Abstract
Background
Hospitalized patients encounter stressors that impact their experience and recovery. There is a need for theoretically based, empirically supported nursing interventions to create a therapeutic and healing environment that decrease stress and improve patients’ experiences.
Purpose
To determine whether pet therapy interventions improve physiological, behavioral and mood outcomes and experiences of hospitalized patients.
Methods
A single group pre- post quasi-experimental design with mixed methods was used in 59 hospitalized patients. Paired t-tests were used to evaluate changes from baseline following a pet therapy intervention. Qualitative data were analyzed using content analysis. .
Results
Compared with baseline, patients had significant decreases in pain, respiratory rate and negative mood state and a significant increase in perceived energy level. Quantitative and qualitative findings provide support for decreased tension/anxiety and fatigue/inertia and improved overall mood.
Conclusions
Pet therapy is a low-tech, low-cost therapy that improved mood and was meaningful to hospitalized patients.
Keywords: Pet Therapy, Therapeutic, Healing, Stress reduction, Recovery
Hospitals can often be lonely and stressful places for patients compromised by illness and separated from family and loved ones. While patients generally rate nurses, doctors and other healthcare workers high on patient satisfaction surveys, they often rate the overall experience of hospitalization low (Cutshall, Fenske, Kelly, Phillips Sundt & Bauer, 2007; 2008 Hospital Pulse Report). Aligned with the goal of creating a more patient responsive health care system (Institute of Medicine, 2001), there is a growing emphasis on improving hospitalization for patients and their families by creating a therapeutic and healing environment (Geary, 2003; Westchester County Business Journal, 2005; Whitehead, 2005). There is a pressing need to develop theoretically based and empirically supported nursing interventions to achieve this goal.
Hospitalized patients encounter multiple stressors, including pain, lack of sleep, concerns about outcomes, and unfamiliar environment, that can impact their experience, well-being and recovery (Broadbent, Petrie, Alley & Booth, 2003; Cutshall et al., 2007; Kiecolt-Glaser; McGuire et al., 2006, Pearson, Maddern, Fitridge, 2005). To help reduce this stress, some hospitals have incorporated complementary therapies such as music, mind-body interventions, therapeutic touch and pets to help patients cope with stressors while hospitalized (Cutshall, et.al. 2007; Stanley-Hermanns & Miller, 2002). Complementary and alternative therapies, including pet therapy, are among the domains directed toward creating a healing environment identified by the National Institutes of Health (Johnson, Meadows, Haubner & Sevedge, 2003), but current descriptive knowledge needs to be expanded to develop the evidence needed for practice and policy (Filan & Llewellyn-Jones, 2006; Johnson, 2002; Wilson & Barker, 2003). Interventions that enhance coping and improve patient responses to symptoms are among the priorities for knowledge development (National Center for Complementary and Alternative Medicine, n.d.; National Institute of Nursing Research, n.d.). The purpose of this study was to evaluate the efficacy of a pet therapy intervention as a complementary therapy to improve stress-related outcomes for hospitalized patients.
Background
By introducing multiple strategies to decrease stress, patients have choices around those interventions that are most beneficial to them in improving their well-being. One major teaching hospital in the Northeastern United States has introduced comforting techniques (Barron, Coakley, Fitzgerald, & Mahoney, 2008) along with implementing a Pet Therapy program, co-led by the Department of Nursing and the Volunteer Department. The Pet Therapy program uses volunteer handlers and their own dogs to visit patients on twelve inpatient and one outpatient department two afternoons each week. Each dog is screened by an outside agency specializing in evaluating animals to be part of pet therapy programs in healthcare settings. The current program initially began on 3 inpatients units in 2003. As part of the initial trial period, the first fifty patients visited by dogs were asked to complete a semantic differential scale to rate their experience with the pet therapy program. All of the participants rated the experience as very favorable and recommended that the program continue. Many patients handwrote comments on the data collection form. For example, one participant described the dog as a connection to the outside world, and that touching a warm friendly dog made them feel connected and cared for. While all of the comments were very positive, one statement seemed to capture the essence of the program: “I thought that I would not smile today, and then I saw Maggie!” The current study builds on this preliminary support
Conceptual Framework
The Science of Unitary Humans (Rogers, 1970) provided the conceptual framework for the pet therapy intervention. Rogers described all living matter as an energy field. An energy field consists of the body, mind, emotions and environment. Energy fields are dynamic and in continuous interaction with the environmental field. When something like an animal is introduced into the patient’s energy field, the experience changes for the person. One dog handler noted that “patients started to smile as soon as I enter the hospital with a dog, (Evans, personal communication, 2003). Feedback from patients and nurses, the visits with dogs used in the pilot pet therapy program provided comfort to patients, stress decreased and the hospital experience was seen as more positive. When patients have less stress and feel better about their hospital stay, it is expected that these changes will have a positive impact on their recovery.
