Abstract
Non-typhoidal salmonellosis, which is increasing nowadays in Korea as well as in the developed countries, is manifested as enteritis in most cases, but it also encompasses bacteremia, intraabdominal infections, and bone, joint and soft tissue infections. These rare diseases are known to result from primary gastrointestinal infection and subsequent bacteremia with or without symptoms. We experienced a case of neck abscess caused by Salmonella serotype D, which is a rare but important differential diagnosis of neck abscess. We herein report it.
Keywords: Salmonella, Salmonella infection, abscess, neck, liver cirrhosis
INTRODUCTION
Salmonella is an enteroinvasive bacterium which can cause protean clinical diseases. Gastroenteritis is most commonly encountered manifestation, and many other diseases could follow during or after bacteremia.1 Neck abscess is caused by several bacteria, however, cases with Salmonella are relatively rare. In the present case, neck abscess caused by Salmonella serotype D in a patient with liver cirrhosis and diabetic was successfully treated with antibiotics and surgical drainage.
CASE REPORT
A 67 year-old female patient visited our hospital complaining of fever, chill, and painful swelling of right anterior aspect of neck for seven days. She had been diagnosed as idiopathic liver cirrhosis twenty years ago and also as diabetes mellitus seven years ago. She had also a history of admission to our hospital because of esophageal variceal bleeding and hepatic encephalopathy. She didn't have abdominal pain, vomiting, or diarrhea on admission. General weakness started first, and then fever and intractable chilling followed, the swelling of neck area was getting larger, and more painful. On admission, vital sign was stable. Body temperature was 36.7℃, and then arose to 39℃ with severe chills. On physical examination, her right anterior aspect of neck was severely swollen, of which the size was 5 cm by 5 cm, with tenderness, and local heat, and the overlying skin appeared normal. Laboratory findings revealed white cell count of 8.2×109/L with 86% neutrophils, 6.0% lymphocytes; hemoglobin 10.1 g/dL, hematocrit 28.8%, platelet count 61×109/L. Routine laboratory chemistry revealed blood urea nitrogen 37.1 mg/dL, creatinine 1.41 mg/dL, aspartate aminotransferse 19 U/L, alanine aminotransferase 7 U/L, total bilirubin 1.17 mg/dL, sodium 123 mmol/L, potassium 5.77 mmol/L, glucose 732 mg/dL, HbA1C 10.1%, and C-reactive protein 19.9 mg/dL. Abscess was seen confined to neck area on ultrasonography (Fig. 1A) and Neck CT (Fig. 1B). After ultrasonography-guided aspiration of abscess, intravenous ampicilin-sulbactam was started. Abdominal CT showed normal gallbladder, and analysis and culture of ascites were unremarkable. No organism was grown from blood culture. We couldn't obtain stool specimen for culture and did not perform proctosigmoidoscopy or colonoscopy. Under local anesthesia I & D was done to drain pus. We let the incision site open for further drainage, and then fever disappeared. Salmonella serotype D was isolated from abscess culture, therefore, ampicillin-sulbactam, to which the organism is susceptible, was continued for total 14 days. Swelling of neck improved, and follow-up CT after 2 weeks revealed the abscess with remarkably reduced size. Incision site on anterior neck healed without surgical closure, she was discharged on oral ciprofloxacin uneventfully.
Fig. 1.
