Abstract
AIM: To determine the frequency and clinical impact of incidental findings detected with magnetic resonance imaging (MRI)-enterography in patients with suspected or known Crohn’s disease (CD).
METHODS: Incidental findings were defined as unexpected lesions outside the small intestine, not previously known or suspected at the time of referral, and not related to inflammatory bowel disease. Through a systematic review of medical charts we analyzed the clinical impact of incidental findings, and compared the MRI findings with subsequent diagnostic procedures.
RESULTS: A total of 283 patients were included in the analysis, and MRI detected active CD in 31%, fistula in 1.4% and abscess in 0.7%. Extra-intestinal findings not related to CD were recorded in 72 patients (25%), of which 58 patients (20%) had 74 previously unknown lesions. Important or incompletely characterized findings were detected in 17 patients (6.0%). Incidental findings led to 12 further interventions in 9 patients (3.2%) revealing previously unknown pathological conditions in 5 (1.8%). One patient (0.4%) underwent surgery and one patient was diagnosed with a malignant disease. MRI detected incidental colonic lesions in 16 patients of which additional work-up in 4 revealed normal anatomy. Two patients (0.7%) benefitted from the additional examinations, whereas incidental findings led to unnecessary examinations in 9 (3.2%).
CONCLUSION: In a minority of patients with suspected or known CD, important incidental findings are diagnosed at MRI-enterography. However, a substantial number of patients experience unnecessary morbidity because of additional examinations of benign or normal conditions.
Keywords: Magnetic resonance imaging, Incidental findings, Crohn’s disease, Small intestine
INTRODUCTION
In recent years magnetic resonance imaging (MRI) has been increasingly used for the assessment of small bowel Crohn’s disease (CD). MRI has a high diagnostic accuracy[1-12] and reproducibility[12], both with enteroclysis and the oral contrast method (enterography), for evaluating CD. Unlike conventional enteroclysis, MRI enables visualization of disease extension beyond the intestinal wall, i.e. abscesses and fistulas. In comparison with enteroclysis, MRI detects additional extra-intestinal lesions in 24%-58% of patients[1,3]. However, some extra-intestinal findings are unexpected and not related to CD, and are often referred to as incidental findings. The ability to detect incidental findings presents a clinical dilemma. On one hand, modern imaging techniques may detect early extra-intestinal malignant disease or disease requiring clinical intervention, thereby reducing morbidity and mortality. On the other hand, incidental findings may lead to further diagnostic work-up or surgery of benign lesions causing increased morbidity.
Only one previous study has analyzed the frequency of incidental findings in MRI-enteroclysis. Herfarth et al[13] found extra-intestinal lesions in 57% of 710 patients with suspected or known inflammatory bowel disease. Lesions of major clinical importance were detected in 12% of patients, of which the majority consisted of extra-intestinal manifestations of CD (abscesses). Findings were classified as tumor, metastasis or mass in 1.3% of patients. Ajaj et al[14] performed MRI-colonography in 375 patients with suspected colonic diseases and detected extra-colonic lesions in 69%, with 12% requiring additional examinations Approximately half of the extra-colonic lesions were previously unknown. These results emphasize that extra-intestinal findings are common when performing MRI of the abdomen. A significant proportion of incidental findings are clinically important and have an impact on clinical decision-making. However, these studies did not include the results of subsequent diagnostic work-up to reveal the benefit from detection of incidental findings.
The purpose of this study was to determine the frequency and clinical impact of incidental findings detected at MRI-enterography in patients with known or suspected CD.
MATERIALS AND METHODS
This retrospective study was conducted in the Department of Radiology, Vejle Hospital part of Lillebaelt Hospital, Denmark. The Department introduced MRI-enterography in December 2003, and a study period from December 2003 to November 2007 was chosen, allowing a minimum of 1 year follow-up after MRI. All MRI-enterographies performed in the study period were identified in the hospital’s computerized radiology information system, and radiology reports were printed out. Through a systematic review of medical charts we analyzed the clinical impact of incidental findings and compared the MRI findings with subsequent diagnostic procedures. All reports were reviewed independently by the first author.
