Abstract
The harm produced by tobacco products is a result of frequent use of a highly toxic product. Reducing the adverse public health impact of tobacco products might be most effectively achieved by reducing the likelihood of their use and the toxicity of the products. Products that retain some characteristics of cigarettes, but have been altered with the intention of reducing toxicity have been referred to as modified risk tobacco products or potential reduced exposure products (MRTP/PREPS). Evaluation of their content, emission, and toxicity is discussed in other articles in this special issue. Here, we discuss the methodology that has been used to examine the likelihood of abuse or addiction. Abuse liability assessment (ALA) methodology has been used by the Food and Drug Administration (FDA) and other drug regulatory agencies world-wide for decades to assess the risks posed by a wide variety of pharmacologically active substances. ALA is routinely required among other evaluations of safety during the premarket assessment of new drugs, and is continually adapted to meet the challenges posed by new drug classes and drug formulations. In the 2009 law giving FDA regulation over tobacco products, FDA is now required to evaluate new tobacco products including MRTP/PREPs to determine their risk for abuse and toxicity at the population level. This paper describes the traditional tools and methods of ALA that can be used to evaluate new tobacco and nicotine products including MRTP/PREPs. Such ALA data could contribute to the scientific foundation on which future public policy decisions are based.
Keywords: MRTP, PREP, nicotine, cigarette, addiction, abuse liability
Introduction
It has long been understood that the harm associated with tobacco use is related to the level and duration of toxicant exposure, commonly expressed as cigarettes smoked per day and years of smoking (1–3). It has also been acknowledged that reduced risk of disease can be achieved by the complete substitution of less harmful products (e.g., medicinal nicotine) for cigarettes or for other harmful tobacco products. However, there is concern that the population benefit of products with reduced toxicity might be diluted or completely negated if those products were to be used at higher rates than cigarettes due either to their inherent likelihood of abuse and dependence or to marketing efforts by manufacturers (3–7)..
These public health concerns associated with tobacco products are amenable to evaluation within an established framework for abuse liability assessment (ALA) that has been used by the Food and Drug Administration (FDA) and other drug regulatory agencies world-wide for decades to assess the risk posed by a wide variety of drugs and drug products. Moreover, the need for the comprehensive ALA of tobacco and nicotine products has been recently codified within the Family Smoking Prevention and Tobacco Control Act of the 111th Congress (8). This law gave the FDA broad authority to regulate tobacco products to achieve the ultimate goals of preventing tobacco use and promoting cessation, with issues of “particular concern to public health officials” including “the use of tobacco by young people and dependence upon tobacco” (8, Section 3). New products and modified risk tobacco products must henceforth be evaluated and approved before they may be marketed. Such evaluations of new (and existing) products will include the likelihood of their persistent use in addition to their predicted toxicity and harmful consequences (8, Sections 910 and 911).
Fortunately, traditional ALA methodologies, developed for assessing risk of drug abuse and dependence, provide an extensively researched and applied approach whose strengths and limitations have been well-documented (9–13). ALA includes a broad range of specific tests that can provide a scientifically validated basis for predicting the likelihood that a new product will be abused or cause dependence (also known as “addiction”) (9–13). In fact, ALA was used to provide key data relied upon by the National Institute on Drug Abuse and US Surgeon General in the 1980s and later by the FDA in their determinations that cigarettes met objective criteria as addictive drugs (14–18). The ALA of drugs used to treat tobacco dependence has also been critical in their approval, labeling, and approach to their regulation (16, 17; Chantix labeling).
ALA is both strengthened and complicated by the fact that there are many potential tests for abuse liability that can be applied depending on the stage of development of a product, the specific questions of interest, including the intent of the product's sponsor (or manufacturer) for its marketing approach and potential claims (e.g., “reduced risk”). There are also a wide variety of potential regulatory implications including product communications, warnings, and labeling that will be considered by FDA in the United States, by regulatory agencies outside of the United States, and by the World Health Organization (WHO) in its assistance to member states which have ratified the WHO Framework Convention on Tobacco Control (FCTC) as delineated in Articles 9–11 (19, 20).
Components Associated with Abuse Liability of Tobacco Products
ALA involves determination of both the likelihood that individuals will engage in persistent or problematic use (e.g., become addicted to) a drug and the likelihood that individuals will experience undesirable consequences as a result of its use (e.g., adverse medical or psychological effects, impaired psychomotor or cognitive performance effects, physical dependence; (12, 21). The likelihood that the self-administration of a drug will result in persistent use or abuse is associated with its psychoactive or central nervous system effects, which can result in both positive and negative subjective effects; its reinforcing effects; and with tolerance, craving, and withdrawal that can result after repeated use of the drug (14). Complicating ALA is that the abuse liability of a drug also depends on its pharmacokinetics; that is, the speed of drug delivery and absorption, the dose(s) delivered, and the rate of clearance of the drug. A greater likelihood of abuse is associated with faster speed of drug delivery, greater amount of drug absorption, or faster clearance of a drug (22–27). Thus, smaller doses of more rapidly delivered nicotine might produce stronger addictive effects, referred to in some tobacco industry documents as “kick” (16, 17, 28–30). Adverse effects from a drug also play a critical role in abuse liability (31). For example, the occurrence of undesirable side effects such as nausea can lower the likelihood of abuse, whereas other undesirable side effects such as cancer increase the liability or adverse consequences associated with using a drug or drug product.
Most research on tobacco addiction has primarily focused on the role of nicotine, which is considered to be the primary tobacco constituent that is responsible for tobacco addiction (3, 14, 32, 33). However, other tobacco ingredients or smoke emissions have been proposed to enhance the reinforcing or rewarding effects of nicotine. Ammonia is a chemical that increases the pH of the product leading to greater available free or un-ionized nicotine, which is more readily absorbed by cells (20, 34–37). Acetaldehyde increases the formation of acetaldehyde-biogenic amine adducts such as harman and salsolinol, which have been shown to have reinforcing effects by themselves and also to enhance the reinforcing effects of nicotine (38). Flavorants such as cocoa, licorice, fruit extracts, or menthol have been suggested to increase the attractiveness of tobacco products and might be particularly appealing to youth (20, 32). Other constituents such as nornicotine, a tobacco alkaloid and metabolite of nicotine (39–41) and inhibitors of monoamine oxidase (an enzyme that inhibits the metabolism of catecholamines) have been suggested to directly contribute to the reinforcing effects of tobacco products (42, 43). The ALA methodology discussed in this article can be used to study the role of different drugs or constituents alone or in combination, and has been used by Philip Morris to do precisely that (29, 44).
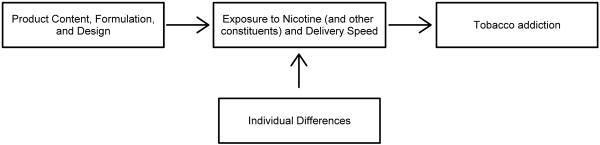
The formulation and design of a product can also contribute to its abuse liability (20, 36). For example, products that are inhaled into the lungs are associated with faster rate of absorption than products that are used orally and tend to have greater abuse liability (22). Ventilated filters can potentially enhance the abuse liability of a product by facilitating the deep inhalation of nicotine and increasing the administration of free or un-ionized nicotine (45–47), and by facilitating compensatory smoking (48). The size of the cut tobacco leaves can also influence the amount of nicotine that is delivered by the products (3, 20, 36). In addition, the abuse liability of a drug can also be affected by individual differences in response to the drug, such as the differences in the rate of drug (e.g., nicotine) metabolism (49–52). Figure 1 depicts the relationship between product content, formulation and design, which influences the speed and amount of exposure to nicotine overall or nicotine in an un-ionized form in particular, which as described above is more readily absorbed. The speed and amount of exposure to nicotine and other constituents that are associated with tobacco's reinforcing effects will contribute to the risk for tobacco addiction.
Figure 1.
Factors that contribute to the risk of addiction to tobacco products
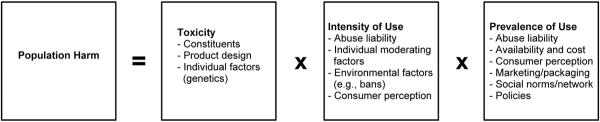
As noted previously, abuse liability as traditionally measured in the human and non-human laboratories focuses primarily on the drug or product itself. However, actual abuse of a drug or drug product is also influenced by contextual, environmental, economic, and social factors (14, 53). For example, in addition to the abuse liability of a drug or product, actual abuse can be affected by the ease with which drug can be extracted from the product, drug availability (e.g., ease of purchase, drug price), pleasurable sensory effects (e.g., sight, smell, taste, and mouth feel), marketing or promotion, labeling, packaging, beliefs and expectations about the utility of or harms associated with the drug, and the extent of social acceptance and use of the drug (e.g., the extent of bans against the drug, peer drug use). These factors are typically not examined in traditional ALA, but have been discussed with respect to tobacco products by the World Health Organization's Study Group on Tobacco Product Regulation (TobReg). Abuse liability, although a critical area for potential reduced exposure product (MRTP/PREP) assessment, is only one component necessary for evaluating potential effects of a MRTP/PREP on public health. Figure 2 shows the various factors that contribute to the impact of a tobacco product on population harm (e.g., tobacco-related morbidity or mortality for the population as a whole) and extends the traditional concepts and methods associated with abuse liability to include actual abuse, dependence, and harm. Abuse liability will affect how much of the drug is used (and therefore, the extent of tobacco-related toxicant exposure) and the rate or prevalence of drug use (and therefore, the extent of population exposure). The extent of toxicant exposure and the prevalence of drug use have a significant impact on the individual and population harms associated with the drug. For example, the high abuse liability of cigarettes most often leads to daily cigarette use and contributes to the persistence in smoking, which subsequently leads to prolonged exposure to tobacco toxicants and tobacco-related morbidity and mortality. Thus, the high abuse liability of cigarettes has resulted in over 1.3 billion smokers and several million users of oral tobacco products world-wide (54), which in turn will lead to approximately 6 million deaths per year by 2010 (55, 56).
Figure 2.
Components to assess population harm
The determination of what is an acceptable level of abuse liability for a MRTP/PREP is likely to rest largely on the toxicant profile of the PREP. For example, if a PREP has a significantly reduced toxicant level compared to a conventional product (e.g., medicinal nicotine products compared to cigarettes), then public health might benefit even if the product has likelihood for use or abuse. On the other hand, the availability of a product with likelihood for abuse might lead to a greater number of consumers who sustain their addiction to nicotine or individuals who will initiate use of the new product. These issues are critical, but require a considerable amount of thought and policy analysis which are beyond the scope of this paper.
To date, there are a number of different types of products that could be considered MRTP/PREPs including low nicotine yield cigarettes (e.g., Quest, 22nd Century Limited), smokeless tobacco (e.g., Marlboro Snus, Altria Group, Inc.; Camel Snus, RJ Reynolds Tobacco Co.), compressed dissolving tobacco powder (e.g., Camel Orbs; R.J. Reynolds Tobacco Co.), and nicotine vaporization devices (e.g., Ruyan, N-Joy, Crown 7; various manufacturers). Given the diversity of materials, formulations, and methods of use across these products, it is important to understand how different characteristics such as the dose of nicotine delivered, the pharmacokinetics of nicotine delivery, and non-pharmacological factors such as taste and other sensory aspects, affect different products' liability for and of abuse (26, 57). Menthol and other scents and flavorings (e.g., spice) can serve as robust sensory stimuli that can become conditioned reinforcers when paired with nicotine. Nicotine itself has noxious organoleptic properties, that can be masked by other ingredients in the tobacco product to make tobacco use more pleasurable and more likely to lead to addiction (16, 17, 20, 28). Thus, it is not surprising that companies manufacturing MRTP/PREPs are applying various techniques to increase the palatability of their products. For example, multi-modal sensory stimuli are associated with a brand of dissolvable compressed powder tobacco called “frost”. These stimuli consist of a mint flavor, mint odor, tingling sensation at the site of application (upper lip), and cold temperature, the latter if used shortly after purchase from one of the company's branded refrigerated cases (Camel Snus Advertisement; R.J. Reynolds Tobacco Co.). The contribution and interaction of these various factors to the abuse liability of a MRTP/PREP presents challenges to the existing methods for assessing abuse liability.
The goal of this paper is to provide an overview of established methods and measures used to assess the abuse liability of drugs that can be applied to tobacco products in general (for example, to assist FDA in its development of product performance standards described in section 907 of the authorizing legislation), as well as new tobacco products (described in section 910), and MRTP/PREPs (as described in sections 910 and 911 (8). This paper is not intended to serve as a comprehensive review or meta-analysis of all abuse liability studies, but rather to provide guidance regarding the current and future ALA of MRTP/PREPs based upon the current best practices in ALA, as they are applied to illicit drugs and pharmaceutical products. The studies cited within this review have been included as illustrative examples of the methodology that is described in several extensive reviews of laboratory ALA methodology (12, 21, 58, 59). All of these methods have previously been used to assess the abuse liability of cigarettes, and many formulations of nicotine including FDA approved pharmaceuticals, as has been reviewed elsewhere (10, 14, 60, 61).
Other reviews have addressed the assessment of abuse and misuse in the clinical setting (62–64) and the role of formulations in ALA (11, 65, 66). A review of studies that have specifically examined the abuse liability of MRTP/PREPs is described in an accompanying paper in this issue Clinical Methods and Measures for the Assessment of PREPs (67). The present paper will also identify current research gaps and recommend directions for future research.
Measurement of the abuse liability of a product
Over the last several decades, well-validated methodologies for assessing the likelihood/severity of abuse and likelihood/severity of the consequences of abuse in human subjects in a laboratory setting have been developed (10, 12, 21, 58, 68–70). These methods, each of which will be discussed in more detail in subsequent sections, include 1) drug discrimination, 2) acute dose-effect comparisons, 3) suppression of withdrawal and craving), 4) self-administration (including the determination of progressive ratio breakpoints) and 5) choice procedures. These laboratory procedures have been shown to have good internal validity and predictive validity. That is, drugs that are liked and self-administered by human recreational drug users in the laboratory tend to be used and abused recreationally outside of the laboratory setting (59, 69, 71). We also will discuss some methods such as brain imaging procedures that are less well-established for ALA, but might be useful for examining potential mechanisms of action within functional brain areas. Finally, we will describe some of the highly useful information about abuse liability that can be derived from clinical trials and post-marketing surveillance.
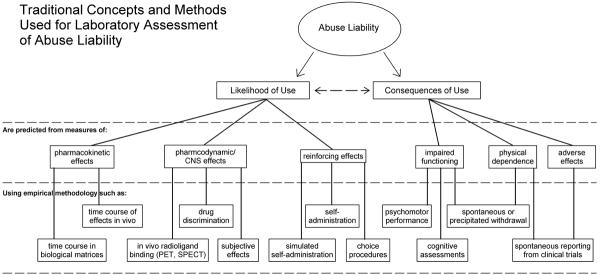
Figure 3 shows the various areas of ALA and the models or methods that have been used to undertake these assessments. In this figure two broad areas of abuse liability are measured: likelihood of abuse and consequence of abuse. The likelihood of abuse can be determined by examining the pharmacokinetic effects of a drug, the pharmacodynamics and CNS effects, and the reinforcing effects. ALA in each of these areas can be conducted by acute dosing studies (pharmacokinetics and pharmacodynamics); drug discrimination studies (pharmacodynamics); brain imaging (CNS effects) studies; and drug self-administration studies including the analysis of progressive ratio breakpoints, behavioral economic functions, and preferences or forced-choice trials. Consequences of excessive use of an abusable product might include impaired cognitive function, the development of physical dependence, and other adverse effects from the drug. These negative consequences can be assessed in acute dosing studies, clinical trials, and post-marketing surveillance.
Figure 3.
Traditional concepts and methods used for laboratory assessment of abuse liability.
Table 1 provides a summary of these various methods and models that have been used to assess the abuse liability of illicit drugs and pharmaceutical products. Each of the following sections will describe how these methods have been adapted to examine the abuse liability of a variant of nicotine delivery product, including conventional tobacco cigarettes.
Table 1.
