Abstract
Object
A Glasgow Coma Scale (GCS) score of 3 on presentation in patients with severe traumatic brain injury due to blunt trauma has been recognized as a bad prognostic factor. The reported mortality rate in these patients is very high, even approaching 100% in the presence of fixed and dilated pupils in some series. Consequently, there is often a tendency to treat these patients less aggressively because of the low expectations for a good recovery. In this paper, the authors’ purpose is to report their experience in the management of this patient population, analyzing the mortality rate, prognostic factors, and functional outcome of survivors.
Methods
The authors performed a retrospective review of patients who presented between 1997 and 2007 with blunt head trauma and a GCS score of 3. Demographics, mechanism of injury, examination, blood alcohol level, associated injury, intracranial pressure (ICP), surgical procedures, and outcome were all recorded.
Results
A total of 189 patients met the inclusion criteria and were included in this study. The overall mortality rate was 49.2%. At the 6-month follow-up, 13.2% of the entire series achieved a good functional outcome (Glasgow Outcome Scale [GOS] score of 1 or 2).
The patient population was then divided into 2 groups: Group 1 (patients who survived [96]) and Group 2 (patients who died [93]). Patients in Group 1 were younger (mean 33.3 ± 12.8 vs 40.3 ± 16.97 years; p = 0.002) and had lower ICP on admission (mean 16.3 ± 11.1 vs 25.7 ± 12.7 mm Hg; p < 0.001) than those in Group 2. The difference between the 2 groups regarding sex, mechanism of injury, hypotension on admission, alcohol, surgery, and associated injuries was not statistically significant.
The presence of bilateral fixed, dilated pupils was found to be associated with the highest mortality rate (79.7%). Although not statistically significant because of the sample size, pupil status was also a good predictor of the functional outcome at the 6-month follow-up; a good functional outcome (GOS Score 1 or 2) was achieved in 25.5% of patients presenting with bilateral reactive pupils, and 27.6% of patients presenting with a unilateral fixed, dilated pupil, compared with 7.5% for those presenting with bilateral fixed, nondilated pupils, and 1.4% for patients with bilateral fixed, dilated pupils.
Conclusions
Overall, 50.8% of patients survived their injury and 13.2% achieved a good functional outcome afterat 6 months of follow-up (GOS Score 1 or 2). Age, ICP on admission, and pupil status were found to be significant predictive factors of outcome. In particular, pupil size and reactivity appeared to be the most important prognostic factor since the mortality rate was 23.5% in the presence of bilateral reactive pupils and 79.7% in the case of bilateral fixed, dilated pupils. The authors believe that patients having suffered traumatic brain injury and present with a GCS score of 3 should still be treated aggressively initially since a good functional outcome can be obtained in some cases.
Keywords: blunt head injury, Glasgow Coma Scale, outcome
To date, head injury remains the leading cause of death and severe disability in young adults,1,11,14 and it is also the most important single injury contributing to traumatic mortality and morbidity. In a large study of patients who suffered trauma, it was found that the presence of head injury resulted in a 1.5-times increase in death when compared with the presence of extracranial injuries but no head trauma.6
Multiple independent risk factors predicting the outcome of patients with severe head injuries have been identified, the most widely accepted ones being age, GCS score, pupil reactivity, CT scanning findings, and associated extracranial injuries.2,4,12 In particular, a GCS score of 3 at presentation has been associated with a significantly poor outcome.3,8,13 Due to the high mortality rate, even approaching 100% when the score is associated with bilateral fixed and dilated pupils in some series,13 questions have been raised as to whether these patients should be treated aggressively, and whether they have any chance of a meaningful recovery.
Consequently, an accurate early prediction of survival and functional outcome appears to be of paramount importance and allows for informed counseling of relatives and helps the treating physician in deciding the aggressiveness of treatment. In this series, we report our experience in the treatment of patients with blunt head trauma presenting with a GCS score of 3. Our primary objective was to determine the overall mortality and 6-month functional outcome. Our secondary objective was to identify risk factors allowing prediction of mortality and morbidity in this patient population.
