Abstract
Background:
Urgent débridement of open fractures has been considered to be of paramount importance for the prevention of infection. The purpose of the present study was to evaluate the relationship between the timing of the initial treatment of open fractures and the development of subsequent infection as well as to assess contributing factors.
Methods:
Three hundred and fifteen patients with severe high-energy lower extremity injuries were evaluated at eight level-I trauma centers. Treatment included aggressive débridement, antibiotic administration, fracture stabilization, and timely soft-tissue coverage. The times from injury to admission and operative débridement as well as a wide range of other patient, injury, and treatment-related characteristics that have been postulated to affect the risk of infection within the first three months after injury were studied, and differences between groups were calculated. In addition, multivariate logistic regression models were used to control for the effects of potentially confounding patient, injury, and treatment-related variables.
Results:
Eighty-four patients (27%) had development of an infection within the first three months after the injury. No significant differences were found between patients who had development of an infection and those who did not when the groups were compared with regard to the time from the injury to the first débridement, the time from admission to the first débridement, or the time from the first débridement to soft-tissue coverage. The time between the injury and admission to the definitive trauma treatment center was an independent predictor of the likelihood of infection.
Conclusions:
The time from the injury to operative débridement is not a significant independent predictor of the risk of infection. Timely admission to a definitive trauma treatment center has a significant beneficial influence on the incidence of infection after open high-energy lower extremity trauma.
Level of Evidence:
Prognostic Level II. See Instructions to Authors for a complete description of levels of evidence.
Open fractures routinely are listed among musculoskeletal diagnoses requiring urgent surgical intervention. Prevention of deep infection by means of operative irrigation and débridement within six hours after the injury is a widely accepted standard of care1,2. Although urgent treatment logically is appropriate for open fractures, an arbitrary time window for optimum treatment cannot be justified on the basis of existing medical evidence. Furthermore, early operative intervention often is problematic because of the need to transfer patients with complex injuries to treatment centers with advanced capabilities and because of ongoing resuscitative requirements for multiply injured patients. The purpose of the present study was to evaluate the relationship between the timing of initial treatment and the development of subsequent infection in a cohort of 315 patients with severe open lower extremity fractures that were treated at eight level-I trauma centers.
Materials and Methods
Study Population
The patients in the current analysis constituted a subgroup of a larger study (the Lower Extremity Assessment Project [LEAP]) that was conducted to assess the differences in outcomes between amputation and reconstruction after limb-threatening lower extremity trauma. The primary study was described in detail previously3-5. Patients were eligible for the present study if they were between the ages of sixteen and sixty-nine years and had been admitted to one of eight participating level-I trauma centers for the treatment of limb-threatening lower extremity trauma distal to the femur. Inclusion criteria for the current study were Gustilo Type-IIIB, IIIC, and selected IIIA6 open tibial, ankle, pilon, and foot fractures defined by the treating surgeon as representing limb-threatening injuries. Patients were excluded if they had a Glasgow Coma Scale score of <15 at twenty-one days after hospitalization or discharge7, a spinal cord deficit, previous amputation, or third-degree burn. Patients were also excluded if they had been transferred to the definitive treatment center more than twenty-four hours after the injury, if they did not speak English or Spanish, if they had a documented psychiatric disorder, or if they were on active military duty. The study protocol required the involvement of an attending orthopaedic surgeon during the initial evaluation and treatment of all cases of major limb trauma. All patients were managed with a protocol that included aggressive fracture débridement, antibiotic coverage, fracture stabilization, repeat débridement, and early soft-tissue coverage. Three hundred and fifteen subjects with open tibial, ankle, pilon, and foot fractures that were treated with lower extremity reconstruction met the inclusion criteria. Time to treatment and outcome data were available for 307 patients (97.5%).
Procedures
Patients were enrolled in the study during a forty-month period (from March 1994 through June 1997) and were followed prospectively for a minimum of three months after the injury. Before hospital discharge, patients were assessed by an orthopaedic surgeon and a physical therapist and were interviewed by the study coordinator. At each follow-up examination, the patients were asked to participate in a musculoskeletal evaluation to ascertain the occurrence of complications, including infection. The patients’ medical records were abstracted after initial hospital discharge and after each rehospitalization during the follow-up period. The study was approved by the institutional review boards at the coordinating center and each study site. Informed consent was obtained from all study participants.