Methods for Abuse Liability Assessment
| Model | Goal(s) of the Model | Methods | Outcome Measures | Subject Characteristics |
|---|---|---|---|---|
| Drug Discrimination | To determine if a drug or product has similar discriminative stimulus effects (and by implication, pharmacological effects) as a drug or product with known pharmacology. Similar pharmacological effects suggest that drugs might have similar abuse liability. | Within subjects (crossover) design in which individuals are first trained to discriminate between two or more drugs or conditions (e.g., placebo, drug A, and drug B). Training involves the differential reinforcement of responses that indicate a correct identification of the condition. Testing involves administration of training conditions or novel conditions (i.e., drugs or doses) and all responding is either reinforced or not reinforced (i.e., there are no "correct" answers under test conditions). | The primary outcome measure is percentage of responses or the percentage of choices on the option that has been paired with drug during training (i.e., drugappropriate responding). Physiological measures can be used to ensure that pharmacologically active doses of drug were studied. Subjective effects measures can be used to examine how individuals were able to discriminate between drugs or placebo. | Never users of tobacco, former users, occasional users, regular or dependent users. An N of 10–20 participants is common. |
| Acute Dose-Effect Comparison Study | To determine if a drug or product results in greater positive subjective effects, ratings of liking, or willingness to pay for the drug or take the drug again at doses or levels of use that produce similar physiological or behavioral effects as a positive control. Greater positive subjective effects (likelihood of use) and greater impairment (consequences of use) suggest greater abuse liability. | Within subjects, double-blind administration of placebo and several doses of the test drug or product and a positive control are studied across the time course of the drugs. A range of measures are collected repeatedly throughout the time course and retrospective ratings of the drug effects are often collected as well. | The primary outcome measures are typically subjective reports of liking, good effects, and willingness to take the drug again. Physiological (e.g., heart rate, blood pressure, pupil diameter, skin temperature), subjective (e.g., lightheaded, anxious, drowsy), and cognitive/behavioral measures (attention, working memory) are also typically included. Retrospective measures of liking, willingness to take the drug again, or indifference points from the Multiple Choice Procedure are often used as proxies for reinforcing effects. | Regular or dependent users of tobacco are typically recruited. Never, former, or occasional users could be included using a prequalifying session that confirms a positive response to a positive control. An N of 10–15 participants is common; however, 20–40 participants might be necessary for making comparisons between similar drugs or drug products. |
| Suppression of Withdrawal and Craving | To determine if a drug or product can prevent or reverse the effects of abstinence in nicotine-dependent individuals. Suppression of craving or withdrawal suggests abuse liability in individuals who are physically dependent. | Within subjects design in which one or more products, often including participants' regular brand of cigarettes, are used after a period of abstinence from smoking. A range of measures are taken at baseline after a (typically overnight) period of abstinence and changes in those measures are examined after smoking one's regular brand of cigarettes, denicotinized cigarettes, or a PREP. | The primary outcome measures are typically subjective reports of withdrawal symptoms (e.g., irritability, anxiety, difficulty concentrating) that are assessed via visual analog scales or questionnaires such as the Minnesota Nicotine Withdrawal Scale or the Questionnaire of Smoking Urges. Smoking abstinence is typically confirmed by breath CO. Changes in other physiological measures (e.g., heart rate, skin temperature) are also often assessed as signs of withdrawal. | Regular or dependent users of tobacco are typically recruited to ensure that withdrawal signs and symptoms will occur upon discontinuation of smoking. An N of 10–30 participants is common. |
| Drug Self-administration | To determine if the drug or product maintains a rate of self-administration behavior higher than placebo and comparable to a positive control. A rate of self-administration greater than control suggests abuse liability. | Within subjects design in which nicotine, a cigarette or puff from a cigarette (often including participants' preferred brand), or a PREP is made available after a period of abstinence from smoking. Subsequent smoking behavior or use of a PREP is examined over a period of a day to weeks in the laboratory or over weeks to months of outpatient use. | The primary outcome measures in laboratory studies typically include the rate of responding for nicotine or puffs of cigarettes, the number of puffs taken from a cigarette(s), or the number of cigarettes smoked. Laboratory studies can also include measures of smoking topography such as puff duration, puff volume, and inter-puff interval. Progressive ratio studies report breakpoints, or the highest ratio as which drug was self-administered. | Occasional, regular or dependent users of a product similar to the novel product being studied (i.e., smokers or oral tobacco users). An N of 10–20 participants is common. |
| Behavioral Economics/Cigarette Purchase Task | To determine how much of a drug or product is consumed at different prices to compare the elasticity or sensitivity of changes in consumption relative to changes in price across different drugs or products. Consumption that is less sensitive to increases in price suggests greater abuse liability. | Within subjects design in which participants who are familiar with the drug or product are asked to report how much of the drug or product they would consume at different prices. The examination of novel products would presumably require a sampling phase as described below in the forced-choice procedures. | The primary outcome measure is the amount of consumption across different prices, which is used to generate a demand curve. Demand curves can be used to compare the relative reinforcing effects of drugs or products to each other when available alone and in the face of other concurrently available reinforcers (e.g., money). | Occasional, regular or dependent users of tobacco. An N of 20–50 participants is common. |
| Forced-choice Procedures | To determine if one drug or product is preferred over another. Preference for one drug or product over another suggests greater abuse liability. | Within subjects design in which participants complete a sampling phase in which they self-administer each of the drugs or products. The sampling phase is followed by a “forced” choice phase in which participants choose to receive one of the conditions previously sampled again. | The primary outcome measure is typically the participants' preference or number or percent of choices made for one product over another. | Occasional, regular or dependent users of a product similar to the novel products being studied. An N of 10–40 participants is common. |
| Clinical Trials | To determine escalation in product use, misuse of products (e.g., use with other tobacco products), negative health outcomes and withdrawal symptoms. Escalation of dose or greater rates of misuse (likelihood of use) or adverse events (consequences of use) suggest greater abuse liability. | Phase I trials are typically dose-response trials. Phase II and III trials are longer trials that may involve a crossover design (i.e., switching from one's usual brand of cigarettes to a PREP) including a control group (e.g., no smoking with or without medicinal nicotine, usual brand of tobacco). | Primary outcome measures for Phase I trials include adverse events and acute product effects. Primary outcome measures related to abuse liability for Phase II and III trials include amount of product self-administration, misuse (escalating product use, use with other tobacco products), and withdrawal symptoms upon discontinuation of use. | Phase I trials can involve occasional, regular or dependent users of tobacco. An N of 10–20 participants is common. Phase II and III trials involve regular or dependent users of tobacco. An N of 10–20 in each condition is common in short-term trials and N of 50– 400 in each condition is common in longer-term trials, with most medication trials having Ns of 100 to 300 per condition. Few longer-term trials with PREPs exceeded 75 per condition. |
| Post-marketing surveillance | To determine the rate and extent of use, initiation of use (uptake) of the product, adverse events including health outcomes and misuse. Greater rates of use or misuse and adverse events (consequences of use) suggest greater abuse liability. | Post-market studies typically involve targeting users of the product of interest and surveying or monitoring their use- and health-related measures using questionnaires and potentially biological samples. Surveillance involves national surveys and random sampling of the general population. | Primary outcome measures for post-market and surveillance studies relevant to abuse liability typically include adverse events from product use; amount of product use; misuse of product (increasing amount of product use; use product with other tobacco products; use of the product by adolescents, former quitters, and those who were interested in quitting); dependence on the product including difficulty quitting use of the product; and consumer perception. | Never users, occasional, regular, or dependent users of tobacco. An N in the 100s–1000s is common. |
Application of methods for abuse liability assessment to nicotine delivery products
Drug Discrimination
Drug discrimination is a behavioral procedure that is used to determine whether two stimuli (e.g., drugs) can be differentiated from one another and whether novel or untrained stimuli (e.g., another drug) occasion responding in a similar manner as the trained drug(s). The drug discrimination procedure can be used with human and non-human subjects, which gives it broad applicability and generality. Although drug discrimination does not provide a direct measure of the reinforcing effects of a drug, it is a useful behavioral procedure to study the pharmacology of the drugs that are being tested. Drugs that share discriminative stimulus effects are likely to have a common pharmacological mechanism of action and might also have similar reinforcing effects or abuse liability (72). In human drug discrimination studies, data from subjective effects questionnaires can supplement drug discrimination data to provide insight into what effects or features of the drug experience are deemed important for discriminating between different drugs. Human drug discrimination procedures have been used to study a number of classes of abused drugs including nicotine (73).
Drug discrimination procedures involve a period of initial acquisition of differentially reinforced responding on the basis of the administration of a dose of drug (i.e., drug discrimination). For example, participants might be exposed to two conditions (e.g., a dose of drug and placebo) referred to as conditions “A” and “B” and told that they will subsequently receive “A” or “B” and can earn money for correct identification of the condition. Acquisition of the discrimination proceeds with the presentation of the conditions and the differential reinforcement of correct responses until an a priori criterion of accuracy is met or an a priori amount of time or number of acquisition sessions have occurred without meeting the accuracy criterion, in which case the participant is considered to have not learned the discrimination. The acquisition or training period is followed by a period of testing of the training and novel drug conditions. Additional training sessions may be included between or after the test sessions to ensure that stimulus control is intact (i.e., verify that the training conditions are accurately identified under testing conditions; 74). Identification of the conditions may be qualitative (i.e., an all-or-nothing choice between “A” or “B”, that is, is the novel drug more like “A” or “B”) or quantitative, if the participants are allowed to allocate responses among the conditions or provide a rating of confidence in the choice that was made. Under test conditions, participants are reinforced (i.e., paid) independently of their responding because the test conditions can be neither of the training conditions in which case there is no “correct” answer (74).
Smokers and non-smokers can be trained to discriminate doses of nicotine from placebo (73, 75, 76), lending validity to the use of this model testing tobacco products. Given that administration of nicotine before sessions can interfere with the accurate discrimination of nicotine within the procedure (e.g., 77), smokers are typically instructed to maintain abstinence from smoking overnight, which can be verified by breath levels of carbon monoxide (CO) the following day (75). Even when smokers maintain overnight abstinence, they tend to be somewhat less sensitive than non-smokers to the discriminative stimulus and subjective effects of the same doses of nicotine, suggesting that they are somewhat tolerant to the discriminative stimulus effects of nicotine (75). However, smokers and non-smokers have been shown to be able to discriminate the same lowest “threshold” dose of nicotine from placebo (76), and when smokers and non-smokers were trained to discriminate progressively lower doses of nicotine, the nicotine dose effect curve shifted leftward in both groups of individuals (78). Together, these results suggest that smokers and non-smokers are able to discriminate between placebo and a range of doses of nicotine. Although smokers (as would be expected) exhibit tolerance to the effects of nicotine, they are able to discriminate (low) doses of nicotine that are discriminable by non-smokers.
Intra-nasal drug delivery is one of the most useful routes for ALA involving nicotine and the route that has been used in many human studies examining the effects of nicotine on cognition, performance, and abuse potential (e.g., 14, 24). This is the same route used to deliver dry powdered snuff tobacco as well as one of the marketed nicotine replacement medicines. The advantage of dosing with an intranasal spray is that it allows for accurate dosing on a per body weight basis and produces subjective and physiological effects with a similar pharmacokinetic profile as tobacco smoke. The novelty of the route (to smokers) avoids conditioned reinforcing effects of non-drug stimuli associated with smoking, and allows for the administration of nicotine to non-smokers that are unable or unwilling to inhale tobacco smoke for the purpose of a research study (75, 79). Smokers and non-smokers can reliably discriminate doses of intranasal nicotine from 2–20 μg/kg (75, 76, 80). For the purpose of ALA, drug discrimination is a very useful procedure for studying the pharmacological mechanisms of drug action. Nicotine binds to nicotinic acetylcholine (nACh) receptors, which are thought to be primarily responsible for the discriminative stimulus and reinforcing effects of nicotine (81, 82). Studies have shown mecamylamine, a non-competitive antagonist at central and peripheral nACh receptors, attenuates the discriminative stimulus effects and subjective effects of nicotine in humans (78, 83). In contrast, the peripheral nACh receptor antagonist trimethaphan did not attenuate the discriminative stimulus effects of nicotine in a different human drug discrimination study, suggesting that the discriminative stimulus effects of nicotine in humans are mediated by central nACh receptors (78).
With regard to the testing of MRTP/PREPs or other tobacco products, drug discrimination testing can be used to identify the threshold dose for the detection of nicotine and to study factors that might moderate this threshold (e.g., age, sex, degree of dependence). This type of study may be important when examining products that are aimed at reducing the prevalence of tobacco use (e.g., reduced nicotine cigarettes or MRTP/PREPs). In addition drug discrimination can be used to examine products that produce nicotine-like discriminative stimulus or pharmacological effects (e.g., nicotine analogues) and therefore may substitute for nicotine, the public health effects of which would depend on the consequences of use associated with the product (i.e., cigarettes and medicinal nicotine produce nicotine-like discriminative stimulus effects, but have different consequences of use and therefore different effects on public health). This method of testing can also be used to determine whether constituents of tobacco produce discriminative stimulus effects similar to those of nicotine (which would suggest a common mechanism of action). Such testing might be useful to not only better understand the effects of the many individual constituents of tobacco but also tobacco smoke as well as interactions among constituents. For example, if a constituent suspected to contribute to abuse liability is found to be discriminable over a wide range of plausible doses, and alters the dose response function for nicotine by increasing the apparent potency of nicotine (e.g., shifting the dose response function to the left), or increasing the functional strength of nicotine (e.g., increasing the magnitude of nicotine's effects), then this would suggest an effect of increasing abuse liability. Such data would also be useful in the next stage of abuse liability assessment, which might include studies of reinforcing effects in non-human and/or human studies and assessment of the nature of the subjective responses of humans.
Acute Dose-Effect Comparison Studies
The most widely used procedure for assessing the relative abuse liability of drugs across drug classes is the acute dose-effect comparison study. Most of the acute dose-effect studies that have examined the abuse liability of different classes of drugs have employed a similar experimental design, which includes within-subject, double-blind, placebo-controlled administration of several doses of drugs, including large or supratherapeutic doses, to recreational drug users (58). In these studies, drug concentrations (pharmacokinetics), physiological, psychomotor, subjective, and cognitive (e.g., memory, attention) effects of a range of doses are characterized over the complete time course of the drug (12). Retrospective end-of-day or next-day questionnaires are also often used to provide an assessment of the entire (previously experienced) drug effect under conditions in which the drug has not been administered.
A sample size of 10–15 participants has typically provided enough statistical power for comparisons between placebo and novel drug conditions in previous abuse liability studies (24, 84, 85); however, sample sizes of 20–40 participants might be necessary for making additional comparisons between different dose conditions and specifically for the evaluation of MRTP/PREPs, which are likely to differ from positive and negative controls (and each other) in more subtle ways than existing tobacco products (59, 86). The participant population selected for an abuse liability evaluation must be one in which the positive control comparison drug (drug with high abuse liability) or product (e.g., cigarettes) will test unequivocally positive. DSM-IV criteria for abuse or dependence (i.e., addiction) are often used to identify appropriate volunteers; however, unlike the users of illicit drugs, users of nicotine/tobacco products might be less likely to satisfy some of the DSM-IV criteria for substance abuse (e.g., to have substance-related legal problems, fail to fulfill a major role obligation; (87). Therefore, criteria for inclusion of smokers in abuse liability studies of nicotine or tobacco products have typically included a minimum number of self-reported cigarettes smoked per day (24), a minimum breath CO level (85), a minimum score on the Fagerstrom Test of Nicotine Dependence (86), or a combination thereof.
Participants that currently use nicotine or tobacco provide the most appropriate and face valid population for the ALA of MRTP/PREPs because current users represent the population at greatest risk for becoming dependent upon the novel products and because current users are less likely generate false positive (significant response to the placebo condition) and false negative (lack of response to the positive control condition) results (88, 89). In particular, participants who smoke can use their prior smoking experience as a context from which to provide meaningful ratings of the use of MRTP/PREPs such as low-nicotine yield cigarettes or nicotine vaporization devices in the laboratory (24, 84). Similarly, participants who primarily use smokeless tobacco might be the most appropriate population to evaluate MRTP/PREPs consisting of dissolvable compressed tobacco powder, which is intended to be used in a similar manner as “dip” or other oral smokeless tobacco formulations (26, 90). However, cigarette smokers would also represent a population of interest for such studies given that they have extensive experience with nicotine self-administration and they will likely be the intended population for such products.
In an additional effort to reduce the likelihood of false negative and false positive reports in abuse liability trials, screening or qualifying procedures that identify volunteers who differentially recognize and report the effects of a positive control and placebo condition have been used to further “enrich” the population of volunteers who are allowed to participate in the study (86). Although adult smokers are the most commonly used and most appropriate population for abuse liability testing, there can also be rationale for the assessment of abuse liability in populations that are not typically recruited for abuse liability studies such as adolescent smokers (85) or non-smokers (86) to control for factors such as tolerance or nicotine withdrawal. The rationale for excluding non-smokers on the basis of their lack of smoking experience has been considered weak for trials in which the test conditions do not include products that must be smoked (86). However, careful consideration must be given to introducing nicotine containing products to naïve subjects unless the product being tested is considered a priori to have low abuse liability (e.g., nicotine gum).
