Abstract
This article presents a brief review of the 2007 World Health Organization classification of tumours of the central nervous system.
Keywords: Brain tumours, WHO classification
Introduction
The World Health Organization (WHO) published the first international classification of human tumours in 1957. Published editions of the classification of brain tumours are based on the consensus of an international expert Working Group. The 1st edition of the WHO Blue Book was published in 1979[1], the 2nd edition was published 1993[2], the 3rd edition in 2000[3]. The most recent edition (the 4th edition) was published in 2007[4–6].
In the 2007 WHO classification of brain tumours there are three categories: (a) clinico-pathological entities; (b) variants of entities; and (c) histological patterns.
A new entity is characterized by:
distinctive morphology
location
age distribution
biological behaviour
New variants have:
reliable identified histologically
relevance for clinical outcome
part of a previously defined entity
Histological patterns have:
identifiable histological appearance
no distinct clinical or pathological significance
New entities
Eight new entities have been included:
angiocentric glioma
atypical choroid plexus papilloma (ACPP)
extraventricular neurocytoma (ENV)
papillary glioneural tumor (PGNT)
rosette-forming glioneural tumor of the 4th ventricle (RGNT)
papillary tumour of the pineal region (PTPG)
pituicytoma
spindle cell oncocytoma of the adenohypophysis (SCO)
Angiocentric glioma
Angiocentric glioma is a cortex-based tumour of childhood and young adults and usually presents with refractory epilepsy. It is a benign neoplasm (Grade I) which can be cured by surgery[7–10].
Atypical choroid plexus papilloma
Atypical choroid plexus papilloma (Grade II) is indistinguishable on imaging from typical plexus papilloma, and has the following characteristics: intermediate features, higher mitotic activity, increased cellular density, and higher recurrence rate.
Extraventricular neurocytoma
Extraventricular neurocytoma is located outside the ventricular system, and has been described in the cerebral hemispheres, pons, cerebellum, spinal cord, cauda equina, retina. It has similar biological behaviour to central neurocytoma. Extraventricular neurocytoma has been described as well-demarcated mass, partly or mainly cystic (50%), variably enhancing, with or without edema.
Papillary glioneuronal tumour
Papillary glioneuronal tumour (PGNT) is a rare tumour with favourable course and is a WHO grade I tumour. It was first introduced in 1998, and was considered a variant of ganglioglioma in the 2000 WHO classification.
Rosette-forming glioneuronal tumour of the IV ventricle
Rosette-forming glioneuronal tumor of the IV ventricle (RGNT) was first described in 1998, a detailed description followed in 2002 (11 cases) and it became a new entity in the 2007 WHO classification. RGNTs are rare, slowly growing neoplasms of the fourth ventricular region preferentially affecting young adults. On magnetic resonance (MR) images, RGNTs are usually seen as a circumscribed mass, which is heterogeneous, partially cystic or even multiloculated with focal and curvilinear, ring, or spot-like enhancement scattered within the lesion. Dense calcifications have also been reported[11].
Papillary tumour of the pineal region
Papillary tumour of the pineal region (PGNT) (WHO grade II/III) arises form the specialized ependyma of the subcommisural organ, has moderate mitotic activity and low vascularity.
Pituicytoma
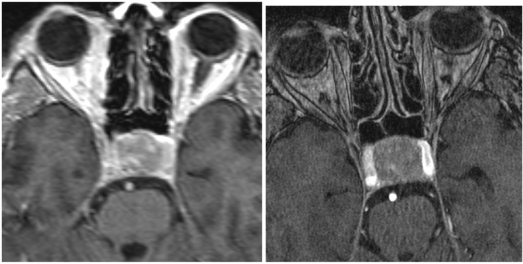
Pituicytoma is a low grade glioma of the neurohypophysis (Fig. 1).
Figure 1.
Surgically proven pituicytoma in a 67-year-old man. MR imaging of the brain shows a well-defined pituitary mass with enhancement, indistinguishable from pituitary adenoma.
Spindle cell oncocytoma of the adenohypophysis
Spindle cell oncocytoma of the adenohypophysis (SCO) is a WHO grade II neoplasm. It is an oncocytic, non-endocrine neoplasm of the anterior pituitary gland and occurs in adults.
New variants
Three new variants have been include in the 2007 WHO classification:
pilomyxoid astrocytoma
anaplastic medulloblastoma
medulloblastoma with extensive nodularity
Pilomyxoid astrocytoma
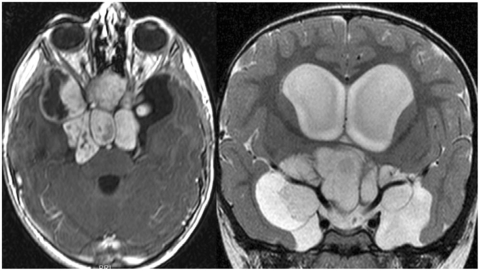
Pilomyxoid astrocytoma (PMA) was first described by Jänisch et al. in 1985. This tumour is neurofibromatosis type 1 (NF1), occurs in infants and children and has a poor prognosis. Fifty percent of PMAs are located in the hypothalamic/chiasmatic region; other locations include the cerebral hemispheres, cerebellum, basal ganglia, and the 4th ventricle region. Approximately 50% have uniform enhancement; in 2% no enhancement was observed. Intratumoral hemorrhage is present in 25% of the cases (Fig. 2).