Characterizing Patients and Their Injuries
Extensive baseline data were collected regarding patient environment, demographic characteristics, and health habits. These measures have been described previously4. All lower extremity injuries were prospectively classified at the time of admission and were assessed with use of standard classification systems and limb-salvage indices proposed in the literature. For analysis, injuries were summarized according to (1) the type and extent of bone injury according to the Orthopaedic Trauma Association system for the classification of tibial fractures8, the Arbeitsgemeinschaft für Osteosynthesefragen/Association for the Study of Internal Fixation (AO-ASIF) system for the classification of tibial fractures9, the Hannover Fracture Scale10, the Limb Salvage Index11, and the Predictive Salvage Index12; (2) the extent of skin, neurovascular, muscle, and tendon injury according to the AO-ASIF system for the classification of soft-tissue injury of the tibia, the Hannover Fracture Scale, the Limb Salvage Index, and the Predictive Salvage Index; (3) plantar sensation and shock as defined by the Mangled Extremity Severity Score13; and (4) overall open fracture assessment with the use of the Gustilo classification system6. Associated injuries were classified with use of the Abbreviated Injury Scale14 and the Injury Severity Score15; two scores denoting the maximum Abbreviated Injury Scale severity of contralateral and ipsilateral non-amputation-threatening lower extremity injuries also were calculated.
The time of injury, the time of admission to each facility, and transfer times were abstracted from the medical records by a trained study coordinator at each definitive treatment site. At the time of the index operative débridement, the treating orthopaedic surgeon recorded the time of the injury and the time of the operative procedure. The time of soft-tissue coverage also was recorded by the treating orthopaedic surgeon.
Outcome Measures
The primary outcome measure used in the present analysis was the diagnosis of wound infection or osteomyelitis within the first three months after the injury. The diagnosis was made by the treating orthopaedic surgeon either at the scheduled three-month study visit or during inpatient or outpatient visits occurring before the three-month visit. At both time points, surgeons were specifically asked whether a diagnosis of infection was present. For this analysis, we created two outcome variables: (1) any diagnosis of infection, whether treated on an inpatient or outpatient basis (any infection), and (2) a diagnosis of infection or osteomyelitis resulting in rehospitalization (major infection). A patient was defined as having any diagnosis of infection if an infectious complication involving the injury site developed and was treated on either an inpatient or an outpatient basis within the first three months after the injury. Infections not involving the injury site were excluded. External fixator pin-track infections were included only if they involved the open fracture site. Repeat débridements for the treatment of necrosis were not automatically defined as representing an infectious complication unless they were associated with a specific diagnosis of infection by the attending surgeon. When clinically indicated, culture results were assessed by the attending orthopaedic surgeon.
Data Analysis
The primary goal of the analysis was to test the hypothesis that the time to treatment predicts the likelihood of infection after severe lower extremity trauma. The relationships between the two infection outcome measures and four time-to-treatment variables were examined, both at the bivariate level and with use of multivariate logistic regression techniques to adjust for the effects of potential confounders. Significance at the bivariate level was assessed with use of the chi-square and t tests. The results of multivariate logistic regression are presented as odds ratios with p values. Model selection was guided by the results of bivariate analyses and previous analyses16. Covariates with a significance level of p < 0.2 and those whose removal changed the magnitude of the remaining regression coefficients were retained in the model. Because two outcome measures were tested against four hypothesized predictors, a Bonferroni-adjusted significance level of 0.00625 was calculated to account for the increased possibility of a type-I error. For the outcome of “All Infections,” the study was powered at 0.8 to detect differences in infection rates of ≥17%. For the outcome of “Major Infections,” the study was powered at 0.8 to detect differences in infection rates of ≥13%.
All p values reported as p < 0.01 also met this more conservative significance criterion.
Source of Funding
Funding for the original LEAP study was provided through a grant from the National Institutes of Health—National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS R01-AR42659). Funds from this grant were used to support costs associated with investigator time, data collection, and data analysis. No additional funding was provided for this particular sub-analysis of the LEAP study.
