Abstract
A crucial step in the arenavirus life cycle is the biosynthesis of the viral envelope glycoprotein (GP) responsible for virus attachment and entry. Processing of the GP precursor (GPC) by the cellular proprotein convertase site 1 protease (S1P), also known as subtilisin-kexin-isozyme 1 (SKI-1), is crucial for cell-to-cell propagation of infection and production of infectious virus. Here, we sought to evaluate arenavirus GPC processing by S1P as a target for antiviral therapy using a recently developed peptide-based S1P inhibitor, decanoyl (dec)-RRLL-chloromethylketone (CMK), and the prototypic arenavirus lymphocytic choriomeningitis virus (LCMV). To control for off-target effects of dec-RRLL-CMK, we employed arenavirus reverse genetics to introduce a furin recognition site into the GPC of LCMV. The rescued mutant virus grew to normal titers, and the processing of its GPC critically depended on cellular furin, but not S1P. Treatment with the S1P inhibitor dec-RRLL-CMK resulted in specific blocking of viral spread and virus production of LCMV. Combination of the protease inhibitor with ribavirin, currently used clinically for treatment of human arenavirus infections, resulted in additive drug effects. In cells deficient in S1P, the furin-dependent LCMV variant established persistent infection, whereas wild-type LCMV underwent extinction without the emergence of S1P-independent escape variants. Together, the potent antiviral activity of an inhibitor of S1P-dependent GPC cleavage, the additive antiviral effect with ribavirin, and the low probability of emergence of S1P-independent viral escape variants make S1P-mediated GPC processing by peptide-derived inhibitors a promising strategy for the development of novel antiarenaviral drugs.
Arenaviruses merit significant attention as tractable experimental model systems and clinically important human pathogens (6). The Old World arenavirus Lassa virus (LASV) causes a severe hemorrhagic fever with high mortality in humans and infects several hundred thousand individuals yearly in its West African region of endemicity (12, 23). On the South American continent, the New World arenaviruses Junin (JUNV), Machupo, Guanarito, and Sabia viruses have emerged as causative agents of severe hemorrhagic fevers in Argentina, Bolivia, Venezuela, and Brazil, respectively (31). Moreover, compelling evidence indicates that the globally distributed prototypic arenavirus lymphocytic choriomeningitis virus (LCMV) is a neglected human pathogen of clinical significance, especially in cases of congenital infection leading to hydrocephalus, mental retardation, and chorioretinitis in infants (1, 26). In addition, LCMV poses a special threat to immunocompromised individuals, as tragically illustrated by recent cases of transplant-associated infections by LCMV with fatal outcomes (11, 28). These public health concerns are aggravated by the lack of licensed vaccines or effective treatment for these important human pathogens.
A hallmark of fatal arenavirus infection is rapid multiplication of the virus that overwhelms the patient's immune system, resulting in uncontrolled infection. Accordingly, the virus load in the patient's blood is a highly predictive factor for disease outcome. Those who survive develop a vigorous antiviral immune response, control the infection, and ultimately clear the virus (23, 31). These findings suggest that antiviral drugs aimed at reducing arenavirus multiplication and spread may provide the infected individual with a window of opportunity to develop an effective antiviral defense response to prevent or minimize arenavirus-associated disease.
A crucial step in the life cycle of arenaviruses is the biosynthesis of the mature envelope glycoprotein (GP) responsible for receptor attachment and cell entry (6). Initially synthesized as a single polypeptide, arenavirus GP precursor (GPC) undergoes proteolytic processing by the cellular proprotein convertase site 1 protease (S1P), also known as subtilisin-kexin-isozyme 1 (SKI-1), yielding the peripheral virion attachment protein GP1 and the fusion-active transmembrane protein GP2 (2, 17, 21, 37).
S1P is involved in the proteolytic processing of a defined set of cellular proteins, including the brain-derived neurotrophic factor precursor protein (49); the sterol regulatory element-binding proteins (SREBP-1 and SREBP-2), membrane-associated transcription factors that regulate genes involved in lipid metabolism (5, 43); and the activating transcription factor 6 (ATF6), involved in the regulation of the cellular response to endoplasmic reticulum (ER) stress (48, 53). The key role of S1P in the regulation of lipid metabolism has raised considerable interest in developing inhibitors of S1P activity. Efforts to design specific inhibitors of S1P resulted in the identification of recombinant serpins able to specifically block S1P activity (34). While of great value for proof of principle, protein-based S1P inhibitors are not cell permeable, making their use as antiviral drugs for treatment of human arenavirus infection difficult. In the present study, we evaluated a recently developed cell-permeable, peptide-based S1P inhibitor combining a chloromethylketone (CMK) moiety with peptides derived from the RRLL recognition motif of S1P, decanoyl (dec)-RRLL-CMK (30), in the context of productive arenavirus infection using the prototypic arenavirus LCMV.
MATERIALS AND METHODS
Viruses and cell lines.
Stocks of LCMV were prepared in Syrian golden hamster kidney (BHK21) cells, and titers were determined as reported previously (9). The production and titer determination of retroviral pseudotypes were done as described previously (39, 40). African green monkey kidney (VeroE6) cells were maintained in minimal essential medium (Gibco BRL, NY) containing 7% fetal bovine serum and supplemented with glutamine and penicillin/streptomycin. Human embryonic kidney (HEK293) cells, human lung epithelial (A549) cells, and BHK21 cells were maintained in Dulbecco's modified Eagle's medium (Gibco BRL, NY) containing 10% fetal bovine serum and supplemented with nonessential amino acids, glutamine, and penicillin/streptomycin. Chinese hamster ovary (CHO)-K1 cells and FD11 CHO cells deficient in furin (13) were grown at 37°C and 5% CO2 in Dulbecco's modified Eagle's medium nutrient mixture F-12 Ham (GIBCO BRL) supplemented with 10% fetal calf serum, 100 units/ml penicillin, and 0.1 mg/ml streptomycin. The S1P-deficient CHOK1-derived cell line SRD12B (35) and other cell lines treated with dec-RRLL-CMK were maintained in complete medium supplemented with 5 μg/ml cholesterol (Sigma), 1 mM sodium mevalonate (Sigma), and 20 μM sodium oleate (Sigma).
Antibodies.
Monoclonal antibodies (MAbs) 113 (anti-LCMV nucleoprotein [NP]) and 83.6 (anti-LCMV GP) were described previously (7, 52). Other MAbs included anti-α-tubulin (Sigma, St. Louis, MO), anti-HA F7 (immunoglobulin G2a [IgG2a]; Santa Cruz Biotechnology, CA), anti-ER calnexin (IgG1; BD Biosciences), and anti-GM-130 (IgG1; BD Biosciences). Rabbit polyclonal anti-Flag antibody was from Sigma (St. Louis, MO). Rhodamine-X-conjugated anti-mouse and -rabbit IgG and fluorescein isothiocyanate (FITC)-conjugated anti-mouse, anti-rabbit, biotin anti-mouse IgG, and streptavidin-Cy5 were from Jackson Immuno-Research (West Grove, PA). Anti-mouse IgG1, anti-mouse IgG2a, and horseradish peroxidase-conjugated anti-rabbit IgG were obtained from Pierce. 4′-6-Diamidino-2-phenylindole (DAPI) was from Invitrogen.
Generation of recombinant LCMV containing mutant GPs.
The mutant LCMV GP-RRRR was generated by introducing the point mutations L264R and A265R by PCR amplification using the cDNA of LCMV ARM53b variant clone 13 as a template. A 5′ fragment was amplified with the primers FUR1 (5′-TGC TCT AGA CGA GTT ACC AAT ACC TGA TTA-3′) and FUR2 (5′-TTA GCG ACG TCT CCT AGT GAA GAA CTT AGT-3′) and a 3′ fragment was amplified using primers FUR3 (5′-CTC ATT AGG AGA CGT CGC GGC ACA TTC ACC TGG ACT TTG-3′) and FUR4 (5′-CAT TTC GCA ACT GCT GTG TTC-3′). PCR fragments were cut with XbaI/AatII and AatII/PstI, respectively, and subcloned into pBluescript. An NdeI-PstI fragment was retrieved and inserted into the expression vector pC-LCMVGP (17). The mutation A265L to yield the protease recognition sequence RRLL was introduced into LCMV GP by PCR amplification of a 5′ fragment with the primers FUR1 and 5′-ACT AGA CGT CTA CTC GGC ACA TTC ACC TGG ACT TTG-3′ and of a 3′ fragment using the primers 5′-TTT AAG ACG TCT AGT GAG GAA CTT AGT CTT CTC TTG GGA-3′ and FUR4. PCR fragments were cut with XbaI/AatII and AatII/PstI. After being subcloned into pBluescript, an NdeI-PstI fragment was retrieved and inserted into the expression vector pC-LCMVGP. The constructs were verified by double-stranded DNA sequencing.
