Abstract
Maternal depression has been linked to deficits in parenting that contribute to youth’s development of externalizing and/or internalizing problems. Maternal sensitivity has been implicated within the infant literature as a foundational aspect of parenting contributing to a child’s adjustment. This study examines the main and moderating effects of a construct labeled maternal sensitivity, within the context of depressive symptoms, on youth externalizing and internalizing problems in a sample of 65 mothers with a history of depression and their 84 children ages 9–15 years. Sensitivity was related to child externalizing problems. Although two-way interactions were not significant, exploratory moderation analyses indicated a significant three-way interaction among maternal depressive symptoms, maternal sensitivity, and youth gender for internalizing problems: among girls only, high depressive symptoms, low sensitivity, and the combination of these two variables were each associated with high levels of internalizing problems.
Keywords: maternal sensitivity, maternal depressive symptoms, child externalizing problems, child internalizing problems
Affecting nearly 20% of Americans, major depressive disorder (MDD) is a leading cause of disability in the nation (Kessler et al., 2003). Unfortunately, this staggering statistic only partially portrays the adverse affects of depression in our society, as the consequences of the disorder reach beyond the impact on the individual. Specifically, children with a depressed parent are four times more likely to develop depression (Beardslee, Versage, & Gladstone, 1998), and two to five times more likely to have an externalizing disorder, than children without a depressed parent (Cummings, Davies, & Campbell, 2000). Because of the increased rates of adverse outcomes for children of depressed parents, researchers have begun to focus on the roles of variables that may protect or exacerbate children’s psychosocial adjustment in these families (Goodman & Tully, 2006).
Parenting is one variable that has received substantial attention. A meta-analysis of 46 observational studies by Lovejoy, Graczyk, O’Hare, and Neuman (2000) identified three parenting behaviors affected by depression: negative/coercive behaviors, engagement, and positive behaviors. These behaviors, in turn, have been shown to relate to externalizing problems (for reviews, see McMahon, Wells, & Kotler, 2006; McKee, Colletti, Rakow, Jones, & Forehand, 2008a) and, to a lesser extent, internalizing problems (McKee et al., 2008b).
Although there is support in the literature for a link between specific parenting behaviors and both child internalizing and externalizing problems, meta-analytic reviews have suggested that this role may be minimal. McLeod and colleagues found that parenting only accounted for a small percent of the variance in childhood depression (8%; McLeod, Weisz, & Wood, 2007a) and anxiety (4%; McLeod, Wood, & Weisz, 2007b). Similarly, Rothbaum and Weisz (1994) earlier found that parenting accounted for only 6% of the variance in childhood externalizing disorders. Although McLeod et al. (2007a, 2007b) concluded that variables other than parenting should be considered when attempting to identify causes of these disorders, an equally plausible interpretation is that parenting variables other than those traditionally studied and included in the meta-analytic reviews may be important in examining the association between parenting and child externalizing and internalizing problem behaviors.
One avenue for identifying parenting variables that are important for child outcomes may be to examine potential underlying or foundational parenting behaviors that underlie more specific parenting behaviors. That is, if there is a core parenting construct which forms the foundation for the development of specific parenting skills, this construct may provide a greater understanding of the role of parenting in child externalizing and internalizing problems than would specific parenting skills. As an example of such an approach, Dishion and McMahon (1998) proposed that the parent-adolescent relationship formed the foundation for more specific parenting skills such as monitoring. Similar to their approach, we draw from the infancy literature, where a core parenting construct referred to as “maternal sensitivity” has been identified as important to infant development. (McElwain & Booth-LaForce, 2006).
Maternal sensitivity has been defined as the ability to recognize and respond both effectively and promptly to the distress and needs of one’s child (Ainsworth, Blehar, Waters, & Wall, 1978). During infancy, maternal sensitivity is positively associated with secure attachment which, in turn, predicts both socioemotional and behavioral outcomes during childhood and adolescence (e.g., Bakermans-Kranenburg, van IJzendoorn, & Juffer, 2003; Teti & Candelaria, 2002). Furthermore, maternal insensitivity (i.e., negative or mismatched affect, intrusiveness, distraction) has been shown to predict infant withdrawal and disorganized attachment (Crockenberg, Leerkes, & Lekka, 2007; Moran, Forbes, Evans, Tarabulsy, & Madigan, 2008). Thus, this parenting construct is considered one of the most crucial aspects of mother-infant interaction during the first few years of life (De Wolff & van IJendoorn, 1997; Moran et al., 2008). Although the study of maternal sensitivity has been limited to its role in infancy and early childhood, there is reason to suggest that it also plays a role in later developmental periods of childhood and adolescence, particularly those that are stressful (Eisenberg et al., 2008). Maternal sensitivity may be especially important during the transition to and through early adolescence due to the developmental demands that characterize this period.
As adolescents strive for independence, parents often have difficulty allowing them to make decisions and seek new experiences (Forehand & Wierson, 1993). Unless parents respond sensitively to the developing adolescent’s need for independence and skillfully negotiate these changes in the parent-child relationship, conflict is likely to increase, particularly in families experiencing a high level of stress (e.g., parental depressive symptoms, marital conflict; Eisenberg et al., 2008; Wierson & Forehand, 1992). Sensitivity may be a foundational construct that allows parents to maintain their relationship with their adolescent during these often conflict-filled and turbulent years.
Whereas the maternal sensitivity construct is well-supported within the infant literature, it remains relatively understudied among school-age and adolescent populations. In contrast, more specific parenting skills, such as praise, structure, and monitoring, have received a great deal of attention in empirical studies (See McMahon et al., 2006, for a review). This emphasis on more specific parenting behaviors overlooks foundational aspects of the parent-child relationship such as sensitivity. Following the pathway model from sensitivity to attachment to emotional and behavioral adjustment illustrated in the infant literature, sensitivity may set the stage for other positive parenting behaviors in a similar fashion as Dishion and McMahon’s (1998) conceptualization of parent-adolescent relationships as a basis for more specific behaviors. Considering sensitivity from this perspective requires examining the construct as an aspect of parenting that is central to child development.
An emerging body of literature, largely based on longitudinal data collected as part of the NICHD Study of Early Child Care, examines the relation between sensitivity and externalizing and internalizing problem behaviors in children beyond infancy through the fifth grade. This study defined sensitivity by aggregating across individually observed behavioral codes collected during parent-child interactions. In infancy, these codes were “sensitivity to nondistress, positive regard, and intrusiveness (reversed).” The codes used in fifth grade were “three conceptually similar but more age-appropriate” constructs (i.e., supportive presence, respect for autonomy, and hostility (reversed) (p. 1300). Maternal sensitivity, measured as an average of sensitivity scores assessed when children ranged in age from 6 to 84 months, contributed unique variance to child externalizing, but not internalizing, problems when children were 6 years old (Campbell, Matestic, Stauffenberg, Mohan, & Kirchner, 2007). Furthermore, maternal sensitivity assessed at these early ages continued to predict externalizing problems when the children were in the fifth grade (Bradley & Corwyn, 2007).