Results
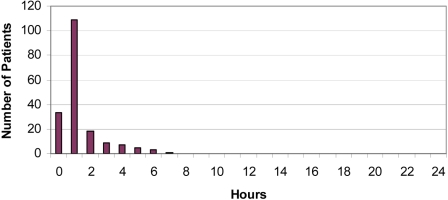
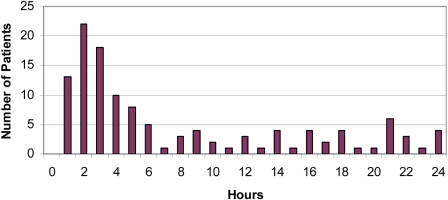
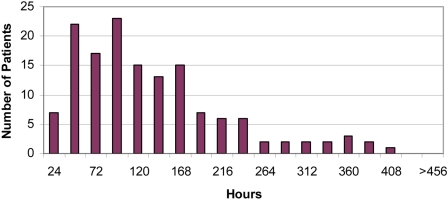
All patients who were admitted directly from the scene of injury to the definitive trauma treatment center were admitted within eight hours after the injury (Fig. 1-A). Patients who were transferred to the definitive trauma treatment center from another hospital arrived at variable times within the first twenty-four hours after the injury (Fig. 1-B).
Fig. 1-A Fig. 1-B.
Figs. 1-A and 1-B Bar graphs illustrating the time from injury to admission for the group of patients who were admitted directly to the definitive trauma treatment center (Fig. 1-A) and the group of patients who were transferred to the definitive trauma treatment center (Fig. 1-B). The mean time (and standard deviation) was 3.9 ± 5.7 hours for the overall group (n = 307), 1.4 ± 1.3 hours for the direct group (n = 185), and 7.9 ± 7.2 hours for the transfer group (n = 122). The difference between the direct and transfer groups was significant (p < 0.0001).
Three hundred and seven patients with high-energy lower extremity trauma met the inclusion criteria. On bivariate analyses, the patients with and without infection did not differ with regard to age, sex, insurance status, level of education, poverty status, smoking status, or number of comorbidities. Among patients who had development of a major infection, bivariate analyses demonstrated significant differences (p < 0.01) in infection rates for those with >2 cm of bone loss. In addition, patients with Gustilo Type-IIIC tibial fractures were significantly (p < 0.01) more likely to have development of infection than those with Gustilo Type-IIIA or IIIB tibial fractures, although no differences were observed in the rate of major infection.
In comparisons of other injury characteristics of the study population, including the degree of nerve damage, muscle damage, relative size of the skin defect, Injury Severity Score, and the surgeon's perception of the degree of contamination, bivariate analyses revealed no significant differences between the group that eventually had development of infection and the group that did not.
When the study populations were compared on the basis of treatment characteristics, patients who were managed with intramedullary nail fixation were less likely to have development of infection than those who were managed with external fixation or a plate (p < 0.1). There were no other significant differences between the patients with and without infection when the groups were compared on the basis of treatment characteristics.
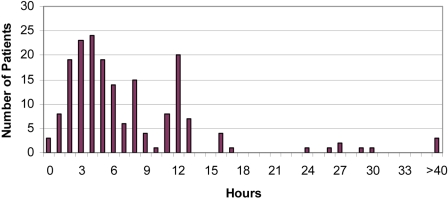
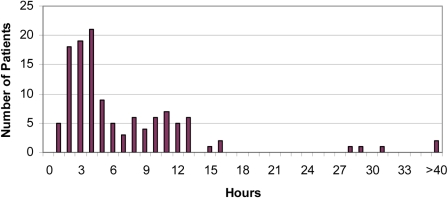
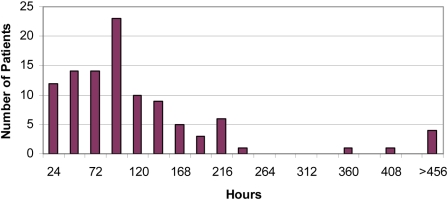
An evaluation of the risk of development of any type of infection (major or minor) showed that time from injury to admission to the definitive trauma treatment center was a significant predictor of the likelihood that infection would develop (Table I). Time from injury to débridement and time from admission to débridement (Figs. 2-A and 2-B) were evaluated separately. Although the range of time from injury to débridement in the present series was fairly narrow (with most injuries being treated with operative débridement within twenty-four hours after occurrence), within the context of that limitation, no significant difference was observed in terms of the mean time to débridement between the group of patients who had development of infection and the group of patients who did not (Table II). Similarly, the time from initial débridement to eventual soft-tissue coverage (Figs. 3-A and 3-B) was not an independent predictor of the development of infection on either multivariate or bivariate analysis.