Methods
The records of patients with head injury who presented to the emergency center at Ben Taub General Hospital (a level I trauma center) between 1997 and 2007 were reviewed. Inclusion criteria were as follows: blunt mechanism head trauma, documented neurological examination prior to administration of sedation or paralytics, and a GCS score of 3 on presentation. Exclusion criteria included the following: penetrating head injury and dead-on-arrival. Patient demographics (age, sex, and race), mechanism of injury, time to reach the hospital, neurological examination findings on presentation (including GCS score and pupils size and reactivity), hemodynamic status, AIS scores, Injury Severity Score, alcohol level, associated injury, head CT scanning findings, ICP on presentation, treatment, surgical procedures, and outcome at the 6-month follow-up were all recorded. Dilated pupils were defined as ≥ 4 mm in diameter to allow comparison of the results with other similar published reports.13 The outcome was reported as death or survival: in the case of death, the time elapsing between presentation and death was recorded; in the case of survival, the functional outcome at the 6-month of follow-up was reported using the GOS score. The 6-month follow-up data were determined by a neuropsychology technician through direct interviews with the patients in the clinic or occasionally by phone when the direct interview was not possible.
The subsequent analysis was done by comparing 2 groups. Group 1 included patients who survived, and Group 2 included patients who died. Results were compared using either the chi-square test or Student t-test to determine the statistical significance of the differences observed. A statistically significant difference was indicated by a probability value < 0.05.
Medical Treatment
The medical treatment was performed according to a standard protocol. All patients underwent CT scanning of the brain in the emergency room on presentation. Patients with a surgically treatable mass (SDH, EDH, large contusion with mass effect, and so on) were taken immediately to the operating room. A decompressive craniectomy was performed concomitantly to the evacuation of a SDH in some cases; the decision to perform the craniectomy or not was made by the operating surgeons based on the intraoperative findings. All patients underwent ICP monitor insertion at presentation either in the intensive care unit or intraoperatively in the case of a surgically treatable lesion. All patients were intubated and sedated. The head of the bed was kept elevated at 30°. Patients were kept euvolemic and isothermic, and enteral feeding was started 24 hours after admission. Hypotensive episodes were treated using fluid replacement and vasopressors. Intra cranial pressure levels > 20 mm Hg were treated with ventricular drainage of CSF, mannitol, and moderate hyperventilation (PaCO2 35 mm Hg). If treatment of raised ICP was not successful, barbiturate coma with burst suppression was induced. Decompressive craniectomy was then indicated for the management of intractable high ICP if all other measures failed.
Results
A total of 189 patients (157 male and 32 female patients) met our inclusion criteria and were included in the study. The mean age was 36.5 years (range 13–82 years). The mechanisms of injury included MVA in 77 patients (40.7%), auto-pedestrian accident in 42 patients (22.2%), fall in 30 patients (15.9%), assault in 18 patients (9.5%), and unknown in 22 patients (11.6%). Mean values are presented ± SDs.