Parenting variables may not only relate to problem behaviors of late childhood and adolescence but may serve an important protective role for children living in families with a parent with a history of depression (e.g., Brennan, Le Brocque, & Hammen, 2003). In the one study examining sensitivity as a moderator of parental depression group status (i.e., chronic, sometimes, or never depressed), the NICHD Early Child Care Research Network (NICHD ECCRN, 1999) found that high levels of this parenting construct protected children from a parent’s depression for two (i.e., more cooperative behavior, higher expressive language scores on the Reynell Developmental Language Scale) of six outcomes. This finding suggests partial support for maternal sensitivity as a buffer for children from the deleterious effects of maternal depression.
The purpose of the current study was twofold. First, the role of maternal sensitivity in the internalizing and externalizing problems of 9- to 15-year-old preadolescent children of mothers with a history of depression was examined. Maternal sensitivity was defined by an aggregation of behaviors similar to Campbell et al. (2007). It was hypothesized that as maternal sensitivity increased, both internalizing and externalizing problems would decrease. Second, the role of maternal sensitivity as a moderator of the link between maternal depressive symptoms and child internalizing and externalizing problems was examined. Prior research suggests that at preadolescent ages, maternal sensitivity can serve as a protective factor (i.e., moderator) in the association between maternal depressive symptoms and child problem behaviors (NICHD ECCRN, 1999). Thus, we expected that, at higher levels of depressive symptoms, higher levels of sensitivity, relative to lower levels, would be associated with lower levels of internalizing and externalizing problem behaviors.
Finally, we examined the role of adolescent gender in the above hypothesized associations. Specifically, we examined whether gender qualifies any of our findings. For example, maternal sensitivity may relate to adolescent problem behaviors only for boys or may moderate the relation of depressive symptoms to problem behaviors only for girls. Substantial evidence suggests that boys and girls may have different risk and protective factors for externalizing and internalizing problems (see Crick & Zahn-Waxler, 2003); nevertheless, as maternal sensitivity has not been considered in the context of gender of the child, we viewed these analyses as exploratory and, as a consequence, do not offer specific hypotheses.
The current study examines current maternal depressive symptoms in a sample of mothers with a history of clinical depression. Such a sample provides the opportunity for a higher level of depressive symptoms than would be found in a community sample and thus a more sensitive assessment of the relation between this variable and child outcomes. The current study also extends the study of a construct labeled as maternal sensitivity to children aged 9–15, permitting the collection of child reports of both internalizing and externalizing symptoms. In contrast, in previous research with younger children, only parents could serve as reporters of child outcomes (e.g., NICHD ECCRN, 1999). As some research suggests that preteens and adolescents are better reporters of internalizing problems than parents (Hope et al., 1999), use of child reports may improve the measurement of this outcome. As a consequence, and in contrast to prior research (Bradley & Corwyn, 2007; Campbell et al., 2007), maternal sensitivity may emerge as an important variable not only for child externalizing, but also internalizing, problems.
Consistent with previous research, the current study used observational data to measure the maternal sensitivity construct. However, unlike previous research using observations of positive play interactions (Bradley & Corwyn, 2007; Campbell et al., 2007; NICHD ECCRN, 1999), the current study used observations of parent-child interactions in a stressful context. Such a context is one in which maternal sensitivity should be particularly critical for negotiating interactions with a child in the early adolescent years.
Method
Participants
Data were gathered during the baseline assessment of a cognitive-behavioral intervention designed to prevent mental health problems among youth in families where at least one parent has a history of MDD or Dysthymia. A total of 65 families from Burlington, Vermont and Nashville, Tennessee were included in the current study. In each family, the mother had a history of MDD or Dysthymia during the lifetime of the oldest participating child. Participating children ranged in age from 9 years, 0 months to 15 years, 11 months. All children in the family between the ages 9 and 15 were included in the project, resulting in 84 mother-child dyads.
An initial sample of 68 mothers with 88 children had been recruited and had parent-child interactional data coded at the time of the current study. However, because of missing data on independent or dependent variables of interest, 3 families (4 children) were excluded, resulting in the final sample of 65 families with 84 children (51% male). Demographic information is presented in Table 1. Only families in which mothers (not fathers) had a history of depression were included in the study, as previous research has focused exclusively on the link between maternal sensitivity and child outcome (e.g., Crockenberg et al., 2007; Moran et al., 2008). This initially resulted in the exclusion of nine families in which the fathers had a history of depression.
Table 1.
Demographic Variables
| Variable | Mean | Standard Deviation | Percentage |
|---|---|---|---|
| Parent agea | 40.68 | 7.23 | |
| Parent race | 25 | ||
| Racial minority | |||
| Racial majority | 75 | ||
| Parent lives with a partner in the home | |||
| Yes | 59.5 | ||
| No | 40.5 | ||
| Parent education | |||
| Less than high school | 11.9 | ||
| High school graduate | 7.1 | ||
| Some college | 32.1 | ||
| College degree | 27.4 | ||
| Graduate education | 21.4 | ||
| Income | |||
| Under $5,000 | 7.1 | ||
| $5,000–$ 9,999 | 8.3 | ||
| $10,000–14,999 | 1.2 | ||
| $15,000–$24,999 | 11.9 | ||
| $25,000–$39,999 | 20.2 | ||
| $40,000–$59,999 | 15.5 | ||
| $60,000–$89,999 | 17.9 | ||
| $90,000–$179,999 | 15.5 | ||
| Over $180,000 | 2.4 | ||
| Child ageb | 11.36 | 1.96 | |
| Child gender | |||
| Male | 51.2 | ||
| Female | 48.8 | ||
| Child race | |||
| Racial minority | 29.8 | ||
| Racial majority | 70.2 |
Range = 26–69.
Range = 9–15.
Inclusion and Exclusion Criteria
Because of the goals of the intervention project, exclusionary criteria for the parents included a current Global Assessment of Functioning Score (GAF; American Psychiatric Association, 2000) of ≤50, lifetime Bipolar-I Disorder, or lifetime Schizophrenia as assessed by the Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P; First, Spitzer, Gibbon, & Williams, 2001). Exclusionary criteria were used to ensure that parents could actively participate in the assessment and family-based intervention. Parents who were currently depressed with high functional impairment (i.e., GAF Scores ≤50) were reasoned to lack the emotional resources to actively participate. However, all currently depressed or dysthymic parents with GAF Scores of 51 or higher were included in the study.