Criteria for inclusion and exclusion
MRI-enterographies performed in patients with suspected or known CD having symptoms consistent with disease activity or complications were included in the study. The subsequent analysis focused on incidental findings defined as unexpected findings outside the small intestine not previously known or suspected at the time of referral and not related to inflammatory bowel disease. Hence, extra-intestinal manifestations of CD (abscesses and fistulas) were not regarded as incidental findings.
Examinations performed on indications other than CD, repeated MRI-enterographies, and examination failures because of technical malfunctions or patient discomfort were excluded. In order to minimize selection bias, the study population was restricted to patients with no previous MRI-enterographies. The likelihood of previously unknown findings outside the small intestine is substantially reduced in repeated scans during a short study period. Therefore, in cases of 2 or more examinations performed, only the first MRI scan was included.
A total 354 patients underwent MRI-enterography. Twenty-nine scans were performed on indications other than inflammatory bowel disease, and additionally 2 scans were excluded because of failure to perform the examination. Both patients were unwilling to ingest the enteral contrast. A total of 40 scans in 29 patients were excluded because of repeated MRI-enterographies in the study period. Hence, a total of 283 MRI-enterography examinations in 283 patients were included in the analysis.
A clinical impact was defined as one or more subsequent interventions, i.e. additional diagnostic work-up, medical and/or surgical treatment, solely caused by the incidental finding at MRI-enterography. The clinical impact was assessed by analyzing the number of patients with subsequent clinical interventions, and the number and type of interventions performed in each patient. Incidental findings were classified as true or false positive on the basis of the diagnostic work-up and as beneficial or unnecessary for the patient. Data were collected from radiological reports, medical charts, laboratory data and the results of subsequent diagnostic procedures. Information was collected from the hospital’s computerized medical charts and radiology information system. In patients referred from other hospitals, referrals and medical charts were collected from the department in charge of treatment.
Ethics
The study was approved by the local ethics committee of Southern Denmark and the Danish Data Protection Agency. In a few patients diagnostic work-up was performed at other hospitals, and prior to collecting these data, patients gave informed consent.
Imaging technique
Scans were carried out with an Intera 1.5T MRI system with a 5 element Syn-body coil (Philips Medical Systems, Eindhoven, The Netherlands). The evening before the examination, patients were instructed to eat a light meal and fast overnight. They were allowed to drink water prior to the examination. Patients received 1000 mL water mixed with psyllium husk fiber ingested gradually over one hour. Patients were examined in the supine position. The protocol contained the sequences Cor T1 (TR/TE, 7/3.4; flip angel 15; slice thickness 4 mm; 208 matrix; FOV 375), Cor T2 (B-FFE; TR/TE, 4.1/2.0 ms; flip angle, 60; slice thickness 5 mm; 224 matrix; FOV 400), Cor SPIR (TR/TE, 3000/125 ms; flip angel 90; slice thickness 7 mm; 256 matrix; FOV 400) and axial T1W (TR/TE, 7/3.4; flip angel 15; slice thickness 4 mm; 208 matrix; FOV 375) with discontinuous breath-hold before and after contrast. Gadodiamide 0.1 mmol/kg (GE Healthcare, Medical Diagnostics, Oslo, Norway) was given intravenously, and hyoscinbutylbromide 20 mg (Buscopan, Boehringer Ingelheim, Basel, Switzerland) was administered to reduce peristalsis during the procedure. All images were evaluated using an Impax PACS workstation (Agfa, Mortsel, Belgium) with 2 Coronis monitors (1600 × 1200 pixels) (Megapixels Diagnostic Display System, Barco, Kortijk, Belgium). Radiologists performing the studies were all specialist doctors with experience in abdominal MRI techniques.
Classification of scans
MRI-enterographies were classified according to the most important incidental finding. Lesions were assessed as proposed by Zalis et al[15] for computed tomography (CT) colonography. E0 is an examination in which technical factors severely limit evaluation, e.g. because of artifacts. E1 denotes a normal examination or variants in anatomy that are not expected to affect the patient’s health status. E2 refers to examinations with clinically unimportant extra-intestinal findings. E3 denotes incompletely characterized findings that are likely to be benign and E4 refers to examinations with potentially important extra-intestinal findings. Classification of scans was performed by the first author on the basis of the radiological reports and prior to analyzing the clinical impact of incidental findings. The co-authors subsequently evaluated the classification of incidental findings, and agreement was attained. Incidental findings located in the colon were analyzed separately.
