Abstract
Background
The aim of this paper is to summarise what is known about human response to heat and to use this knowledge to provide guidance on how to maintain the health, comfort and performance of people in heat waves.
Design
The use of power and especially water are critical in providing cooling. A practical method of cooling people in a water bath is described. A warm bath slowly cooled will provide effective cooling but not thermal trauma.
Result
It is concluded that for sedentary and light activities, it is not necessary to cool offices or homes below 25°C for thermal comfort.
Conclusion
To compare the costs due to loss of productivity caused by a heat wave, with the cost of taking action, more research is needed into the relationship between levels of heat stress and how much distraction and ‘time off task’ it causes.
Keywords: heat physiology, heat waves, health, comfort, productivity
The principles behind how people respond to heat and conditions which would influence health, comfort and human performance have been extensively studied and are well understood (1). To avoid unacceptable heat strain in specific populations and in specific contexts requires the application of those principles into guidelines and heat management systems. How to do that is not well understood.
Heat stress is determined by the metabolic heat production of the body, which increases with level of activity (even at rest a person produces around 100 W of heat) and the ability to lose heat to the environment so that heat stored in the body does not raise body temperature to unacceptable levels. Clothing will restrict heat loss (or gain) between the skin and the environment, which is determined by air temperature, radiant temperature, humidity and air velocity. It is the interaction and combined effect of these six factors that determines the level of heat stress.
Heat strain is a consequence of the response of the body to heat stress. Increased heart rate and blood flow to the skin, and sweating can cause illness and death in vulnerable people even when internal body temperatures are at what would normally be considered to be acceptable levels. Sweating can lead to dehydration and as well as increased body temperature can lead to collapse, heat stroke and death.
This paper provides a summary of physiological responses to heat and presents methods for reducing heat strain. The aim of the paper is to consider the application of knowledge of human response to heat, to provide methods for maintaining the health, comfort and productivity of people during a prolonged and atypical period of hot weather (a heat wave).
Physiological response to heat
In heat stress the body temperature may rise and receptors sensitive to change in temperature in the skin, muscle, stomach and other areas of the central nervous system, as well as in the anterior hypothalamus itself, all send signals via the central nervous system to the anterior hypothalamus. The ratio of sodium to calcium ions is also monitored. Where temperatures are above ‘set point’ levels, blood circulation is controlled in specific areas of the body through the sympathetic nervous system which dilates the cutaneous vascular bed, and hence increases skin blood flow and invokes the sweating mechanism if necessary. This provides greater potential for heat to flow from the body and hence maintain body temperature. Because the heart cannot supply blood to all of the body's organ systems, the autonomic nervous and endocrine system control allocation of blood to competing organs.
During exercise there is an initial sympathetic vasoconstriction, so that blood may flow to active muscles. If heat is required to be dissipated there is an increased cutaneous blood flow. During continuous work, in the heat, central nervous blood volume decreases as the cutaneous vessels dilate. The stroke volume falls and the heart rate must increase to maintain cardiac output. The effective circulatory volume also decreases as water is lost through sweating.
Sweat glands are stimulated by cholinergic sympathetic nerves and secrete sweat onto the surface of the skin. Sweat rates of 1 L per hour are common and for each litre evaporated, 675 W of heat are lost per hour (2). However, large sweat losses reduce body water content and hence thermoregulatory effectiveness. During sweating, salt is lost at about 4 g per litre (1 g per litre in acclimatised persons). As a normal diet provides 8–14 g of salt per day, then a normal diet is often sufficient. Salt tablets can irritate the stomach and heavier use of salt at meals is preferred, but salt supplementation will normally not be required (2). Potassium is also lost in sweat and a high salt intake may increase potassium loss. In most cases, however, potassium will be replaced by a normal diet (especially fruits and vegetables).
The overall physiological response for continued heat storage is therefore vasodilatation to increase skin temperature and then sweating leading to profuse sweating (including ineffective dripping of some sweat losing insignificant heat but important water). As ‘core’ temperature continues to rise and the skin is completely wet, hidromeiosis (a reduction in sweating) may occur due to swelling and blocking of sweat glands in the wet humid conditions (3). This is often confused with so-called sweat gland fatigue. The decrease in sweating promotes a further, often rapid, increase in ‘core’ temperature to beyond 38–39°C, where collapse may occur to above 41°C (rectal temperature) and heat stroke may occur. There will be mental confusion, behavioural changes, failure in central nervous thermoregulation and sweating, and death with eventual denaturing of body protein. National Institute for Occupational Safety and Health (NIOSH) (2) consider age, gender, body fat, drugs (including alcohol) and other non-thermal disorders as important individual factors. There is a large individual variability in the mechanisms of response, which are not fully understood. Physical fitness, however, has been shown to be of great importance. The mnemonic, ‘SHAFTS’ can be used to advise people how to increase tolerance to heat. This is: Sensible (i.e. appropriate behaviour; reduce exercise or work activity); Hydrated; Acclimatised; Fit; Thin: and Sober (including avoidance of alcohol and other drugs).
