Abstract
It is a case study of a 62-yr-old female with crusted (Norwegian) scabies, which appeared during her treatment with systemic and topical corticosteroid therapy, under the diagnosis of erythroderma. In the same time, the patient had been suffered from hypothyoidism, and her skin changes were misdiagnosed, because it was thought that they are associated with her endocrine disorder. Suddenly, beside the erythema, her skin became hyperkeratotic, with widespread scaling over the trunk and limbs, and crusted lesions appeared on her scalp and ears. The microscopic examination of the skin scales with potassium hydroxide demonstrated numerous scabies mites and eggs. Repeated topical treatments with lindan, benzoyl benzoat and 10% precipitated sulphur ointment led to the complete resolution of her skin condition.
Keywords: Sarcoptes Scabiei, Diagnosis, Therapy
INTRODUCTION
Scabies is common parasitosis of the skin caused by Sarcoptes scabiei var. hominis. The infestation occurs in all geografic areas, all age groups, races and social classes. Poor economical conditions, and lack of proper hygiene are risk factors for the disease (1, 2). Scabies is transmitted by close physical contact. Main symptom is intensive pruritus which worsens in the night or in the conditions where the body temperature is raised. Typical skin lesions are burrows, papules, excoriations and sometimes vesicles.
Crusted scabies is a rare, highly contagious uncommon form of scabies which is characterized by presence of huge number of Sarcoptes scabiei in the horny layer of the epidermis. As a reaction, the horny layer thickens and forms warty crusts (3). In most cases it is associated with some underlying diseases and usually affects immunocompromised patients (4-7). Also, the host response can be modified by immunosuppressive therapy (8, 9).
Topical or systemic use of corticosteroids may mask the clinical picture of scabies and lead to another uncommon presentation-scabies incognito (10, 11), which can easily be mistaken for other skin diseases.
CASE REPORT
The patient is 62-yr-old woman with skin changes which started 3 yr ago with diffuse erythematous, slightly infiltrated plaques on her trunk and extremities, with no clear borders, associated with moderate pruritus. Because she had been suffered from hypothyroidosis for 20 yr, at the first dermatological examination, she was misdiagnosed and her skin changes were thought to be in relation with the endocrine disorder. First, she was treated with topical potent corticosteroids (Betametasone valerate 0.1%, triamcinolone acetonide 0.1%, fluocinonide 0.05%), in 1 to 2 weeks repeated courses, over five months, without effect. In next six months her skin changes became more extensive, erythrodermic with scaling and showed tendency for generalization, and then her diagnosis was erythroderma, also thought to be secondary to her hypothyreoidism. Pruritus was persistently present and intensive. In that time, she began with systemic corticosteroid therapy in medium doses (40 mg/day of prednisone). In first month of therapy her skin changes improved, and erythema and pruritus became less intensive, but every time with reduction of dose of steroids, she had an exacerbacion. Sistemic corticosteroid therapy lasted almost one year with pauses and with doses between 20 and 40 mg of prednisone daily. Biopsy specimens were taken several times, but on microscopic examination there were only signs of nonspecific inflammation. Suddenly, she came to a hospital with widespread skin eruptions which had developed during previous few weeks.
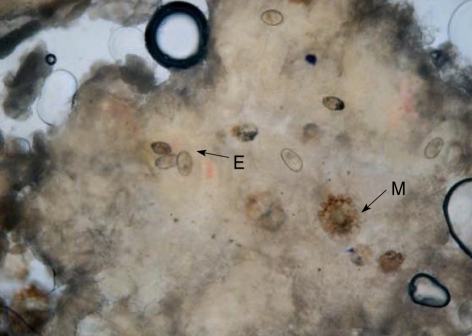
Examination showed generalized erythema and scaling of the whole body and face with large hyperkeratotic plaques on her trunk and limbs and crusted lesions on her scalp and external ears (Fig. 1, 2). Also, she had fever and raised body temperature. Laboratory examination showed an elevated sedimentation rate (46 mm) and leukocgtosis with eosinophilia (1.3×109/L). The haematologic (urea, creatinine, hepatic enzimes, glukose level) and urine analyses were normal. Pruritus was very intensive, so she could not sleep. At this time crusted scabies was suspected and microscopical examination of scrapings from the hyperkeratotic lesions from trunk (we did not examined tips of fingers and toes) showed numerous mites and eggs (Fig. 3). In that time we did not perform biopsy, because we made diagnosis. She was treated first with 1% lindane (one application, left on skin 24 hr) with remarkable improvement. After treatment no live mites were found on microscopic examination, but after three days we repeated antiscabiotic treatment first with 25% benzyl benzoat and then with 10% precipitated sulphur ointment (for three consecutive days). At the follow up controls after one, three and six months she had no signs of skin disease.
Fig. 1.

Hyperkeratotic plaques on trunk and limbs and crusted lesions on her scalp and external ears.
Fig. 2.
Hyperkeratotic plaques on trunk and limbs and crusted lesions on her scalp and external ears (A, B, C, D).
Fig. 3.
Microscopical examination of scrapings from the hyperkeratotic lesions from trunk showed (arrow) mites (M) and eggs (E) (magnification ×40).
