Abstract
AIM: To examine whether acupuncture can prevent prolonged postoperative ileus (PPOI) after intraperitoneal surgery for colon cancer.
METHODS: Ninety patients were recruited from the Fudan University Cancer Hospital, Shanghai, China. After surgery, patients were randomized to receive acupuncture (once daily, starting on postoperative day 1, for up to six consecutive days) or usual care. PPOI was defined as an inability to pass flatus or have a bowel movement by 96 h after surgery. The main outcomes were time to first flatus, time to first bowel movement, and electrogastroenterography. Secondary outcomes were quality of life (QOL) measures, including pain, nausea, insomnia, abdominal distension/fullness, and sense of well-being.
RESULTS: No significant differences in PPOI on day 4 (P = 0.71) or QOL measures were found between the groups. There were also no group differences when the data were analyzed by examining those whose PPOI had resolved by day 5 (P = 0.69) or day 6 (P = 0.88). No adverse events related to acupuncture were reported.
CONCLUSION: Acupuncture did not prevent PPOI and was not useful for treating PPOI once it had developed in this population.
Keywords: Acupuncture, Gastrointestinal motility, Gastrointestinal disorders, Gastrointestinal neoplasms
INTRODUCTION
Bowel dysfunction following abdominal surgery is common and usually temporary, lasting no more than 3 d; however, if patients are unable to tolerate an oral diet, pass flatus, or have a bowel movement by postoperative day 4, they are considered to have prolonged postoperative ileus (PPOI). PPOI is uncomfortable for patients and potentially dangerous. The collection of gas and secretions related to PPOI causes pain and discomfort with bloating, distention, and often emesis[1]. Delayed gastric emptying also increases the risk of aspiration in patients during the early postoperative period. Patients with PPOI cannot be discharged from the hospital until the ileus has resolved. Few published studies have estimated the cost of PPOI, but expenses related to longer hospital stays, nursing care, laboratory/diagnostic testing, and interventional treatments are likely to be considerable.
Current treatment for postoperative ileus in China is primarily supportive and includes nasogastric suction, intravenous fluids, parenteral nutrition, and gradual ambulation with simple exercises. However, a variety of preventive interventions[2-6] for PPOI, such as preoperative carbohydrate loading, wrapping patients in warm blankets in the operating room, chewing gum, and rocking in a rocking chair postoperatively to stimulate gastrointestinal function, have been mentioned in the literature. Further research is needed, however, to evaluate the efficacy of these approaches. Two studies published by Sculati and colleagues have concluded that a preoperative bran-enriched diet (lasting 8-10 d) may help prevent PPOI[7,8], but this is often not practical for patients undergoing gastrointestinal surgery.
Although prevention and treatment of PPOI with various pharmacologic agents has been explored for several years, success has been limited[9-17]. Alternatives to systemic opioid analgesia, such as thoracic epidural analgesia[18] and non-opioid analgesics such as ketorolac tromethamine[10,11], have been shown to shorten the duration of PPOI when compared with opioids, but non-opioid analgesia does not adequately control pain in all patients[10,11]. The combined use of a local anesthetic for chemical sympathectomy and sparing amounts of narcotic for improved pain control has been proposed, but there is no clear guidance as to which combination best promotes bowel motility while maintaining adequate pain control[17].
A 2008 Cochrane review of the use of prokinetic agents in PPOI has concluded that there was no evidence to support the use of erythromycin, and insufficient evidence for cisapride, cholecystokinin-like drugs such as cerulein, and dopamine antagonists such as metoclopramide, propranolol and vasopressin[19]. Neostigmine rapidly decompresses the colon and has shown some potential in PPOI; however, side effects such as bradycardia, bronchospasm, and increased risk of anastomotic dehiscence are of major concern[17,20]. Lubiprostone, a bicyclic fatty acid that acts as a chloride channel opener and thereby increases intestinal water secretion, has been shown to be effective in constipation[21] and is currently being investigated in PPOI[16].
Narcotic receptor antagonists represent another major class of drugs studied in the treatment of PPOI. Naloxone, for example, is limited by its central nervous system effects and potential to reverse analgesia[17]. Methylnaltrexone, a quaternary derivative of naltrexone that does not cross the blood-brain barrier, has shown some efficacy in opioid-induced constipation[22,23], but preliminary results from two trials in PPOI showed no benefit over placebo[24]. In May 2008, alvimopan, a selective mu-receptor antagonist, was the first drug to receive United States Food and Drug Administration (FDA) approval specifically for the treatment of PPOI after showing benefit in several phase III trials[25,26]. However, there are concerns about the cost-benefit ratio of this drug, given that it shows only a modest reduction in hospital stay (7-15 h) and costs nearly $1000/treatment cycle[27,28].
Some research has suggested that traditional Chinese herbal medicines can also help bowel motility[29,30]. For example, saussura cappa and the formula Liu Jun Zi Tang have been associated with improved stomach and intestinal emptying time and increased plasma motilin levels[29,31]. Although herbal medicine shows some benefit for gastrointestinal motility, abdominal surgery patients generally cannot have anything by mouth during the perioperative period.