Human abuse liability studies typically involve the assessment of several doses of the novel compound or product compared to placebo and several doses of a positive control compound. However, for the evaluation of MRTP/PREPs, very few studies have examined multiple doses and have typically examined different dosing regimens (e.g., specific number of puffs on a cigarette) across study products (67). In most cases, abuse liability evaluations in recreational drug users or in the case of MRTP/PREPs, regular smokers, have been conducted in controlled laboratory settings, which permit rigorous controlled assessment of outcome measures in the context of appropriate medical support while minimizing the risks and confounds of the use of other drugs (67, 91). However, studies in cigarette smokers are also conducted on an outpatient or ambulatory basis, with participants reporting to a clinical pharmacology laboratory and providing a biological specimen (e.g., breath, saliva, urine) for evaluation of CO, cotinine, or nicotine to confirm past use or abstinence from nicotine or tobacco (24, 26, 86). (See 67 for more detailed information of studies conducted with PREPs).
Standard clinical pharmacology methods require that the participant and the staff who interact with the participant remain blind to the specific drug conditions administered on a given session (i.e., double-blind procedures). In addition, a placebo condition is included to control for effects of expectancy or accidental bias. MRTP/PREPs exist and are delivered in a variety of different formulations including lozenge, pouch, sticks, strips, vapor, or smoke, and as such, placebo conditions might vary widely to mimic the non-drug stimuli of the active product under study (e.g., the use of Lifesavers candy as a control lozenge; 85). Given the variety of formulations, constituents, and additives associated with MRTP/PREPs that might alter the availability or delivery of nicotine from different products, it will also be very important to control for (i.e., match) the different amounts of nicotine that are delivered from different products. Ideally, three or four “doses” of each drug or product (e.g., in the case of a MRTP/PREP, varying number of puffs on a cigarette, duration of product use, or number of products used) are studied. Studying a range of doses of both the novel and the comparator drug(s) allows for the comparison of the slopes of the dose effect functions across different measures, which might be important for drawing conclusions regarding abuse liability (92). It is also essential to the validity of an abuse liability trial that a sufficiently high dose of the novel drug or product is tested. With any new drug or product, it must be assumed that some users will not be guided by the recommended instructions or package insert in their selection of doses, frequency, or duration of use (93). Thus, in determining the maximum dose or frequency of the novel drug or product to be tested, the manufacturer's intended use of the product is only marginally relevant (58, 86) and in the case of most tobacco products, irrelevant.
The drug or product used as a positive control should have measurable abuse liability previously established through experimental studies and epidemiological data. For the evaluation of nicotine/tobacco products, cigarettes from a smoker's preferred brand represent a face valid positive control (24). Doses of amphetamine have also been used as positive controls and have been shown to produce dose-related statistically significant increases on primary measures of abuse liability in smokers and non-smokers (85, 86). For example, doses of amphetamine could be particularly useful positive controls for the evaluation of smokeless tobacco products in non-smokers. To the extent that the initiation of use (i.e., uptake) of a MRTP/PREP in non-smokers is of interest, studies designed to examine the abuse liability of smokeless MRTP/PREPs will require smokeless positive controls for comparison. The choice of a positive control can also be particularly important in studies that compare products in which the abuse liability of each product is hypothesized to be minimal (e.g., a study comparing PREPs to each other; 94). A failure to demonstrate that a drug or product that is abused produces significant increases on the primary measures of abuse invalidates the study or study methods.
Physiological measures are often included in abuse liability studies because these measures are objective (e.g., cardiovascular effects, drug or drug metabolite levels in biological samples; 26, 57) and might provide information on the safety of the drug (e.g., changes in blood pressure; 84). Importantly, physiological measures can also be used to determine whether pharmacologically equivalent doses of the test drug/product and the positive control(s) were studied. For example, different types of MRTP/PREPs and different products can deliver different amounts of nicotine (57). When making comparisons regarding ratings of positive drug effects or reversal of negative effects (i.e., craving or withdrawal) it is important to control for the different amounts of nicotine that are delivered. Products that deliver greater amounts of nicotine might be preferred by nicotine-dependent individuals on the basis of this property alone (i.e., dose) and products that deliver lesser amounts of nicotine might be used more frequently or more intensively to obtain greater nicotine self-administration (94). Thus, attention should be paid to standardizing and equating the use of different products in experimental studies to obtain similar levels of nicotine or equivalent effects on another physiological measure (95). This can be done with PREPs, for example, by delivering a different number of “single use doses” of the PREP (e.g., one, two, or three Ariva tablets) to examine the dose-response curve and how this curve compares with other PREP products or conventional tobacco products. Similarly, behavioral and cognitive measures (e.g., reaction time, attention, memory) might be included to provide objective assessments of impairment (due to direct drug effects or effects of nicotine withdrawal), reversal of impairment, or enhancement of function across these measures (96).
Although subjective measures are not a substitute for behavioral measures of reinforcing effects, they are widely used in ALA (e.g., 84, 85). Subjective ratings of drug liking (i.e. asking participants how much they like the drug) have face validity, have been used in most studies of abuse liability, and tend to be one of the most sensitive and reliable measures of likelihood of abuse (58, 59, 97). Other participant ratings that generally co-vary with liking include ratings of good effects, bad effects, degree to which you would like to take the drug again, estimations of the street value of the drug, and estimations of the amount of money the participant would personally be willing to pay for the drug (e.g., 98). In addition to assessing these measures repeatedly over the time course of drug action, the measures are often also assessed retrospectively after the drug effects have dissipated (e.g., in the form of a Next Day Questionnaire, given 24 h after drug administration). Retrospective ratings have the advantage of assessing the overall drug experience, or at least the remembered portion of that experience, under drug-free conditions and are thought to provide valuable indices of the likelihood that an individual, when drug-free, would seek out an opportunity to re-administer the compound.
Of particular importance to the ALA of tobacco products that are smoked or inhaled, sensory stimuli associated with smoking appear to be important for at least some of the positive subjective effects reported after use of those products. Thus, many studies include subjective ratings of measures such as “satisfaction” or “pleasantness” (99). For example, ratings of satisfaction or liking after smoking a denicotinized cigarette were comparable to those after smoking a nicotine-containing cigarette in smokers who had been abstinent overnight (100, 101). Local anesthesia of the mouth and respiratory tract have been shown to decrease the subjective ratings of satisfaction after smoking a cigarette (102) and a number of studies have shown that smoking a denicotinized cigarette can reduce subjective ratings of craving (97, 100, 103). The sensory effects of smoking are likely mediated by nicotinic and non-nicotinic mechanisms (101). The peripheral nicotinic antagonist trimethaphan has been shown to attenuate the sensory effects of smoking and the subjective ratings of the strength and desirability of smoke from smokers preferred brands of cigarettes (101, 104).
To summarize, acute dose-effect comparison studies can be used to compare the effects of MRTP/PREPs to the effects of smokers' usual brand of tobacco product and to denicotinized cigarettes or sham smoking (i.e., placebo), and possibly though less frequently, to other positive controls (e.g., amphetamine). In these studies, a range of doses of the MRTP/PREP (which may take the form of puffs, cigarettes, amount of dip, time in mouth) and of the positive control should be examined so that dose-response curves can be compared. Measures such as the concentration of drug in a biological sample or a physiological or subjective response to the product can be used to equate nicotine dose exposure across different products, providing valuable information about the pharmacological profile of effects of different products (e.g., dose of nicotine delivered per unit such as puff, cigarette, pouch, stick, tablet) with important implications for abuse liability (e.g., greater likelihood of abuse of products that provide higher doses and/or more rapid administration of drug).
Negative reinforcement and suppression of withdrawal and craving
Physical dependence is manifested by time-limited biochemical, physiological, or behavioral changes (i.e., a withdrawal syndrome) that occur upon termination of chronic drug administration. Physical dependence is distinct from the absence of a drug effect (i.e., a return to baseline) and occurs as a result of an organism's acclimation to chronic drug administration. Meta-analyses have shown that irritability, anger, anxiety, depression, difficulty concentrating, impatience, insomnia, and restlessness are reliable withdrawal symptoms that are reported in the days to weeks following cessation of smoking or use of a nicotine-containing product (105, 106). Some studies suggest that other signs and symptoms that have been studied during nicotine discontinuation such as dry mouth, headache, increased heart rate, rash, sweating, and tremor are less reliable measures of nicotine withdrawal (107–110). Other measures such as decreased heart rate and weight gain have been proposed as being somewhat unique to withdrawal from nicotine/tobacco compared to other drugs (111). The Minnesota Nicotine Withdrawal Scale (107) and the Shiffman-Jarvik withdrawal scale (112) are two of the most widely used self-report questionnaires for the assessment of nicotine withdrawal signs and symptoms. The Fagerstrom Test for Nicotine Dependence is also commonly used as a measure of the magnitude of physical dependence to nicotine (113).
Use of a MRTP/PREP could be initiated and maintained through a mechanism of negative reinforcement whereby its use prevents or suppresses signs and symptoms of nicotine withdrawal. Negative reinforcement describes a process by which the avoidance or escape from a stimulus increases the probability that a behavior will occur. In this regard, craving and withdrawal are thought to contribute to the negative reinforcing effects of tobacco products. That is to say that at least some addictive smoking behavior is maintained by the avoidance of withdrawal symptoms. Nicotine replacement (and taper) therapies are founded on this principle. Therefore, the ability to relieve craving or withdrawal (like cigarettes do) might suggest that a product has liability for abuse, but also suggests that the product might allow an individual to switch to from a conventional tobacco product to a PREP, which could be in the interest of public health if the consequences of use of the product that was switched to are low (e.g., like for medicinal nicotine). Indeed several MRTP/PREPs such as Accord™ (a smoking system in which tobacco is heated by an electronic igniter only when puffed), Advance™ (cigarettes made with tobacco that is cured in a way to reduce nitrosamine content), and Ariva™ (compressed oral tobacco tablets) have been evaluated for their ability to suppress withdrawal signs and symptoms in cigarette smokers following overnight abstinence (95, 114, 115). In withdrawal suppression studies 10–30 smokers are typically enrolled and required to maintain abstinent from smoking overnight, which is verified by levels of breath CO and/or urinary cotinine. On days following overnight abstinence, products or doses are examined for their ability to alleviate signs (e.g., changes in heart rate, skin temperature, and psychomotor performance) and symptoms (e.g., changes in subjective effect ratings of irritability or urge to smoke) of withdrawal. Administration of the drug or product might be limited by the device (e.g., eight puff/cigarette limit with Accord) or by the investigator (e.g., a fixed number of Ariva tablets or puffs from a cigarette; 94, 95, 114, 116). Alternatively, suppression of withdrawal may be examined after smoking a cigarette in the laboratory without puff restrictions (115) or after ad lib smoking of cigarettes on an outpatient basis (117). Allowing individuals to smoke freely in the laboratory setting allows for the evaluation of smoking topography including measures of puff volume, puff duration, puff number, and inter-puff interval (115).
Craving is a construct that has typically been described as a subjective desire or urge to use a drug (118, 119) that can be a result of wanting to seek the positive reinforcing effects of a drug or to relieve negative effects such as withdrawal symptoms or stress. The assessment of craving is thought to be important for the evaluation of nicotine/tobacco products because decreases in craving have been reported to be associated with reduced drug use or maintenance of abstinence (120) and increases in craving have been reported to precede relapse to smoking (121–124). Craving has been measured using single and multiple question 100-mm visual analog scales or Likert scales (119, 125). The Tobacco Craving Questionnaire, and more recently, a short from of the Tobacco Craving Questionnaire have been developed to specifically assess craving during abstinence (126). The most widely used scale is the Smoking Urges Questionnaire (118).
In summary, examination of nicotine concentration and behavioral, cognitive, and subjective drug effects, including craving and withdrawal symptoms from cessation of usual brand tobacco products, will help determine the potential for the continued use of a MRTP/PREP or the ease of switching from usual brand tobacco products to a MRTP/PREP. Assessing withdrawal symptoms from a MRTP/PREP is also critical in evaluating its abuse liability, but would likely require prolonged use of a MRTP/PREP and would involve clinical trial-like methodology (see below) or the examination of a population of smokers who are already using the product (99).
Drug self-administration
Subjective reports of drug liking or satisfaction are useful proxy measures of reinforcing effects (and therefore of abuse liability) and generally correlate well with the actual abuse of a drug. Nevertheless, the reinforcing effects of a drug, device, or medication are determined by whether drug taking behavior is sustained at a rate greater than placebo using a drug self-administration procedure. Drug self-administration is a key test of the abuse liability of a drug, device, or medication (69, 70). As with the acute dose-effect comparison abuse liability studies, human self-administration studies involve participants with histories of drug abuse, and typically include participants that are drug dependent (71). For laboratory-based studies of drug self-administration it is important that the positive control drug of abuse (e.g., usual brand cigarettes or smokeless tobacco products) tests unequivocally positive. Thus, current smokers are the most appropriate population for evaluation of the abuse liability of novel nicotine- or tobacco-containing products.
Smokers have been shown to self-administer intravenous (iv) doses of nicotine at rates greater than those of saline (103, 127–130). These studies, which have identified nicotine as the primary reinforcer in tobacco, have typically included 8–16 smokers. Some studies have been conducted on an outpatient basis and have required overnight abstinence from smoking (103); others have been conducted in an inpatient/residential setting and smoking was not allowed only one hour before and during the 3-hour experimental session (128). In each case, participants were allowed to make operant responses (e.g., working on a task) to receive iv doses of nicotine through an indwelling catheter. Self-administration of iv nicotine has been shown to be sensitive to manipulations of dose, response requirement (i.e., number of responses required to obtain a dose of the drug or unit price), and pharmacological antagonism (103, 128).
While predicting self-administration of drugs in the natural environment is the ultimate goal of abuse liability testing, it is nonetheless very useful to study self-administration in a laboratory setting. Although this introduces some artificiality, it allows for control of intake parameters such as the number, volume, and spacing of puffs; and the depth of inhalation (e.g., 68, 131). This amount of experimental control can be particularly important for the study of cigarettes or other smoked products where smoking behaviors can significantly influence the rate and magnitude of nicotine exposure from a cigarette or other nicotine delivery device (94).
Some studies have controlled smoking behavior by instructing participants to take a fixed number of puffs, a fixed puff volume, and/or fixed inter-puff intervals (131, 132). This is useful when asking questions about the relative potential of products to deliver a constituent such as nicotine when equal doses of smoke are inhaled. Studies of the purportedly low toxicant yield cigarettes Advance, for example, have shown that amounts of nicotine that are equal to or greater than those delivered by smokers' preferred brands are ingested after smoking a fixed number of puffs (94, 115). Control of smoke intake behaviors will standardize smoke intake across participants, but precludes the examination of possible changes in smoking behavior (i.e. compensatory smoking) that has been reported with low nicotine containing cigarettes (133–135). One solution is to use a combination of approaches such as limiting the number of puffs and opportunities for smoking (e.g., a fixed 8-puff bout every 30 min), but measuring rather than limiting the volume and duration of puffs taken (116)..
Other studies have examined compensatory smoking behavior by allowing all smoking topography parameters to vary. For example, in a study that compared two different types of MRTP/PREPs (Advance and Eclipse™) to smokers' preferred brands, Advance cigarettes delivered the same amount of nicotine as the smokers' preferred brand, but resulted in less CO exposure. In contrast, the Eclipse product under uncontrolled puffing conditions delivered less nicotine than the smokers' preferred brand, but resulted in increased CO exposure, possibly as a result of greater puff volume, puff duration, and puff frequency (136). In a similar study that compared Eclipse cigarettes to another low nicotine yield brand Accord, the Accord system resulted in less nicotine delivery than Eclipse even though puff volume and puff duration were greater for Accord than for Eclipse. These results suggest that there may be a trade-off with new products between work requirement (i.e. amount of puffing needed to extract constituents) and nicotine delivery that could affect their abuse liability. Specifically, products that require less effort to obtain a similar dose of nicotine might be preferred.