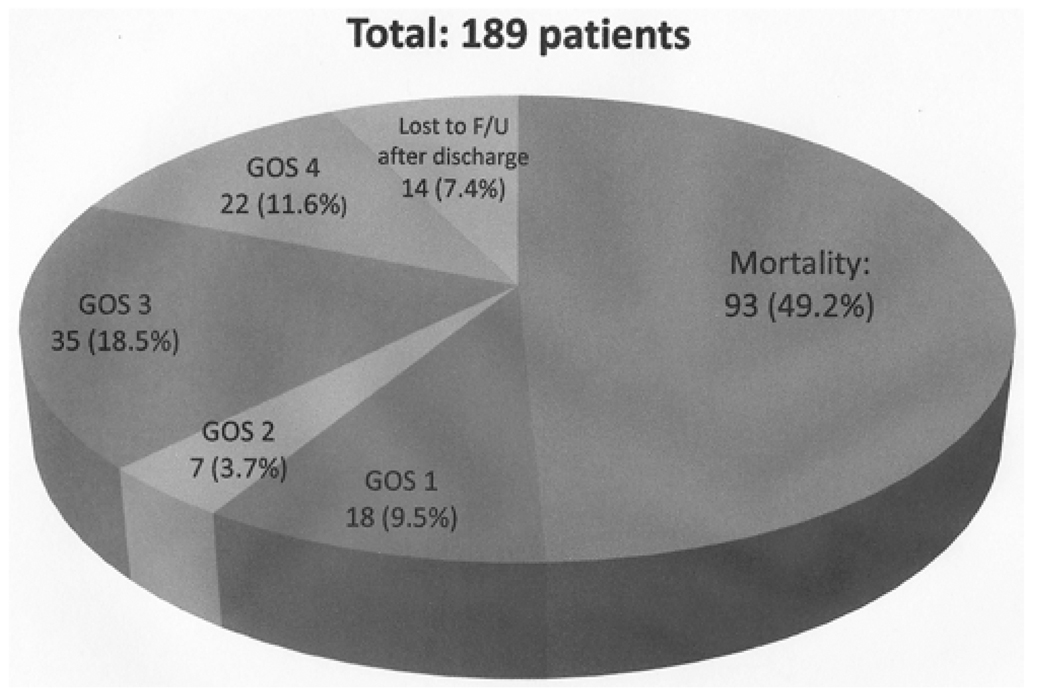
Overall, 93 patients died and 96 survived (overall mortality rate 49.2%). The deaths occurred on average 8.1 days after presentation (range 0–88 days). All survivors were discharged from the hospital to their home, to a nursing home, or most commonly to a rehabilitation center. A 6-month follow-up study was available in 82 of 96 survivors; GOS scores of 1, 2, 3, and 4 were achieved in 18 (22.0%), 7 (8.5%), 35 (42.7%), and 22 (26.8%) patients, respectively (Fig. 1).
Fig. 1.
Diagram showing the overall outcome of the 189 patients with blunt head injury and a GCS score of 3 at presentation. F/U = follow-up.
The alcohol level on presentation was documented in 125 patients (66.1% of the series); the level was negative in 71 patients and positive in 54 patients. The mortality rates were 46.3 and 43.6% in the alcohol-negative and alcohol-positive groups, respectively. The difference in the mortality rates observed in these 2 groups was not statistically significant (p = 0.91)
The patient population was then divided into 2 groups: Group 1, patients who survived and Group 2, patients who died. Characteristics of the patients in each group are summarized in Table 1. Patients in Group 1 were younger (mean 33.3 ± 12.8 vs 40.3 ± 16.97 years; p = 0.002) and had lower ICP on admission (mean 16.3 ± 11.1 vs 25.7 ± 12.7 mm Hg; p < 0.001). The difference between the 2 groups in terms of sex ratio, mechanisms of injury, presence of hypotension on presentation, alcohol, associated extracranial injuries (defined as the presence of ≥ 1 other organ with a serious injury AIS score ≥ 3) was not statistically significant.
TABLE 1.
