Abstract
The type and amount of physical activity needed for prevention of weight regain are not well understood. We prospectively examined the associations between patterns of discretionary physical activity and 6-year maintenance of intentional weight loss among 4,558 healthy premenopausal women who were 26–45 years old in 1991 and had lost >5% of their body weight in the previous two years. Participants reported their physical activity and weight in 1991 and 1997. The outcome was weight regain, defined as regaining in 1997 >30% of the lost weight between 1989 and 1991. Between 1991 and 1997, 80% of women regained >30% of their previous intentional weight loss. An increase of 30 minutes/day in total discretionary activity between 1991 and 1997 was associated with less weight regain (−1.36kg, 95% confidence interval (CI) = −1.61, −1.12), particularly among overweight women (body mass index ≥25) (−2.45kg, −3.12 to −1.78). Increased jogging or running was associated with less weight regain (−3.26kg; −4.41 to −2.10) than increased brisk walking (−1.69kg; −2.15 to −1.22) or other activities (−1.26kg; −1.65 to −0.87). Compared to women who remained sedentary, women were less likely to regain >30% of the lost weight if they maintained 30+ minutes/day of discretionary physical activity (OR=0.69, 0.53 to 0.89) or increased to this activity level (OR=0.48, 0.39 to 0.60). Conversely, risk was elevated in women who decreased their activity. Increased physical activity, particularly high intensity activities, is associated with better maintenance of weight loss. The benefits of activity were greater among overweight/obese than normal weight women.
Keywords: Weight regain prevention, weight loss maintenance, exercise, physical activity type, duration, and intensity
Introduction
Approximately 40% of adult women in the US are trying to lose weight (1). Although many will be at least partially successful in losing weight, few will be able to maintain the weight loss (2, 3). Unfortunately, factors that promote maintenance of intentional weight loss are poorly understood.
Insufficient physical activity is a contributing factor to the obesity epidemic; nevertheless, physical activity recommendations for successful long-term weight loss maintenance have been inconsistent. Whereas several observational studies have suggested that physical activity promotes long-term weight loss maintenance (4–6), other observational studies have failed to show any benefit (7, 8). Similarly, while some randomized controlled clinical trials have shown a benefit (9, 10), others have not shown any benefit (11–14), or even a negative effect (15). Reasons for discrepancies in results include lack of a consistent definition of weight loss maintenance, differences in activity assessments, differences in study design, short follow-up, small sample size, lack of adjustment for potential confounders, and lack of adjustments for baseline body weight.
To better understand the effects of activity on weight loss maintenance in premenopausal women, we used data from the Nurses’ Health Study II, to investigate the duration and type of activity required to prevent weight regain over 6 years among women who lost more than 5% of their baseline body weight.
METHODS AND PROCEDURES
Sample
The Nurses’ Health Study II is an ongoing prospective study of 116,608 female nurses aged 25–42 years when they responded to a mailed questionnaire in 1989 about their medical history, lifestyle, and health-related behaviors. Follow-up questionnaires have been mailed biennially. Body weight was assessed on every questionnaire; physical activity (PA) was assessed on the 1991 and 1997 questionnaires, and a food frequency questionnaire has been included every 4 years starting 1991. The response rate over the follow-up years was >90%. Additional details have been reported elsewhere (16). To assess whether weight loss was intentional, two questions were asked on the 1993 questionnaire: 1) how many times participants had lost specific amounts of weight purposefully in the last 4 years, and 2) the primary methods used (e.g. low calorie diet; low fat diet; skipped meals; diet pills; commercial weight loss programs; gastric surgery; increased exercise; decreased alcohol intake; resumed/increased smoking) for their most recent weight loss of 10 or more pounds. A positive answer to any of these questions would classify the weight loss as intentional.
In this analysis, we excluded women who originally had a BMI in 1989<20 (n=253) and did not lose a clinically significant amount (>5%) of their weight between 1989 and 1991 (n=69,733) intentionally (n=194), or who had extreme weight losses (>91 kg) (n=4,824). At any point during the follow-up, women were further excluded if they had unreasonable data, i.e. weights (<38 Kg or >182 Kg) (n=581), BMI values (<15 or >55 Kg/m2) (n=2), or weight losses (>91 kg) (n=0); were no long premenopausal in 1997 (n=26,875); missed reporting their PA (n=412) or weight (n=0); reported activity values > 240 minutes/day (n=389); were pregnant or within 12-month postpartum of reporting weight (n=7,946); reported chronic conditions impairing exercise (n=442), myocardial infarction, stroke, diabetes (total n=281), or cancer (n=112) anytime through 1997 and missed reporting information on some of the covariates (n=5). After these exclusions, 4,558 women were eligible for the primary analysis. As a secondary comparative analysis of changes in PA and weight, these women with 2-year prior weight loss (n=4,558) were then compared to women without 2-year prior weight loss.
Assessment of Physical Activity and Sedentary Behavior
In 1991 and 1997, participants were asked to report the average time spent per week in the previous year in each of the following eight activities: walking or hiking, jogging (>10 minutes/mile), running (≤10 minutes/mile), bicycling, calisthenics/aerobics/aerobic dance/rowing machine, tennis/squash/racquetball, lap swimming, or mowing. For each activity, women chose one of the 11 duration categories that ranged from zero to ≥11 hours/week. Women also reported their usual walking pace: easy (<2 miles per hour [mph]), average (2–2.9 mph), brisk (3–3.9 mph), very brisk (≥4 mph), or unable to walk. Moreover, women were asked to report the average number of flights of stairs they climbed daily. Stair climbing (min/d) was then estimated. Total discretionary activity (min/d) was the sum of the duration reported in each of the nine activities. Another PA unit is the metabolic equivalent (MET) score. One MET is the energy spent at rest. The MET score is defined as the ratio of metabolic rate of an activity over the resting metabolic rate. All activities on the questionnaire were considered to be moderate-to-vigorous exercises (a MET score of 3 or more) except for walking at an easy pace. MET-hours/week for one activity is the MET score multiplied by the numbers of hours/week for that activity. The values for each activity were summed to give a total MET-hours/week. The questionnaire has been validated in a random representative sample of Nurses’ Health Study II participants (n=147) (16). Using past-week activity recalls and 7-day activity diaries as the referent methods, the correlation between activity reported on questionnaires and that of recalls was 0.79, and that reported on diaries was 0.62. Self-reported weight and height were strongly correlated in adults (r=0.97) with measured weight and height (17).