Exclusionary criteria for children included Current MDD, Current Conduct Disorder, Lifetime Bipolar-I Disorder, Lifetime Schizophrenia, Lifetime Autism/Aspergers, or Current Substance Abuse/Dependence as assessed by the Kiddie-Schedule for Affective Disorders and Schizophrenia for School Aged Children, Present and Lifetime Version (K-SADS-PL; Kaufman et al., 1997). Because the affiliated randomized control trial focused on the prevention of child depression and other forms of psychopathology, it was essential that children not meet DSM-IV criteria for depression or dysthymia upon entering the study. Despite the above exclusionary criteria, preliminary data from the Youth Self Report (YSR; Achenbach & Rescorla, 2001) indicated sufficient variability around an overall elevated raw score in the current sample (Externalizing problems M = 10.38, SD = 7.63, Internalizing problems M = 14.48; SD = 9.05) to detect significant relations among the variables of interest.
Procedure
Participants were recruited through a variety of community sources in both the Burlington, Vermont and the Nashville, Tennessee areas, including referrals from mental health agencies, doctors’ offices, and hospitals; advertisements in local newspapers, on television, and on the radio; and flyers posted throughout the community. All parents interested in participating underwent an initial screening in the form of a diagnostic telephone interview. After meeting initial eligibility criteria as determined by the phone screen, parents and their child/adolescent were invited to come to a local university where they provided consent and/or assent and participated in a baseline assessment. During this assessment, experienced interviewers administered the SCID-I/P to the parent (First et al., 2001) and the K-SADS-PL (Kaufman et al., 1997) separately to the child/adolescent and parent to determine final eligibility. Children/adolescents completed on-line or paper versions of questionnaire measures, including the YSR; parents also completed on-line or paper versions of questionnaires, including the BDI-II.
After completion of interview and questionnaire-based data collection, mothers and children participated in two 15-minute videotaped interactions conducted in a private, confidential laboratory space. During the first interaction, the mother-child dyad discussed a pleasant activity they recently did together. As described above, the second interaction focused on a time when the parent felt down, irritable, depressed, or grouchy and made things stressful for the family. For the purposes of this study, sensitivity was only examined during the second, stressful interaction. After the interactions were completed, the research assistant returned, turned off the camera, and debriefed the participants. The research assistant discussed any concerns with the family until the family felt prepared to leave.
In families with more than one child in the 9- to -15-year-old age range, baseline procedures were repeated for each child. Families were compensated for their participation in the baseline phase of the study (US$40 for each participating child and US$40 per child for the target parent).
Measures
Eligibility Criteria
The SCID-I/P (First et al., 2001) was used to screen parents for a history of MDE during the target child’s lifetime and for the exclusionary criteria described above. Adequate reliability and validity have been established for each of the DSM-IV diagnoses of interest (e.g., Skre, Onstad, Torgersen, & Kringlen, 1991; Zanarini et al., 2000).
The K-SADS-PL (Kaufman et al., 1997) was used to determine eligibility of children. Child and parent report of children’s symptom counts for Current Depression, Bi-polar I Disorder, Schizophrenia, Current Substance Abuse, and Current and Lifetime Conduct Disorder were collected. The higher score from the two reporters was used for the purpose of generating diagnoses. Adequate reliability and convergent and discriminant validity have been established for the K-SADS-PL (Kaufman et al., 1997).
Interviewers
Interviewers administering the SCID-I/P (First et al., 2001) and K-SADS-PL (Kaufman et al., 1997) had bachelor or masters degrees, typically in psychology. They initially underwent approximately 25 hours of training. Training included the following steps: (a) a detailed overview of each instrument followed by practice with a previously trained and reliable interviewer, (b) listening to and scoring of a previously administered interview, (c) resolution of any discrepancies from the original scoring of that interview by a master trainer, (d) a reliability check out interview with a community parent and/or child, (e) resolution of discrepancies in the scoring of that check out interview through discussion between the interviewer and master trainer, and (f) mandatory interviewer refresher meetings to prevent interviewer drift.
Reliability checks, conducted in approximately 20% of the interviews resulted in adequate interviewer agreement. For example, for each of the SCID-I/P diagnostic categories of interest, the percent agreement was .90 or higher (100% in 55% of the categories). The kappa coefficient was above .60 (reflecting substantial agreement, Landis & Koch, 1977) for all primary categories of interest.
Parent Depressive Symptoms
Parental depressive symptoms were measured by parent report on the Beck Depression Inventory, 2nd Edition (BDI-II; Beck, Steer, & Brown, 1996). The BDI-II is a 21-item, self-report inventory that assesses the presence and severity of current depressive symptoms in adults. Each item consists of four statements describing varying degrees of symptom severity, which correspond to ratings from 0 to 3, with 0 indicating an absence of that particular symptom and 3 indicating the most severe level of that symptom. Ratings from the 21 items are summed to calculate a total score ranging from 0 to 63; higher scores indicate more severe current depressive symptomatology. The BDI-II has been shown to have excellent internal consistency (α = 92) and to correlate highly with other measures of depression (r = .93; Beck, Steer, Ball, & Ranieri, 1996). The alpha coefficient for the current sample was .89.
Maternal Sensitivity
Direct observations of parent-child interactions were used in the present study as a means to sample maternal sensitivity in the stressful context that characterizes families struggling with depression. The Iowa Family Interaction Rating Scales (IFIRS; Melby & Conger, 2001), a global behavioral coding system, was used to code videotaped 15-minute conversations occurring in the laboratory between the mothers and each of their participating children. Each parent-child dyad was instructed to discuss a recent time when the mother’s sad, down, or grouchy mood made it difficult for the parent and child to get along. IFIRS is a global coding system designed to measure behavioral and emotional characteristics at both the individual and dyadic level. The validity of the IFIRS system has been well established using correlational and confirmatory factor analyses (Kashy & Kenny, 1990).