Stress and Recovery
Psychoneuroimmunology (PNI) provides a foundation for understanding the relationship between stress and recovery and supports a theoretical linkage of psychobehavioral and physiological outcomes that can be achieved with the complementary Pet Therapy intervention. For example, PNI suggests that psychological variables have a direct effect on “stress” hormones and that in turn can modulate immune function and psychological well-being (Cole, Gawlinski, Steers & Kotlerman, 2007; Johnson, Meadows, Hauber & Sevedge, 2008). The main theme of the PNI theory is that stress interferes with recovery. Complementary therapy interventions may modulate this relationship by reducing stress and enhancing coping and have been identified as a priority for nursing research (McCain, Gray, Walter & Robins, 2005). Preliminary studies support the potential of Pet Therapy as such an intervention. Theoretically-based, non-invasive indicators of stress management applicable to acutely ill and hospitalized patients include vital signs, perceived pain and energy, mood and subjective patient experience.
Literature Review
Pet Therapy and Patient Outcomes
According to literature from the past decade, pet therapy has been beneficial to patients in intensive care settings, pediatrics, with spinal cord injuries and the elderly (Cole & Gawlinski, 2000, Giuliano, Bloniasz, & Bell, 1999, Bouchard, Landry, Belles-Isles, & Gagnon, 2004, Counsell, Abram, & Gilbert, 1997). Patient responses to this intervention include feeling happy, more calm and less lonely after a pet visit (Cole & Gawlinski, 1995) as well as having a decrease in anxiety, systolic pulmonary artery pressure, epinephrine and norepinephrine levels (Cole, Gawlinski, Steers & Kotlerman, 2007). A study in pediatrics found that pet therapy distracts children from pain perception and may possibly activate comforting thoughts regarding companionship and home (Sobo, Eng, & Kassity-Krich, 2006). Patients on general care units reported feeling happy, comforted, satisfied, relaxed, attached, and peaceful after a dog visit (Coakley & Somerville 2003). Pet Therapy is an intervention that can provide diversion and comfort by providing a link to the familiar (Johnson, Meadows, Haubner, & Sevedge, 2008).
The literature reports that pets can make a difference for people by decreasing loneliness and isolation. There are a few studies that show how pets can affect these behaviors and responses to patients in the hospital setting including improve mood, comfort and relaxation (Cole & Gawlinski, 1995;; Johnson, Meadows, Haubner & Sevedge, 2008). Despite nursing leaders such as Florence Nightingale who advocated for the importance of animals within the care environment (Brodie & Biley, 1999), pet therapy is a fairly new phenomenon in hospitals. Healthcare administrators have been reluctant to let animals into hospitals because of fear of how animals would respond when emergencies happen, zoonotic infection (infections that can be passed from animals to humans) and fear that they would mess or bark and scare patients and families.
There are a few studies that have examined the experience of pet therapy with patients (Giuliano & Bell, 1999, Bouchard et al. 2004, Cole & Gawlinski, 1995, Counsell et al., 1997, Cole et al., 2007; Sobo et al., 2006), however none that have studied pet therapy program as an intervention that has an impact on recovery. Patients who have less stress after a visit with a dog and are more relaxed should recover more quickly.
Purpose
The purpose of this investigation was to explore conceptually-based outcomes of participation in a Pet Therapy intervention in hospitalized patients. We hypothesized that patients who received the pet therapy visit would have lower vital signs, less pain, more energy and better mood after experiencing the pet therapy intervention compared to these same measures before the pet therapy visit. A second purpose was to describe the patient experience of the pet visit.
Methods
Sample and Setting
After approval from the Institutional Review Board, a convenience sample of 61 patients who met the hospital Pet Therapy eligibility criteria (see Table 1) was recruited for the study. Inclusion criteria were: English speaking; 18 years of age or older; and able to give informed consent. Patients were excluded from the study if they were hemodynamically unstable. Initial screening for eligibility was completed by staff nurses caring for the patients and then verified by research nurses who explained the study and sought patient consent. The study took place on three inpatient units where the pet therapy program had been implemented.
Table 1.
Pet Therapy Eligibility Criteria
| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Patient | Infection Control | |
| In patient | Dog allergies | Tuberculosis |
| Outpatient | Fear of dogs | Immunosuppressed |
| Uncovered open wounds | Hepatitis | |
| Salmonella | ||
| Fever of unknown origin | ||
| Communicable virus | ||
| Staphylococcus aureus | ||
Design
A single group pre- post quasi-experimental design with mixed methods was used to evaluate the effect of pet therapy on patient outcomes and experience.
