Abstract
Background
Global climate change is already increasing the average temperature and direct heat exposure in many places around the world.
Objectives
To assess the potential impact on occupational health and work capacity for people exposed at work to increasing heat due to climate change.
Design
A brief review of basic thermal physiology mechanisms, occupational heat exposure guidelines and heat exposure changes in selected cities.
Results
In countries with very hot seasons, workers are already affected by working environments hotter than that with which human physiological mechanisms can cope. To protect workers from excessive heat, a number of heat exposure indices have been developed. One that is commonly used in occupational health is the Wet Bulb Globe Temperature (WBGT). We use WBGT to illustrate assessing the proportion of a working hour during which a worker can sustain work and the proportion of that same working hour that (s)he needs to rest to cool the body down and maintain core body temperature below 38°C. Using this proportion a ‘work capacity’ estimate was calculated for selected heat exposure levels and work intensity levels. The work capacity rapidly reduces as the WBGT exceeds 26–30°C and this can be used to estimate the impact of increasing heat exposure as a result of climate change in tropical countries.
Conclusions
One result of climate change is a reduced work capacity in heat-exposed jobs and greater difficulty in achieving economic and social development in the countries affected by this somewhat neglected impact of climate change.
Keywords: climate change, work, heat, occupational health, productivity
Global climate change will affect living and working environments, and create health threats for millions of people (1, 2). The average global temperature is increasing and it is estimated that it will go up a further 1.8–4.0°C (estimated average 3.0°C) by 2100 (1), depending on actions to limit greenhouse gas emissions. The extent of local climate change will vary depending on geographic and local meteorological conditions. Modern urban development can add several degrees to local temperatures through heat absorption in concrete buildings, road tar-seal, etc.: the ‘urban heat island effect’ (3).
Increasing local ambient temperature means higher human exposure to heat, which during hot seasons in hot parts of the world can create very unhealthy environments for people who are not able to protect themselves with air conditioning or other cooling methods. Both general living environments and working environments are affected. The latter may create impacts both on workers’ health and on economic conditions (4). Workers in low and middle-income tropical countries are likely to be at highest risk of excessive heat exposure.
The aim of this paper is to briefly introduce the most commonly used occupational heat stress index and how working people are likely to be affected at different heat exposure levels, an important aspect of the health effects of climate change (5). We will highlight the potential impacts of increasing heat exposure due to climate change in low and middle-income tropical countries.
Physiological and clinical impacts of heat stress
The human body is designed to maintain a core body temperature of 37°C. A person carrying out physical activity (for instance while working) creates metabolic heat inside the body, which needs to be transferred to the person's external environment in order to avoid a dangerous increase of core body temperature (6). The body heat balance is determined by the ‘six fundamental factors’ (6):
air temperature;
radiant temperature;
humidity;
air movement (wind speed);
clothing; and
the metabolic heat generated by human physical activity.
If cooling via sweating and convection (via contact with cooler air and air movement) is not sufficient, the metabolic heat generation needs to be reduced to avoid heat strain and heat stroke (7). This creates limits to the extent to which physical activity and work output can be maintained without rest periods.
When physical activity is high in a hot working environment, the worker is at risk of increased core body temperature (above 38°C), diminished physical work capacity (8, 9), diminished mental task ability (10), increased accident risk (11) and eventually heat exhaustion or heat stroke (12). The main factor underlying these effects is the increased core body temperature (13), but dehydration due to sweating and inadequate liquid intake is also of major importance (14). Symptomatic exhaustion and clinical diseases, particularly kidney disease (14), can be the result of excessive dehydration (9).
When body temperature exceeds 39°C, acute heat disorders (heat stroke) may occur, and above 40.6°C life-threatening ‘severe hyperpyrexia’ starts to occur (13). Many of these references may look outdated, but the fact is that much of the relevant research was carried out several decades ago, and more recent studies have confirmed the understanding of the basic mechanisms (9).
Assessing workplace heat stress
To protect workers from the effects of heat exposure ‘heat stress indices’ and protective guidelines have been developed (7). The most commonly used in occupational health is the Wet Bulb Globe Temperature (WBGT) index developed by the US Army many decades ago (15). This index takes into account air temperature, radiant temperature, humidity and air movement, and is the basis for time limitations of work in different heat exposure standards. Other indices of heat exposure (e.g. heat stress index, index of thermal stress, predicted four-hour sweat rate) (8) are likely to be correlated to WBGT.