For the construction of the antigenomic S (Sag) RNA segment containing GP-RRRR, Pol I-MGNP-Bsm(+)/LCMVGP-RRRR, an NdeI/KpnI fragment was excised from pC.LCMVGP-RRRR and inserted into the plasmid PolI S(+) (44) cut with NdeI/KpnI. The resulting construct, Pol I-MGNP-Bsm(+)/LCMVGP-RRRR, contained the complete cDNA of the antigenomic S (Sag) RNA segment of LCMV ARM53b, including the mutations L264R and A265R. The Sag sequence in this construct is flanked at its 5′ end by the promoter sequences of the mouse RNA polymerase I (Pol I) and at its 3′ end by the Pol I terminator sequences. For the rescue of recombinant wild-type (WT) rLCMV-RRLA, the previously used antigenomic S (Sag) RNA segment containing GP-WT (GP-RRLA) was used (44). Rescue of rLCMV-RRRR and rLCMV-RRLA was performed as described previously (44). Briefly, BHK21 cells (7.5 × 105 per well) were seeded in six-well plates and cotransfected with plasmids encoding the LCMV NP (pC-NP; 0.8 μg) and l-polymerase (pC-L; 1 μg) and either Pol I-MGNP/Bsm(+)/LCMVGP-RRRR or Pol I-MGNP/Bsm(+)/LCMVGP-WT (0.8 μg), together with Pol I L(+)v2 (1.4 μg), a plasmid that directs Pol I-mediated intracellular synthesis of the Lag RNA segment of LCMV ARM53b. Transfection was performed as described previously (44), and cell culture supernatants were collected after 48, 72, and 96 h. For the detection of infectious virus, serial dilutions of supernatants were added to monolayers of fresh VeroE6 cells, and infectious virus was detected by immunofluorescence (IF) analysis after 16 h as described previously (44). Infectious titers in culture supernatants were determined by plaque assay on VeroE6 cells. For the production of initial seed stocks, rLCMV from the 48-h supernatant was used to infect fresh monolayers of BHK21 cells (multiplicity of infection [MOI] = 0.1). The supernatants were harvested after 48 h, and the titers were determined by plaque assay on VeroE6 cells.
Cytotoxicity assay.
The cytotoxicities of dec-RRLL-CMK and dec-RVKR-CMK in different cell lines were assessed using the CellTiter-Glo Luminescent Cell Viability Assay (Promega), which determines the number of viable cells in a culture by quantification of ATP. For the assay, 104 cells were plated per well of a 96-well plate and cultured overnight, resulting in monolayers. The cells were treated with increasing concentrations of inhibitors. After 36 h, CellTiter-Glo reagent was added, the assay was performed according to the manufacturer's recommendations, and the concentrations causing 50% cytotoxicity (CC50) were calculated.
Virus infection of cells.
For infection of cells with viruses, seed stocks were diluted to the indicated MOI and added to cells for 1 h at 37°C. After 1 hour of incubation at the indicated temperature, the inoculum was removed and the cells were washed twice with medium without serum and incubated for the indicated times at 37°C and 5% CO2. Infected cells were determined based on NP expression detected by IF analysis using MAb 113 (anti-LCMV NP) combined with fluorescence-labeled secondary antibodies (8). Infection of cells with retroviral pseudotypes was performed as described previously (39) using the Steady Glo luciferase assay (Promega).
Pharmacological inhibitors.
The S1P inhibitor dec-RRLL-CMK was synthesized by Bachem (Switzerland), and the furin inhibitor dec-RVKR-CMK was purchased from Calbiochem. Stocks of the peptide inhibitors were prepared in ultrapure, water-free dimethyl sulfoxide and stored at −80°C. Ribavirin (1-β-d-ribofuranosyl-1,2,4-triazole-3-carboxamide) was purchased from Sigma. Unless otherwise indicated, inhibitors were added at the indicated time points and were present for the duration of the experiment.
Expression of recombinant proteins and immunoblotting.
HEK293 cells were transfected with SuperFect (Qiagen) (38), and CHOK1, FD11, and SRD12B cells were transfected using Lipofectamine (17). Transfection efficiencies as determined by IF detection of transgenes were >90% for HEK293 cells and >60% for CHOK1, FD11, and SRD12B cells. For Western blot analysis, cell lysates were prepared as described previously (17), and proteins were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis and transferred to nitrocellulose membranes. After being blocked in 5% (wt/vol) skim milk in phosphate-buffered saline (PBS), the membranes were incubated with 10 μg/ml primary antibody, and MAb 83.6 anti-LCMV-GP2 and MAb anti-α-tubulin were diluted in 2% (wt/vol) skim milk-PBS and incubated overnight at 6°C. After several washes in PBS-0.1% (wt/vol) Tween 20, secondary antibodies coupled to horseradish peroxidase were applied 1:5,000 in PBS-0.1% (wt/vol) Tween 20 for 1 h at room temperature. Blots were developed using Super Signal West Pico ECL Substrate (Pierce).
RNA analysis by RT-PCR.
The levels of LCMV NP mRNA in persistently infected cells were assessed by RT-PCR as described previously (18). Briefly, total RNA was isolated from the cells by using TRIreagent. Before the reverse transcription (RT), contaminant DNA was removed by using the DNA-free kit (Ambion, Austin, TX). The RT reaction was performed with 5 μg RNA using SuperScript II and random hexamer primers (both from Invitrogen). PCR was done by using Taq polymerase with the NP-specific primers and primers for the control housekeeping GAPDH (glyceraldehyde-3-phosphate dehydrogenase) described previously (18). PCR products were separated on agarose gels and visualized by staining them with ethidium bromide. Images were acquired using an Eagle-Eye digital camera.
Confocal microscopy and flow cytometry.
Confocal microscopy was performed as described previously (36). Briefly, 104 HEK293 cells transfected with Flag-tagged variants of LCMV GP and hemagglutinin (HA)-tagged S1P the day before were transferred to eight-well LabTek chamber slides (Nunc) precoated with poly-l-lysine. After 24 h, the cells were fixed with 4% (wt/vol) paraformaldehyde-PBS for 15 min at room temperature. Primary antibodies were applied at 10 μg/ml for 1 h at room temperature, followed by fluorochrome-conjugated secondary antibodies at a dilution of 1:100 for 45 min at room temperature in the dark. For confocal laser scanning microscopy, cells were analyzed using a Bio-Rad 1024 confocal laser microscope and a 63× oil immersion Plan Apo 1.4-numerical-aperture objective for high resolution. Fluorescein was excited at 488 nm, rhodamine at 568 nm, and Cy5 at 647 nm, all with a krypton-argon mixed-gas laser recording simultaneously in three separate channels. Images were analyzed using LSM Image Examiner (Zeiss) and Image J (http://rsb.info.nih.gov/ij) and then assembled using Adobe Photoshop.
Cell surface staining of recombinant LCMV GP and intracellular staining for LCMV NP were performed as described previously (17). Specimens were analyzed with a FACSCalibur flow cytometer (Becton Dickinson, San Jose, CA) using Cell Quest software.
RESULTS
Previous studies demonstrated specific inhibitory activity of dec-RRLL-CMK for S1P (30), making this peptide-derived, cell-permeable inhibitor an attractive candidate for the evaluation of antiarenaviral activity. However, the cytotoxicity of dec-RRLL-CMK reported for some cell lines, such as VeroE6 (30), likely due to inhibition of S1P's endogenous functions, was a major concern. To compensate for effects of the S1P inhibitor on lipid metabolism, the culture medium of cells was supplemented with a previously described lipid cocktail containing cholesterol that is used for the culture of S1P-deficient CHOK1 cells (35). To address toxicity based on other functions of S1P, we determined the dose-dependent reduction of cell viability in different mammalian cell lines using the CellTiter-Glo Luminescent Cell Viability Assay, which measures the viability of cells by quantification of cellular ATP. To assess if toxicity was due to the specific inhibition of S1P, we compared dec-RRLL-CMK to a well-described furin inhibitor, dec-RVKR-CMK, which has been used to block furin-mediated processing of viral GPs in human cells and showed only mild cytotoxicity up to a concentration of 100 μM (14). Briefly, VeroE6, A549, HeLa, HEK293, BHK21, and CHOK1 cells were treated with increasing concentrations of dec-RRLL-CMK or dec-RVKR-CMK for 36 h; cell viability was determined with the CellTiter-Glo assay; and the CC50 was calculated (Table 1). Compared to dec-RVKR-CMK, dec-RRLL-CMK showed overall higher toxicity (lower CC50) in all cell lines. Consistent with published data (30), dec-RRLL-CMK caused significantly higher toxicity in VeroE6 cells than in CHOK1 cells, which were therefore used for our subsequent studies. The consistently lower CC50 for dec-RRLL-CMK in all cell lines suggested that the different specificities of the inhibitors, as defined by their peptide sequences, are involved in the effect. To confirm the role of S1P in the cytotoxicity of dec-RRLL-CMK, we compared the viabilities of CHOK1 WT cells and CHOK1 cells deficient in S1P (SRD12B) (35). dec-RRLL-CMK showed similar cytotoxicities in S1P-deficient and WT cells, suggesting that an off-target effect unrelated to S1P may be responsible (Table 1). The absence of additional cytotoxicity due to the inhibition of S1P would be in line with the fact that S1P deficiency does not result in a cytopathic effect, provided the cells are grown in the presence of lipid and cholesterol supplement (35).