Activity cut-points were based on activity distribution in the Nurses’ Health Study II. In our sample, the mean value at baseline was 37 min/d for total discretionary activity, and the median value was 27 min/d. We chose a cut-off point of 30 min/d for low versus high total activity. Participants were cross-classified by their reported 1991 and 1997 activity levels, which yielded 4 groups: high (≥30 min/d) in both 1991 and 1997 (hi91hi97), high in 1991 and low (<30 min/d) in 1997 (hi91lo97), low in 1991 and high in 1997 (lo91hi97), and low in both 1991 and 1997 (lo91lo97). In additional analyses, total discretionary activity in 1991 and 1997 was categorized into 5 groups (≤10; 11–20; 21–30; 31–60; 61–240 min/d). The highest (>60 min/d) and the lowest (0–10 min/d) categories in 1991 were cross-classified with the five 1997 categories, which yielded 10 groups. This allowed us to assess any potential dose-response relationship between PA changes and weight regain. Similar analyses were repeated for walking and for activities “other than walking”, (i.e., moderate-to-vigorous activities). To account for walking intensity, walking MET-hours/week were used. According to Ainsworth et al., the MET intensity for walking varies between 2.0 (<2.0 mph) and 8.0 (5.0 mph) METs (18). To classify participants’ walking levels as high or low, we used a cut-off of 9 MET-hours/week (~3 hours/week of average-pace walking).
Hours/week of watching TV were used as a measure of sedentary behavior (i.e., inactivity). The question “How many hours per week do you spend: sitting at home while watching TV/VCR?” was asked in 1991 and 1997. Because TV watching has been associated with obesity (19) and thus confounds the associations with activity, we included change in hours of TV watching in our models.
Other Predictors and Confounders
Weight was assessed at baseline (1991) and on each follow-up questionnaire through 1997. Baseline body mass index (BMI; kg/m2) was calculated from height (1989) and weight (1991).
Because some components of diet have been observed to be predictive of weight gain (20–23), they were included in the analysis. Using a validated food frequency questionnaire, intakes of sugar-sweetened beverages, energy-adjusted trans-fats, dietary fiber, and alcohol were assessed in 1991 and 1995. Approximately 4% in 1991 and 9% in 1995 of these covariates had missing values; therefore an indicator variable for missing responses was created. Values in both 1991 and 1995 were included in the model to account for the changes in these covariates. Smoking status (never, past, or current) at baseline and in 1997 were included in the models. Oral contraceptive use (never, past, current), parity (nulliparous, 1, 2, 3 or more births), and anti-depressant intake (never, past, current) in 1997 were included in the analysis. All these risk factors, in addition to inactivity (1991/1997) and baseline age were controlled for in our statistical models.
Outcome Definitions
The primary outcome was 6-year weight change after an intentional weight loss of >5% of body weight between 1989 and 1991. As a secondary outcome, we assessed predictors of successful long-term weight loss maintenance, which we defined as not regaining more than 30% of the lost weight (or 1.5% of their baseline 1989 weight) after 6 years.
Statistical Methods
In the first set of analyses, multiple linear regression was used to assess the association of activity subtypes with 6-year weight change. Weight change was modeled as weight in 1997 as the outcome and baseline weight as the primary predictor. Activity was partitioned among brisk walking, non-brisk walking, jogging/running, and other activities (biking, swimming, mowing, aerobics, tennis, and stair-climbing). Estimates from linear regression models represent the comparison of weight regain in kg for every 30 min/d PA increase between 1991 and 1997, while holding the levels of other activities and other covariates constant. To assess effect modification by weight status for total discretionary PA and weight change association, the analysis was stratified by baseline weight status [underweight and normal weight (BMI<25) vs. overweight or obese (BMI≥25)].
As a comparative analysis of changes in PA and weight, women with 2-year prior weight loss were compared to those who had not lost weight.
In a second set of analyses, logistic regression was used to estimate the association between activity change (1991–1997) and risk of regaining >30% of the intentionally lost weight within six years.
RESULTS
The 1991 baseline characteristics of the study population by levels of discretionary activity are outlined in Table 1. Active women had a lower BMI at baseline, consumed more fiber, and less trans-fat and sugar-sweetened beverages. Baseline median discretionary activity was 27 min/d, while 10% of the women reported zero or less than 5 min/d. Walking was the most popular activity in this cohort, contributing to 45% of the total discretionary activity.
Table 1.
Age-standardized 1991 characteristics according to daily levels of reported discretionary physical activity among premenopausal women who had lost more than 5% of their body weight.
| Physical Activity (1991), minutes per day (min/d) | |||||
|---|---|---|---|---|---|
| <10 | 10–20 | 21–30 | 31–60 | >60 | |
| N | 954 | 799 | 720 | 1191 | 894 |
| Age, years, (mean) | 35.2 | 35.1 | 35.0 | 35.1 | 34.9 |
| Total discretionary physical activity, min/d, (mean) | 5.1 | 14.3 | 24.5 | 42.5 | 95.6 |
| Walking, min/d, (mean) | 2.7 | 6.5 | 11.3 | 18.2 | 42.3 |
| Other than walking, min/d, (mean) | 2.4 | 7.8 | 13.2 | 24.4 | 53.4 |
| Body mass index, kg/m2, (mean) | 24.2 | 24.0 | 23.8 | 23.6 | 23.5 |
| Lost weight, previous 2 years, kg, (mean) | −7.2 | −7.3 | −7.6 | −7.8 | −7.8 |
| TV watching, hours/wk, (mean) | 9.6 | 8.7 | 8.5 | 8.7 | 8.3 |
| Energy intake, kcals/day, (mean) | 1,736 | 1,742 | 1,749 | 1,716 | 1,777 |
| Alcohol intake, grams/day, (mean) | 2.6 | 2.8 | 2.8 | 3.1 | 2.9 |
| Sugar-sweetened beverage intake†, servings/day, (mean) | 0.5 | 0.4 | 0.4 | 0.3 | 0.3 |
| Trans fat‡, grams/day, (mean) | 3.4 | 3.3 | 3.1 | 3.1 | 2.9 |
| Fiber‡, grams/day, (mean) | 17.4 | 18.0 | 18.8 | 19.3 | 21.0 |
| Current smoking (%) | 14.0 | 14.2 | 12.5 | 11.9 | 12.0 |
| Oral contraceptive use (%) | 12.9 | 12.9 | 14.4 | 12.5 | 13.1 |
| Parity (mean) | 1.7 | 1.6 | 1.7 | 1.6 | 1.5 |
| Antidepressant use (%) | 1.3 | 1.5 | 2.5 | 1.3 | 2.1 |
Sugar-sweetened beverages include sugar-sweetened carbonated beverages, punch, fruit drinks, lemonade, or ice tea.
Adjusted for total energy intake.