Statistical analysis
Data were analyzed using descriptive statistics. Difference in means was calculated using the Wilcoxon rank-sum test and P-values less than 0.05 were considered significant.
RESULTS
Of the 283 patients included in the study, 193 (68%) were female. The mean age of the study population was 38.7 years (range 9.9-84.9 years). The indication for MRI was suspected CD in 156, and newly diagnosed or known CD in 127. MRI examinations revealed active CD in 31%, fistula in 1.4%, and abscess in 0.7% of patients (Table 1). There was no difference in mean age between patients with known and suspected CD (P = 0.9).
Table 1.
Indications and results of 283 MRI investigations of the small intestine
| Clinical indication for MRI | n | Total | |
| Suspected CD | Diagnostic MRI in patients with suspected CD not confirmed at endoscopy | 156 | 156 |
| Known CD | Extension of newly diagnosed CD detected at endoscopy | 17 | |
| Evaluation of disease activity and extension or suspected complications of known CD | 110 | 127 | |
| Total | 283 | ||
| Results of MRI- enterographies | CD in the small intestine | 87 | 31% |
| Stenosis | 38 | 13% | |
| Entero-enteric fistula | 4 | 1.4% | |
| Intra-abdominal abscess | 2 | 0.7% | |
| Suspected IBD in the colon | 35 | 12% |
MRI: Magnetic resonance imaging; CD: Crohn’s disease; IBD: Inflammatory bowel disease.
Extra-intestinal incidental findings
Extra-intestinal findings were recorded in 72 patients, of which 58 patients (20%) had previously unknown findings. Forty-one scans were classified E2, 11 were E3, and 5 were E4. In 225 scans no or previously known extra-intestinal lesions were recorded. In one examination the radiologist suspected multi-cystic ovaries, but evaluation of extra-intestinal organs was significantly compromised. The examination was classified E0, even though the finding led to further diagnostic work-up.
Seventy four incidental findings were detected in 58 patients (Table 2). In 43 patients only one finding was recorded, 14 patients had 2 findings, and 3 findings were recorded in one patient. The most frequent findings were benign cysts in the kidneys, ovaries and liver requiring no further work-up (n = 39). In 12 patients (4.2%) incompletely characterized extra-intestinal findings (E3) were detected. Of these, 2 patients had a large bladder suggesting previously unknown lower urinary tract disease, and one scan revealed a large hepatic cyst with a diameter of 15 cm displacing the right kidney. Potentially important findings (E4) were recorded in 5 patients (1.8%). Three patients had an undetermined mass or a cystic lesion in conjunction to the ovaries and pelvis wall, and further work-up was recommended. One scan revealed a focal hepatic lesion (atypical hemangioma), and one patient was diagnosed with an abdominal aortic aneurysm (Figure 1).
Table 2.
Previously unknown extra-intestinal findings in 58 patients
| Finding | n | ||
| E0 | Female genitals | Suspected multi-cystic ovaries | 1 |
| E2 | Liver | Hepatic cysts | 3 |
| Gallstones | 7 | ||
| Kidney | Renal cysts | 19 | |
| Renal anatomical variants | 3 | ||
| Reduced kidney size | 1 | ||
| Metallic artifact in the kidney | 1 | ||
| Female genitals | Leiomyomas in the uterus | 4 | |
| Ovarian cysts | 14 | ||
| Miscellaneous | Atrophy of the abdominal musculature after surgery | 1 | |
| Small amounts of free abdominal fluid | 3 | ||
| 56 | |||
| E3 | Liver | Large hepatic cyst with displacement of the right kidney | 1 |
| Urinary tract | Bilateral nephropathy with reduced kidney size1 | 2 | |
| Large bladder | 2 | ||
| Female genitals | Free fluid in the pelvis and suspected leiomyoma of the uterus | 1 | |
| Two lobulated and cystic lesions in the pelvis | 1 | ||
| Miscellaneous | Splenomegaly | 1 | |
| Ascites | 1 | ||
| Bilateral hip joint effusion | 1 | ||
| Lymphadenopathy in the mesentery | 1 | ||
| Spondylosis and spinal stenosis | 1 | ||
| 12 | |||
| E4 | Focal hepatic lesion (atypical hepatic hemangioma) | 1 | |
| Unexplained mass in conjunction to the ovaries | 3 | ||
| Abdominal aortic aneurysm | 1 | ||
| 5 | |||
| Total | 74 | ||
Both patients had a normal S-creatinine at the time of MRI-enterography with intravenous contrast.
