Abstract
Interleukin-11 (IL-11) up-regulates the proliferative and invasive capacity of many cancers. Coexpression of glycoprotein 130 (GP130) and IL-11 receptor α (IL-11Rα) is necessary for high-affinity binding of IL-11 to IL-11Rα. This study investigated the expression of IL-11 and role of prostaglandin F2α-F-prostanoid receptor (FP receptor) signaling in the modulation of IL-11 expression in endometrial adenocarcinoma cells. Localization of IL-11, IL-11Rα, and GP130 expression was performed by immunohistochemistry. IL-11 and regulator of calcineurin 1 isoform 4 (RCAN1-4) mRNA and protein expression were determined by real-time RT-PCR and/or enzyme-linked immunosorbent assay/Western blot analysis using Ishikawa endometrial adenocarcinoma cells stably expressing the FP receptor (FPS cells) and endometrial adenocarcinoma explants. IL-11 mRNA expression was significantly elevated in endometrial adenocarcinoma samples compared with normal endometrium and increased with tumor grade. IL-11 protein expression localized with FP receptor, IL-11Rα, and GP130 in the neoplastic glandular epithelium of endometrial adenocarcinomas. Prostaglandin F2α-FP receptor signaling significantly elevated the expression of IL-11 mRNA and protein in a Gq-protein kinase C-calcium-calcineurin-nuclear factor of activated T cells-dependent manner in FPS cells. The calcineurin signaling pathway is known to be controlled by the RCAN (RCAN1-4). Indeed, RCAN1-4 expression was significantly elevated in well-differentiated endometrial adenocarcinoma compared with normal endometrium and was found to decrease with tumor grade and negatively regulate IL-11 expression in vitro. This study has highlighted a new mechanism regulating IL-11 expression in endometrial adenocarcinoma cells by the FP receptor via the calcium-calcineurin-nuclear factor of activated T cells pathway.
Endometrial cancer is the most common female gynecological malignancy in the Western world, ranking fourth in incidence among invasive tumors in women.1–3 Most cases of endometrial carcinomas are sporadic estrogen-dependent disorders that occur in pre- or postmenopausal women as low-grade (well differentiated, type I) endometrioid adenocarcinomas.4 However, ∼20% of tumors in postmenopausal women are not estrogen dependent and have a poor prognosis.1–4 In these patients, predominantly high-grade (poorly differentiated, type II) tumors arise either as endometrioid adenocarcinomas, uterine papillary serous carcinomas, or clear cell carcinomas with a high frequency of myometrial invasion and spread into the pelvic lymph nodes.5
Although the mechanisms regulating endometrial adenocarcinomas are still poorly defined, there is much evidence for a role for cyclooxygenase (COX) enzymes and prostaglandins (PGs) in uterine pathology. We and others6,7 have demonstrated elevated expression of COX-2, biosynthesis of PG, and elevated expression of nuclear6 and membrane-bound G protein-coupled receptors6,8 like the F-prostanoid (FP) receptor8 in endometrial adenocarcinomas. Moreover, we have shown that elevated PGF2α-FP receptor signaling, via the Gq activation of inositol-1,4,5-trisphosphate, leads to up-regulation of tumorigenic and angiogenic genes including COX-2,9 fibroblast growth factor 2,10 and vascular endothelial growth factor,11 indicating that PGF2α-FP receptor signaling can promote endometrial tumor growth by regulating vascular function. Furthermore, FP receptor can regulate the proliferation of endometrial epithelial cells and can alter their adhesiveness to extracellular matrix and motility via the reorganization of the actin cytoskeleton and activation of focal adhesion kinase.8,12,13 These findings suggest that PGF2α-FP receptor signaling plays a multifactorial role in regulating endometrial adenocarcinoma by promoting an environment for angiogenesis and tissue remodeling to facilitate tumor growth.
In addition to the regulation of cell architecture and growth factors by the COX-PG axis, a link between PG and chemoattractive cytokines (chemokines) such as CXCL1 has been demonstrated in colorectal cancer,14 where PGE2 signaling has been shown to induce CXCL1 expression in colorectal cancer cells to enhance tumor growth. Similarly in COX-2-overexpressing breast cancer cells that had metastasized to bone, Singh et al15 have shown recently that the pleiotropic cytokine interleukin-11 (IL-11) is significantly elevated.15 IL-11 mediates its function via the IL-11 receptor α (IL-11Rα). On ligand binding to IL-11Rα, the glycoprotein (GP) 130 subunit, critical for signal transduction of IL-11, is recruited to form a IL-11/IL-11Rα/GP130 complex.16 Once activated, the IL-11/IL-11Rα/GP130 complex can activate signal transduction pathways17 to modulate target gene expression. IL-11 and IL-11Rα expression has been shown to correlate with cellular growth, differentiation, invasiveness, tumor progression, and poor prognosis in breast and colorectal cancer;18–20 however, the expression and regulation of IL-11 in endometrial cancer has yet to be reported.
Here we investigated the expression profile of IL-11, IL-11Rα, and GP130 in endometrial adenocarcinomas compared with normal proliferative-phase endometrium and its regulation in an in vitro model of endometrial adenocarcinoma cells by PGF2α via the FP receptor.
Materials and Methods
Reagents
YM-254890 was donated by Astellas Pharma (Tsukuba, Japan). Cyclosporin A and Inhibitor of nuclear factor of activated T cells (NFAT)-calcineurin association-6 (Inca-6), 4-cyano-3-methylisoquinoline, and RO-318220 were purchased from Calbiochem (Nottingham, UK). PGF2α, AL8810, and EGTA were purchased from Sigma Chemical (Dorset, UK).
Cell Line, Culture, and Treatments
Ishikawa cells engineered to stably express the full-length human FP (PTGFR, accession no. NM_000959) receptor to the levels observed in endometrial adenocarcinomas, referred to as FPS cells, were cultured as described previously.11 FPS cells were manufactured commercially, clonally selected, and verified as described in our previous study.11 The concentrations of all chemical inhibitors and antibodies were determined empirically by titration using the manufacturer's guidelines as described in our previous studies.21,22 Cell viability in the presence of chemical inhibitor was determined using the CellTitre 96 AQueous One Solution assay (Promega, Southampton, UK) as described previously.22 Cells were treated with 100 nmol/L PGF2α alone or in the presence of AL8810 (50 μmol/L), YM254890 (1 μmol/L), 43CMQ (1 μmol/L), RO-318220 (1 μmol/L), AG1478 (200 nmol/L), cyclosporine A (1 μmol/L), Inca-6 (40 μmol/L), and EGTA (1.5 mmol/L) for the time indicated. In parallel, cells treated with vehicle and chemical inhibitor served as a control for each treatment. Fold increase was calculated by dividing the values obtained from the PGF2α/PGF2α-inhibitor treatments by the vehicle/vehicle-inhibitor treatments. All in vitro cell culture experiments were performed in duplicate.
Human Tissue
Poorly differentiated (grade 3; n = 10), moderately differentiated (grade 2; n = 10), and well-differentiated (grade 1; n = 10) endometrial adenocarcinoma tissues with clinical characteristics as outlined in Table 1 were collected from women undergoing hysterectomy and who had been prediagnosed on endometrial biopsy to have endometrial adenocarcinoma of the uterus of the endometrioid type. The patients had received no treatment before surgery. All patients were postmenopausal women with ages that ranged between 50 and 71 years of age and presented with complaint of postmenopausal bleeding. The median age of all patients in our study was 60.5 years. Total abdominal hysterectomy specimens with bilateral salpingo-oophorectomy for adenocarcinoma were collected from the operating theater and placed on ice. With minimal delay, the specimens were opened by a gynecological pathologist. Small samples (∼5 mm to 3 cm) of polypoidal adenocarcinoma tissue were collected from the endometrial lumen. Tissue samples were transferred into neutral-buffered formalin (for paraffin wax embedding for immunohistochemistry and immunofluorescence studies), snap-frozen in dry ice and stored at −70°C (for RNA extraction), and placed in RPMI 1640 culture medium containing 2 mmol/L l-glutamine, 100 U of penicillin, 100 μg/ml streptomycin, and 8.4 μmol/L indomethacin (to inhibit endogenous COX activity) for ex vivo explant cultures. The diagnosis of endometrial adenocarcinoma was confirmed histologically in all cases as defined in Table 1 and the percentage of tumor cells to stroma was estimated to be not less than 75%:25%. Normal endometrium from the proliferative phase of the menstrual cycle, with clinical parameters as outlined in Table 2 (n = 10), was collected with an endometrial suction curette from women undergoing surgery for gynecological procedures including surgical sterilization or abnormal uterine bleeding in whom histological examination of endometrium was normal with no underlying endometrial pathology (Pipelle, Laboratoire CCD, Paris, France). This phase of the menstrual cycle was chosen as a comparator for the endometrial cancer samples as it exhibits all of the hallmarks of endometrial tumorigenesis, namely low progesterone levels, rapid cellular proliferation, differentiation and tissue remodeling and is the phase of the menstrual cycle with the highest expression of FP receptor.13 All women had regular menstrual cycles (25 to 35 days) and the tissue collected was processed exactly as described above. The ages of the control women ranged from 21 to 39 years of age with a median age of 30.5 years. None of the control women had received a hormonal preparation in the 3 months preceding biopsy collection. Biopsies were dated according to stated last menstrual period and confirmed by histological assessment according to the criteria of Noyes et al.23 Ethical approval was obtained from Lothian Research Ethics Committee, and written informed consent was obtained from all subjects before tissue collection.