The average 2-year weight loss between 1989 and 1991 was −7.6 ± 4.9 kg and the median was −5.9 kg. During the 6-year follow-up, the average weight change of these participants with 2-year prior weight loss was 8.4± 8.8 kg. Only 20.5% of the women in the study population were able to maintain their weight losses for at least 6 years. These women exercised more than their counterparts; their median time spent in discretionary activity increased from 25 min/d at baseline to 29 min/d in 1997, as compared to their counterparts who decreased from 27 min/d at baseline to 20 min/d in 1997. In contrast, women without prior weight loss (average 1989–1991 weight change= + 2.3± 4.0 kg) had an average weight change of + 4.1± 6.6 kg in the following 6 years.
Physical activity types and 6-year weight change after weight loss (linear regression)
Approximately 10.5% of the women increased their discretionary activity by at least 30 min/day between 1991 (mean PA= 29.5 min/d) and 1997 (mean PA= 87 min/d). Their average 6-year weight change was 5.0±7.2 kg. When PA was considered as a continuous variable, an increase of 30 min/d in total discretionary activity was significantly associated with less weight regain (−1.36 kg; 95%CI= −1.61, −1.12) (Table 2). In addition, there was a significant independent association between an increase in TV watching (by 30 min/d) and increased risk of weight regain (0.45kg; 95%CI= 0.34, 0.56).
Table 2.
Multiple linear regression models for a 30-minute/day increase in physical activity predicting 6-year weight change after intentional weight lossamong 4,558 women.
| All women | BMI<25 | BMI≥25 | |
|---|---|---|---|
| TOTAL | β (95%CI)b (kg) | β (95%CI)c (kg) | β (95%CI)c (kg) |
| Total discretionary activity (min/d) | −1.36 (−1.61, −1.12) | −1.01 (−1.24, −0.78) | −2.45 (−3.12, −1.78) |
| TV watching (min/d) | 0.45 (0.34, 0.56) | 0.30 (0.19, 0.41) | 0.62 (0.39, 0.85) |
| Partition modela | |||
| Brisk walking | −1.69 (−2.15, −1.22) | −1.19 (−1.61, −0.77) | −3.74 (−5.17, −2.31) |
| Non-brisk walking | −0.54 (−1.07, −0.02) | −0.02 (−0.54, 0.50) | −1.61 (−2.82, −0.40) |
| Jogging/Running | −3.26 (−4.41, −2.10) | −2.69 (−3.67, −1.70) | −6.66 (−11.30, −2.01) |
| Other activities | −1.26 (−1.65, −0.87) | −1.00 (−1.35, −0.64) | −2.08 (−3.17, −0.98) |
| TV watching | 0.45 (0.35, 0.56) | 0.30 (0.19, 0.41) | 0.62 (0.38, 0.85) |
Total discretionary activity partitioned among brisk walking; non-brisk walking; jogging + running; and other activities (biking, swimming, mowing, aerobics, tennis, and stair climbing). Each regression coefficient (95% CI) represents a comparison of weight regain (in kg) for every 30 min/day increase in the predictor variable;
All models are adjusted for baseline (1991) age (years), weight (1991) (kg), height (1991) (m), total average alcohol intake (1991; 1995), (0; >0-<2.5; 2.5–5; >5–10; >10 g/day); sugar-sweetened beverage intake (1991, 1995), (0; >0–0.5; >0.5–1; >1 servings/day); energy-adjusted trans-fat (1991, 1995), (≤2.5; >2.5–3; >3–4; >4 g/day); energy-adjusted fibers (1991–1995) (5–15; >15–20; >20–25; >25 g/day); oral contraceptive use (1997) (never; current; past), smoking (1989; 1997) (never; past: 0–7 pack years; past: 8+ pack years; current: >0–19 pack years; current: 20+ pack years), parity (1997) (never given birth; one birth; two births; 3+ births), anti-depressant intake (1997) (never; current; past), and hours of TV watching (1991, 1997). (maintain low level; maintain high level; increase TV watching hours; decrease TV watching hours).
All models are adjusted for the same covariates above except for baseline height.
When total activity was partitioned, the estimated weight differences associated with a 30 min/d increase were significantly greater for an increase in jogging/running (−3.26 kg; 95%CI= −4.41, −2.10) than brisk walking (−1.69 kg; 95%CI = −2.15, −1.22) or other activities (−1.26 kg; 95%CI = −1.65, −0.87) (Table 2). A 30 min/day increase in total discretionary activity predicted less weight regain (−2.45 kg; 95%CI = −3.12, −1.78) among overweight women (BMI≥25) compared with their leaner peers (−1.01 kg; 95%CI = −1.24, −0.78) (P-interaction<0.01). Brisk walking, jogging/running, and other activities were associated with less weight regain in all BMI groups, but non-brisk walking was associated with decreased weight regain only among women with excess weight (−1.61 kg; 95%CI = −2.82, −0.40).
Our weight loss maintenance definition required a weight regain in the 6-year period not exceeding 30% of prior weight loss or 1.5% of prior original weight in 1989. Based on the overall relation between change in physical activity and change in weight between 1991 and 1997, the estimated amount of PA for no increase in weight would be 3.2 hours/day for women with BMI<25 and 2.3 hours/day for women with BMI≥25.
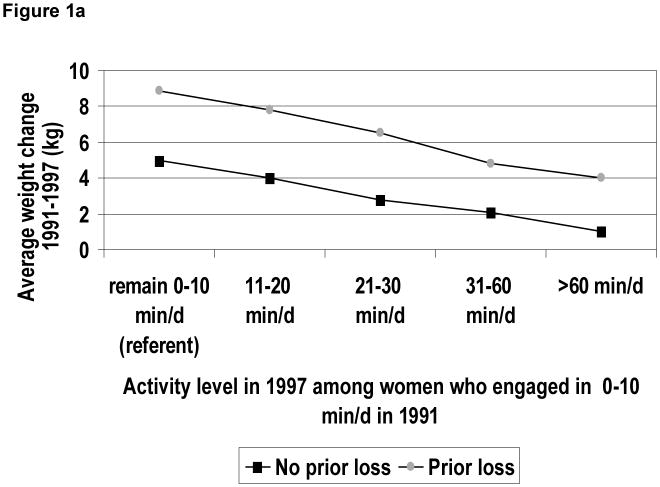
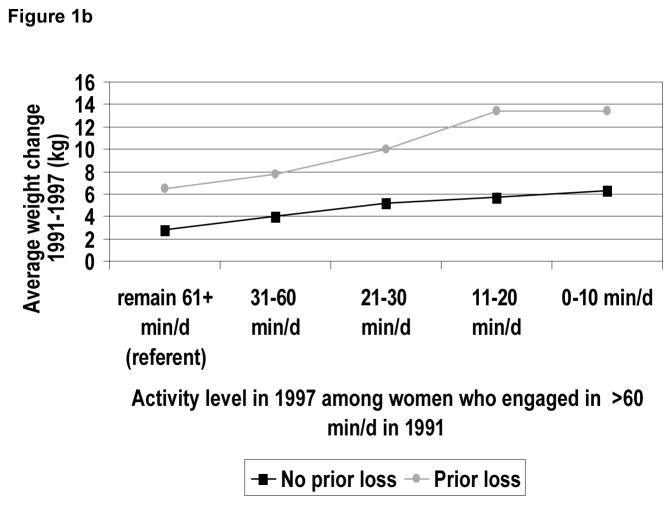
There was considerable variation in weight regain as evidenced by the distance between the 10th and the 90th percentile in weight change. For instance, over the six years, the average (unadjusted) weight regains were +8.4 kg for women with prior 2-year weight loss (10th percentile= 0 kg; 90th percentile= +20 kg). Women without 2-year prior weight loss had an average 6-year weight change of + 4.1 kg (10th percentile= −2.3 kg; 90th percentile= +11.4 kg). In terms of baseline (1991) activity in women with prior 2-year weight loss, those who remained inactive (<10 min/d) over the 6 years regained 9.0 kg (10th percentile= 0 kg; 90th percentile= +20.5 kg), and those who increased their activity up to 31–60 min/d in 1997 regained less weight on average (+4.9 kg; 10th percentile= −2.3 kg; 90th percentile= +14.5 kg) (Figure 1a). Conversely, while women who remained active (61+ min/d) over the years regained 6.6 kg (10th percentile= −0.5 kg; 90th percentile= +15.9kg), those who decreased their activity to 0–10 min/d in 1997 regained more weight on average (+13.4 kg; 10th percentile= +2.3 kg; 90th percentile= +27.3 kg) (Figure 1b). A similar pattern was observed in women without 2-year prior weight loss, but the amount of weight regain was consistently lower in this group (Figures 1a,b).