Some studies using MRTP/PREPs involve self-administration procedures without a work requirement and involve ad lib smoking during a specified period of time. For example studies have compared cigarettes with widely divergent nicotine yields (i.e., nicotine delivering versus “denicotinized” cigarettes). Typically, 10–18 participants are instructed to not smoke for several hours (e.g., overnight) before experimental sessions and are then provided access to each of the different yield cigarettes for a stated period of time (e.g. 3 hours). Dependent measures include the number of cigarettes consumed, the amount of tobacco burned, and latency to the first smoking (91, 132). Studies such as these have shown that smokers will continue to use cigarettes that deliver inconsequential amounts of nicotine over a relatively prolonged period of time, demonstrating that the conditioned reinforcing effects of smoking (without substantial nicotine delivery) can maintain this behavior (91). Studies that have allowed ad lib smoking have also demonstrated nicotine satiation when high doses of nicotine are delivered rapidly (puffing every 6 sec) prior to a self-administration opportunity. Under the conditions described above, subsequent cigarette smoking was decreased after participants rapidly smoked nicotine-containing cigarettes compared to having rapidly smoked denicotinized cigarettes (132).
The self-administration study by Donny et al. (91) has shed further light on the reinforcing effects of “denicotinized” cigarettes that deliver very low amounts of nicotine. In that study, participants smoked either nicotine-containing (Quest 0.6 mg) or denicotinized (Quest 0.05 mg) cigarettes for 11 days while living on a residential research unit. The denicotinized cigarettes were rated as less enjoyable than the higher yield cigarettes and their consumption decreased over the course of the study whereas the consumption of the higher yield cigarettes increased over time. These self-administration data suggest that denicotinized cigarettes have lower reinforcing effects and therefore lower abuse liability compared to (higher) nicotine containing cigarettes in regular smokers during a relatively lengthy self-administration protocol. Interestingly, smokers continued to smoke the denicotinized cigarettes (albeit at a lower rate) throughout the 11-day study, highlighting the relatively strong conditioned reinforcing effects of smoking and the relatively lengthy amount of time that might be required to extinguish these effects.
A possible limitation of laboratory-based studies is the relatively short duration over which smoking behavior is examined. Exposure duration might be particularly important for the abuse potential assessment of MRTP/PREPs if there is reason to suspect that compensatory smoking (or increased use) might lead to escalation of use over time (e.g., 135). One solution is to use experimental designs that combine the assessment of outpatient ad lib use and in-laboratory smoking/product use topography, physiological measures, and subjective effects (135, 136). These designs can allow participants to gain “real-world” experience with the product before smoking behavior and self-reported effects are assessed in the laboratory. Further, this in-laboratory and outpatient mixed design might be an especially good way to assess the validity of some laboratory procedures. Given the concerns related to compensatory smoking or the compensatory use of MRTP/PREPs, studies that allow participants to use the products repeatedly and over prolonged periods of time are likely to be important for the assessment of abuse potential.
Progressive ratio procedures
Self-administration studies that use fixed ratio (FR) schedules require the same number of responses to be made (e.g., 10 key presses) for the delivery of each reinforcer (e.g., a single puff from a cigarette). In contrast, progressive ratio (PR) schedules require that each time a reinforcer (e.g., a puff) is earned, a greater number of responses is required to earn the next reinforcer, thus requiring progressively greater effort for the same amount of drug. In human drug self-administration studies, PR schedule response requirements typically start around 50 or 100 responses (e.g., key presses) and can escalate to thousands of responses required for single administration. Generally, participants are allowed to continue to make responses within the confines of a several hour session until they decide to stop. The primary dependent measure is the breakpoint or the highest ratio at which a reinforcer was earned, although other measures such as the number of responses made, the number of ratios completed, or the number of doses earned might also be reported. PR schedules have been most frequently used in the human laboratory to compare the relative reinforcing effects of stimulant and opioid drugs (69, 137, 138). However, self-administration using PR schedules have also been used to study smoking behavior. In the study by Donny et al. (91) breakpoints on the PR schedule were the only measures that showed a pattern of change over time that suggested a gradual and continuing loss of reinforcing effects of the denicotinized cigarettes over time. Thus, PR schedules might be particularly sensitive or useful for comparing the relative reinforcing effects of nicotine containing products.
Behavioral economic procedures
Self-administration studies using FR schedules can vary the amount of effort (i.e., the ratio or number of responses) required for delivery of drug and the amount of drug or product delivered (e.g., number of puffs) at each administration. The behavioral economic approach to self-administration involves systematically varying these experimental parameters to examine the amount of drug that is self-administered across a range of unit prices (effort or cost per amount of drug available; (139, 140). As described above, self-administration studies using PR schedules are designed to determine the ratio or “price” at which a reinforcer is no longer self-administered. However, an important difference between data obtained from PR schedules and data obtained from behavioral economic studies is that the self-administration data from the PR schedule is qualitative in nature (i.e., it is binary, the drug is self-administered at a given ratio or it is not), whereas data obtained from behavioral economic studies are quantitative in that the amount of consumption or self-administration is captured at each unit price. This is an important difference because the behavioral economic approach provides additional information with regard to the sensitivity of self-administration or consumption relative to price; a concept known in economic terms as the elasticity of demand for that product (141).
The analysis of characteristics of the demand curve such as elasticity can be used to directly compare the reinforcing effects of drugs from different classes (e.g., alfentanil, nalbuphine, cocaine, and methohexital; 142) and could also be used to directly compare the reinforcing effects of different types of MRTP/PREPs to one another. However, the examination of self-administration behavior across a range of unit prices typically requires a large number of experimental conditions that could be prohibitively expensive or unrealistic to conduct for the purpose of an abuse liability trial. As a result, procedures to assess the hypothetical purchase or consumption of drugs have been developed to efficiently examine the simulated consumption of drugs. These procedures, often referred to as drug purchase tasks, have been used to assess the hypothetical purchase or consumption of heroin (143), cigarettes, (144), and alcohol (145, 146) and results from these studies have been shown to resemble actual drug use (143) and accurately predict the future consumption of that drug (147). In a cigarette purchase task, for example, participants would be asked “How many cigarettes would you smoke if they were _____ each?” Prices would span a range of values (e.g., $0.01–$1,120) from which a demand curve could be constructed. For the evaluation of MRTP/PREPs, participants would presumably have to sample the new product and could then be asked how many doses or products they would consume at different prices.
Behavioral economic procedures and analyses can be used to determine differences in the demand curves of different MRTP/PREPs. The further development of drug purchase tasks that are specifically designed to compare the demand elasticity for different MRTP/PREPs in nicotine dependent individuals could yield information that is useful for predicting the relative abuse liability, preference, and demand for different products at different (or similar) retail prices (141). Demand is an important measure to consider alongside traditional abuse liability measures of estimated value or worth on the market because two different MRTP/PREPs that have the same estimated market value might be consumed in different quantities thereby reflecting a difference in demand and abuse potential for the two MRTP/PREPs.
In summary, the extent to which a product is self-administered either in a laboratory or natural setting comprises an important aspect of the likelihood of abuse and ALA. Self-administration can be characterized by the number of times a dose is administered, the amount of drug or product that is administered (e.g. cumulative puff volume), or how hard an individual is willing to work for the dose or product (i.e., breakpoint on a PR schedule). In each case, the drug or product being examined is determined to have reinforcing effects if self-administration occurs at rates greater than a placebo control (product not containing nicotine). Thus, the inclusion of a placebo control is necessary for demonstrating reinforcing effects. The inclusion of other positive and negative controls such as different types of cigarettes, medicinal nicotine products, and other combustible or non-combustible MRTP/PREPs can aid in the interpretation of a novel product's relative abuse liability (12). As described above, cigarettes (or tobacco products) of a user's preferred brand represent a face valid positive control; however, additional experimental conditions might be required to mimic and control for characteristics of the formulation (e.g., dissolvable compressed tobacco) under evaluation.
Choice procedures
The increasing development of new MRTP/PREPs of varied formulations will necessitate that abuse liability methodology be able to adequately compare new products to existing products across different drug delivery platforms (11). In fact, the identification of procedures that can validly and reliably compare different drugs and drug formulations is critically important for the evaluation of products and claims that a particular drug product has lower abuse liability compared to another product. Choice procedures can be used to examine participants' preferences for different drugs, doses, or products and can be determined independently of a drug or product's reinforcing effects. For example, formulations of medicinal nicotine or MRTP/PREPs might have relatively weak reinforcing effects (i.e., that they are not self-administered at rates or up to breakpoints much greater than a placebo control); however, they might still be more or less preferred compared to placebo or traditional cigarettes under different conditions (148), which would suggest that “real-world” use of the medicinal product or MRTP/PREP could affect the consumption of nicotine-containing cigarettes or of other MRTP/PREPs.
Choice procedures might be especially well suited to examine preferences for different products including comparing the relative abuse liability of nicotine across different drug delivery platforms (e.g., cigarette, nasal spray, gum; 139, 148, 149). Most choice procedures use behavioral methods in which participants are asked to choose between two options. They may be choosing, for example, between different doses of nicotine to self-administer (129) or between different types of tobacco products or MRTP/PREPs (150, 151). Such studies allow for conclusions to be drawn regarding the relative abuse liability of the drugs or products. Across these choice procedure studies, typically 6–40 smokers complete a “sampling phase,” which may include a single administration of a dose (e.g., 129) or the regular use of a product for a week or more (e.g., 150, 151). Following the sampling phase, participants are asked to choose between the sampled conditions or products, which could also include a placebo condition (e.g., 129) or the smokers' preferred brand of cigarettes (e.g., 151). The preference, number, or percent of choices for a product is most frequently reported as the primary dependent variable.
Although choice procedures have not been used as frequently as other procedures for the comparative assessment of nicotine containing products, their use is recommended in future studies of MRTP/PREPs due to the ability to provide information about discrete product comparisons. Such information may be used to place new products and formulations along a continuum of products from those that have been shown to have very little abuse liability (e.g., medicinal nicotine) to those that are known to have very high abuse liability (e.g., cigarettes). It is also important to note that different products might lie at different places across such a continuum of abuse liability for different populations such as current smokers, ex-smokers, oral tobacco users, never smokers, adolescents, etc.
The Multiple-Choice Procedure is a questionnaire that is commonly used in acute dose effect comparison studies and is comprised of a series of questions that ask whether participants would prefer a dose of drug (that they have experienced in the laboratory) or an amount of money (152, 153). Typically, after making a series of discrete choices between drug and money, one of the choices made is randomly picked and the participant is actually given the chosen alternative (drug or money) at the end of the session. Thus, while this procedure presents choices between drug and money as opposed to choices between different drugs, the monetary value at which money is preferred over drug (i.e., the crossover point) is taken as the participant's valuation of the dose of drug and can be compared across drugs and doses. Moreover, because participants are reminded that one of the choices will be delivered at the end of the session, choices made in the Multiple-Choice Procedure are not strictly hypothetical, while still allowing for relative ease and low cost of administration of the procedure. The Multiple-Choice Procedure has been used to study the abuse liability of doses of iv nicotine (154) and crossover points for iv nicotine have been shown to be sensitive to manipulations such as pre-treatment with transdermal nicotine (155). A variation of the procedure also allows for the assessment of the punishing (i.e., aversive) effects of a drug (i.e., how much money a participant is willing to forfeit so as not to receive the drug again; 156).
In summary, drug choice procedures are used to determine the monetary value of doses and drugs and to assess preferences for doses, drugs, and products relative to one another. Each of these measures can be used to draw inferences regarding the relative abuse liability of different drugs or products. Behavioral economic approaches that examine how demand curves and preferences are affected by the concurrent availability of other products at fixed or variable costs might offer additional “real-world” validity for assessing how the consumption of one product might change when another is made available (139, 149, 157). For example, the demand curves of two different products (e.g., usual brand cigarettes vs. MRTP/PREP, MRTP/PREP vs. medicinal nicotine product) can be compared when the products are offered concurrently (148). Thus, these procedures should prove especially useful for future assessments of new cigarettes and nicotine delivery products.
Brain activity and brain imaging
Studies of brain activity and brain imaging can provide useful information about what areas of the brain are activated and which receptors or neurotransmitter systems are involved in the use and withdrawal from nicotine/tobacco. These techniques are not typically employed for the purposes of ALA per se, but rather to better understand the mechanisms of action of the drugs. This information, thereby provides information relevant to ALA.
Electroencephalography (EEG) is a non-invasive technique that allows for the transcranial recording of neuronal activity. EEG has been shown to be sensitive to the administration of nicotine (158, 159) with an increase in frequency in response to cigarette smoking and a decrease in frequency in response to the smoking of denicotinized cigarettes (160). EEG frequency has also been shown to decrease during nicotine (cigarette) withdrawal; an effect that can be reversed by cigarette smoking (161, 162). Moreover, the effects of nicotine on EEG measures are attenuated by mecamylamine, suggesting that the effects of nicotine on EEG activity are receptor mediated (163). These studies suggest that EEG might serve as a useful measure for evaluating nicotine-mediated responses to MRTP/PREPs.
Magnetic resonance imaging (MRI), proton magnetic resonance spectroscopy 1HMRS), and functional magnetic resonance imaging (fMRI) are non-invasive techniques that utilize strong magnetic fields to examine brain structure, brain chemistry, and brain activity, respectively. Using these tools, activity in specific parts of the brain has been associated with the administration and reinforcing effects of nicotine (164, 165). Radiological techniques such as positron emission tomography (PET) and single photon emission computed tomography (SPECT) are relatively non-invasive methods for examining brain activity via water or energy utilization or receptor binding. Selective nicotinic receptor ligands have been radiolabeled to study the in vivo binding of nicotine to (α4β2) nicotinic receptors in human subjects (166). This receptor subtype is considered to be associated with the reinforcing effects of nicotine (167). Data from these studies have shown that 1 to 2 puffs from a cigarette can result in 50% α4β2 nicotinic receptor occupancy and smoking an entire cigarette can result in greater than 88% receptor occupancy of the same receptors (168). Similar studies have shown that smoking a “denicotinized” or low-nicotine containing cigarette resulted in 26% and 79% occupancy of α4β2 nicotinic receptors, respectively (169). These studies have important implications for the evaluation of MRTP/PREPs because even “denicotinized” or low nicotine containing cigarettes can result in substantial nicotinic receptor occupancy. However, the precise relationship between nicotinic receptor occupancy and reinforcing effects is not clear.
The release of dopamine in some parts of the brain is thought to be important for the reinforcing effects of drugs. PET studies using radiolabeled dopamine receptor ligands such as (11C) raclopride have examined the effects of nicotine administration on in vivo dopamine binding (and by inference, dopamine release) in humans. These studies have shown that nicotine administration and cigarette smoking result in dopamine release in the ventral striatum and nucleus accumbens, effects that are associated with subjective reports of positive mood and are not replicated by smoking a denicotinized cigarette (169). Moreover, genetic studies have shown that smokers with genes associated with low resting dopaminergic tone exhibited greater smoking-induced dopamine release, suggesting that there is a genetic predisposition to the magnitude of the smoking-induced release of dopamine (170). The extent of dopamine release in specific brain regions in response to the use of different MRTP/PREPs could be compared to positive control conditions (i.e., cigarettes).
In summary, brain activity measures and imaging techniques can be used to assess the extent of nicotine exposure across different MRTP/PREPs compared to a positive control such as conventional, usual brand cigarettes or a negative control such as medicinal nicotine products, denicotinized cigarettes, or placebo (i.e., that involves neither nicotine nor smoking). Brain or receptor activity (dopamine or nicotine) that resembles that observed with conventional cigarettes will suggest potentially similar abuse liability. In the future, genetic contributions (such as polymorphisms on genes associated with relevant nicotinic receptor subtypes or specific neurotransmitter receptor or transporter systems) to these drug effects in the brain can also be considered.
Assessment of Abuse Liability in Clinical Trials
The assessment of abuse liability can occur at all stages of clinical trials (12, 63, 68). Typically for the testing of medications, Phase I trials often involve the testing of multiple doses of a drug under close medical supervision, which allows for an initial opportunity to collect data on the potential for abuse in human volunteers outside of a formal abuse liability study, and in some cases, without the potential confounds of a lifelong history of smoking (e.g. among occasional smokers, never users). Phase II and Phase III trials are conducted in individuals with the disease or disorder that the drug is intended to treat (e.g., smokers for smoking cessation therapies). In trials for smoking cessation, participants are typically smokers of at least 10 cigarettes per day for at least a year with Fagerstrom Test for Nicotine Dependence scores at or above a specified level (e.g., 171, 172, 173). Phase II and Phase III trials provide an opportunity to collect information relevant to abuse liability and acceptability of a product in the population that will be most frequently exposed to the product. These trials also tend to involve administration of drug for longer durations of time, which allows for the prospective evaluation of withdrawal signs and symptoms upon discontinuation of use.
