Abstract
Intraventricular hemorrhage (IVH) is a major complication of prematurity. IVH typically initiates in the germinal matrix, which is a richly vascularized collection of neuronal-glial precursor cells in the developing brain. The etiology of IVH is multifactorial and is primarily attributed to the intrinsic fragility of the germinal matrix vasculature and the disturbance in the cerebral blood flow. While this review broadly describes the mechanism underlying IVH, the main focus is on the recent development in molecular mechanisms that elucidates the fragility of the germinal matrix vasculature. The microvasculature of the germinal matrix is frail because of an abundance of angiogenic blood vessels that exhibit paucity of pericytes, immaturity of basal lamina and deficiency of glial fibrillary acidic protein (GFAP) in the ensheathing astrocytes-endfeet. High VEGF and angiopoietin-2 levels activate a rapid angiogenesis in the germinal matrix. The elevation of these growth factors may be ascribed to a relative hypoxia of the germinal matrix perhaps resulting from high metabolic activity and oxygen consumption of the neural-progenitor cells. Hence, the rapid stabilization of the angiogenic vessels and the restoration of normal cerebral blood flow on the first day of life are potential strategies to prevent IVH in premature infants.
About twelve thousand premature infants develop intraventricular hemorrhage (IVH) every year in the United States alone (1,2). The incidence of IVH in very low birth weight infants (<1500g) has declined from 40–50% in the early 1980s to 20% in the late 1980s (3). However, in the last two decades the occurrence of IVH has remained stationary (4). In extremely premature infants weighing 500–750g, IVH occurs in about 45% of neonates (5). Thus, IVH continues to be a major problem of premature infant in modern neonatal intensive care units worldwide.
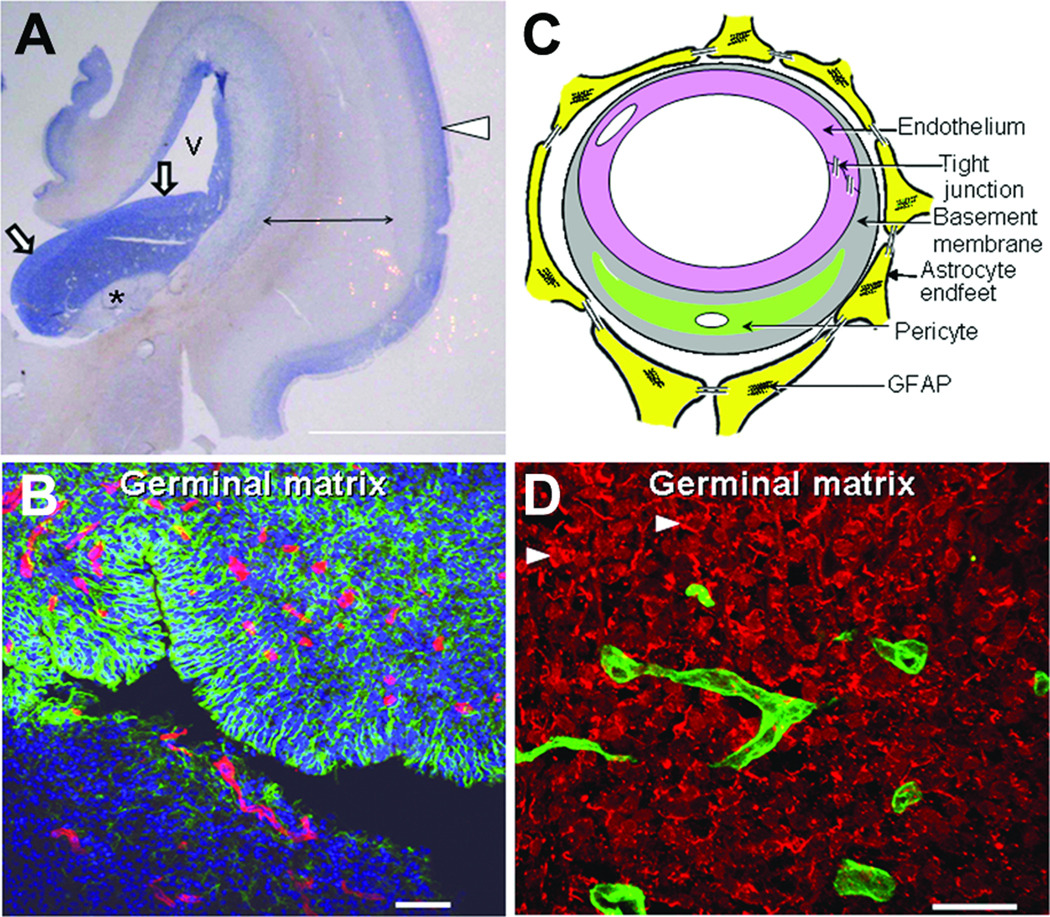
IVH characteristically initiates in the periventricular germinal matrix. The germinal matrix, located on the head of caudate nucleus and underneath ventricular ependyma, is a highly vascular collection of glial and neuronal precursor cells (Fig 1A, B). This periventricular region is selectively vulnerable to hemorrhage in premature infants predominantly in the first 48 h of life. When the hemorrhage in the germinal matrix is substantial, the ependyma breaks, and the cerebral ventricle fills up with blood. Thus, IVH is typically a progression of germinal matrix hemorrhage. Majority of these infants are asymptomatic and the diagnosis is based on screening cranial ultrasound. Some infants manifest with subtle abnormalities in the level of consciousness, movement, tone, respiration and eye movement; and uncommonly, there is a catastrophic deterioration presenting with stupor, coma, decerebrate posturing, generalized tonic seizure, and quadriparesis.
Figure 1. Morphology of germinal matrix.
A) Representative cresyl violet staining of coronal section of the right-sided cerebral hemisphere of a 20-week fetus. Note cortical plate (arrowhead), white matter (arrow with 2 pointers), germinal matrix (arrow head), caudate nucleus (asterisk), and lateral ventricle (indicated by “v”). Germinal matrix (violet staining) surrounds the whole ventricle, but is most conspicuous on the head of caudate nucleus. Scale bar, 0.5 cm. B) Representative immunofluorescence of cryosection from germinal matrix of a 24 week premature infant labeled with DAPI (blue), GFAP (green) and CD34 (red). Note: germinal matrix is highly vascular (vascular endothelium in red) and enriched with GFAP (+) glial cells (green). C) Coronal brain section was double labeled with doublecortin (red, labels neuronal precursors) and CD34 (green, labels endothelium) specific antibodies. Note doublecortin (+) neuronal precursor cells are abundantly present in the germinal matrix. Scale bar; 50 (B) and 20µm (C). D) Schematic drawing of the blood brain barrier in cross section showing endothelium, endothelial tight junction, basal lamina, pericyte and astrocyte endfeet.
IVH reduces the survival of premature infants and enhances the risk of a number of neurological sequelae. A higher mortality rate in premature infants with severe IVH has been reported compared to infants without IVH (6). Premature infants with moderate to severe IVH (grade 3–4) are at high risk of post-hemorrhagic hydrocephalus, cerebral palsy and mental retardation, while infants with mild IVH (grade 1–2) are at risk of developmental disabilities (7,8). About 45–85% of premature infants with moderate-to-severe IVH develop major cognitive deficits and approximately 75% of these infants need special education in school (9). A recent study has shown better functional outcome of surviving preterm infants with perventricular hemorrhagic infarction at school age than previously thought (10).
Pathogenesis of IVH is multifactorial and is primarily ascribed to a) inherent fragility of the germinal matrix vasculature, b) disturbance in the cerebral blood flow (CBF) and c) platelet and coagulation disorders. A number of risk factors including vaginal delivery, low Apgar score, severe respiratory distress syndrome, pneumothorax, hypoxia, hypercapnia, seizures, patent ductus arteriosus, thrombocytopenia, infection, and others predispose to the development of IVH (Table 1) (11–14). These risk factors appear to induce IVH primarily by disturbing the cerebral blood flow. However, thrombocytopenia contributes to IVH by causing hemostatic failure.
Table 1.
Neonatal risk factors in the pathogenesis of IVH.
| Major Pathogenic mechanism |
Putative mechanisms* | Risk factors | |
|---|---|---|---|
| 1 | Disturbance in CBF | 1. Fluctuation in CBF | Hypoxia Hypercarbia Severe acidosis Asynchrony between infants and ventilator breathe Severe RDS Patent ductus arteriosis Frequent suctioning of airway Rapid infusion of NaHCO3 |
| 2. High cerebral venous pressure |
Pneumothorax High ventilator pressure Prolonged labor and vaginal delivery |
||
| 3. Abnormal blood pressure | Hypotension Hypertension Sepsis Dehydration |
||
| 4. Pressure passive circulation |
Extreme prematurity and low birth weight (<1000g) Clinically unstable resulting from respiratory compromise, sepsis or other reasons |
||
| 2 | inherent fragility of germinal matrix vasculature |
Might be worsened by an inflammatory injury to the blood brain barrier |
Hypoxic ischemic insult Sepsis |
| 3. | Platelet and coagulation disturbances |
Hemostatic failure | Thrombocytopenia Disseminated intravascular coagulopathy |
Correlation of mechanisms with the risk factor is based on available evidence and author’s speculations.