Heat physiology and health
Leithead and Lind (4) conclude that heat disorders occur for one or more of three reasons:
the existence of factors such as dehydration or lack of acclimatisation;
the lack of proper appreciation of the dangers of heat, either on the part of the supervising authority or of the individuals at risk; and
accidental or unforeseen circumstances leading to exposure to very high heat stress.
They conclude that many heat-related deaths can be attributed to neglect and lack of consideration and that even when disorders do occur much can be done if all the requirements for the correct and prompt remedial treatment are available. In climates such as those found in Singapore, military personnel are exposed to hot, humid conditions and must carry out essential tasks in protective clothing. Although heat stroke will occur, severe consequences have been avoided by organisational methods including extensive training of personnel and an efficient back-up system to transport casualties rapidly to hospital.
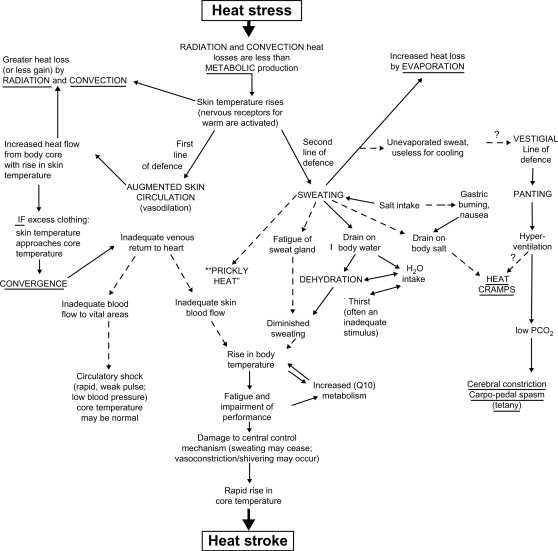
There are a number of classification systems for heat disorders. The mechanisms are summarised in Fig. 1 (5) and a description is provided in Table 1 (6).
Fig. 1.
Causes of heat stroke (from Ref. (5))
Table 1.
Classification, medical aspects and prevention of heat illness (from (6))
| Category and clinical features | Predisposing factors | Underlying physiological disturbance | Treatment | Prevention |
|---|---|---|---|---|
| 1. Temperature regulation heatstroke | ||||
| Heatstroke: (1) hot dry skin usually red, mottled or cyanotic; (2) tre, 40.5°C (104°F) and over; (3) confusion, loss of consciousness, convulsions, tre continues to rise; fatal if treatment delayed | (1) Sustained exertion in heat by unacclimatised workers; (2) lack of physical fitness and obesity; (3) recent alcohol intake; (4) dehydration; (5) individual susceptibility; and (6) chronic cardiovascular disease | Failure of the central drive for sweating (cause unknown) leading to loss of evaporative cooling and an uncontrolled accelerating rise in tre, there may be partial rather than complete failure of sweating | Immediate and rapid cooling by immersion in chilled water with massage or by wrapping in wet sheet with vigorous fanning with cool dry air, avoid overcooling, treat shock if present | Medical screening of workers, selection based on health and physical fitness, acclimatisation for 5–7 days by graded work and heat exposure, monitoring workers during sustained work in severe heat |
| 2. Circulatory hypostasis heat syncope | ||||
| Fainting while standing erect and immobile in heat | Lack of acclimatisation | Pooling of blood in dilated vessels of skin and lower parts of body | Remove to cooler area, rest recumbent position, recovery prompt and complete | Acclimatisation, intermittent activity to assist venous return to the heart |
| 3. Water and/or salt depletion | ||||
| (a) Heat exhaustion | ||||
| (1) Fatigue, nausea, headache and giddiness; (2) skin clammy and moist; complexion pale, muddy or hectic flush; (3) may faint on standing with rapid thready pulse and low blood pressure; (4) oral temperature normal or low but rectal temperature usually elevated (37.5–38.5°C) (99.5–101.3°F); water restriction type; urine volume small, highly concentrated; salt restriction type; urine less concentrated, chlorides less than 3 g/L | (1) Sustained exertion in heat; (2) lack of acclimatisation; and (3) failure to replace water lost in sweat | (1) Dehydration from deficiency of water; (2) depletion of circulating blood volume; (3) circulatory strain from competing demands for blood flow to skin and to active muscles | Remove to cooler environment, rest recumbent position, administer fluids by mouth, keep at rest until urine volume indicates that water balances have been restored | Acclimatise workers using a breaking-in schedule for 5–7 days, supplement dietary salt only during acclimatisation, ample drinking water to be available at all times and to be taken frequently during work day |
| (b) Heat cramps | ||||
| Painful spasms of muscles used during work (arms, legs or abdominal); onset during or after work hours | (1) Heavy sweating during hot work; (2) drinking large volumes of water without replacing salt loss | Loss of body salt in sweat, water intake dilutes electrolytes, water enters muscles, causing spasm | Salted liquids by mouth or more prompt relief by I-V infusion | Adequate salt intake with meals; in unacclimatised workers supplement salt intake at meals |