For the testing of MRTP/PREPs, many different measures could potentially be incorporated into Phase I-type trials (i.e., acute dosing studies) for which the primary purpose might be to examine the extent of toxicant exposure or adverse effects. Same day and next day measures of drug liking, good effects, bad effects, and the degree to which the participants would like to take the drug again (e.g., to relax, or for pleasurable effects) could be quickly and easily collected in a Phase I-type trial. However, it is important to note that there is a risk of obtaining false negative reports from individuals without histories of nicotine self-administration (e.g., for nicotine replacement products). Thus, care must be taken to distinguish false positive and false negative signals from true positive and true negative signals of abuse liability. This could be done by evaluating a positive control (i.e., drug with known abuse liability). For example, an abuse liability study that examined the abuse liability of the partial nicotinic agonist varenicline in non-smokers included two doses of amphetamine as positive controls (86).
In Phase II and III type trials, medication compliance is monitored in many clinical trials because missing doses can result in decreased estimates of effectiveness; however, the evaluation of medication compliance is also important from an abuse liability perspective because lack of compliance can indicate escalation of dose, diversion of the drug, lack of interest in using the drug, or supplementation of a drug with other drugs or products. Unlike medications, MRTP/PREPs rarely include specifications for the appropriate (frequency and amount of) use in the real world. On the other hand, appropriate use can be clearly specified within the clinical evaluation of MRTP/PREPs (67). Given that Phase II and Phase III trials often involve administration of the drug or product over several weeks, participants can also be given the flexibility to titrate their dose (see 174). Such a design might more closely model the real world use of MRTP/PREPs by consumers and would also allow for the prospective monitoring of dose escalation and possible misuse, that is, in the case of MRTP/PREPs, use with other tobacco products. Participants in a trial with an open titration schedule might be more likely to report increased use of the drug or other early signals of misuse because they could do so without admitting to non-compliance and risk being discontinued from the study. However, care must be taken to document the context and rationale for a patient's titration to larger doses such that titration up for maintenance of a specific level of nicotine is not misinterpreted escalation of use for positive subjective effects.
Phase II and Phase III trials that involve administration of drug over longer periods of time also allow for the study of the possible emergence of withdrawal signs and symptoms upon termination of drug administration. This can be done at the end of a long-term study (172, 173), or might involve a second randomization of patients to different treatment conditions that includes a placebo condition (175). The prospective monitoring of specific signs and symptoms of withdrawal (e.g., items on the Minnesota Nicotine Withdrawal Scale in the case of nicotine replacement therapies or nicotinic agonists or partial agonists) can provide valuable information regarding the relative risks associated with abrupt discontinuation of the drug (175).
As an example of using a Phase III trial to assess abuse liability and dependence potential of nicotine replacement products, West and colleagues (99) compared 4 nicotine replacement therapy products (patch, gum, spray, inhaler) on a comprehensive battery of measures related to abuse liability. Measures included subjective ratings of pleasantness and satisfaction, subjective ratings of dependence while using the product during 12 weeks of treatment, withdrawal symptoms from the product (objective measure of dependence) after 12 weeks of use, and continued use of NRT beyond recommended period of use (behavioral measure of dependence). Although evidence for any abuse liability was minimal across all the products and measures, continued use of the product after 12 weeks of treatment was sufficiently sensitive to differentiate and rank order the products, yielding a rank order of abuse potential that reflected the rate of nicotine delivery from the product. This type of trial with the associated outcome measures can easily be adapted to MRTP/PREPs.
Post-marketing Surveillance
The authorizing legislation for the Food and Drug Administration's new regulatory authority over tobacco products states that the regulations and guidance on the assessment of modified risk tobacco products shall, “establish minimum standards for post market studies, that shall include regular and long-term assessments of health outcomes and mortality, intermediate clinical endpoints, consumer perception of harm reduction and the impact on quitting behavior and new use of tobacco products, as appropriate; and shall establish minimum standards for required post market surveillance, including ongoing assessments of consumer perception.”
Post-marketing surveillance typically involves the collection of data regarding unanticipated and undesired (i.e., adverse) events related to a pharmaceutical product after it has been introduced to the market. For tobacco products, this might include indicators of abuse liability that might not emerge in the controlled environment of clinical trials. Identification of signals of abuse liability is a process of gathering and processing quantitative and qualitative data. Data collection can range from the more passive collection of spontaneous reports of adverse events (AEs) to more active collection methods in which physicians, patients, drug users, state agencies, and national surveys are queried about the occurrence of any AEs, misuse, or abuse (176). Ideally, reports of AEs will include the severity, duration, and relatedness of the AE to the drug or product, however the reality is AE reports are often less than complete.
The Internet is also increasingly used in post-marketing surveillance of drugs for potential abuse (176, 177). Although quantitative estimates of prevalence and rates of abuse are not readily assessed by Internet monitoring, the Internet provides a rich source of qualitative data about modalities of product use, factors that make some product more or less attractive than others, reasons for use, trends, and how products might be tampered with to alter their psychoactive effects (176, 177). Information can also be obtained about perceptions and attitudes about various products. For example, Internet websites and online chat rooms may include warnings about which products to avoid due to risks and which products are believed to be less risky and/or more rewarding. Internet derived signals that are suggestive of greater harm in the intended population of current smokers, or in other populations such as non-smokers or adolescents, would be cause for concern and further investigation. Assessing signals of abuse involves the integration of a number of disparate data sources and should take in to account the frequency and strength of the associations, the consistency of the findings, evidence of clustering, and potential for mitigation, among other factors (176). (See 178 in this issue for more in depth description of tobacco product surveillance methods).
A key question for post-marketing surveillance, then, is how the abuse liability of a MRTP/PREP compares to other current products (e.g., cigarettes and other MRTP/PREPs) in the real world and all the contexts inherent therein. Given that most MRTP/PREPs would contain nicotine, which is known to produce dependence and somatic AEs (e.g., dizziness, nausea), all MRTP/PREPs would be expected to have some abuse liability (likelihood and consequences of abuse). In addition, MRTP/PREPs have potential for accidental or intentional misuse (e.g., 179) and they might also be diverted to children and adolescents. Other concerns involve a return to nicotine use via a MRTP/PREP by individuals who have already quit smoking cigarettes and the continued use of a MRTP/PREP among individuals who were initially interested in quitting all tobacco products. Yet another concern involves questions related to the potential concurrent use of MRTP/PREPs with other tobacco products such as cigarettes or other MRTP/PREPs. Exposure to toxicants and subsequent disease could be greater in individuals who use multiple tobacco or nicotine products concurrently and the known difficultly associated with quitting smoking (together with the relatively unknown difficulty associated with quitting use of different MRTP/PREPs) could increase the likelihood that the concurrent use of multiple products will occur. Assessing abuse potential when several different medications or products are used concurrently, while important from a real world perspective, might require a new level of sophistication in abuse liability testing.
Recommendations for assessing tobacco products including new products and MRTP/PREPs
It appears that that the law authorizing FDA regulation of tobacco gives FDA flexibility to base standards for existing products and claims for new products submitted for consideration as MRTP/PREPs, at least in part on a determination of their addictiveness. ALA data will provide the agency with one important type of scientific evidence for such decision making.
As reviewed in this paper, the methodology for ALA in humans, as listed in Table 1, is well-established. Originally developed for use in testing opioids, sedatives, and stimulants (11, 180), these methods have been successfully applied to gain important information about the abuse potential of cigarettes with altered characteristics (e.g. denicotinized) and other nicotine delivery products including medications and MRTP/PREPs (57, 67, 181). Instead of selecting a single approach to recommend for use in future testing, it is recommended that several approaches be used to gather information about abuse potential (21). As described in the introduction, selection of approaches for tobacco products, as for drug products, will depend in part on the nature of the product, its state in development, and the questions of specific interest by the product sponsor and the FDA. In particular, an ideal testing approach would include subjective effects as assessed in acute dose effect comparison studies as well as drug choice and self-administration measures of the new products in laboratory settings. This recommendation is consistent with FDA draft guidelines for ALA developed in July 1990 that state, “there is no single test or assessment procedure that, in itself, is likely to provide a full and complete characterization (of abuse liability). Rather, the assessment of abuse liability must be based upon review of all available data that concerns the action of the substance, its chemistry, pharmacology, clinical considerations and summary risks attendant to the public health following introduction of the substance to the general population.” Thus, a number of different types of laboratory studies, such as those describe herein, would likely be conducted concurrently or sequentially. Priorities for use of one method over other methods cannot be delineated because of the need for concordant results across assessment methods and because different methods may address unique aspects of abuse liability. As an example, if the goal is to determine the abuse liability of a low toxicant MRTP/PREP (or a medicinal nicotine product) relative to highly toxic conventional cigarettes, testing might include assessment of the pharmacokinetics and pharmacodynamics of the products, the acute dose-response effects of both products to determine how different doses of the product lead to different physiological and subjective responses and how the curves compare against each other, a behavioral economics analysis to determine the ease with which the MRTP/PREP substitutes for conventional cigarette product, and a self-administration trial to determine how hard subjects are willing to work for one product versus another. Other studies might examine the extent to which the product reduces withdrawal symptoms during use of conventional cigarettes. A clinical trial might also be conducted to determine the pattern and extent of product use, the frequency with which other currently available products are used together with the MRTP/PREP (that is, the extent to which substitution occurs), and the potential for the development or reduction of physical dependence as a result of using the product. Depending on the questions posed and results from each of these tests, one can conclude that the product under evaluation has a greater or lesser likelihood of resulting in recurrent or problematic use and a greater or lesser likelihood of resulting in adverse or harmful consequences compared to conventional products and possibly, compared to other MRTP/PREPs.
In spite of the high predictive validity of existing ALA methodology, the actual abuse liability of any product, including MRTP/PREPs, will ultimately depend on the findings from clinical trials and post-marketing surveillance. However, the predictive validity of the procedures for assessing abuse liability described in this review has been clearly established across many other classes of medications. This provides a good degree of certainty that they will also be valid for assessing new nicotine-containing products. Nonetheless, future MRTP/PREP abuse liability trials might involve designs that include both inpatient and outpatient assessment methods (e.g., 90, 115, 136) to further enhance the validity and generalizability of these laboratory-based assessments to “real-world” abuse and addiction.
One area that might be of particular importance to the ALA of MRTP/PREPs is the examination of their abuse liability in different populations. This would include the ALA of MRTP/PREPs in light and heavy smokers, ex-smokers, users of oral tobacco products, and in some cases, never smokers. Moreover, the examination of MRTP/PREPs in different populations might require different experimental designs or controls as described above. Gender differences should be examined in light of previous research that has reported differences between men and women with regard to discriminative stimulus (182, 183) and positive subjective effects (79, 184) of nicotine as well as withdrawal-related distress and craving (114, 185).
Most assessments of abuse liability of medicinal nicotine or tobacco products have been in physically and mentally healthy smokers. Consideration should also be given to the assessment of abuse liability of MRTP/PREPs in smokers with comorbid psychiatric or substance use disorders. There is a relatively high rate of comorbidity between cigarette smoking and psychiatric disorders (e.g., bipolar, schizophrenia, ADHD; (186–189). However, patients with psychiatric diagnoses are often excluded from laboratory studies and clinical trials. It is possible that the abuse liability of new products will differ in these groups of individuals (190) with the potential for greater likelihood of abuse or greater adverse consequences of abuse in some clinical populations as compared to the general population.
An important regulatory challenge for the future will be how to use these methods to go beyond the macro testing of whole products and to parse out the positive subjective effects and reinforcing effects of the complex mixture of chemicals that might be present in new products as well as product design features that might influence their abuse liability. Factors or characteristics of products that might be associated with increased abuse liability include the amount of nicotine contained in the product, the rate of nicotine delivery, the product formulation or design, the ease of extraction of nicotine or other constituents, sensory aspects associated with use of the product (e.g., menthol), and added constituents in the product that influence absorption, pharmacokinetics, and other pharmacological and non-pharmacological factors.
As a final comment, this review has primarily focused on the traditional methods that have been used to test abuse liability of the drugs and various formulations of drugs (11, 180). However, pharmacological abuse liability is not the sole determinant of whether a product will be used and if so whether addiction will develop. Many other factors related to the appeal or attractiveness of the product are important including convenience of purchase, perceptions of risk, and in the case of orally used products, taste, odor, and other organoleptic properties. Some of the factors might interact with pharmacological factors. For example, crack cocaine is not only highly reinforcing, it is also a convenient means of cocaine administration (14, 191).
As described in the introduction, the actual patterns of use and risk of addiction are also likely to be influenced by marketing, packaging, claims, and therefore consumer perception of a MRTP/PREP; the cost of the product relative to other nicotine-containing products, how widely the product is sold, any restrictions on purchase, the use of the product by members of an individual's social network as well as social norms for use, and the ease by which it could used given policies such as bans on smoking or tobacco use. Thus, novel approaches to ALA will need be explored (e.g., 11, 192). In addition, consumer product testing methods, many of which are already used by the tobacco industry (16, 17, 193), will be important to more accurately predict use, abuse, and addiction (20).
Conclusions and Future Research Directions
Assessing the abuse liability of new tobacco and non-tobacco nicotine-containing products including MRTP/PREPs will be essential in order to determine the extent to which the products are likely to be used and abused and the extent to which the sustained use of the products will positively or negatively impact public health. The ALA of different types of products can also potentially determine how various constituents and design features interact to impact abuse liability and which groups or populations might be especially vulnerable to misuse or abuse of the product. Laboratory-based abuse liability methodology for medications or drugs has been well-developed and some of these methods have already been applied to cigarettes and other nicotine containing products. Future challenges will involve adapting these methods to answer a broader array of questions including the following, which have also been raised by the WHO Study Group on Tobacco Product Regulation (6, 20).
How do individual constituents of a product and the potential interactions between constituents, particularly non-nicotine constituents, affect abuse liability?
How do product design features including sensory characteristics and ease of use affect the abuse liability of new products?
How do marketing, packaging, labeling, pricing, and consumer perceptions affect the abuse liability of a product?
How do patterns of use and abuse liability differ in various target populations? These include adolescents (for initiation of use), occasional smokers, regular light smokers, regular heavy smokers, smokers who want to quit, smokers with comorbid health or psychiatric disorders, smokers of different racial/ethnic groups and smokers of lower socioeconomic status.
In order to address these questions, collaboration among scientists with a broad array of expertise is critical (e.g., toxicologists, engineers, neurobiologists, social scientists, behavioral scientists, and individuals in communications and marketing) along with a conceptual framework that describes important predictors of abuse liability and critical areas of investigation for the assessment of abuse liability.
Acknowledgements
We would like to thank Drs. Roland Griffiths, Edward Sellers, and Mark Parascandola for their editorial comments, as well as the thoughtful comments of the reviewers. We also thank Kathy Longley for her valuable contributions.
Supported by National Cancer Institute contract N01-PC-64402 - Laboratory Assessment of Tobacco Use Behavior and Exposure to Toxins Among Users of New Tobacco Products. This article is one in a series of articles on the methods and measures for the evaluation of potential reduced exposure products.