Fragility of Germinal Matrix Vasculature
Premature infants primarily bleed into the germinal matrix and not in the cortical mantle or white matter, suggesting that there is an intrinsic weakness in the germinal matrix vasculature compared to the other brain regions. Endothelial tight junctions, basement membrane, pericytes, and astrocyte end-feet ensheathing the blood vessels constitute the blood brain barrier, and immaturity or weakness of any of these components can potentially cause fragility of germinal matrix vasculature (Fig 1C). The author’s research group has been able to focus on the morphological and molecular evaluation of germinal matrix vasculature and has unraveled a number of mysteries associated with the components of the blood brain barrier of this enigmatic brain region (15–20).
Morphology of germinal matrix vasculature
The density and cross-sectional area of the blood vessels are the largest in the human germinal matrix followed by the cerebral cortex and then white matter for all gestational ages (17–40 weeks) (15). In addition, the vascular density and vasculature area in cross-section significantly increases with the advancing gestational age in all the three forebrain regions--germinal matrix, cerebral cortex, and white matter. Interestingly, blood vessels in the germinal matrix are circular in the coronal section, while vessels in the cerebral cortex and white matter are relatively flat. The rounded contour of the blood vessel in cross-section indicates immaturity of germinal matrix vasculature (21). The rich vascularity of the germinal matrix is to meet the high metabolic demand of proliferating and maturing neural precursor cells constituting this brain region. The high vascularity of the germinal matrix enhances the probability of hemorrhage compared to low vascular brain regions; however, this does not entirely explain the mechanism of its intrinsic fragility and propensity to hemorrhage.
Endothelial tight junction of germinal matrix
The tight junction is composed of three integral membrane proteins, namely claudin, occludin and junction adhesion molecules as well as a number of cytoplasmic accessory proteins--ZO1, ZO2, ZO3, cingulin, and others (22). Tight junction molecules foster cell-to-cell adhesion between endothelial cells and thus contribute to the structural integrity of blood vessels. In addition, tight junction forms a blood brain barrier to limit the paracellular flux of blood-born substances from entering the brain. The major tight junction proteins, including claudin, occludin, and junction adhesion molecules, have been evaluated in postmortem tissues from human fetuses, preterm and term infants. Immunohistochemistry and Western blot analysis have shown that the expression of these molecules is similar in the germinal matrix, cerebral cortex, and white matter (16). Thus, endothelial tight junctions are unlikely to be liable for the propensity of germinal matrix vasculature to hemorrhage. Nevertheless, it will be important to evaluate the integrity of signaling events that control the tight junction molecules in the three brain regions. The studies performed on human autopsy material of short postmortem interval are invaluable. However, the limitations of such studies are exposure of premature infants to a number of prenatal and postnatal variables including prenatal steroid, mechanical ventilation, medications and others, which can potentially confound the results.
Perivascular coverage by astrocyte endfeet in the germinal matrix
Astrocyte endfeet ensheathe the cerebral vasculature to form a blood brain barrier and are viewed as providers of structural integrity to the blood vessels. The perivascular coverage by astrocyte endfeet has been evaluated in the forebrain of human fetuses, premature and mature infants (17). Immunolabeling and analyses of high-resolution images have revealed that perivascular coverage by glial fibrillary acidic protein (GFAP) positive astrocyte end-feet are lesser in the germinal matrix compared to the cerebral cortex or white matter (17). As GFAP provides shape and mechanical strength to astrocytes, reduced GFAP expression in the astrocytes endfeet might contribute to the fragility of germinal matrix vasculature. Developmentally, GFAP positive astrocytes are first seen at 9-week gestational age in spinal cord, 14 week in internal capsule and thalamus, and 14–19 week in the ependyma of the frontal cortex (23–25). As prenatal glucocorticoids reduce the incidence of IVH, it is important to know how steroids affect the expression of GFAP. There is a lack of in vivo data, however, in vitro studies have shown that glucocorticoids upregulate GFAP (26). Together, paucity of GFAP protein in perivascular endfeet of the germinal matrix vasculature might contribute to its fragility and propensity to hemorrhage. It is also likely that prenatal glucocorticoids protect against IVH by upregulating GFAP in the astrocyte endfeet.
Vascular basal lamina of the germinal matrix is deficient in fibronectin
The basal lamina in the cerebral vasculature is composed of laminin, collagen, fibronectin and the heparan sulfate proteolgycan and perlecan (27,28). Mice engineered to eliminate fibronectin, collagen IV, laminin, or perlecan gene have revealed that these molecules are essential for blood vessel formation and its stabilization (29–31) Furthermore, fibronectin promotes cell adhesion, cell migration, and cytoskeletal organization (32). In addition, its polymerization controls the stability of the extracellular matrix by providing tensile and mechanical strength to tissues (33,34).
Based on the above premise, a number of investigators have evaluated basal lamina in animal model and postmortem brains from human premature infants. In newborn beagle pups, immunolabeling and confocal microscopy showed that immunoreactivity for laminin and collagen V in the germinal matrix markedly increased on postnatal day 4 compared to day 1, but not in the white matter (35). A subsequent study from the same group revealed that postnatal indomethacin treatment significantly increased the staining intensity of laminin and collagen V. These studies suggests that laminin and collagen V deposition with advancing age or indomethacin therapy might stabilize the germinal matrix vasculature (36). Another group of investigators has evaluated collagen I, II and IV in the germinal matrix compared to the cortex and white matter in immuno-labeled human brain sections from fetuses and pre-mature infants (37). They found no difference in the expression of these molecules among the three brain regions.
A comprehensive molecular assessment of the components of basal lamina in autopsy materials from human fetuses and premature infants has shown significantly lower fibronectin protein levels in the germinal matrix relative to the cortical mantle or white matter (18). By contrast, laminin (α1, α4, and α5), perlecan, α1 and α4(IV) collagen levels are comparable in the three brain regions (18). In addition, low dose prenatal betamethasone treatment increases fibronectin expression (18). Since polymerization of fibronectin into the extracellular matrix stabilizes vasculature and because fibronectin-null mice display cerebral hemorrhage with embryonic death, diminished expression of fibronectin in the germinal matrix may contribute to the selective fragility of the blood vessels in this brain region. Thus, discovering a novel therapy to upregulate fibronectin in the germinal matrix vasculature and its validation in animal model might hold promise in the prevention of IVH.
Importantly, both transforming growth factor β (TGFβ) and fibronectin levels are lesser in the germinal matrix compared to the other brain regions. As elevated TGFβ upregulates fibronectin in addition to other components of extracellular matrix (38), low levels of fibronectin in the germinal matrix might be attributed to diminished TGFβ expression of this periventricular brain region. Thus, upregulation of TGFβ would enhance fibronectin level in the germinal matrix and might strengthen the frail vasculature of this brain area. However, TGFβ has diverse functions and its upregulation to reduce the fragility of germinal matrix vasculature may not be a safe therapeutic strategy to prevent IVH.
Paucity of pericytes in the germinal matrix
Pericytes are cells of microvasculature--capillaries, venules, and arterioles--that wrap around the endothelial cells. They provide stability and structural integrity to the microvasculature (39). They are engaged in different stages of angiogenesis including initiation, sprout extension, migration, and maturation of blood vessels (40). With the initiation of angiogenesis, they degrade the basal lamina, migrate out of the blood vessels, and regulate endothelial proliferation and migration. Towards the end of angiogenesis, they resume their position and reinforce the vessel by synthesizing extracellular matrix and endothelial differentiation (41). At least four ligand-receptor system regulates pericyte recruitment and vessel maturation, the ligands being TGF-β, platelet derived growth factor-B (PDGF-B), angiopoietin and sphingosine-1-phosphate1 (S1P1) (41). Mouse engineered to be deficient in any of the ligands or receptors develop endothelial tubes, but pericytes fail to associate with endothelial cells, resulting in irregular dilated vasculature with propensity to hemorrhage (42,43).