| 4. Skin eruptions | ||||
| (a) Heat rash (miliaria rubra; ‘prickly heat’) | ||||
| Profuse tiny raised red vesicles (blister-like) on affected areas, pricking sensations during heat exposure | Unrelieved exposure to humid heat with skin continuously wet with unevaporated sweat | Plugging of sweat gland ducts with retention of sweat and inflammatory reaction | Mild drying lotions, skin cleanliness to prevent infection | Cool sleeping quarters to allow skin to dry between heat exposures |
| (b) Anhydrotic heat exhaustion (miliaria profunda) | ||||
| Extensive areas of skin which do not sweat on heat exposure, but present gooseflesh appearance, which subsides with cool environments; associated with incapacitation in heat | Weeks or months of constant exposure to climatic heat with previous history of extensive heat rash and sunburn | Skin trauma (heat rash; sunburn) causes sweat retention deep in skin, reduced evaporative cooling causes heat intolerance | No effective treatment available for anhydrotic areas of skin, recovery of sweating occurs gradually in return to cooler climate | Treat heat rash and avoid further skin trauma by sunburn, periodic relief from sustained heat |
| 5. Behavioural disorders | ||||
| (a) Heat fatigue – transient | ||||
| Impaired performance of skilled sensorimotor, mental or vigilance tasks, in heat | Performance decrement greater in unacclimatised and unskilled worker | Discomfort and physiologic strain | Not indicated unless accompanied by other heat illness | Acclimatisation and training for work in the heat |
| (b) Heat fatigue – chronic | ||||
| Reduced performance capacity, lowering of self-imposed standards of social behaviour (e.g. alcoholic over-indulgence), inability to concentrate, etc. | Workers at risk come from temperate climates, for long residence in tropical latitudes | Psychosocial stresses probably as important as heat stress, may involve hormonal imbalance but no positive evidence | Medical treatment for serious cases, speedy relief of symptoms on returning home | Orientation on life in hot regions (customs, climate, living conditions, etc.) |
There are a number of other complaints related to heat exposure. For example, in mildly sunburnt skin, sweat can be trapped and accumulate under the dead surface layer and cause discomfort as well as reducing evaporative efficiency. In industries where chemicals and particulates are present in the air, they may interact with sweat on the skin surface to cause complaints. The interaction between chemical substances in the air and a sweating person has yet to be fully explored but can be significant. Pollution and poor air quality may be an additional hazard along with heat and in combination may cause and exacerbate respiratory disorders. Protective clothing and equipment may promote sweating and will reduce the ability to evaporate sweat to cool down. This will often increase the risk for the person the clothing is protecting against and dangerous levels can occur at what would normally be considered to be moderate temperatures.
Acclimatisation
Acclimatisation refers to the increased ability of a person to reduce heat strain due to experience of exposure to heat. It takes two forms: behavioural and physiological. Behavioural acclimatisation is most effective and is mainly gained in the context of the heat exposure. If we go to a hot climate, we soon learn to drink appropriately and keep out of the sun. Physiological acclimatisation involves adjustments to our ability to thermoregulate and allow a greater capacity for and more efficient vasodilatation and in particular, sweating. When people become exposed to heat they increase their ability to sweat (7). Significant changes occur even after only three days of exposure. It is possible to gain physiological acclimatisation by exposing people for a few hours per day to high levels of heat (e.g. in a laboratory – called acclimation) and this is often used as a technique to reduce strain when people are about to travel to a hot climate.
In short, if a person is used to being exposed to heat then he/she will adjust physiologically to some extent and learn how to behave to tolerate the heat. In extremely hot tropical environments this ‘behavioural change’ will include a reduction of physical activity workload, and an increase of frequency and length of rest breaks. If they are not used to the heat and when the weather suddenly becomes hot, then they will be more vulnerable to heat strain.