TABLE I.
Time to Treatment and Risk of Infection
| Time*(hr) |
|||||
| N | From Injury to Admission | From Admission to Débridement | From Injury to Débridement | From Débridement to Soft-Tissue Coverage | |
| All infections | |||||
| Present | 84 | 5.2 ± 6.5† | 6.5 ± 6.3 | 11.6 ± 9.3 | 117.8 ± 89.6 |
| Absent | 223 | 3.5 ± 5.2 | 8.0 ± 9.6 | 11.5 ± 10.6 | 131.1 ± 121.8 |
| Major infections | |||||
| Present | 50 | 6.2 ± 7.5† | 7.3 ± 7.4 | 13.5 ± 10.6 | 106.3 ± 79.8 |
| Absent | 257 | 3.5 ± 5.1 | 7.7 ± 9.1 | 11.2 ± 10.1 | 137.2 ± 118.4 |
The values are given as the mean and the standard deviation.
P < 0.01, t test.
Fig. 2-A Fig. 2-B.
Figs. 2-A and 2-B Bar graphs illustrating the time from admission to first débridement for the group of patients who were admitted directly to the definitive trauma treatment center (Fig. 2-A) and the group of patients who were transferred to the definitive trauma treatment center (Fig. 2-B). The mean time (and standard deviation) was 7.6 ± 8.8 hours for the overall group (n = 307), 7.8 ± 8.9 hours for the direct group (n = 185), and 7.3 ± 8.7 hours for the transfer group (n = 122). The difference between the direct and transfer groups was not significant (p = 0.60).
TABLE II.
Time from Injury to Débridement and Risk of Infection*
| Time from Injury to Débridement | N | Percentage with Infection | Percentage with Major Infection |
| <5 hr | 93 | 28.0 | 15.1 |
| 5 to 10 hr | 86 | 29.1 | 14.0 |
| >10 hr | 128 | 25.8 | 18.8 |
No significant differences were detected at the p < 0.05 level.
Fig. 3-A Fig. 3-B.
Figs. 3-A and 3-B Bar graphs illustrating the time from débridement to soft-tissue coverage in the group of patients admitted directly to the definitive trauma treatment center (Fig. 3-A) and the group of patients transferred to the definitive trauma treatment center (Fig. 3-B). The mean time (and standard deviation) was 127.2 ± 113.3 hours for the overall group (n = 307), 129.1 ± 85.8 hours for the direct group (n = 185), and 124.6 ± 143.8 hours for the transfer group (n = 122). The difference between the direct and transfer groups was not significant (p = 0.75).
Table III examines the influence of prolonged prehospital time and the effect of prolonged time at the initial hospitals before transfer to definitive trauma treatment centers. Among patients who were primarily admitted to a definitive trauma treatment center, those for whom the time at the scene or in transit was prolonged (more than two hours from the time of injury to admission) were significantly more likely to have development of infection than those for whom the time from injury to admission was two hours or less (56% compared with 20%, respectively, for all infections and 30% compared with 11%, respectively, for major infections; p < 0.01). Multivariate regression modeling of the likelihood of infection, performed to control for additional patient, injury, and treatment-related variables, showed that patients who were admitted directly to a definitive trauma treatment center more than two hours after the injury were 5.4 times more likely to have development of infection and 3.1 times more likely to have development of major infection (p < 0.01) as compared with those who were admitted to the definitive trauma treatment center within two hours after the injury (Table IV). Patients who were transferred from the initial receiving institutions to the definitive trauma treatment center within three hours after the original injury were significantly less likely to have development of infection than those who were transferred eleven to twenty-four hours after the injury (Table III). This result also remained true with similar multivariate regression modeling (Table IV).
