Abstract
Background:
Gallbladder cancer is the most common malignancy of the biliary tract. Radical surgery (including liver resection and regional lymphadenectomy) is applied for some gallbladder cancers, but the benefits of these procedures are unproven. For patients with T1b cancers discovered incidentally on cholecystectomy specimens, the utility of radical surgery remains debated.
Methods:
A decision analytic Markov model was created to estimate and compare life expectancy associated with management strategies for a simulated cohort of patients with incidentally discovered T1b gallbladder cancer after routine cholecystectomy. In one strategy, patients were treated with no additional surgery; in another, patients were treated with radical resection. The primary (base-case) analysis was calculated based on a cohort of 71-year-old females and incorporated best available input estimates of survival and surgical mortality from the literature. Sensitivity analysis was performed to assess the effects of model uncertainty on outcomes.
Results:
In the base-case analysis, radical resection was favoured over no further surgical resection, providing a survival benefit of 3.43 years for patients undergoing radical resection vs. simple cholecystectomy alone. Sensitivity analysis on the age at diagnosis demonstrated that the greatest benefit in gained life-years was achieved for the youngest ages having radical resection, with this benefit gradually decreasing with increasing age of the patient. High peri-operative mortality rates (≥36%) led to a change in the preferred strategy to simple cholecystectomy alone.
Conclusions:
Decision analysis demonstrates that radical resection is associated with increased survival for most patients with T1b gallbladder cancer.
Keywords: gallbladder cancer, T1b, decision analysis, surgery
Introduction
Gallbladder cancer is the most common malignancy of the biliary tract.1 Curative surgical resection remains the best method for achieving long-term survival. There is considerable debate as to whether T1b gallbladder cancers (tumour invading into, but not through, the muscularis propria) are best treated by simple cholecystectomy alone or by radical resection (including liver resection and regional lymphadenectomy).2,3 Although some authors suggest that simple cholecystectomy is sufficient,1,4–9 others advocate radical resection.3,10–17
Because of the low incidence of gallbladder cancer, it is unlikely that controlled clinical trials that would resolve this debate will ever be conducted.
Decision analysis provides an ideal method for assessing treatment paradigms for the management of T1b gallbladder cancer, enabling incorporation of risks and benefits of each strategy. In this study, the survival benefit of radical gallbladder resection was evaluated using decision-analytic techniques. A decision-analytic Markov model was developed to estimate life expectancy associated with each intervention for a simulated cohort of patients with incidentally discovered T1b gallbladder cancer found on gallbladder specimens. One group had no additional surgery and patients were observed. In the second group, patients were treated with radical resection. The stability of results to changes in key parameters were evaluated in sensitivity analysis.
Material and methods
Decision tree
A decision-analytic Markov model was developed to estimate life expectancy for 71-year-old women with T1b gallbladder cancer (Fig. 1). The primary (base-case) analysis incorporated specified best available model input estimates. Stability of results over changes in model estimates was evaluated in secondary (sensitivity) analysis. The age of 71 was used, as it was the mean age of diagnosis reported in a recently published study of over 4000 patients with early-stage gallbladder cancers in the Surveillance, Epidemiology, and End Results (SEER) tumour registry.18 In this same study, women comprised the majority of patients with early gallbladder cancer.18 The model decision tree was constructed and analysed using software (TreeAge Pro, 2007; TreeAge Software, Williamstown, MA, USA).
Figure 1.
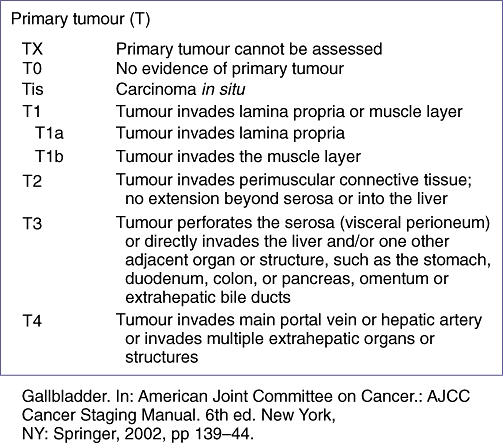
Gall bladder cancer T-stage as described in: American Joint Committee on Cancer.: AJCC Cancer Staging Manual. 6th ed. New York, NY: Springer, 2002, pp 139–144
Markov model
The cohorts' post-treatment life-time course was estimated using a Markov model with a 1-year cycle length. We constructed this model in keeping with widely accepted methods for Markov modelling in medicine.19
Patients entered the model after incidental discovery of T1b gallbladder cancer after or during simple cholecystectomy. Some patients had no additional surgery, whereas the others were treated with radical gallbladder resection in a second operation. Patients in the ‘radical resection’ group were faced with an initial risk of peri-operative death. Patients in both groups faced potential cancer-specific mortality each year after diagnosis. Patients in both groups were also subject to non-cancer mortality.