Instruments and Measures
Physiologic measures
Vital signs, including blood pressure, pulse and respirations were used as non-invasive indices of physiological stress. The blood pressure was measured using a mercury sphygmomanometer, and a stethoscope. An appropriate cuff size was used for each subject. The systolic blood pressure was recorded at the first phase of the Korotkoff sounds and the diastolic blood pressure was recorded at the fifth phase of Korotkoff sounds. Heart rate was measured by counting the radial pulse for one minute. Respiratory rate was measured by counting inspirations and expirations for one minute.
Behavioral measures
Patient perceptions of pain and level of energy were measured as an index of theoretically-based behavioral responses to the pet therapy intervention. Level of pain was measured using a Visual Analog Scale (VAS) for pain with 0 equal to “no pain” and 10 equal to “pain as bad as it can be”. A VAS is a scale determined by a straight line that represents the continuum of the dimension being measured with anchors at either end to help delineate boundaries of a measure (McDowell & Newell, 1987). The scale was printed horizontally and required about 30 seconds to complete. Each patient was asked to rate his/her level of pain prior to and immediately following the pet visit.
Level of energy was measured using a Visual Analog Scale (VAS) with 0 equal to “no energy” and 10 equal to “as much as energy as possible”. Each patient was asked to rate his/her perceived level of energy prior to and immediately following the pet visit.
Mood state
The Profile of Mood States survey (POMS) (McNair, Lorr, & Doppleman, 1981) is a self report assessment of six transient mood states: tension-anxiety, depression-dejection, anger-hostility, vigor-activity, fatigue-inertia and confusion-bewilderment. A total mood disturbance score also can be calculated. Participants are asked to respond to adjectives that reflect current mood on a 5-point Likert scale. Choices range from not at all (0) to extremely (4). The higher the scores indicate a more negative mood with the exception of the vigor-activity subscale. The 30-item brief form, takes 5-minutes to complete, is used often with the elderly and with those recovering from surgery (McNair, 1992).The POMS has well-established evidence of internal consistency and test-retest reliability and predictive, construct and factorial validity (Frank-Stromborg & Olsen, 1997; McNair, Heuchert, & Shilony, 2003). Internal consistency reliability for this study was conducted on each of the subscales and the total scores and ranged from ά.70-.92
Exit Interview
Three open-ended questions were asked to capture patients’ perceptions about their experience with the visit with the dog: 1) “What has this experience with a dog visit been like for you?”: 2) “Was the visit with the dog what you expected it to be?”; and 3) “Would you want to have another visit with a dog if you were a patient at this hospital again?”
Procedure
Staff nurses from the three-inpatient units helped to identify eligible patients for the study. All data were collected by research nurses from the General Clinical Research Center (GCRC) on the inpatient units. Baseline assessments were performed immediately prior to the pet therapy intervention. Follow-up assessments occurred immediately following the dog visit with patients serving as their own control in order to evaluate change in response to the intervention.
Procedure
The research protocol was designed around an existing pet therapy program. Two days per week from September 2004 to July 2007, staff nurses on the three in-patient units identified participants who had requested to participate in the pet therapy program. The nurse determined the appropriateness of the referral by utilizing the Patient Inclusion and Exclusion Criteria and the Infection Control guidelines (Table 1). The patient’s nurse discussed the purpose of the Pet Therapy Program with the patient and obtained verbal consent. The nurse contacted the Volunteer Department that coordinated each visit by verifying patient’s name, date, time, and location of visit. The appropriateness of the visit was determined at the discretion of the nurse caring for the patient. The nurse caring for the patient supervised pet visitation as appropriate, to assure that handlers followed established infection control policy and guidelines. While nurses were instructed to curtail the visit if adverse behaviors were observed, and there were no instances when this was necessary.
Immediately prior to the visit with the dog, the research nurse collected baseline measures of vital signs, pain and energy levels at the bedside and all participants completed the short version POMS. The research nurse waited outside the room as the volunteer handler and the dog entered the room. After the handler and dog left the room, the research nurses returned to obtain post-visit measures of vital signs, pain and energy VAS, and POMS immediately following the intervention. Additionally, all subjects were asked to answer pre-determined open ended questions about their perception of the Pet Therapy experience.
Pet Therapy intervention
The volunteers introduced themselves to the patient. The pet therapy intervention was conducted in an individualized manner within the standard protocol based on patient preference. Some patients preferred to talk with the handler about the dog, their own dogs or other pets from their childhood. Other patients wished to visit quietly with the dog while the handler stood nearby. The pet therapy interventions lasted on average of 10 minutes with each subject.
