Our understanding of the impact of diabetes on organ function has been evolving since the discovery of insulin in the 1920s. At that time insulin was a miracle drug that appeared to cure diabetes, but over time it became clear that death and disability from diabetes complications involving the eyes, kidneys, peripheral nerves, heart, and vasculature could occur even with treatment. With the improvement in diabetes care over the past 20 years, fewer patients are developing the traditional diabetes complications. However, as people live long and well with the disease, it has become apparent that diabetes can alter function and structure in tissues not typically associated with complications such as the brain and bone. Alteration in brain structure and function are particularly of concern because of the impact of dementia and cognitive dysfunction on overall quality of life.
From large epidemiological studies, it has been demonstrated that both vascular and Alzheimer's dementia are more common in patients with type 2 diabetes (1). Why this might be true has been difficult to define. Certainly these patients can be expected to have more risk factors such as previous cardiovascular disease, history of hypertension, and dyslipidemia than aged matched control subjects, but when these variables are controlled, the risk for patients with diabetes appears to be higher than that of other subject groups. Persistent hyperglycemia appears to play an important role in cerebral dysfunction. Many years ago, Reaven et al. (2) demonstrated that performance on cognitive tasks assessing learning, reasoning, and complex psychomotor performance was inversely related to glycemic control in a small population of subjects with type 2 diabetes. This issue was recently readdressed in the much larger ACCORD population, where an elevated A1C was found to be linked to reduced performance on neurocognitive tests assessing memory, learning, and executive functions in nearly 3,000 subjects with type 2 diabetes (3). However, the relevance of these observations to younger patients with type 2 diabetes and to patients with type 1 diabetes who may have fewer cardiovascular risk factors is uncertain. Is the dementia and cognitive dysfunction identified in elderly subjects with type 2 diabetes related to their comorbidities and age, or is it the result of a diabetes-related process that begins years earlier?
From studies performed in adults with type 1 diabetes, we now know that reductions in measures of motor speed and psychomotor efficiency can be seen in patients in midlife (4). These neurocognitive changes have been associated with a reduction in white matter volume or an alteration in white matter microstructure in some (5,6) but not all (7,8) investigations. Reduction in gray matter density in brain regions responsible for language processing and memory (8) and generalized atrophy (9) have also been identified in young adults with long-standing type 1 diabetes. Patients with chronic hyperglycemia (10), early onset of disease (11), or recurrent severe hypoglycemia (12) appear to be at particular risk for the development of changes in brain structure and function over time, although these associations have not been consistently observed in all groups of subjects with type 1 diabetes who have been investigated (7,8). If the abnormalities seen in these adults with type 1 diabetes are specific to diabetes, they may also be seen in younger patients with type 2 diabetes. Careful assessment of cerebral structure and function in young adults with type 2 diabetes but without other comorbidities that increase the risk of vascular disease could help us understand the impact of diabetes on the brain. Examination of children with diabetes may also provide more insight into the specific effects of diabetes on the brain.
In the current issue of Diabetes, Hershey et al. (13) present imaging data collected from a large cohort of children with type 1 diabetes. They made the surprising observation that hippocampal volumes were increased in the children with the largest number of severe hypoglycemic episodes. These observations demonstrate the sensitivity of the hippocampus to acute hypoglycemia but are contrary to the data collected in adults with long-standing type 1 diabetes where no changes in hippocampal volume have been observed (9). Hershey et al. speculate that the developing brain may respond differently than the adult brain to a hypoglycemic insult, which has been demonstrated in animal models where postnatal age influences the regional vulnerability to hypoglycemia (14).
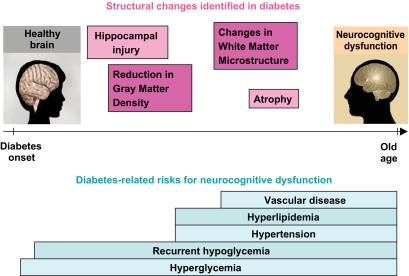
Defining the impact of diabetes and related risk factors on cerebral structure and function is very important to patients with diabetes. To do so will require careful prospective evaluation of subjects with type 1 diabetes over their life span using both sophisticated imaging technology and comprehensive neurocognitive testing. As depicted in Fig. 1, we must understand if the increases in hippocampal volumes seen by Hershey et al. in children with diabetes and frequent hypoglycemia are linked to the abnormalities in white matter microstructure and neurocognitive function identified by Kodl et al. (5) in population of older type 1 diabetic subjects. Of equal importance is learning whether the structural and neurocognitive abnormalities identified in midlife in patients with type 1 diabetes are related to the more severe levels of cognitive dysfunction seen in older subjects with type 2 diabetes who also experience hypertension, hyperlipidemia, and vascular disease. If so, we ultimately must determine which interventions can be used to prevent this progression. These are critical questions deserving of study in the upcoming years. For the sake of all people with diabetes, we must not wait to see whether dementia is the expected outcome in people growing old with diabetes before we come to understand the full impact of the disease on the brain.