Model data and data sources
For data collection of probabilities, an initial systematic Medline search was conducted using the keyword search terms ‘gallbladder cancer and survival and surgery’ to identify survival data for patients undergoing surgical treatment for T1b gallbladder cancer. Upon detailed review of the selected articles and corresponding references, additional articles were subsequently identified that met inclusion criteria. Critical appraisal of each study was performed and studies were selected on the basis of the inclusion criteria used for this analysis (See Fig. 2).
Figure 2.
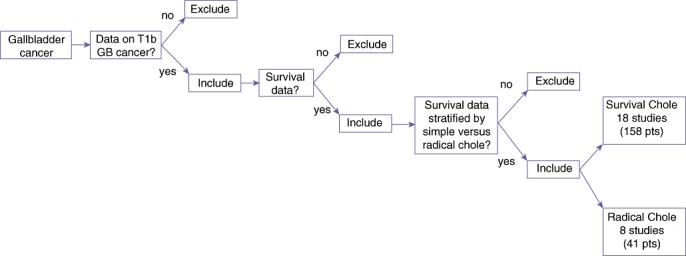
Algorithm illustrating criteria used for inclusion and exclusion of literature reporting 5-year survival for T1b gallbladder cancer patients treated with simple cholecystectomy or radical resection
For the purposes of this study, reviewed publications were excluded from our analysis if: (i) the number of patients undergoing surgical resection; or (ii) 5-year survival data for those patients were unavailable.
A second search was conducted using the keywords ‘gallbladder cancer and perioperative mortality and radical cholecystectomy’ in order to obtain peri-operative mortality statistics. Representative studies containing peri-operative mortality for patients undergoing radical resection (not just those for T1b cancers) were included.
Letters, reviews without original data, animal studies, studies without survival data and overlapping studies were also excluded from our analysis.
For survival data in the simple cholecystectomy alone group, data were included regardless if the procedure was performed by laparoscopic or open technique. In the radical resection group, survival data were included if the procedure was completed during the initial operation (cancer discovered intraoperatively) or if a simple cholecystectomy was performed on the initial operation and followed at a later date with a more extended resection (e.g. discovered on pathology reports post-operatively followed by radical resection). For the radical resection group, we initially attempted to include only those patients undergoing at least a wedge resection of the liver bed and regional lymphadenectomy. However, in a few studies survival data include a few patients who had undergone less extensive procedures (only a lymphadenectomy and cholecystectomy) or slightly more extensive procedures (cholecystectomy, liver resection, bile duct resection).
In studies that did not explicitly state survival time periods in the text, we have estimated the survival based on the data given in tables, text, or presented Kaplan–Meier survival curves.
Peri-operative mortality was defined as death within 30 days of the surgery. However, in-hospital or operative mortality (procedure-related) was used as a substitute for peri-operative mortality when death within 30 days of surgery was not reported.
Non-cancer-related mortalities were incorporated into the model using data from the United States Year 2000 Life-Tables.20
Decision analysis models and calculations
Weighted means were calculated for the: (i) 5-year survival for those patients undergoing simple cholecystectomy; (ii) 5-year survival for those patients undergoing radical cholecystectomy; and (iii) peri-operative mortality associated with a radical cholecystectomy. Weighted means were considered baseline estimates and were weighted based on the number of patients contributing to the particular mean.
Calculated 5-year cancer-specific survival probabilities were converted to 1-year cancer-specific mortality probabilities for use in the decision-analytic Markov model, using the standard assumption of an exponential relationship between an event probability (p) and hazard rate (r) over a specified time period (t), which can be expressed as p = 1 − e−rt.21,22
For those studies reporting overall (not cancer specific-) survival, we calculated an adjusted cancer-specific mortality rate utilizing data of female, age-based mortality rates from the United States Life Tables, 2000.20
Sensitivity analysis
Sensitivity analysis was performed to evaluate the effects of model assumptions and parameters on results. Specifically, sensitivity analysis was performed for the peri-operative mortality rate, age of diagnosis and gender. A threshold value was calculated in cases for which a change in the preferred strategy was traversed.
Results
Studies used in the analysis are shown in Tables 1 and 2 for the group undergoing simple cholecystectomy alone and the group undergoing radical cholecystectomy, respectively. Overall, a total of 18 studies including 157 patients and 7 studies including 40 patients were used to calculate baseline probabilities for the simple- and radical cholecystectomy groups, respectively. For the simple cholecystectomy alone group, we calculated a weighted mean 5-year cancer-specific survival of 61.3%. For those patients undergoing radical resection we obtained a mean 5-year survival of 87.5% (Table 4). Weighted peri-operative mortality was slightly less than 2% (Tables 3 and 4). For those 40 patients having a radical cholecystectomy, we calculated a weighted probability of lymph node metastases to be 2.5%.
Table 1.