Figure 1.
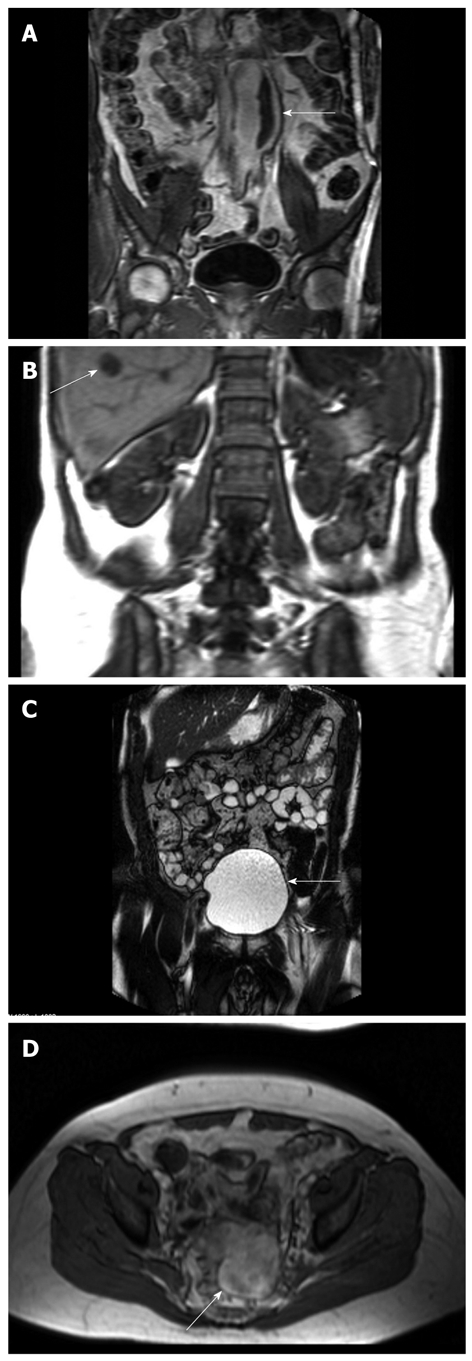
Incidental findings at MRI-enterography. A: Abdominal aortic aneurysm (arrow). CT scan confirmed the aneurysm and ruled out rupture; B: Atypical hepatic hemangioma (arrow). The results of ultrasound-guided biopsy were benign; C: Large bladder leading to diagnostic work-up and diagnosis of prostate cancer (arrow); D: A lesion with a diameter of 6 cm in the small pelvis (arrow) was confirmed with transvaginal ultrasound. Surgery showed a torquated leiomyoma in the top of the uterus.
Significantly more scans were classified E3 and E4 in patients with suspected CD (15 out of 156) than known CD (one out of 127) suggesting that incidental findings necessitating further diagnostic work-up are more common in this group of patients (P = 0.001). Except for bilateral hip joint effusion, all E3 and E4 findings were detected in patients with suspected CD, and one patient had 2 E3 findings (Table 2).
Clinical impact of extra-intestinal findings
Extra-intestinal findings resulted in 12 clinical interventions in 9 patients (3.2%). The interventions consisted of ultrasound examination in one, ultrasound-guided biopsy in one, contrast-enhanced ultrasound and biopsy in one, CT-scan in one, gynecological examination including transvaginal ultrasound in 5, surgery in one and biochemical tests in one (Table 3). Succeeding work-up resulted in 5 true positive extra-intestinal findings and 3 false positive findings. One patient with bilateral hip joint effusion failed to attend the follow-up ultrasound examination.