Figure 2.
MR imaging of a histologically proven pilomyxoid astrocytoma in a 4-year-old boy. MR images of the brain show a markedly enhanced midline mass (hypothalamic region). The mass has high signal on the T2-weighted image, well-defined borders, no vessel involvement, and no perifocal oedema.
Medulloblastoma (MB)
Two new variants of medulloblastoma have been included in the 2007 classification: anaplastic medulloblastoma and medulloblastoma with extensive nodularity (MBEN). Both variants are Grade IV neoplasms. MBEN was previously called ‘cerebellar neuroblastoma’. The extended histological spectrum (currently 4 MB variants are recognized) shows overlapping features on MR imaging when comparing classic MB and MB variants. Certain MR imaging characteristics may favour MB-EN and desmoplastic/nodular MB variants. Anaplastic and large cell MB do not have any distinctive imaging features[12].
References
- 1.Zülch KJ., editor. Histological typing of tumours of the central nervous system. Geneva: World Health Organization; 1979. [Google Scholar]
- 2.Kleihues P, Burger PC, Scheithauer BW. The new WHO classification of brain tumours. Brain Pathol. 1993;3:255–68. doi: 10.1111/j.1750-3639.1993.tb00752.x. doi:10.1111/j.1750-3639.1993.tb00752.x. PMid:8293185. [DOI] [PubMed] [Google Scholar]
- 3.Kleihues P, Cavenee WK., editors. World Health Organization classification of tumours. pathology and genetics of tumours of the nervous system. Lyon: IARC Press; 2000. [Google Scholar]
- 4.Louis DN, Ohgaki H, Weistler OD, Cavenee WK., editors. WHO classification of tumours of the central nervous system. 4th. Lyon: IARC Press; 2007. p. 309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brat DJ, Parisi JE, Kleinschmidt-DeMasters BK, et al. A review of changes introduced by the WHO Classification of Tumours of the Central Nervous System. 4th ed. Arch Pathol Lab Med. 2008;132:993–1007. doi: 10.5858/2008-132-993-SNUARO. [DOI] [PubMed] [Google Scholar]
- 6.Fritz A, et al., editors. ICD-O International classification of diseases for oncology. Geneva: World Health Organization; 2000. [Google Scholar]
- 7.Preusser M, Hoischen A, Novak K, et al. Angiocentric glioma. Report of clinico-pathologic and genetic findings in 8 cases. Am J Surg Pathol. 2007;31:1709–18. doi: 10.1097/PAS.0b013e31804a7ebb. doi:10.1097/PAS.0b013e31804a7ebb. PMid:18059228. [DOI] [PubMed] [Google Scholar]
- 8.Amemiya S, Shibahara J, Aoki S, Takao H, Ohtomo K. Recently established entities of central nervous system tumors: review of radiological findings. J Comput Assist Tomogr. 2008;32:279–85. doi: 10.1097/RCT.0b013e31814ce981. doi:10.1097/RCT.0b013e31814ce981. PMid:18379318. [DOI] [PubMed] [Google Scholar]
- 9.Wang M, Tihan T, Rojiani AM, et al. Monomorphous angiocentric glioma: a distinctive epileptogenic neoplasm with features of infiltrating astrocytoma and ependymoma. J Neuropathol Exp Neurol. 2005;64:875–81. doi: 10.1097/01.jnen.0000182981.02355.10. doi:10.1097/01.jnen.0000182981.02355.10. PMid:16215459. [DOI] [PubMed] [Google Scholar]
- 10.Lellouch-Tubiana A, Boddaert N, Bourgeois M, et al. Angiocentric neuroepithelial tumor (ANET): a new epilepsy-related clinicopathological entity with distinctive MRI. Brain Pathol. 2005;15:281–6. doi: 10.1111/j.1750-3639.2005.tb00112.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Preusser M, Dietrich W, Czech T, Prayer D, Budka H, Hainfellner JA. Rosette-forming glioneuronal tumor of the fourth ventricle. Acta Neuropathol (Berl) 2003;106:506–8. doi: 10.1007/s00401-003-0758-2. [DOI] [PubMed] [Google Scholar]
- 12.Frühwald-Pallamar J, Puchner S, Osborn AG, Thurnher MM. Presented at ASNR 47th Annual Meeting, Vancouver, Canada, May 18–21, 2009. MR imaging features of medulloblastoma (MB) variants. [Google Scholar]