Published studies reporting 5-year survival for patients with T1b gallbladder cancers treated with simple cholecystectomy alone
| Author | Institution | Patients | 5-year survival |
|---|---|---|---|
| Wagholikar et al.13 | Sanjay Gandhi, India | 7 | 57 |
| Cangemi et al.12 | University of Rome, Italy | 8 | 37.5 |
| Mizumoto et al.29 | Mie University, Japan | 9 | 100 |
| Kim et al.30 | Catholic University, Korea | 3 | 100 |
| Wakai et al.9 | Niigata University, Japan | 13 | 100 |
| Ouchi et al.31 | Miyagi Cancer Cent, Japan | 2 | 50 |
| Principe et al.15 | University of Bologna, Italy | 1 | 0 |
| Kwon et al.2 | Kansai University, Japan | 2 | 100 |
| Yagi et al.32 | Keio University, Japan | 1 | 100 |
| Foster et al.33 | Roswell Park, Buffalo, USA | 2 | 50 |
| Cucinotta et al.14 | University of Messina, Italy | 6 | 0 |
| Sun et al.8 | Yonsei University, Japan | 5 | 100 |
| Nevin et al.34 | M.C.V. & Memorial Hosp, USA | 5 | 100 |
| Benoist et al.35 | French Cooperative Group | 23 | 74 |
| Shibata et al.36 | Oita University, Japan | 1 | 100 |
| Yamamoto et al.37 | Kobe University, Japan | 15 | 93a |
| Goetze et al.23 | Multiple centers, Germany | 49 | 45a |
| Puhalla et al.38 | University of Vienna, Austria | 5 | 44a |
Calculated cancer-specific mortality.
Table 2.
Published studies reporting 5-year survival for patients with T1b gallbladder cancers treated with radical cholecystectomy
| Author | Institution | Patients | 5-year survival |
|---|---|---|---|
| Cangemi et al.12 | University of Rome, Italy | 3 | 100 |
| Mizumoto et al.29 | Mie University, Japan | 3 | 100 |
| Kim et al.30 | Catholic University, Korea | 2 | 100 |
| Wakai et al.9 | Niigata University, Japan | 7 | 92 |
| Ouchi et al.31 | Miyagi Cancer Cent., Japan | 1 | 100 |
| Shibata et al.36 | Oita University, Japan | 1 | 0 |
| Goetze et al.23 | Multiple centers, Germany | 23 | 85a |
Calculated cancer-specific mortality.
Table 4.
Study variables
| Variable | Weighted average (%) | Range (%) |
|---|---|---|
| 5-year survival (simple cholecystectomy) | 61.3 | 0–100 |
| 5-year survival (radical cholecystectomy) | 87.5 | 0–100 |
| Perioperative mortality | 2 | 0–6 |
Table 3.
Published studies reporting peri-operative mortality associated with radical resection for gallbladder cancer
| Author | Institution | Patients | Periop mortality |
|---|---|---|---|
| Cubertafond et al.39 | French Surgical Association | 724 | 22 |
| Tsukada et al.40 | First Department of Surgery, Japan | 106 | 0.9 |
| Todoroki et al.41 | Institute of Clinical Medicine, Japan | 135 | 3.7 |
| Bartlett et al.42 | Memorial Sloan, USA | 23 | 0 |
| Ouchi et al.31 | Miyagi Cancer Cent., Japan | 4 | 0 |
| Shirai et al.43 | Niigata University, Japan | 14 | 7.1 |
| Fong et al.44 | Memorial Sloan, USA | 19 | 5.3 |
| Todoroki et al.41 | University of Tsukuba, Japan | 135 | 3.7 |
| Muratore et al.10 | Umberto I Mauriziano Hospital, Italy | 33 | 3 |
| Yoshida et al.45 | Oita Medical University, Japan | 35 | 0 |
| Suzuki et al.46 | Fujimnomiya City General Hospital, Japan | 12 | 0 |
| Mondragon-Sanchez et al.47 | Instituto Nacional de Cancerologia, Mexico | 20 | 10 |
| Frena et al.48 | Regional Hospital of Bolzano, Italy | 20 | 0 |
| Yamaguchi et al. | Kyushu University, Japan | 4 | 0 |
| Onoyama et al.49 | Saiseikai Nakatsu Hospital, Japan | 32 | 0 |
| Puhalla et al.38 | University of Vienna, Austria | 32 | 6.3 |
| Behari et al.50 | Sanjay Gandhi, India | 42 | 4.8 |
| Toyonaga et al.7 | Kyushu University, Japan | 21 | 0 |
| Taner et al.51 | Mayo Clinic, USA | 60 | 1.7 |
| Yildirim et al.52 | Ankara, Turkey | 28 | 0 |
| Foster et al.33 | Roswell Park, USA | 13 | 0 |
| Yagi et al.32 | Keio University, Japan | 47 | 0 |
| Chan et al.53 | University of Hong Kong, China | 12 | 0 |
| Principe et al.15 | University of Bologna, Italy | 29 | 0 |
| Benoist et al.35 | Hopital Henri-Mondor, France | 21 | 4.8 |
| Schauer et al.5 | Ludwig-Maximilian University, Germany | 23 | 0 |
| Cangemi et al.12 | Peitro Valdoni, Italy | 3 | 0 |
| Wagholikar et al.13 | Sanjay Gandhi, India | 2 | 0 |
| Reddy et al.54 | Duke University, USA | 22 | 4.5 |
| Shih et al.28 | Johns Hopkins, USA | 50 | 4 |
| Ito et al.55 | Brigham and Women's, USA | 8 | 0 |
Our Markov model (shown in Fig. 3) demonstrates the two potential treatment arms: radical resection vs. no additional surgery. Patients in the radical resection group were faced with an initial potential for a peri-operative death. Patients in both groups faced potential cancer-specific mortality each year after diagnosis. And finally, patients in both groups were subject to non-cancer-related mortalities.