Figure 1.
Figure 1a. Average unadjusted 6-year weight change associated with increases in discretionary activity (1991–1997) among women who engaged in low physical activity (≤10 min/day) at baseline (1991).
Figure 1b. Average unadjusted 6-year weight change associated with decreases in discretionary activity (1991–1997) among women who engaged in high physical activity (>60 min/day) at baseline (1991).
Failure to maintain weight loss for 6 years
Compared with women who engaged in less than 30 min/d of activity in both 1991 and 1997, those who engaged in ≥30 min/d of discretionary activity in both 1991 and 1997 or who increased their activity pattern from low (<30 min/d) to high (≥30 min/d) in 1997 were less likely to regain >30% of lost weight (odds ratio (OR)=0.69, 95% confidence interval (CI) 0.53 to 0.89 and OR=0.48, 95% CI 0.39 to 0.60, respectively, see Table 3). Furthermore, in age-adjusted models there was a suggestion that a decrease in PA predicted weight regain (age-adjusted OR=1.30, 95%CI=1.04 to 1.61) but this association lost significance when TV watching and other covariates were in the model (OR=1.18, 95%CI=0.91 to 1.53). A decrease in TV watching was independently associated with a decreased risk of weight regain.
Table 3.
Discretionary activity and TV watching patterns and odds of weight regain throughout 6 years, among 4,558 women.
| Total activity pattern (min/d) | n | Age OR(95%CI) | MV-OR(95%CI)a |
|---|---|---|---|
| Lo91lo97 (<30 min/d in 1991 and 1997) | 1,904 | 1.00 (Referent) | 1.00 (Referent) |
| Hi91hi97 (≥30 min/d in 1991 and 1997) | 1,160 | 0.72 (0.60–0.86) | 0.69 (0.53–0.89) |
| lo91hi97 | 569 | 0.49 (0.40–0.60) | 0.48 (0.39–0.60) |
| hi91lo97 | 925 | 1.30 (1.04–1.61) | 1.18 (0.91–1.53) |
| TV watching (hours/week) | |||
| Maintain lo (<8hrs/wk in 1991 and 1997) | 1,416 | 1.00 (Referent) | 1.00 (Referent) |
| Maintain hi (8+ hrs/week in 1991 and 1997) | 1,671 | 1.16 (0.97–1.39) | 1.11 (0.92–1.34) |
| Increase inactivity | 685 | 1.29 (1.02–1.63) | 1.24 (0.97–1.58) |
| Decrease inactivity | 786 | 0.76 (0.62–0.93) | 0.75 (0.61–0.93) |
adjusted for baseline age (1991) and BMI (1991) (<25; 25+ kg/m2); total average alcohol intake (1991; 1995), (0; >0-<2.5; 2.5–5; >5–10; >10 g/day); sugar-sweetened beverage intake (1991, 1995), (0; >0–0.5; >0.5–1; >1 servings/day); energy-adjusted trans-fat (1991, 1995), (≤2.5; >2.5–3; >3–4; >4 g/day); energy-adjusted fibers (1991–1995) (5–15; >15–20; >20–25; >25 g/day); oral contraceptive use (1997) (never; current; past), smoking (1989; 1997) (never; past: 0–7 pack years; past: 8+ pack years; current: >0–19 pack years; current: 20+ pack years), parity (1997) (never given birth; one birth; two births; 3+ births), anti-depressant intake (1997) (never; current; past), and hours of TV watching (1991, 1997). (maintain low level; maintain high level; increase TV watching hours; decrease TV watching hours).