Characteristics of the patients in the 2 groups*
| Characteristic | Group 1 (patients who survived) |
Group 2 (patients who died) |
p Value |
|---|---|---|---|
| no. of patients | 96 | 93 | |
| mean age (yrs) | 33.3 ± 12.8 | 40.3 ± 16.97 | 0.002 |
| sex (M/F) | 78/18 | 79/14 | 0.629 |
| mechanism of injury | 0.098 | ||
| MVA | 48 | 29 | |
| auto vs pedestrian | 20 | 22 | |
| assault | 8 | 10 | |
| fall | 11 | 19 | |
| unknown | 9 | 13 | |
| no. of patients w/ hypotension on presentation | 17 | 24 | 0.240 |
| alcohol | 0.558 | ||
| positive | 29 | 25 | |
| negative | 40 | 31 | |
| unknown | 27 | 37 | |
| op | 49 | 61 | 0.006 |
| mean ICP on presentation (mm Hg) | 16.3 ± 11.1 | 25.7 ± 12.7 | <0.001 |
| mean ISS | 30.19 ± 9.24 | 29.47 ± 7.81 | 0.562 |
| no. of patients w/ ≥1 other organ w/ serious injury (AIS score ≥3) | 27 | 24 | 0.845 |
| pupil size & reactivity | <0.001 | ||
| bilat reactive | 39 | 12 | |
| unilat fixed, dilated | 20 | 9 | |
| bilat fixed not dilated | 23 | 17 | |
| bilat fixed, dilated | 14 | 55 |
Values represent the number of patients, unless stated otherwise. Mean values are presented as ± SD. Abbreviation: ISS = Injury Severity Score.
Surgery was performed in 110 patients; patients most commonly underwent surgery for evacuation of an SDH. The other indications for surgery included large contusions with mass effect and midline shift, and decompressive craniectomy for severe brain edema. In 12 cases, a decompressive craniectomy was done concomitantly with the evacuation of an SDH; 6 of these patients survived and 6 died. Although not statistically significant, surgical interventions were more common in Group 2. Among those who underwent evacuation of an SDH, the addition of a decompressive craniectomy did not appear to have a significant influence on the outcome in this series; the mortality rate was 50% with decompressive craniectomy (6 of 12) compared with 48.3% without craniectomy (29 of 60). Of note, 5 patients underwent surgery mainly for an EDH, and 4 of them survived.
Group 1 patients were also more likely to have bilateral reactive pupils (41% in Group 1 vs 12.9% in Group 2), whereas those in Group 2 patients were more likely to have bilateral fixed and dilated pupils (14.6% in Group 1 vs 59.1% in Group 2). The pupil size and reactivity were significant predictors of the mortality rate (Table 2). The mortality rate was the highest in the presence of bilateral fixed and dilated pupils (p < 0.001) and lowest in the presence of bilateral reactive pupils. A multivariate analysis was performed and confirmed that age, ICP, and pupil status were independent predictive factors of survival, while other factors such as alcohol, sex, and extracranial injuries did not appear to have a significant influence.
TABLE 2.
Pupil size and reactivity at presentation as a predictor of mortality rate
| Pupil Status | No. of Patients | Mortality Rate (%) |
|---|---|---|
| bilat reactive | 51 | 23.5 |
| unilat fixed & dilated | 29 | 31.0 |
| bilat fixed not dilated | 40 | 42.5 |
| bilat fixed dilated | 69 | 79.7 |
There was also a correlation between the pupil status on presentation and the 6-month functional outcome. Patients who presented with bilateral reactive pupils or unilateral fixed, dilated pupils were more likely to achieve a good outcome (GOS Score 1 or 2) than those who presented with bilateral fixed (dilated or not) pupils (Table 3 and Table 4). Statistical analysis was not done for this part because the numbers were small and because of a significant number of patients who were lost to follow-up.
TABLE 3.
Outcome at 6 months in 82 of 96 patients who survived stratified by pupil status on presentation
| GOS Score |
||||
|---|---|---|---|---|
| Pupil Status | 1 | 2 | 3 | 4 |
| bilat reactive | 9 | 4 | 14 | 3 |
| unilat fixed & dilated | 7 | 1 | 7 | 4 |
| bilat fixed not dilated | 1 | 2 | 10 | 9 |
| bilat fixed, dilated | 1 | 0 | 4 | 6 |
TABLE 4.