Figure 3.
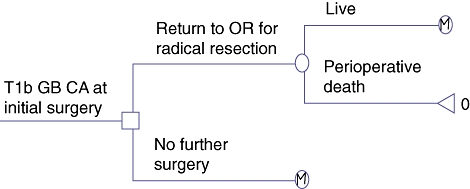
Decision tree for treatment of patients with incidentally discovered T1b gallbladder cancer after routine cholecystectomy. Therapeutic strategies are shown after decision node (to right of □). Probabilistic outcome is shown after chance node (to the right of ○). Terminal nodes signify death (Δ) or that Markov model defines ensuing pathway (M). OR, operating room
For our cohort of patients, the base-case decision analysis favoured radical resection over simple cholecystectomy without additional surgery. Life-expectancy after simple cholecystectomy alone was 6.42 years after diagnosis. In contrast, radical resection improved life-expectancy to 9.85 years after diagnosis, providing an additional 3.43 years survival benefit over simple cholecystectomy alone.
Sensitivity analysis
One-way sensitivity analyses in which the age-at-diagnosis was varied is shown in Fig. 4. Varying the age from 20 to 100 years at the time of diagnosis demonstrated that the greatest benefit from radical resection in terms of gained life-years was achieved when the diagnosis was made at a young age.
Figure 4.
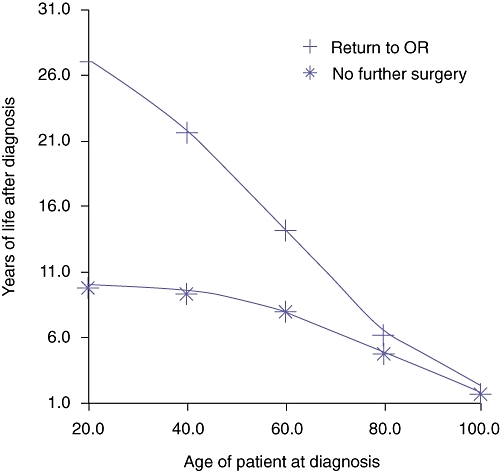
One-way sensitivity analysis varying the age at diagnosis from 20 to 100 years. The greatest benefit in terms of gained life-years was achieved for the youngest ages having radical resection, with this benefit gradually decreasing with increasing age of the patient subset. OR, operating room
For all ages, men had a slightly decreased survival benefit compared with females, likely secondary to their slightly shorter overall life expectancy (Table 5).
Table 5.
Age at diagnosis, gender and outcomes
| Age at diagnosis | Gender | Procedure | Life expectancy (years) |
|---|---|---|---|
| 35 | Male | Simple cholecystectomy | 9 |
| Radical cholecystectomy | 19 | ||
| 35 | Female | Simple cholecystectomy | 9 |
| Radical cholecystectomy | 20 | ||
| 65 | Male | Simple cholecystectomy | 7 |
| Radical cholecystectomy | 11 | ||
| 65 | Female | Simple cholecystectomy | 7 |
| Radical cholecystectomy | 12 |
The decision to perform a radical resection for T1b gallbladder cancer over a simple cholecystectomy is sensitive to the perioperative mortality rate. When the probability of peri-operative mortality is ≥36% (intersection of the lines in Fig. 5) the analysis favours treatment with simple cholecystectomy alone over radical resection.
Figure 5.