Table 3.
Previously unknown extra-intestinal findings leading to further examinations and the result of diagnostic work-up
| Extra-intestinal finding | Clinical intervention | Result of diagnostic work-up | |
| 5 true positive findings | Abdominal aortic aneurysm (E4) | CT-scan of the aorta | Abdominal aortic aneurism without rupture |
| Focal hepatic lesion (E4) | Contrast-enhanced US and biopsy (atypical hemangioma) | Hemangioma | |
| Two unexplained masses in conjunction to the ovaries (E4) | GE and transvaginal US | Leiomyomas | |
| Surgery | |||
| Free fluid in the pelvis and suspected leiomyoma of the uterus (E3) | GE and transvaginal US | Leiomyoma | |
| Large bladder (E3) | Transrectal US and biopsy | Prostate cancer | |
| Abdominal CT scan | |||
| Biochemistry (PSA) | |||
| 3 false positive findings | 4.5 cm cystic lesion with an excrescens associated with the cyst wall (E4) | GE and transvaginal US | Normal |
| 2.9 cm solid lesion in the pelvis and displacement of the uterus (E4) | GE and transvaginal US | Normal | |
| Multicystic ovaries (E0) | GE and transvaginal US | Normal | |
| Results not available | Bilateral hip joint effusion (E3) | Referred for US examination | The patient did not attend the examination |
US: Ultrasound; GE: Gynecological examination; PSA: Prostate-specific antigen; CT: Computed tomography.
In a patient with suspected CD, MRI showed an enlarged bladder. The patient was referred for further urological examinations, and was subsequently diagnosed with a previously unknown prostate cancer. In another patient, MRI revealed a 6 cm wide and 9 cm long abdominal aortic aneurysm. CT scan of the aorta confirmed the aneurysm, and ruled out rupture. Five patients diagnosed with one or more lesions associated with the female genitals had further diagnostic work-up. In one patient, MRI showed a 6 cm large lesion in the small pelvis, and the finding was confirmed with transvaginal ultrasound. The patient underwent surgery, which showed a 5 cm × 4 cm × 5 cm torquated leiomyoma in the top of the uterus and 2 smaller leiomyomas in the anterior wall of the uterus. The surgeon performed a hysterectomy.
Incidental findings in the colon
MRI revealed incidental findings located in the colon and not related to inflammatory bowel disease in 16 patients (5.7%, Table 4), of whom 5 also had an extra-intestinal finding (E2 in all). In 12 patients, colonic findings were of minor or no clinical relevance. Four patients underwent additional examinations because of mucosal changes not characteristic of inflammatory bowel disease. The examinations revealed no pathological conditions.
Table 4.
Sixteen incidental findings located in the colon and their clinical impact
| Finding | n | Clinical intervention | Result of diagnostic work-up |
| Suspected benign neoplasia (3 cm large polyp) | 1 | Colonoscopy and CT-colonography | Normal |
| Coprostasis | 7 | - | - |
| Indeterminate thickening of the cecum mucosa | 2 | Colonoscopy | Normal |
| Displacement of the cecum | 3 | - | - |
| Diverticulosis | 2 | - | - |
| Suspected malignant neoplasia | 1 | Colonoscopy and abdominal CT scan | Normal |
DISCUSSION
Few studies have dealt with incidental findings in abdominal MRI. In a recent retrospective study, Herfarth et al[13] analyzed extra-intestinal findings in MRI-enteroclysis. In 710 patients with suspected or known inflammatory bowel disease 57% had extra-intestinal lesions and 12% of the observed lesions were of major clinical importance. In 5 patients (0.7%) extra-intestinal findings were suspicious of previously unknown malignant disease. However, findings of major importance were mainly abscesses related to CD, and comparison with the present study is difficult because of different study designs.