Maintaining health in heat waves
There is no reason why a person should suffer ill health in a heat wave as the principles of reducing heat strain are well understood. The requirement is that we have adequate management systems based upon these principles. Physiological responses to heat have generally been studied on fit young males and under conditions that could be regarded as very hot and towards the extremes of weather conditions. For less fit and vulnerable people, physiological responses such as increased heart rate, prolonged sweating and respiratory responses (related to air quality or dryness) will pose a threat. Increased body temperature will eventually be a threat to health, but it may not be the primary cause of illness and death in a heat wave.
So what we do to maintain health? We set up a management system to ensure that people are not exposed to unacceptable heat stress. Heat stress is determined by the interaction of air temperature, radiant temperature, air velocity and humidity. It is also greatly influenced by the clothes a person is wearing and the activity they are performing. Consideration of these six factors must form the basis of any management programme. A full discussion of management programme for heat waves is provided in (8). Of particular importance will be the availability of household water and electrical power. Moving people away from hot homes to cooler areas (e.g. public libraries or modern shopping centres) will reduce heat strain but may not be practicable. The use of water provides an effective and often practical method of keeping cool in the heat. Simply plunging the hands and feet into cool water reduces thermal strain. Immersing hands and arms in cool water is a practical way for vulnerable people to avoid health problems in the heat. For those with a bathtub, running a normal warm bath (e.g. 38°C water temperature) to half full and getting in, then running in cool water to fill the bath allows a non-stressful method of keeping cool. The initial warm water will promote vasodilatation and will not cause thermal shock, which will occur with cool water and raise blood pressure. The body will not detect the slow cooling and at around 30°C a ‘cool’ bath will greatly enhance heat loss.
Spraying water on the face or exposed skin and enhancing evaporative cooling with fans, for example, will reduce heat loss even when the air temperature is above desired internal body temperature. The direction and strength of fans, however, has to be controlled as evaporation of mucous from the airways and moisture from the eyes can cause irritation and respiratory problems.
The use of air conditioning is very effective in reducing air temperature and hence thermal strain. It requires electrical power, however, and if electric grid systems cannot meet capacity then lack of power can cause a critical problem. The above discussion provides methods for keeping cool in a heat wave. It is not exhaustive and the reader is referred to (8) for a complete discussion.
Maintaining comfort in heat waves
Conditions for thermal comfort are well described by Fanger (9) and were later adopted worldwide in ISO 7730 (10). They are, that for a person to be in thermal comfort, he/she must be in heat balance (maintaining internal body temperature) and that skin temperatures and sweat rates must be within comfort limits. A method is derived from those three premises that allows the prediction (from air temperature, radiant temperature, air velocity, humidity, clothing and activity) of thermal comfort conditions and of any thermal discomfort. The predicted mean vote (PMV) index predicts the mean rating of a large group of people exposed to thermal conditions (six factors above) on the scale: +3 hot; +2 warm; +1 slightly warm; 0 neutral; –1 slightly cool; –2 cool; –3 cold. For a given PMV value, the predicted percentage of dissatisfied (PPD) provides the likely level of dissatisfaction.
Parsons (1) and Hodder and Parsons (11) extend the scale from 7 to 11 points by adding very hot/cold and extremely hot/cold on either end. They then provide a simple rule of thumb method for taking account of the direct sun on a person. For every 200 Wm−2 of solar radiation (from 0 Wm−2 totally cloudy to 600 blue sky to 1,000 absolute maximum), the PMV (now PMVsolar) is increased by one scale value. It is emphasised that this rule of thumb provides a simplistic practical method which accounts for main effects. For a more accurate assessment, direct and diffuse radiation, depending upon turbidity and cloudiness, elevation of the sun, posture of the person and more, also play a role but involve increasingly complex analysis.