Table 1.
Clinical Parameters and Tumor Characteristics for Poorly (Poor, n = 10), Moderately (Mod, n = 10), and Well-Differentiated (Well, n = 10) Endometrial Adenocarcinomas
| Sample no. | Grade | FIGO stage |
|---|---|---|
| 1 | Poor | Ia |
| 2 | Poor | IIIa |
| 3 | Poor | Ib |
| 4 | Poor | Ib |
| 5 | Poor | IIIa |
| 6 | Poor | Ib |
| 7 | Poor | Ib |
| 8 | Poor | IIIa |
| 9 | Poor | IIIa |
| 10 | Poor | IIb* |
| 11 | Mod | Ib |
| 12 | Mod | Ic |
| 13 | Mod | IIb* |
| 14 | Mod | IIIa |
| 15 | Mod | Ic |
| 16 | Mod | Ic |
| 17 | Mod | Ic |
| 18 | Mod | Ia |
| 19 | Mod | Ib |
| 20 | Mod | IIb |
| 21 | Well | Ib |
| 22 | Well | Ib |
| 23 | Well | Ia |
| 24 | Well | Ic |
| 25 | Well | IIIa |
| 26 | Well | Ib |
| 27 | Well | Ib |
| 28 | Well | Ib |
| 29 | Well | Ia |
| 30 | Well | Ia |
All endometrial adenocarcinomas studied were of pure or predominantly of endometrioid type. There were no pure serous or clear cell subtypes in the series, and none of the tumors showed carcinosarcoma.∗ In these two samples myometrial invasion was <50%.
Table 2.
Clinical Parameters for Normal Endometrial Samples from Proliferative-Phase Endometrium (n = 10)
| Sample no. | Histology | Progesterone (nmol/)L | Estradiol (pmol/L) |
|---|---|---|---|
| 1 | Proliferative | 4.26 | 339.38 |
| 2 | Proliferative | 2.22 | 641.37 |
| 3 | Proliferative | 4.62 | 525.00 |
| 4 | Proliferative | 4.57 | 495.00 |
| 5 | Proliferative | 2.82 | 214.00 |
| 6 | Proliferative | 1.78 | 400.00 |
| 7 | Proliferative | 4.80 | 204.00 |
| 8 | Proliferative | 3.12 | 731.00 |
| 9 | Proliferative | 2.32 | 1796.00 |
| 10 | Proliferative | 0.17 | 989.70 |
TaqMan Quantitative RT-PCR
Total RNA was extracted from FPS cells and proliferative-phase endometrium (n = 10; samples 1 to 10 in Table 2), poorly differentiated (n = 10; samples 1 to 10 in Table 1), moderately differentiated (n = 10; samples 11 to 20 in Table 1), and well-differentiated (n = 10; samples 21 to 30 in Table 1) adenocarcinoma tissues using Total RNA Isolation Reagent (Abgene, Epsom, UK), according to the manufacturer's instruction. Tissue lysis was performed using a tissue lyser (Qiagen, Crawley, UK). Quantified RNA samples were reverse transcribed, and quantitative RT-PCR was performed as described before8 using the following primers and probes: IL-11, forward, 5′-CCCAGTTACCCAAGCATCCA-3′, and reverse, 5′-AGACAGAGAACAGGGAATTAAATGTGT-3′, and probe, 5′-FAM-CCCCAGCTCTCAGACAAATCGCCC-3′; IL-11Rα, forward, 5′-CCAGCCAGATCAGCGGTTTA-3′, and reverse, 5′-TGGCTATCAGCTCCTAGGACTGT-3′, and probe, 5′-FAM-CCACCCGCTACCTCACCTCCTACAGG-3′; and GP130, forward, 5′-CTGAATGGGCAACACACAAGTT-3′, and reverse, 5′-CCAGACTTCAATGTTGACAAAATACA-3′, and probe, 5′-FAM-CAAAGCAAAACGTGACACCCCCACC-3′. Primers and data were analyzed and processed using Sequence Detector version 1.6.3 (Applied Biosystems, Warrington, UK). Expression of analyzed genes was normalized to RNA loading for each sample using the 18S ribosomal RNA as an internal standard. Results are expressed either as relative mRNA expression or as fold increase above vehicle-treated cells. Data are presented as mean ± SEM Cell culture experiments were repeated three times in duplicate.
Immunohistochemistry
Immunohistochemistry for IL-11, IL-11Rα, and GP130 was performed using poorly (n = 10; samples 1 to 10 in Table 1), moderately (n = 10; samples 11 to 20 in Table 1), and well-differentiated (n = 10; samples 21 to 30 in Table 1) endometrial adenocarcinomas and proliferative-phase endometrium (n = 10; Table 2) using the Vision Biosystems Bond Immunostaining Robot (Leica Microsystems, Wetzlar, Germany) as described previously.7,8,10 Control sections were incubated with equivalent concentration of normal IgG from host species.
Immunofluorescence and Confocal Laser Microscopy
Colocalization of FP receptor, IL-11Rα, and IL-11 protein expression was investigated using a random selection of tissues from patient samples as outlined in Tables 1 and 2, comprising normal proliferative (n = 5; samples 1 to 5 in Table 2) and well-differentiated endometrial cancer tissues (n = 4; samples 21 to 24 in Table 1). Five-micrometer paraffin wax-embedded tissue sections were cut and mounted onto coated slides. Sections were dewaxed in xylene, rehydrated in graded ethanol, and washed in water. Antigen retrieval was performed by pressure cooking the slides for 5 minutes in 0.01 M sodium citrate (pH 6). After antigen retrieval, endogenous endoperoxidase activity was blocked by incubating slides in methanol containing 3% H2O2. For the triple immunofluorescence, sections were blocked in normal goat serum (NGS) and incubated overnight with a polyclonal anti-IL-11Rα antibody at 1/600 (C-20; Santa Cruz Biotechnology, Santa Cruz, CA). Sections were washed, incubated in goat anti-rabbit peroxidase (1/500 in NGS for 30 minutes), followed by fluorochromes tissue specific antigen-plus cyanide 3 (1/50 in diluent for 10 minutes; PerkinElmer, Wellesley, MA; Applied Biosystems). Sections were washed, and antigen retrieval in citrate buffer and blocking in NGS was repeated before being incubated overnight with a polyclonal anti-FP receptor antibody at 1/600 (Cayman Chemical, Ann Arbor, MI). Sections were washed, incubated in goat anti-rabbit peroxidase (1/500 in NGS), followed by fluorochromes tissue specific antigen-plus cyanide 5 (1/50 in diluent). Finally, after further antigen retrieval and blocking steps, sections were incubated overnight with a monoclonal anti-IL-11 antibody at 1/100 (R&D Systems, Oxford, UK). Sections were washed, incubated in goat anti-mouse peroxidase (1/500 in NGS), followed by fluorochromes tissue specific antigen-plus flourescein (green) (1/50 in diluent). All sections were washed, mounted in Permafluor, and visualized using a laser-scanning microscope (meta confocal; Carl Zeiss, Jena, Germany). Matched serial control sections from each tissue were incubated with equivalent concentration of normal IgG from host species.