TABLE 1.
Cytotoxicities of dec-RRLL-CMK and dec-RVRK-CMV in different mammalian cell linesa
| Cell line | CC50 (μM) |
|
|---|---|---|
| dec-RRLL-CMK | dec-RVKR-CMK | |
| VeroE6 | 25.1 ± 3.2 | 84.7 ± 8.1 |
| A549 | 31.5 ± 4.1 | >100 |
| HEK293 | 38.5 ± 5.1 | >100 |
| HeLa | 43.1 ± 6.7 | >100 |
| BHK21 | 42.7 ± 5.0 | 92.5 ± 10.3 |
| CHOK1 | 78.5 ± 4.2 | >100 |
| SRD12B | 61.1 ± 7.1 | >100 |
Cells were treated with increasing concentrations of inhibitors. After 36 h, a CellTiter-Glo assay was performed, and the CC50 was calculated (means ± standard deviations; n = 3).
Generation of an LCMV mutant expressing GPC and containing a furin recognition site.
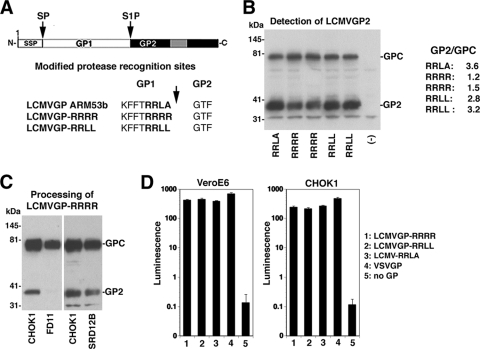
The evaluation of the antiarenaviral activity of dec-RRLL-CMK required a suitable viral control to exclude the S1P-unrelated off-target effects revealed by our cytotoxicity studies. For this purpose, we employed arenavirus reverse genetics to introduce a furin recognition site into the GPC of the prototypic arenavirus LCMV. The proprotein convertase furin has a preference for R-Xn-R (where n = 0, 2, 4, or 6, and X is a variable amino acid), whereas S1P shows a distinct recognition site, R-X-(hydrophobic)-X (49, 51). The S1P recognition site (RRLA) in the GPC of LCMV ARM53b was replaced by a canonical furin recognition site, RRRR (GP-RRRR) (Fig. 1A). In addition, we generated LCMV GP containing the S1P recognition site RRLL found in the proform of S1P (51) and the GP of LASV (21). Upon transient transfection into HEK293 cells, GP-WT (GP-RRLA), GP-RRLL, and GP-RRRR exhibited similar expression levels. Compared to GP-RRLA and GP-RRLL, processing of GP-RRRR occurred to a lesser extent (Fig. 1B). Despite this difference, all GP variants were efficiently transported to the cell surface as assessed by immunostaining with a MAb to a conserved epitope in LCMV GP2 and flow cytometry (data not shown). As expected, processing of recombinant GP-RRRR was markedly reduced in the furin-deficient CHO cell line FD11 but occurred normally in S1P-deficient SRD12B cells (Fig. 1C). To evaluate incorporation into virus particles and function in cell entry, mutant and WT GPs were inserted by pseudotyping into recombinant retroviruses containing a luciferase reporter gene (40). Infectious pseudotype titers were determined by infection of VeroE6 monolayers, followed by a luciferase assay. Similar pseudotype titers were obtained for WT and mutant GPs (Fig. 1D), indicating no adverse effect of the altered protease recognition sequence on the viral GP's function in host cell attachment and entry.
FIG. 1.
Recombinant LCMV GP containing a furin recognition site. (A) Schematic representation of LCMV GP with modified protease recognition sites. GP1 and GP2 are indicated, and the gray box corresponds to the transmembrane domain. SSP, stable signal peptide; arrows, sites of proteolytic processing by signal peptidase (SP) and S1P. (B) Expression of recombinant LCMV GPs. LCMV GP WT (RRLA), LCMV GP-RRRR (RRRR), and LCMV GP-RRLL (RRLL), as well as a GFP control (−), were detected in lysates of transfected HEK293 cells by Western blotting using an anti-LCMV GP2 antibody. The positions of the GPC and mature GP2 are indicated. The extent of cleavage of GP2/GPC was determined by densitometric analysis of the signals. (C) Detection of LCMV-RRRR in total lysates of transfected WT CHOK1 cells, furin-deficient FD11 cells, and S1P-deficient SRD12B cells by Western blotting using an anti-LCMV GP2 antibody. (D) Generation of recombinant retroviral vectors pseudotyped with recombinant LCMV GP. The packaging cell line GP2293 stably transfected with murine leukemia virus (MLV) gag and pol, was cotransfected with a plasmid containing the packable MLV genome, pLZRS-Luc-Gfp, carrying a luciferase and a GFP reporter, and an expression plasmid for recombinant LCMV GP variants, the GP of VSV, and empty vectors (no GP). Retroviral pseudotypes released into the cell supernatant were added to VeroE6 cells, and 48 h later, infection was assessed with the Steady Glo luciferase assay (means plus standard deviations; n = 3). Luminescence is given as the increase (n-fold) over background.
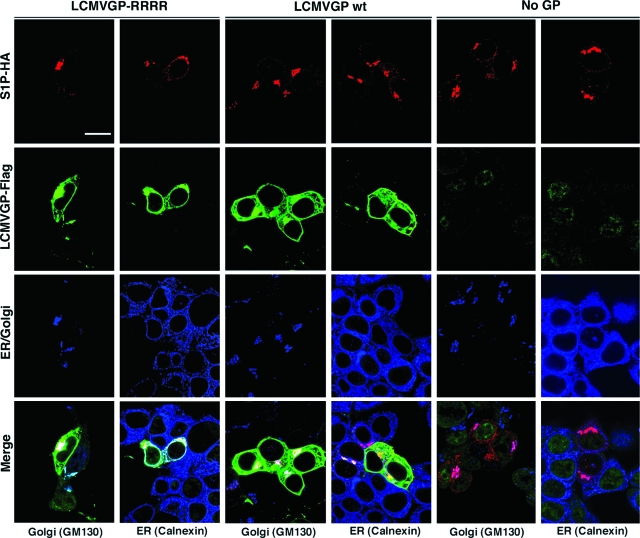
S1P is a transmembrane protein predominantly localized in the Golgi apparatus (33), whereas furin cycles between the plasma membrane, endosomes, and the trans-Golgi network (4, 27, 45, 46). To address a possible impact of the altered proteolytic processing on the subcellular localization of LCMV GP, we examined the cellular distribution of GP-RRRR and GP-WT by confocal microscopy. To this end, we transfected HEK293 cells with Flag-tagged mutant and WT GPs either alone or in combination with HA-tagged S1P. The subcellular distribution of GPs was examined by immunocytochemistry using antibodies to the Flag and HA tags, combined with antibodies to specific markers for the ER (Calnexin) and Golgi apparatus (GM130). The WT and mutant GP-RRRR showed similar patterns of subcellular distribution (Fig. 2) and colocalized with S1P predominantly in the Golgi apparatus. In sum, our data showed that replacement of the endogenous S1P recognition sequence with a canonical furin site does not affect the expression, trafficking, and biological activity of LCMV GP.
FIG. 2.
Colocalization of LCMV GP with S1P. HEK293 cells were transfected with HA-tagged S1P, either alone or in combination with Flag-tagged WT LCMV GP or LCMV GP-RRRR. After 48 h, the cells were fixed, permeabilized, and stained for LCMV GP with a rabbit polyclonal anti-Flag antibody, MAb F7 anti-HA (mouse IgG2a), combined with MAbs to the ER marker Calnexin (mouse IgG1) and the Golgi apparatus marker GM130 (mouse IgG1). Primary antibodies were detected with specific secondary antibodies: anti-rabbit IgG-FITC (green), anti-mouse IgG2a-Rhodamine RedX (red), and anti mouse IgG1-Cy5 (blue). The Images were analyzed using LSM Image Examiner and Image J. Overlap of red and green signals appears white in the merged image. Bar = 10 μM.