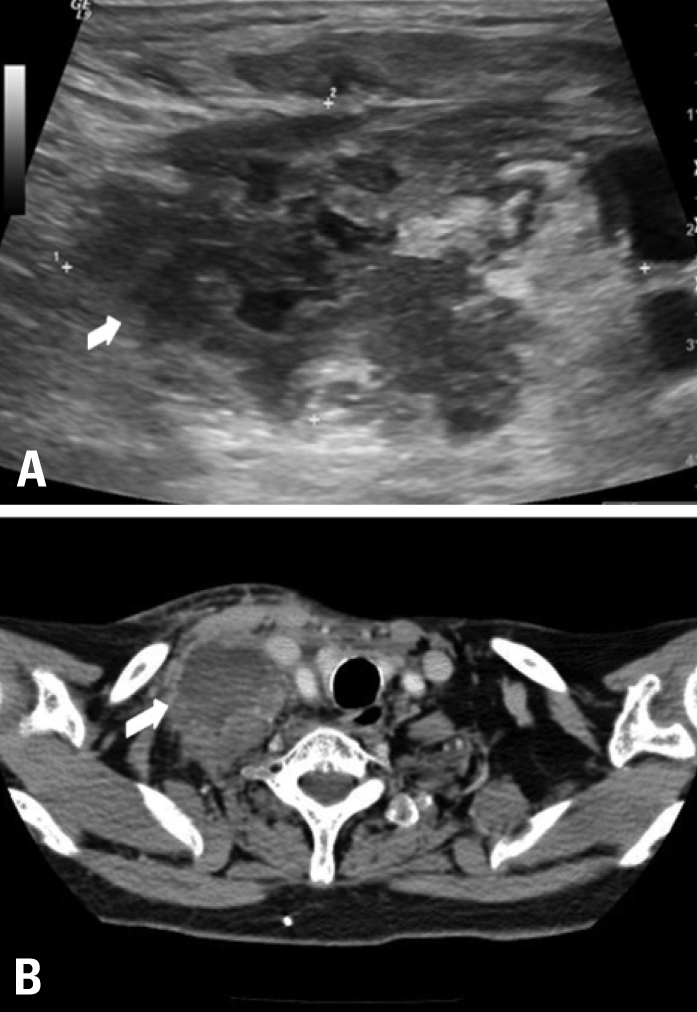
Ultrasonographic and CT findings of neck abscess. Ultrasonography (A) and CT (B) showed 4.5 cm×4.5 cm sized heterogenous mass (arrow).
DISCUSSION
Salmonella infection is mediated mainly through fecal-oral route, and as hygiene improves, typhoidal Salmonella infection emerges less frequently in developing and developed countries, whereas infection by non-typhoidal Salmonella is increasing nowadays throughout the world. Non-typhoidal infections are mainly intraabdominal infections such as enteritis, liver abscess, splenic abscess and cholecystitis,1 and less than one percent of infections are known extraintestinal. Extraintestinal infections are composed of urinary tract infection, pneumonia, infection of central nervous system, bone and soft tissue. These infections are thought to result from bacteraemia with or without symptoms followed by primary gastrointestinal infection. Our patient had no history of abdominal pain, diarrhea or constipation, and no open trauma that allow direct inoculation of the bacteria. However, the majority of Salmonella infection originate from gastrointestinal focus, and some of them are asymptomatic and don't present with diarrhea. In the present case, we did not have definite evidence such as positive stool culture, however, we thought that gastrointestinal focus would be most likely. Other rare extraintestinal locations are thyroid gland, brain, cervical spinal, or epidural space.2-7
Head and neck infections normally arise mainly from Streptococcus, Staphylococcus, Haemophilus, or other anaerobic species, and infection by Salmonella is rare.8 As far as we are aware of, there have been about 10 cases of neck abscess with soft tissue involvement by Salmonella reported worldwide in the last 10 years. In most cases, patients had concomitant diabetes mellitus, and surgical drainage as well as intravenous or oral antibiotics therapy was required.1,8-14
Conditions associated with higher risk of infection are gastrectomy, achlorhydria, antacid medicine use, impaired bowel motility, which allows the bacterial entry and survival more easily, haemolytic anaemia, and immunocompromise, such as patients with diabetes mellitus, connective tissue disorders or use of immnossuppressive agents for many different diseases.15 On the other hand, only a few cases of immunocompetent patients with Salmonella infection have been reported.16 Uncontrolled diabetes and liver cirrhosis can contribute to compromise of humoral- and cell-mediated immunity for Salmonella clearance, and these might act as risk factors for the present patient. To our best knowledge, there are about 5 cases of Salmonella neck abscess in cirrhotic patients reported.