TABLE III.
Time from Injury to Admission and Risk of Infection
| N | Percentage with Infection | Percentage with Major Infection | |
| Patients admitted directly to trauma center | |||
| ≤2 hr | 142 | 20.4 | 11.3 |
| >2 hr | 43 | 55.8* | 30.2* |
| Patients transferred to trauma center | |||
| 1 to 3 hr | 53 | 17.0 | 13.2 |
| 4 to 10 hr | 33 | 27.3 | 12.1 |
| 11 to 24 hr | 36 | 36.1† | 27.8† |
The risks of infection and major infection were significantly higher for patients for whom the time at the scene or in transit was prolonged (more than two hours from the time of injury to admission) as compared with those for whom the time from injury to admission was two hours or less (p < 0.01, chi-square test).
The risks of infection and major infection were significantly higher in the eleven-to-twenty-four-hour group as compared with the one-to-three-hour group (p < 0.05, chi-square test of homogeneity).
TABLE IV.
Multivariate Regression Model of Likelihood of Infection
| All Infections |
Major Infections |
|||
| Unadjusted* | Adjusted† | Unadjusted* | Adjusted† | |
| Patients admitted directly to trauma center | ||||
| ≤2 hr | Reference | Reference | Reference | Reference |
| >2 hr | 4.3‡ | 5.4‡ (2.5 to 11.5) | 2.7‡ | 3.1‡ (1.4 to 7.0) |
| Patients transferred to trauma center | ||||
| 1 to 3 hr | Reference | Reference | Reference | Reference |
| 4 to 10 hr | 1.1 | 1.5 (0.6 to 3.6) | 0.8 | 0.9 (0.3 to 3.1) |
| 11 to 24 hr | 1.6§ | 1.9§ (0.9 to 4.3) | 2.2§ | 2.6‡ (1.1 to 6.2) |
| Bone loss | ||||
| ≤2 cm | Reference | Reference | Reference | Reference |
| >2 cm | 2.2§ | 1.7§ (0.8 to 3.7) | 3.3‡ | 3.0‡ (1.3 to 6.5) |
| Tibial fracture | ||||
| Grade IIIA/B | Reference | Reference | Reference | Reference |
| Grade IIIC | 2.8‡ | 1.9‡ (1.0 to 6.3) | 1.4 | 1.5 (0.4 to 4.7) |
| Compartment syndrome | ||||
| Absent | Reference | Reference | Reference | Reference |
| Present | 2.0§ | 1.7§ (1.1 to 7.3) | 1.7 | 1.5 (0.4 to 5.3) |
| Fixation device | ||||
| Nail | Reference | Reference | Reference | Reference |
| External fixator/plate | 2.3§ | 1.6§ (1.1 to 3.0) | 2.2§ | 2.0§ (0.8 to 4.9) |
| Education | ||||
| No college | Reference | Reference | Reference | Reference |
| Some college | 0.6§ | 0.7 (0.3 to 1.2) | 0.7 | 0.8 (0.4 to 1.8) |
| Smoking | ||||
| Nonsmoker | Reference | Reference | Reference | Reference |
| Smoker | 1.7§ | 1.7§ (0.8 to 3.3) | 1.7 | 1.5 (0.6 to 3.4) |
The values are given as odds ratios.
The values are given as odds ratios, with 95% confidence intervals in parentheses.
p < 0.01.
p < 0.1.
Discussion
The time from the injury to the initial operative débridement was not a significant independent predictor of the risk of infection in this patient population; however, this finding should not be interpreted as an argument that operative débridement of open fractures should not be accomplished urgently. At the time that the patients were recruited into the present study, it was the treatment standard among the institutions involved to proceed with operative débridement of high-energy lower extremity injuries as safely and expeditiously as possible within the context of the patient's overall physiological condition. Therefore, no control group of patients with severe high-energy lower extremity trauma who were admitted to the definitive trauma treatment center underwent delayed débridement of open fractures because of surgeon or institutional convenience. Similarly, the results do not indicate that emergent débridement of open fractures reduces the risk of infection. Although many authors have declared débridement of open fractures to be an orthopaedic emergency, this declaration seems to be based on theory and minimal data. The results of the present study suggest that the components of treatment associated with admission to a definitive trauma treatment center are at least as critical as the time to operative débridement with regard to the risk of development of an infection.
