Abstract
Burkholderia mallei is a facultative intracellular pathogen that causes severe disease in animals and humans. Recent studies have shown that the cluster 1 type VI secretion system (T6SS-1) expressed by this organism is essential for survival in a hamster model of glanders. To better understand the role of T6SS-1 in the pathogenesis of disease, studies were initiated to examine the interactions of B. mallei tssE mutants with RAW 264.7 murine macrophages. Results obtained by utilizing modified gentamicin protection assays indicated that although the tssE mutants were able to survive within RAW 264.7 cells, significant growth defects were observed in comparison to controls. In addition, analysis of infected monolayers by differential interference contrast and fluorescence microscopy demonstrated that the tssE mutants lacked the ability to induce multinucleated giant cell formation. Via the use of fluorescence microscopy, tssE mutants were shown to undergo escape from lysosome-associated membrane protein 1-positive vacuoles. Curiously, however, following entry into the cytosol, the mutants exhibited actin polymerization defects resulting in inefficient intra- and intercellular spread characteristics. Importantly, all mutant phenotypes observed in this study could be restored by complementation. Based upon these findings, it appears that T6SS-1 plays a critical role in growth and actin-based motility following uptake of B. mallei by RAW 264.7 cells.
Burkholderia mallei is a nonmotile, facultative intracellular, Gram-negative bacillus that causes glanders in humans and animals. This zoonotic pathogen is an obligate animal parasite that is primarily responsible for disease in solipeds (26, 41, 50, 64). In Asia, the Middle East, Africa, and South America, where glanders remains endemic, chronically infected horses are the only known reservoir of this host-adapted pathogen (35). Disease in equines presents as chronic or acute illnesses characterized by lung involvement, ulcerative nasal/tracheal lesions, and visceral abscess formation. Human infections, although rare, are thought to be acquired via the inoculation of mucocutaneous tissues with aerosols or secretions from diseased animals. The clinical progression of human glanders is similar to that observed in solipeds and may manifest as chronic or acute localized infections, acute pulmonary infections, or fulminating septicemias. Diagnosis and treatment of disease can be challenging, and in the absence of chemotherapeutic intervention, human glanders is invariably fatal (3, 16, 63). At present, there are no human or veterinary vaccines available for immunization against the disease. Due to the high risk of aerosol infection and the potential for misuse of this organism as an agent of biological warfare and terrorism, B. mallei is currently listed as a select agent by the Centers for Disease Control and Prevention (CDC) (43, 60).
B. mallei has been shown to express several important virulence factors that are required for survival in a variety of animal models of infection (18, 32, 45, 56, 57). Included among these are a capsular polysaccharide, lipopolysaccharide, a complex quorum-sensing system, an animal pathogen-like type III secretion system (T3SSAP) and the VirAG two-component regulatory system (10, 13, 18, 36, 56, 57). B. mallei is a facultative intracellular pathogen that can survive and replicate in number of eukaryotic cell lines (11, 24, 42). Following uptake, this pathogen escapes from endocytic vacuoles into the host cell cytoplasm where it uses actin-based motility to promote intra- and intercellular spread (42, 51). Recent studies have demonstrated that T3SSAP is essential for early vacuolar escape and survival in J774.2 murine macrophages (42). It also appears that the T3SSAP is necessary for intra- and intercellular actin-based motility by providing B. mallei access to intracellular pools of actin (56). Interestingly, B. mallei is also known to stimulate multinucleated giant cell (MNGC) formation, a unique phenomenon that is thought to be due in part to actin motility-induced fusion of host cell membranes (11, 24). At present, little else is known regarding the molecular mechanisms used by this organism to persist within eukaryotic cells or how this organism specifically evades innate and acquired host immune defenses.
Type VI secretion (T6S) is a recently characterized mechanism for protein transport that is widespread among Gram-negative bacteria that interact closely with eukaryotic cells (6, 14, 21, 65). Several studies have shown that T6S systems (T6SSs) are key virulence determinants expressed by a variety of bacterial pathogens (33, 34, 39, 45, 66). Although relatively little is known about the structure and function of the T6S apparatus, there is mounting evidence suggesting that these systems are similar in nature to bacteriophage tail complexes (30, 37, 38). Associated with these systems are a set of conserved T6SS core proteins including T4SS IcmF- and IcmH/DotU-like proteins, a putative outer membrane lipoprotein (SciN), a ClpV ATPase, an interacting pair of proteins (VipA/VipB) that form tubules, hemolysin-coregulated pilus (Hcp), and valine glycine repeat (VgrG) homologs (8, 14). The IcmF, IcmH, and SciN are predicted to be structural components of the T6S apparatus while VipA, VipB, and ClpV are critical for T6SS assembly and function (14). Hcp and VgrG have been shown to be secreted via T6S and are predicted to be important both as effectors and as components of the T6SS machinery (19, 38, 66). Recent studies suggest that Hcp and VgrG may be involved in puncturing host cell membranes (14, 38). In general, T6SSs appear to be highly regulated at the genetic level and typically involve two-component systems, transcriptional activator proteins, or posttranslational regulation (1, 17, 19, 33, 39, 45). In a variety of pathogens, the upregulation of T6SS gene clusters has been shown to occur following interactions with host cells (17, 22, 33, 34, 46).
Four intact T6SS gene clusters have been identified in the B. mallei ATCC 23344 genome (45). The cluster 1 T6SS (T6SS-1) is part of the VirAG regulon and is essential for B. mallei virulence in the hamster model of glanders (45). T6SS-1 consists of 19 genes including homologs of the eight conserved core components associated with most T6SSs (14, 45). This gene cluster is adjacent to and is coregulated with virAG and the Burkholderia intracellular motility genes (bimBCADE) (45). T6SS-1 has been shown to be expressed in vivo and can be activated in vitro by overexpression of the VirAG two-component system or the AraC-type regulator BMAA1517 (45). Mass spectroscopy studies have demonstrated that when VirAG is overexpressed in B. mallei, Hcp1 is the major protein secreted into culture supernatants (45). In addition, both tssD and tssE, genes predicted to encode components of the T6SS-1 apparatus, appear to be required for Hcp1 secretion (45).
At present, the specific function of B. mallei T6SS-1 remains undefined. In order to address this, we utilized a combination of molecular genetic, cellular, and immunological approaches to characterize the interactions of B. mallei tssE mutants with RAW 264.7 murine macrophages. The main objective of this study was to develop a better understanding of the role of T6SS-1 in the pathogenesis of disease caused by this organism.
MATERIALS AND METHODS
Bacterial strains, growth conditions, and reagents.
The bacterial strains used in this study are described in Table 1. Escherichia coli strains were grown at 37°C on Luria Bertani-Lennox (LBL; Difco) agar or in LBL broth. B. mallei strains were grown at 37°C on LBL agar or in LBL broth supplemented with 4% glycerol (LB4G). Brucella agar (Difco) supplemented with 4% glycerol (BB4G) was used for plate counts. When appropriate, antibiotics were added at the following concentrations: 25 μg/ml kanamycin (Km), 50 μg/ml zeocin (Zeo), or 15 μg/ml polymyxin B (Pm) for E. coli and 5 μg/ml kanamycin or zeocin for B. mallei. For macrophage survival assays, bacteria were subcultured 1:100 into LB4G broth from overnight cultures and grown at 37°C for ∼4 h. Bacterial stocks were maintained at −80°C as 20% glycerol suspensions. All studies utilizing viable Burkholderia pseudomallei and B. mallei were conducted under biosafety level three containment. Zeocin was purchased from Invitrogen. Unless stated otherwise, all reagents were purchased from Sigma.
TABLE 1.