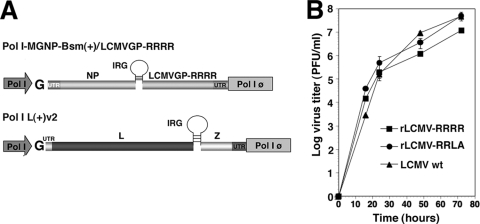
For the rescue of rLCMV-RRRR, we employed a recently developed reverse genetics system for LCMV (44). As a control, we also rescued LCMV containing GP-WT (rLCMV-RRLA). Briefly, the open reading frame (ORF) of GP-RRRR was inserted into the plasmid Pol I-MGNP/Bsm(+), which allowed transcription of the LCMV S antigenome (Sag) RNA under the control of a Pol I promoter (Fig. 3A), together with plasmids expressing the minimal viral trans-acting factors l-polymerase and NP. Infectious viruses were readily detected after 48 h in the supernatants collected from cells transfected with the plasmid cocktails for viral rescue, but not from control samples lacking the plasmid expressing l-polymerase. Determination of the growth kinetics in VeroE6 and BHK21 cells revealed no significant attenuation of the recombinant rLCMV-RRRR and rLCMV-RRLA compared to WT LCMV (Fig. 3B).
FIG. 3.
Rescue of recombinant LCMV expressing mutant GPs. (A) Schematics of plasmids encoding antigenomic LCMV S and L RNA Pol I-MGNP-Bsm(+)/LCMVGP-RRRR and Pol I L(+), respectively, flanked by a Pol I promoter and a Pol I terminator (Pol I φ). The ORFs for LCMV NP (NP), LCMV GP-RRRR, LCMV L (L), and LCMV Z (Z), as well as the intergenic region (IRG) separating the ORFs and the flanking untranslated regions (UTR), are indicated (for details, see the text). (B) Growth of rLCMVs. VeroE6 cells were infected with rLCMVs or WT LCMV ARM53b cl-13 (MOI = 0.1), and virus titers were determined in the supernatants after the indicated time points by plaque assay on VeroE6 cells.
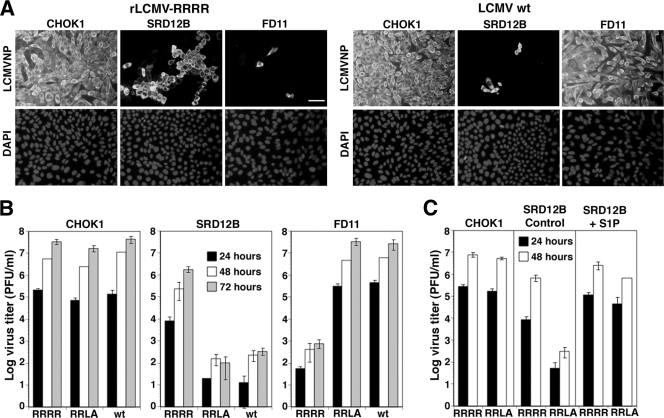
To verify the furin dependence of rLCMV-RRRR, we examined virus multiplication in furin-deficient FD11 cells. Monolayers of FD11 cells, S1P-deficient SRD12B cells, and WT CHOK1 cells were infected with mutant and WT LCMV at a low (0.01) MOI. At 36 h postinfection, the cells were fixed, and infection was detected by IF staining for LCMV NP (8). Cell-to-cell spread of rLCMV-RRRR was severely restricted in FD11 cells, as indicated by the small size of infectious foci (Fig. 4A), and a marked reduction in infectious titers was detected in cell culture supernatants (Fig. 4B). Consistent with previous findings (9, 10), WT LCMV and rLCMV-RRLA multiplied normally in FD11 cells but showed reduced spread and multiplication in S1P-deficient SRD12B cells (Fig. 4A and B). Interestingly, rLCMV-RRRR exhibited a mild but consistent reduction in virus spread (Fig. 4A) and virus production (Fig. 4B) in S1P-deficient cells compared to WT CHOK1 cells. This finding was unexpected, as GPC processing of GP-RRRR appeared normal in the absence of S1P (Fig. 1C).
FIG. 4.
Furin processing is required for production of infectious LCMV-RRRR and cell-to-cell propagation. (A) Monolayers of furin-deficient (FD11), S1P-deficient (SRD12B), and WT CHOK1 cells were infected with WT LCMV (LCMV wt) and rLCMV-RRRR at an MOI of 0.01. After 36 h, the cells were fixed, and infected cells were detected by immunostaining them with MAb 113 to LCMV NP using a FITC-labeled secondary antibody. Nuclei were counterstained with DAPI. Bar = 50 μM. (B) Production of infectious virus in FD11, SRD12B, and CHOK1 cells. The cells were infected with WT LCMV (wt), rLCMV-RRRR (RRRR), and rLCMV-RRLA (RRLA) at an MOI of 1. The cell supernatants were harvested at the indicated times, and infectious-virus titers were determined by plaque assay on VeroE6 cells (means ± standard deviations; n = 3). (C) Expression of recombinant S1P in S1P-deficient cells restores multiplication of rLCMV-RRLA and rLCMV-RRRR. CHOK1 cells and SRD12B cells were transiently transfected with either an expression plasmid for recombinant S1P (SRD12B + S1P) or empty vector (SRD12B control) and subsequently infected with rLCMV-RRLA and rLCMV-RRRR. After 48 h, virus titers in the supernatant were determined as for panel B.
To test if the observed reduction in rLCMV-RRRR multiplication was due to the deficiency in S1P or other factors present or absent in SRD12B cells, S1P expression in SRD12B cells was reconstituted by transient transfection of recombinant S1P. Transfection with an expression plasmid for S1P, but not empty vector, resulted in production levels of rLCMV-RRLA and rLCMV-RRRR comparable to those of WT CHOK1 cells (Fig. 4C).
Antiviral activity of dec-RRLL-CMK.
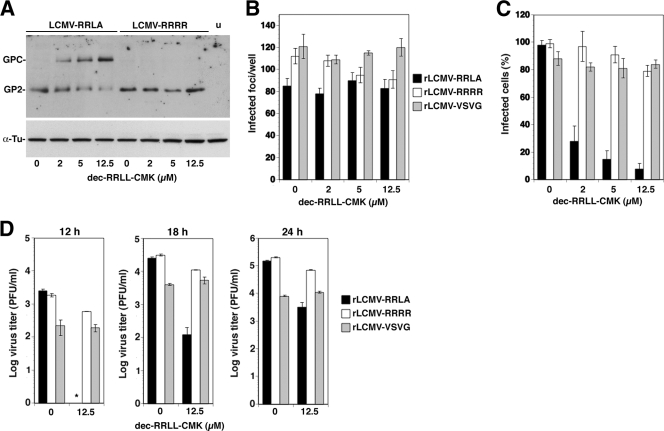
To asses the inhibition of LCMV GPC processing by dec-RRLL-CMK in the context of productive arenavirus infection, we infected CHOK1 cells with rLCMV-RRLA and rLCMV-RRRR at a high MOI (3), which resulted consistently in >98% of the cells expressing viral antigen. At 1 h postinfection, we treated the cells with increasing concentrations of dec-RRLL-CMK, and 36 h later, cell lysates were prepared for Western blot analysis to assess GPC processing (Fig. 5A). The processing of GPC of rLCMV-RRLA, but not rLCMV-RRRR, was inhibited by dec-RRLL-CMK in a dose-dependent manner with consistent inhibition of >90% at 12.5 μM. At a higher concentration, dec-RRLL-CMK affected the overall expression level of GPC, likely due to nonspecific cytotoxicity (data not shown).
FIG. 5.
The S1P inhibitor dec-RRLL-CMK shows specific antiviral activity. (A) Inhibition of GPC processing by dec-RRLL-CMK. CHOK1 cells cultured in lipid-supplemented medium were infected with rLCMV-RRRR and rLCMV-RRLA (MOI = 3) or left uninfected (u). One hour postinfection, the indicated concentrations of dec-RRLL-CMK were added for 36 h. The processing of GPC was examined by Western blot analysis using an antibody to LCMV GP2. Unprocessed GPC and mature (processed) GP2 are indicated. For normalization, α-tubulin (α-Tu) was detected. (B) The S1P inhibitor dec-RRLL-CMK has no effect on early LCMV infection. Monolayers of CHOK1 cells in LabTek tissue culture chambers were pretreated with the indicated concentrations of dec-RRLL-CMK for 1 hour and then infected with 100 PFU of rLCMV-RRRA, rLCMV-RRRR, and rLCMV-VSVG. After 16 h in the presence of dec-RRLL-CMK, the cultures were fixed, and foci of infected cells were detected by IF using MAb 113 to LCMV NP (means ± standard deviations; n = 4). (C) The S1P inhibitor reduces cell-to-cell propagation of infection. Monolayers of CHOK1 cells were infected with the recombinant LCMV variants at an MOI of 0.01. One hour postinfection, the indicated concentrations of dec-RRLL-CMK were added, and the cells were cultured in the presence of inhibitor. After 36 h, the cells were detached by mild trypsinization and fixed, and intracellular staining for NP was performed, followed by quantification of NP-positive cells by flow cytometry (see Materials and Methods). The percentages of NP-positive cells are given (means ± standard deviations; n = 3). (D) The S1P inhibitor reduces virus production. CHOK1 monolayers were infected with rLCMV-RRLA, rLCMV-RRRR, and rLCMV-VSVG (MOI = 3), and dec-RRLL-CMK (12.5 μM) was added at 1 hour postinfection. The cell culture supernatants were harvested and dialyzed against Hanks balanced salt solution to remove the inhibitor, and infectious-virus titers were determined by IF assay on VeroE6 cells (means ± standard deviations; n = 4).