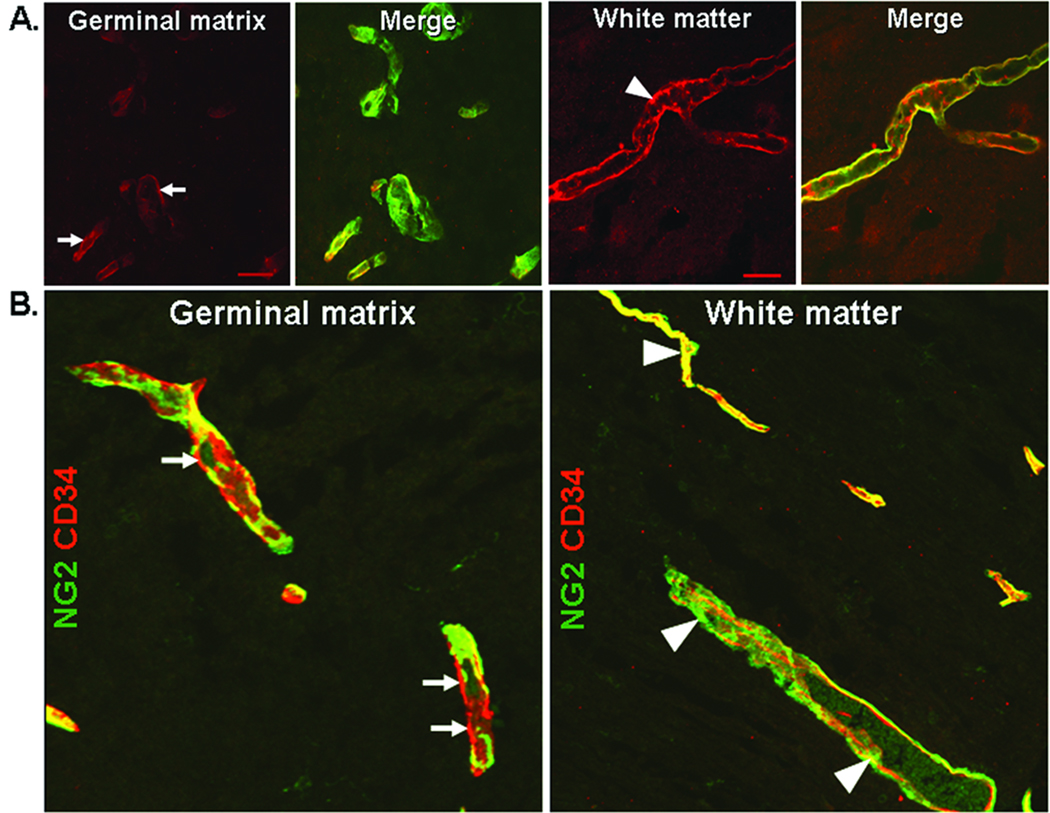
Pericytes have been quantified in immuno-stained brain sections and electron micrographs of autopsy brain samples from fetuses and premature infants as well as in premature rabbit pups. Importantly, pericyte coverage and density are lesser in the germinal matrix vasculature than in the cortex or white matter in human fetuses, premature infants, and premature rabbit pups (Fig. 2B) (19). To determine the basis of fewer pericytes in the germinal matrix, the expression of four ligand-receptor system has been evaluated. The expression of PDGF-B and its receptor, PDGFRβ, as well as angiopoietin-1 and its receptor Tie are comparable in the germinal matrix, cortex, and white matter (19). TGF-β1 protein expression is lower, while S1P and N-cadherin levels are higher in the germinal matrix than in the cortex or white matter (19). TGF-β1 contributes to stabilization of blood vessels by differentiation of pericytes from mesenchymal cells. Elevated S1P1 with N-cadherin assist vascular maturation. Low concentration of TGF-β1 activates endothelial proliferation, whereas high dose of TGF-β1 inhibits it (44). In conclusion, reduced density of pericytes in the germinal matrix vasculature may contribute to its propensity to hemorrhage, and low expression of TGF-β1 could be a basis of paucity of pericytes in its vasculature.
Figure 2. Germinal matrix is deficient in fibronectin and pericytes.
A) Representative immunofluorescence of cryosection from germinal matrix and white matter of a 24-week premature infant labeled with fibronectin (red) and CD34 (green) specific antibody. Fibronectin is strongly expressed in the white matter (arrowheads) whereas it is weakly expressed in the germinal matrix (arrows). B) Cryosection from germinal matrix and white matter of a 24-week premature infant was double-labeled with CD34 (endothelium, red) and NG2 (pericyte, green) specific antibody. NG2 positive pericytes are intimately associated with the outer endothelial surface. The coverage of the endothelia by NG2 positive astrocytes is interrupted and incomplete in the germinal matrix (arrow). In contrast, in the white matter, the vascular coverage by pericytes is continuous and complete (arrowhead). Scale bar; 20µm.
Rapid angiogenesis in the germinal matrix vasculature
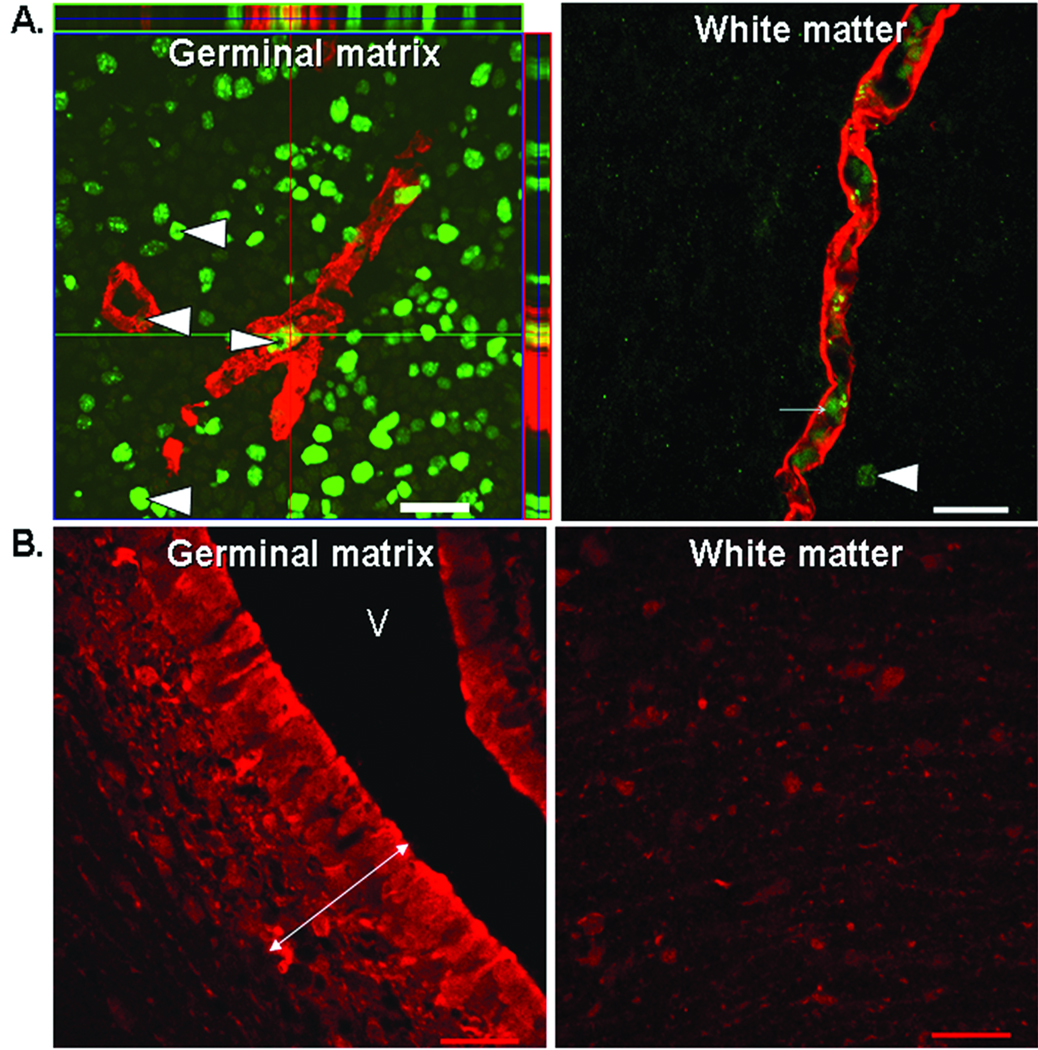
The germinal matrix exhibits rapid endothelial proliferation and accordingly, vascular endothelial growth factor (VEGF) and angiopoietin-2 levels are higher in the germinal matrix than in the cerebral cortex or white mater in both humans and rabbits (Fig. 3A) (20). In addition, endothelial proliferation is greater in fetuses, who succumb within a few hours of birth, compared to premature infants of mean postnatal age of 7 days (20). This indicates that angiogenesis in the germinal matrix diminishes shortly after birth. More importantly, suppression of VEGF by prenatal celecoxib (a COX-2 inhibitor) or ZD6474 (VEGFR2 inhibitor) treatment suppresses the incidence of glycerol-induced IVH in premature rabbit pups (20). Treatment with these antiangiogenic agents suppresses endothelial proliferation, reduces vascular density, and increases pericyte coverage in the germinal matrix (19). This suggests that angiogenic inhibition results in pruning of nascent vessels deficient in pericytes. Thus, suppressing angiogenesis and trimming of germinal matrix vasculature can potentially result in hypoxia of the germinal matrix.