In the present study, we included a mixed group of tibial and foot injuries because it often is difficult for field providers to ascertain the exact location of high-energy lower extremity injury. Often, the zone of injury extends from the foot through the lower extremity. Field providers often are faced with a question of whether to transport a patient with an isolated high-energy lower extremity injury to a trauma center that is capable of extensive limb-salvage surgery or to a local facility. The present study suggests that complication rates, at least in terms of the rate of infection, were higher when patients were first admitted to a center that did not definitively treat the open lower extremity injury and when patients remained at the initial treatment center for eleven hours or more than they were when patients were transferred sooner or when they arrived at the definitive treatment center directly from the scene of the injury within two hours after the injury.
A very large difference in infection rates was shown between patients who were admitted directly to a trauma center from the scene of the injury more than two hours after the injury and those who were admitted directly to a trauma center from the scene of injury within two hours after the injury, which possibly indicates that prolonged out-of-hospital time is associated with higher infection rates. The reasons for the prolonged time from the injury to the initial admission to the hospital require additional investigation. It is possible that the delayed patients were entrapped for a prolonged period of time. It also is possible that the prolonged period of time represents a marker of increased injury severity. Patients whose limbs were crushed or otherwise pinned as a result of the index trauma might have been more likely to sustain an infection than those whose lower extremity injuries were more rapidly mobilized. It also is possible that being in an ambulance in a less stable environment outside the hospital increases the propensity for infection. Finally, it is possible that the degree to which fluid resuscitation and the administration of antibiotics occur outside the hospital is less than the degree to which they are accomplished within the hospital and that patients who were admitted to the trauma center directly from the scene more than two hours after the injury were unlikely to receive prehospital care that was comparable with the hospital care received by the group admitted earlier.
The data indicate that patients who were transferred to the trauma center one to three hours after admission to the initial hospital had a trend toward lower infection rates than those who were transferred four to ten hours after admission to the outside institution and significantly lower infection rates than those transferred to definitive trauma treatment centers eleven to twenty-four hours after the index injury. Regression modeling suggested that the differences were not related to the severity of injury, patient characteristics, or treatment characteristics. This finding strongly suggests that, if transfer to an institution capable of extensive limb-salvage surgery is deemed necessary for the definitive treatment of a high-energy lower extremity fracture, such transfer should be expedited. In most cases in which patients were transferred, we do not know the exact time of admission to the original hospital because that information was not included in the original data set extracted from the medical records. It is possible that for patients who were transferred to the definitive treatment facility, delay in arrival at the initial treatment hospital was also predictive of infection.
The overall reported infection rate in the present series (27%) was high compared with those in some other series of open fractures reported in the literature17-19. We believe that this infection rate was higher than those seen in some other series for several reasons. First, our definition of infection was intentionally broad. Our purpose was to determine whether the timing of treatment was important in predicting the risk of infection. We thus sought to be more inclusive in order to avoid missing an effect of timing on the risk of infections not postulated to be deep. Second, we believe that the level of injury severity in the present study was higher than that in other studies. Direct comparison of injury severity between published series in the literature is difficult, making this hypothesis difficult to test; however, the LEAP study was designed to examine outcomes primarily in the subset of patients with high-energy lower extremity trauma for whom amputation was a serious treatment consideration.
Because the present analysis specifically addresses the question of the role of time from injury to treatment as a risk factor for the development of a complication, the accuracy of the data regarding the time of injury is of importance. Information about time of injury was recorded by the treating surgeon at the time of the initial operative treatment of the fracture. While it is possible that errors occasionally occurred in determining the time of injury, it seems unlikely that any consistent source of error associated with any bias was present. It is also likely that this information is relatively accurate relative to that in other studies in the literature addressing the timing of operative treatment of open fractures as our information was collected prospectively. Information about the time of admission to the initial treatment facilities and to the definitive treatment facilities was also likely accurate given that it was extracted directly from the medical records from the individual hospitals involved. Cases were excluded from the final analysis if reliable data were not available (with only eight cases [2.5%] being excluded overall).