Strains and plasmids used in this study
| Strain or plasmid | Relevant characteristic(s) | Reference or source |
|---|---|---|
| E. coli strains | ||
| TOP10 | General cloning strain; Kms Zeos | Invitrogen |
| S17-1 | Mobilizing strain; transfer genes of RP4 integrated on chromosome: Pms Kms Zeos | 48 |
| B. pseudomallei ΔsctUBp3 | DD503 derivative; ΔbsaZ | 61 |
| B. mallei strains | ||
| ATCC 23344 | Type strain; isolated in 1944 from a human case of glanders; Pmr Gms Kms Zeos | 36 |
| SR1A | ATCC 23344 derivative; sucrose-resistant; Δ(BMAA0437-BMAA0497) Pmr Gms Kms Zeos | This study |
| BM0739 | SR1A derivative; ΔtssE Pmr Gms Kms Zeos | This study |
| BM0739G | SR1A derivative; ΔtssE::gfp Pmr Gms Kms Zeos | This study |
| BM1533 | SR1A derivative; ΔbsaZ Pmr Gms Kms Zeos | This study |
| BM0739Z | SR1A derivative; ΔtssE::gfp ΔbsaZ Pmr Gms Kms Zeos | This study |
| Plasmids | ||
| pEM7/Zeo | Sh ble cassette vector; Zeor | Invitrogen |
| pEX18Tc | Gene replacement vector; sacB lacZα oriT Tcr | 25 |
| pEX18Zeo | pEX18Tc derivative containing Sh ble cassette from pEM7/Zeo; sacB lacZα oriT Zeor | This study |
| pGRV2-ΔA0739 | pGRV2 containing tssE with an internal 135-bp deletion; Gmr | 45 |
| pEX18Z-ΔtssE | pEX18Zeo containing tssE with an internal 135-bp deletion; Zeor | This study |
| pEX18Z-ΔtssEgfp | pEX18Z-ΔtssE containing a promoterless gfp amplified from pBHR4-GFP; Zeor | This study |
| pEX18Z-ΔbsaZ | pEX18Zeo containing bsaZ with an internal 1,063-bp deletion; Zeor | This study |
| pBHR1 | Broad-host-range cloning vector; pBBR1 oriR oriT Cmr Kmr | MoBiTec |
| pA0739 | pBHR1 derivative containing a wild-type copy of B. mallei tssE; Kmr | 45 |
| pBHR2-virAG | pBHR1 derivative containing a wild-type copy of B. mallei virAG; Kmr | 45 |
| pBHR4-GFP | Broad-host-range vector containing gfp from pQBI T7 GFP (Quantum Biotech); Gmr | 45 |
| pBHR1-TG | pBHR1 containing gfp amplified from pBHR4-GFP with gfp-upE/gfp-RMCS; Kmr | This study |
| pA0739G | pBHR1-TG containing a wild-type copy of B. mallei tssE downstream of gfp; Kmr | This study |
Recombinant DNA techniques.
DNA manipulations were performed using standard methods. Restriction enzymes (New England BioLabs), shrimp alkaline phosphatase (SAP; Promega), and Klenow DNA polymerase (Promega) were used according to manufacturer's instructions. PCR was performed using an Expand High Fidelity PCR System (Roche Applied Science). PCR and restriction digested products were purified using a QIAquick Gel Extraction Kit (Qiagen). Ligation reactions were performed using a Fast-Link Quick Ligase Kit (Epicentre Technologies). Plasmids were purified using a QIAprep Spin Miniprep Kit (Qiagen). Genomic DNA was purified using a Wizard Genomic DNA Purification kit (Promega). Chemically competent Escherichia coli TOP10 cells were transformed as per the manufacturer's instructions (Invitrogen). Oligonucleotide primers were obtained from Integrated DNA Technologies (Coralville, IA). DNA sequencing was performed by ACGT, Inc. (Wheeling, IL). The oligonucleotide primers used in this study are described in Table 2.
TABLE 2.
Oligonucleotide primers used in this study
| Primer | Sequence (5′-3′)a |
|---|---|
| zeo-F | TGTTGACAATTAATCATCGGC |
| EXZeo-E | AGCGGATAACAATTTCACACAGG |
| EXZeo-H | GATTAAGTTGGGTAACGCCAGGG |
| tssE-FKp | CATGGGTACCGAGCTGTATCTGTTCGGCTGCGTG |
| tssE-RH | CATGAAGCTTAGGGGTTGAGCTGTTCGATCAACGG |
| bsaZ-FKp | CATGGGTACCCTTCACGTCACGTCATGCCGAGCGACACG |
| bsaZ-RH | CATGAAGCTTTGTTGGCTAGTGGTCGTTCCC |
| gfp-upSal | CATGGTCGACCTTTGTTAGCAGCCGGATCC |
| gfp-dnSal | CATGGTCGACCCCCTCTAGAAATAATTTTG |
| gfp-upE | CATGGAATTCCTTTGTTAGCAGCCGGATCC |
| gfp-RMCS | CATGCCATGGAAGCTTGAGCTCGGTACCGGATCCTCTAGATCAGTTGTACAGTTCATCCATGCC |
Restriction sites in the linker regions are underlined.
Construction of pEX18Zeo and pBHR1-TG.
The plasmids used in this study are described in Table 1. To facilitate allelic exchange, the sacB-based gene replacement vector pEX18Zeo was constructed as follows. Briefly, pEX18Tc was digested with EcoRV and NruI to excise the tetracycline resistance marker and then dephosphorylated with SAP. In addition, pEM7/Zeo was digested with XhoI and EcoRI, following which the reaction mixture was treated with Klenow DNA polymerase to yield a ∼450-bp blunt-ended DNA fragment harboring the Sh ble ORF. The ∼450-bp fragment was then cloned into the pEX18Tc backbone creating pEX18Zeo. Orientation of the Sh ble ORF was confirmed by sequencing of pEX18Zeo constructs using the zeo-F primer.
For complementation studies, the tandem expression vector pBHR1-TG was constructed as follows. Briefly, the gfp-up/gfp-RMCS primer pair was used to PCR amplify the gfp allele from pBHR4-GFP (where GFP is green fluorescent protein). The PCR product was then digested with EcoRI and NcoI and cloned into pBHR1 digested with the same enzymes. To facilitate cloning of tssE downstream of the constitutively expressed gfp allele, BamHI-KpnI-SacI-HindIII restriction sites were incorporated into the primer gfp-RMCS.
Mutant construction and complementation.
To facilitate the construction of mutant strains, a spontaneous sucrose-resistant derivative of B. mallei ATCC 23344, designated SR1A, was obtained and confirmed as previously described (55). Gene replacement experiments with B. mallei SR1A were performed using the sacB-based allelic exchange vector pEX18Zeo. To construct pEX18Z-ΔtssE, the tssE-FKp/tssE-RH primer pair was used to PCR amplify the ΔtssE allele from pGRV2-ΔA0739. The PCR product was then digested with KpnI and HindIII and cloned into pEX18Zeo digested with the same enzymes. To construct pEX18Z-ΔtssEgfp, a promoterless gfp was PCR amplified from pBHR4-GFP using the gfp-upSal/gfp-dnSal primer pair. The PCR product was then digested with SalI and cloned into pEX18Z-ΔtssE digested with the same enzyme. To construct pEX18Z-ΔbsaZ, the bsaZ-FKp/bsaZ-RH primer pair was used to PCR amplify the ΔbsaZ allele from B. pseudomallei ΔsctUBp3 genomic DNA. The PCR product was then digested with KpnI and HindIII and cloned into pEX18Zeo digested with the same enzymes.
To construct the mutants used in this study, E. coli S17-1 was used to mobilize the pEX18Zeo derivatives into the various B. mallei strains via conjugative mating for 18 h at 37°C. To select for transconjugates, conjugation mixtures were plated onto LB4G-Zeo-Pm agar and incubated for 48 h at 37°C. To isolate sucrose-resistant colonies, individual transconjugates were streaked onto M9 minimal medium agar containing 0.4% glucose and 5% sucrose and incubated for 4 to 5 days at 37°C. Sucrose-resistant colonies were then screened for the presence of mutant alleles by PCR. To construct pA0739G for complementation experiments, the tssE-FKp/tssE-RH primer pair was used to PCR amplify a wild-type copy of tssE from B. mallei ATCC 23344 genomic DNA. The PCR product was then digested with KpnI and cloned into pBHR1-TG digested with KpnI and ScaI. E. coli S17-1 was used to mobilize all of the broad-host-range plasmids into the various B. mallei strains as described above.
Cell culture.
The murine macrophage cell line RAW 264.7 (ATCC TIB-71) was obtained from the American Type Culture Collection (ATCC, Rockville, MD). Cells were maintained in Dulbecco's modified Eagle's medium (DMEM; Invitrogen) supplemented with 10% (vol/vol) heat-inactivated fetal bovine serum (FBS; Invitrogen) and a standard mixture of antibiotics (100 U/ml penicillin, 100 μg/ml streptomycin, and 250 μg/ml amphotericin B) at 37°C under an atmosphere of 5% CO2. For macrophage survival assays and microscopy studies, RAW 264.7 cells were resuspended in DMEM supplemented with FBS (DMEM-10), transferred into the wells of 24-well tissue culture plates, with or without coverslips, and incubated overnight.
Macrophage survival assays.
Bacterial uptake and survival were quantitated using modified gentamicin protection assays as previously described (11). In brief, bacterial suspensions (∼1 × 106 CFU) were added onto RAW 264.7 cells (∼1 × 106 cells/well) in triplicate. Monolayers were incubated with the bacteria for 1 h and then washed twice with Hanks' balanced salt solution (HBSS; Invitrogen) to remove extracellular bacteria. Fresh DMEM-10 containing 200 μg/ml Gm was then added to suppress the growth of residual extracellular bacteria. Monolayers were lysed at various time points postinfection with 0.2% (vol/vol) Triton X-100, and serial dilutions of the lysates were plated onto BB4G agar and incubated at 37°C for 48 h. Plate counts were then used to enumerate bacterial loads. Uptake and intracellular survival were routinely quantified at 3 and 24 h postinfection. For time course experiments, uptake and survival were quantitated at 3, 6, 12, 18, and 24 h postinfection.