Data Analysis
Quantitative data were analyzed using SPSS version 15. Descriptive statistics were performed on demographic, physiological, behavioral and mood variables. Data were analyzed to determine if they were normally distributed and met the assumptions of the planned analyses. A paired t-test was used to analyze pre-post quantitative data. To minimize potential Type 1 error, Bonferroni’s procedure, which controls for the escalation of significance across multiple comparisons, was used. Experiment wide alpha was set at p <.05 such that each test had to reach a level of p < .004 (.05/13) to be considered statistically significant. One-tailed tests were used for hypothesis testing.
Qualitative data from the exit questionnaires were analyzed by the PI of this study and a research student not involved in data collection. Content Analysis was used to analyze this data. The unit of analysis was identified as phrases or sentences contained from the responses that were transcribed by the Principal Investigator. Inter-rater reliability was established and key findings were synthesized into categories reflecting the subscales of the POMS when both individuals came together with their own identified themes. Content Analysis is a qualitative research method that is used to isolate and interpret themes, issues and repeated patterns (Denzin & Lincoln, 1994) and refine understanding as new insights about the data emerge. The strategies for analysis outlined by Downe-Wamboldt (1993) were followed.
Results
Characteristics of the Sample
Sixty-one subjects participated in the study. Two subjects did not complete the post-test and were dropped from the analysis, resulting in a final sample of 59 patients. Descriptive characteristics of the sample are presented in Table 2. There was a wide range in both age (median = 61) and length of stay (median = 3). Medical diagnoses included cancer, asthma, AIDS, heart failure, diabetes, coronary artery disease and gastrointestinal (GI) bleeding. Surgical diagnoses included amputation, hysterectomy, aneurysm repair, venous bypass surgery, GI surgery and carotid endarterectomy.
Table 2.
Baseline demographic characteristics of the sample (N = 59)
| Characteristic | M (SD) | Range |
|---|---|---|
| Age (years) | 59.56 (15.68) | 24 – 88 |
| Length of stay (days) | 6.32 (9.76) | 1 – 60 |
| Characteristic | n | % |
| Gender (n=53) | ||
| Female | 24 | 45.3 |
| Male | 29 | 49.2 |
| Current Pet Owner | ||
| Yes | 28 | 47.5 |
| No | 31 | 52.5 |
| Primary Diagnosis | ||
| Medical | 30 | 52.6 |
| Surgical | 27 | 47.4 |
| Not recorded | 2 | 3.4 |
Physiologic and Behavioral Outcomes
The first hypothesis, that there would be a significant decrease in blood pressure, heart rate, respiratory rate and pain, and increase in energy perception, from baseline to post-pet therapy was partially supported. Mean scores and differences pre- and post-pet therapy visits for vital signs, pain and energy are depicted in Table 3. Compared with baseline scores, patients had small but significant decreases in respiratory rate and pain and a corresponding increase in energy levels following the pet therapy intervention. There were no significant changes in systolic or diastolic blood pressure or pulse.
Table 3.
Comparison of vital signs, pain and energy levels at baseline and post-pet therapy visit (N=59)
| Variable | Pre-test | Post-test | Difference | t | p* |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | ||||
| Systolic blood pressure, mm Hg | 119.88 (19.1) | 122.39 (16.8) | 2.50 | 1.49 | .07 |
| Diastolic blood pressure, mm Hg | 66.22 (11.4) | 66.27 (10.8) | .05 | .05 | .48 |
| Pulse | 76.56 (14.4) | 76.93 (13.5) | .37 | −.41 | .34 |
| Respiration | 18.0 (2.0) | 17.23(1.8) | −.77 | −3.47 | .000 |
| Pain VAS | 3.15 (2.8) | 2.47 (2.6) | −.69 | −3.30 | .001 |
| Energy VAS | 4.12 (2.4) | 4.90 (2.6) | .78 | 3.18 | .001 |
Criterion for significance p <.004; one-tailed
Mood State Outcomes
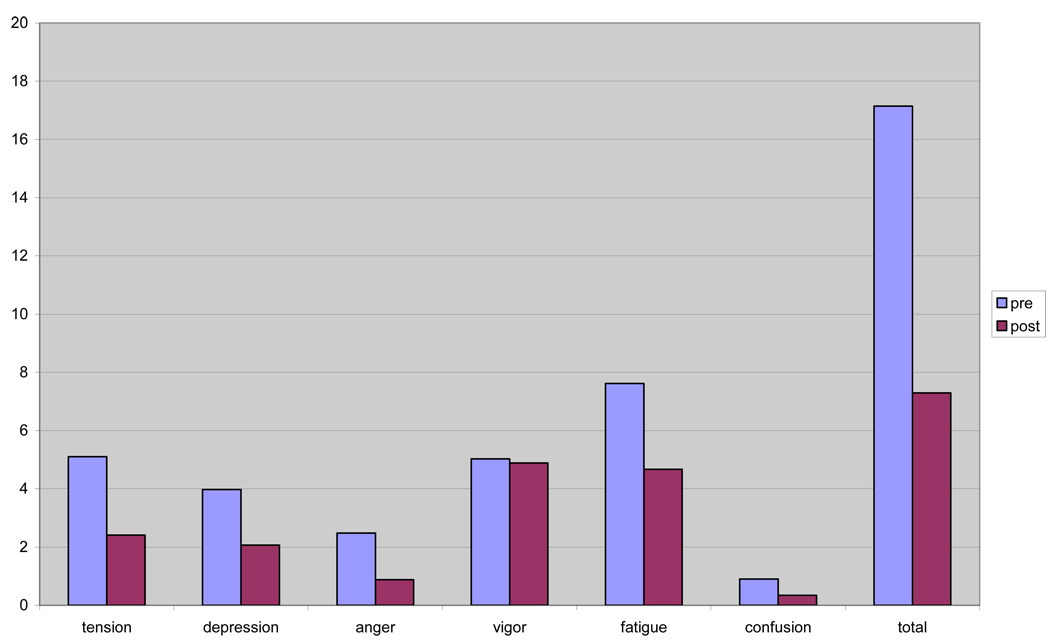