Acupuncture has been used in China for thousands of years to treat a variety of gastrointestinal problems[32]. The advantages of acupuncture are that it is a cost-effective, minimally invasive procedure with a very low incidence of side effects. Although prior studies have investigated the effects of acupuncture on gastrointestinal motility in humans[33], few randomized clinical trials have been published. Controlled animal studies supported by plausible physiological and laboratory evidence have, however, shown that acupuncture has positive effects on gastric and intestinal motility[34-38]. Although the exact mechanisms are not fully understood, one hypothesis is that acupuncture may help regulate the gastrointestinal tract via the autonomic nervous system. Several animal studies have revealed that the effect of acupuncture on gastrointestinal function is mediated through sympathetic and parasympathetic efferent pathways[39,40].
To the best of our knowledge, only one study[41] has evaluated the efficacy of acupuncture in preventing PPOI after abdominal surgery. However, in that trial, the incidence of PPOI assessed at postoperative day 4 after ileostomy/colostomy closure was too small to show significance between the treatment and control groups. Therefore, in the current prospective, randomized study, we investigated whether acupuncture could prevent PPOI after invasive colon cancer surgery. Bowel motility was determined by time to first flatus, time to first bowel movement, and by electrogastroenterography (EGEG), a device that detects electrical signals from the abdomen. Secondary objectives were to compare postsurgical quality of life (QOL) between the treatment and control groups in terms of pain, nausea, insomnia, abdominal distension/fullness, and sense of well-being.
MATERIALS AND METHODS
Patient eligibility
Patients were recruited from the Fudan University Cancer Hospital between July 2004 and October 2006 and were enrolled in the trial after providing written informed consent. Regardless of sex or ethnicity, all patients 18-75 years old, who had colon cancer with a Duke A to D stage diagnosis (as long as metastatic disease did not affect bowel function) and were scheduled to undergo intraperitoneal surgery, were identified at the time of preoperative evaluation and screened for eligibility. Eligible patients had to meet the following criteria: physical status classification of category III or better according to criteria established by the American Society of Anesthesiologists[42]; planned use of epidural infusion for post-surgical pain management; no upper or lower extremity deformity or local skin infections that could interfere with accurate acupuncture point location; no active systemic infection; no chronic functional constipation as defined by Rome I criteria prior to the cancer diagnosis[43]; and no history of cerebrovascular accident or spinal cord injury. Patients were also excluded if they had chronic pain currently treated with any form of major opioid or with weak opioids at morphine equivalent doses > 30 mg/24 h; had a cardiac pacemaker; were mentally incapacitated or had a significant emotional or psychiatric disorder that precluded study participation; were pregnant; were using laxatives or other medicines known to affect bowel function, such as herbal preparations, high-dose vitamins, or iron sulfates; had known bleeding abnormalities or were on heparin or warfarin; had any parasurgical complications needing intensive care; or were currently using acupuncture.
Procedures
The study was designed collaboratively and conceived by faculty from Fudan University Cancer Hospital and M.D. Anderson Cancer Center, The University of Texas. An experienced statistician was involved in all stages of study development and analysis. The protocol was approved by both Institutional Review Boards. Two nurses from Fudan Cancer Hospital spent 3 mo at M.D. Anderson Cancer Center undergoing research nurse training, two physicians underwent 2 mo of faculty research training, and the acupuncturist from Fudan University Cancer Hospital spent 1 mo at M.D. Anderson Cancer Center. The acupuncturist was trained specifically in aspects of quality control and fidelity to study-related acupuncture procedures. During the course of the trial, faculty and staff from M.D. Anderson Cancer Center also visited Fudan Cancer Hospital four times to review the trial. Video conferences were conducted twice each month.
At the Fudan University Cancer Hospital, patients are generally admitted for preoperative evaluation 3-5 d prior to surgery. All patients were recruited during this time. The first 30 patients were randomized using simple randomization; however, group differences were noted for route of anesthesia administration. Therefore, from the 31st patient forward, in order to ensure group balance for anesthesia administration, patients were randomized into either treatment or control groups by a form of adaptive randomization, minimization[44]. Before a participant was assigned to a treatment group, the number of already randomized participants with similar covariate characteristics was totaled. The totals were computed based on marginal sums so that each covariate was considered separately. The treatment assignment for a participant was then based on which treatment group assignment would produce the best overall balance with respect to the covariate characteristics. The patient characteristic used for group assignment was the mode of anesthesia (iv, epidural, or iv plus epidural).
After surgery, if the patient continued to meet all eligibility criteria, she/he was randomized with equal probability into either the treatment or control group. Data were collected and recorded twice a day for 6 d or until the first bowel movement. Patients had to have a bowel movement prior to discharge; therefore, participation ended at the time of discharge for anyone leaving prior to the sixth postoperative day, regardless of whether they had received acupuncture treatment.
Acupuncture treatment
The acupuncture treatments were performed in the patient’s room by a hospital accredited physician who has over 30 years of acupuncture experience and is routinely involved in postoperative care to patients. Patients in the treatment group received acupuncture once a day, starting on postoperative day 1, for six consecutive days or until the first bowel movement, whichever came first. After the skin was prepped with 70% alcohol, the needles were inserted and remained in place for approximately 20 min with each treatment. The treatment frequency was agreed upon by a small panel of experienced acupuncturists. Patients in the control group received standard postoperative care with no acupuncture.