Extensive work has been done on extra-intestinal findings in CT-colonography. Results are summarized in a comprehensive review from 2005 including 17 studies. In total 40% of patients were recorded to have extra-colonic abnormalities, 14% had further diagnostic work-up and extra-colonic cancers were detected in 2.7%[16]. The cancer detection rate was reported in 5 studies and varied from 0.4% to 4.6% with the highest rates in the elderly.
In the present study, MRI-enterography revealed incidental findings located outside the small intestine and not related to CD in 25% of patients resulting in additional examinations in 5%. Additional investigations confirmed abnormal lesions in 1.8%, and one patient had a malignant disease. Two patients benefitted from the additional examinations (aortic aneurysm and prostate cancer), whereas incidental findings led to unnecessary examinations in 9 patients. Detection of extra-intestinal manifestations of CD was rare (1.8%).
Incompletely characterized or clinically important findings were more common in patients with suspected than known CD, suggesting that findings necessitating additional work-up are more frequent in this group of patients. Because of the retrospective nature of this study, and the small number of patients referred for additional examinations, it was not possible to elucidate further on this assumption or whether incidental findings could explain the patients’ symptoms. A prospective study would clarify this issue.
Comparing studies can be troublesome because of differences in population characteristics, classification systems, examination protocols and study designs. In the present study we used an MRI technique with intravenous contrast in a young population with a low risk of malignant disease. Compared to the study by Ajaj et al[14] we detected fewer extra-intestinal lesions, and the frequency of malignant disease was much higher when performing MRI-colonography. In an overall comparison with CT studies we also found a lower frequency of extra-intestinal findings and a lower rate of additional work-up. These discrepancies probably arise from differences in age, prior morbidity and the risk of malignant disease in the study populations.
MRI-enterography is a relatively new modality for evaluating CD in the small intestine. Ileo-colonoscopy, CT-enterography, capsule endoscopy, abdominal ultrasound and small bowel enteroscopy are alternative examinations. Choosing between modalities relies on several factors. Primarily a modality with a high sensitivity and specificity for luminal abnormalities as well as pathology in the bowel wall and extra-intestinal manifestations of CD is essential. Also other aspects of the investigations should be considered: risk of complications (aspiration, capsule retention, radiation exposure, etc.), patient discomfort, complexity of the examinations, accessibility, costs, and finally the impact of incidental findings. In the present study, the detection rate of clinically significant lesions outside the small intestine was low. In contrast, incidental findings led to unnecessary examinations in a substantial number of patients. Hence, in comparison with other modalities the detection rate of important incidental lesions was too low to be an argument in itself for performing MRI-enterography in patients with suspected or known CD.
Our study was limited by its retrospective design. Radiological reports were not performed with the focus on incidental findings, and underestimation of clinically unimportant findings are likely. The study population contained a preponderance of women (ratio 2:1), which is reflected by the frequency of incidental findings in the female genitalia. The second most common finding was ovarian cysts, and lesions in the female genitals were common in all classification groups. It is well established that CD is more common in females (1.2-1.5:1) and in specialized centers for inflammatory bowel diseases the prevalence of women with irritable bowel syndrome is up to 4 times as high as that of men[17,18].
In conclusion, incidental findings were common in patients with known and suspected CD having MRI for evaluation of small intestinal disease. Additional examinations revealed important disease in only a minority of patients. However, a substantial number of patients experienced unnecessary morbidity because of the additional examinations of benign or normal conditions. The detection rate of important incidental lesions not related to CD was too low to be an argument in itself for performing MRI-enterography in this group of patients.
COMMENTS
Background
Magnetic resonance imaging (MRI) is increasingly used in the assessment of small bowel Crohn’s disease (CD). Unlike conventional radiology, MRI enables visualization of disease extension beyond the intestinal wall, i.e. abscesses and fistulas. However, some extra-intestinal findings are unexpected and without relation to CD (incidental findings).
Research frontiers
Only a few studies have described the clinical impact of incidental findings in abdominal MRI. Lesions may represent important diseases and benefit patients, but may also cause unnecessary morbidity because of the diagnostic work-up of benign lesions.