References
- 1.U.S. Department of Health & Human Services . Reducing tobacco use: A report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, Georgia: 2000. [Google Scholar]
- 2.U.S. Department of Health & Human Services . The health consequences of smoking: A report of the Surgeon General. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta, GA: 2004. [Google Scholar]
- 3.Stratton K, Shetty P, Wallace R, Bondurant S, editors. Institute of Medicine. National Academy Press; Washington, DC: 2001. Clearing the Smoke: Assessing the Science Base for Tobacco Harm Reduction. [PubMed] [Google Scholar]
- 4.Hatsukami D, Henningfield J, Kotlyar M. Harm reduction approaches to reducing tobacco-related mortality. Annu Rev Public Health. 2004;25:1–19. doi: 10.1146/annurev.publhealth.25.102802.124406. [DOI] [PubMed] [Google Scholar]
- 5.Bonnie RJ, Stratton K, Wallace RB, editors. Ending the Tobacco Problem: A Blueprint for the Nation. Institute of Medicine, The National Academies Press; Washington, D.C.: 2007. [Google Scholar]
- 6.World Health Organization . The Scientific Basis of Tobacco Product Regulation: Second Report of a WHO Study Group. World Health Organization; Geneva: 2008. Report No.: 978-92-4-120951-9.WHO Technical Report Series, No. 951. [PubMed] [Google Scholar]
- 7.World Health Organization . The Scientific Basis of Tobacco Product Regulation: Report of a WHO Study Group. World Health Organization, Genevap; Geneva: 2007. Technical Report 945. [Google Scholar]
- 8.U.S. Congress . Public Law 111–31; One Hundred Eleventh Congess of the United States of America. U. S. Government Printing Office; Congress US City: 2009. Family Smoking Prevention and Tobacco Control Act. http://frwebgate.access.gpo.gov/cgi-bin/getdoc.cgi?dbname=111_cong_public_laws&docid=f:publ031.111.pdf. [Google Scholar]
- 9.Schuster CR, Henningfield J. Conference on abuse liability assessment of CNS drugs. Drug Alcohol Depend. 2003;70:S1–4. doi: 10.1016/s0376-8716(03)00095-4. [DOI] [PubMed] [Google Scholar]
- 10.Expert Panel Abuse liability assessment of CNS drugs: conclusions, recommendations, and research priorities. Drug Alcohol Depend. 2003;70:S107–14. doi: 10.1016/s0376-8716(03)00103-0. [DOI] [PubMed] [Google Scholar]
- 11.Grudzinskas C, Balster RL, Gorodetzky CW, et al. Impact of formulation on the abuse liability, safety and regulation of medications: the expert panel report. Drug Alcohol Depend. 2006;83(Suppl 1):S77–82. doi: 10.1016/j.drugalcdep.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 12.Carter LP, Griffiths RR. Principles of laboratory assessment of drug abuse liability and implications for clinical development. Drug Alcohol Depend. 2009 doi: 10.1016/j.drugalcdep.2009.04.003. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johanson CE, Balster RL, Henningfield JE, et al. Risk management and post-marketing surveillance for the abuse of medications acting on the central nervous system: Expert Panel Report. Drug Alcohol Depend. 2009 doi: 10.1016/j.drugalcdep.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.U.S. Department of Health & Human Services . A report of the Surgeon General. U.S. Department of Health & Human Services; 1988. The health consequences of smoking: nicotine and addiction. Report No.: DHHS Publication No. (CDC) 88-8406. [Google Scholar]
- 15.U.S. Department of Health and Human Services . The health consequences of using smokeless tobacco: A report of the Advisory Committee to the Surgeon General. U.S. Department of Health and Human Services, Public Health Service; Bethesda, Maryland: 1986. April. Report No.: NIH Publication No. 86-2874. DHHS Publication No. 86-2874. [Google Scholar]
- 16.Food and Drug Administration Regulations restricting the sale and distribution of cigarettes and smokeless tobacco products to protect children and adolescents; proposed reule analysis regarding FDA's jurisdiction over nicotine-containing cigarettes and smokeless tobacco products; notice. Fed Regist. 1995;60:41314–792. [Google Scholar]
- 17.Food and Drug Administration Regulations restricting the sale and distribution of cigarettes and smokeless tobacco to protect children and adolescents; final rule. Fed Regist. 1996;61:44396–5318. [PubMed] [Google Scholar]
- 18.National Institute on Drug Abuse . Drug Abuse and Drug Abuse Research: The First Triennial Report to Congress from the Secretary. U.S. Government Printing Office; Department of Health and Human Services. Washington, D.C.: 1984. [Google Scholar]
- 19.Burns DM, Dybing E, Gray N, et al. Mandated lowering of toxicants in cigarette smoke: a description of the World Health Organization TobReg proposal. Tob Control. 2008;17:132–41. doi: 10.1136/tc.2007.024158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization Scientific Advisory Committee on Tobacco Product Regulation (SACTob) Recommendation on Tobacco Product Ingredients and Emissions. 2003 http://www.who.int/tobacco/sactob/recommendations/en/ingredients_en.pdf.
- 21.Balster RL, Bigelow GE. Guidelines and methodological reviews concerning drug abuse liability assessment. Drug Alcohol Depend. 2003;70:S13–40. doi: 10.1016/s0376-8716(03)00097-8. [DOI] [PubMed] [Google Scholar]
- 22.Henningfield JE, Keenan R. Nicotine delivery kinetics and abuse liability. J Consult Clin Psychol. 1993;61:743–50. doi: 10.1037//0022-006x.61.5.743. [DOI] [PubMed] [Google Scholar]
- 23.Stitzer ML, de Wit H. Abuse liability of nicotine. In: Benowitz NL, Society for Research on Nicotine and Tobacco, editor. Nicotine Safety and Toxicity. Oxford University Press; New York: 1998. pp. 119–31. [Google Scholar]
- 24.Schuh KJ, Schuh LM, Henningfield JE, Stitzer ML. Nicotine nasal spray and vapor inhaler: abuse liability assessment. Psychopharmacology (Berl) 1997;130:352–61. doi: 10.1007/s002130050250. [DOI] [PubMed] [Google Scholar]
- 25.Houtsmuller EJ, Fant RV, Eissenberg TE, Henningfield JE, Stitzer ML. Flavor improvement does not increase abuse liability of nicotine chewing gum. Pharmacol Biochem Behav. 2002;72:559–68. doi: 10.1016/s0091-3057(02)00723-2. [DOI] [PubMed] [Google Scholar]
- 26.Fant RV, Henningfield JE, Nelson RA, Pickworth WB. Pharmacokinetics and pharmacodynamics of moist snuff in humans. Tob Control. 1999;8:387–92. doi: 10.1136/tc.8.4.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Balster RL. Drug abuse potential evaluation in animals. Br J Addict. 1991;86:1549–58. doi: 10.1111/j.1360-0443.1991.tb01747.x. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization . Advancing knowledge on regulating tobacco products (monograph) World Health Organization; Geneva, Switzerland: 2001. [Google Scholar]
- 29.Wayne GF, Connolly GN, Henningfield JE. Assessing internal tobacco industry knowledge of the neurobiology of tobacco dependence. Nicotine Tob Res. 2004;6:927–40. doi: 10.1080/14622200412331324839. [DOI] [PubMed] [Google Scholar]
- 30.Henningfield JE, Rose CA, Zeller M. Tobacco industry litigation position on addiction: continued dependence on past views. Tob Control. 2006;15(Suppl 4):iv27–36. doi: 10.1136/tc.2005.013789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.deWit H, Zacny J. Abuse potentials of nicotine replacement therapies. CNS Drugs. 1995;4:456–68. [Google Scholar]
- 32.Royal College of Physicians . Helping people who can't quit. Royal College of Physicians; London: 2007. Harm reduction in nicotine addiction. [Google Scholar]
- 33.Buchhalter AR, Fant RV, Henningfield JE. Nicotine. In: Sibley DR, Hanin I, Kuhar M, Skolnick P, editors. Handbook of Contemporary Neuropharmacology Hoboken. John Wiley & Sons; N.J.: 2007. pp. 535–66. [Google Scholar]
- 34.Henningfield JE, Pankow J, Garrett B. Ammonia and other chemical base tobacco additives and cigarette nicotine delivery: issues and research needs. Nicotine Tob Res. 2004;6:199–205. doi: 10.1080/1462220042000202472. [DOI] [PubMed] [Google Scholar]
- 35.Chen C, Pankow JF. Gas/particle partitioning of two acid-base active compounds in mainstream tobacco smoke: nicotine and ammonia. J Agric Food Chem. 2009;57:2678–90. doi: 10.1021/jf803018x. [DOI] [PubMed] [Google Scholar]
- 36.Slade J, Henningfield JE. Tobacco product regulation: context and issues. Food Drug Law J. 1998;53:43–74. [PubMed] [Google Scholar]
- 37.Belluzzi JD, Wang R, Leslie FM. Acetaldehyde enhances acquisition of nicotine self-administration in adolescent rats. Neuropsychopharmacology. 2005;30:705–12. doi: 10.1038/sj.npp.1300586. [DOI] [PubMed] [Google Scholar]
- 38.Talhout R, Opperhuizen A, van Amsterdam JG. Role of acetaldehyde in tobacco smoke addiction. Eur Neuropsychopharmacol. 2007;17:627–36. doi: 10.1016/j.euroneuro.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 39.Crooks PA, Dwoskin LP. Contribution of CNS nicotine metabolites to the neuropharmacological effects of nicotine and tobacco smoking. Biochem Pharmacol. 1997;54:743–53. doi: 10.1016/s0006-2952(97)00117-2. [DOI] [PubMed] [Google Scholar]
- 40.Green TA, Phillips SB, Crooks PA, Dwoskin LP, Bardo MT. Nornicotine pretreatment decreases intravenous nicotine self-administration in rats. Psychopharmacology. 2000;152:289–94. doi: 10.1007/s002130000524. [DOI] [PubMed] [Google Scholar]
- 41.Bardo MT, Green TA, Crooks PA, Dwoskin LP. Nornicotine is self-administered intravenously by rats. Psychopharmacology (Berl) 1999;146:290–6. doi: 10.1007/s002130051119. [DOI] [PubMed] [Google Scholar]
- 42.Fowler JS, Logan J, Wang G-J, Volkow ND. Monoamine oxidase and cigarette smoking. Neurotoxicology. 2003;24:75–82. doi: 10.1016/s0161-813x(02)00109-2. [DOI] [PubMed] [Google Scholar]
- 43.Fowler JS, Volkow ND, Wang G-J, et al. Inhibition of monoamine oxidase B in the brains of smokers. Nature. 1996;379:733–6. doi: 10.1038/379733a0. [DOI] [PubMed] [Google Scholar]
- 44.DeNoble VJ, Mele PC. Intravenous nicotine self-administration in rats: effects of mecamylamine, hexamethonium and naloxone. Psychopharmacology. 2006:184. doi: 10.1007/s00213-005-0054-z. [DOI] [PubMed] [Google Scholar]
- 45.Ashley DL, Pankow JF, Tavakoli AD, Watson CH. Approaches, challenges, and experience in assessing free nicotine. Handb Exp Pharmacol. 2009:437–56. doi: 10.1007/978-3-540-69248-5_15. [DOI] [PubMed] [Google Scholar]
- 46.Watson CH, Trommel JS, Ashley DL. Solid-phase microextraction-based approach to determine free-base nicotine in trapped mainstream cigarette smoke total particulate matter. J Agric Food Chem. 2004;52:7240–5. doi: 10.1021/jf049455o. [DOI] [PubMed] [Google Scholar]
- 47.Ferris Wayne G, Connolly GN, Henningfield JE. Brand differences of free-base nicotine delivery in cigarette smoke: the view of the tobacco industry documents. Tob Control. 2006;15:189–98. doi: 10.1136/tc.2005.013805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kozlowski LT, O'Connor RJ. Cigarette filter ventilation is a defective design because of misleading taste, bigger puffs, and blocked vents. Tob Control. 2002;11(Suppl 1):I40–50. doi: 10.1136/tc.11.suppl_1.i40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ho MK, Tyndale RF. Overview of the pharmacogenomics of cigarette smoking. Pharmacogenomics J. 2007;7:81–98. doi: 10.1038/sj.tpj.6500436. [DOI] [PubMed] [Google Scholar]
- 50.Johnstone E, Benowitz N, Cargill A, et al. Determinants of the rate of nicotine metabolism and effects on smoking behavior. Clin Pharmacol Ther. 2006;80:319–30. doi: 10.1016/j.clpt.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 51.Pianezza ML, Sellers EM, Tyndale RF. Nicotine metabolism defect reduces smoking. Nature. 1998:393–750. doi: 10.1038/31623. [DOI] [PubMed] [Google Scholar]
- 52.Malaiyandi V, Sellers EM, Tyndale RF. Implications of CYP2A6 genetic variation for smoking behaviors and nicotine dependence. Clin Pharmacol Ther. 2005;77:145–58. doi: 10.1016/j.clpt.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 53.O'Brien CP. Drug addiction and drug abuse. In: Brunton LL, Lazo JS, Parker KL, editors. Goodman and Gilman's The Pharmacological Basis of Therapeutics. 11th ed. McGraw-Hill; New York: 2006. pp. 607–28. [Google Scholar]
- 54.Guindon GE, Boisclair D. Past, current and future trends in tobacco use. The World Bank; Washington, DC: 2003. http://repositories.cdlib.org/cgi/viewcontent.cgi?article=1118&context=tc. [Google Scholar]
- 55.Shafey O. The tobacco atlas [1 atlas (128 p):] American Cancer Society; Atlanta, Ga: 2009. American Cancer Society. [Google Scholar]
- 56.Hatsukami DK, Parascandola M. Tobacco Harm Reduction. In: Boyle P, Gray N, Henningfield J, Seffrin J, Zatonski W, editors. Tobacco, Science, Policy, and Public Health. Oxford University Press; in press. [Google Scholar]
- 57.Kotlyar M, Mendoza-Baumgart MI, Li ZZ, et al. Nicotine pharmacokinetics and subjective effects of three potential reduced exposure products, moist snuff and nicotine lozenge. Tob Control. 2007;16:138–42. doi: 10.1136/tc.2006.018440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Griffiths RR, Bigelow GE, Ator NA. Principles of initial experimental drug abuse liability assessment in humans. Drug Alcohol Depend. 2003;70:S41–S54. doi: 10.1016/s0376-8716(03)00098-x. [DOI] [PubMed] [Google Scholar]
- 59.Schoedel KA, Sellers EM. Assessing abuse liability during drug development: changing standards and expectations. Clin Pharmacol Ther. 2008;83:622–6. doi: 10.1038/sj.clpt.6100492. [DOI] [PubMed] [Google Scholar]
- 60.Stolerman IP, Jarvis MJ. The scientific case that nicotine is addictive. Psychopharmacology (Berl) 1995;117:2–10. doi: 10.1007/BF02245088. discussion 4–20. [DOI] [PubMed] [Google Scholar]
- 61.Henningfield JE, London ED, Pogun S. Handbook of experimental pharmacology 192. Nicotine psychopharmacology. Preface. Handb Exp Pharmacol. 2009:v–viii. [PubMed] [Google Scholar]
- 62.Arfken CL, Cicero TJ. Postmarketing surveillance for drug abuse. Drug Alcohol Depend. 2003;70:S97–S105. doi: 10.1016/s0376-8716(03)00102-9. [DOI] [PubMed] [Google Scholar]
- 63.Brady KT, Lydiard RB, Brady JV. Assessing abuse liability in clinical trials. Drug Alcohol Depend. 2003;70:S87–95. doi: 10.1016/s0376-8716(03)00101-7. [DOI] [PubMed] [Google Scholar]
- 64.Mansbach RS, Feltner DE, Gold LH, Schnoll SH. Incorporating the assessment of abuse liability into the drug discovery and development process. Drug Alcohol Depend. 2003;70:S73–85. doi: 10.1016/s0376-8716(03)00100-5. [DOI] [PubMed] [Google Scholar]
- 65.McColl SL, Sellers EM. Research design strategies to evaluate the impact of formulations on abuse liability. Drug Alcohol Depend. 2006;83(Suppl 1):S52–62. doi: 10.1016/j.drugalcdep.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 66.Mansbach RS, Moore RA., Jr. Formulation considerations for the development of medications with abuse potential. Drug Alcohol Depend. 2006;83(Suppl 1):S15–22. doi: 10.1016/j.drugalcdep.2005.10.018. [DOI] [PubMed] [Google Scholar]