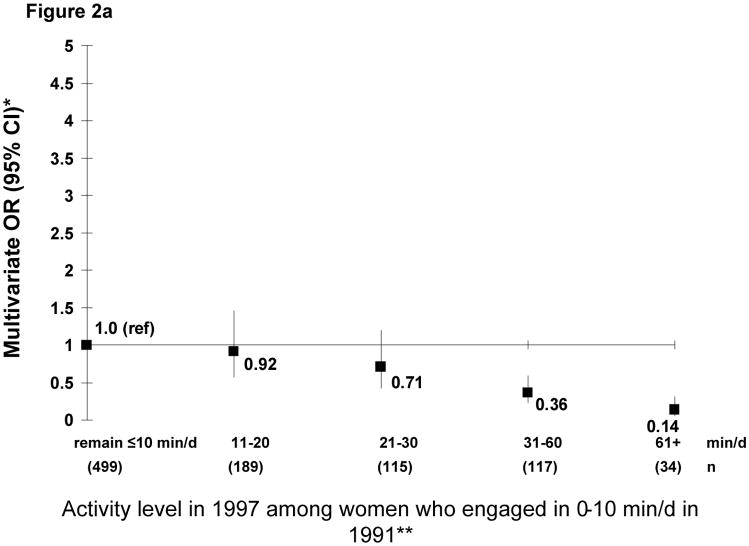
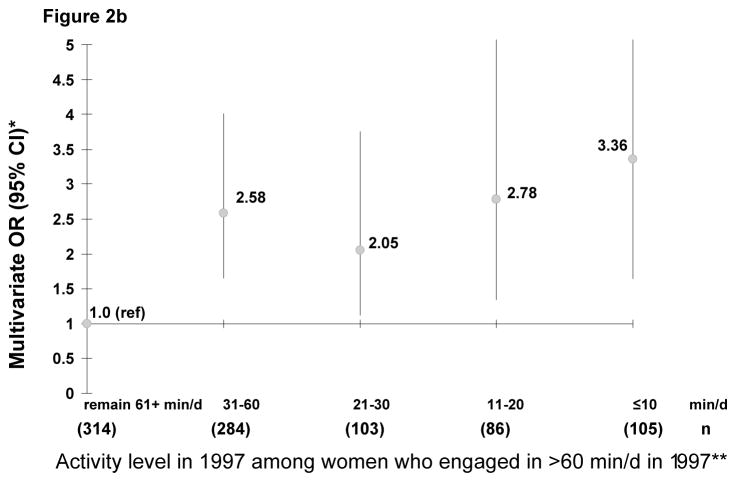
In logistic models assessing changes in min/d of total discretionary PA between 1991 and 1997, we examined activity increases among women who were initially low in activity level (0–10 min/d) (Figure 2a), and activity decreases among women who were initially high in activity level (61–240 min/d) (Figure 2b). Among the women initially low in activity, there was a significant inverse dose response relationship between increased PA and weight regain (P-trend=0.01). However, the associations were not significant for activity increases less than 31–60 min/day. Conversely, women who engaged in > 1 hour/day of activity in 1991 and decreased their total activity in 1997 to ≤1 hour/day had higher risk of weight regain as compared to those who maintained >1 hour/day (P for trend <0.001).
Figure 2.
Figure 2a. Odds Ratios (ORs) of weight regain by increases in daily minutes of discretionary activity (1991–1997) among women who engaged in low physical activity (≤10 min/day) at baseline (1991).
* adjusted for baseline age (1991) and BMI (1991) (<25; 25+ kg/m2); total average alcohol intake (1991; 1995), (0; >0-<2.5; 2.5–5; >5–10; >10 g/day); sugar-sweetened beverage intake (1991, 1995), (0; >0–0.5; >0.5–1; >1 servings/day); energy-adjusted trans-fat (1991, 1995), (≤2.5; >2.5–3; >3–4; >4 g/day); energy-adjusted fibers (1991–1995) (5–15; >15–20; >20–25; >25 g/day); oral contraceptive use (1997) (never; current; past), smoking (1989; 1997) (never; past: 0–7 pack years; past: 8+ pack years; current: >0–19 pack years; current: 20+ pack years), parity (1997) (never given birth; one birth; two births; 3+ births), anti-depressant intake (1997) (never; current; past), and hours of TV watching (1991, 1997). (maintain low level; maintain high level; increase TV watching hours; decrease TV watching hours).
** P-for-trend<0.01
Figure 2b: Odds Ratios (ORs) of weight regain by decreases in daily minutes of discretionary activity (1991–1997) among women who engaged in high physical activity (>60 min/day) at baseline (1991). * adjusted for baseline age (1991) and BMI (1991) (<25; 25+ kg/m2); total average alcohol intake (1991; 1995), (0; >0-<2.5; 2.5–5; >5–10; >10 g/day); sugar-sweetened beverage intake (1991, 1995), (0; >0–0.5; >0.5–1; >1 servings/day); energy-adjusted trans-fat (1991, 1995), (≤2.5; >2.5–3; >3–4; >4 g/day); energy-adjusted fibers (1991–1995) (5–15; >15–20; >20–25; >25 g/day); oral contraceptive use (1997) (never; current; past), smoking (1989; 1997) (never; past: 0–7 pack years; past: 8+ pack years; current: >0–19 pack years; current: 20+ pack years), parity (1997) (never given birth; one birth; two births; 3+ births), anti-depressant intake (1997) (never; current; past), and hours of TV watching (1991, 1997). (maintain low level; maintain high level; increase TV watching hours; decrease TV watching hours).
** P-for-trend<0.01
Walking intensity and duration in relation to weight loss maintenance
Because walking was the most common form of activity, it was thus investigated further. We examined the association between walking in 1991 and 1997 and risk of weight regain among women who reported walking but did not engage in any other exercise for ≥10 min/day (n=1,772). Women who maintained a high walking level (≥9 MET-hrs/week in 1991 and 1997) (OR=0.45; 95%CI=0.22–0.91) and women who increased to that level (OR=0.51; 95%CI=0.35–0.74) were less likely to regain the lost weight compared with those who maintained a low level (Table 4).
Table 4.
Association of walking (MET-hours/week) with weight regain over 6 years
| Walkinga | Walkinga | ||
|---|---|---|---|
| n | Age-OR (95%CI) | MV-OR (95%CI)b | |
| Lo91lo97 (<9 MET-hrs/week in 1991 & 1997) | 1,300 | 1.00 (Referent) | 1.00 (Referent) |
| Hi91hi97 (≥9 MET-hrs/week in 1991 & 1997) | 104 | 0.52 (0.33–0.83) | 0.45 (0.22–0.91) |
| lo91hi97 | 187 | 0.52 (0.36–0.73) | 0.51 (0.35–0.74) |
| hi91lo97 | 181 | 1.19 (0.76–1.87) | 1.00 (0.52–1.92) |
Women were excluded if they engaged in ≥10 min/day of any exercise other than walking in 1991 or 1997; women with zero activity in 1991 and 1997 were removed from this analysis.
adjusted for baseline age (1991) and BMI (1991) (<25; 25+ kg/m2); total average alcohol intake (1991; 1995), (0; >0-<2.5; 2.5–5; >5–10; >10 g/day); sugar-sweetened beverage intake (1991, 1995), (0; >0–0.5; >0.5–1; >1 servings/day); energy-adjusted trans-fat (1991, 1995), (≤2.5; >2.5–3; >3–4; >4 g/day); energy-adjusted fibers (1991–1995) (5–15; >15–20; >20–25; >25 g/day); oral contraceptive use (1997) (never; current; past), smoking (1989; 1997) (never; past: 0–7 pack years; past: 8+ pack years; current: >0–19 pack years; current: 20+ pack years), parity (1997) (never given birth; one birth; two births; 3+ births), anti-depressant intake (1997) (never; current; past), and hours of TV watching (1991, 1997). (maintain low level; maintain high level; increase TV watching hours; decrease TV watching hours).