Innovations and breakthroughs
In 2 recent studies using abdominal MRI techniques, extra-intestinal lesions of major clinical importance were common. However, these studies did not include the results of subsequent diagnostic work-up to reveal the benefit from detection of these findings. In the present study, incidental findings were common in patients having MRI for evaluation of small bowel CD. Additional examinations revealed important disease in a minority of patients. However, a substantial number of patients experienced unnecessary morbidity arising from the additional examinations of benign or normal conditions.
Applications
Several modalities for diagnosing small bowel CD are available. The present study emphasized that the detection rate of important incidental lesions was too low to be an argument in itself for performing MRI-enterography in this group of patients.
Peer review
Jensen et al gave a nice and clear description of the research background, materials, methods, results and conclusions. Significant points have been presented and compared with data from prior research. Used methods are advanced, and detailed descriptions are provided allowing other investigators to reproduce or validate them. The statistical methods are appropriate. From the presented results, sufficient data can be drawn. In discussion, valuable conclusions are provided. References are appropriate and relevant. Tables and figures reflect the major findings of the study.
Footnotes
Peer reviewer: Marko Duvnjak, MD, Department of Gastroenterology and Hepatology, Sestre milosrdnice University Hospital, Vinogradska cesta 29, 10 000 Zagreb, Croatia
S- Editor Tian L L- Editor Cant MR E- Editor Ma WH
References
- 1.Masselli G, Casciani E, Polettini E, Gualdi G. Comparison of MR enteroclysis with MR enterography and conventional enteroclysis in patients with Crohn’s disease. Eur Radiol. 2008;18:438–447. doi: 10.1007/s00330-007-0763-2. [DOI] [PubMed] [Google Scholar]
- 2.Negaard A, Paulsen V, Sandvik L, Berstad AE, Borthne A, Try K, Lygren I, Storaas T, Klow NE. A prospective randomized comparison between two MRI studies of the small bowel in Crohn’s disease, the oral contrast method and MR enteroclysis. Eur Radiol. 2007;17:2294–2301. doi: 10.1007/s00330-007-0648-4. [DOI] [PubMed] [Google Scholar]
- 3.Schreyer AG, Geissler A, Albrich H, Schölmerich J, Feuerbach S, Rogler G, Völk M, Herfarth H. Abdominal MRI after enteroclysis or with oral contrast in patients with suspected or proven Crohn’s disease. Clin Gastroenterol Hepatol. 2004;2:491–497. doi: 10.1016/s1542-3565(04)00168-5. [DOI] [PubMed] [Google Scholar]
- 4.Masselli G, Casciani E, Polettini E, Lanciotti S, Bertini L, Gualdi G. Assessment of Crohn’s disease in the small bowel: Prospective comparison of magnetic resonance enteroclysis with conventional enteroclysis. Eur Radiol. 2006;16:2817–2827. doi: 10.1007/s00330-006-0338-7. [DOI] [PubMed] [Google Scholar]
- 5.Gourtsoyiannis NC, Grammatikakis J, Papamastorakis G, Koutroumbakis J, Prassopoulos P, Rousomoustakaki M, Papanikolaou N. Imaging of small intestinal Crohn’s disease: comparison between MR enteroclysis and conventional enteroclysis. Eur Radiol. 2006;16:1915–1925. doi: 10.1007/s00330-006-0248-8. [DOI] [PubMed] [Google Scholar]
- 6.Del Vescovo R, Sansoni I, Caviglia R, Ribolsi M, Perrone G, Leoncini E, Grasso RF, Cicala M, Zobel BB. Dynamic contrast enhanced magnetic resonance imaging of the terminal ileum: differentiation of activity of Crohn’s disease. Abdom Imaging. 2008;33:417–424. doi: 10.1007/s00261-007-9267-4. [DOI] [PubMed] [Google Scholar]