During the acupuncture treatment, each patient lay in a supine position in his or her hospital bed. A tight abdominal dressing and binder was placed after surgery and not removed for 2-3 d, therefore, only points located on the extremities were selected. Electrical stimulation was applied concomitantly and continuously to two pairs of points [SJ-6 (positive) and GB-34 (negative)] bilaterally by placing lead wires on the needles connected to an electro-acupuncture stimulator (Model 980; Shanghai Medical Equipment Co. Ltd., Shanghai, China). This unit applied consistent stimulation throughout the treatment at a frequency of 2 Hz.
The acupuncture needles used (Huatuo, Suzhou, China) conformed to the requirements of the ISO 9002, EN46002 and CE certification, United States FDA International Good Manufacturing Practices, and the World Health Organization’s standards for quality and safety. These stainless steel needles are 1.5 cun in length by 32-gauge diameter and are provided in individual sterile packages.
Standardized techniques for point location were used and were based on anatomical landmarks as well as proportional measurements of the patient’s body. For example, finger breadth refers to the patient’s middle finger, and the proportional unit of measure was the “cun”, defined as the distance between the two medial ends of the creases of the interphalangeal joints when the patient’s middle finger is flexed[32]. The following bilateral acupuncture points were selected specifically for the purpose of improving bowel motility. (1) SJ-6: located 3 cun proximal to the dorsal crease of the wrist, on the line connecting Yangchi (SJ-4) and the tip of olecranon, between the radius and ulna, on the radial side of the extensor digitorum communis muscle. The Chinese name for this point is Zhigou. According to the underlying theory of Traditional Chinese Medicine (TCM), this is a major point for stimulating the intestines[45] and is often paired with GB-34 to treat constipation. (2) GB-34: located in the depression anterior and inferior to the head of the fibula. The Chinese name for this point is Yanglingquan. This point is often paired with SJ-6 to treat constipation due to qi stagnation or heat[45]. (3) ST-36: on the lateral surface of the leg, 3 cun distal to the lower border of the patella, one finger’s breadth from the tibia tuberosity between the tibia digitorum tibialis anterior muscle and the tendon of longus pedis. The Chinese name for this point is Zusanli. It lies just over the deep peroneal nerve and is commonly used by acupuncturists to harmonize (i.e. regulate) the gastrointestinal tract[45]. (4) ST-37: located 3 cun below Zusanli (St-36) and one finger’s breadth (middle finger) from the anterior border of the tibia. The Chinese name for this point is Shangjuxu. Based on TCM theory, this point also regulates the intestines[45].
Outcome measures
The main outcome measure of bowel motility was assessed by asking patients to record the exact date and time that they first passed flatus and the exact date and time of their first bowel movement after surgery. Time 0 was the time anesthesia ended according to the anesthetic record. The total numbers of hours between time 0 and the passage of flatus and between time 0 and the first bowel movement were then calculated. PPOI was defined as having no bowel movement for more than 96 h (4 d) after surgery.
Secondary measures included EGEG and QOL assessments. Electrical signals from the stomach and intestines associated with gastrointestinal motility were monitored via EGEG (Huake Electronic Technical Research Institute, Beijing, China). The surgeon placed the leads for EGEG monitoring at the time of wound closure and prior to placement of the abdominal dressing and binder. According to standard postoperative care at this hospital, the abdominal dressing and binder were not removed until postoperative day 2 or 3; therefore, assessment of bowel sounds was not performed. EGEG monitoring occurred twice per day. After attachment of the electrodes to the leads, the patient rested for 1 min, and then two consecutive 3-min recordings were obtained. Both frequency (per minute) and amplitude were measured using two channels.
Data related to postoperative QOL were obtained from the nursing and physician progress notes and the patient’s self-evaluation using the Quality of Life Status (QOLS) assessment tool, which is based on the Edmonton Symptom Assessment System (ESAS)[46-48]. The QOLS used in this study was a slightly modified version of the ESAS and consisted of five items (pain, nausea, insomnia, abdominal distention, and general sense of well-being), which were rated using a 0-10 numeric rating scale.
Statistical analysis
Our primary analysis was to determine the proportion of patients with ileus in each group at day 4 and to determine if the two groups differed in the proportions of ileus observed, using a binomial test. We powered our study to be able to estimate each proportion to within at most 16% by including 40 patients in each group. For example, if 50% of patients in one group (20 out of 40) developed ileus, the 95% confidence interval of this estimate would be 34%-66%. In addition, if we found that 40% of patients (16 out of 40) in one group developed ileus and 11% or fewer (≤ 4) in the second group developed ileus, this difference would be considered statistically significant with 80% power and a two-sided significance level of 5%.
The time of occurrence of bowel motility indicators (i.e. first passage of flatus and first bowel movement) was subtracted from the time anesthesia ended, and compared between groups using the Wilcoxon two-samples test. Unpaired t tests were used to compare EGEG indicators and QOL outcomes between groups.