The maternal sensitivity score was created by a composite of the following observational codes from the IFIRS: maternal communication, child-centered interactions, positive reinforcement, and listener responsiveness (Melby & Conger, 2001). Similar to the procedure used in the NICHD ECCRN (1999) study, these codes were selected based on their conceptual similarity to behaviors used in the infant literature but adapted for age-appropriateness. In addition, significant correlations between each of these codes ranged from .80 to .86, p < .05, suggesting they were measuring one construct. Definitions for these codes are as follows: (a) communication measures the extent to which the parent uses explanations, clarification, and reasoning in communication and the level of solicitation of the other’s views; (b) child centered interactions measures the extent to which the mother is aware of the child’s needs, moods, interests, and capabilities; (c) positive reinforcement assesses the degree to which the parent uses praise, approval, rewards, privileges, and smiles during the interaction, contingent on the child’s behavior; and (d) listener responsiveness is defined as the extent to which the listener attends to, shows interest in, and validates the other’s verbalizations (Melby & Conger, 2001). Behaviors being used to measure maternal sensitivity in the current study are similar to those typically used to assess sensitivity with children beyond infancy (e.g., ages 3–12; Kertz, Smith, Chapman, & Woodruff-Borden, 2008).
IFIRS codes are structured to weigh the affect, intensity, frequency, duration, and proportion of behaviors when determining a rating. Trained coders rate each of the above items on a scale ranging from 1 (no evidence of the behavior) to 9 (high frequency of the behavior). As specified by the IFIRS coding manual, each interaction was viewed a total of five times: once to garner an overall sense of the interaction and two additional times per focal (i.e., parent and child). Each tape was scored by two independent coders. For any code in which the two raters were off by one point, the higher of the two scores was used as the consensus code; however, for any code in which the two raters’ scores were two points or more apart, the raters met to establish a consensus score. Consensus codes were used as the measure of sensitivity in the present study; however, individual codes were used to establish interrater reliability. For the current study, interrater reliability was calculated by dividing the number of items rated the same by both coders by the total number of items. This procedure yielded an interrater reliability of 71% for the four behaviors coded.
Coders
Training for coding the IFIRS consisted of in-depth studying of the manual and a written test of the scale definitions and coding conventions. Successful completion of training consisted of passing the written test with at least 90% correct and achieving at least 80% reliability on observational tests. Raters remained blind to the diagnostic status of the mother and independently coded the interactions. Weekly training meetings were held to prevent coder drift and to provide a forum in which questions about the different codes could be addressed. Coders met to establish consensus on any discrepant codes (i.e., a difference in the score of two or more).
Child Externalizing and Internalizing Problems
Children completed the Youth Self Report (YSR; Achenbach & Rescorla, 2001) as an assessment of their behavioral and emotional problems over the last 6 months. Each item is rated using the following scale: 0 = not true, 1 = somewhat or sometimes true, or 2 = very or often true. The YSR yields two broad-based factors, Internalizing and Externalizing Problems, both of which were used in this study. Because children in the current sample ranged in age from 9 to 15, raw scores were used in all analyses in the current study as T-scores are not available for children younger than 11. The internal consistency for these younger children (n = 46) was adequate for internalizing (α = .90) and externalizing (α = .88) problems.
The Achenbach System of Empirically Based Assessment, which includes the YSR, has strong test-retest reliability (r = .79–.95). Criterion-related validity has also been established (Achenbach & Rescorla, 2001). The alpha coefficients for the current sample were .89 and .88 for internalizing and externalizing problems, respectively.
Overview of Analyses
Because multiple children from the same family were included in the data analyses, weighted correlations were used in the preliminary analyses. Primarily analyses consisted of two-level Linear Mixed Models (LMM) analyses in SPSS examining the relations between mother-reported depressive symptoms, maternal sensitivity, and youth externalizing and internalizing problems. LMM accounts for the shared variance associated with data reported on multiple children from the same family by estimating the parameters of the statistical model on two levels: Level 1 represents observations at the individual level (i.e., child report of externalizing and internalizing problems); Level 2 denotes clusters of units within the data set that maintain a constant relationship across all children within the same family (i.e., maternal depressive symptoms and maternal sensitivity). In the case of the current two-level clustered data set, LMM assumes a compound symmetry covariance structure and nests children from the same family into a single cluster. In the models tested, the fixed effects are the regression coefficients that describe the relations between each independent and dependent variable, whereas the random effects are associated with the number of children per family. Thus, in the current study, LMM controlled for the variability in the dependent variable associated with the inclusion of multiple children per family (West, Welch, & Galecki, 2008).
Results
Preliminary Analyses
Mother-child dyads were excluded if there was missing data on one or more of the outcome variables of interest (n = 4). Parents and children with complete data were compared to those with missing data. Although the sample size for those with missing data was too small for statistical analysis to be conducted, demographic, independent, and dependent variables were similar for the two groups.
With exception of family income, no demographic data were missing. The mean for the demographic variable income was substituted in four cases where families were missing data. The relation between each demographic variable and externalizing problems, internalizing problems, and sensitivity was calculated. Analysis of variance was used for dichotomous demographic variables and correlations were used for continuous demographic variables. Significant between-group differences for parent race, which was dichotomized as racial minority (score of 0) and racial majority (score of 1), emerged for sensitivity, F(1, 83) = 12.47, p < .01, externalizing problems, F(1, 83) = 5.81, p < .05, and internalizing problems, F(1, 83) = 7.73, p < .01. Parent education and income were related to sensitivity, r = .32, p < .01; r = .40, p < .01, respectively. Significant between-group differences emerged for child gender (boys = score of 1; girls = score of 2) for externalizing problems, F(1, 83) = 5.32, p < .05. Significant differences for child race (racial minority = score of 0; racial majority = score of 1) emerged for internalizing problems, F(1, 83) = 11.93, p < .01. Maternal age was also related to internalizing problems r =−.26, p < .05. These variables were controlled in the primary analyses.
Means and standard deviations of the independent variables (i.e., BDI-II, maternal sensitivity) and the dependent variables (i.e., child reported externalizing symptoms, child reported internalizing symptoms), as well as the correlations among these variables, are presented in Table 2.
Table 2.
Means, Standard Deviations, and Ranges of, as Well as Correlations Between, Maternal Depressive Symptoms, Maternal Sensitivity, Child Reported Externalizing Problems (ext), and Child Reported Internalizing Problems (int)
| Mean | Standard Deviation |
Range | BDI-II | Maternal Sensitivity |
Ext Prob | Int Prob |
|
|---|---|---|---|---|---|---|---|
| Maternal depressive symptomsa |
18.53 | 10.63 | 0–46 | — | −.27* | .07 | .23* |
| Maternal sensitivityb |
23.79 | 5.59 | 11–34 | — | −.29* | −.20 | |
| Externalizing problemsc |
10.38 | 7.63 | 0–27 | — | .69** | ||
| Internalizing problemsd |
14.48 | 9.05 | 0–40 | — |
Beck Depression Inventory-II; possible range of scores 0 to 63.