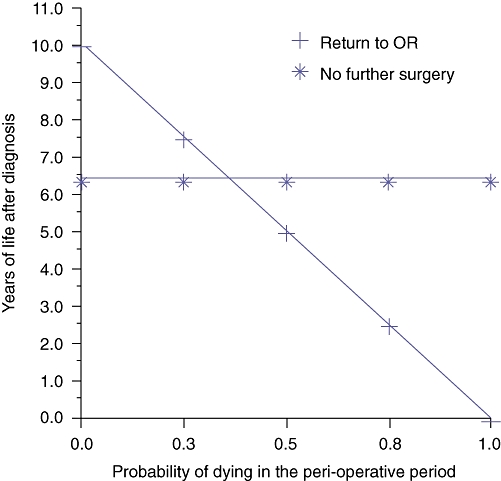
One-way sensitivity analysis varying probability of peri-operative mortality. The decision to treat with radical cholecystectomy vs. simple cholecystectomy is sensitive to varying the peri-operative mortality. Once peri-operative mortality reaches a threshold of ≥36% (intersection of the two lines in the graph) the analysis favours no further surgery over radical resection. OR, operating room
Discussion
Radical gallbladder resection in the management of T1b gallbladder cancers is controversial. Despite the fact that radical resection for these patients is recommended by many hepatobiliary surgeons, a recently published administrative database study suggests that less than 5% of patients with T1b gallbladder cancer in the United States currently undergo radical resection.18
In our analysis, we demonstrated increased long-term survival for patients with T1b gallbladder cancer who undergo radical resection vs. those treated with simple cholecystectomy alone. This finding is robust (note the high threshold value for peri-operative mortality rate on sensitivity analysis) and valid over a wide range of patient age at which gallbladder cancer is diagnosed.
Prior analysis of outcomes associated with T1b gallbladder cancer have been limited to small single institution series.9,23 Two analyses of the Surveillance, Epidemiology, and End Results (SEER) registry database for gallbladder cancer have been reported; however, in neither report were outcomes associated with simple cholecystectomy vs. radical resection compared specifically for patients with T1b lesions.18,24
A decision analysis study, such as ours, is not without potential limitations, which we enumerate here. In addition to the limited number of published studies that met inclusion criteria for our analysis (as noted above), we are using published data from multiple different authors and institutions which has lead to variability in the pooled data. For example, there were variations in the specific surgical procedures performed between (and even within) studies. In the simple cholecystectomy group, some patients had open cholecystecomy performed whereas others had laparoscopic procedures. However, we do not believe this variability adversely affects our results to a great extent as data from previously published studies indicates no survival difference between treatment with conventional open procedure vs. laparoscopic surgery for those patients with early gallbladder cancer.25–27 Ouchi et al., for example, found little difference upon comparing outcomes data from 498 patients with gallbladder cancer treated laparoscopically to their survival data from standard open procedures.27 They determined that laparoscopic cholecystectomy did not have any adverse effects on the long-term outcomes of these patients.27
Similarly, in the radical cholecystectomy group, some patients were treated with radical cholecystectomy during the initial operation whereas others were ‘re-resected’ at a later date after an initial simple cholecystectomy. Again, we do not believe this issue affects our findings. Shih et al. determined that there was no difference in survival between patients who were discovered to have gallbladder cancer incidentally on laparoscopic cholecystectomy and immediately converted to an open resection and those who had a completed laparoscopic cholecystectomy and were re-explored at a later point when found to have gallbladder cancer by subsequent pathology.28
Additional shortcoming of our analysis include an inability (because of a lack of published data) to stratify survival data based on resection margin status, lymph node involvement and adjuvant therapy. Furthermore, the findings from this study, while useful on a population basis, do not take into account individual patient characteristics (e.g. co-morbidities, medications, family history), nor individual patient wishes for treatment. It must be reiterated, as such, that decisions to treat with one modality vs. another need to be made on a case-by-case basis taking into account all relevant factors.
In conclusion, decision analysis based on data available for the subset of patients with T1b gallbladder cancer demonstrates that radical cholecystectomy is associated with improved survival for most patients with T1b gallbladder cancer.