To determine the ability of dec-RRLL-CMK to block viral spread, monolayers of CHOK1 cells were infected at a low (0.01) MOI with rLCMV-RRLA and rLCMV-RRRR and treated with increasing concentrations of inhibitor. As an additional control, a recombinant LCMV expressing the GP of vesicular stomatitis virus (VSV) was included. In contrast to WT LCMV GP and LCMV GP-RRRR, the biosynthesis of fusion-competent VSV GP does not depend on proteolytic processing by cellular proteases (41). To assess the possible effects of dec-RRLL-CMK on early steps of LCMV infection, the inhibitor was added 1 hour prior to infection, and the cultures were fixed after one round of viral replication (16 h). Infected cells were detected by IF staining for LCMV NP, and the number of infected foci was determined. Up to 12.5 μM, dec-RRLL-CMK had no significant effect on the number of infected foci, excluding inhibition of viral entry and other early steps of the viral life cycle (Fig. 5B). To assess inhibition of cell-to-cell propagation of infection, cells were infected at an MOI of 0.01 and the inhibitor was added at 1 hour postinfection. The cells were cultured for 36 h, and the percentage of infected cells was determined by intracellular staining for LCMV NP in flow cytometry. Increasing concentrations of dec-RRLL-CMK resulted in a dose-dependent reduction in the numbers of NP-positive cells in cultures infected with rLCMV-RRLA, but not rLCMV-RRRR and rLCMV-VSV G (Fig. 5C).
Next, we assessed the ability of dec-RRLL-CMK to block virus production from infected cells. For this purpose, CHOK1 cells were infected at a high MOI (3) and virus production was determined in the presence and absence of inhibitor. Treatment with dec-RRLL-CMK resulted in a significant reduction of rLCMV-RRLA titers; only mild reduction in rLCMV-RRRR, which was not consistently observed; and no significant drop in rLCMV-VSVG titers (Fig. 5D). Compared with the infection of S1P-deficient cells with rLCMV-RRRR, inhibition of S1P with dec-RRLL-CMK showed a weaker impact on virus production (compare Fig. 5D with Fig. 4B). The reason for this is not entirely clear, but it may be due to the incomplete inhibition of S1P activity in dec-RRLL-CMK-treated cells, as illustrated by the detection of residual GPC processing at the inhibitor concentration used (Fig. 5A).
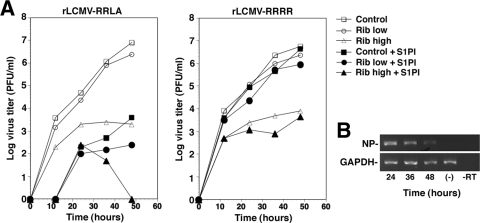
Inhibition of GPC processing and ribavirin show additive antiviral effects.
The only licensed drug for the treatment of human arenavirus infection is the nucleoside analogue ribavirin (29). In vitro and in vivo studies have documented the prophylactic and therapeutic value of ribavirin against several arenaviruses, including LCMV (42), LASV (24), Machupo virus (15), and JUNV (25). Experimental studies with LCMV revealed that a main mechanism by which ribavirin exerts its antiviral effect is by inhibiting virus replication (42), opening the possibility of additive effects with inhibitors of arenavirus GPC processing. To investigate this possibility, CHOK1 cells were treated for 6 hours with either a low dose (50 μM) or a high dose (400 μM) of ribavirin, followed by infection at a low (0.1) MOI. One hour postinfection, dec-RRLL-CMK (12.5 μM) was added, and infectious virus production was monitored over time. Due to the instability of dec-RRLL-CMK, a second dose of inhibitor was added after 24 h. The combination of high-dose ribavirin with dec-RRLL-CMK resulted in an additive antiviral effect in cells infected with rLCMV-RRLA, but not rLCMV-RRRR (Fig. 6A) . Low-dose ribavirin combined with dec-RRLL-CMK resulted in an additive antiviral effect, and the combination of high-dose ribavirin with the S1P inhibitor resulted in undetectable titers of infectious virus after 48 h as assessed by IF staining in CHOK1 cells. However, despite the absence of detectable infectious-virus titers, we consistently detected viral RNA by RT-PCR in cells treated with high-dose ribavirin and dec-RRLL-CMK after 48 h (Fig. 6B), arguing against complete extinction of the virus. A possible concern with the combined application of furin inhibitor and ribavirin was excessive toxicity due to some unknown synergistic effects of the two compounds on normal host cell metabolism. To address this issue, we assessed the cytotoxicities of the individual compounds and combinations thereof using the CellTiter-Glo assay. The combination of dec-RRLL-CMK with ribavirin did not significantly increase cytotoxicity beyond that observed with ribavirin and dec-RRLL-CMK alone (Table 2), suggesting that the additive antiviral effects are not due to increased toxicity of the combined treatments.
FIG. 6.
Inhibition of GPC processing enhances the antiviral activity of ribavirin. (A) Treatment of infected cells with ribavirin and S1P inhibitor. CHOK1 cells were treated for 6 hours with 50 μM ribavirin (Rib low), 400 μM ribavirin (Rib high), or vehicle (Control) and then infected with rLCMV-RRRA and rLCMV-RRRR at an MOI of 0.1. At 1 hour postinfection, 12.5 μM dec-RRLL-CMK was added. Virus titers were determined by IF assay on VeroE6 cells. Each time value represents the average of two independent experiments. (B) Detection of viral RNA in cells treated with 400 μM ribavirin and 12.5 μM dec-RRLL-CMK. Total cellular RNA was extracted at the indicated time points and analyzed by RT-PCR. The RT reaction was primed with random hexamers, and the resulting cNDAs were amplified with specific primers for the viral NP or the cellular GAPDH housekeeping gene. RNA from uninfected cells was included as a negative control (−). One out of three representative examples is shown.
TABLE 2.
Cytotoxicity of dec-RRLL-CMK combined with ribavirin in CHOK1 cellsa
| Drug | Cell viability (%) |
|---|---|
| dec-RRLL-CMK | 91.1 ± 2.1 |
| Ribavirin low | 98.1 ± 2.7 |
| Ribavirin high | 88.5 ± 5.6 |
| dec-RRLL-CMK + ribavirin low | 89.5 ± 6.2 |
| dec-RRLL-CMK + ribavirin high | 82.2 ± 5.5 |
Cells were treated with 12.5 μM of dec-RRLL-CMK and ribavirin at a low dose (50 μM) and a high dose (400 μM) for 48 h, and cell viability assessed by CellTiter-Glo assay. The relative cell viability was calculated using the dimethyl sulfoxide control for normalization (means ± standard deviations; n = 3).
Emergence of S1P-independent viral escape variants is an unlikely event.
The use of antiviral drugs is complicated by the frequent emergence of resistant virus variants. In fact, drug-resistant variants have been isolated for virtually any virus for which specific antiviral drugs have been developed. In particular, viruses with an RNA genome, like arenaviruses, have high mutation rates that allow them to rapidly adapt to changes in the environment, e.g., the presence of an antiviral drug. The assessment of the likelihood of such drug-resistant viruses emerging has important practical implications, and we sought to investigate this issue in the context of inhibition of arenavirus GPC processing. The ability of arenaviruses to establish long-term persistent infections provided us with an experimental setting that allowed a continued increase in the number of rounds of intracellular virus replication, facilitating the selection of viral variants whose GPCs could be processed by another protease.