RESULTS
Of the 154 subjects screened, 137 met all the initial eligibility criteria. Forty-seven patients who were eligible declined to participate. Therefore, 65.7% of eligible patients (90 patients) agreed to participate. The overall mean age of the participants was 53.7 years (range, 29-73 years), and there were no group differences in mean age (acupuncture, 54.3 years; control, 53.1 years). There were 38 (45%) women and 47 (55%) men, with an even balance between groups (43% and 46% women in the acupuncture and control groups, respectively). All patients received intraperitoneal surgery, and a representative sample of the population that we wanted to assess was obtained as follows: 47 (52.2%) proctectomy, 21 (23.3%) right hemicolectomy, 11 (12.2%) sigmoidectomy, eight (8.9%) left hemicolectomy and three (3.3%) transverse colectomy. Of 90 patients, 70 (77.78%) received epidural anesthesia (37 acupuncture; 33 controls), 18 (20%) received both epidural and general anesthesia (7 acupuncture, 11 in controls), and two (2.2%) patients in the acupuncture treatment group received general anesthesia only. There were no differences between groups with regard to diagnosis, operation methods, operation time, blood loss, and postoperative complications.
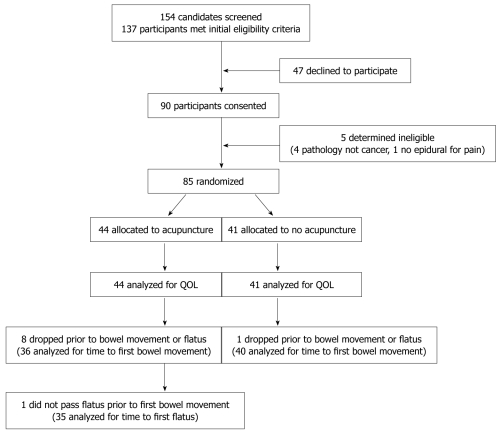
No participants were lost to follow-up. Five participants were dropped from the study after consent but prior to randomization either because a subsequent pathology report indicated that they did not have a cancer diagnosis, or because they did not receive epidural infusion for post-surgical pain management. Eighty-five patients were randomized (acupuncture = 44; no acupuncture = 41). Although some postoperative QOL data were obtained on all patients, eight in the acupuncture group and one in the no acupuncture group were dropped prior to first bowel movement or first passage of flatus, and before PPOI could be assessed on postoperative day 4, because the inconvenience of study participation (acupuncture-4 dropped on postoperative day 1, 2 on day 2, 1 on day 3, and 1 on day 4; no acupuncture-1 dropped on postoperative day 2). Figure 1 shows the flow of participants through enrollment, randomization, follow-up, and analysis.
Figure 1.
Flow of participants through the study.
Table 1 provides a summary of the study results. There were no significant differences between the groups in terms of bowel motility indicators, EGEG, or post-surgical QOL, thus, the null hypothesis was not rejected.
Table 1.
Summary of study results
| Outcome |
Acupuncture |
Control |
P value | ||||
| n | mean ± SD | Median (range) | n | mean ± SD | Median (range) | ||
| Hours to first flatus | 35 | 68.26 ± 23.38 | 72.25 (26.75-124.63) | 40 | 65.24 ± 17.5 | 64.88 (30.25-105.17) | 0.36 |
| Hours to first bowel movement | 36 | 119.04 ± 47.97 | 108.67 (34.00-241.17) | 40 | 119.38 ± 60.21 | 104.25 (37.00-359.00) | 0.77 |
| EGEG at morning (Freq/min) | 44 | 9.66 ± 1.34 | 9.32 (7.34-12.87) | 41 | 9.59 ± 1.63 | 9.65 (6.80-14.98) | 0.83 |
| EGEG at afternoon (Freq/min) | 44 | 9.76 ± 1.51 | 9.6 (6.11-15.93) | 41 | 9.81 ± 1.46 | 9.94 (6.74-14.31) | 0.65 |
| EGEG at morning Amplitude (uv) | 44 | 245 ± 61.1 | 243 (119-391) | 41 | 239 ± 48.3 | 237 (131-343) | 0.75 |
| EGEG at afternoon Amplitude (uv) | 44 | 250 ± 59.8 | 250 (131-380) | 41 | 239 ± 51.7 | 222 (144-345) | 0.39 |
| Pain1 | 44 | 2.51 ± 1.74 | 2.22 (0-6) | 41 | 2.37 ± 1.52 | 2.09 (0-5.73) | 0.82 |
| Nausea1 | 44 | 0.91 ± 1.67 | 0 (0-8) | 41 | 0.45 ± 0.99 | 0 (0-5.25) | 0.35 |
| Insomnia1 | 44 | 5.11 ± 1.9 | 5 (1.83-9.00) | 41 | 5.18 ± 2.06 | 5.17 (0.67-9.33) | 0.76 |
| Abdominal distention1 | 44 | 0.98 ± 1.35 | 0.21 (0-4.75) | 41 | 0.76 ± 1.3 | 0.13 (0-6.50) | 0.46 |
| General well-being1 | 44 | 4.11 ± 1.57 | 4 (1.67-8.00) | 41 | 3.73 ± 1.3 | 3.67 (1.17-6.29) | 0.34 |
Based on a 0-10 numeric rating scale.
