Stakes are high if nonadherence with biologics results in poor outcomes. Are adherence interventions in order?
Abstract
The full benefit of biologic therapies isn’t reached and quality of life is compromised if patients don’t adhere to their medication regimen. Are adherence interventions in order?
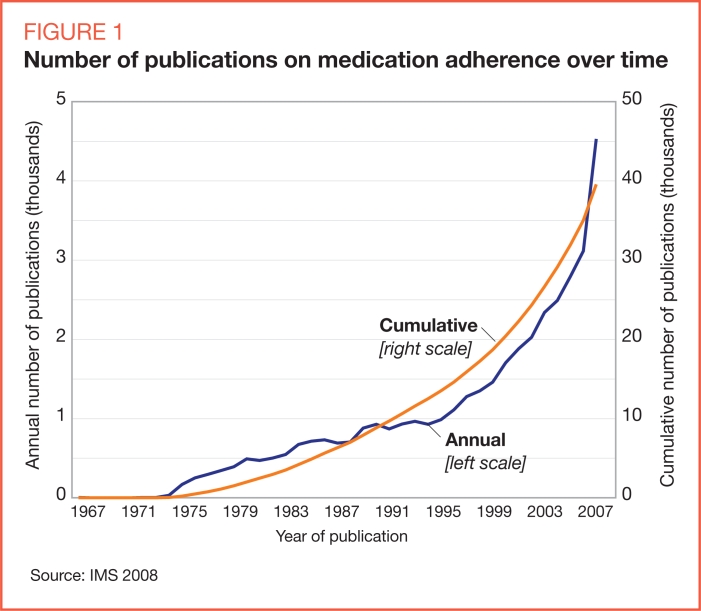
Medication adherence is defined as the level or range of compliance with the provider’s recommended frequency, timing, and dosage of medications (Cramer 2008). The interest in medication adherence, as evidenced by the increase in scientific papers searchable via PubMed, has grown dramatically over the past 10 years (Figure 1).
FIGURE 1.
Number of publications on medication adherence over time
Source: IMS 2008
According to Joshua Benner, PharmD, ScD, research director at the Engelberg Center for Health Care Reform at the Brookings Institution, in Washington, the fact that patient adherence is addressed by almost 40,000 articles in the literature — most of which have been contributed in the past 10–12 years — is a strong indicator of the importance of this topic in the healthcare system (Goldberg 2008).
Poor medication adherence presents a significant global problem. A 2003 World Health Organization (WHO) report found that global medication adherence among patients with chronic diseases averages 50 percent, and that the impact of poor adherence increases as the level of chronic disease increases. The report also notes that nonadherence is a leading cause of preventable morbidity, mortality, and cost (WHO 2003).
Before adherence can be improved, the factors that influence medication-taking behavior must be understood. A recent review on adherence found that predictors of poor adherence include: presence of mental health issues (especially depression); treatment of asymptomatic disease; lack of belief in treatment benefit; poor patient/provider relationship; complex treatment regimen; and high medication costs and/or copayments (Osterberg 2005).
Patient-reported reasons for non-adherence also provide insight as to why patients discontinue or take medications incorrectly. Although forgetfulness is a commonly reported reason, some patients make a conscious decision to skip or omit doses (Osterberg 2005). Patients report nonadherence due to cost, lack of information, and fear of perceived long- or short-term side effects (WHO 2003, Osterberg 2005). Other studies cite poor drug efficacy, patient perception that a medication does not work as well as expected, a dislike of taking medications on a long-term basis, and patient uncertainty about the need for treatment as predominant patient-reported reasons for discontinuation (Simons 1996, Brubaker 2006). Although recent research of patient-reported reasons for non-adherence is limited and the list above is not exhaustive, these examples touch on many of the common barriers to adherence.
The consequences of poor medication adherence are substantial, as this contributes to 33 to 69 percent of hospital admissions in the United States, at a cost of almost $100 billion annually (Osterberg 2005). In addition, medication nonadherence has been demonstrated to cause up to 40 percent of admissions to U.S. nursing homes (Medication Digest 2003). These statistics are particularly important for employers as they pay for medication nonadherence in the form of decreased worker productivity, absenteeism, and rising costs for all health insurance benefits, a large component of which is dependent on the cost of biologics. Given employers’ level of investment in this area, ensuring that patients adhere to prescribed medication regimens is of paramount importance.