Enzyme-Linked Immunosorbent Assay
Secreted IL-11 was quantified using an in-house enzyme-linked immunosorbent assay (ELISA). IL-11 was measured by ELISA using matched pairs of capture and biotinylated labeled detection antibodies for IL-11 (R&D Systems). Briefly, plates were coated overnight at 4°C with capture antibody added at 100 μl/well, followed by 100 μl/well of coating solution for 1 hour at room temperature. The coating solution was removed and the plates stored at −20°C. Before use, the plates were washed twice in wash buffer (0.05% Tween 20, 10 mmol/L Tris, and 0.15 M NaCl). Recombinant IL-11 standard (R&D Systems) was diluted in ELISA buffer (using a concentration range of 4000 to 31.25 pg/ml), and 100 μl of standard or conditioned media sample was added per well in duplicate. Plates were incubated overnight at 4°C and then washed four times as above, before addition of anti-IL-11 detection antibody (R&D Systems) at 100 ng/ml in ELISA buffer. Plates were again washed four times before addition of streptavidin–peroxidase at 1/2000 adding 100 μl/well for 20 minutes at room temperature on a rocker. Plates were again washed four times before addition of tetramethylbenzidine substrate. Color change was monitored and stopped using 2 N sulfuric acid. Plates were read on a plate reader at 450 nm within 10 minutes of quenching. Samples were serially diluted before assay, and the concentration of IL-11 in each sample was interpolated from the within plate standard curve. The minimum detection limit was 16 pg/ml. The interassay and intra-assay coefficient of variance were 7.31 and 6.04%, respectively. Data are represented as mean ± SEM for four individual experiments.
Western Blot Analysis
Proteins were extracted and quantified as described previously.8 Samples were loaded in duplicate. In parallel, cell lysate from Ishikawa cells infected with full-length regulator of calcineurin 1–4 (RCAN1-4) adenovirus as described by Maldonado-Perez et al21 was used as a positive control (data not shown). After resolving and immunoblotting, membranes were incubated overnight at 4°C, with a rabbit anti RCAN1-4 antibody (1/5000), a gift from Dr. E. W. Bush (Myogen, Westminster, CO), together with a mouse anti-β-actin antibody (1/800) (Santa Cruz Biotechnology). The following day, cells were washed and incubated with goat anti-rabbit Alexafluor 680 (1/5000; Invitrogen, Carlsbad, CA) and goat anti-mouse IRDye 800 (1/5000; Rockland, Gilbersville, PA) for 60 minutes at room temperature. Blots were visualized and the protein immunoreactivity quantified using an Odyssey infrared imaging system (LI-COR, Cambridge, UK). RCAN1-4 relative density was calculated by dividing the value obtained for RCAN1-4 by the value obtained for β-actin and expressed as fold above vehicle controls. Data are presented as mean ± SEM from three independent experiments.
Adenovirus Infection
The RCAN adenovirus was constructed using the cDNA of RCAN1-4 (Origene, Rockville, MD) as detailed in our previous study.21 Ishikawa FPS cells were plated in 5-cm dishes or 6-well plates at a density of 200,000 cells/well. Thereafter, cells were infected with RCAN1-4 adenovirus at a multiplicity of infection of five viruses per cell. In parallel, cells were infected with a negative control adenovirus containing a cytomegalovirus promoter with no insert (Rad60)24 at the same multiplicity of infection. For RCAN infection of endometrial adenocarcinoma tissues, four poorly differentiated tissues (samples 1 to 4; Table 1) were used. The tissues were processed in the order in which they were received from the gynecology clinic without bias toward clinical parameters such as International Federation of Gynecology and Obstetrics (FIGO) stage or depth of invasion. Tissues were prepared for infection by finely sectioning using a sterile scalpel blade and incubated with 1 × 106 virus/ml of either the RAD60 or RCAN1-4 adenovirus. Cells and tissues were incubated with virus for 24 hours and serum starved overnight before treatment with vehicle or 100 nmol/L PGF2α. All infections and treatments were conducted in duplicate. Data are presented as mean ± SEM (from four independent experiments for in vitro cell culture and n = 4 for adenocarcinoma explants).
Statistical Analysis
The data in this study were analyzed by unpaired t-test or analysis of variance (ANOVA) to compare groups using Microsoft Excel (Microsoft) and Prism 4.0c (GraphPad, San Diego, CA) with an additional posttest to assess the evidence of a linear trend across grades of adenocarcinomas where appropriate. Values of P < 0.05 were considered significant.
Results
IL-11, IL-11Rα, and GP130 Expression in Endometrial Adenocarcinoma and Normal Proliferative-Phase Endometrium
The relative mRNA expression of IL-11 (Figure 1A), its receptor IL-11Rα (Figure 1B), and its coreceptor GP130 (Figure 1C) was investigated in human endometrial adenocarcinoma and normal proliferative-phase endometrium by TaqMan quantitative RT-PCR analysis. The expression of IL-11 mRNA (Figure 1A) was significantly up-regulated in all endometrial adenocarcinomas represented in Table 1 irrespective of grade or FIGO stage, compared with normal proliferative-phase endometrial tissues listed in Table 2 (t-test, prolif versus Poor P < 0.001; t-test, prolif versus Mod P = 0.005; t-test, prolif versus well P = 0.02). In addition, a significant linear trend was observed across the different grades of cancer for IL-11 mRNA with highest levels of expression observed in poorly differentiated cancer (∗, ANOVA posttest for linear trend; P < 0.0001). Expression of IL-11Rα (Figure 1B) and GP130 (Figure 1C) was significantly decreased in all endometrial adenocarcinomas represented in Table 1 compared with normal proliferative-phase endometrium listed in Table 2 (t-test, prolif versus Poor P = 0.03; t-test, prolif versus Mod P = 0.04; t-test, prolif versus well P = 0.04) and did not appear to vary with tumor grade or FIGO stage.
Figure 1.
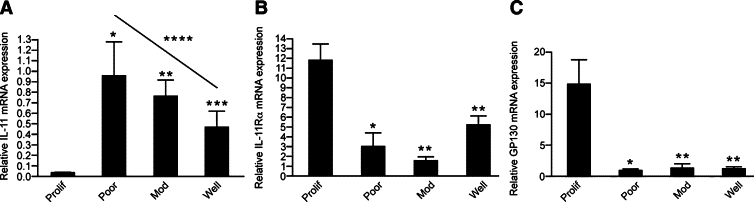
IL-11, IL-11Rα, and GP130 mRNA expression. A: The relative mRNA expression of IL-11 in normal proliferative-phase endometrium (n = 10) and poorly (n = 10), moderately (n = 10), and well-differentiated (n = 10) endometrial adenocarcinoma as determined by real-time quantitative RT-PCR analysis. Data are represented as mean ± SEM proliferation is significantly different from poorly (*P < 0.001), moderately (**P = 0.005), and well-differentiated (***P = 0.02) adenocarcinomas compared with proliferative-phase endometrium; ANOVA posttest for linear trend for IL-11 expression between poorly, moderately, and well-differentiated adenocarcinomas, ****P < 0.0001. The relative mRNA expression of IL-11Rα (B) and GP130 (C) in normal proliferative-phase endometrium (n = 10) and poorly (n = 10), moderately (n = 10), and well-differentiated (n = 10) endometrial adenocarcinoma as determined by real-time quantitative RT-PCR analysis. Data are represented as mean ± SEM proliferation is significantly different from poorly (*P = 0.03), moderately, and well-differentiated (**P = 0.04) adenocarcinomas compared with proliferative-phase endometrium.