There were also no group differences when the data were analyzed on the basis of the subset of 46 patients who developed PPOI by day 4 (21 of 36 acupuncture patients vs 25 of 40 control patients, P = 0.71), and whether their PPOI had resolved by day 5 (8 of 21 acupuncture patients and 11 of 25 controls, P = 0.69) or day 6 (13 of 21 acupuncture vs 16 of 25 controls, P = 0.88). The remaining 17 patients experienced a bowel movement by day 7. There were no adverse events greater than grade I (according to the Common Terminology Criteria for Adverse Events v3.0 (CTCAE)[49] related to the acupuncture treatment reported during the study.
DISCUSSION
PPOI developed in 46 patients, and there was no significant difference in the number of patients with PPOI in the acupuncture group (n = 21) vs the control group (n = 25). Similarly, there were no group differences in bowel activity as assessed by EGEG or in self-reported pain, nausea, insomnia, abdominal distention, or general well-being. In this patient population, PPOI occurred in up to 50% of participants in both groups, which suggested a lack of efficacy of acupuncture to prevent PPOI. Furthermore, analyses of the subset of patients who developed PPOI on day 4 and the resolution of PPOI on days 5 or 6 also revealed no group differences. Although this was a secondary analysis based on a small number of patients, it suggested that acupuncture was not effective in treating PPOI once it developed in this population.
Several important facts, however, were learned that will help with the development of future trials. First, standard postoperative care is different in China than in the United States. At Fudan University Cancer Hospital, patients undergoing this type of surgery often do not ambulate until after postoperative day 3, and in many cases, patients may not ambulate until postoperative day 5 or 6. In addition, patients have a nasogastric tube in place for several days and, thus, progression in diet is much slower than in the United States. Finally, a tight abdominal dressing and binder is placed after surgery and not removed for 2-3 d. Each of these factors could play an important role in gastrointestinal motility postoperatively and were not analyzed separately in the current study. As this was a randomized clinical trial, however, these factors were likely balanced between both groups. No patients in either group were given enteral or nasogastric feeding before passage of first flatus, and all patients in both groups were given similar iv fluids that included fat emulsion, amino acids, glucose and equilibrium liquids.
One limitation of the current study is that the use of epidural anesthesia in the majority of patients may have diminished the possible effects of acupuncture because of the blockade of afferent and efferent pathways, as acupuncture may act on gastrointestinal motility through neural mechanisms. Moreover, opioid use was not tracked and analyzed formally; however, through the process of randomization and based on a brief review of patient records showing consistency in pre- and postoperative medication, the authors believe this was likely to have been similar in both groups. Nevertheless, it is important to note that the acupuncture treatment in this study was designed to stimulate gastrointestinal motility. The efficacy of acupuncture for pain control is well established[50], and future trials should explore whether or not acupuncture designed to reduce pain can also reduce the amount of opioids used, and thus lessen the occurrence of PPOI. Although acupuncture alone may not be sufficient to reduce the risk of developing postoperative ileus, adding acupuncture to a regimen that includes other preventive measures such as less opioid use, increased ambulation, and progressive diet could have a synergistic effect and help prevent this debilitating complication following abdominal surgery. Future acupuncture trials should, therefore, be designed to include evaluation of these factors, as well as different point combinations, treatment schedules, and type of needle stimulation (i.e. manual vs electrical).
To the best of our knowledge, only one previous randomized trial has examined the use of acupuncture to prevent PPOI[41]. That study was conducted in the United States among a population of cancer patients who underwent ileostomy/colostomy reversal, a procedure which is not commonly performed in China. Unfortunately, the incidence of PPOI in that study was too small to determine any statistically significant differences between the groups. It is important to note that no adverse events related to acupuncture were reported during either the previous or current trial.
Providing acupuncture treatment to post-surgical patients at the bedside was found to be feasible, and the logistics of so doing were determined in the current study. Future research should evaluate the efficacy of acupuncture in a different population and for other postoperative conditions, such as anxiety, pain, nausea, vomiting, and wound healing.
In conclusion, this study confirmed findings from previous research[42] that acupuncture can be safely administered in a postoperative setting; however, it was not found to be effective in preventing PPOI in this population. Future studies examining the use of acupuncture for PPOI should include assessment of activity, diet, and postoperative pain control, as well as different point combinations, treatment schedules, and type of needle stimulation. Finally, this was a prevention study, and the efficacy of acupuncture in treating PPOI once it has developed has not been evaluated in a prospective randomized trial. Since prior animal and human data[34-38] have shown that acupuncture can regulate gastrointestinal function, further investigation is warranted.
COMMENTS
Background
Postoperative ileus is a common problem in patients who have major abdominal surgery. The duration is usually short, but prolonged postoperative ileus (PPOI) may lead to increased hospital stay and costs. Acupuncture is often used to treat gastrointestinal disorders in China, but it is still not known whether it is effective for preventing or treating PPOI.
Research frontiers
Information from this study may help surgeons choose appropriate therapy for PPOI after abdominal surgery.