BIOLOGICS: THE ROLE OF MEDICATION ADHERENCE
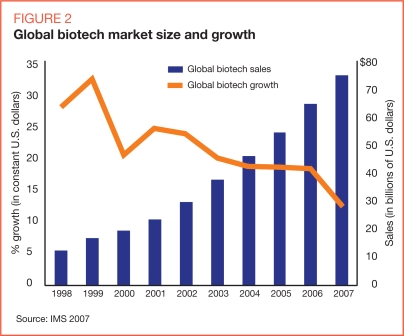
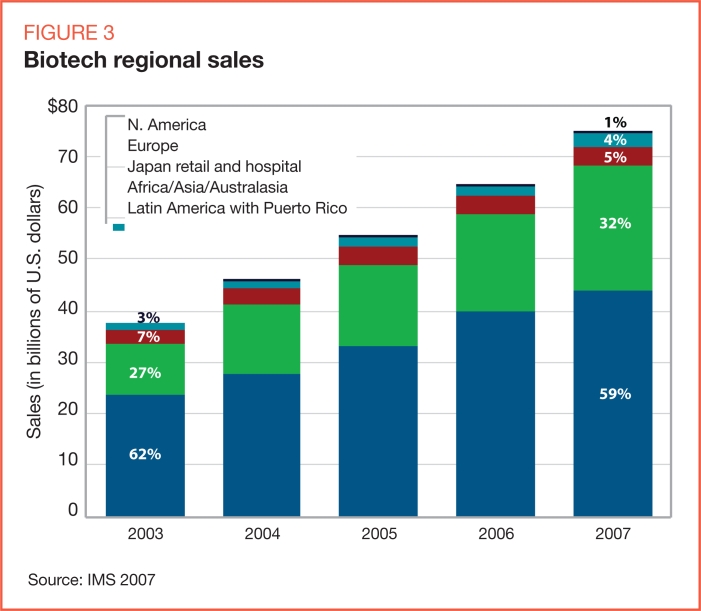
The global demand for biologics to treat patients across a number of disease areas resulted in a $75 billion biotechnology market in 2007 (Figure 2). The impact of biologics on the medical and pharmacy budgets of managed care organizations is evident in the United States, where managed care decision makers are bracing for the next wave of biotechnology products to enter the marketplace (Figure 3).
FIGURE 2.
Global biotech market size and growth
Source: IMS 2007
FIGURE 3.
Biotech regional sales
Source: IMS 2007
Given the high price tags of many biologics, U.S. purchasers — payers and employers — are beginning to demand that biotechnology manufacturers justify the value of their therapies based on rigorous health economic and pharmacoeconomic analysis. However, once the value of a biologic is determined, demonstrated, and communicated, the need to ensure that patients adhere to the therapeutic regimen often is forgotten, despite the financial investment purchasers have made to achieve and realize the potential clinical outcomes.
Although adherence issues with small-molecule oral medications have been widely studied and published, adherence with biologics is just beginning to gain traction in the literature. Early interest has focused on the potentially adverse impact of high patient out-of-pocket costs for biologics on adherence, persistence, and outcomes. It is difficult to generalize adherence lessons learned from oral medications to biologic therapies, because the diverse administration methods for biologics influence how adherence is interpreted and measured (Curkendall 2008). Some biologics require a physician’s visit for distribution, while others are obtained through traditional retail channels and self-administered, similar to oral medications (Goldman 2006). Despite these differences, Benner, of the Brookings Institution, notes that increasing adherence to biologics requires the same attention to patient motivation, education, and barriers as improving adherence to small-molecule pharmaceuticals (Gold-berg 2008).
In a biologics study that excluded physician-administered agents, the probability that a patient would remain on therapy at the end of 1 year dropped from 57 percent for patients with out-of-pocket costs below $50 per week to 32 percent for those who paid more than $50 per week (Hom 2008). This finding suggests that higher copayments may result in a lower likelihood of use by patients who are appropriate candidates for biotech therapies.
However, other research has cast doubt on the link between patient costs and biologic adherence. One study found that coinsurance did not significantly affect the level of spending once a patient initiated biologic use (Goldman 2006). Therefore, although studies of oral medications have shown a small but consistent decrease in adherence when cost sharing increases, uncertainty remains as to whether research on biologics will show the same findings (Goldman 2006).