Figure 3. Rapid endothelial proliferation in the hypoxic germinal matrix.
A) Representative immunofluorescence of cryosection from germinal matrix and white matter of a 21-week fetus labeled with Ki67 (proliferating nuclei, green) and CD34 (red) specific antibody. Note abundant Ki67 positive nuclei in the germinal matrix (arrowhead), but only few in the white matter. CD34 stained vessels with Ki67 signal (arrowhead) indicate endothelial proliferation in the germinal matrix. Left panel also shows orthogonal views in x–z and y–z planes of a composite stack of a series of images acquired by a confocal microscope. Right panel shows CD34 positive blood vessel with RBC in the lumen (arrow), but no Ki67 positive signal in the blood vessel. Scale bar; 20µm. B) A premature rabbit pup (E29) was injected with hypoxyprobe (60 mg/kg dose) immediately after birth and pup was euthanized after 2 hours. Hypoxyprobe is metabolized by nitro-reductase enzymes in case of low pO2 level of to form hypoxyprobe chemical adducts. Frozen sections were stained with hypoxyprobe monoclonal antibody to detect hypoxyprobe adducts. Note: intense immuno-staining (double headed arrow) in the periventricular germinal matrix and weak immunoreactivities in the white matter. V, ventricle. Scale bar; 20µm.
Importantly, the prevailing view was that antiangiogenic therapies destroy the vasculature, thereby depriving the tissue of oxygen and nutrients. However, recent evidence has shown that judicious use of certain angiogenic inhibitors normalize the abnormal structure and function of blood vessels in tumors, resulting in improved tissue oxygenation (45). During the normalization period, VEGFR2 blockade increases pericyte coverage by angiopoieitn-1 upregulation and degrades pathologically thick basal lamina by matrix metalloproteinase activation (46,47). On this basis, we speculate that titrating the dose of COX-2 inhibitor or VEGFR2 blocker might minimize pruning of germinal matrix vasculature and provide vascular stabilization by enhancing pericyte coverage and maturing basal lamina. Thus, prenatal antiangiogenic therapy in low-dose for short period (2–3 days) holds promise in the prevention in of IVH and needs further preclinical testing to determine its safety and efficacy in suitable animal models of IVH.
Why a rapid endothelial turnover in germinal matrix?
The germinal matrix harbors neuronal and glial precursor cells, which are in different stages of proliferation, migration, and maturation. This indicates high metabolic demand and oxygen requirement of the germinal matrix. Notably, VEGF and ANGPT-2 are higher in the germinal matrix than in the cortex or white matter; and hypoxia is a key trigger of these growth factors (48). Therefore, it is tempting to hypothesize that germinal matrix exhibits physiological hypoxia. In a recent experiment, we used hypoxyprobe ™ Kit (Chemicon) to evaluate oxygen gradient between germinal matrix and other brain areas in premature rabbit newborns. Hypoxyprobe is an exogenous nitroaromatic compound [1-[(2-hydroxy-3-piperidinyl)propyl]-2-nitroimidazole hydrochloride] frequently used to study hypoxia in cancer. Hypoxyprobe is metabolized by cellular nitro-reductase enzymes in case of low physiological level of pO2 (pO2 < 10 mmHg). The resulting hypoxyprobe chemical adducts can be detected by specific antibody on immunohistochemistry of hypoxic tissues. Thus, premature rabbit pups (E29) were injected with hypoxyprobe immediately after birth and pups were killed after 2 hours. Frozen sections were labeled with hypoxyprobe monoclonal antibody to detect hypoxyprobe adducts. We noted intense immuno-staining in the germinal matrix and weaker immunoreactivities in the cortex, white matter, and other brain areas (Fig. 3B). The experiment suggests lower tissue oxygen level (relative hypoxia) in the germinal matrix compared to the other brain region. However, the finding of physiological hypoxia in germinal matrix needs confirmation by using other methods such as oxygen microelectrode. Together, the germinal matrix might be hypoxic, resulting from rapid consumption of oxygen, which triggers production of VEGF and angiopoietin-2 (Fig. 4). Moreover, it is plausible that the decrease in VEGF, angiopoietin-2 and endothelial turnover as a function of postnatal age both in rabbits and humans results from increase in postnatal arterial oxygenation.
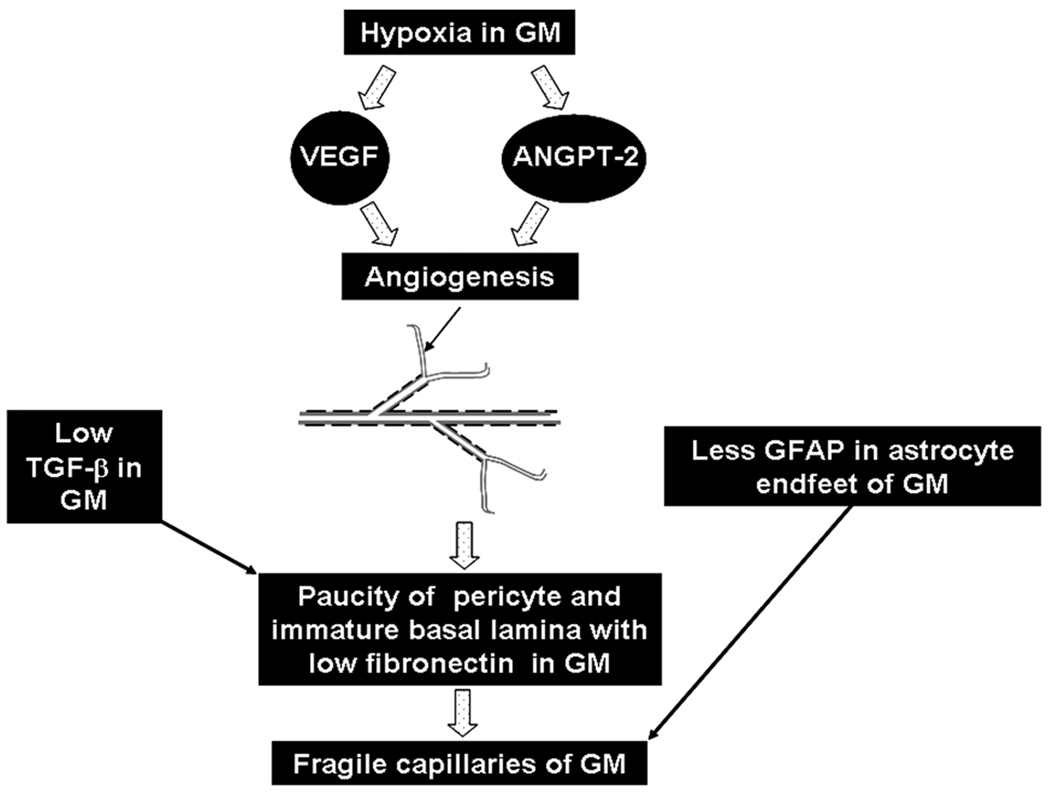
Figure 4. Mechanisms underlying fragility of germinal matrix vasculature.
Hypoxic germinal matrix induces VEGF and angiopoieitn-2 expression. These growth factors trigger angiogenesis. The nascent vessels of the germinal matrix exhibit paucity of pericytes and deficiency of fibronectin in immature basal lamina. In addition, astrocyte endfeet in the germinal matrix vasculature display diminished expression of GFAP. These factors contribute to the fragility of the germinal matrix vasculature. Black arrow in the schematic of neovasculature shows angiogenic blood vessel (grey, endothelium and black, pericyte) lacking pericytes.
In conclusion, fragility of germinal matrix vasculature can be attributed to a lack of pericytes and immaturity of basal lamina in the angiogenic vessels abundantly present in this germinal matrix. Rapid capillary remodeling in the germinal matrix vasculature can ascribe to physiological hypoxia distinctive of this brain region, which possibly results from its high metabolic activity and oxygen consumption of its neural precursor cells.