Innovations and breakthroughs
This study was conducted as part of a unique collaboration between researchers in the United States and China. Only one previous randomized trial, conducted in the United States, has examined the use of acupuncture to prevent PPOI in cancer patients. Standard postoperative care is very different in the United States than in China, and some of these treatment differences could play an important role in postoperative gastrointestinal motility.
Applications
Future studies examining the use of acupuncture to prevent or treat PPOI should include assessment of activity, diet, and postoperative medication for pain control.
Terminology
For the purposes of this study, PPOI was defined as an inability to pass flatus or have a bowel movement by 96 h after surgery.
Peer review
In this study, the authors investigated whether acupuncture can prevent PPOI after intraperitoneal surgery for colon cancer. Their results show that acupuncture cannot prevent PPI in this population. Subset analyses also suggest that acupuncture is not useful for treating PPOI. This was a prospective, randomized study, with novelty and innovation. It will be helpful for the surgeons to choose appropriate therapy for PPOI after abdominal surgery. Presentation and readability of the manuscript is good for publication.
Footnotes
Supported by US National Cancer Institute (NCI) grants CA108084 and CA12153031
Peer reviewers: Dr. Kalpesh Jani, MS, DNB, FNB, MNAMS, FICS, FACS (USA), Consultant GI & Laparoscopic Surgeon, SIGMA Surgery, 390011 Baroda, Gujarat, India; Naoki Hiki, MD, PhD, Cancer Institute Hospital, 3-10-6, Ariake, Koto-ku, Tokyo 135-8550, Japan
S- Editor Wang JL L- Editor Kerr C E- Editor Ma WH
References
- 1.Condon RE, Frantzides CT, Cowles VE, Mahoney JL, Schulte WJ, Sarna SK. Resolution of postoperative ileus in humans. Ann Surg. 1986;203:574–581. doi: 10.1097/00000658-198605000-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Livingston EH, Passaro EP Jr. Postoperative ileus. Dig Dis Sci. 1990;35:121–132. doi: 10.1007/BF01537233. [DOI] [PubMed] [Google Scholar]
- 3.Witte CL, Witte MH. Ileus and ignorance. West J Med. 1993;158:532–534. [PMC free article] [PubMed] [Google Scholar]
- 4.Waldhausen JH, Schirmer BD. The effect of ambulation on recovery from postoperative ileus. Ann Surg. 1990;212:671–677. doi: 10.1097/00000658-199012000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barker P, Allcutt D, McCollum CN. Pulsed electromagnetic energy fails to prevent postoperative ileus. J R Coll Surg Edinb. 1984;29:147–150. [PubMed] [Google Scholar]
- 6.Disbrow EA, Bennett HL, Owings JT. Effect of preoperative suggestion on postoperative gastrointestinal motility. West J Med. 1993;158:488–492. [PMC free article] [PubMed] [Google Scholar]
- 7.Sculati O, Bardi M, Radrizzani D, Paganoni A, Iapichino G, Giampiccoli G. Preoperative fibre and postoperative ileus. Lancet. 1980;1:1252–1253. doi: 10.1016/s0140-6736(80)91712-2. [DOI] [PubMed] [Google Scholar]
- 8.Sculati O, Giampiccoli G, Gozzi B, Minissale V, Zambetti N, Iapichino G, Ipezzoli C, Giacomelli M, Lazzari P, Franzosi MG. Bran diet for an earlier resolution of post-operative ileus. J Int Med Res. 1982;10:194–197. doi: 10.1177/030006058201000310. [DOI] [PubMed] [Google Scholar]
- 9.McCallum RW. Clinical pharmacology forum: motility agents and the gastrointestinal tract. Am J Med Sci. 1996;312:19–26. doi: 10.1097/00000441-199607000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Ferraz AA, Cowles VE, Condon RE, Carilli S, Ezberci F, Frantzides CT, Schulte WJ. Nonopioid analgesics shorten the duration of postoperative ileus. Am Surg. 1995;61:1079–1083. [PubMed] [Google Scholar]
- 11.Kelley MC, Hocking MP, Marchand SD, Sninsky CA. Ketorolac prevents postoperative small intestinal ileus in rats. Am J Surg. 1993;165:107–111; discussion 112. doi: 10.1016/s0002-9610(05)80412-x. [DOI] [PubMed] [Google Scholar]
- 12.Tollesson PO, Cassuto J, Faxén A, Rimbäck G, Mattsson E, Rosén S. Lack of effect of metoclopramide on colonic motility after cholecystectomy. Eur J Surg. 1991;157:355–358. [PubMed] [Google Scholar]