The site of IL-11, IL-11Rα, and GP130 protein expression in endometrial adenocarcinomas was determined by immunohistochemistry (Figure 2). Strong apical and baso-lateral immunoreactive staining was observed for IL-11 (Figure 2, A, D, and G), IL-11Rα (Figure 2, B, E, and H), and GP130 (Figure 2, C, F, and I) in the glandular epithelium and vascular endothelium (BV, Figure 2, M–O, as indicated by the arrow; representative sample 29; Table 1) of poorly differentiated (representative sample 2; Table 1), moderately differentiated (Mod, representative sample 15; Table 1), and well-differentiated (representative sample 26; Table 1) endometrial adenocarcinomas with stromal staining observed for all three biomarkers. The expression patterns of IL-11, IL-11Rα, and GP130 were similar within each respective grade irrespective of clinical parameter outlined in Table 1. The pattern of staining for IL-11, IL-11Rα, and GP130 was similar in endometrial adenocarcinomas to that observed for normal proliferative endometrium (Figure 2, J–L). IL-11 localized to the apical surface (dark arrow) with punctuate lateral and basal (white arrow) surface staining (Figure 2J, representative sample 2; Table 2) in proliferative-phase endometrium with low levels of staining observed for IL-11 in the stroma. IL-11Rα exhibited higher intensity of staining on the apical (dark arrow) compared with basal or lateral surfaces (Figure 2K, representative sample 2; Table 2) with greater intensity of staining observed in the stroma compared with IL-11. GP130 immunoreactivity was localized to the apical and baso-lateral surfaces of the luminal and glandular epithelium with stromal reactivity, which was greater than that observed for IL-11 or IL-11Rα (Figure 2L, representative sample 2; Table 2). Incubating sections with nonimmune IgG from the host species showed no immunoreactivity (inset shown; Figure 2L). Furthermore, the expression of FP receptor (Figure 3, A and B, lower left panel, blue channel), IL-11Rα (Figure 3, A and B, upper right panel, red channel), and IL-11 protein (Figure 3, A and B, upper left panel, green channel) colocalized (Figure 3, A and B, lower right panel, merged purple channel) in glandular epithelium and vascular endothelium in proliferative-phase endometrium (Figure 3A, representative sample 9; Table 2) and well-differentiated endometrial adenocarcinoma (Figure 3B, representative sample 27, Table 1) by immunofluorescence. The control section (Figure 3C, representative of serial section sample 9; Table 2) was negative for immunoreactivity for all three biomarkers.
Figure 2.
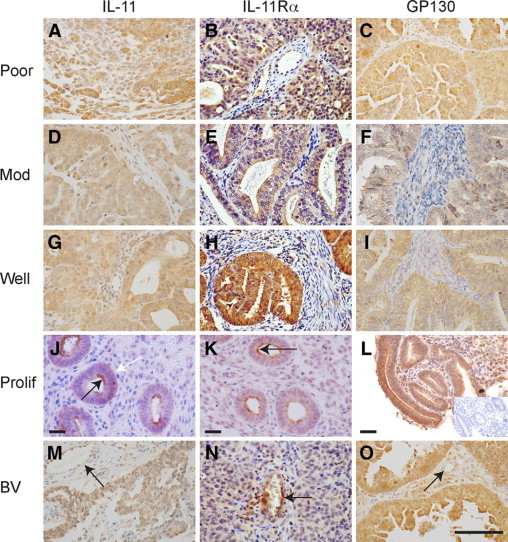
Localization of the site of expression of IL-11, IL-11Rα, and GP130 in endometrial adenocarcinomas and normal proliferative endometrium. The site of expression of IL-11 (A, D, G, J, and M), IL-11Rα (B, E, H, K, and N), and GP130 (C, F, I, L, and O) in samples of poorly (poor, A–C, representative sample 2; Table 1), moderately (mod, D–F; representative sample 15; Table 1), and well-differentiated (G–I, representative sample 26; Table 1) endometrial adenocarcinomas and proliferative-phase endometrium (J–L, representative sample 2; Table 2) by serial section. Intense immunoreactivity as indicated by the brown 3,3′-diaminobenzidine staining was observed to be localized to the glandular epithelial and vascular compartment (BV, M–O as indicated by the arrow, representative sample 29; Table 1) with diffuse stromal immunoreactivity in all tissue sections with no discernable difference in staining pattern observed within each grade or stage of adenocarcinoma. IL-11 and IL-11Rα displayed distinct immunoreactivity on the apical surface in proliferative-phase endometrium (black arrow for IL-11 and IL-11Rα, J and K, respectively) with lesser punctuate staining on the basal (white arrow, for IL-11, J) and lateral surfaces. Control sections were negative for immunoreactivity (Inset, representative serial section of L, representative sample 2; Table 2). Scale bar = 50 μmol/L.
Figure 3.
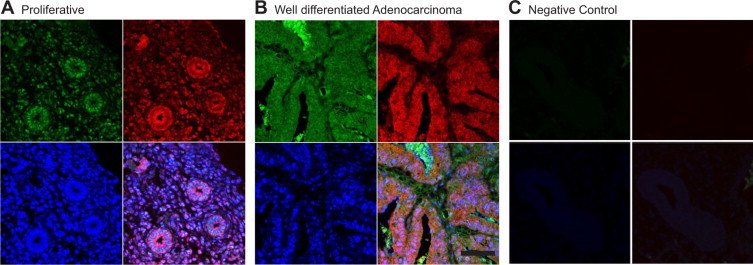
Colocalization of expression of FP receptor, IL-11, and IL-11Rα in well-differentiated endometrial adenocarcinoma and proliferative-phase endometrium. Colocalization of the expression of FP receptor (A and B, lower left panel, blue channel), IL-11Rα (A and B, upper right panel, red channel), and IL-11 protein (A and B, upper left panel, green channel) colocalized (A and B, lower right panel, merged purple channel) in the glandular epithelium and vascular endothelium in proliferative-phase endometrium (A, representative sample 9; Table 2) and well-differentiated endometrial adenocarcinoma (B, representative sample 27; Table 1) by immunofluorescence. The control section C (representative of serial section of representative sample 9; Table 2) was negative for immunoreactivity for all three markers. Scale bar = 50 μmol/L.
PGF2α-FP Receptor Activation Induces IL-11 Expression and Release in Ishikawa FPS Cells
Because FP receptor, IL-11, and IL-11Rα colocalized in the glandular epithelium in endometrial adenocarcinomas, PGF2α signaling to IL-11 was investigated using a human endometrioid endometrial adenocarcinoma cell line stably transfected with the FP receptor (Ishikawa FPS cells).11 FPS cells were stimulated with vehicle or 100 nmol/L PGF2α for the times indicated in the figure legend. PGF2α stimulation resulted in a significant time-dependent increase in the relative expression of IL-11 mRNA (Figure 4A, ANOVA, P < 0.001) and protein in FPS cells (Figure 4B, ANOVA, P < 0.001), with maximal responses observed after 16 and 72 hours, respectively. In contrast, PGF2α-FP receptor stimulation of FPS cells promoted a significant time-dependent down-regulation of IL-11Rα mRNA expression compared with control (Figure 4C, t-test, P = 0.04, 0.03, and 0.03 for 8, 12 and 16 hours, respectively). No significant alteration in mRNA expression of GP130 was observed in FPS cells in response to PGF2α-FP receptor activation (data not shown).
Figure 4.
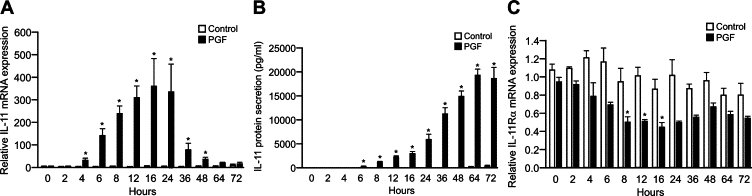
IL-11 and IL-11Rα expression in Ishikawa FPS cells in response to 100 nmol/L PGF2α. IL-11 mRNA (A) and protein (B) expression in Ishikawa FPS cells following treatment of cells for 0, 2, 4, 6, 8, 12, 16, 24, 36, 48, 64, and 72 hours with vehicle or 100 nmol/L PGF2α as measured by real-time quantitative RT-PCR analysis and ELISA, respectively. Data are represented as mean ± SEM *P < 0.001 for PGF treatment compared with control treatment. C: IL-11Rα mRNA expression in Ishikawa FPS cells following treatment of cells for 0, 2, 4, 6, 8, 12, 16, 24, 36, 48, 64, and 72 hours with vehicle or 100 nmol/L PGF2α as measured by real-time quantitative RT-PCR analysis. Data are represented as mean ± SEM *P = 0.04, for 8 hours, and **P = 0.03 for 12, and 16 hours, for PGF treatment compared with control treatment.