The WBGT is a combination of three local climate measurements (16): the natural wet bulb temperature, Tnwb; the globe temperature, Tg; and the air temperature, Ta. WBGT-outdoors = 0.7×Tnwb+0.2×Tg+0.1×Ta; WBGT-indoors = 0.7×Tnwb+0.3×Tg. Special equipment is required to measure Tnwb and Tg (6), and these variables are not routinely measured at weather stations. Descriptions of the equipment and the physical science basis for the three temperature measurements can be found on web-sites or in textbooks (6).
In order to assess time trends of human heat exposure in the past and likely future trends during climate change, it would be very useful if available weather station data could be used to estimate WBGT. However, the relationships between the different variables are complex.
Different mathematical models to calculate WBGT from weather station data have been developed and a recent one, based on a detailed analysis of the physical principles behind heat and energy transfer (17), appears the most accurate. The computer software can be obtained from the authors on request (17). This elaborate model makes it possible to compare calculated WBGT estimates for different seasons and places.
Occupational heat exposure guidelines based on WBGT (16, 18) state maximum heat exposures in jobs at different work intensity (in Watts). The international standard (18) presents the proportions of work hours during which workers need to take rest periods, depending on work intensity and WBGT, in order to avoid the core body temperature exceeding 38°C for an average worker. A table in the international standard presents WBGT ‘reference values’ (the point at which some preventive action should be taken) (Table 1) shows the WBGT levels that require no hourly rest, or rest to the extent of 25, 50 and 75% (rest/work ratios) during the working hour. The US guidelines (16) also includes a WBGT level at which no work should be carried out without special protective clothing at a higher level of heat exposure. These standards have been summarised in Table 2.
Table 1.
Reference values for WBGT (°C) at different work intensity levels (in Watts = W), light clothing
| Metabolic rate classa (work intensity) | 0 (rest) | 1 (light work) | 2 (medium work) | 3 (intense work) | 4 (very intense work) |
|---|---|---|---|---|---|
| Approximate metabolic rate, M (W) | 100 | 200 | 300 | 400 | 500 |
| WBGT reference valuesb (°C) | 33 | 30 | 28 | 25 | 23 |
aThe metabolic rate classes are: 0 = resting, M < 117 W; 1 = light work, 117 < M<234 W; 2 = sustained medium level work, 234 < M<360 W; 3 = intense work, 360 < M<468 W; 4 = very intense work, M > 468 W.
bThe ISO standard (18) says: ‘If these values are exceeded, it is necessary either to reduce the direct heat stress at the workplace, or to carry out a detailed analysis of exposure and prevention.’…‘These values represent the mean effect’, so short peak exposures may be acceptable. However, the values are set to avoid over-heating (>38°C) in ‘almost all individuals’. Thus, some people would be more sensitive and risk over-heating.
Table 2.
Recommended maximum WBGT exposure levels (°C) at different work intensities and rest/work ratios for an average acclimatised worker wearing light clothinga
| Metabolic rate class (work intensity) | 1 (light work) WBGT (°C) | 2 (medium work) WBGT (°C) | 3 (heavy work) WBGT (°C) | 4 (very heavy work) WBGT (°C) |
|---|---|---|---|---|
| Continuous work, 0% rest/hour | 31 | 28 | 27 | 25.5 |
| 25% rest/hour | 31.5 | 29 | 27.5 | 26.5 |
| 50% rest/hour | 32 | 30.5 | 29.5 | 28 |
| 75% rest/hour | 32.5 | 32 | 31.5 | 31 |
| No work at all (100% rest/hour)b | 39 | 37 | 36 | 34 |
aThese WBGT values are taken from a graphic in the international standard (ISO, 18) and are approximate.
bFrom recommendations by NIOSH (16).
At light work intensity (200 Watts) the need for rest periods each hour starts at a WBGT of 31°C, while at heavy work intensity (500 W) this threshold occurs at a WBGT of approximately 25.5°C (Table 2). The need for preventive actions to avoid excessive heat exposure starts even earlier in accordance with the ‘reference values’ (30 and 23°C, respectively; Table 2).