Possible range of scores 4 to 36.
Youth Self Report; raw scores; possible range of scores: 0–64.
Youth Self Report; raw scores; possible range of scores: 0–62.
p < .05.
p < .01.
Mean scores suggest that maternal depressive symptoms, on average, were elevated and in the high end of the range for mild depression (BDI-II scores of 14–19). Over one-third (36.9%) of mothers scored in the moderate to severe range (BDI-II scores of 20 or greater). Based on the possible range of scores (4–36), mothers exhibited a relatively high level of sensitivity during the negative interaction task. According to children’s T-scores, which were used only for the following comparison to a normative sample, children’s externalizing problems were in the average range; approximately the same percentage of children fell in the clinical range (12%) relative to the normative sample (10%) reported by Achenbach and Rescorla (2001). Children’s internalizing problems, on average, approached the clinical range; approximately 2.5 times as many children fell in the clinical range (25.3%) relative to the normative sample (10%).
Maternal depressive symptoms were negatively correlated with maternal sensitivity, which, in turn, was negatively correlated with externalizing problems. Maternal sensitivity was not significantly correlated with internalizing problems. Maternal depressive symptoms were positively and significantly correlated with internalizing, but not externalizing problems. The association between maternal depressive symptoms and child internalizing problems suggests the importance of examining maternal sensitivity as a protective factor for this type of child problem behavior.
Primary Analyses
Main Effects Analyses
In order to test the hypothesis that higher levels of maternal sensitivity would be associated with lower levels of youth externalizing and internalizing problems, two separate sets of LMM analyses were conducted. In the first set of analyses, youth externalizing symptoms served as the dependent variable while maternal sensitivity served as the independent variable. Demographic control variables (i.e., mother’s race, child’s gender) were entered in Model 1 and maternal sensitivity was added in Model 2. Maternal sensitivity was significantly associated with child report of externalizing symptoms (see Model 2 in Table 3, β = −.22, p < .05) such that higher levels of maternal sensitivity was related to lower levels of externalizing symptoms. In the second set of analyses, child internalizing symptoms served as the dependent variable. Demographic control variables (i.e., mother’s age, mother’s race, child’s race, child’s gender) were entered in Model 1 and maternal sensitivity was entered in Model 2. Maternal sensitivity was not significantly associated with child reported internalizing symptoms (see Model 2 in Table 3).
Table 3.
Main and Interaction Effects of Maternal Sensitivity, Maternal Depressive Symptoms, and Child Gender on Child-Reported Externalizing and Internalizing Problems
| Externalizing Problems | Internalizing Problems | |||||
|---|---|---|---|---|---|---|
| F | β | SE | F | β | SE | |
| Model 1 | ||||||
| Child’s race | 5.22 | .27 | 1.53 | 4.17* | .37 | 3.60 |
| Mother’s race | 6.90 | .26 | 1.71 | .09 | .06 | 0.13 |
| Child’s gender | 1.09 | −.11 | 1.88 | |||
| Mother’s age | 2.57 | −.17 | 0.13 | |||
| Model 2 | ||||||
| Sensitivity | 4.28* | −.22 | 0.14 | 0.93 | −.11 | 0.18 |
| Model 3 | ||||||
| BDI-II | 0.01 | .01 | 0.07 | 0.26 | .06 | 0.10 |
| Sensitivity | 3.95* | −.22 | 0.15 | 0.57 | −.63 | 0.19 |
| Model 4 | ||||||
| BDI-II × Sensitivity | 1.16 | .09 | 0.01 | 2.07 | .15 | 0.02 |
| Child gender × BDI-II | 0.59 | .08 | 0.16 | 0.35 | .06 | 0.19 |
| Child gender × Sensitivity | 0.41 | .01 | 0.30 | 0.17 | .05 | 0.37 |
| Model 5 | ||||||
| Child Gender × Sensitivity × BDI-II | 3.79 | .22 | 0.03 | 7.67** | 0.34 | 0.03 |
Note: N = 84; BDI-II: Beck Depression Inventory-II measuring maternal depressive symptoms.
p ≤ .05.
p ≤.01.
Moderational Analyses
In order to test the hypothesis that maternal sensitivity would moderate the relation between maternal depressive symptoms and youth externalizing and internalizing problems, additional models were added to the linear mixed models analyses presented in Table 3. First, all relevant variables (i.e., all demographic control variables, maternal depressive symptoms, maternal sensitivity, and child gender) were centered. Next, for both externalizing and internalizing problems, maternal depressive symptoms were added in Model 3, and three two-way interactions, maternal sensitivity by maternal depressive symptoms, child gender by maternal sensitivity, and child gender by maternal depressive symptoms, were added in Model 4.
Sensitivity maintained a significant relationship with youth externalizing problems (see Model 3 in Table 3) when maternal depressive symptoms were added in Model 3. However, the maternal depressive symptoms by maternal sensitivity interaction was not significant in Model 4. (Note: In order to examine the maternal depressive symptoms by maternal sensitivity interaction for externalizing and internalizing problems without other two-way interactions in the model, the regression analysis was repeated without the gender by sensitivity and gender by depressive symptoms interaction terms in the model. Nonsignificant findings still emerged for externalizing (β = .09) and internalizing (β = .22) problems.
Maternal sensitivity continued to have a nonsignificant relation with internalizing problems when maternal depressive symptoms were added in Model 3 (see Table 3). In Model 4, the maternal depressive symptoms by maternal sensitivity interaction was not significant.
The Qualifying Role of Child Gender
In order to examine if child gender qualified the relations of maternal sensitivity and maternal depressive symptoms to the child outcomes examined, Models 4 in Table 3 can be examined. The child’s gender did not interact significantly with either of these variables for externalizing or internalizing problems. To examine if child gender qualified the interaction between maternal depressive symptoms and maternal sensitivity, a three-way interaction, child gender by maternal depressive symptoms by maternal sensitivity, was added in Model 5. The three-way interaction was not significant for externalizing problems (see Model 5 in Table 3, β = .22) but was significant for internalizing problems (see Model 5, Table 3, β = .34, p < .01).