Disturbance in Cerebral Blood Flow Fluctuating cerebral blood flow
Fluctuating CBF is associated with the development of IVH (49–51). Doppler technique has been employed to measure CBF velocity in the premature infants with respiratory distress syndrome, who are on mechanical ventilator, on the first day of life. Two patterns of CBF velocity are delineated: a stable or a fluctuating CBF pattern. Stable CBF pattern consists of equal peak and trough of systolic and diastolic flow velocity, while fluctuating CBF pattern comprises continuous alteration in systolic and diastolic blood flow velocity. The neonates with fluctuating CBF velocity have higher incidence of IVH compared to infants with stable CBF pattern (50). Similar observations were made by a subsequent investigator (52). Importantly, elimination of fluctuating CBF velocity by intravenous pancuronium substantially reduces the incidence of IVH (51). As paralysis removes an infant’s contribution to the ventilation and prevents asynchrony between infant and ventilator breath, there is diminution in CBF fluctuation resulting in restoration of stable pattern. However, routine use of neuromuscular blocking agent in ventilated newborn infants is not recommended because of an uncertainly regarding the long-term neurologic and pulmonary adverse effects of this medication. Notably, newer modes of ventilation, including synchronized intermittent mandatory ventilation and assist control are now widely practiced in modern neonatal intensive care units worldwide which synchronize patient and machine breathing and reduce the fluctuation in CBF velocity in infants (53). Other clinical conditions, including hypercarbia, hypotension, patent ductus arteriosus and restlessness, also contribute to the fluctuation in the cerebral blood flow and have been correlated with the development of IVH (52,54,55).
Pressure passivity of cerebral blood flow
Cerebral autoregulation is an ability of cerebral vessels to maintain a relatively constant CBF despite fluctuation in arterial blood pressure. The popular notion prevails that the sick premature infants are not able to sustain constant CBF at autoregulatory plateau, thus exhibiting pressure passivity of cerebral circulation. Cerebral autoregulation has been assessed by xenon clearance in earlier studies and more recently by Doppler, near-infrared spectroscopy (NIRS) or spatially resolved spectroscopy (SRS) (56–58). The pressure passivity of CBF directly correlates with lower gestational age and birth weight, and is more frequently seen in sick, ventilated, and clinically unstable premature infants compared to clinically stable infants. In one of the earlier studies, the effect of acute changes in CO2 and blood pressure on global cerebral blood flow was measured in premature infants on mechanical ventilator using xenon-133 clearance (59). It was noted that infants with pressure passive circulation and reduced CO2 vaso-reactivity developed IVH in contrast to infants with preserved autoregulation and CO2 vaso-reactivity. In addition, global cerebral blood flow was 20% less in infants who subsequently developed IVH compared to those who did not. Accordingly, evaluation of CBF by NIRS showed that the infants with impaired cerebral autoregulation were associated with a higher occurrence rate of IVH compared to neonates with effective autoregulation (60). Subsequent investigators realized the value of continuous recording of CBF for long periods using NIRS because cerebral autoregulation is not an ‘all-or-none’ phenomena but a dynamic and evolving process.(61) A successive larger study on VLBW infants (1500g) showed that cerebral perfusion was pressure-passive for an average of 20% of the time while in some extremely low birth weight infant, this event exceeded 50% of the recording time (57). In this study, no relationship between occurrence of IVH and pressure passivity of cerebral circulation or systemic hypotension was observed (57). In another recent report, cerebral autoregulation was assessed by spatially resolved spectroscopy, which is a recent development of NIRS and continuously measures cerebral oxygen saturation (tissue oxygen index). In this study, impaired autoregulation does not predict the development of IVH, but the pressure passivity of cerebral circulation in sick premature infants was associated with subsequent mortality (58). Thus, a static single evaluation of CBF by xenon clearance or NIRS may result in an erroneous interpretation, while continuous monitoring of CBF by NIRS or SDS is considered a preferred method to assess impaired autoregulation. Thus, impaired autoregulation and the subsequent development of IVH appear to be unrelated, but needs further confirmation.
Abnormal blood pressure, cerebral venous pressure, and other complications of prematurity
Hypotension is a diagnosis in 20–45% of premature infants, while hypertension is infrequent in these neonates (62,63). A number of investigators have shown that systemic hypotension predisposes to IVH (64–66). Other investigators have, however, found no association between hypotension and IVH (57,67,68). Elevations of cerebral venous pressure have been implicated in contributing to the occurrence of IVH (69). Indeed, germinal matrix hemorrhage has been demonstrated to be primarily venous in origin in an evaluation of autopsy materials from premature infants (70). Importantly, cerebral venous pressure is elevated in pneumothorax and during mechanical ventilation or any positive pressure ventilation; and high cerebral venous pressure might reduce the cerebral perfusion pressure (CPP). CPP is the difference between mean arterial pressure (MAP) and intracranial pressure (CPP=MAP−ICP). However, when cerebral venous pressure (CVP) is high with normal or low ICP, cerebral perfusion pressure (CPP=MAP−CVP) is reduced resulting in a decrease in cerebral blood flow.
There is disagreement on the pathogenetic role of rapid infusion of sodium bicarbonate or hyperosmolar fluids in IVH (71,72). These factors can potentially contribute to IVH by causing episodic increase in the CBF. A rapid sodium bicarbonate infusion can also result in high arterial CO2 that can cause cerebral vasodilation. Sick premature infants in NICU undergo a number of events including hypercarbia, hypoxia, apnea, bradycardia, non-closure of ductus arteriosus, requirement of high ventilator pressure, and others, which could result in fluctuation in blood pressure and alteration in cerebral hemodynamics. Determining accurately the effect of each of these events on CBF in the presence of several confounders and establishing a causal relationship of these clinical conditions with the development of IVH is quite challenging.
Regulation of cerebral blood flow: cellular and molecular mechanisms
Cerebral circulation is equipped with protective mechanisms to ensure adequate blood supply to the brain. One such mechanism is cerebral autoregulation and the other is functional hyperemia (73). Cerebral autoregulation, an inherent ability to maintain a relatively steady-state CBF despite fluctuation in arterial blood pressure, is attributed to an intrinsic ability of smooth muscle cells and pericytes to constrict or relax to minimize variation in CBF (myogenic response). The signaling event underlying myogenic response consists of an activation of stretch-activated Ca2+ channels by an increase in intravascular pressure (74). This results in an elevation in intracellular Ca2+ and subsequent stimulation of phospholipase A2, leading to release of arachidonic acid from membrane phospholipids. Arachidonic acid metabolites, 20-HETEs inhibit Ca2+-dependent K+ channels resulting in depolarization of smooth muscles and vasoconstriction.
Functional hyperemia implies an increase in cerebral blood flow induced by neural activity to meet the local metabolic demand. This is a well-coordinated event involving neurons, astrocytes, and vascular cells. The interactions between these cells are not well understood. However, the prevailing view is that activation of glutamate receptors results in a post-synaptic increase in calcium, which stimulate enzymes that produce vaso-active agents (75). A number of vasoactive agents, including CO2, hydrogen ion, K+, adenosine, nitric oxide, arachidonic acid metabolites and cytokines, have been linked with an increase in CBF (73). The vasodilatory effects of adenosine is mediated by cAMP via KATP channels in vascular smooth muscles (76). Both nitric oxide and adenosine are key regulators of functional hyperemia (73). COX-2 derived postanoids also enhance CBF and COX-1 products have role in astrocyte-induced vasodilation (77,78). Indeed, indomethacin used for PDA closure in premature newborns reduces CBF (79).
Disorders of Hemostasis: Platelet, Coagulation, and Cytokine Disturbances
A number of studies have shown that thrombocytopenia is a risk factor for IVH (80,81). The Role of coagulopathy in pathogenesis of IVH has not been conclusively proved (82). Since inflammatory mediators and coagulation factors might contribute to the development of IVH, polymorphisms in TNFα, IL-1β, IL-4, IL-6, and IL-10 as well as mutations in coagulation proteins have been evaluated as probable genes to modify the risk and severity of IVH (83–85). There is preliminary evidence suggesting a role for cytokine genes as risk modifiers for IVH.
Conclusion
Despite major efforts made to elucidate the pathogenesis and prevent IVH in the last few decades, prevention of IVH remains an unsolved problem. Disturbance in CBF and fragility of germinal matrix vasculature primarily contributes to the development of IVH. Hence, determining means either to effectively restore normal CBF without the use of harmful sedatives and paralytic agents or to enhance the stability of germinal matrix vasculature can potentially lead to a valid strategy in the prevention of IVH.
Acknowledgements
We thank Joanne Abrahams for technical assistance with images.
Financial Support: NIH/NINDS NS050586 grant.