The US Army and Air Force has issued advice on heat effect prevention (15) that is similar to the levels in Table 1, but this advice naturally assumes that a soldier can cope with somewhat more heat. For example, at WBGT = 32°C a soldier doing moderate work in relatively light clothing (425 W) is allowed to work 20 minutes of every hour, while the National Institute for Occupational Safety and Health (NIOSH) recommendation is for 15 minutes work per hour. As pointed out in Table 2, all of these recommendations depend on the clothing worn. The heavier the clothing is, the more rest time is required.
The WBGT is not considered ideal as an occupational heat stress index for individual work situations (19, 20) and other alternatives have been proposed; e.g. the Required Sweat Rate index (21), the Predicted Heat Strain index (22) and the Thermal Work Limit (23, 24). For the purposes of this paper we used WBGT primarily as an illustration of one of the potential consequences at population level of global climate change.
Table 2 shows a strikingly narrow WBGT range between the heat exposure level that is acceptable for continuous workplace exposure (e.g. 25.5°C at 500 W) and a 75% rest time requirement (31°C at 500 W). Kjellstrom (4) defined work capacity as the percentage of a working hour that a worker can perform his/her intended work. If no rest time is needed, because of heat, during a working hour, then the work capacity is 100%. If 75% rest time is needed, the work capacity is 25%, etc. Using this approach, Table 2 can be used to estimate loss of work capacity in heat exposed occupations for every hour of the day.
Impacts of workplace heat exposure on clinical health
Heat-related deaths at work have occasionally been reported, starting with classical studies in South Africa (25). A recent study of 423 heat-related deaths among agricultural workers in the USA, 1992–2006 (26) shows that the problem is still occurring. There are few systematic studies in low and middle-income countries of deaths or serious clinical heat stroke among heat-exposed workers, except for India where considerable research on the physiology of heat exposure and preventive approaches has been carried out by Nag and colleagues at the National Institute of Occupational Health. For instance, one study using experimental exposure chambers quantifies the ‘tolerance time’ of work at different intensities until core body temperature reaches 39°C (27). At a WBGT of 34°C, the tolerance time in heavy work goes below one hour, and it reduces by 4–5 minutes per 1°C increase of WBGT (27). These WBGT thresholds for ‘safe’ hourly continuous work are higher than those in Tables 1 and 2, but this is a natural result of using 39°C as an acceptable core body temperature rather than 38°C as in the tables. The latter temperature provides a greater safety margin for heat stroke among the workers who are sensitive to heat exposure.
The physiological basis for the different levels of clinical health damage was described briefly above and more details are given by Parsons (6) and Bridger (9). Beyond the acute heat stress, more chronic effects on the heart and kidneys may develop after repeated excessive body heating or dehydration (9).
Impacts of workplace heat exposure on worker productivity
The relationship between occupational heat exposure and productivity was pointed out as long ago as 1974 by Axelsson (28) and was further commented upon by Holmer (29), but very little research has been carried out aiming at quantifying this relationship in work situations where workers are ‘self-paced’. The slowing down of work as a defence mechanism during severe heat exposure is labelled ‘autonomous adaptation’ by climate change researchers (30). Productivity has also been analysed for indoor climates in relation to air conditioning needs (6). The first report on this issue in the context of global climate change (4) likened the heat effect on work output to the ‘disability’ caused by defined diseases, and concluded that this effect may contribute to disability in a population to a greater degree than most diseases.
A number of recent studies have analysed different aspects of the effects of heat exposure on productivity. In indoor environments, increased heat exposure reduces performance (31–33) and reducing humidity of office air in the tropics was shown to improve the perception of the work environment (34). In Bangladesh, heat reduced work performance in metal workshops (35). Protective clothing increased heat stress and reduced performance (36).
Heat stress is likely to be common during hot seasons, but culturally accepted methods to reduce impacts on health and work capacity (such as ‘siesta’) are generally effective in avoiding serious health impacts. However, these culturally accepted methods will undoubtedly reduce the hourly productivity of the exposed workers. More research to document these conditions is needed to make accurate estimates of the impacts of climate change.