Nonadherence in the workplace can have substantial financial and clinical implications. Pitney Bowes’ method of providing healthcare to its employees is often cited as an example of how to improve adherence. The company’s services are based upon a model whereby the employer places target chronic disease medications in the most affordable tier as a means for improving adherence (Hom 2008). Nonadherence in the workplace can have financial and clinical implications.
IMPACT IN THE WORKPLACE
Better medication adherence is associated with improved long-term clinical outcomes for chronic conditions (WHO 2003); similarly, poor medication adherence has the potential to result in a significant decrease in worker productivity and increased employer costs. For example, specific consequences of nonadherence can be seen in three chronic conditions commonly treated with biologics: rheumatoid arthritis (RA), HIV, and cancer.
Among those with RA, work disability occurs in 22 to 44 percent of all cases, often shortly after diagnosis (Doeglas 1995, Backman 2004). In a review of RA-related productivity, a median of 66 percent of employees with RA missed work time, resulting in a median of 39 workdays lost (Burton 2006). In 2003, average total healthcare costs (medical, absenteeism, and short-term disability costs) for workers with RA were estimated to be $4,000 higher per worker than for those without RA (Ozminkowski 2006).
HIV patients treated with highly active antiretroviral therapy must achieve at least 95 percent adherence to maintain virologic suppression (Chesney 2003). Yet a recent review noted that only 30 percent of patients attained such a level (Rueda 2006). As a result, nonadherent HIV patients are at high risk of therapeutic failure and development of drug resistance, which can lead to as expensive tests to identify next treatment steps (Scalera 2002). Nonadherence to HIV regimens also results in such indirect costs as loss of productivity, use of support services, disability benefits, and cost of impaired quality of life (Scalera 2002).
Cancer also causes workplace limitations. A MacArthur Foundation study titled Midlife Development in the United States, a large-scale, nationally representative survey of adults, provided insight into the effects of chronic conditions on work impairment. Researchers found that those with cancer had the highest reported prevalence of impairment and the highest number of work-loss days (defined as being unable to work or perform normal activities due to health problems) in the previous 30 days, compared with all other chronic conditions (Kessler 2001).
These three conditions result in a significant burden on healthcare and productivity costs, the scope of which may be partially attributable to documented gaps in medication adherence. Consequently, their total cost highlights the need for purchasers to consider investing in adherence interventions for biologics. The costs of these programs could be offset by associated decreases in healthcare resource use and higher productivity. However, implementing a successful adherence intervention is not an easy task. The following section describes the difficulties of developing successful adherence interventions for biologics, some of which carry challenges that are similar to those faced during the launch of oral medication adherence programs.
AN APPROACH TO INTERVENTIONS
The medical literature on adherence interventions is filled with evaluations of specific tactics for improving adherence, but as a recent Cochrane review noted, these evaluations lack enough consistency to permit a true quantitative analysis of their effectiveness (Haynes 2008). Not surprisingly, this analysis found that tactic-based interventions had inconsistent effectiveness across studies and clinical conditions. For example, although early telephone contact by pharmacists has been shown to increase short-term adherence to biologic therapies for RA (Clifford 2006, Elliott 2008), no current evidence exists to suggest that this effect would persist for other biologic therapies (or even the same therapies for other indications).
Another finding of the Cochrane review was that multifactorial, long-term interventions tend to have more substantial effects on improving adherence than do short-term interventions (Haynes 2008). This finding was reflected in a modeling study that compared the costs and benefits of various adherence interventions for lipid-lowering therapy. Those interventions with the greatest intensity, such as a brick-and-mortar lipid clinic, or those with the most components, such as pharmacist calls, refill reminders, and mailed education materials, tended to be the most cost-effective (Benner 2002). However, it is difficult to untangle what aspects of multimodal interventions actually are responsible for adherence gains.
Several reviews of adherence interventions have focused on the strategic attributes of successful interventions rather than the specific tactics that they employ (McDonald 2002, Newell 1999, Roter 1998). Strategies associated with successful adherence interventions include: delivering persuasive messages from a source or person trusted by the patient; tailoring messages to the patient’s circumstances and attitudes; continuing to describe the medical need for the treatment; setting appropriate outcome expectations; segmenting that portion of the target population most likely to respond to interventions; and rewarding both the initiation of treatment and its maintenance over time.