FIG. 1.
Patients with diabetes have been found to have several changes in brain structure that appear to develop over time (top) and often experience conditions that present risk for subsequent cognitive dysfunction (bottom). Future study is necessary to define the natural history, structural basis, and risk factors for cognitive dysfunction in diabetes.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
Footnotes
See accompanying original article, p. 236.
REFERENCES
- 1.Ott A, Stolk RP, Hofman A, van Harskamp F, Grobbee DE, Breteler MM: Association of diabetes mellitus and dementia: the Rotterdam Study. Diabetologia 1996;39:1392–1397 [DOI] [PubMed] [Google Scholar]
- 2.Reaven GM, Thompson LW, Nahum D, Haskins E: Relationship between hyperglycemia and cognitive function in older NIDDM patients. Diabetes Care 1990;13:16–21 [DOI] [PubMed] [Google Scholar]
- 3.Cukierman-Yaffe T, Gerstein HC, Williamson JD, Lazar RM, Lovato L, Miller ME, Coker LH, Murray A, Sullivan MD, Marcovina SM, Launer LJAction to Control Cardiovascular Risk in Diabetes-Memory in Diabetes (ACCORD-MIND) Investigators Relationship between baseline glycemic control and cognitive function in individuals with type 2 diabetes and other cardiovascular risk factors: the action to control cardiovascular risk in diabetes-memory in diabetes (ACCORD-MIND) trial. Diabetes Care 2009;32:221–226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study Research Group. Jacobson AM, Musen G, Ryan CM, Silvers N, Cleary P, Waberski B, Burwood A, Weinger K, Bayless M, Dahms W, Harth J: Long-term effect of diabetes and its treatment on cognitive function. N Engl J Med 2007;356:1842–1852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kodl CT, Franc DT, Rao JP, Anderson FS, Thomas W, Mueller BA, Lim KO, Seaquist ER: Diffusion tensor imaging identifies deficits in white matter microstructure in subjects with type 1 diabetes that correlate with reduced neurocognitive function. Diabetes 2008;57:3083–3089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wessels AM, Rombouts SA, Remijnse PL, Boom Y, Scheltens P, Barkhof F, Heine RJ, Snoek FJ: Cognitive performance in type 1 diabetes patients is associated with cerebral white matter volume. Diabetologia 2007;50:1763–1769 [DOI] [PubMed] [Google Scholar]
- 7.Brands AM, Kessels RP, Hoogma RP, Henselmans JM, van der Beek Boter JW, Kappelle LJ, de Haan EH, Biessels GJ: Cognitive performance, psychological well-being, and brain magnetic resonance imaging in older patients with type 1 diabetes. Diabetes 2006;55:1800–1806 [DOI] [PubMed] [Google Scholar]
- 8.Musen G, Lyoo IK, Sparks CR, Weinger K, Hwang J, Ryan CM, Jimerson DC, Hennen J, Renshaw PF, Jacobson AM: Effects of type 1 diabetes on gray matter density as measured by voxel-based morphometry. Diabetes 2006;55:326–333 [DOI] [PubMed] [Google Scholar]
- 9.Lobnig BM, Krömeke O, Optenhostert-Porst C, Wolf OT: Hippocampal volume and cognitive performance in long-standing type 1 diabetic patients without macrovascular complications. Diabet Med 2006;23:32–39 [DOI] [PubMed] [Google Scholar]
- 10.Ferguson SC, Blane A, Perros P, McCrimmon RJ, Best JJ, Wardlaw J, Deary IJ, Frier BM: Cognitive ability and brain structure in type 1 diabetes: relation to microangiopathy and preceding severe hypoglycemia. Diabetes 2003;52:149–156 [DOI] [PubMed] [Google Scholar]
- 11.Ferguson SC, Blane A, Wardlaw J, Frier BM, Perros P, McCrimmon RJ, Deary IJ: Influence of an early-onset age of type 1 diabetes on cerebral structure and cognitive function. Diabetes Care 2005;28:1431–1437 [DOI] [PubMed] [Google Scholar]
- 12.Northam EA, Rankins D, Lin A, Wellard RM, Pell GS, Finch SJ, Werther GA, Cameron FJ: Central nervous system function in youth with type 1 diabetes 12 years after disease onset. Diabetes Care 2009;32:445–450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hershey T, Perantie DC, Wu J, Weaver PM, Black KJ, White NH: Hippocampal volumes in youth with type 1 diabetes. Diabetes 2010;59:236–241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ennis K, Tran PV, Seaquist ER, Rao R: Postnatal age influences hypoglycemia-induced neuronal injury in the rat brain. Brain Res 2008;1224:119–126 [DOI] [PMC free article] [PubMed] [Google Scholar]