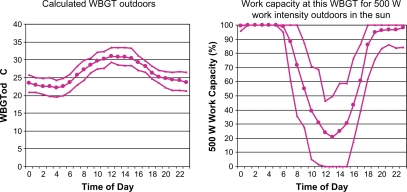
Modelling the impacts of workplace heat exposure
Lemke and Kjellstrom (to be published) used the model by Liljegren et al. (17) to calculate WBGT based on daily weather data for a selection of cities in countries with hot seasons. The WBGT levels during the hot seasons are very high in outdoor work where sun exposure is a major contributor to high WBGTs. For instance, in Delhi the calculated WBGTs during afternoons in May (the hottest month) reach above 30°C on average (Fig. 1). The resulting work capacity during different hours for a person who works at a heavy work intensity of 500 W is very low: on average only 20% of work capacity remains at 12 noon (Fig. 1). In order to avoid the midday work capacity loss, people use ‘siesta’, night work, or similar approaches to work primarily during less hot parts of each 24-hour period. However, night work is not possible for workers who rely on daylight to see their worksite (e.g. poor farmers in tropical countries). Additional examples are provided in recent technical reports (37, 38) where more detail about the methods used and the results for major cities are given.
Fig. 1.
Calculated WBGT outdoors in the sun and resulting work capacity at 500 W work intensity during different hours of a 24-hour period in Delhi, India, May 1999 (based on hourly weather data from the NOAA database; the middle line is the monthly mean, the other lines the 5 and 95 percentiles of recordings on individual days during that month).
Climate change and heat stress trends in tropical countries
The ongoing global climate change has until now been described primarily in terms of the average global temperature change. To describe changes in workplace, heat stress requires trend analysis of local temperature, humidity, wind speed and solar radiation. We will show temperature trends for selected locations as indicators of the likely trends of actual heat stress, but more detailed analysis is required for projections of future heat stress impacts.
The highest expected temperature increase due to climate change is expected close to the North Pole (1), which creates major problems for the environment, but few people live there. Densely populated areas around the planet that are expected to get the highest temperature increases due to global climate change are mainly inland areas within the large continents with an increase of 1–3°C by 2020 and 3–5°C by 2080 (1). In many of these areas the maximum temperatures during the hottest part of the year are already close to 40°C (examples in Kjellstrom et al. (37) and increasing over time (Table 3). An additional 3–5°C will make heavy work (e.g. in agriculture and construction work) very difficult during the hottest periods in most of these cities and in tropical countries in general. The ongoing changes of temperature are caused partly by the ‘heat island effect’ in many of these cities and may only partly be due to global atmospheric change.
Table 3.
Summary of recent temperature trends in selected cities from 1980 to 2007 according to regression lines based on NOAA database weather station data (source (37))
| Time trends, fitted line, temperature increase for | |||
|---|---|---|---|
| City | Maximum temp. (°C/century) | Average temp. (°C/century) | Minimum temp. (°C/century) |
| Johannesburg | +2.97 | –1.27 | –3.86 |
| Atlanta | –0.89 | +1.85 | +3.77 |
| Managua | +0.27 | +1.29 | +3.51 |
| Cairo | +2.62 | +4.84 | +6.58 |
| Athens | +4.09 | +5.30 | +5.14 |
| Delhi | +2.08 | +0.53 | +0.18 |
| Chennai | +2.87 | +0.41 | –0.43 |
| Bangkok | +4.52 | +5.19 | +5.37 |
| Chiang Mai | –1.13 | +0.22 | +0.77 |
| Osaka | +4.76 | +5.25 | +5.96 |
| Shanghai | +7.06 | +7.77 | +11.79 |
Note: Temperature change per century presented like this is comparable with the IPCC estimates for the twenty-first century, but this approach does not imply that the changes will be linear and continuous for 100 years; change per decade could be more appropriate.
Modelling by the Intergovernmental Panel on Climate Change (1) forecasts substantial increases of future annual average temperatures (and in many places also increases of humidity) in areas populated by billions of people, and it is likely that for many workers increasing WBGT index levels will affect their work capacity and create health risks. The eventual occupational impacts of such increasing heat exposure are dependent on shading from trees or roofs, clothing, radiated heat and wind speed in workplaces, but it is most likely that global climate change is a threat to safe, comfortable and productive thermal working environments for a significant part of the global population. To limit these impacts, urban planning and workplace design should consider the impacts of climate change.
Conclusions
The impact on human function and health in work situations is a ‘neglected’ effect of global climate change. The potential health risks and worker productivity reductions due to climate change are substantial. The lack of attention until recently may well be due to the fact that this is mostly a problem in low and middle-income tropical countries where climate change impacts during this century will be prominent and air conditioning is not widely available, while in high-income countries air conditioning is already very common in workplaces.