Abbreviations
- CBF
cerebral blood flow
- IVH
intraventricular hemorrhage
- GFAP
glial fibrillary acidic protein
- TGFβ
transforming growth factor β
- S1P1
sphingosine-1-phosphate1
References
- 1.Guyer B, Hoyert DL, Martin JA, Ventura SJ, MacDorman MF, Strobino DM. Annual summary of vital statistics--1998. Pediatrics. 1999;104:1229–1246. doi: 10.1542/peds.104.6.1229. [DOI] [PubMed] [Google Scholar]
- 2.Heuchan AM, Evans N, Henderson Smart DJ, Simpson JM. Perinatal risk factors for major intraventricular haemorrhage in the Australian and New Zealand Neonatal Network, 1995–97. Arch Dis Child Fetal Neonatal Ed. 2002;86:F86–F90. doi: 10.1136/fn.86.2.F86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Philip AG, Allan WC, Tito AM, Wheeler LR. Intraventricular hemorrhage in preterm infants: declining incidence in the 1980s. Pediatrics. 1989;84:797–801. [PubMed] [Google Scholar]
- 4.Jain NJ, Kruse LK, Demissie K, Khandelwal M. Impact of mode of delivery on neonatal complications: trends between 1997 and 2005. J Matern Fetal Neonatal Med. 2009;22:491–500. doi: 10.1080/14767050902769982. [DOI] [PubMed] [Google Scholar]
- 5.Wilson-Costello D, Friedman H, Minich N, Fanaroff AA, Hack M. Improved survival rates with increased neurodevelopmental disability for extremely low birth weight infants in the 1990s. Pediatrics. 2005;115:997–1003. doi: 10.1542/peds.2004-0221. [DOI] [PubMed] [Google Scholar]
- 6.Whitelaw A. Intraventricular haemorrhage and posthaemorrhagic hydrocephalus: pathogenesis, prevention and future interventions. Semin Neonatol. 2001;6:135–146. doi: 10.1053/siny.2001.0047. [DOI] [PubMed] [Google Scholar]
- 7.Murphy BP, Inder TE, Rooks V, Taylor GA, Anderson NJ, Mogridge N, Horwood LJ, Volpe JJ. Posthaemorrhagic ventricular dilatation in the premature infant: natural history and predictors of outcome. Arch Dis Child Fetal Neonatal Ed. 2002;87:F37–F41. doi: 10.1136/fn.87.1.F37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pinto-Martin JA, Whitaker AH, Feldman JF, Van Rossem R, Paneth N. Relation of cranial ultrasound abnormalities in low-birthweight infants to motor or cognitive performance at ages 2, 6, and 9 years. Dev Med Child Neurol. 1999;41:826–833. doi: 10.1017/s0012162299001644. [DOI] [PubMed] [Google Scholar]
- 9.Vohr BR, Allan WC, Westerveld M, Schneider KC, Katz KH, Makuch RW, Ment LR. School-age outcomes of very low birth weight infants in the indomethacin intraventricular hemorrhage prevention trial. Pediatrics. 2003;111:e340–e346. doi: 10.1542/peds.111.4.e340. [DOI] [PubMed] [Google Scholar]
- 10.Roze E, Van Braeckel KN, van der Veere CN, Maathuis CG, Martijn A, Bos AF. Functional outcome at school age of preterm infants with periventricular hemorrhagic infarction. Pediatrics. 2009;123:1493–1500. doi: 10.1542/peds.2008-1919. [DOI] [PubMed] [Google Scholar]
- 11.Antoniuk S, da Silva RV. Periventricular and intraventricular hemorrhage in the premature infants. Rev Neurol. 2000;31:238–243. [PubMed] [Google Scholar]
- 12.Kenny JD, Garcia-Prats JA, Hilliard JL, Corbet AJ, Rudolph AJ. Hypercarbia at birth: a possible role in the pathogenesis of intraventricular hemorrhage. Pediatrics. 1978;62:465–467. [PubMed] [Google Scholar]
- 13.DiSalvo D The Developmental Epidemiology Network Investigators. The correlation between placental pathology and intraventricular hemorrhage in the preterm infant. Pediatr Res. 1998;43:15–19. doi: 10.1203/00006450-199801000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Volpe JJ. Intraventricular hemorrhage in the premature infant--current concepts. Part I. Ann Neurol. 1989;25:3–11. doi: 10.1002/ana.410250103. [DOI] [PubMed] [Google Scholar]
- 15.Ballabh P, Braun A, Nedergaard M. Anatomic analysis of blood vessels in germinal matrix, cerebral cortex, and white matter in developing infants. Pediatr Res. 2004;56:117–124. doi: 10.1203/01.PDR.0000130472.30874.FF. [DOI] [PubMed] [Google Scholar]
- 16.Ballabh P, Hu F, Kumarasiri M, Braun A, Nedergaard M. Development of tight junction molecules in blood vessels of germinal matrix, cerebral cortex, and white matter. Pediatr Res. 2005;58:791–798. doi: 10.1203/01.PDR.0000180535.14093.FB. [DOI] [PubMed] [Google Scholar]
- 17.El-Khoury N, Braun A, Hu F, Pandey M, Nedergaard M, Lagamma EF, Ballabh P. Astrocyte end-feet in germinal matrix, cerebral cortex, and white matter in developing infants. Pediatr Res. 2006;59:673–679. doi: 10.1203/01.pdr.0000214975.85311.9c. [DOI] [PubMed] [Google Scholar]
- 18.Xu H, Hu F, Sado Y, Ninomiya Y, Borza DB, Ungvari Z, Lagamma EF, Csiszar A, Nedergaard M, Ballabh P. Maturational changes in laminin, fibronectin, collagen IV, and perlecan in germinal matrix, cortex, and white matter and effect of betamethasone. J Neurosci Res. 2008;86:1482–1500. doi: 10.1002/jnr.21618. [DOI] [PubMed] [Google Scholar]
- 19.Braun A, Xu H, Hu F, Kocherlakota P, Siegel D, Chander P, Ungvari Z, Csiszar A, Nedergaard M, Ballabh P. Paucity of pericytes in germinal matrix vasculature of premature infants. J Neurosci. 2007;27:12012–12024. doi: 10.1523/JNEUROSCI.3281-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ballabh P, Xu H, Hu F, Braun A, Smith K, Rivera A, Lou N, Ungvari Z, Goldman SA, Csiszar A, Nedergaard M. Angiogenic inhibition reduces germinal matrix hemorrhage. Nat Med. 2007;13:477–485. doi: 10.1038/nm1558. [DOI] [PubMed] [Google Scholar]
- 21.Hellstrom M, Gerhardt H, Kalen M, Li X, Eriksson U, Wolburg H, Betsholtz C. Lack of pericytes leads to endothelial hyperplasia and abnormal vascular morphogenesis. J Cell Biol. 2001;153:543–553. doi: 10.1083/jcb.153.3.543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ballabh P, Braun A, Nedergaard M. The blood-brain barrier: an overview: structure, regulation, and clinical implications. Neurobiol Dis. 2004;16:1–13. doi: 10.1016/j.nbd.2003.12.016. [DOI] [PubMed] [Google Scholar]
- 23.Wilkinson M, Hume R, Strange R, Bell JE. Glial and neuronal differentiation in the human fetal brain 9–23 weeks of gestation. Neuropathol Appl Neurobiol. 1990;16:193–204. doi: 10.1111/j.1365-2990.1990.tb01156.x. [DOI] [PubMed] [Google Scholar]
- 24.Gould SJ, Howard S. An immunohistochemical study of the germinal layer in the late gestation human fetal brain. Neuropathol Appl Neurobiol. 1987;13:421–437. doi: 10.1111/j.1365-2990.1987.tb00072.x. [DOI] [PubMed] [Google Scholar]
- 25.Sarnat HB. Role of human fetal ependyma. Pediatr Neurol. 1992;8:163–178. doi: 10.1016/0887-8994(92)90063-5. [DOI] [PubMed] [Google Scholar]
- 26.Morrison RS, De Vellis J, Lee YL, Bradshaw RA, Eng LF. Hormones and growth factors induce the synthesis of glial fibrillary acidic protein in rat brain astrocytes. J Neurosci Res. 1985;14:167–176. doi: 10.1002/jnr.490140202. [DOI] [PubMed] [Google Scholar]
- 27.Hallmann R, Horn N, Selg M, Wendler O, Pausch F, Sorokin LM. Expression and function of laminins in the embryonic and mature vasculature. Physiol Rev. 2005;85:979–1000. doi: 10.1152/physrev.00014.2004. [DOI] [PubMed] [Google Scholar]
- 28.Tilling T, Engelbertz C, Decker S, Korte D, Huwel S, Galla HJ. Expression and adhesive properties of basement membrane proteins in cerebral capillary endothelial cell cultures. Cell Tissue Res. 2002;310:19–29. doi: 10.1007/s00441-002-0604-1. [DOI] [PubMed] [Google Scholar]