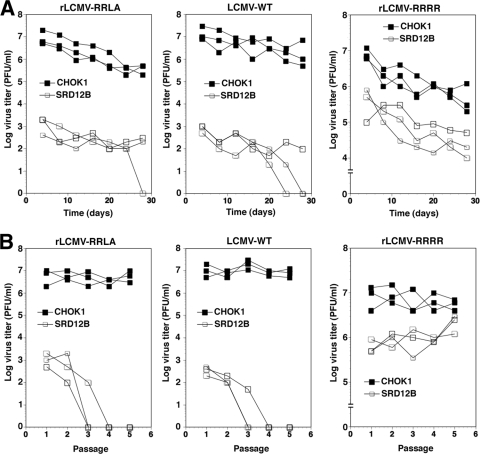
To address this issue, we monitored the emergence of escape variants of LCMV in cells deficient in S1P. Considering the differences in the recognition site of S1P (RRLA) present in LCMV and the sequence specificity of other cellular proprotein convertases (R-Xn-R), the generation of escape variants with altered protease requirements may require two simultaneous nucleotide substitutions, necessitating a large virus population of >106 infectious particles. To ensure a starting population of sufficient size, 5 × 106 cells were infected with rLCMV-RRLA at a high MOI of 1, resulting in >95% infected cells after 48 h, and the cells were then passaged every 4 days for 28 days. At each passage, the virus titers in the cell culture supernatant were determined by IF assay. Parallel cultures were infected with rLCMV-RRRR. As expected, infection of WT CHOK1 cells with all viruses resulted in persistently infected cell lines that produced high levels of infectious virus over time (Fig. 7A). Consistent with our previous findings, rLCMV-RRRR production in S1P-deficient cells was lower than in WT cells. Nevertheless, rLCMV-RRRR established a persistent infection in S1P-deficient cells, with high titers of virus production throughout the experiment. Interestingly, over the entire duration of the experiment, S1P-deficient cells persistently infected with WT LCMV and LCMV-RRLA produced negligible titers of infectious virus (Fig. 7A). We also performed serial passages of virus in S1P-deficient and WT cells. The cells were infected at a high MOI, resulting in >95% infected cells. The supernatants were collected after 3 days and used to initiate serial passages, where each time fresh cell monolayers were infected with tissue culture supernatants from the previous passage. High virus titers were consistently detected in culture supernatants from WT cells, whereas systematic extinction of WT LCMV and rLCMV-RRLA, but not rLCMV-RRRR, in S1P-deficient cells was observed after a few passages (Fig. 7B).
FIG. 7.
Extinction of WT LCMV from S1P-deficient cells. (A) Persistent infection of LCMV-WT, rLCMV-RRLA, and rLCMV-RRRR in S1P-deficient cells. Triplicates of S1P-deficient SRD12B cells and WT CHOK1 cells were infected with WT LCMV (LCMV-WT), rLCMV-RRLA, and rLCMV-RRRR at an MOI of 1 and passaged every 4 days. At the indicated times, virus titers were determined by IF assay on VeroE6 cells. One representative example out of three independent experiments is shown. (B) Triplicates of S1P-deficient SRD12B and CHOK1 cells were infected with LCMV-WT, rLCMV-RRLA, and rLCMV-RRRR at an MOI of 1. After 3 days, conditioned tissue culture supernatant was mixed 1:1 with fresh medium and used to infect fresh monolayers of cells. For each passage, virus titers in supernatants were determined as for panel A. Note the extinction of LVMV-WT and rLCMV-RRLA in S1P-deficient cells.
DISCUSSION
In human arenavirus infections, the strong predictive value of the virus concentration in the patient's blood for disease outcome indicates a close competition between viral spread and replication and the patient's antiviral immune defense. Recently, we and others have identified novel classes of arenavirus entry inhibitors, including DNA aptamers (19) and several potent small-molecule inhibitors (3, 20). While such entry inhibitors are likely efficacious early in infection, they are rather ineffective once the host cell has become infected. It is therefore of great importance to also target later steps of arenavirus multiplication, allowing combinatorial multidrug therapies. Arenavirus GPC processing by cellular S1P is critical for productive arenavirus infection (2, 17, 21, 37), making this late step in the viral life cycle an attractive candidate for complementary therapeutic intervention. Previous studies employed S1P-adapted α1-antitrypsin variants to target S1P-mediated processing of the envelope GP of the human-pathogenic Crimean Congo hemorrhagic fever virus (34) and the GPC of LASV (22). When expressed in mammalian cells, these protein-based S1P inhibitors inhibited cleavage of LASV GPC and reduced LASV infectious titers produced by infected cells (22). Since protein-based S1P inhibitors are not cell permeable, their application for antiviral therapy in vivo may be difficult. In the present study, we therefore evaluated a recently developed peptide-derived inhibitor of S1P, dec-RRLL-CMK (30). Since previous reports documented significant cytotoxicity of this inhibitor, we selected a cell line and experimental conditions that minimized toxicity. To control for off-target effects of dec-RRLL-CMK in our studies, we generated a recombinant LCMV with a furin recognition site in its GPC, rLCMV-RRRR. The rescued virus showed no significant attenuation compared to the WT, despite a complete switch in protease dependence from S1P to furin. The furin-dependent mutant virus was nonlytic and established persistent infection in mammalian cells. Interestingly, despite the S1P-independent processing of rLCMV-RRRR GPC, the mutant virus showed impaired multiplication in S1P-deficient cells. Reconstitution of S1P activity by transient expression of recombinant S1P restored virus production to WT levels, suggesting a role of S1P for optimal LCMV multiplication that is unrelated to GPC cleavage. This finding was somewhat surprising and in apparent contradiction of results obtained with recombinant LCMV expressing the GP of VSV, which grew to similar titers in S1P-deficient and WT CHOK1 cells (32), a finding we were able to confirm (data not shown). The reasons for this discrepancy are currently unclear but might be related to the significantly lower multiplication rate of rLCMV-VSV G due to attenuation (32). Since the S1P-deficient SRD12B cells were supplemented with cholesterol, the impaired multiplication of rLCMV-RRRR might be unrelated to S1P-dependent cholesterol homeostasis. In the host cell, S1P is also crucial for the processing of the activation transcription factor ATF6 implicated in the host cell's ER stress response. We currently cannot exclude the possibility that the effect is related to the cell's ability to cope with ER stress that may occur during arenavirus infection. The roles of ATF6 and the cell's ER stress response in the context of arenavirus infection are currently under investigation in our laboratory.
The availability of a furin-dependent, S1P-independent LCMV variant allowed the evaluation of the specific antiviral effect of dec-RRLL-CMK mediated by blocking of S1P-dependent arenavirus GPC processing. Despite the consistent detection of circa 5% residual cleaved GPC in rLCMV-RRLA-infected cells treated with the maximal concentration of dec-RRLL-CMK used, we observed a marked reduction of cell-to-cell propagation of infection and infectious-virus production. Due to the oligomeric structure of the LCMV GP, which resembles other class I fusion-active viral GPs (10), partial GPC cleavage may perturb the function of GP oligomers, e.g., GP-mediated fusion in acidified endosomes during viral entry, resulting in a significant antiviral effect even with only partial inhibition of processing. Combination with ribavirin, which is currently the only drug used clinically to treat arenavirus infections in humans (16, 24, 47), resulted in additive antiviral effects. This finding suggests that combined drug therapy with ribavirin and inhibitors of GPC processing may allow the use of lower doses, which would reduce unwanted side effects of the drug.
A major concern with each novel class of antiviral drugs is the frequent emergence of resistant virus variants. This is also a problem with arenaviruses, whose error-prone RNA-dependent RNA polymerases facilitate rapid virus evolution and adaptation to changes in the environment, e.g., the presence of antiviral drugs (50). Arenaviruses establish long-term persistent infections in mammalian cells in culture. This provided us with an experimental setting that allowed the selection of viral variants whose GPCs could be processed by another protease. In cells deficient in S1P, the furin-dependent LCMV variant established persistent infection with production of high titers of infectious virus for several weeks. In contrast, persistently WT LCMV- and rLCMV-RRLA-infected S1P-null cells produced negligible or undetectable infectivity despite a continued presence of intracellular viral antigen. A similar effect was previously observed in our laboratory with S1P-deficient cells infected with the New World arenavirus JUNV vaccine strain Candid 1 (37). Moreover, serial passages of rLCMV-RRRR in S1P-null cells maintained productive virus infection, whereas WT LCMV and rLCMV-RRLA underwent rapid and consistent virus extinction after a few passages. Together, the data suggest that the emergence of S1P-independent viral escape variants is an unlikely event. The reasons for this are currently unclear. In theory, an escape variant in S1P-deficient cells will be generated when a processing pathway involving a protease other than S1P becomes operational. This may require some types of mutations at the protease recognition site, but also likely elsewhere in GPC, as S1P recognition appears to involve amino acid residues of GPC outside of the actual protease recognition site (30). In a follow-up to the present study, we aim to characterize the GPC variants present in the low-titer infectious virus released from persistently infected S1P-null cells. It will be interesting to identify specific mutations that allow LCMV to grow independently of S1P and to test the competitive fitness of these viral variants.
The key role of S1P in productive infection with human-pathogenic arenaviruses, together with a low probability of the emergence of S1P-independent escape variants, makes S1P a promising cellular target for the development of novel and potent antiarenaviral drugs. Since S1P plays important roles in a number of physiological processes, the development of inhibitors that specifically target the processing of arenavirus GPC while having minimal effects on the processing of other cellular substrates of S1P has, of course, the highest priority. However, hemorrhagic fevers caused by arenaviruses in humans are acute diseases with a relatively rapid course of infection (12, 23). Consequently, drug intervention to treat hemorrhagic arenaviruses would be restricted to short periods. Dietary supplementation of cholesterol and other lipids for patients in intensive care would counteract the effects of S1P inhibitors on lipid metabolism. Further, cells deficient in S1P are still able to mount an ER stress response at circa 30% of that observed in WT cells (53), indicating that short-term inhibition of the S1P activity is unlikely to result in unacceptable levels of cell and tissue toxicity. Therefore, candidate drugs that lack absolute specificity and to some degree affect the processing of cellular targets of S1P may still represent important candidates to be evaluated as antiviral drugs.