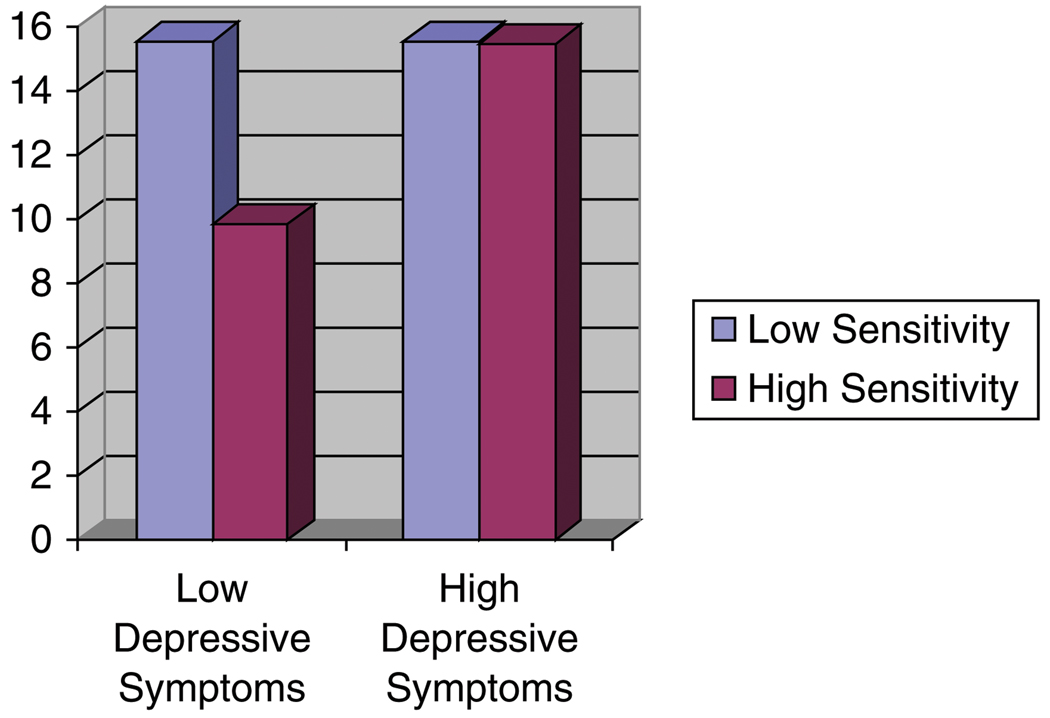
In order to explicate the significant three-way interaction for internalizing problems, separate LMM analyses were conducted for girls and boys. The main effect of sensitivity and the two-way interaction of maternal depressive symptoms by maternal sensitivity were of interest. Main effects were not significant for either sex. However, for girls (β = .40, p < .01), but not boys (β = −.16), the interaction was significant. To further explain the interaction, data for girls only was divided into four groups by median splits: high depressive symptoms, high sensitivity (n = 11); low depressive symptoms, high sensitivity (n = 14); high depressive symptoms, low sensitivity (n = 7); and low depressive symptoms, low sensitivity (n = 9). Means were calculated for each group. Results indicate that the combination of low levels of maternal depressive symptoms and high levels of maternal sensitivity was associated with lower levels of internalizing problems than any of the three remaining combinations, which were similar to each other (see Figure 1).
Figure 1.
Interaction of Maternal Depressive Symptoms and Maternal Sensitivity Predicting Girls’ Internalizing Problems
Discussion
The primary purpose of this study was to examine the relation of a construct labeled maternal sensitivity to child externalizing and internalizing symptoms. First, we examined maternal sensitivity as a main effect; that is, does maternal sensitivity relate to each type of child problem behavior? Next, we examined the role of maternal sensitivity as a moderator of the relation between maternal depressive symptoms and child externalizing and internalizing symptoms. Finally, we examined the role of child gender in qualifying the relations among the variables of interest.
Results indicate that maternal sensitivity acted as a main effect for externalizing symptoms. Our results are consistent with previous literature indicating a negative relation between maternal sensitivity and externalizing problems in children ranging in age from 6 months to 7 years of age and again in fifth grade (e.g., Bradley & Corwyn, 2007; Campbell et al., 2007). The current study extends the research literature to 9- to 15-year-olds. Furthermore, these results stress the importance of sensitive parenting for children entering into and progressing through middle adolescence. The preadolescent and adolescent years are ones in which the impact of parents has been substantially debated (e.g., Arnett, 1999; Laible, 2007). Our findings are compatible with the conclusions reached by Arnett (1999): Parents maintain an important role in the lives of their children during the adolescent years. Within a family context of a history of maternal depression, being sensitive and responsive to youth who are transitioning into and through adolescence is associated with fewer externalizing problems.
In contrast to the main effect found between maternal sensitivity and child externalizing symptoms, maternal sensitivity was not significantly related to child internalizing symptoms. This finding replicates research on maternal sensitivity with younger children (Bradley & Corwyn, 2007). However, a significant correlation between maternal depressive symptoms and child internalizing problems suggested the importance of identifying protective factors, such as parenting, which may moderate this association. When moderational analyses were conducted, a significant maternal sensitivity by depressive symptoms interaction emerged, but only for girls: the presence of low levels of sensitivity, high levels of maternal depressive symptoms, or both was associated with elevated child internalizing problems relative to the combination of high levels of maternal sensitivity and low levels of maternal depressive symptoms. These findings suggest that either insensitive parenting or depressive symptoms may serve as stressors for girls, at least when considering the development of internalizing problems. Previous research (e.g., Davies & Windle, 1997; Thomas & Forehand, 1991; see also Goodman & Tully, 2006) suggests that girls may be particularly vulnerable to interpersonal and family stressors including negative parenting and parental psychopathology (e.g., depressive symptoms). Our findings are consistent with the findings from these earlier studies.
The finding that maternal insensitivity, either alone or in conjunction with maternal depressive symptoms, was associated with higher levels of child internalizing problems in girls is inconsistent with the direction of the moderational hypothesis proposed: maternal sensitivity would buffer adolescents from higher levels of maternal depressive symptoms. The current findings suggest that maternal insensitivity may best be conceptualized as a stressor similar to maternal depressive symptoms. Furthermore, maternal sensitivity appears to be a stressor similar in effect to, but not exacerbated by, maternal depressive symptoms (i.e., individually and in combination, the two stressors are associated with similar elevation in internalizing problems).
There are several limitations to the current study. First, as previously mentioned, the sample size was relatively small, particularly for examining three-way interactions, and the exclusion criteria for included parents and children can be viewed as limitations. Furthermore, the data are cross-sectional, preventing causal conclusions from being reached and failing to consider the possibility that problem behaviors may contribute to less sensitivity parenting. In addition, although there was no significant correlation between age of the child and either internalizing or externalizing problems, the wide age range of the current sample (i.e., 9–17 years) may be a limitation. Maternal sensitivity may relate to internalizing and externalizing problems differently in the preadolescent and adolescent years. Finally, although this study used similar methods as previous research (e.g., NICHD ECCRN, 1999) to operationally define sensitivity, it may be difficult to distinguish the construct from general positivity. Regardless of the label applied to the construct, the findings suggest the importance of the four aggregated behaviors coded in the parent-child interaction for child problem behavior. The study additionally has a major strength: the use of multiple reporters, including mother report of depressive symptoms, child report of externalizing and internalizing symptoms, and an observational measure of maternal sensitivity, prevents common-reporter bias.