The diagnosis of infection in this patient population was necessarily subjective in certain situations. For this reason, we erred on the side of inclusion by considering even diagnoses that were only potentially related to the timing of treatment, such as pin-track infections involving the open fracture wound, to be in the study group. It is possible that such infections were primarily pin-track infections and that the open fracture wound became involved only secondarily. Another inherent weakness is that we were unable to determine when serial operative débridements were necessitated by infection as opposed to progressive tissue necrosis. We relied on the prospectively recorded opinion of the treating surgeon in making this determination. The strength of these data is that the surgeon was specifically questioned as to whether or not he or she thought that infection was present. The weakness is that the data on which the surgeon relied in making this determination were inconsistent.
It also is possible that the administration of antibiotics occurred earlier when patients were admitted directly to the definitive trauma treatment center. Unfortunately, information about the timing of administration of prophylactic antibiotics was not included in the data collection during the initial LEAP study. It also was not possible for us to reliably retrieve this information retrospectively. This represents a major limitation of the current study and eliminates our ability to determine the effect of the time from the injury to antibiotic administration on the risk of infection in this population. We believe that prospective study of the relationship between the time of injury, the time of antibiotic administration, the time of surgical débridement, and the risk of infection is warranted to help surgeons better understand the importance of decisions about the timing of treatment in mitigating the risk of infection after severe high-energy lower extremity fractures.
Several of the findings in the present study are consistent with the widely held belief that injury severity is an important predictor of the risk of infection. Patients with compartment syndrome and those with >2 cm of bone loss had an increased risk of infection. Both compartment syndrome and nerve injury are likely markers of injury severity. The present study should not be interpreted to indicate that injury severity is unimportant. Rather, our data indicate that, after controlling for injury severity, the time from the injury to the arrival at the definitive treatment center is an important independent risk factor whereas the time from the injury to the arrival in the operating room is not. In addition, it is possible that fewer inspections of the wound were performed before operative intervention when patients were admitted directly to the definitive trauma treatment center. However, this by itself does not necessarily explain why a patient who had a short stay at an interim institution fared better than a patient who had a prolonged stay. It is also possible that another variable associated with arrival at the definitive treatment center, such as resuscitation, contributes to the mitigation of the risk of infection. Determining whether fewer wound inspections or improved resuscitation or whether another yet unapparent factor associated with arrival at the definitive treatment facility is responsible for this effect is beyond the scope of the present study but likely warrants additional investigation.
These data indicate that rapid transfer to a trauma center that is capable of definitively treating severe high-energy lower extremity injuries might be associated with the possibility of decreasing infection rates after injury. This effect seems to be independent of any effect on time from the injury to the surgical débridement of the open fracture. The results of the present study suggest that prospective evaluation that allows better investigation of the potential confounding effects of variables such as the time from injury to antibiotic administration and the time from injury to completion of resuscitation is warranted. If the results of the current investigation were to be confirmed, the findings would seem to support development of protocols for Emergency Medical Service field providers dictating that patients with high-energy lower extremity open injuries should be transferred expeditiously from the scene of the injury to a center capable of definitive treatment of the injuries whenever feasible.
Supplementary Material
Footnotes
Disclosure: In support of their research for or preparation of this work, one or more of the authors received, in any one year, outside funding or grants in excess of $10,000 from the National Institutes of Health—National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS R01-AR42659). Neither they nor a member of their immediate families received payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity in direct or indirect support of this work.