The second hypothesis, that mood would improve in response to the pet therapy intervention, was supported. Total mood disturbance (TMD) scores improved significantly from baseline to post pet therapy follow-up, decreasing by 57%. Table 4 depicts these changes in POMS total and subscale scores from baseline to post pet therapy intervention. As shown in Figure 1, changes in several negative mood state subscales accounted for the change in TMD. Statistically significant improvements were noted for tension/anxiety, anger/hostility, fatigue/inertia and depression/dejection subscales. Clinically important changes in mood state, indicated by improvement by more than one-half standard deviation from baseline was achieved with tension/anxiety, fatigue/inertia and TMD. There were no changes in the vigor/activity or confusion/bewilderment subscales.
Table 4.
Comparison of mood states at baseline and post-pet therapy visit (N=59)
| Variable | Pre-test | Post-test | Difference | t | p* |
|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | ||||
| POMS Subscales | |||||
| Tension/anxiety | 5.11 (4.38) | 2.41 (3..38) | −2.70 | 6.10 | .000 |
| Anger/hostility | 2.48 (4.10) | 0.89 (1.90) | −1.59 | 3.28 | .001 |
| Fatigue/inertia | 7.62 (5.33) | 4.67 (4.62) | −2.95 | 5.74 | .000 |
| Depression/dejection | 3.98 (4.73) | 2.08 (3.47) | −1.90 | 3.47 | .000 |
| Vigor/activity† | 5.04 (4.75) | 4.89 (4.02) | −0.14 | 0 24 | .40 |
| Confusion/bewilderment | 0.90 (3.82) | 0.35 (3.36) | −0.56 | 1.56 | .06 |
| POMS Total Mood Disturbance | 17.16 (21.01) | 7.30 (16.07) | −9.86 | 4.24 | .000 |
Criterion for significance p < .004; one-tailed
higher scores more positive
Figure 1.
POMS subscale and total scores before and after pet therapy intervention
Qualitative comments made by the subjects at the end of the pet therapy visit reflected these mood state changes. For example, the decrease in tension and anxiety was noted by several patients. Five patients reported that the dog visit was calming, one patient called it nice, another patient called it comforting and one said “there was a reduction of anxiety.” Patients also experienced a decrease in depression-dejection. Comments that reflect this change include; “good therapy;” “great, enjoyed it immensely;” and “forgot about everything else.” Three patients said it “brought my spirits up”. In terms of anger-hostility, many patients called the experience rewarding, happy, very pleasurable, comforting, “brightens your day/better mood.” Reflecting improvements in fatigue-inertia, patients said the visit with the dog was relaxing, one person said “it takes away some of the tiredness” and another reported “I’m moving my arms more”. While the vigor-activity subscale had almost no change in score, twenty-five patients reported that they enjoyed the visit. Patient comments included: “Oh, I loved it!” “Wonderful;” “Breath of fresh air;” and “Cheered me up.” There were no negative comments.
Discussion
The purpose of this study was to evaluate the efficacy of a pet therapy program in improving theory-based physiological, behavioral and experiential outcomes in hospitalized patients. Participants reported improved levels of pain and energy and most mood scores following the visits with the dogs. Although blood pressure and pulse did not change, the qualitative data collected at the end of the pet therapy visit indicated that the participants felt more calm, relaxed, engaged, “cheered up” and that they valued the experience, supporting previous reports. Johnson and her team (2008) argued that patients' expressions of the benefits of visits with dogs may have even more meaning than the measurable results. While this study did demonstrate positive behavioral outcomes, compatible with those of Cole and Gawlinski (2007) and supportive of the Unitary Transformative perspective, the qualitative responses about the experience complement hypothesized relationships and also add to knowledge of how short-term improvements in energy and pain and mood might facilitate recovery from acute illness. .