PGF2α-FP Receptor Activation Induces the Expression of IL-11 via the Calcineurin-NFAT Pathway
The signal transduction pathways mediating PGF2α-FP receptor signaling to IL-11 were investigated. FPS cells were stimulated with vehicle or 100 nmol/L PGF2α for 24 hours. In parallel, cells were also treated with vehicle or PGF2α in the presence of the FP receptor antagonist AL8810 or chemical inhibitors of Gq/11 (YM254890), protein kinase (PK)C (RO-318220), PKA (4-cyano-3-methylisoquinoline), calcineurin (cyclosporine A), NFAT (Inca-6), or calcium chelator EGTA. Treatment of FPS cells with PGF2α promoted a significant increase in IL-11 mRNA (Figure 5A, t-test P = 0.01) and protein expression (Figure 5B, t-test P = 0.01). Cotreatment of FPS cells with FP receptor antagonist AL8810 (t-test P = 0.001) or chemical inhibitors of Gq/11 (YM254890; t-test, P = 0.02), PKC (RO-318220; t-test, P = 0.01), calcineurin (cyclosporine A; t-test P = 0.03), NFAT (Inca-6; t-test, P = 0.03), or calcium chelator EGTA (P = 0.03) but not PKA (4-cyano-3-methylisoquinoline; t-test, P = 0.12) significantly inhibited the expression of IL-11 mRNA (Figure 5A) and release of IL-11 protein (Figure 5B). These data indicate that IL-11 expression and release is regulated via the PGF2α-FP receptor activation of the Gq-PKC-calcium-calcineurin-NFAT signal transduction pathway.
Figure 5.
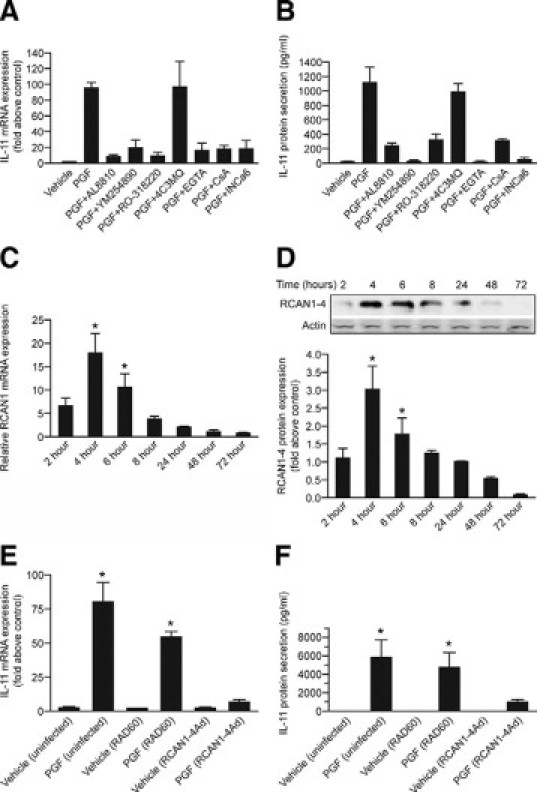
IL-11 is regulated by PGF2α via the calcium-calcineurin-NFAT pathway. IL-11 mRNA expression (A) and protein secretion (B) in FPS cells treated for 24 hours, respectively, with vehicle, 100 nmol/L PGF2α (P = 0.01), 100 nmol/L PGF2α in the absence/presence of AL8810 (50 μmol/L; P = 0.001), YM254890 (1 μmol/L; P = 0.02), RO-318220 (1 μmol/L; P = 0.01), 4-cyano-3-methylisoquinoline (4C3MQ) (1 μmol/L; P = 0.12), EGTA (1.5 mmol/L; P = 0.03), cyclosporine A (CsA) (1 μmol/L; P = 0.03), or Inca-6 (40 μmol/L; P = 0.03) as determined by quantitative RT-PCR analysis and ELISA, respectively. Data are represented as mean ± SEM; PGF treatment is significantly different from PGF and inhibitor treatment or PGF and vehicle control treatment at the previously listed values. RCAN1-4 mRNA (C) and protein expression (D) in FPS cells treated with 100 nmol/L PGF2α for 2, 4, 6, 8, 24, 48, and 72 hours as determined by quantitative RT-PCR and Western blot analysis, respectively. Data are represented as mean ± SEM, *P < 0.001 for PGF treatment compared vehicle control treatment at each time point. E: FPS cells were infected with either RAD60 control adenovirus or RCAN1-4 adenovirus for 24 hours or left uninfected. Cells were then treated with vehicle or 100 nmol/L PGF2α for 24 hours and IL-11 mRNA, and protein expression (F) was determined by quantitative RT-PCR analysis and ELISA, respectively. Data are represented as mean ± SEM for PGF treatment compared with vehicle control treatment for mRNA (E, *P = 0.03) and protein (F, *P = 0.02).
Having identified that the PGF2α-FP receptor activation of IL-11 was mediated via the calcineurin-NFAT signaling pathway, the regulation of IL-11 by the RCAN1, previously known as Down syndrome critical region gene 1 or Adapt 78, which is known to endogenously modulate calcineurin-NFAT signaling25 was explored. RCAN1 isoform 4 (RCAN1-4) is known to bind to calcineurin and inhibit activation of NFAT when overexpressed26 and has been shown by our laboratory to be a negative regulator of chemokine expression.21 The temporal regulation of RCAN1-4 in FPS cells by PGF2α was investigated by quantitative RT-PCR and Western blot analysis. Treatment of FPS cells with 100 nmol/L PGF2α resulted in rapid time-dependent induction of RCAN1-4 mRNA (Figure 5C; ANOVA, P < 0.001) and protein (Figure 5D; ANOVA, P < 0.001), with maximal expression after 4 hours with subsequent reduction to basal level. The reciprocal nature of RCAN1-4 expression compared with IL-11 (Figure 4, A and B) suggested that it could be a negative regulator of IL-11 expression. To investigate this, an adenoviral construct expressing the full-length RCAN1-4 cDNA was used. FPS cells were infected with either a control (RAD60) adenovirus or RCAN1-4 adenovirus for 24 hours before stimulation or left uninfected. Cells were stimulated with vehicle or 100 nmol/L PGF2α for 24 hours. Overexpression of RCAN1-4 in FPS cells significantly reduced the PGF2α-FP receptor-mediated induction of IL-11 mRNA expression (Figure 5E; t-test, P = 0.03) and protein secretion (Figure 5F; t-test, P = 0.02) compared with cells infected with the control virus or control cells, which were uninfected.
Expression and Regulation of RCAN1-4 in Endometrial Tissues
Because PGF2α-FP receptor signaling to IL-11 was regulated by RCAN1-4, the mRNA expression of RCAN1-4 (Figure 6A) in human endometrial adenocarcinoma compared with normal proliferative-phase endometrium was investigated by quantitative RT-PCR analysis. RCAN1-4 expression was significantly higher in well-differentiated adenocarcinoma compared with normal proliferative phase endometrium (t-test P = 0.03). Interestingly, we observed a significant linear trend for RCAN1-4 mRNA expression, which decreased with increasing tumor grade, such that RCAN1-4 mRNA expression was significantly lower in poorly differentiated endometrial adenocarcinomas (Figure 6A, ANOVA, ∗posttest for linear trend, P = 0.002).
Figure 6.