These attributes are not accidental; they are consistent with some of the leading theories of health behavior change. Numerous theories have informed medication adherence interventions, but the Trans-theoretical Model (TTM) (Prochaska 1983, Prochaska 1997) and the Health Belief Model (HBM) are among the most frequently cited (Rosenstock 1966, Becker 1974). Both models have been updated to reflect a construct called “self-efficacy” from social learning theory (Bandura 1977, DiClemente 1985, Rosenstock 1988).
Three principles drawn from these theories may hold the greatest promise for improving the return on investment (ROI) for biologics adherence interventions. TTM proposes that patients move through several motivational stages on the way to adopting and maintaining new health behaviors. The model suggests that interventions will be most effective when they probe for a patient’s current motivational stage and deliver messages appropriate for reaching the next stage. HBM suggests that evaluating and correcting patients’ perceived risk of adverse health outcomes from non-adherence maximizes their motivation to continue treatment. Finally, social learning theory posits that motivation can be increased through assessment of a patient’s belief as to whether the prescribed treatment can be completed. The key to all of these principles is that interventions cannot be successful without continuous collection and use of feedback from the patients targeted by the intervention.
FACTORS TO CONSIDER
Asking patients who recently discontinued medications about reasons for doing so can provide significant advantages in the development of adherence interventions. The following questions may provide valuable insight when designing messages to overcome specific motivational barriers to adherence:
Do you believe that your condition is serious enough to warrant taking the prescribed injectable medication?
Do you understand and agree with your healthcare provider’s stated rationale for prescribing the injectable medication?
How often do you worry that your condition may require you to take an injectable medication for the rest of your life?
Explicit questions like these are likely to accelerate the development of theory-based interventions that increase the adherence-related returns of biologic therapies.
CONCLUSION
Purchasers face significant challenges when managing healthcare costs, and biologic therapies may seem to require focused and aggressive cost containment. However, there is substantial reason to believe that some patients miss the full benefit of biologic treatments because of nonadherence. The consequences are likely to mirror the increased morbidity, mortality, healthcare costs, and productivity losses observed among patients taking oral medications where poor adherence is documented. Although the science behind adherence is still young, basic and well-tested principles can be used to develop adherence interventions customized for specific patient populations using biologics. Well-designed interventions can earn employers and payers a significant return on investment through reduced healthcare costs and increased productivity.
Footnotes
Disclosures
Erica L. Goldberg, Mitch DeKoven, MHSA, Vernon F. Schabert, PhD, and Katharine Coyle report that they have no financial arrangements or affiliations with manufacturers or products mentioned in this article.
REFERENCES
- Backman CL. Employment and work disability in rheumatoid arthritis. Curr Opin Rheumatol. 2004;16:148–152. doi: 10.1097/00002281-200403000-00014. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Becker MH, editor. The health belief model and personal health behavior. Thorofare, N.J.: Slack; 1974. [Google Scholar]
- Benner JS, Ganz DA, Weinstein MC, et al. Is it cost-effective to improve compliance with lipid-lowering therapy? Value Health. 2002;5:126. [Google Scholar]
- Brubaker L, Nichol M, Fanning K, et al. Patient-reported reasons for discontinuing overactive bladder (OAB) medications. Presented at The International Continence Society Annual Meeting; Nov. 27–Dec. 1, 2006; Christchurch, New Zealand. [Google Scholar]
- Burton WN, Morrison A, Maclean R, Ruderman E. Systematic review of studies of productivity loss due to rheumatoid arthritis. Occup Med (Lond) 2006;56:18–27. doi: 10.1093/occmed/kqi171. [DOI] [PubMed] [Google Scholar]
- Chesney M. Adherence to HAART regimens. AIDS Patient Care STDS. 2003;17:169–177. doi: 10.1089/108729103321619773. [DOI] [PubMed] [Google Scholar]
- Clifford S, Barber N, Elliott R, et al. Patient-centered advice is effective in improving adherence to medicines. Pharm World Sci. 2006;28:165–170. doi: 10.1007/s11096-006-9026-6. [DOI] [PubMed] [Google Scholar]
- Cramer J, Roy A, Burrell A. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11:44–47. doi: 10.1111/j.1524-4733.2007.00213.x. [DOI] [PubMed] [Google Scholar]
- Curkendall S, Patel V, Gleeson M, et al. Compliance with biologic therapies for rheumatoid arthritis: do patient out-of-pocket payments matter? Arthritis Rheum. 2008;59:1519–1526. doi: 10.1002/art.24114. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Prochaska JO, Gibertini M. Self-efficacy and the stages of self-change in smoking. Cognitive Ther Res. 1985;9:181–200. [Google Scholar]
- Doeglas D, Suurmeijer T, Krol B, et al. Work disability in early rheumatoid arthritis. Ann Rheum Dis. 1995;54:455–460. doi: 10.1136/ard.54.6.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott RA, Barber N, Clifford S, et al. The cost effectiveness of a telephone-based pharmacy advisory service to improve adherence to newly prescribed medicines. Pharm World Sci. 2008;30:17–23. doi: 10.1007/s11096-007-9134-y. [DOI] [PubMed] [Google Scholar]
- Goldberg E. Personal communication. 2008.