Rogers and other nurse theorists from a Unitary Transformative perspective (Picard & Jones, 2005) describe human energy fields and environmental fields as dynamic and reciprocal. Changes in one field can affect the other. In this study, the introduction of a dog into a patient’s field altered the environment and resulted in actual and perceived changes in the recipient of pet therapy. This study contributes to the literature on creating therapeutic and healing environments in healthcare settings through the implementation of complementary interventions as a way to benefit patients.
A pet therapy program is one example of these interventions and is similar to other complementary interventions in that they provide an opportunity for nurses to focus on their patients in a unique and interactive way. The findings in this study are similar to those of Barron, et al. (2008) who reported that by providing therapeutic touch (TT) to oncology patients, nurses were able to focus on their patients and make a connection with them in a more meaningful way. Through this connection nurses were able to help patients recover in a way that is different from the more traditional biomedical approach. Either through distraction from hospital routines and treatments or through the presence and interaction with an animal as in the case of this study or through the interaction with the nurse using TT in the case of the Barron article, patients reported both interventions as comforting and relaxing.
The results of this investigation are positive and indicate there are benefits of pet therapy visits with hospitalized patients. However in this current investigation, the visits with patients were only on average ten minutes in length which may explain why some of the physiological metrics did not change as much as hypothesized. Additionally, the pet visits were only evaluated once during a hospitalization so it is unknown if repeated visits with dogs would yield different perhaps stronger results.
Limitations
There are important limitations to this study that include the lack of a control group, the small number of subjects and the convenience sample. In addition, there was potential for subject bias as there was a relatively short period of time between the completion of pre-post data collection and the risk that subjects could have remembered their earlier responses when completing the post-pet visit questionnaires. However, it is also noteworthy that scores consistently changed in a positive direction. During this study, pet therapy was conducted in the usual manner with patients deciding what was most therapeutic for them, either visiting with the dog or visiting with the handler or both, thus individualizing the intervention. Other studies that have evaluated Pet Therapy programs have separated visits with the dogs from visits with the handlers. This may account for different and significant findings in this study compared to the Johnson et al. (2008) study that separated the dog visits from visits with people and found no significant study results. Similar to the intervention used in this study, Cole and Gawlinski (2007) found that the combination of volunteer and dog resulted in more improvements in cardiopulmonary pressures, neurohormone levels and state anxiety compared to volunteer only and usual care control groups. Johnson and others (e.g. Wilson & Barker, 2003) have raised key questions about the design of control conditions that are salient to the study of complementary therapies where “presence,” choice and individualization may be critical intervention components.
Another limitation of this study may have been the scope of the pet therapy program at the study site. Currently, dogs visit with patients on Tuesdays and Thursdays, because of the challenges related to recruiting and retaining dog handler volunteers. Since dog visits were limited to two days per week and the availability of nurse data collectors, some patients had data collected at the beginning of their hospitalization while others were getting ready for discharge. There may have been stronger effects if all patients have been seen by the dog when they were the most ill.
We recommend that future studies include a comprehensive integrative care program that offers different evidence-based therapeutic interventions to patients to help them relax, decrease pain and reflect on the interaction with a nurse that is different from the traditional biomedical approach that is currently offered to patients during hospitalization. Randomized control studies are needed to look at the relationship between stress, relaxation and recovery in patients who have visits with a dog compared to those who do not. Further work is needed to learn more about how this low tech, low cost intervention provides an opportunity for hospitalized patients to interact with animals and have an experience that is humanistic in nature. It is important to look at how these complementary interventions programmatically may have an impact on creating a healing and therapeutic environment and ultimately on the recovery of hospitalized patients.
Acknowledgements
The authors wish to acknowledge Mary Sullivan RN, MS, Jane Flanagan APRNC, PhD, Kathy Habeeb RN, BSN, Mary Elizabeth McAuley RN, BSN, Sharon Bouvier RN, MS, Jacqueline Somerville RN, PhD and Paul Bartush for their contributions and support of the Pet Therapy program and this research study.
Funding:
The project described was supported by Grant Number M01-RR-01066, Massachusetts General Hospital General Clinical Research Center, from the National Center for Research Resources. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health…
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest statement:
There are not conflict of interest associated with this study or this manuscript.
Contributor Information
Amanda Bulette Coakley, Massachusetts General Hospital, Founders House 345, Massachusetts General Hospital, Boston, MA 02114 USA, abcoakley@partners.org.