Conflicts of interest
None declared.
References
- 1.Reid KM, Ramos-De la Medina A, Donohue JH. Diagnosis and surgical management of gallbladder cancer: a review. J Gastrointest Surg. 2007;11:671–681. doi: 10.1007/s11605-006-0075-x. [DOI] [PubMed] [Google Scholar]
- 2.Kwon AH, Imamura A, Kitade H, Kamiyama Y. Unsuspected gallbladder cancer diagnosed during or after laparoscopic cholecystectomy. J Surg Oncol. 2008;97:241–245. doi: 10.1002/jso.20944. [DOI] [PubMed] [Google Scholar]
- 3.Shukla PJ, Barreto G, Kakade A, Shrikhande SV. Revision surgery for incidental gallbladder cancer: factors influencing operability and further evidence for T1b tumours. HPB (Oxford) 2008;10:43–47. doi: 10.1080/13651820701867794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kinoshita H, Hashino K, Hashimoto M, Kodama T, Nishimura K, Kawabata M, et al. Clinicopathological evaluation of surgical treatment for early gallbladder cancer. Kurume Med J. 2001;48:267–271. doi: 10.2739/kurumemedj.48.267. [DOI] [PubMed] [Google Scholar]
- 5.Schauer RJ, Meyer G, Baretton G, Schildberg FW, Rau HG. Prognostic factors and long-term results after surgery for gallbladder carcinoma: a retrospective study of 127 patients. Langenbecks Arch Surg. 2001;386:110–117. doi: 10.1007/s004230000189. [DOI] [PubMed] [Google Scholar]
- 6.Darabos N, Stare R. Gallbladder cancer: laparoscopic and classic cholecystectomy. Surg Endosc. 2004;18:144–147. doi: 10.1007/s00464-002-9269-9. [DOI] [PubMed] [Google Scholar]
- 7.Toyonaga T, Chijiiwa K, Nakano K, Noshiro H, Yamaguchi K, Sada M, et al. Completion radical surgery after cholecystectomy for accidentally undiagnosed gallbladder carcinoma. World J Surg. 2003;27:266–271. doi: 10.1007/s00268-002-6609-9. [DOI] [PubMed] [Google Scholar]
- 8.Sun CD, Zhang BY, Wu LQ, Lee WJ. Laparoscopic cholecystectomy for treatment of unexpected early-stage gallbladder cancer. J Surg Oncol. 2005;91:253–257. doi: 10.1002/jso.20318. [DOI] [PubMed] [Google Scholar]
- 9.Wakai T, Shirai Y, Yokoyama N, Nagakura S, Watanabe H, Hatakeyama K. Early gallbladder carcinoma does not warrant radical resection. Br J Surg. 2001;88:675–678. doi: 10.1046/j.1365-2168.2001.01749.x. [DOI] [PubMed] [Google Scholar]
- 10.Muratore A, Polastri R, Capussotti L. Radical surgery for gallbladder cancer: current options. Eur J Surg Oncol. 2000;26:438–443. doi: 10.1053/ejso.1999.0918. [DOI] [PubMed] [Google Scholar]
- 11.You DD, Lee HG, Paik KY, Heo JS, Choi SH, Choi DW. What is an adequate extent of resection for T1 gallbladder cancers? Ann Surg. 2008;247:835–838. doi: 10.1097/SLA.0b013e3181675842. [DOI] [PubMed] [Google Scholar]
- 12.Cangemi V, Fiori E, Picchi C, De Cesare A, Cangemi R, Galati G, et al. Early gallbladder carcinoma: a single-center experience. Tumori. 2006;92:487–490. doi: 10.1177/030089160609200604. [DOI] [PubMed] [Google Scholar]
- 13.Wagholikar GD, Behari A, Krishnani N, Kumar A, Sikora SS, Saxena R, et al. Early gallbladder cancer. J Am Coll Surg. 2002;194:137–141. doi: 10.1016/s1072-7515(01)01136-x. [DOI] [PubMed] [Google Scholar]
- 14.Cucinotta E, Lorenzini C, Melita G, Iapichino G, Curro G. Incidental gall bladder carcinoma: does the surgical approach influence the outcome? ANZ J Surg. 2005;75:795–798. doi: 10.1111/j.1445-2197.2005.03528.x. [DOI] [PubMed] [Google Scholar]
- 15.Principe A, Del Gaudio M, Ercolani G, Golfieri R, Cucchetti A, Pinna AD. Radical surgery for gallbladder carcinoma: possibilities of survival. Hepatogastroenterology. 2006;53:660–664. [PubMed] [Google Scholar]
- 16.Miller G, Jarnagin WR. Gallbladder carcinoma. Eur J Surg Oncol. 2008;34:306–312. doi: 10.1016/j.ejso.2007.07.206. [DOI] [PubMed] [Google Scholar]
- 17.Mekeel KL, Hemming AW. Surgical management of gallbladder carcinoma: a review. J Gastrointest Surg. 2007;11:1188–1193. doi: 10.1007/s11605-007-0115-1. [DOI] [PubMed] [Google Scholar]
- 18.Jensen EH, Abraham A, Habermann EB, Al-Refaie WB, Vickers SM, Virnig BA, et al. Analysis of the surgical management of early-stage gallbladder cancer in the United States. J Gastrointest Surg. 2008;13:722–727. doi: 10.1007/s11605-008-0772-8. [DOI] [PubMed] [Google Scholar]
- 19.Beck JR, Pauker SG. The Markov process in medical prognosis. Med Decis Making. 1983;3:419–458. doi: 10.1177/0272989X8300300403. [DOI] [PubMed] [Google Scholar]