Our findings have a number of implications. First, this study partially replicates the results of the NICHD ECCRN study, thereby providing evidence for the association between sensitivity and externalizing problems across a wide age range and for both boys and girls. Second, the current study suggests that, as children enter into and move through adolescence, gender may be an important variable for consideration when examining family stressors such as maternal insensitivity and depressive symptoms. Within the context of maternal depression, girls, more than boys, may require sensitive parenting from their mothers in order to successfully navigate the early adolescent period.
Third, the findings may have important implications for understanding parenting within the context of parental depression. The current findings suggest that maternal sensitivity continues to play an important role within families affected by maternal depression as children move into adolescence. By extending measurement of specific parenting variables, such as positive reinforcement or parent-child communication, to the broader foundational construct of sensitivity, more key dimensions of parenting during adolescence within these families can be captured. Nevertheless, it is important to note that our analyses do not address whether maternal sensitivity, as defined in this study, is a foundational construct that is more strongly associated with child problems than are individual parenting behaviors. Future research should examine this question.
Current parenting programs that teach specific skills (e.g., positive reinforcement, good communication) have been implemented without a thorough examination and understanding of the context, including maternal depression, within which these skills are utilized. As these specific parenting skills have been found to have arguably weak (McLeod et al., 2007a, 2007b) and nonspecific (McKee et al., 2008a) effects, it may be necessary to consider more foundational aspects of parenting, such as sensitivity, to enhance the effectiveness of intervention. Parents do not use specific skills in a vacuum. Rather, these skills must occur within the context of not only a parent’s depression but also the parent-child relationship. The attention and interest a parent displays toward a child, and the parent’s ability to respond sensitively to his/her child, are skills that enhance the foundation of the parent-child relationship. As has occurred in the infant literature, these contextual skills can be labeled as the foundational construct “sensitivity” (McElwain & Booth-LaForce, 2006). Subsequent research can then dismantle maternal sensitivity and identify the specific aspects of this construct that can be taught to parents.
Acknowledgments
This research was supported by grants R01MH069940 and R01 MHO69928 from the National Institute of Mental Health.
Biographies
Emily Priscilla Garai is a graduate student in Clinical Psychology at the University of Vermont. Her research interests include adolescent psychopathology, generally, and comorbid anxiety, depression, and substance use, specifically.
Rex L. Forehand is University Distinguished Professor and Director of Clinical Psychology at the University of Vermont. His research interests include the role of family factors in children’s psychosocial adjustment and prevention of child psychopathology.
Christina J. M. Colletti is a graduate student in Clinical Psychology at the University of Vermont. Her research interests include the prevention and treatment of child psychopathology.
Kristen Reeslund is a graduate student in Clinical Psychology at Vanderbilt University. Her research interests include the prevention of child psychopathology.
Jennifer Potts is a second year student in the Clinical Psychology Doctoral Program at Vanderbilt University. Her research interests include developmental psychopathology and prevention efforts for children of depressed parents.
Bruce Compas is Patricia and Rodes Hart Professor of Psychology and Human Development, Professor of Pediatrics, and Co-Director of the Clinical Psychology Program at Vanderbilt University. His research interests include the role of coping in the development of child psychopathology.
Contributor Information
Emily Priscilla Garai, University of Vermont.
Rex L. Forehand, University of Vermont
Christina J. M. Colletti, University of Vermont
Kristen Reeslund, Vanderbilt University.
Jennifer Potts, Vanderbilt University.
Bruce Compas, Vanderbilt University.
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA school-age forms & profiles. Burlington: University of Vermont, Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- Ainsworth M, Blechar M, Waters E, Wall S. Patterns of attachment: A psychological study of the strange situation. Hillsdale, NJ: Lawrence Erlbaum; 1978. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed., Text Rev. Washington, DC: Author; 2000. [Google Scholar]
- Arnett JJ. Adolescent storm and stress, reconsidered. American Psychologist. 1999;54:317–326. doi: 10.1037//0003-066x.54.5.317. [DOI] [PubMed] [Google Scholar]
- Bakermans-Kranenburg MJ, van IJzendoorn MH, Juffer F. Less is more: Meta-analyses of sensitivity and attachment interventions in early childhood. Psychological Bulletin. 2003;129:195–215. doi: 10.1037/0033-2909.129.2.195. [DOI] [PubMed] [Google Scholar]
- Beardslee WR, Versage EM, Gladstone TRG. Children of affectively ill parents: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:1134–1141. doi: 10.1097/00004583-199811000-00012. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Ball R, Ranieri WF. Comparison of Beck Depression Inventories-IA and –II in psychiatric outpatients. Journal of Personality Assessment. 1996;67:588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory—Second Edition manual. San Antonio: Psychological Corporation; 1996. [Google Scholar]
- Bradley RH, Corwyn RF. Externalizing problems in fifth grade: Relations with productive activity, maternal sensitivity, and harsh parenting from infancy through middle childhood. Developmental Psychology. 2007;43:1390–1401. doi: 10.1037/0012-1649.43.6.1390. [DOI] [PubMed] [Google Scholar]
- Brennan PA, Le Brocque R, Hammen C. Maternal depression, parent child relationships, and resilient outcomes in adolescence. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42:1469–1477. doi: 10.1097/00004583-200312000-00014. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Matestic P, von Stauffenberg C, Mohan R, Kirchner T. Trajectories of maternal depressive symptoms, maternal sensitivity, and children’s functioning at school entry. Developmental Psychology. 2007;43:1202–1215. doi: 10.1037/0012-1649.43.5.1202. [DOI] [PubMed] [Google Scholar]
- Crick NR, Zahn-Waxler C. The development of psychopathology in females and males: Current progress and future challenges. Development and Psychopathology. 2003;15:719–742. [PubMed] [Google Scholar]