Outcome of patients stratified by the size and reactivity of their pupils on presentation
| No. of Patients (%) |
|||||
|---|---|---|---|---|---|
| Pupil Status | Dead | GOS Score 3 or 4 |
GOS Score 1 or 2 |
Lost to Follow- Up |
Total |
| bilat reactive | 12 (23.5) | 17 (33.3) | 13 (25.5) | 9 (17.6) | 51 |
| unilat fixed, dilated | 9 (31.0) | 11 (37.9) | 8 (27.6) | 1 (3.4) | 29 |
| bilat fixed, not dilated | 17 (42.5) | 19 (47.5) | 3 (7.5) | 1 (2.5) | 40 |
| bilat fixed, dilated | 55 (79.7) | 10 (14.5) | 1 (1.4) | 3 (4.3) | 69 |
Among all patients who presented with bilateral fixed, dilated pupils, only 1 ultimately achieved a good functional outcome. This was a 43-year-old man who sustained a head injury after an MVA. He was found to have an acute SDH and underwent surgical evacuation with decompressive craniectomy on an emergency basis. He had slow progressive recovery thereafter. Three other patients were lost to follow-up after discharge from the hospital, so their functional outcome at 6 months was unknown (Table 4).
Discussion
Overall Mortality Rate and Functional Outcome
In published series reporting the outcome of patients with severe blunt head injury, a GCS score of 3 on presentation has been found to be a particularly poor prognostic factor. Fearnside et al.5 reported a mortality rate 65%, and Phuenpathom et al.10 reported a mortality rate of 100% in patients with acute SDH and a GCS score 3. This has resulted in an ongoing debate as to whether these patients should be treated aggressively.
Few series have exclusively studied this patient population. Tien et al.13 retrospectively reviewed a series of 173 patients who suffered blunt head trauma and had a GCS score of 3. They reported in-hospital mortality rates 100% in patients with bilateral fixed, dilated pupils (104 patients) and 42% in patients with reactive pupils (69 patients). The overall mortality rate was 76.8%. Admittedly, patients with bilateral fixed, dilated pupils were treated less aggressively despite the fact that they were more likely to have a surgically treatable hemorrhage. A similar outcome was reported by Lieberman et al.9 who reported 100% mortality in the case of fixed, dilated pupils and 66.6% mortality in the case of reactive pupils.
However, other published series have reported a lower mortality rate with a number of patients achieving good recovery, arguing that aggressive treatment should not be denied to these patients. Demetriades et al.3 reviewed their experience in managing head injury in patients with a GCS score of 3 on admission. The mortality rate in blunt head trauma was 65%; however, when they excluded patients with no vital signs on presentation and those with major extracranial injuries the mortality rate decreased to 52%. Of patients who survived in their series (combining blunt and penetrating head injuries), 10% had a good functional outcome at the time of hospital discharge. Waxman et al.15 found a mortality rate of 64% in 117 patients. Of those who survived, 13 achieved a good recovery (GOS Score 1 in 10 patients and GOS Score 2 in 3 patients). As a result, 11.1% of the patients had a good functional outcome, knowing that follow-up data were not available for 17 of the survivors. In addition in the series reported by Lieberman et al.,9 a number of patients were found to be completely independent on follow-up (of 33 patients with GCS score of 3 and reactive pupils, 11 survived and 3 were completely independent).
In this series, we report a lower mortality rate than that in other studies (23.5% in the case of bilateral reactive pupils and 79.7% in the case of bilateral fixed, dilated pupils). Two main factors can potentially account for this. The first factor is age; the mean age of survivors was 33.3 years and that of those who died was 40.3 years. Most of the other reported series had a higher mean age (40.6 and 42.4 years in the fixed, dilated pupils group and 50.2 and 39.3 years in the reactive pupils group for the series reported by Lieberman et al.9 and Tien et al.,13 respectively). The other factor is the aggressiveness in the management; in our center patients with a GCS score of 3 are treated similarly aggressively to other patients with severe blunt head injury. The relatively high percentage of patients treated surgically is a reflection of this management strategy. Although surgeries were more frequent in Group 2, it would be impossible to predict the overall survival and functional outcome had a more conservative approach been adopted. In accordance with the findings of Waxman et al.,15 we found that 13.2% of the entire series achieved a good functional outcome, knowing that overall 7.4% were lost to follow-up after their discharge from the hospital.