- 20.Arias E. United States life tables, 2000. Natl Vital Stat Rep. 2002;51:1–38. [PubMed] [Google Scholar]
- 21.Beck JR, Pauker SG, Gottlieb JE, Klein K, Kassirer JP. A convenient approximation of life expectancy (the ‘DEALE’). II. Use in medical decision-making. Am J Med. 1982;73:889–897. doi: 10.1016/0002-9343(82)90787-2. [DOI] [PubMed] [Google Scholar]
- 22.Beck JR, Kassirer JP, Pauker SG. A convenient approximation of life expectancy (the ‘DEALE’). I. Validation of the method. Am J Med. 1982;73:883–888. doi: 10.1016/0002-9343(82)90786-0. [DOI] [PubMed] [Google Scholar]
- 23.Goetze TO, Paolucci V. Immediate re-resection of T1 incidental gallbladder carcinomas: a survival analysis of the German Registry. Surg Endosc. 2008;22:2462–2465. doi: 10.1007/s00464-008-9747-9. [DOI] [PubMed] [Google Scholar]
- 24.Coburn NG, Cleary SP, Tan JC, Law CH. Surgery for gallbladder cancer: a population-based analysis. J Am Coll Surg. 2008;207:371–382. doi: 10.1016/j.jamcollsurg.2008.02.031. [DOI] [PubMed] [Google Scholar]
- 25.Chan KM, Yeh TS, Jan YY, Chen MF. Laparoscopic cholecystectomy for early gallbladder carcinoma: long-term outcome in comparison with conventional open cholecystectomy. Surg Endosc. 2006;20:1867–1871. doi: 10.1007/s00464-005-0195-5. [DOI] [PubMed] [Google Scholar]
- 26.Goetze T, Paolucci V. Does laparoscopy worsen the prognosis for incidental gallbladder cancer? Surg Endosc. 2006;20:286–293. doi: 10.1007/s00464-005-0121-x. [DOI] [PubMed] [Google Scholar]
- 27.Ouchi K, Mikuni J, Kakugawa Y. Laparoscopic cholecystectomy for gallbladder carcinoma: results of a Japanese survey of 498 patients. J Hepatobiliary Pancreat Surg. 2002;9:256–260. doi: 10.1007/s005340200028. [DOI] [PubMed] [Google Scholar]
- 28.Shih SP, Schulick RD, Cameron JL, Lillemoe KD, Pitt HA, Choti MA, et al. Gallbladder cancer: the role of laparoscopy and radical resection. Ann Surg. 2007;245:893–901. doi: 10.1097/SLA.0b013e31806beec2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mizumoto R, Ogura Y, Kusuda T. Definition and diagnosis of early cancer of the biliary tract. Hepatogastroenterology. 1993;40:69–77. [PubMed] [Google Scholar]
- 30.Kim EK, Lee SK, Kim WW. Does laparoscopic surgery have a role in the treatment of gallbladder cancer? J Hepatobiliary Pancreat Surg. 2002;9:559–563. doi: 10.1007/s005340200074. [DOI] [PubMed] [Google Scholar]
- 31.Ouchi K, Sugawara T, Ono H, Fujiya T, Kamiyama Y, Kakugawa Y, et al. Diagnostic capability and rational resectional surgery for early gallbladder cancer. Hepatogastroenterology. 1999;46:1557–1560. [PubMed] [Google Scholar]
- 32.Yagi H, Shimazu M, Kawachi S, Tanabe M, Aiura K, Wakabayashi G, et al. Retrospective analysis of outcome in 63 gallbladder carcinoma patients after radical resection. J Hepatobiliary Pancreat Surg. 2006;13:530–536. doi: 10.1007/s00534-006-1104-6. [DOI] [PubMed] [Google Scholar]
- 33.Foster JM, Hoshi H, Gibbs JF, Iyer R, Javle M, Chu Q, et al. Gallbladder cancer: defining the indications for primary radical resection and radical re-resection. Ann Surg Oncol. 2007;14:833–840. doi: 10.1245/s10434-006-9097-6. [DOI] [PubMed] [Google Scholar]
- 34.Nevin JE, Moran TJ, Kay S, King R. Carcinoma of the gallbladder: staging, treatment, and prognosis. Cancer. 1976;37:141–148. doi: 10.1002/1097-0142(197601)37:1<141::aid-cncr2820370121>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 35.Benoist S, Panis Y, Fagniez PL. Long-term results after curative resection for carcinoma of the gallbladder. French University Association for Surgical Research. Am J Surg. 1998;175:118–122. doi: 10.1016/s0002-9610(97)00269-9. [DOI] [PubMed] [Google Scholar]
- 36.Shibata K, Uchida H, Iwaki K, Kai S, Ohta M, Kitano S. Lymphatic invasion: an important prognostic factor for stages T1b-T3 gallbladder cancer and an indication for additional radical resection of incidental gallbladder cancer. World J Surg. 2009;33:1035–1041. doi: 10.1007/s00268-009-9950-4. [DOI] [PubMed] [Google Scholar]
- 37.Yamamoto M, Onoyama H, Ajiki T, Yamada I, Fujita T, Saitoh Y. Surgical results of operations for carcinoma of the gallbladder. Hepatogastroenterology. 1999;46:1552–1556. [PubMed] [Google Scholar]
- 38.Puhalla H, Wild T, Bareck E, Pokorny H, Ploner M, Soliman T, et al. Long-term follow-up of surgically treated gallbladder cancer patients. Eur J Surg Oncol. 2002;28:857–863. doi: 10.1053/ejso.2002.1301. [DOI] [PubMed] [Google Scholar]