To take account of the ability for people to change behaviour or adapt to the environment, Parsons (1) suggested an Iequiv index which allows the clothing insulation value, used in the calculation of PMV, to be adjusted to take account of the effects of any adaptive opportunities in the environment (e.g. ability to reduce clothing, open windows, etc.). The Iequiv method provides a simplistic but direct method of accounting for adaptive opportunities available to people. Estimates of adaptive opportunity, however, remain necessarily subjective. There are other, less rational or ‘causal’ adaptive models which relate indoor comfort temperatures to outside conditions based upon data from thermal comfort surveys (e.g. 12). The ‘causal’ model assumed in such models is that the effects of the adaptive opportunity, such as that used in the Iequiv method, are captured in the behaviour of people to outside conditions, for example, a reduction in clothing when outside temperatures are high. The Iequiv method suggests that a consequence of this is to provide the suggestion that for reasonable levels of adaptive opportunity, it will not be necessary to cool offices or homes below 25°C to provide thermal comfort. This measure is related to sustainable thermal comfort discussions (13) and will also have the effect of significantly reducing electrical power requirements and hence avoiding power failure. It is interesting to note that in Japan a few years ago, the government in Tokyo ran a campaign to set a lower limit for cooling offices to 28°C air temperature. The Prime Minister at the time advised businessmen not to wear a tie. The 28°C limit clearly requires less energy to achieve in hot outside conditions than a limit of 25°C or below, however, it is likely to cause some discomfort. The practical point is that it is a common practice to cool rooms to around 20°C (and often causes cold discomfort) in hot outside conditions. This is an unnecessary and inefficient use of energy. Energy saving by not cooling below 25°C would be highly significant worldwide and it is generally agreed would still allow thermal comfort.
Maintaining productivity in heat waves
The most effective way to maintain human performance and productivity during a heat wave is to provide thermal comfort conditions. This is not always possible, however, and in hot conditions productivity is likely to fall. This is by no means certain, however, and motivation, morale and team spirit will all be significant factors. There have been numerous studies into the effects of heat on manual dexterity and cognitive performance. The most direct and measurable effect on productivity, however, is ‘time off task’ (1) caused by work having to be stopped or due to heat causing a distraction to people (e.g. concentrating or finding fans or adjusting control systems or simply paying attention to the heat). This will apply to people in homes, offices and other work places. The relationship between the level of distraction caused by heat and the level of heat stress is not known. Further investigation is needed if the full economic costs of heat waves are to be determined. For practical purposes the costs in terms of health and loss in productivity can be weighed against the costs of systems for ensuring the avoidance of unacceptable thermal strain during heat waves.
Conclusions
Much is known about human response to heat and basic principles can be used to provide guidance on effective heat management systems.
With electrical power and especially water, it is possible to avoid health problems due to heat.
For sedentary and light activities it is not necessary to cool rooms below 25°C to provide thermal comfort.
There is a need to determine the relationships between levels of heat stress and how much distraction and time off work it causes.
Conflict of interest and funding
The author has not received any funding or benefits from industry to conduct this study.
References
- 1.Parsons K. Human thermal environments. London: Taylor & Francis; 2003. [Google Scholar]
- 2.NIOSH. DHHS (NIOSH) Publication No. 86–113. Washington, DC: National Institute for Occupational Safety and Health; 1986. Occupational exposure to hot environments. [Google Scholar]
- 3.Kerslake D Mck. Cambridge: Cambridge University Press; 1972. The stress of hot environments. [PubMed] [Google Scholar]
- 4.Leithead CS, Lind AR. Heat stress and heat disorders. London: Cassell; 1964. [Google Scholar]
- 5.Belding HS. The search for a universal heat stress index. In: Hardy JD, Thomas CC, editors. Physiological and behavioural temperature regulation. IL: Springfield; 1970. [Google Scholar]
- 6.Goldman RF. Standards for human exposure to heat. In: Mekjavic IB, Banister EW, Morrison JB, editors. Environmental ergonomics. London: Taylor & Francis; 1988. pp. 99–136. [Google Scholar]
- 7.Clark RP, Edholm OG. Man and his thermal environment. London: Edward Arnold; 1985. [Google Scholar]
- 8.Menne B, Ebi KI. Climate change and adaptation strategies for human health. Darmstadt: Springer; 2006. [Google Scholar]
- 9.Fanger PO. Thermal comfort. Copenhagen: Danish Technical Press; 1970. [Google Scholar]
- 10.ISO 7730. Ergonomics of the thermal environment – analytical determination and interpretation of thermal comfort using calculation of the PMV and PPD indices and local thermal comfort. Geneva, Switzerland: ISO; 2005. [Google Scholar]
- 11.Hodder S, Parsons KC. The effects of solar radiation on thermal comfort. Int J Biometeorol. 2006;51:233–50. doi: 10.1007/s00484-006-0050-y. [DOI] [PubMed] [Google Scholar]
- 12.De Dear RJ, Brager GS. ASHRAE Transactions; 1998. Developing an adaptive model of thermal comfort and preference. [Google Scholar]
- 13.Parsons K. Sustainable thermal comfort. Materials for energy efficiency and comfort in occupied spaces. In: Hall M, editor. Woodhead Publishing; in press. [Google Scholar]