Immunofluorescence staining and microscopy.
RAW 264.7 cells (∼2.5 × 105 to 5 × 105 cells/well) were grown overnight on 12-mm glass coverslips (Fisher Scientific) in 24-well tissue culture plates. For MNGC and actin polymerization studies, monolayers were infected with the B. mallei strains using ∼1 × 106 to ∼1 × 108 CFU. For all other assays, monolayers were infected using ∼1 × 107 CFU. For all assays, infected monolayers were washed with phosphate-buffered saline (PBS), fixed with 2.5% paraformaldehyde (PFA) for 15 min, and then washed extensively with PBS prior to staining with specific antibodies, phalloidin (Invitrogen), or DRAQ5 (Alexis Biochemicals). Monolayers were immunostained at room temperature essentially as previously described (11, 29).
To facilitate differential staining of extracellular versus intracellular bacteria, RAW 264.7 cells were infected for 3 h, fixed, and then stained with the B. mallei lipopolysaccharide (LPS)-specific 3D11 monoclonal antibody (MAb; Research Diagnostics Inc), diluted 1:1,000 in PBS containing 10% normal goat serum (Invitrogen) in the absence of a permeabilizing agent. Cells were then washed several times with PBS containing 0.05% (wt/vol) saponin (S-PBS) and incubated with Alexa Fluor 568 goat anti-mouse IgG (Invitrogen) diluted 1/800 in PBS containing 10% normal goat serum and 0.1% (wt/vol) saponin (SS-PBS).
For lysosome-associated membrane protein 1 (LAMP-1) colocalization studies, RAW 264.7 cells were infected for 3 h, fixed, and stained with the rat anti-mouse LAMP-1 clone 1D4B MAb (Developmental Studies Hybridoma Bank) diluted 1:100 in SS-PBS. Monolayers were then washed several times with S-PBS and incubated with Alexa Fluor 568 goat anti-rat IgG (Invitrogen) and DRAQ5 diluted 1/800 and 1/2,000, respectively, in SS-PBS. Association of SR1A (pBHR1-TG) and BM0739G (pBHR1) with LAMP-1-positive vacuoles was quantitated by scoring the colocalization phenotypes of at least 50 individual bacteria from each of three different coverslips. Percent association was then expressed as the mean ± standard deviation.
To assess MNGC or actin motility phenotypes, RAW 264.7 cells were infected with B. mallei strains as per the macrophage survival assays. For assays utilizing a multiplicity of infection (MOI) of ≥10, infected monolayers were also incubated in the presence of 200 μg/ml aminoguanidine (AG) (11, 47). At 12 and 24 h postinfection, monolayers were fixed and incubated with Alexa Fluor 568-phalloidin (Invitrogen) and DRAQ5 diluted 1/200 and 1/2,000, respectively, in SS-PBS.
Following staining, coverslips were washed with PBS, rinsed with water, and then mounted onto glass slides with Mowiol. Fluorescence and differential interference contrast (DIC) microscopy were performed with a Nikon Eclipse 90i imaging system using either a CFI Plan Fluor 40×/0.75 objective or a CFI Plan APO VC 60×/1.4 oil objective (Nikon Instruments Inc.). Images were acquired using NIS-Elements Advanced Research software (Nikon Instruments Inc.).
Transmission electron microscopy (TEM).
RAW 264.7 cells (∼5 ×105 cells/well) were grown overnight on 13-mm diameter Thermanox coverslips (Nunc, Inc., Naperville, IL) in 24-well tissue culture plates and infected with B. mallei strains (∼1 × 107 CFU) in the presence of 200 μg/ml AG as per macrophage survival assays (11). At 6 h postinfection, monolayers were washed and then fixed overnight in 100 mM sodium cacodylate buffer (pH 7.2) containing 2.5% glutaraldehyde and 4% PFA. Samples were then prepared for TEM as previously described (12). Ultrathin sections were obtained using an MT-7000 ultra microtome (Research and Manufacturing Company, Inc.) and collected on 200-mesh copper grids. Images were obtained using a Philips CM-10 TEM (Philips) with a bottom-mounted AMT (Advanced Microscopy Techniques) camera. Chemicals used for TEM sample preparation were obtained from either Ted Pella, Inc., or Electron Microscopy Services.
RESULTS
B. mallei T6SS-1 is expressed following uptake by RAW 264.7 cells.
Previous studies have shown that B. mallei T6SS-1 mutants are avirulent in the hamster model of glanders (45). To better understand the role of T6SS-1 in the pathogenesis of disease caused by B. mallei, we initiated studies to characterize the interactions of tssE mutants with RAW 264.7 murine macrophages. To facilitate these studies, we constructed both B. mallei BM0739 (ΔtssE) and B. mallei BM0739G (ΔtssE::gfp) strains. To confirm the phenotype of the green fluorescent protein (GFP) reporter strain, BM0739G was transformed with pBHR2-virAG or the vector control pBHR1. Consistent with previous observations, BM0739G grown in LB4G medium or DMEM-10 did not express GFP unless virAG was overexpressed from the multicopy plasmid (data not shown).
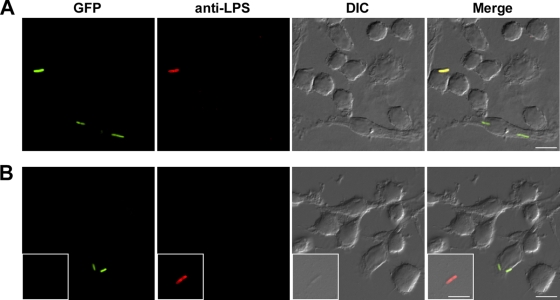
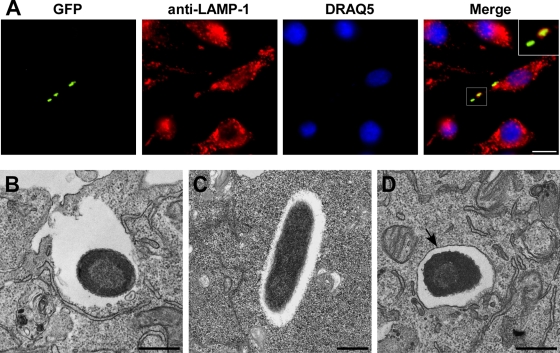
To determine if T6SS-1 was expressed following uptake by RAW 264.7 cells, monolayers were infected with BM0739G (pBHR1). For control purposes, monolayers were also infected with BM0739G (pBHR2-virAG). At 3 h postinfection, monolayers were fixed, stained, and then examined using a combination of DIC and fluorescence microscopy. To enable differentiation between intracellular and extracellular bacteria, the fixed monolayers were stained with a B. mallei-specific MAb under nonpermeabilizing conditions. As predicted, analysis of BM0739G (pBHR2-virAG)-infected monolayers demonstrated that while both the intracellular and extracellular bacteria expressed GFP, only the extracellular bacteria reacted with the MAb, thus exhibiting red fluorescence (Fig. 1A). In contrast, analysis of BM0739G (pBHR1)-infected monolayers demonstrated that while the extracellular bacteria exhibited red fluorescence, only the intracellular bacteria expressed GFP (Fig. 1B). These findings indicated that B. mallei T6SS-1 was expressed following interaction with RAW 264.7 cells and that internalization was required for operon expression.
FIG. 1.
T6SS-1 is expressed following uptake of B. mallei by RAW 264.7 macrophages. Monolayers infected with B. mallei BM0739G (pBHR2-virAG) or BM0739G (pBHR1) were fixed at 3 h postinfection, immunostained under nonpermeabilizing conditions, and examined by DIC and fluorescence microscopy. GFP-expressing bacteria are shown in green while extracellular bacteria stained with the 3D11 MAb are shown in red. (A) Constitutive expression of GFP by B. mallei BM0739G (pBHR2-virAG). (B) Inducible expression of GFP by BM0739G (pBHR1) following uptake into RAW 264.7 cells; inset demonstrates inability of extracellular bacteria to express GFP. Micrographs are representative of at least three independent experiments. Scale bar, 10 μm.
tssE is required for optimal growth of B. mallei in RAW 264.7 cell monolayers.
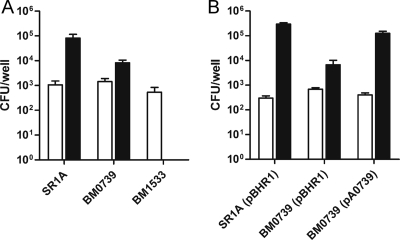
Several studies have shown that B. mallei can survive and replicate in J774.2 and RAW 264.7 murine macrophage cell lines (11, 42, 45, 47). To examine the ability of B. mallei tssE mutants to survive within RAW 264.7 cells, bacterial uptake and intracellular survival phenotypes were characterized utilizing modified gentamicin-protection assays. Monolayers were infected with SR1A (parent strain), BM1533 (T3SSAP mutant), or BM0739 at an MOI of 1. Following uptake (3 h), results indicated that intracellular levels of bacteria were similar for all three strains (Fig. 2A). Quantitation of bacterial loads at 24 h postinfection, however, demonstrated that while intracellular levels of SR1A increased ∼100-fold over the course of the assay, BM1533 was completely cleared from the monolayers (Fig. 2A). In addition, although BM0739 could be recovered from infected monolayers, bacterial loads were ∼10-fold lower than those of the parent strain, indicating an apparent growth defect (Fig. 2A). Similar results were also observed for BM0739G (data not shown). Importantly, this phenotype could be complemented since expression of a plasmid-borne copy of tssE by BM0739 (pA0739) restored growth of the deletion mutant back to wild-type levels (Fig. 2B).