- 13.Tollesson PO, Cassuto J, Rimbäck G, Faxén A, Bergman L, Mattsson E. Treatment of postoperative paralytic ileus with cisapride. Scand J Gastroenterol. 1991;26:477–482. doi: 10.3109/00365529108998569. [DOI] [PubMed] [Google Scholar]
- 14.Bonacini M, Quiason S, Reynolds M, Gaddis M, Pemberton B, Smith O. Effect of intravenous erythromycin on postoperative ileus. Am J Gastroenterol. 1993;88:208–211. [PubMed] [Google Scholar]
- 15.Yeo CJ, Barry MK, Sauter PK, Sostre S, Lillemoe KD, Pitt HA, Cameron JL. Erythromycin accelerates gastric emptying after pancreaticoduodenectomy. A prospective, randomized, placebo-controlled trial. Ann Surg. 1993;218:229–237; discussion 237-238. doi: 10.1097/00000658-199309000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maron DJ, Fry RD. New therapies in the treatment of postoperative ileus after gastrointestinal surgery. Am J Ther. 2008;15:59–65. doi: 10.1097/MJT.0b013e31804c6f37. [DOI] [PubMed] [Google Scholar]
- 17.Stewart D, Waxman K. Management of postoperative ileus. Am J Ther. 2007;14:561–566. doi: 10.1097/MJT.0b013e31804bdf54. [DOI] [PubMed] [Google Scholar]
- 18.Jørgensen H, Wetterslev J, Møiniche S, Dahl JB. Epidural local anaesthetics versus opioid-based analgesic regimens on postoperative gastrointestinal paralysis, PONV and pain after abdominal surgery. Cochrane Database Syst Rev. 2000:CD001893. doi: 10.1002/14651858.CD001893. [DOI] [PubMed] [Google Scholar]
- 19.Traut U, Brügger L, Kunz R, Pauli-Magnus C, Haug K, Bucher HC, Koller MT. Systemic prokinetic pharmacologic treatment for postoperative adynamic ileus following abdominal surgery in adults. Cochrane Database Syst Rev. 2008:CD004930. doi: 10.1002/14651858.CD004930.pub3. [DOI] [PubMed] [Google Scholar]
- 20.Ponec RJ, Saunders MD, Kimmey MB. Neostigmine for the treatment of acute colonic pseudo-obstruction. N Engl J Med. 1999;341:137–141. doi: 10.1056/NEJM199907153410301. [DOI] [PubMed] [Google Scholar]
- 21.Johanson JF, Morton D, Geenen J, Ueno R. Multicenter, 4-week, double-blind, randomized, placebo-controlled trial of lubiprostone, a locally-acting type-2 chloride channel activator, in patients with chronic constipation. Am J Gastroenterol. 2008;103:170–177. doi: 10.1111/j.1572-0241.2007.01524.x. [DOI] [PubMed] [Google Scholar]
- 22.Thomas J, Karver S, Cooney GA, Chamberlain BH, Watt CK, Slatkin NE, Stambler N, Kremer AB, Israel RJ. Methylnaltrexone for opioid-induced constipation in advanced illness. N Engl J Med. 2008;358:2332–2343. doi: 10.1056/NEJMoa0707377. [DOI] [PubMed] [Google Scholar]
- 23.Yuan CS, Wei G, Foss JF, O’Connor M, Karrison T, Osinski J. Effects of subcutaneous methylnaltrexone on morphine-induced peripherally mediated side effects: a double-blind randomized placebo-controlled trial. J Pharmacol Exp Ther. 2002;300:118–123. doi: 10.1124/jpet.300.1.118. [DOI] [PubMed] [Google Scholar]
- 24.Kraft MD. Methylnaltrexone, a new peripherally acting mu-opioid receptor antagonist being evaluated for the treatment of postoperative ileus. Expert Opin Investig Drugs. 2008;17:1365–1377. doi: 10.1517/13543784.17.9.1365. [DOI] [PubMed] [Google Scholar]
- 25.Wolff BG, Weese JL, Ludwig KA, Delaney CP, Stamos MJ, Michelassi F, Du W, Techner L. Postoperative ileus-related morbidity profile in patients treated with alvimopan after bowel resection. J Am Coll Surg. 2007;204:609–616. doi: 10.1016/j.jamcollsurg.2007.01.041. [DOI] [PubMed] [Google Scholar]
- 26.Delaney CP, Weese JL, Hyman NH, Bauer J, Techner L, Gabriel K, Du W, Schmidt WK, Wallin BA. Phase III trial of alvimopan, a novel, peripherally acting, mu opioid antagonist, for postoperative ileus after major abdominal surgery. Dis Colon Rectum. 2005;48:1114–1125; discussion 1125-1126; author reply 1127-1129. doi: 10.1007/s10350-005-0035-7. [DOI] [PubMed] [Google Scholar]
- 27.Crowell MD, DiBaise JK. Is alvimopan a safe and effective treatment for postoperative ileus? Nat Clin Pract Gastroenterol Hepatol. 2007;4:484–485. doi: 10.1038/ncpgasthep0899. [DOI] [PubMed] [Google Scholar]
- 28.Tan EK, Cornish J, Darzi AW, Tekkis PP. Meta-analysis: Alvimopan vs. placebo in the treatment of post-operative ileus. Aliment Pharmacol Ther. 2007;25:47–57. doi: 10.1111/j.1365-2036.2006.03150.x. [DOI] [PubMed] [Google Scholar]
- 29.Chen SF, Li YQ, He FY. [Effect of Saussurea lappa on gastric functions] Zhongguo Zhongxiyi Jiehe Zazhi. 1994;14:406–408. [PubMed] [Google Scholar]