Acknowledgments
We thank Amalio Telenti (University of Lausanne) and Michael B. A. Oldstone (Scripps Research Institute, La Jolla, CA) for their generous support and Esteban Domingo and Antonella Pasquato for valuable discussions. We further acknowledge Bruce Beutler (Scripps) for the recombinant S1P cDNA and J. L. Goldstein for kindly providing the S1P-deficient cell line SRD12B. The retroviral construct pLZRs-Luc-gfp was provided by Gary Nabel.
This research was supported by Swiss National Science Foundation grant 3100A0-120250/1 (S.K.), U.S. PHS grant AI065560 (S.K.), and NIH grant AI47140 (J.C.D.L.T.). S.K. was further supported by a Medical Research Position Award from the Foundation Max Cloetta (Switzerland) and the Marie Curie International Reintegration Grant 224780 from the European Community.
Footnotes
Published ahead of print on 21 October 2009.
REFERENCES
- 1.Barton, L. L., M. B. Mets, and C. L. Beauchamp. 2002. Lymphocytic choriomeningitis virus: emerging fetal teratogen. Am. J. Obstet Gynecol. 187:1715-1716. [DOI] [PubMed] [Google Scholar]
- 2.Beyer, W. R., D. Popplau, W. Garten, D. von Laer, and O. Lenz. 2003. Endoproteolytic processing of the lymphocytic choriomeningitis virus glycoprotein by the subtilase SKI-1/S1P. J. Virol. 77:2866-2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bolken, T. C., S. Laquerre, Y. Zhang, T. R. Bailey, D. C. Pevear, S. S. Kickner, L. E. Sperzel, K. F. Jones, T. K. Warren, S. Amanda Lund, D. L. Kirkwood-Watts, D. S. King, A. C. Shurtleff, M. C. Guttieri, Y. Deng, M. Bleam, and D. E. Hruby. 2006. Identification and characterization of potent small molecule inhibitor of hemorrhagic fever New World arenaviruses. Antiviral Res. 69:86-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bosshart, H., J. Humphrey, E. Deignan, J. Davidson, J. Drazba, L. Yuan, V. Oorschot, P. J. Peters, and J. S. Bonifacino. 1994. The cytoplasmic domain mediates localization of furin to the trans-Golgi network en route to the endosomal/lysosomal system. J. Cell Biol. 126:1157-1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown, M. S., and J. L. Goldstein. 1997. The SREBP pathway: regulation of cholesterol metabolism by proteolysis of a membrane-bound transcription factor. Cell 89:331-340. [DOI] [PubMed] [Google Scholar]
- 6.Buchmeier, M. J., J. C. de la Torre, and C. J. Peters. 2007. Arenaviridae: the viruses and their replication, p. 1791-1828. In D. L. Knipe and P. M. Howley (ed.), Fields virology, 4th ed. Lippincott-Raven, Philadelphia, PA.
- 7.Buchmeier, M. J., H. A. Lewicki, O. Tomori, and M. B. Oldstone. 1981. Monoclonal antibodies to lymphocytic choriomeningitis and pichinde viruses: generation, characterization, and cross-reactivity with other arenaviruses. Virology 113:73-85. [DOI] [PubMed] [Google Scholar]
- 8.Cao, W., M. D. Henry, P. Borrow, H. Yamada, J. H. Elder, E. V. Ravkov, S. T. Nichol, R. W. Compans, K. P. Campbell, and M. B. Oldstone. 1998. Identification of alpha-dystroglycan as a receptor for lymphocytic choriomeningitis virus and Lassa fever virus. Science 282:2079-2081. [DOI] [PubMed] [Google Scholar]
- 9.Dutko, F. J., and M. B. Oldstone. 1983. Genomic and biological variation among commonly used lymphocytic choriomeningitis virus strains. J. Gen. Virol. 64:1689-1698. [DOI] [PubMed] [Google Scholar]
- 10.Eschli, B., K. Quirin, A. Wepf, J. Weber, R. Zinkernagel, and H. Hengartner. 2006. Identification of an N-terminal trimeric coiled-coil core within arenavirus glycoprotein 2 permits assignment to class I viral fusion proteins. J. Virol. 80:5897-5907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fischer, S. A., M. B. Graham, M. J. Kuehnert, C. N. Kotton, A. Srinivasan, F. M. Marty, J. A. Comer, J. Guarner, C. D. Paddock, D. L. DeMeo, W. J. Shieh, B. R. Erickson, U. Bandy, A. DeMaria, Jr., J. P. Davis, F. L. Delmonico, B. Pavlin, A. Likos, M. J. Vincent, T. K. Sealy, C. S. Goldsmith, D. B. Jernigan, P. E. Rollin, M. M. Packard, M. Patel, C. Rowland, R. F. Helfand, S. T. Nichol, J. A. Fishman, T. Ksiazek, and S. R. Zaki. 2006. Transmission of lymphocytic choriomeningitis virus by organ transplantation. N. Engl. J. Med. 354:2235-2249. [DOI] [PubMed] [Google Scholar]
- 12.Geisbert, T. W., and P. B. Jahrling. 2004. Exotic emerging viral diseases: progress and challenges. Nat. Med. 10:S110-S121. [DOI] [PubMed] [Google Scholar]
- 13.Gordon, V. M., K. R. Klimpel, N. Arora, M. A. Henderson, and S. H. Leppla. 1995. Proteolytic activation of bacterial toxins by eukaryotic cells is performed by furin and by additional cellular proteases. Infect. Immun. 63:82-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hallenberger, S., V. Bosch, H. Angliker, E. Shaw, H. D. Klenk, and W. Garten. 1992. Inhibition of furin-mediated cleavage activation of HIV-1 glycoprotein gp160. Nature 360:358-361. [DOI] [PubMed] [Google Scholar]
- 15.Kilgore, P. E., T. G. Ksiazek, P. E. Rollin, J. N. Mills, M. R. Villagra, M. J. Montenegro, M. A. Costales, L. C. Paredes, and C. J. Peters. 1997. Treatment of Bolivian hemorrhagic fever with intravenous ribavirin. Clin. Infect. Dis. 24:718-722. [DOI] [PubMed] [Google Scholar]
- 16.Kunz, S., and J. C. de la Torre. 2005. Novel antiviral strategies to combat human Arenavirus infections. Curr. Mol. Med. 5:735-751. [DOI] [PubMed] [Google Scholar]
- 17.Kunz, S., K. H. Edelmann, J.-C. de la Torre, R. Gorney, and M. B. A. Oldstone. 2003. Mechanisms for lymphocytic choriomeningitis virus glycoprotein cleavage, transport, and incorporation into virions. Virology 314:168-178. [DOI] [PubMed] [Google Scholar]
- 18.Kunz, S., J. M. Rojek, A. J. Roberts, D. B. McGavern, M. B. Oldstone, and J. C. de la Torre. 2006. Altered central nervous system gene expression caused by congenitally acquired persistent infection with lymphocytic choriomeningitis virus. J. Virol. 80:9082-9092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee, A. M., J. M. Rojek, A. Gundersen, U. Stroher, J. M. Juteau, A. Vaillant, and S. Kunz. 2008. Inhibition of cellular entry of lymphocytic choriomeningitis virus by amphipathic DNA polymers. Virology 372:107-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee, A. M., J. M. Rojek, C. F. Spiropoulou, A. T. Gundersen, W. Jin, A. Shaginian, J. York, J. H. Nunberg, D. L. Boger, M. B. Oldstone, and S. Kunz. 2008. Unique small molecule entry inhibitors of hemorrhagic fever arenaviruses. J. Biol. Chem. 283:18734-18742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lenz, O., J. ter Meulen, H. D. Klenk, N. G. Seidah, and W. Garten. 2001. The Lassa virus glycoprotein precursor GP-C is proteolytically processed by subtilase SKI-1/S1P. Proc. Natl. Acad. Sci. U. S. A. 98:12701-12705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maisa, A., U. Stroher, H. D. Klenk, W. Garten, and T. Strecker. 2009. Inhibition of Lassa virus glycoprotein cleavage and multicycle replication by site 1 protease-adapted alpha(1)-antitrypsin variants. PLoS Negl. Trop. Dis. 3:e446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McCormick, J. B., and S. P. Fisher-Hoch. 2002. Lassa fever. Curr. Top. Microbiol. Immunol. 262:75-109. [DOI] [PubMed] [Google Scholar]
- 24.McCormick, J. B., I. J. King, P. A. Webb, C. L. Scribner, R. B. Craven, K. M. Johnson, L. H. Elliott, and R. Belmont-Williams. 1986. Lassa fever. Effective therapy with ribavirin. N. Engl. J. Med. 314:20-26. [DOI] [PubMed] [Google Scholar]