FIG. 2.
B. mallei tssE mutants exhibit apparent growth defects in RAW 264.7 macrophages. Monolayers were infected with the various B. mallei strains at an MOI of 1. Bacterial uptake (white bars) and intracellular survival (black bars) were quantitated at 3 h and 24 h postinfection, respectively. (A) Uptake and survival phenotypes of B. mallei parent and mutant strains. (B) Complementation analysis of B. mallei BM0739 harboring pA0739 (tssE+) or pBHR1 (vector control). Values represent the means ± standard deviations (SDs) of three independent experiments.
To determine if the growth phenotype associated with the tssE mutants was due to survival or replication defects, a time course assay was performed. Following infection of the RAW 264.7 monolayers, intracellular loads of SR1A, BM1533, and BM0739 were quantitated at various time points postinfection. As expected, uptake levels (3 h) were similar for all three strains (Fig. 3). Consistent with previous results, analysis of SR1A-infected monolayers demonstrated that bacterial loads increased ∼100-fold over 24 h while BM1533 was rapidly cleared from monolayers by 6 h postinfection (Fig. 3). Interestingly, while the growth rates of BM0739 were similar to the growth of SR1A between 3 and 12 h, they began to slow between 12 and 24 h postinfection (Fig. 3). Importantly, the growth rates of BM0739 and SR1A were virtually identical when they were grown in LB4G medium (data not shown). Based upon these findings, it appears that B. mallei tssE mutants do not exhibit overt survival defects in RAW 264.7 cell monolayers. It cannot be ruled out, however, that the slower growth rate of the tssE mutants between 12 and 24 h may be due in part to enhanced sensitivity to macrophage effectors.
FIG. 3.
Survival and replication kinetics of B. mallei strains in RAW 264.7 cells. Monolayers were infected with B. mallei SR1A (black circles), BM0739 (white circles), or BM1533 (black diamonds) at an MOI of 1, and intracellular loads of bacteria were enumerated at 3, 6, 12, 18, and 24 h postinfection. Values represent the means ± SDs of three independent experiments.
B. mallei tssE mutants do not induce MNGC formation following infection of RAW 264.7 monolayers.
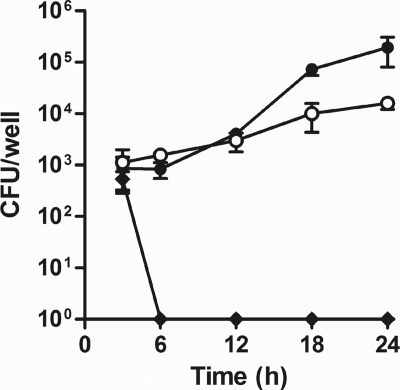
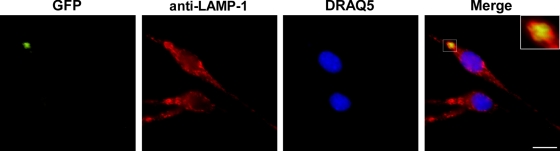
Previous studies have shown that B. mallei induces MNGC formation following infection of RAW 264.7 cells (11, 24). Consistent with these findings, SR1A and BM0739 (pA0739) caused RAW 264.7 cell monolayers to undergo obvious morphological changes during the course of the uptake/survival assays. Interestingly, however, no such changes were associated with BM0739-infected monolayers during the same time frame (data not shown). To further investigate this phenomenon, coverslips seeded with RAW 264.7 cells were infected with strain SR1A (pBHR1-TG), BM0739 (pBHR1-TG), or BM0739 (pA0739G) that constitutively expresses GFP from plasmid-borne copies of gfp. At 12 and 24 h postinfection, monolayers were fixed, stained, and examined by DIC and fluorescence microscopy. Results of these studies demonstrated that monolayers infected with SR1A (pBHR1-TG) and BM0739 (pA0739G) consistently exhibited the presence of MNGC formation Fig. 4A, B, and C). In contrast, no evidence of MNGCs was observed in monolayers infected with BM0739 (pBHR1-TG, Fig. 4D and E). In addition, when monolayers were infected at an MOI of 2, high numbers of GFP-expressing bacteria were associated only with those monolayers exhibiting MNGC formation (Fig. 4B, C, and E), which was consistent with results from the uptake/survival studies. Importantly, even when monolayers were infected with 100-fold more BM0739 (pBHR1-TG) than SR1A (pBHR1-TG), no evidence of MNGC formation was observed at 24 h postinfection (Fig. 4F). Taken together, these findings suggest that B. mallei T6SS-1 is required for both MNGC formation and optimal intracellular growth.
FIG. 4.
RAW 264.7 cell monolayers infected with B. mallei tssE mutants do not exhibit MNGC formation. Monolayers infected with B. mallei SR1A (pBHR1-TG) (A and B), BM0739 (pA0739G) (C), or BM0739 (pBHR1-TG) (D, E, and F) were fixed at 12 (A and D) or 24 h (B, C, E, and F) postinfection, stained, and examined by DIC and fluorescence microscopy. For panels A to E, monolayers were infected at an MOI 2. For panel F, monolayers were infected at an MOI of 200. Bacteria expressing GFP are shown in green while the nuclei stained with DRAQ5 are shown in blue. Micrographs are representative of at least three independent experiments. Scale bar, 50 μm.
B. mallei tssE mutants undergo vacuolar escape following uptake by RAW 264.7 cells.
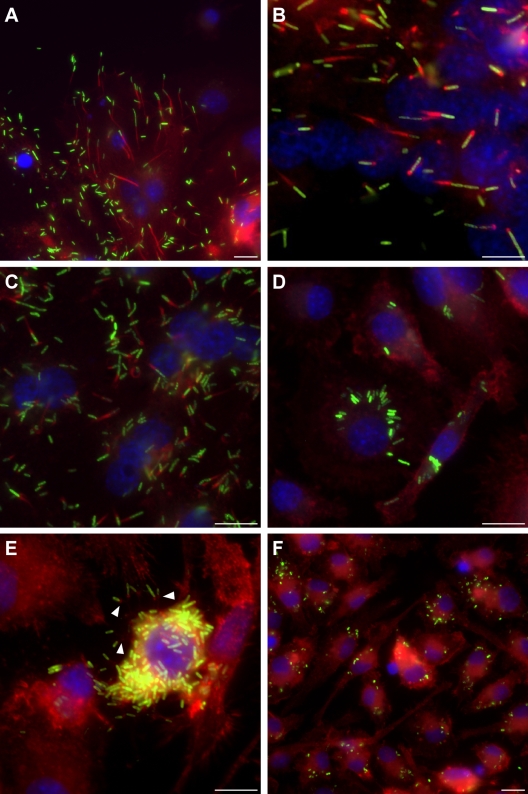
Previous studies have shown that B. mallei must escape from LAMP-1-positive vacuoles in order to survive and replicate in J774.2 cells (42). In addition, it has also been shown that T3SSAP plays a critical role in this process (42). Because the tssE mutants examined in this study exhibited apparent growth defects following uptake by RAW 264.7 cells, studies were initiated to determine what role, if any, T6SS-1 might play in vacuolar escape. To facilitate these studies, coverslips seeded with RAW 264.7 cells were infected with B. mallei SR1A (pBHR1-TG), BM0739G (pBHR1), and BM1533 (pBHR1-TG). To determine whether the tssE mutant or control strains were capable of undergoing escape from LAMP-1-associated vacuoles, monolayers were washed, fixed, and then stained with the 1D4B MAb prior to examination by fluorescence microscopy. Consistent with previous observations, SR1A (pBHR1-TG) was found to promote escape from LAMP-1-positive vacuoles, whereas the T3SSAP mutant, BM1533 (pBHR1-TG), was unable to do so (data not shown). Importantly, and similar to the parent strain, BM0739G (pBHR1) was shown to both associate with and then escape from LAMP-1-positive vacuoles (Fig. 5A). Additionally, quantitative analyses revealed no obvious differences between the LAMP-1 colocalization phenotypes of SR1A (pBHR1-TG; 21.6% ± 4.4% association) and BM0739G (pBHR1; 26.9% ± 1.3% association) at 3 h postinfection.
FIG. 5.