Activities other than walking and weight loss maintenance
Activities “other than walking” included moderate-to-vigorous activities, such as jogging, running, biking, swimming, mowing, aerobics, tennis, and stair-climbing. Increasing activities from <20 min/d to 20–29 min/d (OR=0.58; 95%CI=0.43–0.78) or to 30 + min/d (OR=0.46; 95%CI=0.34–0.61) was beneficial in weight loss maintenance; however, only women who maintained 30+ min/d in 1991 and 1997 (OR=0.53; 95%CI=0.36–0.79) had a significant lower risk of weight regain by 6 years than those who maintained 20–29 min/d (OR=0.66; 95%CI=.0.41–1.07), or those who decreased their activity duration (data not shown).
DISCUSSION
To our knowledge, this study provides the first detailed results on the association between PA and weight loss maintenance in a large population-based sample of premenopausal women throughout the United States. Furthermore, our definition of successful weight loss maintenance brings novelty owing to its relativity to baseline body weight and percent of lost weight, as opposed to generalizing an absolute number of weight losses onto all the participants of heterogeneous baseline weights, as seen in other studies (4, 5, 8, 24). Approximately 20.5% of the women successfully maintained their intentional weight loss, defined as intentionally losing >5% of body weight and having regained no more than 30% of their weight loss (or 1.5% of their baseline 1989 weight) over 6 years. Although diet is an important aspect of the energy balance equation, studies have shown that exercise may be a stronger determinant than diet for long-term weight loss maintenance (25, 26). We observed that overweight and obese women who increased their activity level were more likely to regain less body weight than their peers. Also, for 30 min/d increase in exercise duration, jogging or running appears to be the most protective type of activity against weight regain. Non-brisk walking was only protective among women who were overweight or obese. Women who sustained or increased to ≥30 min/d of total discretionary PA were more likely than their peers to maintain the lost weight for 6 years, as were women who sustained ≥9 MET-Hours/week of walking (~3 hours/week of average-pace walking), and women who sustained 30+ min/d of moderate-to-vigorous activity. However, among sedentary women, PA increase had to exceed 30 min/d to be beneficial and a significant dose-response relationship with less weight regain was evident. In addition, there was an independent association between decreased TV viewing and reduced risk of weight regain.
The rationale for choosing 5% as the minimal magnitude of weight reduction was because this level is regarded as a clinically significant change, particularly in terms of weight loss (27) and in terms of reduction of risk factors of diabetes and heart disease (28). The rationale for choosing a cut off of 30% of the lost weight (or 1.5% of baseline weight) is because the literature shows that advancing years is inevitably accompanied with weight gain, even for those who maintain a steady exercise schedule (25). Hence, if we were to be stringent in our weight loss maintenance success definition and we were to allow 0% regain of the lost weight, only 11.95% of our sample would be successful maintainers (n=545) as compared to our current maintainers (20.49%; n=934).
Our data showed that higher PA levels were important for preventing weight regain. This is concordant with other studies showing that successful weight loss maintainers reported engaging in activity as part of their behavioral treatment program (4, 6, 29). Nevertheless, modest age-associated weight regains were still observed in our cohort, suggesting that maintenance of long-term weight loss appears to require increased exercise with aging. This is consistent with Jeffery and colleagues (26) who found that even relatively high PA levels may not be sufficient to protect against any weight regain. In our cohort, the estimated amount of total discretionary PA required to prevent any weight regain (zero weight regain) varied between 3.2 hours/d for lean women and 2.3 hours/day for overweight/obese women. Although few people would be willing to engage in that activity level, which is typical of many traditional lifestyles, lower amounts of activity were sufficient for women to maintain their weight loss and more moderate amounts of activity appear to have some benefits. In our cohort, while 9% of the women who maintained their body weight after 6 years reported using exercise and diet as a mean of long-term weight loss maintenance, only 0.5% of them reported using exercise alone without diet.
For clinical and public health approaches to weight control, it is commonly accepted that an energy expenditure of 150 kcal/d (~20 min/d of activity) is needed; yet there is little empirical evidence to support this speculation (26). Over time, PA guidelines have changed substantially. In 1996, the Surgeon General’s report emphasized the health benefits of engaging in moderate levels of PA (sufficient to burn 150 calories per day), such as 30 min/d of brisk walking (30) and the NIH consensus development panel advised a regular performance of 30 min/d of moderate PA to maintain the different health benefits such as coronary vascular disease prevention (31). In 2001, Wing and Hill found in a study of 3000 subjects (average 45 years) in the National Weight Control Registry that successful weight loss maintainers who lost at least 17 kg for at least 1 year exercised for about 1 hour/day; however the denominator for these successes is not known. According to the 2008 Dietary Guidelines, at least 60 to 90 minutes of daily moderate-intensity activity are needed while not exceeding caloric intake requirements to sustain weight loss (32). Our study, however, observed that PA increase to at least 31–60 min/d was necessary for weight loss maintenance over the 6-year follow-up, and participants who reduced their PA regained weight. Our findings are consistent with other studies (8, 33). Our results also showed that even higher increases (>30 min/d) were needed among sedentary women, similar to Jakicic and colleagues (34) who reported that an average PA increase by 30 to 40 min/d improved long-term weight loss maintenance in women who were overweight and sedentary. Moreover, Schoeller et al (5) found that an average of 80 min/d of moderate activity or 35 min/d of vigorous activity was needed to minimize weight regain in sedentary women. Additionally, our results indicate that greater increases in discretionary activity are needed among sedentary women who are trying to maintain weight loss than sedentary women who are trying to prevent weight gain (35). One possible explanation to why more min/d are needed for prevention of weight regain than for weight gain is that subjects with chronic excess weight may experience metabolic alterations, and may thus require more effort to achieve a substantial weight loss (36).
Although the American Dietary Guidelines recommend 60–90 min/d of PA to sustain weight loss, some adults may be discouraged by the 90 min/d recommendation and thus may not engage in any activity. Fogelholm and colleagues (37) showed that poor long-term adherence may be related to an overly time-consuming program. In our analysis, it appeared durations less than 60 to 90 min/d will on average still have benefit and will be sufficient to sustain weight loss. Furthermore, consistently with other longitudinal studies (25, 38), our results showed the benefits of activity increase in 1997, independent of baseline activity, were more than twice as high among overweight women; our results also indicated that baseline activity was not associated with 6-year weight regain prevention, similar to what we previously found with 8-year weight gain prevention (35).
Congruent with our findings that increased television watching was positively associated with weight regain, a substantial body of evidence suggested that reductions in TV viewing would result in decreases in BMI or prevalence of obesity in adolescents(39). Importantly, the effects of sedentary behavior appear to be independent of active physical activity, suggesting that weight control programs should address both of these dimensions.