The increasing heat exposure due to local climate changes is likely to create occupational health risks and to have a significant impact on the productivity of many workers, unless effective preventive measures (‘adaptation’) reducing the occupational heat stress are implemented. This may be practically and economically possible for indoor environments, but it is much more difficult for outdoor environments. Eventually, this will hamper economic and social development in affected countries unless appropriate preventive measures are taken in the planning processes for workplaces and urban development.
Acknowledgements
Part of this information was presented at the International Conference on Biometeorology in Tokyo, Japan, in September 2008. The research was supported by funds from the Australian National University and Lund University.
Conflict of interest and funding
The authors have not received any funding or benefits from industry to conduct this study.
References
- 1.IPCC. Cambridge: Cambridge University Press; 2007. Fourth assessment report. Geneva, Inter-governmental Panel on Climate Change. Available from: www.ipcc.ch [cited 18 October 2008] [Google Scholar]
- 2.Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, et al. Lancet-University College London Institute for Global Health Commission). Managing the health effects of climate change. The Lancet. 2009;373:1693–733. doi: 10.1016/S0140-6736(09)60935-1. [DOI] [PubMed] [Google Scholar]
- 3.Oke TR. City size and the urban heat island. Atmosph Environ. 1973;7:769–79. [Google Scholar]
- 4.Kjellstrom T. Climate change, heat exposure and labour productivity. Epidemiology. 2000;11:S144. [Google Scholar]
- 5.Kjellstrom T. Climate change, direct heat exposure, health and well-being in low and middle-income countries. Global Health Action. 2009 doi: 10.3402/gha.v2i0.1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parsons K. The effects of hot, moderate and cold temperatures on human health, comfort and performance. 2nd edition. New York: CRC Press; 2003. Human thermal environment. [Google Scholar]
- 7.Ramsey JD, Bernard TE. Heat stress. Chapter 22. In: Harris RL, editor. Patty's industrial hygiene. 5th edition. New York: John Wiley and Sons; 2000. pp. 925–84. [Google Scholar]
- 8.Kerslake DM. The stress of hot environments. Cambridge: Cambridge University Press; 1972. [PubMed] [Google Scholar]
- 9.Bridger RS. Introduction to ergonomics. 2nd edition. London: Taylor & Francis; 2003. [Google Scholar]
- 10.Ramsey JD. Task performance in heat: a review. Ergonomics. 1995;38:154–65. doi: 10.1080/00140139508925092. [DOI] [PubMed] [Google Scholar]
- 11.Ramsey JD, Burford CL, Beshir MY, Jensen RL. Effects of workplace thermal conditions on safe working behavior. J Safety Res. 1983;14:105–14. [Google Scholar]
- 12.Hales JRS, Richards DAB. Heat stress-physical exertion and environment. Amsterdam: Excerpta Medica; 1987. [Google Scholar]
- 13.Leithead CS, Lind AR. Heat stress and heat disorders. London: Cassell; 1964. [Google Scholar]
- 14.Schrier RW, Hano J, Keller HI, Finkel RM, Gilliland PF, Cirksena WJ, et al. Renal, metabolic, and circulatory responses to heat and exercise. Ann Int Med. 1970;73:213–23. doi: 10.7326/0003-4819-73-2-213. [DOI] [PubMed] [Google Scholar]
- 15.USDAAF. Technical bulletin TB MED 507/AFPAM 48-152 (I) Washington, DC: US Department of the Army and Air Force; 2003. Heat stress control and heat casualty management. [Google Scholar]
- 16.NIOSH. NIOSH Publication No. 86-113. Atlanta, GA: National Institute of Occupational Health; 1986. Criteria for a recommended standard: occupational exposure to hot environments. [Google Scholar]
- 17.Liljegren JC, Carhart RA, Lawday P, Tschopp S, Sharp R. Modeling the Wet Bulb Globe Temperature using standard meteorological measurements. J Occup Environ Hyg. 2008;5:645–55. doi: 10.1080/15459620802310770. [DOI] [PubMed] [Google Scholar]
- 18.ISO. ISO Standard 7243. Geneva: International Standards Organization; 1989. Hot environments – estimation of the heat stress on working man, based on the WBGT-index (wet bulb globe temperature) [Google Scholar]