Ellen K. Mahoney, Cushing Hall, Boston College, Chestnut Hill, Ma 02467, ellen.mahoney@bc.edu.
REFERENCES
- Barron AM, Coakley AB, Fitzgerald E, Mahoney E. Integrating Therapeutic touch in Nursing Practice on an Inpatient Oncology and Bone Marrow Transplant Unit: An Exploratory Study. International Journal of Human Caring. 2008 [Google Scholar]
- Baun MM, Bergstrom N, Langston NF, Thoma L. Physiologic effects of the human/companion animal bonding. Nursing research. 1983;33(3):126–129. [PubMed] [Google Scholar]
- Broadbent E, Petrie KJ, Alley PG, Booth RJ. Psychological stress impairs early wound repair following surgery. Psychosomatic Medicine. 2003;65:865–869. doi: 10.1097/01.psy.0000088589.92699.30. [DOI] [PubMed] [Google Scholar]
- Brodie SJ, Biley FC. An exploration of the potential benefits of pet-facilitated therapy. Journal of clinical nurses. 1999;8(4):329–337. doi: 10.1046/j.1365-2702.1999.00255.x. [DOI] [PubMed] [Google Scholar]
- Bouchard F, Landry M, Belles-Isles M, Gagnon J. A magical dream: a pilot project in animal-assisted therapy in pediatric oncology. Cancer Oncology Nursing Journal. 2004;1:14–17. doi: 10.5737/1181912x1411417. [DOI] [PubMed] [Google Scholar]
- Coakley A, Somerville J. Hospital-based pet therapy. Alpha Chi News. 2003;26(1):4–5. [Google Scholar]
- Cole KM, Gawlinski A. Animal assisted therapy in the intensive care unit: A staff nurse's dream come true. Nursing Clinics of North America. 1995;3:529–536. [PubMed] [Google Scholar]
- Cole KM, Gawlinski A. Animal-assisted therapy: the human-animal bond. AACN Clinical Issues. 2000;1:139–149. doi: 10.1097/00044067-200002000-00015. [DOI] [PubMed] [Google Scholar]
- Cole KM, Gawlinski A, Steers N, Kotlerman J. Animal-assisted therapy in patients hospitalized with heart failure. American journal of critical care. 2007;16(6):575–585. [PubMed] [Google Scholar]
- Counsell CM, Abram J, Gilbert M. Animal assisted therapy and the individual with spinal cord injury. SCI Nursing. 1997;2:52–55. [PubMed] [Google Scholar]
- Cutshall SM, Fenske LL, Kelly RF, Phillips BR, Sundt TM, Bauer BA. Creation of a healing enhancement program at an academic medical center. Complementary Therapies in Clinical Practice. 2007;13(4):217–223. doi: 10.1016/j.ctcp.2007.02.001. [DOI] [PubMed] [Google Scholar]
- Denzin NK, Lincoln YS. Handbook of qualitative research. Thousand Oaks, CA: Sage Publications; 1994. [Google Scholar]
- Downe-Wamboldt B. Content analysis: Method, applications, and issues. Health Care for Women International. 1993;13:313–321. doi: 10.1080/07399339209516006. [DOI] [PubMed] [Google Scholar]
- Evans B. Personal communication. 2003.
- Felten DL, Felten SY. Innervation of lymphoid tissue. In: Ader R, Felten DL, Cohen, editors. (1994) Psychoneuroimmunology. San Diego, CA: Academic Press; 1991. pp. 87–101. [Google Scholar]
- Filan SL, Llewellyn-Jones RH. Animal-assisted therapy for dementia: a review of the literature. International pschogeriatrics. 2006;18(4):597–611. doi: 10.1017/S1041610206003322. [DOI] [PubMed] [Google Scholar]
- Francis GM. “Here come the puppies”: The power of the human-animal bond. Holistic Nursing Practice. 1991;5(2):38–41. doi: 10.1097/00004650-199101000-00009. [DOI] [PubMed] [Google Scholar]
- Frank-Stromborg M, Olsen SJ, editors. Instruments for Clinical Health-Care Research. 2nd ed. Sudbury, MA: Jones and Bartlett Publishers; 1997. [Google Scholar]
- Friedman E, Katcher A, Lynch J. Social interaction and blood pressure: Influence of animal companions. JNerv Ment Dis. 1983;171:8. doi: 10.1097/00005053-198308000-00002. [DOI] [PubMed] [Google Scholar]
- Geary H. Facilitating an organizational culture in an Urban Medical Center. Nursing Administration Quarterly. 2003;27(3):231–239. doi: 10.1097/00006216-200307000-00010. [DOI] [PubMed] [Google Scholar]
- Giuliano KK, Bloniasz E, Bell J. Implementation of a pet visitation program in critical care. Critical Care Nurse. 1999;3:43–50. [PubMed] [Google Scholar]
- Crossing the Quality Chasm. National Academies Press; 2001. Institute of Medicine. [PubMed] [Google Scholar]