There are several limitations to the present study. First, the full set of PA questions was not included on the 1993 and 1995 questionnaires; thus it is not known when during the interval activity levels changed, nor for how long the actual change was maintained. Second, there may be other types of activities such as weight training or sleep that could have an impact on body weight, we could not account for these variables because they were not included in all of our questionnaires. Also, our measurements of PA were inevitably imperfect, which will have tended to underestimate the benefits of PA and overestimate the amount of PA needed to prevent weight gain; however, this has not prevented epidemiology from identifying the importance of PA and disease in a variety of prospective cohort studies. While objective measures of PA may have been desirable, they too have error, and good validity of our PA questions has been documented (16). Third, we cannot be sure that all the weight loss between 1989 and 1991 was intentional as 1993 was the year when measures of intentional weight loss were collected; however, a strong reason that this was most likely intentional is that participants were relatively young, healthy, and they needed to be alive and respond in 1997. Fourth, dietary intake was not assessed in 1997, the follow-up year for determining change in PA and weight. However, in this analysis, excluding the dietary variables from the models did not meaningfully affect the results. Fifth, the sample was not a random sample from the United States. Moreover, we did not include women who were pregnant or recently pregnant. Thus it is not clear whether these results can be generalized to pregnancy-related weight gain; however, this relationship is more complicated and deserves a separate investigation, as discussed elsewhere (6).
Despite these limitations, our study has several strengths. First, it included a large sample of women who were followed with repeated assessments over a 6-year period. Second, the prospective design allowed us to assess the activity exposure before the weight changes’ outcome. Third, we were also able to control for sedentary behavior by measuring the total number of TV watching hours. Moreover, information on a wide variety of potentially confounding behavioral and demographic variables was collected at each assessment, which allowed us to assess activity patterns and weight change associations independent of these potential confounders. Fourth, despite the different weight loss maintenance definitions in the literature in terms of both, weight loss magnitude and maintenance duration, our continuous outcome of weight change represents a sensitivity analysis justifying our criteria when defining weight loss maintenance as a dichotomous outcome. Parallel to Wing and Hill’s definition(40) of intentionally losing at least 10% of body weight and keeping it off for a year, we defined our outcome as losing >5% of body weight and keeping it off for 6 years while remaining within 30% of weight loss (or 1.5% of initial weight). Finally, we were able to exclude women with conditions affecting weight, such as pregnancy-related or post-delivery weight gain.
Our prospective study indicates that a high PA level is needed to maintain an intentional weight loss. At least 30 min/d of moderate-to-vigorous PA are needed to prevent regaining >30% of weight loss; however, a larger increase (by at least 31–60 min/d) may be needed in sedentary women to improve weight loss maintenance. Adults who are unwilling to increase their activity level substantially should be reminded to reduce caloric intake and to engage in PA to prevent weight regain. Adults of any weight should increase their exercise as they age to prevent weight regain after weight loss.
Acknowledgments
This work was supported by grants DK072117 and CA098566 from the National Institutes for Health. We thank Susan Malspeis for her assistance in SAS programming and Dr Bernie Rosner for his invaluable suggestions to analyze these data.
Footnotes
DISCLOSURE
The authors declare no conflict of interest.
References
- 1.Williamson DF, Serdula MK, Anda RF, Levy A, Byers T. Weight loss attempts in adults: goals, duration, and rate of weight loss. Am J Public Health. 1992;82:1251–7. doi: 10.2105/ajph.82.9.1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jeffery RW, Drewnowski A, Epstein LH, et al. Long-term maintenance of weight loss: current status. Health Psychol. 2000;19:5–16. doi: 10.1037/0278-6133.19.suppl1.5. [DOI] [PubMed] [Google Scholar]
- 3.Saris WH, Blair SN, van Baak MA, et al. How much physical activity is enough to prevent unhealthy weight gain? Outcome of the IASO 1st Stock Conference and consensus statement. Obes Rev. 2003;4:101–14. doi: 10.1046/j.1467-789x.2003.00101.x. [DOI] [PubMed] [Google Scholar]
- 4.Klem ML, Wing RR, McGuire MT, Seagle HM, Hill JO. A descriptive study of individuals successful at long-term maintenance of substantial weight loss. Am J Clin Nutr. 1997;66:239–46. doi: 10.1093/ajcn/66.2.239. [DOI] [PubMed] [Google Scholar]
- 5.Schoeller DA, Shay K, Kushner RF. How much physical activity is needed to minimize weight gain in previously obese women? Am J Clin Nutr. 1997;66:551–6. doi: 10.1093/ajcn/66.3.551. [DOI] [PubMed] [Google Scholar]
- 6.Field AE, Wing RR, Manson JE, Spiegelman DL, Willett WC. Relationship of a large weight loss to long-term weight change among young and middle-aged US women. International Journal of Obesity. 2001;25:1113–21. doi: 10.1038/sj.ijo.0801643. [DOI] [PubMed] [Google Scholar]
- 7.Sarlio-Lahteenkorva S, Rissanen A, Kaprio J. A descriptive study of weight loss maintenance: 6 and 15 year follow-up of initially overweight adults. Int J Obes Relat Metab Disord. 2000;24:116–25. doi: 10.1038/sj.ijo.0801094. [DOI] [PubMed] [Google Scholar]
- 8.McGuire MT, Wing RR, Klem ML, Lang W, Hill JO. What predicts weight regain in a group of successful weight losers? J Consult Clin Psychol. 1999;67:177–85. doi: 10.1037//0022-006x.67.2.177. [DOI] [PubMed] [Google Scholar]
- 9.Fogelholm M, Kukkonen-Harjula K, Nenonen A, Pasanen M. Effects of walking training on weight maintenance after a very-low-energy diet in premenopausal obese women: a randomized controlled trial. Arch Intern Med. 2000;160:2177–84. doi: 10.1001/archinte.160.14.2177. [DOI] [PubMed] [Google Scholar]
- 10.Pavlou KN, Krey S, Steffee WP. Exercise as an adjunct to weight loss and maintenance in moderately obese subjects. Am J Clin Nutr. 1989;49:1115–23. doi: 10.1093/ajcn/49.5.1115. [DOI] [PubMed] [Google Scholar]