B. mallei tssE mutants undergo escape from LAMP-1-associated vacuoles. (A) Fluorescence micrographs of RAW 264.7 cells infected with B. mallei BM0739G (pBHR1). Monolayers were fixed at 3 h postinfection, immunostained, and visualized by fluorescence microscopy. Intracellular bacteria expressing GFP are shown in green, LAMP-1 stained with the 1D4B MAb is shown in red, and the nuclei stained with DRAQ5 are shown in blue. (B to D) Transmission electron micrographs of B. mallei-infected RAW 264.7 cells. Monolayers infected with B. mallei SR1A (B), BM0739 (C), or BM1533 (D) were fixed at 6 h postinfection and examined by TEM. The black arrow in panel D indicates the vacuolar membrane associated with the T3SSAP mutant. All micrographs are representative of at least three independent experiments. Scale bars, 10 μm (A) and 500 nm (B to D).
To further confirm the vacuolar escape phenotypes of the parent and mutant strains, infected RAW 264.7 cell monolayers were also prepared for analysis by TEM. Results demonstrated that both SR1A and BM0739 were capable of disrupting vacuolar membranes, providing entry into the cytosol of the host cells (Fig. 5B and C). Consistent with results from the LAMP-1 colocalization studies, BM1533 was unable to undergo vacuolar escape and remained trapped within membrane-bound vacuoles (Fig. 5D). Collectively, these findings indicated that the growth defect associated with the tssE mutants was not due to vacuolar escape defects.
B. mallei T6SS-1 is expressed prior to escape from LAMP-1-associated vacuoles.
Previous studies indicate that the T6SSs expressed by a variety of different bacteria are upregulated following interactions with phagocytic cells (17, 22, 33, 34, 46). In the present study, results suggested that B. mallei T6SS-1 was expressed following uptake by RAW 264.7 cells but prior to escape of the organism from LAMP-1-positive vacuoles into the host cytosol. In order to confirm these observations, coverslips seeded with RAW 264.7 cells were infected with B. mallei BM0739Z, washed, fixed, and stained with anti-LAMP-1 antibodies. The reporter strain, BM0739Z (ΔbsaZ ΔtssE::gfp), was used for this purpose to take advantage of the fact that B. mallei ΔbsaZ mutants remain trapped within membrane-bound vacuoles (Fig. 5D). Consistent with previous assays, results demonstrated that GFP was expressed within 3 h postinfection and that, as expected, BM0739Z was incapable of escape from LAMP-1-associated vacuoles (Fig. 6). Taken together, these findings demonstrated that the signal required for T6SS-1 expression was provided prior to disruption of and escape from late phagosomes.
FIG. 6.
B. mallei T6SS-1 is expressed prior to escape from LAMP-1-associated vacuoles. Monolayers infected B. mallei BM0739Z were fixed at 3 h postinfection, immunostained, and visualized by fluorescence microscopy. Intracellular bacteria expressing GFP are shown in green, LAMP-1 stained with the 1D4B MAb is shown in red, and the nuclei stained with DRAQ5 are shown in blue. Micrographs are representative of at least three independent experiments. Scale bar, 10 μm.
B. mallei tssE mutants exhibit actin polymerization and intercellular spread defects in RAW 264.7 cells.
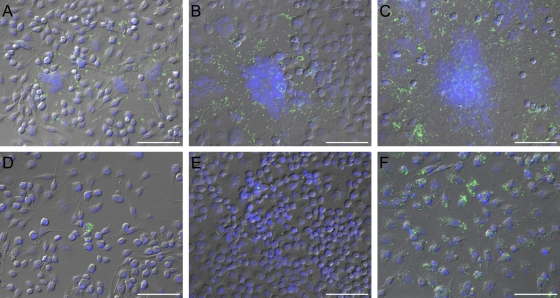
It has been previously shown that following vacuolar escape into the cytosol, B. mallei is able to polymerize host cell actin (11, 42, 51). By polymerizing actin tails at its pole, B. mallei appears to propel itself throughout the cytoplasm, facilitating both intra- and intercellular spread (11, 42, 51). In addition, studies in our lab suggest that that actin-based motility may play a role in B. mallei-induced MNGC formation (unpublished data). To determine if the inability of the B. mallei tssE mutants to stimulate MNGC formation was due to actin polymerization defects, coverslips seeded with RAW 264.7 cells were infected with strain SR1A (pBHR1-TG), BM0739G (pBHR1), or BM0739G (pA0739). At 24 h postinfection, monolayers were fixed, stained, and examined by fluorescence microscopy. Results of these studies demonstrated that RAW 264.7 monolayers infected with either SR1A (pBHR1-TG) or BM0739G (pA0739) exhibited obvious signs of intra- and intercellular motility as well as MNGC formation (Fig. 7A, B, and C). Consistent with the results shown in Fig. 4B and C, high numbers of bacteria were also observed in monolayers infected with these strains (Fig. 7A, B, and C). In contrast, monolayers infected with BM0739G (pBHR1) exhibited observable actin polymerization defects and no signs of MNGC formation (Fig. 7D). Consistent with Fig. 4E, low numbers of the mutant were also typically seen in infected monolayers (Fig. 7D). Such findings are supportive of the apparent growth defects observed throughout this study. In addition, macrophages containing high numbers of BM0739G (pBHR1) were also sporadically observed (Fig. 7E). Interestingly, even in such instances, actin-based motility appeared inefficient, cell-to-cell spread was lacking, and MNGC formation was absent (Fig. 7E). Even when monolayers were infected with a high dose of BM0739G (pBHR1-TG) (MOI of 200), no obvious signs of actin polymerization were observed (Fig. 7F). Collectively, these findings suggest that T6SS-1 plays an important role in facilitating actin-based motility, intercellular spread, and MNGC formation following infection of RAW 264.7 cells with B. mallei.
FIG. 7.
B. mallei tssE mutants demonstrate actin motility and intercellular spread defects in RAW 264.7 cells. Monolayers infected with B. mallei SR1A (pBHR1-TG) (A and B), BM0739G (pA0739G) (C) or BM0739G (pBHR1) (D, E, and F) were fixed at 24 h postinfection, stained, and examined by fluorescence microscopy. For panels A to E, monolayers were infected at an MOI of 20. For panel F, monolayers were infected at an MOI of 200. Bacteria expressing GFP are shown in green, host cell actin stained with Alexa Fluor 568-phalloidin is shown in red, and nuclei stained with DRAQ5 are shown in blue. White arrowheads in panel E indicate evidence of actin tail formation and potential intercellular spread. Micrographs are representative of at least three independent experiments. Scale bar, 10 μm.
DISCUSSION
B. mallei is a facultative intracellular pathogen that causes fatal disease in both humans and animals. The ability of this organism to survive and replicate within eukaryotic cells likely represents an important virulence strategy for persistence within susceptible hosts. Previous studies have demonstrated the presence of B. mallei within phagocytic cells and MNGCs in animal models of glanders (20, 23, 31). Consistent with these observations, several recent studies have shown that B. mallei can survive and replicate in a variety of murine macrophage cell lines (11, 42, 62). In the present study, we characterized the interactions of B. mallei tssE mutants with RAW 264.7 murine macrophages and provided evidence that T6SS-1 is required for optimal growth and actin-based motility within this cell line.
Several studies suggest that the expression of T6SSs by Gram-negative bacteria requires intimate contact with or uptake by eukaryotic cells (17, 22, 33, 34, 46). In most instances, the regulation of T6SSs appears to be dependent on regulatory mechanisms that involve two-component systems and activators of the AraC or sigma 54 families (1, 17, 19, 33, 39, 45). Such complex gene regulation likely ensures that T6SSs are expressed only at appropriate times during the infection process (14). Activation of B. mallei T6SS-1 has been shown to involve both the virulence-associated VirAG two-component regulatory system and the AraC type regulator BMAA1517 (45). In the present study, we demonstrated that overexpression of VirAG by B. mallei BM0739G (pBHR2-virAG) resulted in the production of GFP by the mutant reporter strain. Importantly, it was also shown that GFP was expressed by B. mallei BM0739G (pBHR1) only after internalization by RAW 264.7 cells. These findings are consistent with previous studies by Shalom et al. demonstrating that the expression of a homologous T6SS by B. pseudomallei is similarly induced following uptake by RAW 264.7 cells (46). On the basis of these observations, it is evident that T6SS-1 is expressed early during the infection process, thus implicating a critical role for this system following uptake of B. mallei by phagocytic cells.