Pupil Size and Reactivity
Pupil size and reactivity was found to be a strong predictor of survival and functional outcome in this series. The best outcome was observed in patients with bilateral reactive pupils (mortality rate 23.5%; good outcome rate 25.5%), and the worst was seen in patients with bilateral fixed, dilated pupils (mortality rate 79.7%; good outcome rate 1.5%). Patients with unilateral fixed, dilated pupil and bilateral fixed, nondilated pupils had an intermediate outcome (mortality rate 31 and 42.5%; good outcome rate 27.5 and 7.5%, respectively). Pupil status has been widely recognized as a strong prognostic factor in this setting.9,10,13 Although the presence of fixed, dilated pupils in association with a GCS score of 3 has led to a 100% mortality rate in a number of studies,9,13 our findings show that survival and even good outcome (although very rare) are still possible. Some of the limitations of using fixed, dilated pupils as an absolute prognostic factor can be related to direct facial and eye trauma,7 prior eye surgery, recent ophthalmological examination, unreported administration before or during transfer of certain medications, and so on.
A GCS Score of 3 and EDH
Although the number of patients with EDHs in this series is very small, their apparently better outcome deserves special interest. Five patients underwent surgery for evacuation of an EDH, and 4 of them survived. Similarly, Kotwica et al.,8 found that in a series of 111 patients with blunt head injury and a GCS score of 3, patients with EDH fared much better than the rest in the series. Although the overall mortality rate of the series was 89%, 4 of 8 patients who underwent surgery for evacuation of an EDH survived. Large series of patients with EDHs and a GCS score of 3 on presentation are lacking; however, it appears that this subgroup of patients has a significantly higher survival rate than those with other types of intracranial injuries. In general, we believe that patients who present with a GCS score of 3 due to mass effect from a hematoma (especially an EDH) have a higher chance of survival and functional recovery than patients whose neurological status is mainly caused by diffuse shear injury.
Limitations of the Study
This study has several weaknesses that should be accounted for. Due to the retrospective nature of the study conclusions related to predictive factors of outcome should be taken with caution. Furthermore, a number of data were not available (alcohol level for a number of patients), and several patients were lost to follow-up adding to the limitations of the analysis. Consequently a simple statistical analysis (rather than a detailed one) was performed to determine the main factors that appeared to influence the outcome. Although the overall outcome is likely related to the aggressive medical and surgical management undertaken, the potential impact of such a management strategy could only be indirectly evaluated by comparing our results to those of others where a more conservative attitude was advocated.
Conclusions
We believe that patients with blunt head injury presenting with a GCS score of 3 should be treated aggressively. Our results showed that 50.8% of these patients survived their injury and 13.2% achieved a good functional outcome at the 6-month follow-up. Younger age, lower ICP on presentation, and the presence of reactive pupils were identified as the main prognostic factors in this patient population. There was also a trend toward a higher survival rate in the case of EDHs; however, the number of patients was too small to draw strong conclusions.