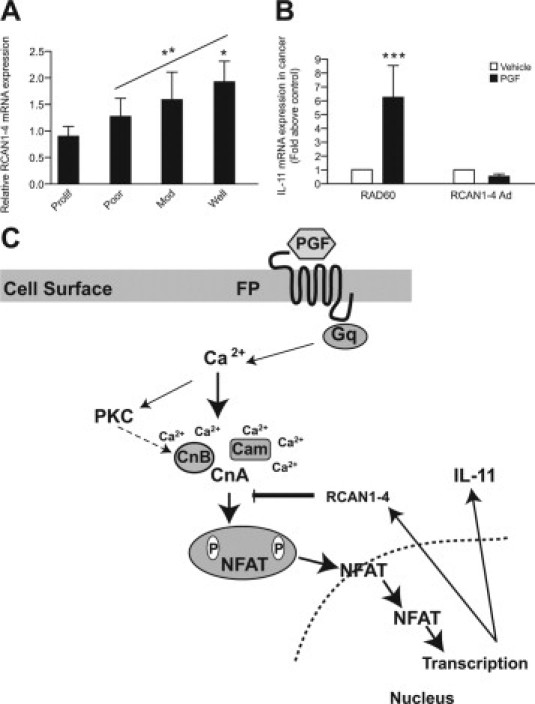
RCAN1-4 expression in endometrial tissues. A: Relative mRNA expression of RCAN1-4 in normal proliferative-phase endometrium (n = 10) and poorly (n = 10), moderately (n = 10), and well-differentiated (n = 10) endometrial adenocarcinoma as determined by real-time quantitative RT-PCR analysis. Data are represented as mean ± SEM *P < 0.03 for well-differentiated adenocarcinoma compared with proliferative-phase endometrium ANOVA posttest for linear trend between poor, moderate, and well-differentiated adenocarcinomas; **P = 0.002. B: Poorly differentiated endometrial adenocarcinomas explants (samples 1 to 4; Table 1) were infected with either RAD60 control adenovirus or RCAN1-4 adenovirus for 24 hours and then stimulated with vehicle or 100 nmol/L PGF2α for 24 hours and subjected to quantitative RT-PCR analysis for IL-11 mRNA expression. Data are represented as mean ± SEM ***P < 0.003 for PGF treatment compared with vehicle control treatment. C: A schematic summary. PGF2α-FP receptor activation in endometrial adenocarcinoma cells promotes the induction of RCAN1-4 and IL-11 via the Gq-phospholipase C-PKC-calcium (Ca2+)-calcineurin-NFAT cascade. RCAN1-4 is temporally activated in a reciprocal manner to IL-11 by PGF-FP receptor signaling and acts as a negative regulator of the calcineurin pathway to regulate IL-11 expression.
RCAN1-4 Is a Negative Regulator of IL-11 Expression in Endometrial Adenocarcinoma Explants
Finally, the role of RCAN1-4 as a negative regulator of IL-11 in endometrial adenocarcinomas was investigated ex vivo. Four poorly differentiated endometrioid endometrial adenocarcinoma explants (samples 1 to 4; Table 1) were infected with either a control (RAD60) adenovirus or RCAN1-4 adenovirus for 24 hours before stimulation with vehicle or 100 nmol/L PGF2α for 24 hours (Figure 6B). Overexpression of RCAN1-4 in these endometrial adenocarcinoma samples significantly reduced the PGF2α-FP receptor-mediated induction of IL-11 mRNA expression in explants compared with control virus-infected tissue (t-test, P = 0.003).
Discussion
IL-11 has been shown to regulate cell motility, invasion, and metastasis in vitro and in vivo.15, 20, 27, 28 The present study demonstrated elevated expression of IL-11 in endometrial adenocarcinomas compared with normal endometrium from the proliferative phase of the menstrual cycle. As the endometrium of postmenopausal women is no longer under normal hormonal control, the tissue is atrophic and often not attainable for analysis, we chose normal proliferative-phase endometrium as our comparator. This is the phase of the menstrual cycle that exhibits rapid cellular proliferation, differentiation, and tissue remodeling and is the phase of the menstrual cycle with the highest expression of FP receptor.13 Interestingly, the present study highlights a significant variation in expression of IL-11 with grade of adenocarcinomas, with highest levels observed in high-grade (poorly differentiated) adenocarcinomas. Furthermore, IL-11 and IL-11Rα protein expression colocalized with FP receptor expression in normal endometrial tissue and endometrial adenocarcinomas. The pattern of expression of IL-11, IL-11Rα, and its coreceptor GP130 was similar in endometrial adenocarcinoma compared with normal proliferative-phase endometrium in the present study confirming the localization of these biomarkers as reported by others in normal endometrium29–32 and other carcinomas.33,34 Moreover, we have shown that IL-11 is regulated by PGF2α via the FP receptor in an in vitro model system of endometrial adenocarcinoma cells and poorly differentiated endometrial adenocarcinoma explants ex vivo. To our knowledge, this is the first study to report on the expression, localization, and cellular mechanism regulating IL-11 in endometrial adenocarcinomas.
Although little is known of the role of IL-11 in endometrial cancer, IL-11 is essential for normal reproduction in the human and mouse.35,36 IL-11 and IL-11Rα expression are dysregulated in endometrium of infertile women with endometriosis,35,36 and IL-11 in the normal endometrium is known to promote the migration of trophoblast cells.27 IL-11 and IL-11Rα have been shown to correlate with tumor progression, cellular growth and differentiation, and poor prognosis in breast and colorectal cancers18,19 and is associated with breast cancer cell metastases to bone.15 To investigate the regulation of IL-11, IL-11Rα, and GP130 in endometrial adenocarcinomas by the FP receptor, we used Ishikawa FPS cells, stably expressing the FP receptor. This in vitro approach has previously been used by our laboratory and others to interrogate PGF2α-FP receptor signaling.10,11,37–39 Using this model system, we have previously demonstrated that the PGF2α-FP receptor signaling in Ishikawa FPS cells parallels the ex vivo effects of PGF2α on endometrial adenocarcinoma explants, indicating that it is a suitable model system to interrogate FP receptor signaling in endometrial epithelial cells in vitro.10,11
Here we have demonstrated that PGF2α promotes the synthesis and release of IL-11 in Ishikawa FPS cells in a time-dependent manner. We confirmed that PGF2α-FP receptor signaling regulated IL-11 mRNA expression ex vivo using endometrial adenocarcinoma explants. Interestingly, PGF2α-FP receptor interaction promoted a time-dependent decrease in the mRNA expression of IL-11Rα in Ishikawa FPS cells, suggesting that a negative feedback loop was being activated to prevent autocrine induction of the IL-11Rα/GP130 receptor complex by IL-11.
Because expression of IL-11Rα mRNA is significantly reduced in endometrial adenocarcinomas compared with normal proliferative-phase endometrium, it is feasible that activation of the FP receptor in adenocarcinomas in vivo could down-regulate expression of the IL-11Rα mRNA in a similar manner to our observation with the Ishikawa FPS cell line in vitro. We investigated whether the mechanism of down-regulation of IL-11Rα in vitro was mediated via IL-11; however, treatment of FPS cells with the recombinant IL-11 had no effect on IL-11Rα mRNA expression (data not shown), indicating that either PGF2α was having a direct inhibitory effect on IL-11Rα mRNA synthesis or another factor produced by PGF2α-FP receptor signaling was regulating IL-11Rα mRNA in Ishikawa FPS cells in vitro.
The intracellular signal transduction pathways mediating the role of the FP receptor in regulating IL-11 was investigated using chemical inhibitors of intracellular signaling. IL-11 was found to be regulated in FPS cells at the mRNA and protein level by PGF2α via the PKC-calcium-calcineurin-NFAT signaling pathway. NFAT activation by calcineurin, which mediates its dephosphorylation and translocation to the nucleus, is known to be regulated by the RCAN.25 RCAN1-4 is known to bind to calcineurin, and previous studies have shown that overexpression of this protein results in an inhibition of calcineurin activation of NFAT.26,40,41 The temporal pattern of expression of RCAN1-4 mRNA and protein in FPS cells was investigated in response to PGF2α and found to be regulated in a reciprocal manner to IL-11, reaching a peak of expression that preceded IL-11 × 8 hours, suggesting that RCAN1-4 could act as a negative regulator of IL-11 expression. Indeed, overexpression of RCAN1-4 and subsequent inhibition of NFAT activation significantly inhibited the PGF2α-mediated activation and release of IL-11 from FPS cells. This is in agreement with other published observations that show that expression of this isoform is induced by NFAT41 and can negatively regulate chemokines, such as IL-8, in endometrial epithelial cells.21
Dysregulated RCAN (also called Down syndrome candidate region 1) expression has been linked to pathological processes. For example, RCAN overexpression in brains of Down syndrome fetuses40 and Alzheimer's patients42 is thought to enhance neurodegenerative conditions. RCAN expression is known to be up-regulated by glucocorticoids43 and is induced in endothelial cells as a negative feedback regulator of endothelial cell proliferation and branching.41,44 We investigated the expression of RCAN1-4 in normal proliferative-phase endometrium and endometrial adenocarcinomas. We found significantly lower RCAN1-4 expression with advancing tumor grade, such that levels of RCAN1-4 were lowest in high-grade (poorly differentiated) adenocarcinomas, the opposite pattern to that seen for IL-11 expression. Furthermore, RCAN1-4 overexpression could negatively regulate IL-11 expression in cancer explants ex vivo similarly to our observations using the Ishikawa FPS cell line in vitro. Although we found no difference within each grade with respect to FIGO stage, our data show that RCAN1-4 expression reduces coincident with advancing grade of endometrial adenocarcinoma (ie, from well-differentiated or low-grade to poorly differentiated or high-grade cancer). These findings suggest that the natural brake created by RCAN1-4 to control calcineurin signaling and cytokine production is defective in high-grade (poorly differentiated) compared with low-grade (well-differentiated) adenocarcinomas. This results in unopposed PGF2α-FP receptor signaling via the calcium-calcineurin-NFAT pathway to elevate cytokine production such as IL-11 and may confer an advantage to tumor progression and metastasis. However, further studies are needed to determine the prognostic and/or predictive value of IL-11, RCAN1-4, and the calcineurin-NFAT pathway in women with early or advanced endometrial adenocarcinoma.
