dislocations, which are considered stable after reposition.
We advise to test the elbow after reposition for instability by valgus and varus testing and by the lateral pivot-shift test [13]. When the elbow is considered stable one may consider functional after treatment with a pressure bandage. When plaster immobilisation is preferred to treat simple elbow dislocations one has to realise that immobilisation of more than 14 days may be associated with stiffness.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Josefsson PO, Nilsson BE. Incidence of elbow dislocation. Acta Orthop Scand. 1986;57(6):537–538. doi: 10.3109/17453678609014788. [DOI] [PubMed] [Google Scholar]
- 2.Hildebrand KA, Patterson SD, King GJ. Acute elbow dislocations: simple and complex. Orthop Clin North Am. 1999;30(1):63–79. doi: 10.1016/S0030-5898(05)70061-4. [DOI] [PubMed] [Google Scholar]
- 3.Conn J, Jr, Wade PA. Injuries of the elbow: a ten year review. J Trauma. 1961;1:248–268. doi: 10.1097/00005373-196105000-00004. [DOI] [Google Scholar]
- 4.Josefsson PO, Johnell O, Gentz CF. Long-term sequelae of simple dislocation of the elbow. J Bone Joint Surg Am. 1984;66(6):927–930. doi: 10.2106/00004623-198466060-00014. [DOI] [PubMed] [Google Scholar]
- 5.Royle SG (1991) Posterior dislocation of the elbow. Clin Orthop Relat Res 269:201–204 [PubMed]
- 6.Josefsson PO, Gentz CF, Johnell O, et al. Surgical versus non-surgical treatment of ligamentous injuries following dislocation of the elbow joint. A prospective randomized study. J Bone Joint Surg Am. 1987;69(4):605–608. [PubMed] [Google Scholar]
- 7.Rafai M, Largab A, Cohen D, et al. Pure posterior luxation of the elbow in adults: immobilization or early mobilization. A randomized prospective study of 50 cases. Chir Main. 1999;18(4):272–278. [PubMed] [Google Scholar]
- 8.Maripuri SN, Debnath UK, Rao P, et al. Simple elbow dislocation among adults: a comparative study of two different methods of treatment. Injury. 2007;38(11):1254–1258. doi: 10.1016/j.injury.2007.02.040. [DOI] [PubMed] [Google Scholar]
- 9.Riel KA, Bernett P. Simple elbow dislocation. Comparison of long-term results after immobilization and functional treatment. Unfallchirurg. 1993;96(10):529–533. [PubMed] [Google Scholar]
- 10.Mehlhoff TL, Noble PC, Bennett JB, et al. Simple dislocation of the elbow in the adult. Results after closed treatment. J Bone Joint Surg. 1988;70(2):244–249. [PubMed] [Google Scholar]
- 11.Protzman RR (1978) Dislocation of the elbow joint. J Bone Joint Surg Am 60 (4):539–541 [PubMed]
- 12.Schippinger G, Seibert FJ, Steinbock J, et al. Management of simple elbow dislocations. Does the period of immobilization affect the eventual results? Langenbecks Arch Surg. 1999;384(3):294–297. doi: 10.1007/s004230050206. [DOI] [PubMed] [Google Scholar]
- 13.O’Driscoll SW, Jupiter JB, King GJ, et al. The unstable elbow. Instr Course Lect. 2001;50:89–102. [PubMed] [Google Scholar]