- 11.Perri MG, McAllister DA, Gange JJ, Jordan RC, McAdoo G, Nezu AM. Effects of four maintenance programs on the long-term management of obesity. J Consult Clin Psychol. 1988;56:529–34. doi: 10.1037//0022-006x.56.4.529. [DOI] [PubMed] [Google Scholar]
- 12.Weinstock RS, Dai H, Wadden TA. Diet and exercise in the treatment of obesity: effects of 3 interventions on insulin resistance. Arch Intern Med. 1998;158:2477–83. doi: 10.1001/archinte.158.22.2477. [DOI] [PubMed] [Google Scholar]
- 13.Wadden TA, Vogt RA, Foster GD, Anderson DA. Exercise and the maintenance of weight loss: 1-year follow-up of a controlled clinical trial. J Consult Clin Psychol. 1998;66:429–33. doi: 10.1037//0022-006x.66.2.429. [DOI] [PubMed] [Google Scholar]
- 14.Wing RR, Venditti E, Jakicic JM, Polley BA, Lang W. Lifestyle intervention in overweight individuals with a family history of diabetes. Diabetes Care. 1998;21:350–9. doi: 10.2337/diacare.21.3.350. [DOI] [PubMed] [Google Scholar]
- 15.Leermakers EA, Perri MG, Shigaki CL, Fuller PR. Effects of exercise-focused versus weight-focused maintenance programs on the management of obesity. Addict Behav. 1999;24:219–27. doi: 10.1016/s0306-4603(98)00090-2. [DOI] [PubMed] [Google Scholar]
- 16.Wolf A, Hunter D, Colditz GA, et al. Reproducibility and validity of a self-administered physical activity questionnaire. Int J Epidemiol. 1994;23:991–9. doi: 10.1093/ije/23.5.991. [DOI] [PubMed] [Google Scholar]
- 17.Rimm EB, Stampfer MJ, Colditz GA, Chute CG, Litin LB, Willett WC. Validity of self-reported waist and hip circumferences in men and women. Epidemiology. 1990;1:466–73. doi: 10.1097/00001648-199011000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Medicine and science in sports and exercise. 2000;32:S498–504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 19.Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. Jama. 2003;289:1785–91. doi: 10.1001/jama.289.14.1785. [DOI] [PubMed] [Google Scholar]
- 20.Koh-Banerjee P, Chu NF, Spiegelman D, et al. Prospective study of the association of changes in dietary intake, physical activity, alcohol consumption, and smoking with 9-y gain in waist circumference among 16 587 US men. Am J Clin Nutr. 2003;78:719–27. doi: 10.1093/ajcn/78.4.719. [DOI] [PubMed] [Google Scholar]
- 21.Schulze MB, Manson JE, Ludwig DS, et al. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. Jama. 2004;292:927–34. doi: 10.1001/jama.292.8.927. [DOI] [PubMed] [Google Scholar]
- 22.Phelan S, Wyatt H, Nassery S, et al. Three-year weight change in successful weight losers who lost weight on a low-carbohydrate diet. Obesity (Silver Spring, Md) 2007;15:2470–7. doi: 10.1038/oby.2007.293. [DOI] [PubMed] [Google Scholar]
- 23.Kruger J, Blanck HM, Gillespie C. Dietary practices, dining out behavior, and physical activity correlates of weight loss maintenance. Prev Chronic Dis. 2008;5:A11. [PMC free article] [PubMed] [Google Scholar]
- 24.Butryn ML, Phelan S, Hill JO, Wing RR. Consistent self-monitoring of weight: a key component of successful weight loss maintenance. Obesity (Silver Spring, Md) 2007;15:3091–6. doi: 10.1038/oby.2007.368. [DOI] [PubMed] [Google Scholar]
- 25.Wier LT, Ayers GW, Jackson AS, Rossum AC, Poston WS, Foreyt JP. Determining the amount of physical activity needed for long-term weight control. Int J Obes Relat Metab Disord. 2001;25:613–21. doi: 10.1038/sj.ijo.0801586. [DOI] [PubMed] [Google Scholar]
- 26.Jeffery RW, Wing RR, Sherwood NE, Tate DF. Physical activity and weight loss: does prescribing higher physical activity goals improve outcome? Am J Clin Nutr. 2003;78:684–9. doi: 10.1093/ajcn/78.4.684. [DOI] [PubMed] [Google Scholar]
- 27.World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO Consultation on Obesity; Geneva. 3–5 June 1997; Geneva: World Health Organization; 1998. [PubMed] [Google Scholar]
- 28.National Institutes of Health (NIH)/National Heart L, and Blood Institute. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity: the evidence report. Obesity research. 1998;6(Suppl 2) [PubMed] [Google Scholar]
- 29.Jakicic JM, Marcus BH, Gallagher KI, Napolitano M, Lang W. Effect of Exercise Duration and Intensity on Weight Loss in Overweight, Sedentary Women: A Randomized Trial. JAMA. 2003;290:1323–30. doi: 10.1001/jama.290.10.1323. [DOI] [PubMed] [Google Scholar]
- 30.Surgeon General’s report on physical activity and health. From the Centers for Disease Control and Prevention. Jama. 1996;276:522. [PubMed] [Google Scholar]
- 31.Physical activity and cardiovascular health. NIH Consensus Development Panel on Physical Activity and Cardiovascular Health. Jama. 1996;276:241–6. [PubMed] [Google Scholar]
- 32.U.S Department of Health and Human Services. Physical activity guidelines for Americans. 2008 [Google Scholar]
- 33.McGuire MT, Wing RR, Klem ML, Hill JO. Behavioral strategies of individuals who have maintained long-term weight losses. Obesity research. 1999;7:334–41. doi: 10.1002/j.1550-8528.1999.tb00416.x. [DOI] [PubMed] [Google Scholar]
- 34.Jakicic JM, Otto AD. Physical activity considerations for the treatment and prevention of obesity. Am J Clin Nutr. 2005;82:226S–9S. doi: 10.1093/ajcn/82.1.226S. [DOI] [PubMed] [Google Scholar]
- 35.Mekary R, Feskanich D, Malspeis S, Hu F, Willett W, Field A. Physical activity patterns and eight-year weight changes in pre-menopausal women. International Journal of Obesity. 2009 doi: 10.1038/ijo.2009.127. (In press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Leibel RL, Rosenbaum M, Hirsch J. Changes in energy expenditure resulting from altered body weight. N Engl J Med. 1995;332:621–8. doi: 10.1056/NEJM199503093321001. [DOI] [PubMed] [Google Scholar]
- 37.Fogelholm M, Kukkonen-Harjula K. Does physical activity prevent weight gain--a systematic review. Obes Rev. 2000;1:95–111. doi: 10.1046/j.1467-789x.2000.00016.x. [DOI] [PubMed] [Google Scholar]
- 38.Littman AJ, Kristal AR, White E. Effects of physical activity intensity, frequency, and activity type on 10-y weight change in middle-aged men and women. International journal of obesity (2005) 2005;29:524–33. doi: 10.1038/sj.ijo.0802886. [DOI] [PubMed] [Google Scholar]
- 39.Swinburn B, Shelly A. Effects of TV time and other sedentary pursuits. International journal of obesity (2005) 2008;32 (Suppl 7):S132–6. doi: 10.1038/ijo.2008.249. [DOI] [PubMed] [Google Scholar]
- 40.Wing RR, Hill JO. Successful weight loss maintenance. Annu Rev Nutr. 2001;21:323–41. doi: 10.1146/annurev.nutr.21.1.323. [DOI] [PubMed] [Google Scholar]