Signal transduction pathways are important mechanisms used by bacteria to sense, respond to, and adapt to environmental changes. Common signals sensed by components of these pathways include changes in temperature, pH, osmolarity, cation concentration, and oxygen tension (4). Specific examples of virulence-associated two-component systems include the Salmonella enterica PhoPQ system that responds to changes in Mg2+ and Ca2+ concentrations as well as the Bordetella pertussis BvgAS system that responds to changes in temperature (4, 5, 27, 59). To date, the specific environmental cue that triggers the expression of the B. mallei VirAG two-component system remains to be defined. Two important observations from the present study suggest that the signal required for activation of T6SS-1 is provided within the phagosomal environment of RAW 264.7 cells. First, there was no evidence of T6SS-1 expression by extracellular B. mallei following infection of the monolayers. Second, expression of GFP by B. mallei tssE::gfp reporter strains was observed in association with LAMP-1-positive vacuoles, suggesting that T6SS-1 was expressed within endocytic vacuoles prior to escape. In addition, experiments employing a B. mallei T3SSAP/T6SS-1 double mutant confirmed that T6SS-1 was expressed by bacteria confined within membrane-bound vacuoles. These observations are consistent with recent reports demonstrating that expression of Francisella tularensis T6SS genes is induced within the Francisella-containing phagosome and does not require bacterial entry into the host cell cytosol (2, 15). Although further studies will be required to identify the specific signal sensed by VirAG that stimulates T6SS-1 expression, our findings indicate that it appears to be provided subsequent to uptake but prior to phagosomal escape of B. mallei into the host cytoplasm.
Most of the virulence-associated T6SSs described to date have been shown to influence the intracellular behavior of bacteria with phagocytic cells. For example, T6SS mutants of Aeromonas hydrophilia and Burkholderia cenocepacia are less cytotoxic to macrophages than wild-type strains (1, 53). Similarly, Edwardsiella tarda and F. tularensis T6SS mutants exhibit intracellular growth defects in fish phagocytes and murine macrophages, respectively (2, 15, 17, 40). Likewise, in this study, we demonstrated that although B. mallei tssE mutants are able to survive within RAW 264.7 cells, significant growth defects were observed in comparison to the parent strain. Subcellular localization experiments revealed that while B. mallei T3SSAP mutants remained trapped within membrane-bound vacuoles, B. mallei tssE mutants were capable of undergoing escape. These observations are consistent with a previous report demonstrating that a functional T3SSAP is required for vacuolar escape and survival in J774.2 cells and indicate that the apparent growth defect associated with B. mallei tssE mutants was not due to confinement within the phagosomal environment (42). This finding is unique in comparison to F. tularensis, in which T6SS mutations have been shown to prevent or delay bacterial escape from phagosomes (2, 15, 44). Interestingly, our data also appear to differ from previous studies by Shalom et al. demonstrating that B. pseudomallei T6SS mutants replicate to wild-type levels within RAW 264.7 cells (46). Although B. mallei T6SS-1 does not appear to be required for vacuolar escape, it does appear to play an important role following entry into the host cell cytosol. Further studies will be required, however, to determine a specific role for this system with regard to intracellular growth.
Similar to other intracellular pathogens, B. mallei is able to polymerize host cell actin and promote actin-based motility following entry into the cytoplasm. It has been proposed that by doing so, the organism can evade host immune responses by spreading cell to cell undetected. Previous studies have demonstrated that the motility phenotypes exhibited by B. mallei and B. pseudomallei are due in part to the expression of several bim-associated loci (45, 51). In contrast to other microbial species, the specific mechanism used by these organisms to facilitate actin polymerization appears unique (9). Recently, studies by Stevens et al. have shown that B. pseudomallei BimA is an autotransported protein that localizes to the bacterial pole and is required for actin tail formation (51, 52). In addition, B. mallei BimA has been shown to be required for actin-based motility in J774.2 murine macrophages (45). In the current study we demonstrated that, following uptake by RAW 264.7 cells, B. mallei tssE mutants exhibited significant intra- and intercellular spread defects in comparison to control strains. Importantly, these defects could be restored by complementation. To our knowledge, this is the first report of an apparent link between a T6SS and bacterially induced actin-based motility. At present, the molecular basis for these mutant phenotypes is unclear. It is interesting to speculate, however, that T6SS-1 might be required for optimal activity of bim gene products or that it functions to establish a favorable host environment in which B. mallei can efficiently polymerize actin.
B. mallei and B. pseudomallei are known to cause MNGC formation both in vitro and in vivo (7, 11, 20, 24, 28, 49). At present, the relevance of MNGCs with respect to virulence is unclear; however, it has been proposed that giant cells may provide these pathogens with an immune-privileged niche in which to survive and replicate within a host (7). The formation MNGCs from mononuclear cells is thought to be a result of cell fusion events; however, very little is known about the bacterial and host cell factors that are involved in this process (7, 24, 28). To date, both BipB and RpoS have been implicated in B. pseudomallei-induced MNGC formation in murine macrophage cell lines (54, 58). One of the most striking observations from this study was the inability of B. mallei tssE mutants to induce MNGCs following infection of RAW 264.7 cell monolayers. Several previous studies have suggested that MNGC formation may require both actin-based motility and intercellular spread (9, 24, 28, 51). Consistent with this hypothesis, our results demonstrate that the inability of B. mallei tssE mutants to induce MNGCs correlates with the actin polymerization and spread defects exhibited by these strains. The exact role of actin-based motility with regard to MNGC formation, however, remains to be experimentally defined.
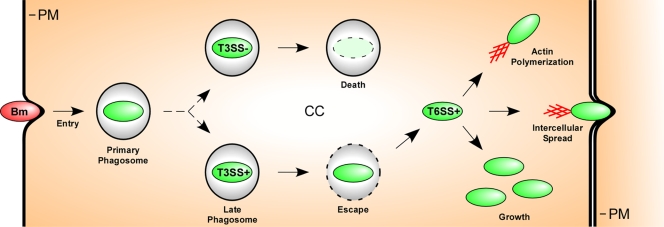
Based on our results as well as those from other groups, we propose a model describing the interactions of B. mallei with RAW 264.7 cells (Fig. 8). In this model, we suggest that a critical relationship exists between the coordinate expression of T3SSAP and T6SS-1. In addition, we indicate that following vacuolar escape, B. mallei T6SS-1 plays an influential role in intracellular growth, actin polymerization, cell-to-cell spread, and MNGC formation during infection. At present, the molecular mechanisms underlying the mutant phenotypes described in this study remain unclear. Studies are ongoing to more fully characterize the function of this important virulence factor in the pathogenesis of disease caused by B. mallei.
FIG. 8.
Proposed model of B. mallei (Bm) interactions with RAW 264.7 cells. Following uptake into primary phagosomes, the intracellular signal sensed by the VirAG two-component regulatory system stimulates expression of T6SS-1. During the process of phagosomal maturation, T3SSAP facilitates escape of B. mallei into the cytoplasm by promoting the disruption of vacuolar membranes. At this point, mutants incapable of undergoing vacuolar escape are rapidly killed by the macrophages. Once free in the host cytosol, T6SS-1 then appears to influence the ability of B. mallei to efficiently grow, spread both intra- and intercellularly via actin-based motility, and induce MNGC formation. PM, plasma membrane; CC, cell cytosol.
Acknowledgments
We thank David Wood and Joseph Brewer for critical review of the manuscript.
This research was supported in part by the Intramural Research Program of the NIH, National Institute of Allergy and Infectious Diseases.
The opinions, interpretations, conclusions, and recommendations are those of the authors and are not necessarily endorsed by the U.S. Army in accordance with AR 70-31.
Editor: J. B. Bliska
Footnotes
Published ahead of print on 2 November 2009.
REFERENCES
- 1.Aubert, D. F., R. S. Flannagan, and M. A. Valvano. 2008. A novel sensor kinase-response regulator hybrid controls biofilm formation and type VI secretion system activity in Burkholderia cenocepacia. Infect. Immun. 76:1979-1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barker, J. R., and K. E. Klose. 2007. Molecular and genetic basis of pathogenesis in Francisella tularensis. Ann. N. Y. Acad. Sci. 1105:138-159. [DOI] [PubMed] [Google Scholar]
- 3.Bartlett, J. G. 1998. Glanders, p. 1578-1580. In S. L. Gorbach, J. G. Bartlett, and N. R. Blacklow (ed.), Infectious diseases, 2nd ed. W. B. Saunders Co., Philadelphia, PA.