- Goldman DP, Joyce GF, Lawless G, et al. Benefit design and specialty drug use. Health Aff. 2006;25:1319–1331. doi: 10.1377/hlthaff.25.5.1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynes RB, Ackloo E, Sahota N, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008;(2):CD000011. doi: 10.1002/14651858.CD000011.pub3. [DOI] [PubMed] [Google Scholar]
- Hom D, Mahoney J, Wells KD, Lednar WM. Leading employers share strategies for managing promising, high-cost biotech medications. Am J Manag Care. 2008;14:S264–S268. [PubMed] [Google Scholar]
- IMS Health Analysis by IMS Consulting. December 2007.
- IMS Health Analysis by IMS Consulting, February 2008.
- Kessler RC, Greenberg PE, Mickelson KD, et al. The effects of chronic medical conditions on work loss and work cutback. J Occup Environ Med. 2001;43:218–225. doi: 10.1097/00043764-200103000-00009. [DOI] [PubMed] [Google Scholar]
- McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: scientific review. JAMA. 2002;288:2868–2879. doi: 10.1001/jama.288.22.2868. [DOI] [PubMed] [Google Scholar]
- Medication Digest. Compliance-Adherence-Persistence. American Pharmacists Association and Pfizer Inc. 2003
- Newell SA, Bowman JA, Cockburn JD. A critical review of interventions to increase compliance with medication-taking, obtaining medication refills, and appointment-keeping in the treatment of cardiovascular disease. Prev Med. 1999;29:535–548. doi: 10.1006/pmed.1999.0579. [DOI] [PubMed] [Google Scholar]
- Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- Ozminkowski RJ, Burton WN, Goetzel RZ, et al. The impact of rheumatoid arthritis on medical expenditures, absenteeism, and short-term disability benefits. J Occup Environ Med. 2006;48:135–148. doi: 10.1097/01.jom.0000194161.12923.52. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM. Why people use health services. Milbank Mem Fund Q. 1966;44S:94–127. [PubMed] [Google Scholar]
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q. 1988;15:175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- Roter DL, Hall JA, Merisca R, et al. Effectiveness of interventions to improve patient compliance: a meta-analysis. Med Care. 1998;36:1138–1161. doi: 10.1097/00005650-199808000-00004. [DOI] [PubMed] [Google Scholar]
- Rueda S, Park-Wyllie LY, Bayoumi AM, et al. Patient support and education for promoting adherence to highly active antiretroviral therapy for HIV/AIDS. Cochrane Database Syst Rev. 2006;3:CD001442. doi: 10.1002/14651858.CD001442.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scalera A, Bayoumi A, Oh P, et al. Clinical and economic implications of non-adherence to HAART in HIV infection. Dis Management Health Outcomes. 2002;10:85–91. [Google Scholar]
- Simons LA, Levis G, Simons J. Apparent discontinuation rates in patients prescribed lipid-lowering drugs. Med J Austr. 1996;164:208–211. doi: 10.5694/j.1326-5377.1996.tb94138.x. [DOI] [PubMed] [Google Scholar]
- (WHO) World Health Organization Adherence to long-term therapies: evidence for action. «http://www.who.int/chp/knowledge/publications/adherence_full_report.pdf» Accessed June 26, 2009.