- 29.George EL, Georges-Labouesse EN, Patel-King RS, Rayburn H, Hynes RO. Defects in mesoderm, neural tube and vascular development in mouse embryos lacking fibronectin. Development. 1993;119:1079–1091. doi: 10.1242/dev.119.4.1079. [DOI] [PubMed] [Google Scholar]
- 30.Forsberg E, Kjellen L. Heparan sulfate: lessons from knockout mice. J Clin Invest. 2001;108:175–180. doi: 10.1172/JCI13561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gould DB, Phalan FC, Breedveld GJ, van Mil SE, Smith RS, Schimenti JC, Aguglia U, van der Knaap MS, Heutink P, John SW. Mutations in Col4a1 cause perinatal cerebral hemorrhage and porencephaly. Science. 2005;308:1167–1171. doi: 10.1126/science.1109418. [DOI] [PubMed] [Google Scholar]
- 32.Mao Y, Schwarzbauer JE. Fibronectin fibrillogenesis, a cell-mediated matrix assembly process. Matrix Biol. 2005;24:389–399. doi: 10.1016/j.matbio.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 33.Hocking DC, Sottile J, Langenbach KJ. Stimulation of integrin-mediated cell contractility by fibronectin polymerization. J Biol Chem. 2000;275:10673–10682. doi: 10.1074/jbc.275.14.10673. [DOI] [PubMed] [Google Scholar]
- 34.Sottile J, Hocking DC, Langenbach KJ. Fibronectin polymerization stimulates cell growth by RGD-dependent and -independent mechanisms. J Cell Sci. 2000;113:4287–4299. doi: 10.1242/jcs.113.23.4287. [DOI] [PubMed] [Google Scholar]
- 35.Ment LR, Stewart WB, Ardito TA, Madri JA. Beagle pup germinal matrix maturation studies. Stroke. 1991;22:390–395. doi: 10.1161/01.str.22.3.390. [DOI] [PubMed] [Google Scholar]
- 36.Ment LR, Stewart WB, Ardito TA, Huang E, Madri JA. Indomethacin promotes germinal matrix microvessel maturation in the newborn beagle pup. Stroke. 1992;23:1132–1137. doi: 10.1161/01.str.23.8.1132. [DOI] [PubMed] [Google Scholar]
- 37.Anstrom JA, Thore CR, Moody DM, Challa VR, Block SM, Brown WR. Morphometric assessment of collagen accumulation in germinal matrix vessels of premature human neonates. Neuropathol Appl Neurobiol. 2005;31:181–190. doi: 10.1111/j.1365-2990.2004.00626.x. [DOI] [PubMed] [Google Scholar]
- 38.Pasinetti GM, Nichols NR, Tocco G, Morgan T, Laping N, Finch CE. Transforming growth factor beta 1 and fibronectin messenger RNA in rat brain: responses to injury and cell-type localization. Neuroscience. 1993;54:893–907. doi: 10.1016/0306-4522(93)90583-2. [DOI] [PubMed] [Google Scholar]
- 39.Balabanov R, Dore-Duffy P. Role of the CNS microvascular pericyte in the blood-brain barrier. J Neurosci Res. 1998;53:637–644. doi: 10.1002/(SICI)1097-4547(19980915)53:6<637::AID-JNR1>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 40.Hirschi KK, D'Amore PA. Control of angiogenesis by the pericyte: molecular mechanisms and significance. EXS. 1997;79:419–428. doi: 10.1007/978-3-0348-9006-9_18. [DOI] [PubMed] [Google Scholar]
- 41.Jain RK. Molecular regulation of vessel maturation. Nat Med. 2003;9:685–693. doi: 10.1038/nm0603-685. [DOI] [PubMed] [Google Scholar]
- 42.Lindahl P, Johansson BR, Leveen P, Betsholtz C. Pericyte loss and microaneurysm formation in PDGF-B-deficient mice. Science. 1997;277:242–245. doi: 10.1126/science.277.5323.242. [DOI] [PubMed] [Google Scholar]
- 43.Yancopoulos GD, Davis S, Gale NW, Rudge JS, Wiegand SJ, Holash J. Vascular-specific growth factors and blood vessel formation. Nature. 2000;407:242–248. doi: 10.1038/35025215. [DOI] [PubMed] [Google Scholar]
- 44.Bertolino P, Deckers M, Lebrin F, ten Dijke P. Transforming growth factor-beta signal transduction in angiogenesis and vascular disorders. Chest. 2005;128:585S–590S. doi: 10.1378/chest.128.6_suppl.585S. [DOI] [PubMed] [Google Scholar]
- 45.Jain RK. Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science. 2005;307:58–62. doi: 10.1126/science.1104819. [DOI] [PubMed] [Google Scholar]
- 46.Winkler F, Kozin SV, Tong RT, Chae SS, Booth MF, Garkavtsev I, Xu L, Hicklin DJ, Fukumura D, di Tomaso E, Munn LL, Jain RK. Kinetics of vascular normalization by VEGFR2 blockade governs brain tumor response to radiation: role of oxygenation, angiopoietin-1, and matrix metalloproteinases. Cancer Cell. 2004;6:553–563. doi: 10.1016/j.ccr.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 47.Uemura A, Ogawa M, Hirashima M, Fujiwara T, Koyama S, Takagi H, Honda Y, Wiegand SJ, Yancopoulos GD, Nishikawa S. Recombinant angiopoietin-1 restores higher-order architecture of growing blood vessels in mice in the absence of mural cells. J Clin Invest. 2002;110:1619–1628. doi: 10.1172/JCI15621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mu D, Jiang X, Sheldon RA, Fox CK, Hamrick SE, Vexler ZS, Ferriero DM. Regulation of hypoxia-inducible factor 1alpha and induction of vascular endothelial growth factor in a rat neonatal stroke model. Neurobiol Dis. 2003;14:524–534. doi: 10.1016/j.nbd.2003.08.020. [DOI] [PubMed] [Google Scholar]
- 49.Tsuji M, duPlessis A, Taylor G, Crocker R, Volpe JJ. Near infrared spectroscopy detects cerebral ischemia during hypotension in piglets. Pediatr Res. 1998;44:591–595. doi: 10.1203/00006450-199810000-00020. [DOI] [PubMed] [Google Scholar]
- 50.Perlman JM, McMenamin JB, Volpe JJ. Fluctuating cerebral blood-flow velocity in respiratory-distress syndrome. Relation to the development of intraventricular hemorrhage. N Engl J Med. 1983;309:204–209. doi: 10.1056/NEJM198307283090402. [DOI] [PubMed] [Google Scholar]
- 51.Perlman JM, Goodman S, Kreusser KL, Volpe JJ. Reduction in intraventricular hemorrhage by elimination of fluctuating cerebral blood-flow velocity in preterm infants with respiratory distress syndrome. N Engl J Med. 1985;312:1353–1357. doi: 10.1056/NEJM198505233122104. [DOI] [PubMed] [Google Scholar]
- 52.Van Bel F, Van de Bor M, Stijnen T, Baan J, Ruys JH. Aetiological role of cerebral blood-flow alterations in development and extension of peri-intraventricular haemorrhage. Dev Med Child Neurol. 1987;29:601–614. doi: 10.1111/j.1469-8749.1987.tb08502.x. [DOI] [PubMed] [Google Scholar]
- 53.Rennie JM, South M, Morley CJ. Cerebral blood flow velocity variability in infants receiving assisted ventilation. Arch Dis Child. 1987;62:1247–1251. doi: 10.1136/adc.62.12.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mullaart RA, Hopman JC, Rotteveel JJ, Daniels O, Stoelinga GB, De Haan AF. Cerebral blood flow fluctuation in neonatal respiratory distress and periventricular haemorrhage. Early Hum Dev. 1994;37:179–185. doi: 10.1016/0378-3782(94)90077-9. [DOI] [PubMed] [Google Scholar]
- 55.Coughtrey H, Rennie JM, Evans DH. Variability in cerebral blood flow velocity: observations over one minute in preterm babies. Early Hum Dev. 1997;47:63–70. doi: 10.1016/s0378-3782(96)01769-0. [DOI] [PubMed] [Google Scholar]
- 56.du Plessis AJ. Cerebrovascular injury in premature infants: current understanding and challenges for future prevention. Clin Perinatol. 2008;35:609–641. doi: 10.1016/j.clp.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 57.Soul JS, Hammer PE, Tsuji M, Saul JP, Bassan H, Limperopoulos C, Disalvo DN, Moore M, Akins P, Ringer S, Volpe JJ, Trachtenberg F, du Plessis AJ. Fluctuating pressure-passivity is common in the cerebral circulation of sick premature infants. Pediatr Res. 2007;61:467–473. doi: 10.1203/pdr.0b013e31803237f6. [DOI] [PubMed] [Google Scholar]