References
- 1.Pollak AN. Timing of débridement of open fractures. J Am Acad Orthop Surg. 2006;14(10 Spec No.):S48-51 [DOI] [PubMed] [Google Scholar]
- 2.Werner CM, Pierpont Y, Pollak AN. The urgency of surgical debridement in the management of open fractures. J Am Acad Orthop Surg. 2008;16:369-75 [DOI] [PubMed] [Google Scholar]
- 3.Bosse MJ, MacKenzie EJ, Kellam JF, Burgess AR, Webb LX, Swiontkowski MF, Sanders RW, Jones AL, McAndrew MP, Patterson BM, McCarthy ML, Travison TG, Castillo RC. An analysis of outcomes of reconstruction or amputation after leg-threatening injuries. N Engl J Med. 2002;347:1924-31 [DOI] [PubMed] [Google Scholar]
- 4.MacKenzie EJ, Bosse MJ, Kellam JF, Burgess AR, Webb LX, Swiontkowski MF, Sanders RW, Jones AL, McAndrew MP, Patterson TM, McCarthy ML. Characterization of patients with high-energy lower extremity trauma. J Orthop Trauma. 2000;14:455-66 [DOI] [PubMed] [Google Scholar]
- 5.MacKenzie EJ, Bosse MJ, Kellam JF, Burgess AR, Webb LX, Swiontkowski MF, Sanders R, Jones AL, McAndrew MP, Patterson B, McCarthy ML, Rohde CA, LEAP Study Group Factors influencing the decision to amputate or reconstruct after high-energy lower extremity trauma. J Trauma. 2002;52:641-9 [DOI] [PubMed] [Google Scholar]
- 6.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24:742-6 [DOI] [PubMed] [Google Scholar]
- 7.Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81-4 [DOI] [PubMed] [Google Scholar]
- 8.Orthopaedic Trauma Association Committee for Coding and Classification Fracture and dislocation compendium. J Orthop Trauma. 1996;10Suppl 1:v-ix, 1-154 [PubMed] [Google Scholar]
- 9.Muller ME, Allgower M, Schneider R, Willenegger H. Manual of internal fixation: techniques recommended by the AO-ASIF Group. New York: Springer; 1991 [Google Scholar]
- 10.Suedkamp NP, Barbey N, Veuskens A, Tempka A, Haas NP, Hoffmann R, Tscherne H. The incidence of osteitis in open fractures: an analysis of 948 open fractures (a review of the Hannover experience). J Orthop Trauma. 1993;7:473-82 [DOI] [PubMed] [Google Scholar]
- 11.Russell WL, Sailors DM, Whittle TB, Fisher DF, Jr, Burns RP. Limb salvage versus traumatic amputation: a decision based on a seven-part predictive index. Ann Surg. 1991;213:473-81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Howe HR, Jr, Poole GV, Jr, Hansen KJ, Clark T, Plonk GW, Koman LA, Pennell TC. Salvage of lower extremities following combined orthopedic and vascular trauma. A predictive salvage index. Am Surg. 1987;53:205-8 [PubMed] [Google Scholar]
- 13.Johansen K, Daines M, Howey T, Helfet D, Hansen ST., Jr Objective criteria accurately predict amputation following lower extremity trauma. J Trauma. 1990;30:568-73 [DOI] [PubMed] [Google Scholar]
- 14.Association for the Advancement of Automotive Medicine The Abbreviated Injury Scale: 1990 revision. Des Plaines, IL: Association for the Advancement of Automotive Medicine; 1990 [Google Scholar]
- 15.Baker SP, O'Neill B, Haddon W, Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187-96 [PubMed] [Google Scholar]
- 16.Castillo RC, Bosse MJ, MacKenzie EJ, Patterson BM, LEAP Study Group Impact of smoking on fracture healing and risk of complications in limb-threatening open tibia fractures. J Orthop Trauma. 2005;19:151-7 [DOI] [PubMed] [Google Scholar]
- 17.Naique SB, Pearse M, Nanchahal J. Management of severe open tibial fractures: the need for combined orthopaedic and plastic surgical treatment in specialized centers. J Bone Joint Surg Br. 2006;88:351-7 [DOI] [PubMed] [Google Scholar]
- 18.Patzakis MJ, Bains RS, Lee J, Shepherd L, Singer G, Ressler R, Harvey F, Holtom P. Prospective, randomized, double-blind study comparing single-agent antibiotic therapy, ciprofloxacin, to combination antibiotic therapy in open fracture wounds. J Orthop Trauma. 2000;14:529-33 [DOI] [PubMed] [Google Scholar]
- 19.Keeling JJ, Gwinn DE, Tintle SM, Andersen RC, McGuigan FX. Short-term outcomes of severe open wartime tibial fractures treated with ring external fixation. J Bone Joint Surg Am. 2008;90:2643-51 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.