- Crockenberg SC, Leerkes EM, Lekka SK. Pathways from marital aggression to infant emotion regulation: The development of withdrawal in infancy. Infant Behavior and Development. 2007;30:97–113. doi: 10.1016/j.infbeh.2006.11.009. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Davies PT, Campbell SB. Applications of developmental psychopathology: Parental depression, families, and children’s development. In: Cummings EM, Davies PT, Campbell SB, editors. Developmental psychopathology and family process: Theory, research, and clinical implications. New York: Guilford; 2000. pp. 299–340. [Google Scholar]
- Davies PT, Windle M. Gender-specific pathways between maternal depressive symptoms, family discord, and adolescent adjustment. Developmental Psychology. 1997;22:657–668. doi: 10.1037//0012-1649.33.4.657. [DOI] [PubMed] [Google Scholar]
- De Wolff M, van IJendoorn MH. Sensitivity and attachment: A meta analysis on parental antecedents of infant attachment. Child Development. 1997;68:571–591. [PubMed] [Google Scholar]
- Dishion TJ, McMahon RJ. Parental monitoring and the prevention of child and adolescent problem behavior: A conceptual and empirical foundation. Clinical Child and Family Psychology Review. 1998;1:61–75. doi: 10.1023/a:1021800432380. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Hofer C, Spinrad TL, Gershoff ET, Valiente C, Losoya S, et al. Understanding mother-adolescent conflict discussions: Concurrent and across-time prediction from youths’ dispositions and parenting. Monographs of the Society for Research in Child Development. 2008;73 doi: 10.1111/j.1540-5834.2008.00470.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2001. [Google Scholar]
- Forehand R, Wierson M. The role of developmental factors in planning behavioral interventions for children: Disruptive behavior as an example. Behavior Therapy. 1993;24:117–141. [Google Scholar]
- Goodman SH, Tully E. Women and depression: A handbook for the social, behavioral, and biomedical sciences. In: Keyes CLM, Goodman SH, editors. Women and depression: A handbook for the social, behavioral, and biomedical sciences. New York: Cambridge University Press; 2006. pp. 241–280. [Google Scholar]
- Kashy DA, Kenny DA. Analysis of family research designs. Communication Research. 1990;17:462–482. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kertz SJ, Smith CL, Chapman LK, Woodruff-Borden J. Maternal sensitivity and anxiety: Impacts on child outcome. Child and Family Behavior Therapy. 2008;30:153–171. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikanga KR, et al. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R) JAMA: Journal of the American Medical Association. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Laible D. Attachment with parents and peers in late adolescence: Links with emotional competence and social behavior. Personality and Individual Differences. 2007;43:1185–1197. [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- McElwain NL, Booth-LaForce C. Maternal sensitivity to infant distress and nondistress as predictors of infant-mother attachment security. Journal of Family Psychology. 2006;20:247–255. doi: 10.1037/0893-3200.20.2.247. [DOI] [PubMed] [Google Scholar]
- McKee L, Colletti C, Rakow A, Jones DJ, Forehand R. Parenting and child externalizing behaviors: Are the associations specific or diffuse? Aggression and Violent Behavior. 2008a;13:201–215. doi: 10.1016/j.avb.2008.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee L, Forehand R, Rakow A, Reeslund K, Roland E, Hardcastle E, et al. Parenting specificity: An examination of the relation between three parenting behaviors and child problem behaviors in the context of a history of caregiver depression. Behavior Modification. 2008b;32:638–658. doi: 10.1177/0145445508316550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod BD, Weisz JR, Wood JJ. Examining the association between parenting and childhood depression: A meta-analysis. Clinical Psychology Review. 2007a;27:986–1003. doi: 10.1016/j.cpr.2007.03.001. [DOI] [PubMed] [Google Scholar]
- McLeod BD, Wood JJ, Weisz JR. Examining the association between parenting and childhood anxiety: A meta-analysis. Clinical Psychology Review. 2007b;27:155–172. doi: 10.1016/j.cpr.2006.09.002. [DOI] [PubMed] [Google Scholar]
- McMahon RJ, Wells KC, Kotler JS. Conduct Problems. In: Mash EJ, Barkley RA, editors. Treatment of childhood disorders. 3rd ed. New York: Guilford; 2006. pp. 137–268. [Google Scholar]
- Melby JN, Conger RD. The Iowa Family Interaction Rating Scales: Instrument summary. In: Kerig PK, Lindahl KM, editors. Family observational coding systems: Resources for systemic research. Mahwah, NJ: Lawrence Erlbaum; 2001. [Google Scholar]
- Moran G, Forbes L, Evans E, Tarabulsy GM, Madigan S. Both maternal sensitivity and atypical maternal behavior independently predict attachment security and disorganization in adolescent mother-infant relationships. Infant Behavior & Development. 2008;31:321–325. doi: 10.1016/j.infbeh.2007.12.012. [DOI] [PubMed] [Google Scholar]
- NICHD Early Child Care Research Network. Chronicity of maternal depressive symptoms, maternal sensitivity, and child functioning at 36 months. Developmental Psychology. 1999;35:1297–1310. doi: 10.1037//0012-1649.35.5.1297. [DOI] [PubMed] [Google Scholar]
- Rothbaum F, Weisz JR. Parental caregiving and child externalizing behavior in nonclinical samples: A meta-analysis. Psychological Bulletin. 1994;116:55–74. doi: 10.1037/0033-2909.116.1.55. [DOI] [PubMed] [Google Scholar]
- Skre I, Onstad S, Torgersen S, Kringlen E. High interrater reliability for the Structured Clinical Interview for DSM III-R Axis I (SCID-I) Acta Psychiatrica Scandinavica. 1991;84:167–173. doi: 10.1111/j.1600-0447.1991.tb03123.x. [DOI] [PubMed] [Google Scholar]
- Teti DM, Candelaria MA. Parenting competence. In: Barnstein MH, editor. Handbook of parenting: Vol. 4. Social conditions and applied parenting. 2nd ed. Mahwah, NJ: Lawrence Erlbaum; 2002. pp. 149–181. [Google Scholar]
- Thomas AM, Forehand R. The relationship between paternal depressive mood and early adolescent functioning. Journal of Family Psychology. 1991;4:260–271. [Google Scholar]
- West BT, Welch KB, Galecki AT. Linear mixed models: A practical guide using statistical software. Boca Raton, FL: Chapman & Hall/CRC; 2008. [Google Scholar]
- Wierson M, Forehand R. Family stressors and adolescent functioning: A consideration of models for early and middle adolescence. Behavior Therapy. 1992;23:671–688. [Google Scholar]
- Zanarini MC, Skodol AE, Bender D, Dolan R, Charles S, Schaefer E, et al. The collaborative longitudinal personality disorders study: Reliability of Axis I and II diagnoses. Journal of Personality Disorders. 2000;14:291–299. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]