- 4.Beier, D., and R. Gross. 2006. Regulation of bacterial virulence by two-component systems. Curr. Opin. Microbiol. 9:143-152. [DOI] [PubMed] [Google Scholar]
- 5.Bijlsma, J. J., and E. A. Groisman. 2005. The PhoP/PhoQ system controls the intramacrophage type three secretion system of Salmonella enterica. Mol. Microbiol. 57:85-96. [DOI] [PubMed] [Google Scholar]
- 6.Bingle, L. E., C. M. Bailey, and M. J. Pallen. 2008. Type VI secretion: a beginner's guide. Curr. Opin. Microbiol. 11:3-8. [DOI] [PubMed] [Google Scholar]
- 7.Boddey, J. A., C. J. Day, C. P. Flegg, R. L. Ulrich, S. R. Stephens, I. R. Beacham, N. A. Morrison, and I. R. Peak. 2007. The bacterial gene lfpA influences the potent induction of calcitonin receptor and osteoclast-related genes in Burkholderia pseudomallei-induced TRAP-positive multinucleated giant cells. Cell Microbiol. 9:514-531. [DOI] [PubMed] [Google Scholar]
- 8.Bonemann, G., A. Pietrosiuk, A. Diemand, H. Zentgraf, and A. Mogk. 2009. Remodelling of VipA/VipB tubules by ClpV-mediated threading is crucial for type VI protein secretion. EMBO J. 28:315-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Breitbach, K., K. Rottner, S. Klocke, M. Rohde, A. Jenzora, J. Wehland, and I. Steinmetz. 2003. Actin-based motility of Burkholderia pseudomallei involves the Arp 2/3 complex, but not N-WASP and Ena/VASP proteins. Cell Microbiol. 5:385-393. [DOI] [PubMed] [Google Scholar]
- 10.Brett, P. J., M. N. Burtnick, D. S. Snyder, J. G. Shannon, P. Azadi, and F. C. Gherardini. 2007. Burkholderia mallei expresses a unique lipopolysaccharide mixture that is a potent activator of human Toll-like receptor 4 complexes. Mol. Microbiol. 63:379-390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brett, P. J., M. N. Burtnick, H. Su, V. Nair, and F. C. Gherardini. 2008. iNOS activity is critical for the clearance of Burkholderia mallei from infected RAW 264.7 murine macrophages. Cell Microbiol. 10:487-498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burtnick, M. N., P. J. Brett, V. Nair, J. M. Warawa, D. E. Woods, and F. C. Gherardini. 2008. Burkholderia pseudomallei type III secretion system mutants exhibit delayed vacuolar escape phenotypes in RAW 264.7 murine macrophages. Infect. Immun. 76:2991-3000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burtnick, M. N., P. J. Brett, and D. E. Woods. 2002. Molecular and physical characterization of Burkholderia mallei O antigens. J. Bacteriol. 184:849-852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cascales, E. 2008. The type VI secretion toolkit. EMBO Rep. 9:735-741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chong, A., T. D. Wehrly, V. Nair, E. R. Fischer, J. R. Barker, K. E. Klose, and J. Celli. 2008. The early phagosomal stage of Francisella tularensis determines optimal phagosomal escape and Francisella pathogenicity island protein expression. Infect. Immun. 76:5488-5499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dance, D. A. B. 1996. Melioidosis and glanders, p. 590-595. In D. J. Weatherall, J. G. G. Ledingham, and D. A.Warrell (ed.), Oxford textbook of medicine, 3rd ed. Oxford University Press, Oxford, United Kingdom.
- 17.de Bruin, O. M., J. S. Ludu, and F. E. Nano. 2007. The Francisella pathogenicity island protein IglA localizes to the bacterial cytoplasm and is needed for intracellular growth. BMC Microbiol. 7:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DeShazer, D., D. M. Waag, D. L. Fritz, and D. E. Woods. 2001. Identification of a Burkholderia mallei polysaccharide gene cluster by subtractive hybridization and demonstration that the encoded capsule is an essential virulence determinant. Microb. Pathog. 30:253-269. [DOI] [PubMed] [Google Scholar]
- 19.Dudley, E. G., N. R. Thomson, J. Parkhill, N. P. Morin, and J. P. Nataro. 2006. Proteomic and microarray characterization of the AggR regulon identifies a pheU pathogenicity island in enteroaggregative Escherichia coli. Mol. Microbiol. 61:1267-1282. [DOI] [PubMed] [Google Scholar]
- 20.Duval, C. W., and P. G. White. 1907. The histological lesions of experimental glanders. J. Exp. Med. 9:352-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Filloux, A., A. Hachani, and S. Bleves. 2008. The bacterial type VI secretion machine: yet another player for protein transport across membranes. Microbiology 154:1570-1583. [DOI] [PubMed] [Google Scholar]
- 22.Folkesson, A., S. Lofdahl, and S. Normark. 2002. The Salmonella enterica subspecies I specific centisome 7 genomic island encodes novel protein families present in bacteria living in close contact with eukaryotic cells. Res. Microbiol. 153:537-545. [DOI] [PubMed] [Google Scholar]
- 23.Fritz, D. L., P. Vogel, D. R. Brown, and D. M. Waag. 1999. The hamster model of intraperitoneal Burkholderia mallei (glanders). Vet. Pathol. 36:276-291. [DOI] [PubMed] [Google Scholar]
- 24.Harley, V. S., D. A. Dance, B. S. Drasar, and G. Tovey. 1998. Effects of Burkholderia pseudomallei and other Burkholderia species on eukaryotic cells in tissue culture. Microbios 96:71-93. [PubMed] [Google Scholar]
- 25.Hoang, T. T., R. R. Karkhoff-Schweizer, A. J. Kutchma, and H. P. Schweizer. 1998. A broad-host-range Flp-FRT recombination system for site-specific excision of chromosomally located DNA sequences: application for isolation of unmarked Pseudomonas aeruginosa mutants. Gene 212:77-86. [DOI] [PubMed] [Google Scholar]
- 26.Howe, C., and W. R. Miller. 1947. Human glanders: report of six cases. Ann. Intern. Med. 26:93-115. [DOI] [PubMed] [Google Scholar]
- 27.Kato, A., and E. A. Groisman. 2004. Connecting two-component regulatory systems by a protein that protects a response regulator from dephosphorylation by its cognate sensor. Genes Dev. 18:2302-2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kespichayawattana, W., S. Rattanachetkul, T. Wanun, P. Utaisincharoen, and S. Sirisinha. 2000. Burkholderia pseudomallei induces cell fusion and actin-associated membrane protrusion: a possible mechanism for cell-to-cell spreading. Infect. Immun. 68:5377-5384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Knodler, L. A., B. A. Vallance, M. Hensel, D. Jackel, B. B. Finlay, and O. Steele-Mortimer. 2003. Salmonella type III effectors PipB and PipB2 are targeted to detergent-resistant microdomains on internal host cell membranes. Mol. Microbiol. 49:685-704. [DOI] [PubMed] [Google Scholar]
- 30.Leiman, P. G., M. Basler, U. A. Ramagopal, J. B. Bonanno, J. M. Sauder, S. Pukatzki, S. K. Burley, S. C. Almo, and J. J. Mekalanos. 2009. Type VI secretion apparatus and phage tail-associated protein complexes share a common evolutionary origin. Proc. Natl. Acad. Sci. U. S. A. 106:4154-4159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lever, M. S., M. Nelson, P. I. Ireland, A. J. Stagg, R. J. Beedham, G. A. Hall, G. Knight, and R. W. Titball. 2003. Experimental aerogenic Burkholderia mallei (glanders) infection in the BALB/c mouse. J. Med. Microbiol. 52:1109-1115. [DOI] [PubMed] [Google Scholar]
- 32.Lopez, J., J. Copps, C. Wilhelmsen, R. Moore, J. Kubay, M. St-Jacques, S. Halayko, C. Kranendonk, S. Toback, D. DeShazer, D. L. Fritz, M. Tom, and D. E. Woods. 2003. Characterization of experimental equine glanders. Microbes Infect. 5:1125-1131. [DOI] [PubMed] [Google Scholar]
- 33.Mougous, J. D., M. E. Cuff, S. Raunser, A. Shen, M. Zhou, C. A. Gifford, A. L. Goodman, G. Joachimiak, C. L. Ordonez, S. Lory, T. Walz, A. Joachimiak, and J. J. Mekalanos. 2006. A virulence locus of Pseudomonas aeruginosa encodes a protein secretion apparatus. Science 312:1526-1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nano, F. E., and C. Schmerk. 2007. The Francisella pathogenicity island. Ann. N. Y. Acad. Sci. 1105:122-137. [DOI] [PubMed] [Google Scholar]
- 35.Neubauer, H., L. D. Sprague, R. Zacharia, H. Tomaso, S. Al Dahouk, R. Wernery, U. Wernery, and H. C. Scholz. 2005. Serodiagnosis of Burkholderia mallei infections in horses: state-of-the-art and perspectives. J. Vet. Med. B Infect. Dis. Vet. Public Health 52:201-205. [DOI] [PubMed] [Google Scholar]