- 25.McKee, K. T., Jr., J. W. Huggins, C. J. Trahan, and B. G. Mahlandt. 1988. Ribavirin prophylaxis and therapy for experimental Argentine hemorrhagic fever. Antimicrob. Agents Chemother. 32:1304-1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mets, M. B., L. L. Barton, A. S. Khan, and T. G. Ksiazek. 2000. Lymphocytic choriomeningitis virus: an underdiagnosed cause of congenital chorioretinitis. Am. J. Ophthalmol. 130:209-215. [DOI] [PubMed] [Google Scholar]
- 27.Molloy, S. S., L. Thomas, J. K. VanSlyke, P. E. Stenberg, and G. Thomas. 1994. Intracellular trafficking and activation of the furin proprotein convertase: localization to the TGN and recycling from the cell surface. EMBO J. 13:18-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Palacios, G., J. Druce, L. Du, T. Tran, C. Birch, T. Briese, S. Conlan, P. L. Quan, J. Hui, J. Marshall, J. F. Simons, M. Egholm, C. D. Paddock, W. J. Shieh, C. S. Goldsmith, S. R. Zaki, M. Catton, and W. I. Lipkin. 2008. A new arenavirus in a cluster of fatal transplant-associated diseases. N. Engl. J. Med. 358:991-998. [DOI] [PubMed] [Google Scholar]
- 29.Parker, W. B. 2005. Metabolism and antiviral activity of ribavirin. Virus Res. 107:165-171. [DOI] [PubMed] [Google Scholar]
- 30.Pasquato, A., P. Pullikotil, M. C. Asselin, M. Vacatello, L. Paolillo, F. Ghezzo, F. Basso, C. Di Bello, M. Dettin, and N. G. Seidah. 2006. The proprotein convertase SKI-1/S1P. In vitro analysis of Lassa virus glycoprotein-derived substrates and ex vivo validation of irreversible peptide inhibitors. J. Biol. Chem. 281:23471-23481. [DOI] [PubMed] [Google Scholar]
- 31.Peters, C. J. 2002. Human infection with arenaviruses in the Americas. Curr. Top. Microbiol. Immunol. 262:65-74. [DOI] [PubMed] [Google Scholar]
- 32.Pinschewer, D. D., M. Perez, A. B. Sanchez, and J. C. de la Torre. 2003. Recombinant lymphocytic choriomeningitis virus expressing vesicular stomatitis virus glycoprotein. Proc. Natl. Acad. Sci. U. S. A. 100:7895-7900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pullikotil, P., S. Benjannet, J. Mayne, and N. G. Seidah. 2007. The proprotein convertase SKI-1/S1P: alternate translation and subcellular localization. J. Biol. Chem. 282:27402-27413. [DOI] [PubMed] [Google Scholar]
- 34.Pullikotil, P., M. Vincent, S. T. Nichol, and N. G. Seidah. 2004. Development of protein-based inhibitors of the proprotein of convertase SKI-1/S1P: processing of SREBP-2, ATF6, and a viral glycoprotein. J. Biol. Chem. 279:17338-17347. [DOI] [PubMed] [Google Scholar]
- 35.Rawson, R. B., D. Cheng, M. S. Brown, and J. L. Goldstein. 1998. Isolation of cholesterol-requiring mutant Chinese hamster ovary cells with defects in cleavage of sterol regulatory element-binding proteins at site 1. J. Biol. Chem. 273:28261-28269. [DOI] [PubMed] [Google Scholar]
- 36.Rojek, J. M., K. P. Campbell, M. B. Oldstone, and S. Kunz. 2007. Old World arenavirus infection interferes with the expression of functional {alpha}-dystroglycan in the host cell. Mol. Biol. Cell 29:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rojek, J. M., A. M. Lee, N. Nguyen, C. F. Spiropoulou, and S. Kunz. 2008. Site 1 protease is required for proteolytic processing of the glycoproteins of the South American hemorrhagic fever viruses Junin, Machupo, and Guanarito. J. Virol. 82:6045-6051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rojek, J. M., A. B. Sanchez, N. T. Nguyen, J. C. de la Torre, and S. Kunz. 2008. Different mechanisms of cell entry by human-pathogenic Old World and New World arenaviruses. J. Virol. 82:7677-7687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rojek, J. M., C. F. Spiropoulou, K. P. Campbell, and S. Kunz. 2007. Old World and clade C New World arenaviruses mimic the molecular mechanism of receptor recognition used by {alpha}-dystroglycan's host-derived ligands. J. Virol. 81:5685-5695. Epub 2007 Mar 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rojek, J. M., C. F. Spiropoulou, and S. Kunz. 2006. Characterization of the cellular receptors for the South American hemorrhagic fever viruses Junin, Guanarito, and Machupo. Virology 349:476-491. [DOI] [PubMed] [Google Scholar]
- 41.Rose, J. K., and M. A. Whitt. 2001. Rhabdoviridae: the viruses and their replication, p. 1221-1244. In B. N. Fields, D. L. Knipe, and P. M. Howley (ed.), Fields virology. Lippincott-Raven, Philadelphia, PA.
- 42.Ruiz-Jarabo, C. M., C. Ly, E. Domingo, and J. C. de la Torre. 2003. Lethal mutagenesis of the prototypic arenavirus lymphocytic choriomeningitis virus (LCMV). Virology 308:37-47. [DOI] [PubMed] [Google Scholar]
- 43.Sakai, J., A. Nohturfft, J. L. Goldstein, and M. S. Brown. 1998. Cleavage of sterol regulatory element-binding proteins (SREBPs) at site-1 requires interaction with SREBP cleavage-activating protein. Evidence from in vivo competition studies. J. Biol. Chem. 273:5785-5793. [DOI] [PubMed] [Google Scholar]
- 44.Sanchez, A. B., and J. C. de la Torre. 2006. Rescue of the prototypic Arenavirus LCMV entirely from plasmid. Virology 350:370-380. [DOI] [PubMed] [Google Scholar]
- 45.Schafer, W., A. Stroh, S. Berghofer, J. Seiler, M. Vey, M. L. Kruse, H. F. Kern, H. D. Klenk, and W. Garten. 1995. Two independent targeting signals in the cytoplasmic domain determine trans-Golgi network localization and endosomal trafficking of the proprotein convertase furin. EMBO J. 14:2424-2435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schapiro, F. B., T. T. Soe, W. G. Mallet, and F. R. Maxfield. 2004. Role of cytoplasmic domain serines in intracellular trafficking of furin. Mol. Biol. Cell 15:2884-2894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schmitz, H., B. Kohler, T. Laue, C. Drosten, P. J. Veldkamp, S. Gunther, P. Emmerich, H. P. Geisen, K. Fleischer, M. F. Beersma, and A. Hoerauf. 2002. Monitoring of clinical and laboratory data in two cases of imported Lassa fever. Microbes Infect. 4:43-50. [DOI] [PubMed] [Google Scholar]
- 48.Schroder, M., and R. J. Kaufman. 2005. The mammalian unfolded protein response. Annu. Rev. Biochem. 74:739-789. [DOI] [PubMed] [Google Scholar]
- 49.Seidah, N. G., S. J. Mowla, J. Hamelin, A. M. Mamarbachi, S. Benjannet, B. B. Toure, A. Basak, J. S. Munzer, J. Marcinkiewicz, M. Zhong, J. C. Barale, C. Lazure, R. A. Murphy, M. Chretien, and M. Marcinkiewicz. 1999. Mammalian subtilisin/kexin isozyme SKI-1: a widely expressed proprotein convertase with a unique cleavage specificity and cellular localization. Proc. Natl. Acad. Sci. U. S. A. 96:1321-1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sevilla, N., E. Domingo, and J. C. de la Torre. 2002. Contribution of LCMV towards deciphering biology of quasispecies in vivo. Curr. Top. Microbiol. Immunol. 263:197-220. [DOI] [PubMed] [Google Scholar]
- 51.Toure, B. B., J. S. Munzer, A. Basak, S. Benjannet, J. Rochemont, C. Lazure, M. Chretien, and N. G. Seidah. 2000. Biosynthesis and enzymatic characterization of human SKI-1/S1P and the processing of its inhibitory prosegment. J. Biol. Chem. 275:2349-2358. [DOI] [PubMed] [Google Scholar]
- 52.Weber, E. L., and M. J. Buchmeier. 1988. Fine mapping of a peptide sequence containing an antigenic site conserved among arenaviruses. Virology 164:30-38. [DOI] [PubMed] [Google Scholar]
- 53.Ye, J., R. B. Rawson, R. Komuro, X. Chen, U. P. Dave, R. Prywes, M. S. Brown, and J. L. Goldstein. 2000. ER stress induces cleavage of membrane-bound ATF6 by the same proteases that process SREBPs. Mol. Cell 6:1355-1364. [DOI] [PubMed] [Google Scholar]