- 19.Malchaire J, Gebhardt HJ, Piette A. Strategy for evaluation and prevention of risk due to work in thermal environments. Ann Occup Hyg. 1999;43:367–76. doi: 10.1093/annhyg/43.5.367. [DOI] [PubMed] [Google Scholar]
- 20.Malchaire J, Kampmann B, Havenith G, Mehnert P, Gebhardt HJ. Criteria for estimating acceptable exposure times in hot working environments: a review. Int Arch Occup Environ Health. 2000;73:215–20. doi: 10.1007/s004200050420. [DOI] [PubMed] [Google Scholar]
- 21.ISO. ISO Standard 7933. Geneva: International Standards Organization; 1989. Hot environments – analytical determination and interpretation of thermal stress using calculation of required sweat rate. [Google Scholar]
- 22.Malchaire J, Piette A, Kampmann B, Mehnert P, Gebhardt H, Havenith G, et al. Development and validation of the Predicted Heat Strain Model. Ann Occup Hyg. 2001;45:123–35. [PubMed] [Google Scholar]
- 23.Brake DJ, Bates GP. Limiting metabolic rate (Thermal Work Limit) as an index of thermal stress. Appl Occup Environ Hygiene. 2002;17:176–86. doi: 10.1080/104732202753438261. [DOI] [PubMed] [Google Scholar]
- 24.Miller VS, Bates GP. The Thermal Work Limit is a simple reliable heat index for the protection of workers in thermally stressful environments. Ann Occup Hyg. 2007;51:553–61. doi: 10.1093/annhyg/mem035. [DOI] [PubMed] [Google Scholar]
- 25.Wyndham CH. A survey of the causal factors in heat stroke and of their prevention in the gold mining industry. J S African Inst Mining and Metallurg. 1965;66:125–55. [Google Scholar]
- 26.MMWR. Heat-related deaths among crop workers – United States, 1992–2006. JAMA. 2008;300:1017–8. [PubMed] [Google Scholar]
- 27.Nag PK, Nag A, Ashtekar SP. Thermal limits of men in moderate to heavy work in tropical farming. Ind Health. 2007;45:107–17. doi: 10.2486/indhealth.45.107. [DOI] [PubMed] [Google Scholar]
- 28.Axelsson O. Influence of heat exposure on productivity. Work Environ Health. 1974;11:94–9. [PubMed] [Google Scholar]
- 29.Holmer I. UFA Bulletin No. 4. Stockholm, Sweden: National Institute of Working Life; 1996. Assessment and prevention of heat stress at work. [Google Scholar]
- 30.Ebi KL, Smith JB, Burton I, editors. Integration of public health with adaptation to climate change. New York: Taylor & Francis; 2005. [Google Scholar]
- 31.Fisk WJ. Health and productivity gains from better indoor environments and their relationship with building energy efficiency. Ann Rev Energy Environ. 2000;25:537–66. [Google Scholar]
- 32.Witterseh T, Wyon DP, Clausen G. The effects of moderate heat stress and open-plan office noise distraction on SBS symptoms and on the performance of office work. Indoor Air. 2004;14:30–40. doi: 10.1111/j.1600-0668.2004.00305.x. [DOI] [PubMed] [Google Scholar]
- 33.Wyon DP. The effects of indoor air quality on performance and productivity. Indoor Air. 2004;14:92–108. doi: 10.1111/j.1600-0668.2004.00278.x. [DOI] [PubMed] [Google Scholar]
- 34.Gunnarsen L, Santos AMB. Reduced heat stress in offices in the tropics using solar powered drying of supply air. Indoor Air. 2002;12:252–62. doi: 10.1034/j.1600-0668.2002.07115.x. [DOI] [PubMed] [Google Scholar]
- 35.Ahasan MR. Work related problems in metal handling tasks in Bangladesh: obstacles to the development of safety and health measures. Ergonomics. 1999;42:385–96. doi: 10.1080/001401399185739. [DOI] [PubMed] [Google Scholar]
- 36.Bernard TE. Heat stress and protective clothing: an emerging approach from the United States. Ann Occup Hyg. 1999;43:321–7. [PubMed] [Google Scholar]
- 37.Kjellstrom T, Lemke B, Dear K. Climate change, urban heat exposure, and occupational health impacts; Report from National Centre for Epidemiology and Population Health, Australian National University; (in press) [Google Scholar]
- 38.Kjellstrom T. Technical report. Stockholm, Sweden: National Institute of Environmental Medicine; 2009. Global climate change and health – a new theme for research in environmental medicine. Available from: http://www.imm.ki.se/klimatrapport [cited October 2009] [Google Scholar]