In conclusion, these data (as summarized in Figure 6C) show that PGF2α-FP receptor activation in endometrial adenocarcinoma cells regulates IL-11 expression via the Gq-phospholipase C-PKC-calcium-calcineurin-NFAT pathway. Moreover, RCAN1-4 was identified as a negative regulator of PGF2α-FP receptor-mediated IL-11 expression in endometrial adenocarcinoma cells stably expressing the FP receptor in vitro and tissue explants ex vivo. Further studies to evaluate whether RCAN signaling can be exploited therapeutically to negatively control calcineurin-NFAT signaling, and IL-11 production may be of potential clinical significance for women with type 11 high-grade (poorly differentiated) endometrial adenocarcinoma.
Acknowledgements
We thank Ms. Anne Saunderson and Sharon McPherson for patient recruitment and sample collection.
Footnotes
Supported by Medical Research Council core funding to H.N.J. (U.1276.00.004.00002.01).
References
- 1.Mant JW, Vessey MP. Ovarian and endometrial cancers. Cancer Surv. 1994;20:287–307. [PubMed] [Google Scholar]
- 2.Persson I. Estrogens in the causation of breast, endometrial and ovarian cancers—evidence and hypotheses from epidemiological findings. J Steroid Biochem Mol Biol. 2000;74:357–364. doi: 10.1016/s0960-0760(00)00113-8. [DOI] [PubMed] [Google Scholar]
- 3.Parazzini F, La Vecchia C, Bocciolone L, Franceschi S. The epidemiology of endometrial cancer. Gynecol Oncol. 1991;41:1–16. doi: 10.1016/0090-8258(91)90246-2. [DOI] [PubMed] [Google Scholar]
- 4.Ryan AJ, Susil B, Jobling TW, Oehler MK. Endometrial cancer. Cell Tissue Res. 2005;322:53–61. doi: 10.1007/s00441-005-1109-5. [DOI] [PubMed] [Google Scholar]
- 5.Bokhman JV. Two pathogenetic types of endometrial carcinoma. Gynecol Oncol. 1983;15:10–17. doi: 10.1016/0090-8258(83)90111-7. [DOI] [PubMed] [Google Scholar]
- 6.Tong BJ, Tan J, Tajeda L, Das SK, Chapman JA, DuBois RN, Dey SK. Heightened expression of cyclooxygenase-2 and peroxisome proliferator-activated receptor-δ in human endometrial adenocarcinoma. Neoplasia. 2000;2:483–490. doi: 10.1038/sj.neo.7900119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jabbour HN, Milne SA, Williams ARW, Anderson RA, Boddy SC. Expression of COX-2 and PGE synthase and synthesis of PGE2 in endometrial adenocarcinoma: a possible autocrine/paracrine regulation of neoplastic cell function via EP2/EP4 receptors. Br J Cancer. 2001;85:1023–1031. doi: 10.1054/bjoc.2001.2033. [DOI] [PubMed] [Google Scholar]
- 8.Sales KJ, Milne SA, Williams AR, Anderson RA, Jabbour HN. Expression, localization, and signaling of prostaglandin F2α receptor in human endometrial adenocarcinoma: regulation of proliferation by activation of the epidermal growth factor receptor and mitogen-activated protein kinase signaling pathways. J Clin Endocrinol Metab. 2004;89:986–993. doi: 10.1210/jc.2003-031434. [DOI] [PubMed] [Google Scholar]
- 9.Jabbour HN, Sales KJ, Boddy SC, Anderson RA, Williams AR. A positive feedback loop that regulates cyclooxygenase-2 expression and prostaglandin F2α synthesis via the F-series-prostanoid receptor and extracellular signal-regulated kinase 1/2 signaling pathway. Endocrinology. 2005;146:4657–4664. doi: 10.1210/en.2005-0804. [DOI] [PubMed] [Google Scholar]
- 10.Sales KJ, Boddy SC, Williams AR, Anderson RA, Jabbour HN. F-Prostanoid receptor regulation of fibroblast growth factor 2 signalling in endometrial adenocarcinoma cells. Endocrinology. 2007;148:3635–3644. doi: 10.1210/en.2006-1517. [DOI] [PubMed] [Google Scholar]
- 11.Sales KJ, List T, Boddy SC, Williams AR, Anderson RA, Naor Z, Jabbour HN. A novel angiogenic role for prostaglandin F2α-FP receptor interaction in human endometrial adenocarcinomas. Cancer Res. 2005;65:7707–7716. doi: 10.1158/0008-5472.CAN-05-0101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sales KJ, Boddy SC, Jabbour HN. F-Prostanoid receptor alters adhesion, morphology and migration of endometrial adenocarcinoma cells. Oncogene. 2008;27:2466–2477. doi: 10.1038/sj.onc.1210883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Milne SA, Jabbour HN. Prostaglandin (PG) F2α receptor expression and signaling in human endometrium: role of PGF2α in epithelial cell proliferation. J Clin Endocrinol Metab. 2003;88:1825–1832. doi: 10.1210/jc.2002-021368. [DOI] [PubMed] [Google Scholar]
- 14.Wang D, Wang H, Brown J, Daikoku T, Ning W, Shi Q, Richmond A, Strieter R, Dey SK, DuBois RN. CXCL1 induced by prostaglandin E2 promotes angiogenesis in colorectal cancer. J Exp Med. 2006;203:941–951. doi: 10.1084/jem.20052124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singh B, Berry JA, Shoher A, Lucci A. COX-2 induces IL-11 production in human breast cancer cells. J Surg Res. 2006;131:267–275. doi: 10.1016/j.jss.2005.11.582. [DOI] [PubMed] [Google Scholar]
- 16.Heinrich PC, Behrmann I, Muller-Newen G, Schaper F, Graeve L. Interleukin-6-type cytokine signalling through the gp130/Jak/STAT pathway. Biochem J. 1998;334:297–314. doi: 10.1042/bj3340297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Katoh M, Katoh M. STAT3-induced WNT5A signaling loop in embryonic stem cells, adult normal tissues, chronic persistent inflammation, rheumatoid arthritis and cancer. Int J Mol Med. 2007;19:273–278. [PubMed] [Google Scholar]
- 18.Hanavadi S, Martin TA, Watkins G, Mansel RE, Jiang WG. Expression of interleukin 11 and its receptor and their prognostic value in human breast cancer. Ann Surg Oncol. 2006;13:802–808. doi: 10.1245/ASO.2006.05.028. [DOI] [PubMed] [Google Scholar]
- 19.Yamazumi K, Nakayama T, Kusaba T, Wen CY, Yoshizaki A, Yakata Y, Nagayasu T, Sekine I. Expression of interleukin-11 and interleukin-11 receptor α in human colorectal adenocarcinoma; immunohistochemical analyses and correlation with clinicopathological factors. World J Gastroenterol. 2006;12:317–321. doi: 10.3748/wjg.v12.i2.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nakayama T, Yoshizaki A, Izumida S, Suehiro T, Miura S, Uemura T, Yakata Y, Shichijo K, Yamashita S, Sekin I. Expression of interleukin-11 (IL-11) and IL-11 receptor α in human gastric carcinoma and IL-11 up-regulates the invasive activity of human gastric carcinoma cells. Int J Oncol. 2007;30:825–833. [PubMed] [Google Scholar]
- 21.Maldonado-Perez D, Brown P, Morgan K, Millar RP, Thompson EA, Jabbour HN. Prokineticin 1 modulates IL-8 expression via the calcineurin/NFAT signaling pathway. Biochim Biophys Acta. 2009;1793:1315–1324. doi: 10.1016/j.bbamcr.2009.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sales KJ, Grant V, Jabbour HN. Prostaglandin E2 and F2α activate the FP receptor and up-regulate cyclooxygenase-2 expression via the cyclic AMP response element. Mol Cell Endocrinol. 2008;285:51–61. doi: 10.1016/j.mce.2008.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Noyes RW, Hertig AT, Rock J. Dating the endometrial biopsy. Fertil Steril. 1950;1:3–25. doi: 10.1016/j.fertnstert.2019.08.079. [DOI] [PubMed] [Google Scholar]