- 36.Nierman, W. C., D. DeShazer, H. S. Kim, H. Tettelin, K. E. Nelson, T. Feldblyum, R. L. Ulrich, C. M. Ronning, L. M. Brinkac, S. C. Daugherty, T. D. Davidsen, R. T. Deboy, G. Dimitrov, R. J. Dodson, A. S. Durkin, M. L. Gwinn, D. H. Haft, H. Khouri, J. F. Kolonay, R. Madupu, Y. Mohammoud, W. C. Nelson, D. Radune, C. M. Romero, S. Sarria, J. Selengut, C. Shamblin, S. A. Sullivan, O. White, Y. Yu, N. Zafar, L. Zhou, and C. M. Fraser. 2004. Structural flexibility in the Burkholderia mallei genome. Proc. Natl. Acad. Sci. U. S. A. 101:14246-14251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pell, L. G., V. Kanelis, L. W. Donaldson, P. L. Howell, and A. R. Davidson. 2009. The phage lambda major tail protein structure reveals a common evolution for long-tailed phages and the type VI bacterial secretion system. Proc. Natl. Acad. Sci. U. S. A. 106:4160-4165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pukatzki, S., A. T. Ma, A. T. Revel, D. Sturtevant, and J. J. Mekalanos. 2007. Type VI secretion system translocates a phage tail spike-like protein into target cells where it cross-links actin. Proc. Natl. Acad. Sci. U. S. A. 104:15508-15513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pukatzki, S., A. T. Ma, D. Sturtevant, B. Krastins, D. Sarracino, W. C. Nelson, J. F. Heidelberg, and J. J. Mekalanos. 2006. Identification of a conserved bacterial protein secretion system in Vibrio cholerae using the Dictyostelium host model system. Proc. Natl. Acad. Sci. U. S. A. 103:1528-1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rao, P. S., Y. Yamada, Y. P. Tan, and K. Y. Leung. 2004. Use of proteomics to identify novel virulence determinants that are required for Edwardsiella tarda pathogenesis. Mol. Microbiol. 53:573-586. [DOI] [PubMed] [Google Scholar]
- 41.Redfearn, M. S., N. J. Palleroni, and R. Y. Stanier. 1966. A comparative study of Pseudomonas pseudomallei and Bacillus mallei. J. Gen. Microbiol. 43:293-313. [DOI] [PubMed] [Google Scholar]
- 42.Ribot, W. J., and R. L. Ulrich. 2006. The animal pathogen-like type III secretion system is required for the intracellular survival of Burkholderia mallei within J774.2 macrophages. Infect. Immun. 74:4349-4353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rotz, L. D., A. S. Khan, S. R. Lillibridge, S. M. Ostroff, and J. M. Hughes. 2002. Public health assessment of potential biological terrorism agents. Emerg. Infect. Dis. 8:225-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Santic, M., M. Molmeret, J. R. Barker, K. E. Klose, A. Dekanic, M. Doric, and Y. Abu Kwaik. 2007. A Francisella tularensis pathogenicity island protein essential for bacterial proliferation within the host cell cytosol. Cell Microbiol. 9:2391-2403. [DOI] [PubMed] [Google Scholar]
- 45.Schell, M. A., R. L. Ulrich, W. J. Ribot, E. E. Brueggemann, H. B. Hines, D. Chen, L. Lipscomb, H. S. Kim, J. Mrazek, W. C. Nierman, and D. Deshazer. 2007. Type VI secretion is a major virulence determinant in Burkholderia mallei. Mol. Microbiol. 64:1466-1485. [DOI] [PubMed] [Google Scholar]
- 46.Shalom, G., J. G. Shaw, and M. S. Thomas. 2007. In vivo expression technology identifies a type VI secretion system locus in Burkholderia pseudomallei that is induced upon invasion of macrophages. Microbiology 153:2689-2699. [DOI] [PubMed] [Google Scholar]
- 47.Shanks, J., M. N. Burtnick, P. J. Brett, D. M. Waag, K. Spurgers, W. J. Ribot, M. A. Schell, R. G. Panchal, F. C. Gherardini, K. D. Wilkinson, and D. DeShazer. 2009. Burkholderia mallei tssM encodes a secreted deubiquitinase that is expressed inside infected RAW 264.7 cells. Infect. Immun. 77:1636-1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Simon, R., U. Priefer, and A. Puhler. 1983. A broad host range mobilization system for in vivo genetic engineering: transposon mutagenesis in Gram negative bacteria. Biotechnology (NY) 1:784-791. [Google Scholar]
- 49.Sirikulchayanonta, V., and T. Subhadrabandhu. 1994. Melioidosis. Another etiology of granulomatous osteomyelitis. Report of 2 cases. Clin. Orthop. Relat. Res. Nov:183-186. [PubMed] [Google Scholar]
- 50.Srinivasan, A., C. N. Kraus, D. DeShazer, P. M. Becker, J. D. Dick, L. Spacek, J. G. Bartlett, W. R. Byrne, and D. L. Thomas. 2001. Glanders in a military research microbiologist. N. Engl. J. Med. 345:256-258. [DOI] [PubMed] [Google Scholar]
- 51.Stevens, J. M., R. L. Ulrich, L. A. Taylor, M. W. Wood, D. Deshazer, M. P. Stevens, and E. E. Galyov. 2005. Actin-binding proteins from Burkholderia mallei and Burkholderia thailandensis can functionally compensate for the actin-based motility defect of a Burkholderia pseudomallei bimA mutant. J. Bacteriol. 187:7857-7862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stevens, M. P., J. M. Stevens, R. L. Jeng, L. A. Taylor, M. W. Wood, P. Hawes, P. Monaghan, M. D. Welch, and E. E. Galyov. 2005. Identification of a bacterial factor required for actin-based motility of Burkholderia pseudomallei. Mol. Microbiol. 56:40-53. [DOI] [PubMed] [Google Scholar]
- 53.Suarez, G., J. C. Sierra, J. Sha, S. Wang, T. E. Erova, A. A. Fadl, S. M. Foltz, A. J. Horneman, and A. K. Chopra. 2008. Molecular characterization of a functional type VI secretion system from a clinical isolate of Aeromonas hydrophila. Microb. Pathog. 44:344-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Suparak, S., W. Kespichayawattana, A. Haque, A. Easton, S. Damnin, G. Lertmemongkolchai, G. J. Bancroft, and S. Korbsrisate. 2005. Multinucleated giant cell formation and apoptosis in infected host cells is mediated by Burkholderia pseudomallei type III secretion protein BipB. J. Bacteriol. 187:6556-6560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ulrich, R. L., K. Amemiya, D. M. Waag, C. J. Roy, and D. DeShazer. 2005. Aerogenic vaccination with a Burkholderia mallei auxotroph protects against aerosol-initiated glanders in mice. Vaccine 23:1986-1992. [DOI] [PubMed] [Google Scholar]
- 56.Ulrich, R. L., and D. DeShazer. 2004. Type III secretion: a virulence factor delivery system essential for the pathogenicity of Burkholderia mallei. Infect. Immun. 72:1150-1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ulrich, R. L., D. Deshazer, H. B. Hines, and J. A. Jeddeloh. 2004. Quorum sensing: a transcriptional regulatory system involved in the pathogenicity of Burkholderia mallei. Infect. Immun. 72:6589-6596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Utaisincharoen, P., S. Arjcharoen, K. Limposuwan, S. Tungpradabkul, and S. Sirisinha. 2006. Burkholderia pseudomallei RpoS regulates multinucleated giant cell formation and inducible nitric oxide synthase expression in mouse macrophage cell line (RAW 264.7). Microb. Pathog. 40:184-189. [DOI] [PubMed] [Google Scholar]
- 59.Veal-Carr, W. L., and S. Stibitz. 2005. Demonstration of differential virulence gene promoter activation in vivo in Bordetella pertussis using RIVET. Mol. Microbiol. 55:788-798. [DOI] [PubMed] [Google Scholar]
- 60.Voskuhl, G. W., P. Cornea, M. S. Bronze, and R. A. Greenfield. 2003. Other bacterial diseases as a potential consequence of bioterrorism: Q. fever, brucellosis, glanders, and melioidosis. J. Okla. State Med. Assoc. 96:214-217. [PubMed] [Google Scholar]
- 61.Warawa, J., and D. E. Woods. 2005. Type III secretion system cluster 3 is required for maximal virulence of Burkholderia pseudomallei in a hamster infection model. FEMS Microbiol. Lett. 242:101-108. [DOI] [PubMed] [Google Scholar]
- 62.Whitlock, G. C., G. A. Valbuena, V. L. Popov, B. M. Judy, D. M. Estes, and A. G. Torres. 2009. Burkholderia mallei cellular interactions in a respiratory cell model. J. Med. Microbiol. 58:554-562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wilkinson, L. 1981. Glanders: medicine and veterinary medicine in common pursuit of a contagious disease. Med. Hist. 25:363-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yabuuchi, E., Y. Kosako, H. Oyaizu, I. Yano, H. Hotta, Y. Hashimoto, T. Ezaki, and M. Arakawa. 1992. Proposal of Burkholderia gen. nov. and transfer of seven species of the genus Pseudomonas homology group II to the new genus, with the type species Burkholderia cepacia (Palleroni and Holmes 1981) comb. nov. Microbiol. Immunol. 36:1251-1275. [DOI] [PubMed] [Google Scholar]
- 65.Yahr, T. L. 2006. A critical new pathway for toxin secretion? N. Engl. J. Med. 355:1171-1172. [DOI] [PubMed] [Google Scholar]
- 66.Zheng, J., and K. Y. Leung. 2007. Dissection of a type VI secretion system in Edwardsiella tarda. Mol. Microbiol. 66:1192-1206. [DOI] [PubMed] [Google Scholar]