- Johnson RA. Human-animal interaction research as an area of inquiry in nursing. Western Journal of Nursing Research. 2002;24:713–715. [Google Scholar]
- Johnson RA, Meadows RL, Haubner JS, Sevedge K. Human-animal interaction. A complementary/alternative medical (CAM) intervention for cancer patients. American Behavioral Scientist. 2003;47(1):55–69. [Google Scholar]
- Johnson RA, Meadows RL, Haubner JS, Sevedge K. Animal-assisted activity among patients with cancer: Effects on mood, fatigue, self-perceived health, and sense of coherence. Oncology Nurse Forum. 2008;35(2):225–232. doi: 10.1188/08.ONF.225-232. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Page GG, Marucha PT, MacCallum RC, Glaser R. Psychological influences on surgical recovery. American psychologist. 1998;53(11):1209–1218. doi: 10.1037//0003-066x.53.11.1209. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, McGuire L, Robles TF, Glaser R. Emotions, morbidity and mortality: new perspectives from psychoneuroimmunology. Annual review of psychology. 2002;53:83–107. doi: 10.1146/annurev.psych.53.100901.135217. [DOI] [PubMed] [Google Scholar]
- McCain NL, Gray DP, Walter JM, Robins J. Implementing a comprehensive approach to a study of health dynamics using the psychoneuroimmunology paradigm. Advances in Nursing Science. 2005;28:320–332. doi: 10.1097/00012272-200510000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDowell I, Newell C. Measuring Health: a guide to rating scales and questionnaires. New York, NY: Oxford University Press; 1987. [Google Scholar]
- McNair DM, Heuchert JWP, Shilony E. Profile of Mood States Bibliography 1964–2002. 2003 https://www.mhs.com/ecom/TechBrochures/POMS%20Bibliography.pdf.
- McNair D, Lorr M, Droppleman L. Profile of mood states manual. North Tonawanda, NY: Multi-Health Systems, Inc.; 1992. [Google Scholar]
- National Center for Complementary and Alternative Medicine. Expanding horizons of health care: Strategic plan 2005–2009 executive summary. (n.d.). Retrieved August 7, 2008, from. http://nccam.nih.gov/about/plans/2005/page4.htm.
- National Institute of Nursing Research. NINR Strategic plan 2006 – 2010. (n.d.) Retrieved August 7, 2008, from http://www.ninr.nih.gov/AboutNINR/NINRMissionandStrategicPlan/.
- Pearson S, Maddern GJ, Fitridge R. The role of pre-operative state-anxiety in the determination of intra-operative neuroendocrine responses and recovery. British Journal of Health Psychology. 2005;10(Pt 2):299–310. doi: 10.1348/135910705X26957. [DOI] [PubMed] [Google Scholar]
- Picard C, Jones D, editors. Giving Voice to What We Know. Boston, Ma: Jones & Bartlett; [Google Scholar]
- Releases. Hospital Pulse Report. retrieved 3-18-08 from http://www.reuters.com/artilce/pressRelease/idUS128290+18-Mar-2008+PRN20080318.
- Rogers ME. An introduction to the theoretical basis of nursing. Philadelphia PA: F.A. Davis Co.; 1970. [Google Scholar]
- Sobo EJ, Eng B, Kassity-Krich N. Canine visitation (pet) therapy: pilot data on decreases in child pain perception. Journal of holistic nursing. 2006;1(24):51–57. doi: 10.1177/0898010105280112. [DOI] [PubMed] [Google Scholar]
- Stanley-Hermanns M, Miller J. Animal-assisted therapy. AJN. 2002;102(10):69–76. doi: 10.1097/00000446-200210000-00028. [DOI] [PubMed] [Google Scholar]
- Westchester County Business Journal: Hospitals design stress reduction treatment to speed recovery. April 25, 2005 retrieved 3, 28, 2008 from http://findarticles.com/p/articles/mi_qa5278/is_200504/ai_n224297734/print.
- Whitehead D. Health promoting hospitals: the role and function of nursing. Journal of clinical nursing. 2005;14:20–27. doi: 10.1111/j.1365-2702.2004.01012.x. [DOI] [PubMed] [Google Scholar]
- Wilson CC, Barker SB. Challenges in designing human-animal interaction research. American Behavioral Scientist. 2003;47(1):16–28. [Google Scholar]
- Press Ganey Associates, Inc.; 2008 Hospital Pulse Report: Patient perspectives on American health care. 2008 Retrieved 3-31-09 from: http://www.pressganey.com/galleries/default-file/2008_Hospital_Pulse_Report.pdf.