- 30.Chen X, Ran R. [Rhubarb decoction prevents intestinal bacterial translocation during necrotic pancreatitis] Huaxi Yike Daxue Xuebao. 1996;27:418–421. [PubMed] [Google Scholar]
- 31.Tatsuta M, Iishi H. Effect of treatment with liu-jun-zi-tang (TJ-43) on gastric emptying and gastrointestinal symptoms in dyspeptic patients. Aliment Pharmacol Ther. 1993;7:459–462. doi: 10.1111/j.1365-2036.1993.tb00120.x. [DOI] [PubMed] [Google Scholar]
- 32.Deng L, Gan Y, He S, Ji X, Li Y, Wang R, Wang W, Wang X, Xu H, Xue X, et al. Chinese acupuncture and moxibustion. In: Cheng X, editor. Beijing: Foreign Languages Press; 1997. [Google Scholar]
- 33.Lin X, Liang J, Ren J, Mu F, Zhang M, Chen JD. Electrical stimulation of acupuncture points enhances gastric myoelectrical activity in humans. Am J Gastroenterol. 1997;92:1527–1530. [PubMed] [Google Scholar]
- 34.Balestrini JL, Tsuchida D, Fukuda H, Pappas TN, Takahashi T. Acupuncture accelerates delayed gastrointestinal transit after abdominal surgery in conscious rats. Scand J Gastroenterol. 2005;40:734–735. doi: 10.1080/00365520510015719. [DOI] [PubMed] [Google Scholar]
- 35.Lin Z, Chen JD. Advances in gastrointestinal electrical stimulation. Crit Rev Biomed Eng. 2002;30:419–457. doi: 10.1615/critrevbiomedeng.v30.i456.70. [DOI] [PubMed] [Google Scholar]
- 36.Dai JL, Ren ZJ, Fu ZM, Zhu YH, Xu SF. Electroacupuncture reversed the inhibition of intestinal peristalsis induced by intrathecal injection of morphine in rabbits. Chin Med J (Engl) 1993;106:220–224. [PubMed] [Google Scholar]
- 37.Dill SG. Acupuncture for gastrointestinal disorders. Probl Vet Med. 1992;4:144–154. [PubMed] [Google Scholar]
- 38.Diehl DL. Acupuncture for gastrointestinal and hepatobiliary disorders. J Altern Complement Med. 1999;5:27–45. doi: 10.1089/acm.1999.5.27. [DOI] [PubMed] [Google Scholar]
- 39.Basika R, Weber-Kraus B, Weber F. Proceedings of the 26th IVAS World Congress on Veterinary Acupuncture & Related Techniques. Beijing: Foreign Languages Press; 2000. p. Vienna, Austria. International Veterinary Acupuncture Society. [Google Scholar]
- 40.Li Y, Tougas G, Chiverton SG, Hunt RH. The effect of acupuncture on gastrointestinal function and disorders. Am J Gastroenterol. 1992;87:1372–1381. [PubMed] [Google Scholar]
- 41.Klauser AG, Rubach A, Bertsche O, Müller-Lissner SA. Body acupuncture: effect on colonic function in chronic constipation. Z Gastroenterol. 1993;31:605–608. [PubMed] [Google Scholar]
- 42.Miller RD. Anesthesia. 3rd ed. New York: Churchill Livingstone; 1990. [Google Scholar]
- 43.Klauser AG, Rubach A, Bertsche O, Müller-Lissner SA. Body acupuncture: effect on colonic function in chronic constipation. Z Gastroenterol. 1993;31:605–608. [PubMed] [Google Scholar]
- 44.Pocock SJ. Clinical Trials: A Practical Approach. New York: Wiley; 1983. [Google Scholar]
- 45.Deadman P, Al-Khafaji M, Baker K. A Manual of Acupuncture. East Sussex: Journal of Chinese Medicine Publications; 1999. [Google Scholar]
- 46.Bruera E, Kuehn N, Miller MJ, Selmser P, Macmillan K. The Edmonton Symptom Assessment System (ESAS): a simple method for the assessment of palliative care patients. J Palliat Care. 1991;7:6–9. [PubMed] [Google Scholar]
- 47.Nekolaichuk CL, Bruera E, Spachynski K, MacEachern T, Hanson J, Maguire TO. A comparison of patient and proxy symptom assessments in advanced cancer patients. Palliat Med. 1999;13:311–323. doi: 10.1191/026921699675854885. [DOI] [PubMed] [Google Scholar]
- 48.Nekolaichuk CL, Maguire TO, Suarez-Almazor M, Rogers WT, Bruera E. Assessing the reliability of patient, nurse, and family caregiver symptom ratings in hospitalized advanced cancer patients. J Clin Oncol. 1999;17:3621–3630. doi: 10.1200/JCO.1999.17.11.3621. [DOI] [PubMed] [Google Scholar]
- 49.Trotti A, Colevas AD, Setser A, Rusch V, Jaques D, Budach V, Langer C, Murphy B, Cumberlin R, Coleman CN, et al. CTCAE v3.0: development of a comprehensive grading system for the adverse effects of cancer treatment. Semin Radiat Oncol. 2003;13:176–181. doi: 10.1016/S1053-4296(03)00031-6. [DOI] [PubMed] [Google Scholar]
- 50.NIH Consensus Conference. Acupuncture. JAMA. 1998;280:1518–1524. [PubMed] [Google Scholar]