- 67.Hatsukami DK, Hanson K, Briggs A, et al. Clinical trials methods for evaluation of potential reduced exposure products. Cancer Epidemiol Biomarkers Prev. doi: 10.1158/1055-9965.EPI-09-0654. in submission. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hatsukami DK, Giovino GA, Eissenberg T, Clark PI, Lawrence D, Leischow S. Methods to assess potential reduced exposure products. Nicotine Tob Res. 2005;7:827–44. doi: 10.1080/14622200500266015. [DOI] [PubMed] [Google Scholar]
- 69.Comer SD, Ashworth JB, Foltin RW, Johanson CE, Zacny JP, Walsh SL. The role of human drug self-administration procedures in the development of medications. Drug Alcohol Depend. 2008;96:1–15. doi: 10.1016/j.drugalcdep.2008.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Haney M, Spealman R. Controversies in translational research: drug self-administration. Psychopharmacology (Berl) 2008;199:403–19. doi: 10.1007/s00213-008-1079-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Haney M. Self-administration of cocaine, cannabis and heroin in the human laboratory: benefits and pitfalls. Addict Biol. 2009;14:9–21. doi: 10.1111/j.1369-1600.2008.00121.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Schuster CR, Johanson CE. Relationship between the discriminative stimulus properties and subjective effects of drugs. Psychopharmacol Ser. 1988;4:161–75. doi: 10.1007/978-3-642-73223-2_13. [DOI] [PubMed] [Google Scholar]
- 73.Perkins KA. Discriminative stimulus effects of nicotine in humans. Handb Exp Pharmacol. 2009:369–400. doi: 10.1007/978-3-540-69248-5_13. [DOI] [PubMed] [Google Scholar]
- 74.Bickel WK, Bigelow GE, Preston KL, Liebson IA. Opioid drug discrimination in humans: stability, specificity and relation to self-reported drug effect. J Pharmacol Exp Ther. 1989;251:1053–63. [PubMed] [Google Scholar]
- 75.Perkins KA, Sanders M, D'Amico D, Wilson A. Nicotine discrimination and self-administration in humans as a function of smoking status. Psychopharmacology (Berl) 1997;131:361–70. doi: 10.1007/s002130050304. [DOI] [PubMed] [Google Scholar]
- 76.Perkins KA, Fonte C, Sanders M, Meeker J, Wilson A. Threshold doses for nicotine discrimination in smokers and non-smokers. Psychopharmacology (Berl) 2001;155:163–70. doi: 10.1007/s002130000660. [DOI] [PubMed] [Google Scholar]
- 77.Perkins KA, Fonte C, Meeker J, White W, Wilson A. The discriminative stimulus and reinforcing effects of nicotine in humans following nicotine pretreatment. Behav Pharmacol. 2001;12:35–44. doi: 10.1097/00008877-200102000-00004. [DOI] [PubMed] [Google Scholar]
- 78.Perkins KA, Fonte C, Sanders M, White W, Wilson A. Effects of training dose and two- versus three-choice testing procedure on nicotine discrimination responding in humans. Psychopharmacology (Berl) 1999;145:418–25. doi: 10.1007/s002130051076. [DOI] [PubMed] [Google Scholar]
- 79.Perkins KA, Epstein LH, Grobe JE, Fonte C. Tobacco abstinence, smoking cues, and the reinforcing value of smoking. Pharmacol Biochem Behav. 1994;47:107–12. doi: 10.1016/0091-3057(94)90118-x. [DOI] [PubMed] [Google Scholar]
- 80.Perkins KA, Sanders M, Fonte C, et al. Effects of central and peripheral nicotinic blockade on human nicotine discrimination. Psychopharmacology (Berl) 1999;142:158–64. doi: 10.1007/s002130050875. [DOI] [PubMed] [Google Scholar]
- 81.Rosecrans JA, Villanueva HF. Discriminative stimulus properties of nicotine: mechanisms of transduction. NIDA Res Monogr. 1991:101–16. doi: 10.1037/e496182006-007. [DOI] [PubMed] [Google Scholar]
- 82.Rose JE. Multiple brain pathways and receptors underlying tobacco addiction. Biochem Pharmacol. 2007;74:1263–70. doi: 10.1016/j.bcp.2007.07.039. [DOI] [PubMed] [Google Scholar]
- 83.Rose JE, Sampson A, Levin ED, Henningfield JE. Mecamylamine increases nicotine preference and attenuates nicotine discrimination. Pharmacol Biochem Behav. 1989;32:933–8. doi: 10.1016/0091-3057(89)90061-0. [DOI] [PubMed] [Google Scholar]
- 84.Henningfield JE, Miyasato K, Jasinski DR. Abuse liability and pharmacodynamic characteristics of intravenous and inhaled nicotine. J Pharmacol Exp Ther. 1985;234:1–12. [PubMed] [Google Scholar]
- 85.Houtsmuller EJ, Henningfield JE, Stitzer ML. Subjective effects of the nicotine lozenge: assessment of abuse liability. Psychopharmacology (Berl) 2003;167:20–7. doi: 10.1007/s00213-002-1361-2. [DOI] [PubMed] [Google Scholar]
- 86.McColl SL, Burstein AH, Reeves KR, Billing CB, Jr., Stolar M, Sellers EM. Human abuse liability of the smoking cessation drug varenicline in smokers and nonsmokers. Clin Pharmacol Ther. 2008;83:607–14. doi: 10.1038/sj.clpt.6100510. [DOI] [PubMed] [Google Scholar]
- 87.Hughes JR. Should criteria for drug dependence differ across drugs? Addiction. 2006;101(Suppl 1):134–41. doi: 10.1111/j.1360-0443.2006.01588.x. [DOI] [PubMed] [Google Scholar]
- 88.de Wit H, Griffiths RR. Testing the abuse liability of anxiolytic and hypnotic drugs in humans. Drug Alcohol Depend. 1991;28:83–111. doi: 10.1016/0376-8716(91)90054-3. [DOI] [PubMed] [Google Scholar]
- 89.Griffiths RR, Weerts EM. Benzodiazepine self-administration in humans and laboratory animals--implications for problems of long-term use and abuse. Psychopharmacology (Berl) 1997;134:1–37. doi: 10.1007/s002130050422. [DOI] [PubMed] [Google Scholar]
- 90.Gray JN, Breland AB, Weaver M, Eissenberg T. Potential reduced exposure products (PREPs) for smokeless tobacco users: clinical evaluation methodology. Nicotine Tob Res. 2008;10:1441–8. doi: 10.1080/14622200802323258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Donny EC, Houtsmuller E, Stitzer ML. Smoking in the absence of nicotine: behavioral, subjective and physiological effects over 11 days. Addiction. 2007;102:324–34. doi: 10.1111/j.1360-0443.2006.01670.x. [DOI] [PubMed] [Google Scholar]
- 92.Carter LP, Griffiths RR, Suess PE, Casada JH, Wallace CL, Roache JD. Relative abuse liability of indiplon and triazolam in humans: a comparison of psychomotor, subjective, and cognitive effects. J Pharmacol Exp Ther. 2007;322:749–59. doi: 10.1124/jpet.107.119693. [DOI] [PubMed] [Google Scholar]
- 93.Hughes JR. Dependence potential and abuse liability of nicotine replacement therapies. Biomed Pharmacother. 1989;43:11–7. doi: 10.1016/0753-3322(89)90185-6. [DOI] [PubMed] [Google Scholar]
- 94.Breland AB, Evans SE, Buchhalter AR, Eissenberg T. Acute effects of Advance: a potential reduced exposure product for smokers. Tob Control. 2002;11:376–8. doi: 10.1136/tc.11.4.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Blank MD, Sams C, Weaver MF, Eissenberg T. Nicotine delivery, cardiovascular profile, and subjective effects of an oral tobacco product for smokers. Nicotine Tob Res. 2008;10:417–21. doi: 10.1080/14622200801901880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hatsukami DK, Fletcher L, Morgan S, Keenan R, Amble P. The effects of varying cigarette deprivation duration on cognitive and performance tasks. J Subst Abuse. 1989;1:407–16. [PubMed] [Google Scholar]
- 97.Butschky MF, Bailey D, Henningfield JE, Pickworth WB. Smoking without nicotine delivery decreases withdrawal in 12-hour abstinent smokers. Pharmacol Biochem Behav. 1995;50:91–6. doi: 10.1016/0091-3057(94)00269-o. [DOI] [PubMed] [Google Scholar]
- 98.Sokolowska M, Setnik B, Jones J, Johnson F, Romach M, Sellers E. Validation of assessments for abuse liability trials. College on Problems of Drug Dependence Annual Meeting; San Juan, Puerto Rico. 2008. 2008. [Google Scholar]
- 99.West R, Hajek P, Foulds J, Nilsson F, May S, Meadows A. A comparison of the abuse liability and dependence potential of nicotine patch, gum, spray and inhaler. Psychopharmacology (Berl) 2000;149:198–202. doi: 10.1007/s002130000382. [DOI] [PubMed] [Google Scholar]
- 100.Westman EC, Behm FM, Rose JE. Dissociating the nicotine and airway sensory effects of smoking. Pharmacol Biochem Behav. 1996;53:309–15. doi: 10.1016/0091-3057(95)02027-6. [DOI] [PubMed] [Google Scholar]
- 101.Rose JE. Nicotine and nonnicotine factors in cigarette addiction. Psychopharmacology (Berl) 2006;184:274–85. doi: 10.1007/s00213-005-0250-x. [DOI] [PubMed] [Google Scholar]
- 102.Rose JE, Zinser MC, Tashkin DP, Newcomb R, Ertle A. Subjective response to cigarette smoking following airway anesthetization. Addict Behav. 1984;9:211–5. doi: 10.1016/0306-4603(84)90060-1. [DOI] [PubMed] [Google Scholar]
- 103.Rose JE, Behm FM, Westman EC, Bates JE. Mecamylamine acutely increases human intravenous nicotine self-administration. Pharmacol Biochem Behav. 2003;76:307–13. doi: 10.1016/j.pbb.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 104.Rose JE, Westman EC, Behm FM, Johnson MP, Goldberg JS. Blockade of smoking satisfaction using the peripheral nicotinic antagonist trimethaphan. Pharmacol Biochem Behav. 1999;62:165–72. doi: 10.1016/s0091-3057(98)00153-1. [DOI] [PubMed] [Google Scholar]
- 105.Hughes JR, Higgins ST, Hatsukami D. Effects of abstinence from tobacco: a critical review. In: Kozlowski LT, Annis H, Cappell HD, et al., editors. Research Advances in Alcohol and Drug Problems. Plenum Press; New York: 1990. pp. 317–98. [Google Scholar]
- 106.Hughes JR. Effects of abstinence from tobacco: valid symptoms and time course. Nicotine Tob Res. 2007;9:315–27. doi: 10.1080/14622200701188919. [DOI] [PubMed] [Google Scholar]
- 107.Hughes JR, Hatsukami D. Signs and symptoms of tobacco withdrawal. Arch Gen Psychiatry. 1986;43:289–94. doi: 10.1001/archpsyc.1986.01800030107013. [DOI] [PubMed] [Google Scholar]
- 108.Gross J, Stitzer ML. Nicotine replacement: ten-week effects on tobacco withdrawal symptoms. Psychopharmacology (Berl) 1989;98:334–41. doi: 10.1007/BF00451684. [DOI] [PubMed] [Google Scholar]
- 109.Hughes JR, Hatsukami DK. Errors in using tobacco withdrawal scale. Tob Control. 1998;7:92–3. doi: 10.1136/tc.7.1.92a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ward MM, Swan GE, Jack LM. Self-reported abstinence effects in the first month after smoking cessation. Addict Behav. 2001;26:311–27. doi: 10.1016/s0306-4603(00)00107-6. [DOI] [PubMed] [Google Scholar]
- 111.Hughes JR, Higgins ST, Bickel WK. Nicotine withdrawal versus other drug withdrawal syndromes: similarities and dissimilarities. Addiction. 1994;89:1461–70. doi: 10.1111/j.1360-0443.1994.tb03744.x. [DOI] [PubMed] [Google Scholar]
- 112.Shiffman SM, Jarvik ME. Smoking withdrawal symptoms in two weeks of abstinence. Psychopharmacology (Berl) 1976;50:35–9. doi: 10.1007/BF00634151. [DOI] [PubMed] [Google Scholar]
- 113.Heatherton TF, Koslowski LT, Frecker RC, Fagerström K-O. Br J Addict. Vol. 86. 1991. The Fagerström Test for nicotine dependence: a revision of the Fagerström Tolerance Questionnaire; pp. 1119–27. [DOI] [PubMed] [Google Scholar]
- 114.Buchhalter AR, Schrinel L, Eissenberg T. Withdrawal-suppressing effects of a novel smoking system: comparison with own brand, not own brand, and de-nicotinized cigarettes. Nicotine Tob Res. 2001;3:111–8. doi: 10.1080/14622200110042636. [DOI] [PubMed] [Google Scholar]
- 115.Breland AB, Acosta MC, Eissenberg T. Tobacco specific nitrosamines and potential reduced exposure products for smokers: a preliminary evaluation of Advance. Tob Control. 2003;12:317–21. doi: 10.1136/tc.12.3.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Breland AB, Buchhalter AR, Evans SE, Eissenberg T. Evaluating acute effects of potential reduced-exposure products for smokers: clinical laboratory methodology. Nicotine Tob Res. 2002;4(Suppl 2):S131–40. doi: 10.1080/1462220021000032780. [DOI] [PubMed] [Google Scholar]
- 117.Buchhalter AR, Acosta MC, Evans SE, Breland AB, Eissenberg T. Tobacco abstinence symptom suppression: the role played by the smoking-related stimuli that are delivered by denicotinized cigarettes. Addiction. 2005;100:550–9. doi: 10.1111/j.1360-0443.2005.01030.x. [DOI] [PubMed] [Google Scholar]
- 118.Tiffany ST, Drobes DJ. The development and initial validation of a questionnaire on smoking urges. Br J Addict. 1991;86:1467–76. doi: 10.1111/j.1360-0443.1991.tb01732.x. [DOI] [PubMed] [Google Scholar]
- 119.Sayette MA, Shiffman S, Tiffany ST, Niaura RS, Martin CS, Shadel WG. The measurement of drug craving. Addiction. 2000;95(Suppl 2):S189–210. doi: 10.1080/09652140050111762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.O'Brien CP. Anticraving medications for relapse prevention: a possible new class of psychoactive medications. Am J Psychiatry. 2005;162:1423–31. doi: 10.1176/appi.ajp.162.8.1423. [DOI] [PubMed] [Google Scholar]
- 121.Killen JD, Fortmann SP. Craving is associated with smoking relapse: findings from three prospective studies. Exp Clin Psychopharmacol. 1997;5:137–42. doi: 10.1037//1064-1297.5.2.137. [DOI] [PubMed] [Google Scholar]
- 122.Shiffman S, West R, Gilbert D. SRNT Work Group on the Assessment of Craving and Withdrawal in Clinical Trials. Recommendation for the assessment of tobacco craving and withdrawal in smoking cessation trials. Nicotine Tob Res. 2004;6:599–614. doi: 10.1080/14622200410001734067. [DOI] [PubMed] [Google Scholar]
- 123.DiFranza JR, Wellman RJ. A sensitization-homeostasis model of nicotine craving, withdrawal, and tolerance: integrating the clinical and basic science literature. Nicotine Tob Res. 2005;7:9–26. doi: 10.1080/14622200412331328538. [DOI] [PubMed] [Google Scholar]
- 124.Ferguson SG, Shiffman S. The relevance and treatment of cue-induced cravings in tobacco dependence. J Subst Abuse Treat. 2009;36:235–43. doi: 10.1016/j.jsat.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 125.Shiffman S, Shadel WG, Niaura R, et al. Efficacy of acute administration of nicotine gum in relief of cue-provoked cigarette craving. Psychopharmacology (Berl) 2003;166:343–50. doi: 10.1007/s00213-002-1338-1. [DOI] [PubMed] [Google Scholar]
- 126.Heishman SJ, Singleton EG, Pickworth WB. Reliability and validity of a Short Form of the Tobacco Craving Questionnaire. Nicotine Tob Res. 2008;10:643–51. doi: 10.1080/14622200801908174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Henningfield JE, Goldberg SR. Nicotine as a reinforcer in human subjects and laboratory animals. Pharmacol Biochem Behav. 1983;19:989–92. doi: 10.1016/0091-3057(83)90405-7. [DOI] [PubMed] [Google Scholar]
- 128.Harvey DM, Yasar S, Heishman SJ, Panlilio LV, Henningfield JE, Goldberg SR. Nicotine serves as an effective reinforcer of intravenous drug-taking behavior in human cigarette smokers. Psychopharmacology (Berl) 2004;175:134–42. doi: 10.1007/s00213-004-1818-6. [DOI] [PubMed] [Google Scholar]
- 129.Sofuoglu M, Yoo S, Hill KP, Mooney M. Self-administration of intravenous nicotine in male and female cigarette smokers. Neuropsychopharmacology. 2008;33:715–20. doi: 10.1038/sj.npp.1301460. [DOI] [PubMed] [Google Scholar]
- 130.Henningfield JE, Miyasato K, Jasinski DR. Cigarette smokers self-administer intravenous nicotine. Pharmacol Biochem Behav. 1983;19:887–90. doi: 10.1016/0091-3057(83)90099-0. [DOI] [PubMed] [Google Scholar]
- 131.Griffiths RR, Henningfield JE, Bigelow GE. Human cigarette smoking: manipulation of number of puffs per bout, interbout interval and nicotine dose. J Pharmacol Exp Ther. 1982;220:256–65. [PubMed] [Google Scholar]