Abbreviations used in this paper
- AIS
Abbreviated Injury Scale
- EDH
epidural hematoma
- GCS
Glasgow Coma Scale
- GOS
Glasgow Outcome Scale
- ICP
intracranial pressure
- MVA
motor vehicle accident
- SDH
subdural hematoma
Footnotes
Disclosure
This study is supported by an NIH Grant No. P01-NS38660. The authors report no other conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
References
- 1.Alexander E., Jr Global Spine and Head Injury Prevention Project (SHIP) Surg Neurol. 1992;38:478–479. doi: 10.1016/0090-3019(92)90124-6. [DOI] [PubMed] [Google Scholar]
- 2.Chesnut RM, Marshall LF, Klauber MR, Blunt BA, Baldwin N, Eisenberg HM, et al. The role of secondary brain injury in determining outcome from severe head injury. J Trauma. 1993;34:216–222. doi: 10.1097/00005373-199302000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Demetriades D, Kuncir E, Velmahos GC, Rhee P, Alo K, Chan LS. Outcome and prognostic factors in head injuries with an admission Glasgow Coma Scale score of 3. Arch Surg. 2004;139:1066–1068. doi: 10.1001/archsurg.139.10.1066. [DOI] [PubMed] [Google Scholar]
- 4.Eisenberg HM, Gary HE, Jr, Aldrich EF, Saydjari C, Turner B, Foulkes MA, et al. Initial CT findings in 753 patients with severe head injury. A report from the NIH Traumatic Coma Data Bank. J Neurosurg. 1990;73:688–698. doi: 10.3171/jns.1990.73.5.0688. [DOI] [PubMed] [Google Scholar]
- 5.Fearnside MR, Cook RJ, McDougall P, McNeil RJ. The West-mead Head Injury Project outcome in severe head injury. A comparative analysis of pre-hospital, clinical and CT variables. Br J Neurosurg. 1993;7:267–279. doi: 10.3109/02688699309023809. [DOI] [PubMed] [Google Scholar]
- 6.Gennarelli TA, Champion HR, Copes WS, Sacco WJ. Comparison of mortality, morbidity, and severity of 59,713 head injured patients with 114,447 patients with extracranial injuries. J Trauma. 1994;37:962–968. doi: 10.1097/00005373-199412000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Goebert HW., Jr Head injury associated with a dilated pupil. Surg Clin North Am. 1970;50:427–432. doi: 10.1016/s0039-6109(16)39090-9. [DOI] [PubMed] [Google Scholar]
- 8.Kotwica Z, Jakubowski JK. Head-injured adult patients with GCS of 3 on admission—who have a chance to survive? Acta Neurochir (Wien) 1995;133:56–59. doi: 10.1007/BF01404948. [DOI] [PubMed] [Google Scholar]
- 9.Lieberman JD, Pasquale MD, Garcia R, Cipolle MD, Mark Li P, Wasser TE. Use of admission Glasgow Coma Score, pupil size, and pupil reactivity to determine outcome for trauma patients. J Trauma. 2003;55:437–442. doi: 10.1097/01.TA.0000081882.79587.17. [DOI] [PubMed] [Google Scholar]
- 10.Phuenpathom N, Choomuang M, Ratanalert S. Outcome and outcome prediction in acute subdural hematoma. Surg Neurol. 1993;40:22–25. doi: 10.1016/0090-3019(93)90164-v. [DOI] [PubMed] [Google Scholar]
- 11.Pickett W, Ardern C, Brison RJ. A population-based study of potential brain injuries requiring emergency care. CMAJ. 2001;165:288–292. [PMC free article] [PubMed] [Google Scholar]
- 12.Signorini DF, Andrews PJ, Jones PA, Wardlaw JM, Miller JD. Predicting survival using simple clinical variables: a case study in traumatic brain injury. J Neurol Neurosurg Psychiatry. 1999;66:20–25. doi: 10.1136/jnnp.66.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tien HC, Cunha JR, Wu SN, Chughtai T, Tremblay LN, Brenneman FD, et al. Do trauma patients with a Glasgow Coma Scale score of 3 and bilateral fixed and dilated pupils have any chance of survival? J Trauma. 2006;60:274–278. doi: 10.1097/01.ta.0000197177.13379.f4. [DOI] [PubMed] [Google Scholar]
- 14.Valadka AB. Injury to the Cranium. In: Mattox KL, Feliciano DV, Moore EE, editors. Trauma. ed 4. New York: McGraw- Hill; 2000. pp. 377–399. [Google Scholar]
- 15.Waxman K, Sundine MJ, Young RF. Is early prediction of outcome in severe head injury possible? Arch Surg. 1991;126:1237–1242. doi: 10.1001/archsurg.1991.01410340079011. [DOI] [PubMed] [Google Scholar]