- 24.Wilkinson GW, Akrigg A. Constitutive and enhanced expression from the CMV major IE promoter in a defective adenovirus vector. Nucleic Acids Res. 1992;20:2233–2239. doi: 10.1093/nar/20.9.2233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Davies KJ, Ermak G, Rothermel BA, Pritchard M, Heitman J, Ahnn J, Henrique-Silva F, Crawford D, Canaider S, Strippoli P, Carinci P, Min KT, Fox DS, Cunningham KW, Bassel-Duby R, Olson EN, Zhang Z, Williams RS, Gerber HP, Perez-Riba M, Seo H, Cao X, Klee CB, Redondo JM, Maltais LJ, Bruford EA, Povey S, Molkentin JD, McKeon FD, Duh EJ, Crabtree GR, Cyert MS, de la Luna S, Estivill X. Renaming the DSCR1/Adapt78 gene family as RCAN: regulators of calcineurin. FASEB J. 2007;21:3023–3028. doi: 10.1096/fj.06-7246com. [DOI] [PubMed] [Google Scholar]
- 26.Chan B, Greenan G, McKeon F, Ellenberger T. Identification of a peptide fragment of DSCR1 that competitively inhibits calcineurin activity in vitro and in vivo. Proc Natl Acad Sci USA. 2005;102:13075–13080. doi: 10.1073/pnas.0503846102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paiva P, Salamonsen LA, Manuelpillai U, Walker C, Tapia A, Wallace EM, Dimitriadis E. Interleukin-11 promotes migration, but not proliferation, of human trophoblast cells, implying a role in placentation. Endocrinology. 2007;148:5566–5572. doi: 10.1210/en.2007-0517. [DOI] [PubMed] [Google Scholar]
- 28.Yoshizaki A, Nakayama T, Yamazumi K, Yakata Y, Taba M, Sekine I. Expression of interleukin (IL)-11 and IL-11 receptor in human colorectal adenocarcinoma: IL-11 up-regulation of the invasive and proliferative activity of human colorectal carcinoma cells. Int J Oncol. 2006;29:869–876. [PubMed] [Google Scholar]
- 29.Karpovich N, Chobotova K, Carver J, Heath JK, Barlow DH, Mardon HJ. Expression and function of interleukin-11 and its receptor α in the human endometrium. Mol Hum Reprod. 2003;9:75–80. doi: 10.1093/molehr/gag012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dimitriadis E, Salamonsen LA, Robb L. Expression of interleukin-11 during the human menstrual cycle: coincidence with stromal cell decidualization and relationship to leukaemia inhibitory factor and prolactin. Mol Hum Reprod. 2000;6:907–914. doi: 10.1093/molehr/6.10.907. [DOI] [PubMed] [Google Scholar]
- 31.Linjawi S, Li TC, Tuckerman EM, Blakemore AI, Laird SM. Expression of interleukin-11 receptor α and interleukin-11 protein in the endometrium of normal fertile women and women with recurrent miscarriage. J Reprod Immunol. 2004;64:145–155. doi: 10.1016/j.jri.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 32.Cullinan EB, Abbondanzo SJ, Anderson PS, Pollard JW, Lessey BA, Stewart CL. Leukemia inhibitory factor (LIF) and LIF receptor expression in human endometrium suggests a potential autocrine/paracrine function in regulating embryo implantation. Proc Natl Acad Sci USA. 1996;93:3115–3120. doi: 10.1073/pnas.93.7.3115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Campbell CL, Guardiani R, Ollari C, Nelson BE, Quesenberry PJ, Savarese TM. Interleukin-11 receptor expression in primary ovarian carcinomas. Gynecol Oncol. 2001;80:121–127. doi: 10.1006/gyno.2000.6064. [DOI] [PubMed] [Google Scholar]
- 34.Campbell CL, Jiang Z, Savarese DM, Savarese TM. Increased expression of the interleukin-11 receptor and evidence of STAT3 activation in prostate carcinoma. Am J Pathol. 2001;158:25–32. doi: 10.1016/S0002-9440(10)63940-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dimitriadis E, Stoikos C, Stafford-Bell M, Clark I, Paiva P, Kovacs G, Salamonsen LA. Interleukin-11. IL-11 receptor α and leukemia inhibitory factor are dysregulated in endometrium of infertile women with endometriosis during the implantation window. J Reprod Immunol. 2006;69:53–64. doi: 10.1016/j.jri.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 36.Dimitriadis E, White CA, Jones RL, Salamonsen LA. Cytokines, chemokines and growth factors in endometrium related to implantation. Hum Reprod Update. 2005;11:613–630. doi: 10.1093/humupd/dmi023. [DOI] [PubMed] [Google Scholar]
- 37.Fujino H, Pierce KL, Srinivasan D, Protzman CE, Krauss AH, Woodward DF, Regan JW. Delayed reversal of shape change in cells expressing FP(B) prostanoid receptors: possible role of receptor resensitization. J Biol Chem. 2000;275:29907–29914. doi: 10.1074/jbc.M003467200. [DOI] [PubMed] [Google Scholar]
- 38.Fujino H, Regan JW. Prostaglandin F2α stimulation of cyclooxygenase-2 promoter activity by the FP(B) prostanoid receptor. Eur J Pharmacol. 2003;465:39–41. doi: 10.1016/s0014-2999(03)01485-7. [DOI] [PubMed] [Google Scholar]
- 39.Srinivasan D, Fujino H, Regan JW. Differential internalization of the prostaglandin F2α receptor isoforms: role of protein kinase C and clathrin. J Pharmacol Exp Ther. 2002;302:219–224. doi: 10.1124/jpet.302.1.219. [DOI] [PubMed] [Google Scholar]
- 40.Fuentes JJ, Genesca L, Kingsbury TJ, Cunningham KW, Perez-Riba M, Estivill X, de la Luna S. DSCR1, overexpressed in Down syndrome, is an inhibitor of calcineurin-mediated signaling pathways. Hum Mol Genet. 2000;9:1681–1690. doi: 10.1093/hmg/9.11.1681. [DOI] [PubMed] [Google Scholar]
- 41.Minami T, Horiuchi K, Miura M, Abid MR, Takabe W, Noguchi N, Kohro T, Ge X, Aburatani H, Hamakubo T, Kodama T, Aird WC. Vascular endothelial growth factor- and thrombin-induced termination factor: Down syndrome critical region-1, attenuates endothelial cell proliferation and angiogenesis. J Biol Chem. 2004;279:50537–50554. doi: 10.1074/jbc.M406454200. [DOI] [PubMed] [Google Scholar]
- 42.Ermak G, Morgan TE, Davies KJ. Chronic overexpression of the calcineurin inhibitory gene DSCR1 (Adapt78) is associated with Alzheimer's disease. J Biol Chem. 2001;276:38787–38794. doi: 10.1074/jbc.M102829200. [DOI] [PubMed] [Google Scholar]
- 43.Faruqi SA, Noumoff MJ, Deger RB, Jalal SM, Antoniades K. Trisomy 21 as the only recurrent chromosomal anomaly in a clinically aggressive ovarian carcinoma. Cancer Genet Cytogenet. 2002;138:165–168. doi: 10.1016/s0165-4608(02)00596-4. [DOI] [PubMed] [Google Scholar]
- 44.Qin L, Zhao D, Liu X, Nagy JA, Hoang MV, Brown LF, Dvorak HF, Zeng H. Down syndrome candidate region 1 isoform 1 mediates angiogenesis through the calcineurin-NFAT pathway. Mol Cancer Res. 2006;4:811–820. doi: 10.1158/1541-7786.MCR-06-0126. [DOI] [PubMed] [Google Scholar]