- 39.Cubertafond P, Mathonnet M, Gainant A, Launois B. Radical surgery for gallbladder cancer. Results of the French Surgical Association Survey. Hepatogastroenterology. 1999;46:1567–1571. [PubMed] [Google Scholar]
- 40.Tsukada K, Hatakeyama K, Kurosaki I, Uchida K, Shirai Y, Muto T, et al. Outcome of radical surgery for carcinoma of the gallbladder according to the TNM stage. Surgery. 1996;120:816–821. doi: 10.1016/s0039-6060(96)80089-4. [DOI] [PubMed] [Google Scholar]
- 41.Todoroki T, Kawamoto T, Takahashi H, Takada Y, Koike N, Otsuka M, et al. Treatment of gallbladder cancer by radical resection. Br J Surg. 1999;86:622–627. doi: 10.1046/j.1365-2168.1999.01085.x. [DOI] [PubMed] [Google Scholar]
- 42.Bartlett DL, Fong Y, Fortner JG, Brennan MF, Blumgart LH. Long-term results after resection for gallbladder cancer. Implications for staging and management. Ann Surg. 1996;224:639–646. doi: 10.1097/00000658-199611000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shirai Y, Yoshida K, Tsukada K, Muto T. Inapparent carcinoma of the gallbladder. An appraisal of a radical second operation after simple cholecystectomy. Ann Surg. 1992;215:326–331. doi: 10.1097/00000658-199204000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fong Y, Heffernan N, Blumgart LH. Gallbladder carcinoma discovered during laparoscopic cholecystectomy: aggressive reresection is beneficial. Cancer. 1998;83:423–427. doi: 10.1002/(sici)1097-0142(19980801)83:3<423::aid-cncr9>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 45.Yoshida T, Matsumoto T, Sasaki A, Morii Y, Ishio T, Bandoh T, et al. Laparoscopic cholecystectomy in the treatment of patients with gall bladder cancer. J Am Coll Surg. 2000;191:158–163. doi: 10.1016/s1072-7515(00)00285-4. [DOI] [PubMed] [Google Scholar]
- 46.Suzuki K, Kimura T, Ogawa H. Long-term prognosis of gallbladder cancer diagnosed after laparoscopic cholecystectomy. Surg Endosc. 2000;14:712–716. doi: 10.1007/s004640000145. [DOI] [PubMed] [Google Scholar]
- 47.Mondragon-Sanchez R, Gonzalez-Geroniz M, Onate-Ocana LF, Garduno-Lopez AL, Mondragon-Sanchez A, Bernal-Maldonado R, et al. A retrospective analysis of patients with gallbladder cancer treated with radical resection versus cholecystectomy plus external radiotherapy. Hepatogastroenterology. 2003;50:1806–1810. [PubMed] [Google Scholar]
- 48.Frena A, La Guardia G, Martin F. Outcome of radical surgery for carcinoma of the gallbladder according to the tumor node metastasis and Japanese Society of Biliary Surgery stages. J Gastrointest Surg. 2004;8:580–590. doi: 10.1016/j.gassur.2003.11.011. [DOI] [PubMed] [Google Scholar]
- 49.Onoyama H, Ajiki T, Takada M, Urakawa T, Saitoh Y. Does radical resection improve the survival in patients with carcinoma of the gallbladder who are 75 years old and older? World J Surg. 2002;26:1315–1318. doi: 10.1007/s00268-002-6163-5. [DOI] [PubMed] [Google Scholar]
- 50.Behari A, Sikora SS, Wagholikar GD, Kumar A, Saxena R, Kapoor VK. Longterm survival after extended resections in patients with gallbladder cancer. J Am Coll Surg. 2003;196:82–88. doi: 10.1016/s1072-7515(02)01611-3. [DOI] [PubMed] [Google Scholar]
- 51.Taner CB, Nagorney DM, Donohue JH. Surgical treatment of gallbladder cancer. J Gastrointest Surg. 2004;8:83–89. doi: 10.1016/j.gassur.2003.09.022. discussion 89. [DOI] [PubMed] [Google Scholar]
- 52.Yildirim E, Celen O, Gulben K, Berberoglu U. The surgical management of incidental gallbladder carcinoma. Eur J Surg Oncol. 2005;31:45–52. doi: 10.1016/j.ejso.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 53.Chan SY, Poon RT, Lo CM, Ng KK, Fan ST. Management of carcinoma of the gallbladder: a single-institution experience in 16 years. J Surg Oncol. 2008;97:156–164. doi: 10.1002/jso.20885. [DOI] [PubMed] [Google Scholar]
- 54.Reddy SK, Marroquin CE, Kuo PC, Pappas TN, Clary BM. Extended hepatic resection for gallbladder cancer. Am J Surg. 2007;194:355–361. doi: 10.1016/j.amjsurg.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 55.Ito H, Matros E, Brooks DC, Osteen RT, Zinner MJ, Swanson RS, et al. Treatment outcomes associated with surgery for gallbladder cancer: a 20-year experience. J Gastrointest Surg. 2004;8:183–190. doi: 10.1016/j.gassur.2003.10.006. [DOI] [PubMed] [Google Scholar]