- 58.Wong FY, Leung TS, Austin T, Wilkinson M, Meek JH, Wyatt JS, Walker AM. Impaired autoregulation in preterm infants identified by using spatially resolved spectroscopy. Pediatrics. 2008;121:e604–e611. doi: 10.1542/peds.2007-1487. [DOI] [PubMed] [Google Scholar]
- 59.Pryds O, Greisen G, Lou H, Friis-Hansen B. Heterogeneity of cerebral vasoreactivity in preterm infants supported by mechanical ventilation. J Pediatr. 1989;115:638–645. doi: 10.1016/s0022-3476(89)80301-4. [DOI] [PubMed] [Google Scholar]
- 60.Tsuji M, Saul JP, du Plessis A, Eichenwald E, Sobh J, Crocker R, Volpe JJ. Cerebral intravascular oxygenation correlates with mean arterial pressure in critically ill premature infants. Pediatrics. 2000;106:625–632. doi: 10.1542/peds.106.4.625. [DOI] [PubMed] [Google Scholar]
- 61.Reynolds KJ, Panerai RB, Kelsall AW, Rennie JM, Evans DH. Spectral pattern of neonatal cerebral blood flow velocity: comparison with spectra from blood pressure and heart rate. Pediatr Res. 1997;41:276–284. doi: 10.1203/00006450-199702000-00020. [DOI] [PubMed] [Google Scholar]
- 62.Al-Aweel I, Pursley DM, Rubin LP, Shah B, Weisberger S, Richardson DK. Variations in prevalence of hypotension, hypertension, and vasopressor use in NICUs. J Perinatol. 2001;21:272–278. doi: 10.1038/sj.jp.7210563. [DOI] [PubMed] [Google Scholar]
- 63.Fanaroff JM, Fanaroff AA. Blood pressure disorders in the neonate: hypotension and hypertension. Semin Fetal Neonatal Med. 2006;11:174–181. doi: 10.1016/j.siny.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 64.Miall-Allen VM, de Vries LS, Whitelaw AG. Mean arterial blood pressure and neonatal cerebral lesions. Arch Dis Child. 1987;62:1068–1069. doi: 10.1136/adc.62.10.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Watkins AM, West CR, Cooke RW. Blood pressure and cerebral haemorrhage and ischaemia in very low birthweight infants. Early Hum Dev. 1989;19:103–110. doi: 10.1016/0378-3782(89)90120-5. [DOI] [PubMed] [Google Scholar]
- 66.Bada HS, Korones SB, Perry EH, Arheart KL, Ray JD, Pourcyrous M, Magill HL, Runyan W, 3rd, Somes GW, Clark FC. Mean arterial blood pressure changes in premature infants and those at risk for intraventricular hemorrhage. J Pediatr. 1990;117:607–614. doi: 10.1016/s0022-3476(05)80700-0. [DOI] [PubMed] [Google Scholar]
- 67.Weindling AM, Wilkinson AR, Cook J, Calvert SA, Fok TF, Rochefort MJ. Perinatal events which precede periventricular haemorrhage and leukomalacia in the newborn. Br J Obstet Gynaecol. 1985;92:1218–1223. doi: 10.1111/j.1471-0528.1985.tb04865.x. [DOI] [PubMed] [Google Scholar]
- 68.Muller AM, Morales C, Briner J, Baenziger O, Duc G, Bucher HU. Loss of CO2 reactivity of cerebral blood flow is associated with severe brain damage in mechanically ventilated very low birth weight infants. Eur J Paediatr Neurol. 1997;1:157–163. [PubMed] [Google Scholar]
- 69.Volpe JJ. Intracranial hemorrhage: Germinal matrix hemorrhage. In: Volpe JJ, editor. Neurology of the newborn. Philadelphia: Saunders Elsevier; 2008. pp. 517–288. [Google Scholar]
- 70.Ghazi-Birry HS, Brown WR, Moody DM, Challa VR, Block SM, Reboussin DM. Human germinal matrix: venous origin of hemorrhage and vascular characteristics. AJNR Am J Neuroradiol. 1997;18:219–229. [PMC free article] [PubMed] [Google Scholar]
- 71.Wigglesworth JS, Keith IH, Girling DJ, Slade SA. Hyaline membrane disease, alkali, and intraventricular haemorrhage. Arch Dis Child. 1976;51:755–762. doi: 10.1136/adc.51.10.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Anderson JM, Bain AD, Brown JK, Cockburn F, Forfar JO, Machin GA, Turner TL. Hyaline-membrane disease, alkaline buffer treatment, and cerebral intraventricular halphaemorrhage. Lancet. 1976;1:117–119. doi: 10.1016/s0140-6736(76)93156-1. [DOI] [PubMed] [Google Scholar]
- 73.Iadecola C, Nedergaard M. Glial regulation of the cerebral microvasculature. Nat Neurosci. 2007;10:1369–1376. doi: 10.1038/nn2003. [DOI] [PubMed] [Google Scholar]
- 74.Hill MA, Sun Z, Martinez-Lemus L, Meininger GA. New technologies for dissecting the arteriolar myogenic response. Trends Pharmacol Sci. 2007;28:308–315. doi: 10.1016/j.tips.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 75.Iadecola C. Neurovascular regulation in the normal brain and in Alzheimer's disease. Nat Rev Neurosci. 2004;5:347–360. doi: 10.1038/nrn1387. [DOI] [PubMed] [Google Scholar]
- 76.Phillis JW. Adenosine and adenine nucleotides as regulators of cerebral blood flow: roles of acidosis, cell swelling, and KATP channels. Crit Rev Neurobiol. 2004;16:237–270. doi: 10.1615/critrevneurobiol.v16.i4.20. [DOI] [PubMed] [Google Scholar]
- 77.Niwa K, Araki E, Morham SG, Ross ME, Iadecola C. Cyclooxygenase-2 contributes to functional hyperemia in whisker-barrel cortex. J Neurosci. 2000;20:763–770. doi: 10.1523/JNEUROSCI.20-02-00763.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Niwa K, Haensel C, Ross ME, Iadecola C. Cyclooxygenase-1 participates in selected vasodilator responses of the cerebral circulation. Circ Res. 2001;88:600–608. doi: 10.1161/01.res.88.6.600. [DOI] [PubMed] [Google Scholar]
- 79.Upton RN, Rasmussen M, Grant C, Martinez AM, Cold GE, Ludbrook GL. Pharmacokinetics and pharmacodynamics of indomethacin: effects on cerebral blood flow in anaesthetized sheep. Clin Exp Pharmacol Physiol. 2008;35:317–323. doi: 10.1111/j.1440-1681.2007.04818.x. [DOI] [PubMed] [Google Scholar]
- 80.Andrew M, Castle V, Saigal S, Carter C, Kelton JG. Clinical impact of neonatal thrombocytopenia. J Pediatr. 1987;110:457–464. doi: 10.1016/s0022-3476(87)80517-6. [DOI] [PubMed] [Google Scholar]
- 81.Lupton BA, Hill A, Whitfield MF, Carter CJ, Wadsworth LD, Roland EH. Reduced platelet count as a risk factor for intraventricular hemorrhage. Am J Dis Child. 1988;142:1222–1224. doi: 10.1001/archpedi.1988.02150110100029. [DOI] [PubMed] [Google Scholar]
- 82.Shirahata A, Nakamura T, Shimono M, Kaneko M, Tanaka S. Blood coagulation findings and the efficacy of factor XIII concentrate in premature infants with intracranial hemorrhages. Thromb Res. 1990;57:755–763. doi: 10.1016/0049-3848(90)90033-9. [DOI] [PubMed] [Google Scholar]
- 83.Gopel W, Hartel C, Ahrens P, Konig I, Kattner E, Kuhls E, Kuster H, Moller J, Muller D, Roth B, Segerer H, Wieg C, Herting E. Interleukin-6-174-genotype, sepsis and cerebral injury in very low birth weight infants. Genes Immun. 2006;7:65–68. doi: 10.1038/sj.gene.6364264. [DOI] [PubMed] [Google Scholar]
- 84.Harding DR, Dhamrait S, Whitelaw A, Humphries SE, Marlow N, Montgomery HE. Does interleukin-6 genotype influence cerebral injury or developmental progress after preterm birth? Pediatrics. 2004;114:941–947. doi: 10.1542/peds.2003-0494-F. [DOI] [PubMed] [Google Scholar]
- 85.Harding D, Brull D, Humphries SE, Whitelaw A, Montgomery H, Marlow N. Variation in the interleukin-6 gene is associated with impaired cognitive development in children born prematurely: a preliminary study. Pediatr Res. 2005;58:117–120. doi: 10.1203/01.PDR.0000163523.49021.53. [DOI] [PubMed] [Google Scholar]