Conventional treatment of Salmonella abscess includes surgical drainage of abscess and appropriate antibiotics for a minimum of 3 weeks.17
In summary, we described a case of neck abscess caused by Salmonella serotype D in a patient with liver cirrhosis, and treated with surgical drainage and antibiotics. She completely recovered uneventfully without sequelae. Neck abscess by Salmonella is a rare disease, but an important differential diagnosis of neck abscess in patients with risk factors makes it possible to be successfully treated with surgical drainage and antibiotics therapy.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Bahar G, Dansuk Z, Kocatürk S, Cakir T, Mert A. Abscess of the neck caused by Salmonella enteritidis. Otolaryngol Head Neck Surg. 2003;129:445–447. doi: 10.1016/S0194-59980300627-2. [DOI] [PubMed] [Google Scholar]
- 2.Dunn DW, McAllister J, Craft JC. Brain abscess and empyema caused by Salmonella. Pediatr Infect Dis. 1984;3:54–57. doi: 10.1097/00006454-198401000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Gudipati S, Westblom TU. Salmonellosis initially seen as a thyroid abscess. Head Neck. 1991;13:153–155. doi: 10.1002/hed.2880130212. [DOI] [PubMed] [Google Scholar]
- 4.Kinsella TR, Yogev R, Shulman ST, Gilmore R, Chadwick EG. Treatment of Salmonella meningitis and brain abscess with the new cephalosporins: two case reports and a review of the literature. Pediatr Infect Dis J. 1987;6:476–480. doi: 10.1097/00006454-198705000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Miller AS, Hunstad DA. Salmonella ovarian abscess in an adolescent. Pediatr Infect Dis J. 2007;26:548–549. doi: 10.1097/INF.0b013e31804b21b2. [DOI] [PubMed] [Google Scholar]
- 6.Moss SD, McLone DG, Arditi M, Yogev R. Pediatric cerebral abscess. Pediatr Neurosci. 1988;14:291–296. doi: 10.1159/000120407. [DOI] [PubMed] [Google Scholar]
- 7.Thomas IL. Salmonella ovarian abscess. Aust N Z J Obstet Gynaecol. 1989;29:272–274. doi: 10.1111/j.1479-828x.1989.tb01740.x. [DOI] [PubMed] [Google Scholar]
- 8.Luo CW, Liu CJ. Neck abscess and necrotizing fasciitis caused by Salmonella infection: a report of 2 cases. J Oral Maxillofac Surg. 2007;65:1032–1034. doi: 10.1016/j.joms.2005.11.052. [DOI] [PubMed] [Google Scholar]
- 9.Cutchavaree A. Salmonella neck abscess. J Med Assoc Thai. 2002;85:388–391. [PubMed] [Google Scholar]
- 10.Lin CH, Chou JC, Lin TL, Lou PJ. Spontaneous resolution of internal jugular vein thrombosis in a Salmonella neck abscess patient. J Laryngol Otol. 1999;113:1122–1124. doi: 10.1017/s0022215100158086. [DOI] [PubMed] [Google Scholar]
- 11.Ray J, Shotton JC, Lobo VJ. A rare case of Salmonella neck abscess. J Laryngol Otol. 1997;111:489–490. doi: 10.1017/s0022215100137727. [DOI] [PubMed] [Google Scholar]
- 12.Vajo Z, Szekacs B, Hitre E, Jakab Z, Balint K. Supraclavicular abscess caused by Salmonella enteritidis in patient without gastrointestinal symptoms. Wien Klin Wochenschr. 1998;110:802–803. [PubMed] [Google Scholar]
- 13.Westblom TU, Gudipati S. Salmonella neck abscesses. Clin Infect Dis. 1997;25:1256–1257. doi: 10.1086/516967. [DOI] [PubMed] [Google Scholar]
- 14.Yamagata K, Takeda M, Onizawa K, Yoshida H. Submandibular abscess caused by Salmonella. Int J Oral Maxillofac Surg. 2006;35:969–971. doi: 10.1016/j.ijom.2006.03.028. [DOI] [PubMed] [Google Scholar]
- 15.Minohara Y, Kato T, Chiba M, Doi K, Kurihara Y, Kusakado M, et al. A rare case of Salmonella soft-tissue abscess. J Infect Chemother. 2002;8:185–186. doi: 10.1007/s101560200033. [DOI] [PubMed] [Google Scholar]
- 16.Galanakis E, Bitsori M, Maraki S, Giannakopoulou C, Samonis G, Tselentis Y. Invasive non-typhoidal salmonellosis in immunocompetent infants and children. Int J Infect Dis. 2007;11:36–39. doi: 10.1016/j.ijid.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 17.Yoshikawa TT, Herbert P, Oill PA. Salmonellosis. West J Med. 1980;133:408–417. [PMC free article] [PubMed] [Google Scholar]