- 7.Maccioni F, Bruni A, Viscido A, Colaiacomo MC, Cocco A, Montesani C, Caprilli R, Marini M. MR imaging in patients with Crohn disease: value of T2- versus T1-weighted gadolinium-enhanced MR sequences with use of an oral superparamagnetic contrast agent. Radiology. 2006;238:517–530. doi: 10.1148/radiol.2381040244. [DOI] [PubMed] [Google Scholar]
- 8.Ochsenkühn T, Herrmann K, Schoenberg SO, Reiser MF, Göke B, Sackmann M. Crohn disease of the small bowel proximal to the terminal ileum: detection by MR-enteroclysis. Scand J Gastroenterol. 2004;39:953–960. doi: 10.1080/00365520410003218. [DOI] [PubMed] [Google Scholar]
- 9.Darbari A, Sena L, Argani P, Oliva-Hemker JM, Thompson R, Cuffari C. Gadolinium-enhanced magnetic resonance imaging: a useful radiological tool in diagnosing pediatric IBD. Inflamm Bowel Dis. 2004;10:67–72. doi: 10.1097/00054725-200403000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Laghi A, Borrelli O, Paolantonio P, Dito L, Buena de Mesquita M, Falconieri P, Passariello R, Cucchiara S. Contrast enhanced magnetic resonance imaging of the terminal ileum in children with Crohn’s disease. Gut. 2003;52:393–397. doi: 10.1136/gut.52.3.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Koh DM, Miao Y, Chinn RJ, Amin Z, Zeegen R, Westaby D, Healy JC. MR imaging evaluation of the activity of Crohn’s disease. AJR Am J Roentgenol. 2001;177:1325–1332. doi: 10.2214/ajr.177.6.1771325. [DOI] [PubMed] [Google Scholar]
- 12.Negaard A, Sandvik L, Mulahasanovic A, Berstad AE, Klöw NE. Magnetic resonance enteroclysis in the diagnosis of small-intestinal Crohn’s disease: diagnostic accuracy and inter- and intra-observer agreement. Acta Radiol. 2006;47:1008–1016. doi: 10.1080/02841850600979071. [DOI] [PubMed] [Google Scholar]
- 13.Herfarth HH, Grunert M, Klebl F, Strauch U, Feuerbach S, Schölmerich J, Rogler G, Schreyer AG. Frequency and nature of incidental extra-enteric lesions found on magnetic resonance enterography (MR-E) in patients with inflammatory bowel diseases (IBD) PLoS One. 2009;4:e4863. doi: 10.1371/journal.pone.0004863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ajaj W, Ruehm SG, Ladd SC, Gerken G, Goyen M. Utility of dark-lumen MR colonography for the assessment of extra-colonic organs. Eur Radiol. 2007;17:1574–1583. doi: 10.1007/s00330-006-0549-y. [DOI] [PubMed] [Google Scholar]
- 15.Zalis ME, Barish MA, Choi JR, Dachman AH, Fenlon HM, Ferrucci JT, Glick SN, Laghi A, Macari M, McFarland EG, et al. CT colonography reporting and data system: a consensus proposal. Radiology. 2005;236:3–9. doi: 10.1148/radiol.2361041926. [DOI] [PubMed] [Google Scholar]
- 16.Xiong T, Richardson M, Woodroffe R, Halligan S, Morton D, Lilford RJ. Incidental lesions found on CT colonography: their nature and frequency. Br J Radiol. 2005;78:22–29. doi: 10.1259/bjr/67998962. [DOI] [PubMed] [Google Scholar]
- 17.Vind I, Riis L, Jess T, Knudsen E, Pedersen N, Elkjaer M, Bak Andersen I, Wewer V, Nørregaard P, Moesgaard F, et al. Increasing incidences of inflammatory bowel disease and decreasing surgery rates in Copenhagen City and County, 2003-2005: a population-based study from the Danish Crohn colitis database. Am J Gastroenterol. 2006;101:1274–1282. doi: 10.1111/j.1572-0241.2006.00552.x. [DOI] [PubMed] [Google Scholar]
- 18.Müller-Lissner SA, Bollani S, Brummer RJ, Coremans G, Dapoigny M, Marshall JK, Muris JW, Oberndorff-Klein Wolthuis A, Pace F, Rodrigo L, et al. Epidemiological aspects of irritable bowel syndrome in Europe and North America. Digestion. 2001;64:200–204. doi: 10.1159/000048862. [DOI] [PubMed] [Google Scholar]