- 132.Dallery J, Houtsmuller EJ, Pickworth WB, Stitzer ML. Effects of cigarette nicotine content and smoking pace on subsequent craving and smoking. Psychopharmacology (Berl) 2003;165:172–80. doi: 10.1007/s00213-002-1242-8. [DOI] [PubMed] [Google Scholar]
- 133.Kassel JD, Greenstein JE, Evatt DP, et al. Smoking topography in response to denicotinized and high-yield nicotine cigarettes in adolescent smokers. J Adolesc Health. 2007;40:54–60. doi: 10.1016/j.jadohealth.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 134.Strasser AA, Lerman C, Sanborn PM, Pickworth WB, Feldman EA. New lower nicotine cigarettes can produce compensatory smoking and increased carbon monoxide exposure. Drug Alcohol Depend. 2007;86:294–300. doi: 10.1016/j.drugalcdep.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 135.Mendes P, Kapur S, Wang J, Feng S, Roethig H. A randomized, controlled exposure study in adult smokers of full flavor Marlboro cigarettes switching to Marlboro Lights or Marlboro Ultra Lights cigarettes. Regul Toxicol Pharmacol. 2008;51:295–305. doi: 10.1016/j.yrtph.2008.04.014. [DOI] [PubMed] [Google Scholar]
- 136.Breland AB, Kleykamp BA, Eissenberg T. Clinical laboratory evaluation of potential reduced exposure products for smokers. Nicotine Tob Res. 2006;8:727–38. doi: 10.1080/14622200600789585. [DOI] [PubMed] [Google Scholar]
- 137.Stafford D, LeSage MG, Glowa JR. Progressive-ratio schedules of drug delivery in the analysis of drug self-administration: a review. Psychopharmacology (Berl) 1998;139:169–84. doi: 10.1007/s002130050702. [DOI] [PubMed] [Google Scholar]
- 138.Stoops WW. Reinforcing effects of stimulants in humans: sensitivity of progressive-ratio schedules. Exp Clin Psychopharmacol. 2008;16:503–12. doi: 10.1037/a0013657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.DeGrandpre RJ, Bickel WK, Higgins ST, Hughes JR. A behavioral economic analysis of concurrently available money and cigarettes. J Exp Anal Behav. 1994;61:191–201. doi: 10.1901/jeab.1994.61-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Madden GJ, Bickel WK, Jacobs EA. Three predictions of the economic concept of unit price in a choice context. J Exp Anal Behav. 2000;73:45–64. doi: 10.1901/jeab.2000.73-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Bickel WK, Marsch LA, Carroll ME. Deconstructing relative reinforcing efficacy and situating the measures of pharmacological reinforcement with behavioral economics: a theoretical proposal. Psychopharmacology (Berl) 2000;153:44–56. doi: 10.1007/s002130000589. [DOI] [PubMed] [Google Scholar]
- 142.Hursh SR, Winger G. Normalized demand for drugs and other reinforcers. J Exp Anal Behav. 1995;64:373–84. doi: 10.1901/jeab.1995.64-373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Jacobs EA, Bickel WK. Modeling drug consumption in the clinic using simulation procedures: demand for heroin and cigarettes in opioid-dependent outpatients. Exp Clin Psychopharmacol. 1999;7:412–26. doi: 10.1037//1064-1297.7.4.412. [DOI] [PubMed] [Google Scholar]
- 144.MacKillop J, Murphy JG, Ray LA, et al. Further validation of a cigarette purchase task for assessing the relative reinforcing efficacy of nicotine in college smokers. Exp Clin Psychopharmacol. 2008;16:57–65. doi: 10.1037/1064-1297.16.1.57. [DOI] [PubMed] [Google Scholar]
- 145.Murphy JG, MacKillop J. Relative reinforcing efficacy of alcohol among college student drinkers. Exp Clin Psychopharmacol. 2006;14:219–27. doi: 10.1037/1064-1297.14.2.219. [DOI] [PubMed] [Google Scholar]
- 146.Mackillop J, Murphy JG, Tidey JW, Kahler CW, Ray LA, Bickel WK. Latent structure of facets of alcohol reinforcement from a behavioral economic demand curve. Psychopharmacology (Berl) 2009;203:33–40. doi: 10.1007/s00213-008-1367-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.MacKillop J, Murphy JG. A behavioral economic measure of demand for alcohol predicts brief intervention outcomes. Drug Alcohol Depend. 2007;89:227–33. doi: 10.1016/j.drugalcdep.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 148.Johnson MW, Bickel WK, Kirshenbaum AP. Substitutes for tobacco smoking: a behavioral economic analysis of nicotine gum, denicotinized cigarettes, and nicotine-containing cigarettes. Drug Alcohol Depend. 2004;74:253–64. doi: 10.1016/j.drugalcdep.2003.12.012. [DOI] [PubMed] [Google Scholar]
- 149.Johnson MW, Bickel WK. The behavioral economics of cigarette smoking: The concurrent presence of a substitute and an independent reinforcer. Behav Pharmacol. 2003;14:137–44. doi: 10.1097/00008877-200303000-00005. [DOI] [PubMed] [Google Scholar]
- 150.Mendoza-Baumgart MI, Tulunay OE, Hecht SS, et al. Pilot study on lower nitrosamine smokeless tobacco products compared with medicinal nicotine. Nicotine Tob Res. 2007;9:1309–23. doi: 10.1080/14622200701704228. [DOI] [PubMed] [Google Scholar]
- 151.Fagerstrom KO, Hughes JR, Callas PW. Long-term effects of the Eclipse cigarette substitute and the nicotine inhaler in smokers not interested in quitting. Nicotine Tob Res. 2002;4(Suppl 2):S141–5. doi: 10.1080/1462220021000032771. [DOI] [PubMed] [Google Scholar]
- 152.Griffiths RR, Rush CR, Puhala K. Validation of the multiple-choice procedure for investigating drug reinforcement in humans. Exp Clin Psychopharmacol. 1996;4:97–106. [Google Scholar]
- 153.Griffiths RR, Troisi JR, Silverman K, Mumford GK. Multiple-choice procedure: an efficient approach for investigating drug reinforcement in humans. Behav Pharmacol. 1993;4:3–13. [PubMed] [Google Scholar]
- 154.Jones HE, Garrett BE, Griffiths RR. Subjective and physiological effects of intravenous nicotine and cocaine in cigarette smoking cocaine abusers. J Pharmacol Exp Ther. 1999;288:188–97. [PubMed] [Google Scholar]
- 155.Sobel BF, Sigmon SC, Griffiths RR. Transdermal nicotine maintenance attenuates the subjective and reinforcing effects of intravenous nicotine, but not cocaine or caffeine, in cigarette-smoking stimulant abusers. Neuropsychopharmacology. 2004;29:991–1003. doi: 10.1038/sj.npp.1300415. [DOI] [PubMed] [Google Scholar]
- 156.Schuh LM, Schuster CR, Hopper JA, Mendel CM. Abuse liability assessment of sibutramine, a novel weight control agent. Psychopharmacology (Berl) 2000;147:339–46. doi: 10.1007/s002130050001. [DOI] [PubMed] [Google Scholar]
- 157.Bickel WK, DeGrandpre RJ, Higgins ST. The behavioral economics of concurrent drug reinforcers: a review and reanalysis of drug self-administration research. Psychopharmacology (Berl) 1995;118:250–9. doi: 10.1007/BF02245952. [DOI] [PubMed] [Google Scholar]
- 158.Pickworth WB, Herning RI, Henningfield JE. Electroencephalographic effects of nicotine chewing gum in humans. Pharmacol Biochem Behav. 1986;25:879–82. doi: 10.1016/0091-3057(86)90401-6. [DOI] [PubMed] [Google Scholar]
- 159.Pickworth WB, Fant RV, Butschky MF, Henningfield JE. Effects of transdermal nicotine delivery on measures of acute nicotine withdrawal. J Pharmacol Exp Ther. 1996;279:450–6. [PubMed] [Google Scholar]
- 160.Pickworth WB, O'Hare ED, Fant RV, Moolchan ET. EEG effects of conventional and denicotinized cigarettes in a spaced smoking paradigm. Brain Cogn. 2003;53:75–81. doi: 10.1016/s0278-2626(03)00205-7. [DOI] [PubMed] [Google Scholar]
- 161.Pickworth WB, Herning RI, Henningfield JE. Spontaneous EEG changes during tobacco abstinence and nicotine substitution in human volunteers. J Pharmacol Exp Ther. 1989;251:976–82. [PubMed] [Google Scholar]
- 162.Herning RI, Jones RT, Bachman J. EEG changes during tobacco withdrawal. Psychophysiology. 1983;20:507–12. doi: 10.1111/j.1469-8986.1983.tb03004.x. [DOI] [PubMed] [Google Scholar]
- 163.Pickworth WB, Herning RI, Henningfield JE. Mecamylamine reduces some EEG effects of nicotine chewing gum in humans. Pharmacol Biochem Behav. 1988;30:149–53. doi: 10.1016/0091-3057(88)90438-8. [DOI] [PubMed] [Google Scholar]
- 164.Azizian A, Monterosso J, O'Neill J, London ED. Magnetic resonance imaging studies of cigarette smoking. Handb Exp Pharmacol. 2009:113–43. doi: 10.1007/978-3-540-69248-5_5. [DOI] [PubMed] [Google Scholar]
- 165.Sharma A, Brody AL. In vivo brain imaging of human exposure to nicotine and tobacco. Handb Exp Pharmacol. 2009:145–71. doi: 10.1007/978-3-540-69248-5_6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Gundisch D, Koren AO, Horti AG, et al. In vitro characterization of 6-[18F]fluoro-A-85380, a high-affinity ligand for alpha4beta2* nicotinic acetylcholine receptors. Synapse. 2005;55:89–97. doi: 10.1002/syn.20096. [DOI] [PubMed] [Google Scholar]
- 167.Cordero-Erausquin M, Marubio LM, Klink R, Changeux JP. Nicotinic receptor function: new perspectives from knockout mice. Trends Pharmacol Sci. 2000;21:211–7. doi: 10.1016/s0165-6147(00)01489-9. [DOI] [PubMed] [Google Scholar]
- 168.Brody AL, Mandelkern MA, London ED, et al. Cigarette smoking saturates brain alpha 4 beta 2 nicotinic acetylcholine receptors. Arch Gen Psychiatry. 2006;63:907–15. doi: 10.1001/archpsyc.63.8.907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Brody AL, Mandelkern MA, Olmstead RE, et al. Ventral striatal dopamine release in response to smoking a regular vs a denicotinized cigarette. Neuropsychopharmacology. 2009;34:282–9. doi: 10.1038/npp.2008.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Brody AL, Mandelkern MA, Olmstead RE, et al. Gene variants of brain dopamine pathways and smoking-induced dopamine release in the ventral caudate/nucleus accumbens. Arch Gen Psychiatry. 2006;63:808–16. doi: 10.1001/archpsyc.63.7.808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Moolchan ET, Robinson ML, Ernst M, et al. Safety and efficacy of the nicotine patch and gum for the treatment of adolescent tobacco addiction. Pediatrics. 2005;115:e407–14. doi: 10.1542/peds.2004-1894. [DOI] [PubMed] [Google Scholar]
- 172.Gonzales D, Rennard SI, Nides M, et al. Varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs sustained-release bupropion and placebo for smoking cessation: a randomized controlled trial. JAMA. 2006;296:47–55. doi: 10.1001/jama.296.1.47. [DOI] [PubMed] [Google Scholar]
- 173.Jorenby DE, Hays JT, Rigotti NA, et al. Efficacy of varenicline, an alpha4beta2 nicotinic acetylcholine receptor partial agonist, vs placebo or sustained-release bupropion for smoking cessation: a randomized controlled trial. JAMA. 2006;296:56–63. doi: 10.1001/jama.296.1.56. [DOI] [PubMed] [Google Scholar]
- 174.Bigelow GE, Griffiths RR, Liebson I, Kaliszak JE. Double-blind evaluation of reinforcing and anorectic actions of weight control medications. Interaction of pharmacological and behavioral treatments. Arch Gen Psychiatry. 1980;37:1118–23. doi: 10.1001/archpsyc.1980.01780230036005. [DOI] [PubMed] [Google Scholar]
- 175.Tonstad S, Tonnesen P, Hajek P, et al. Effect of maintenance therapy with varenicline on smoking cessation: a randomized controlled trial. JAMA. 2006;296:64–71. doi: 10.1001/jama.296.1.64. [DOI] [PubMed] [Google Scholar]
- 176.Dasgupta N, Schnoll SH. Signal detection in post-marketing surveillance for controlled substances. Drug Alcohol Depend. 2009 doi: 10.1016/j.drugalcdep.2009.05.019. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 177.Cone EJ. Ephemeral profiles of prescription drug and formulation tampering: evolving pseudoscience on the Internet. Drug Alcohol Depend. 2006;83(Suppl 1):S31–9. doi: 10.1016/j.drugalcdep.2005.11.027. [DOI] [PubMed] [Google Scholar]
- 178.O'Connor RJ, Cummings KM, Rees VW, et al. Surveillance methods for identifying, characterizing, and monitoring tobacco products: potential reduced exposure products as an example. Cancer Epidemiol Biomarkers Prev. 2009 doi: 10.1158/1055-9965.EPI-09-0429. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Woolf A, Burkhart K, Caraccio T, Litovitz T. Self-poisoning among adults using multiple transdermal nicotine patches. J Toxicol Clin Toxicol. 1996;34:691–8. doi: 10.3109/15563659609013830. [DOI] [PubMed] [Google Scholar]
- 180.World Health Organization . WHO Expert Committee on Drug Dependence, Thirty-third Report, Technical Report Series, No. 915. World Health Organization; 2003. [PubMed] [Google Scholar]
- 181.Le Foll B, Goldberg SR. Nicotine as a typical drug of abuse in experimental animals and humans. Psychopharmacology (Berl) 2006;184:367–81. doi: 10.1007/s00213-005-0155-8. [DOI] [PubMed] [Google Scholar]
- 182.Perkins KA. Individual variability in responses to nicotine. Behav Genet. 1995;25:119–32. doi: 10.1007/BF02196922. [DOI] [PubMed] [Google Scholar]
- 183.Perkins KA, D'Amico D, Sanders M, Grobe JE, Wilson A, Stiller RL. Influence of training dose on nicotine discrimination in humans. Psychopharmacology (Berl) 1996;126:132–9. doi: 10.1007/BF02246348. [DOI] [PubMed] [Google Scholar]
- 184.Kleykamp BA, Jennings JM, Sams C, Weaver MF, Eissenberg T. The influence of transdermal nicotine on tobacco/nicotine abstinence and the effects of a concurrently administered cigarette in women and men. Exp Clin Psychopharmacol. 2008;16:99–112. doi: 10.1037/1064-1297.16.2.99. [DOI] [PubMed] [Google Scholar]
- 185.Leventhal AM, Waters AJ, Boyd S, Moolchan ET, Lerman C, Pickworth WB. Gender differences in acute tobacco withdrawal: effects on subjective, cognitive, and physiological measures. Exp Clin Psychopharmacol. 2007;15:21–36. doi: 10.1037/1064-1297.15.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.McClernon FJ, Kollins SH. ADHD and smoking: from genes to brain to behavior. Ann N Y Acad Sci. 2008;1141:131–47. doi: 10.1196/annals.1441.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness. JAMA. 2000;284:2606–10. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- 188.John U, Meyer C, Rumpf HJ, Hapke U. Smoking, nicotine dependence and psychiatric comorbidity - a population-based study including smoking cessation after three years. Drug Alcohol Depend. 2004;76:287–95. doi: 10.1016/j.drugalcdep.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 189.Newcomer JW. Medical risk in patients with bipolar disorder and schizophrenia. J Clin Psychiatry. 2006;67:e16. [PubMed] [Google Scholar]
- 190.Strasser AA, Kaufmann V, Jepson C, et al. Effects of different nicotine replacement therapies on postcessation psychological responses. Addict Behav. 2005;30:9–17. doi: 10.1016/j.addbeh.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 191.Evans SM, Cone EJ, Henningfield JE. Arterial and venous cocaine plasma concentrations in humans: relationship to route of administration, cardiovascular effects and subjective effects. J Pharmacol Exp Ther. 1996;279:1345–56. [PubMed] [Google Scholar]
- 192.Sellers EM, Schuller R, Romach MK, Horbay GL. Relative abuse potential of opioid formulations in Canada: a structured field study. J Opioid Manag. 2006;2:219–27. doi: 10.5055/jom.2006.0034. [DOI] [PubMed] [Google Scholar]
- 193.Rees VW, Kreslake JM, O'connor RJ, et al. Assessing consumer responses to PREPs: A review of tobacco industry. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]