Maybe the reason of these serious infection is that patient lives in poor hygiene and socioeconomic conditions, she lives alone,without any human care. We have not data about affected neighbors.
There had been outbreak of scabies among the staff (2 doctors, 5 nurses), and 14 patients who were in clinic in the same time.
DISCUSSION
In the current scabies epidemic, when this infestation could be a global problem, esspecially in the developing countries and when it is estimated that about 300 million people is infested (12), classic and typical clinical pictures of scabies became less frequently seen. On the contrary, specific forms became more common. In the past, crusted scabies was a rare form which was seen mostly in immunocompromised and mentally debilitated patients. With increasing use of different immunosuppressive therapies and increasing number of HIV patients, diagnosis of crusted scabies is not so rare as it was in the past. To date more than 200 cases have been reported (13).
The first patient with crusted scabies was described in 1848, and in 1973 the first case attributable to therapy with immunosuppressive drugs was reported (8). There are reports of crusted scabies after locally applied corticosteroids (14), but it has also been seen in patients with normal immune response (15).
Clinically, crusted scabies is a hyperkeratotic skin disease resembling psoriasis, but variable degree of erythema may be usual and it could generalize to erythroderma (13, 16).
One of the problems of giving correct diagnosis is that among general practitioners it is usually a very low level of suspicion of this disease. The diagnosis of scabies always should be considered in patients with advanced malignancies and associated pruritus. Also, this form of scabies may be a complication of immunosuppressant therapy and it may appear in immunocompromised patients, as in patients with prolonged use of corticosteroids, both topically and systemically, as in our patient.
We think our patient almost certainly had scabies incognito at the first time she visited dermatologist, when she was misdiagnosed as having a skin condition like eczema secondary to her hypothyroidism. It might be that the first clinical appearance of skin changes was uncommon because of her underlying disease. After that, she was treated continuously about two years with corticosteroids, both topically (Betametasone valerate 0.1%, triamcinolone acetonide 0.1%, fluocinonide 0.05%) and systemic (20-40 mg of prednisolone daily) with little improvement, and the pruritus was persistent almost all the time. It is known that locally applied corticosteroids alter the skin immune system, the inflammatory response is reduced and the cellular immune response is suppressed (17). The fact that until then, after antiscabiotic therapy, one year later, she is without skin changes, suggest that she had scabies all along.
In view of its contagious nature physicians should be aware of the possibility of development crusted scabies in a patient who develops widespread hyperkeratotic eruptions. So, we could say that nowadays this diagnosis become challenge for the both general practitioners and dermatologists.
It is very important to make a correct dignosis of crusted scabies, because misdiagnosis could be associated with serious consequences such as spreading of the infestation and superinfection of the lesions (18), inducing sometimes life-threatening consequences.
References
- 1.Landwehr D, Keita SM, Ponnighaus JM, Tounkara C. Epidemiologic aspects of scabies in Mali, Malawi and Cambodia. Int J Dermatol. 1998;37:588–590. doi: 10.1046/j.1365-4362.1998.00367.x. [DOI] [PubMed] [Google Scholar]
- 2.Cox NH, Paterson WD. Epidemiology of scabies: the new epidemic. Lancet. 1991;337:1547–1548. doi: 10.1016/0140-6736(91)93239-6. [DOI] [PubMed] [Google Scholar]
- 3.Burns DA. Diseases caused by arthropods and other noxious animals. In: Champion RH, Burton JL, Burns DA, Breathnach SM, editors. Rook, Wilkinson Textbook of Dermatology. 6th ed. Oxford: Blackwell Science; 1998. pp. 1423–1482. [Google Scholar]
- 4.Portu JJ, Santamaria MJ, Zubero Z, Almeida-Liamas M, Etxebarria San Sebastian MA, Gutierrez AR. Atypical scabies in HIV positive patients. J Am Acad Dermatol. 1996;34:915–917. doi: 10.1016/s0190-9622(96)90079-1. [DOI] [PubMed] [Google Scholar]
- 5.Suzumiya J, Sumiyoshi A, Kuroki Y, Inoue S. Crusted (Norwegian) scabies with adult T-cell leukemia. Arch Dermatol. 1985;121:903–904. [PubMed] [Google Scholar]
- 6.Dourmishev AL, Serafimova KD, Dourmishev AL, Mualla AM, Papaharalambous V, Malchevsky T. Crusted scabies of the scalp in dermatomyositis patients: three cases treated with oral ivermectin. Int J Dermatol. 1998;37:231–234. doi: 10.1046/j.1365-4362.1998.00330.x. [DOI] [PubMed] [Google Scholar]
- 7.Van der Wal VB, Van Voorst Vader PC, Mandema JM, Jonkman MF. Crusted (Norwegian) scabies in a patient with dystrophic epidermolysis bullosa. Br J Dermatol. 1999;141:918–921. doi: 10.1046/j.1365-2133.1999.03170.x. [DOI] [PubMed] [Google Scholar]
- 8.Paterson WD, Allen BR, Beverige GW. Norwegian scabies during immunosuppressive therapy. Br Med J. 1973;4:211–212. doi: 10.1136/bmj.4.5886.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jaramillo-Ayerbe F, Berrio-Munoz J. Ivermectin for crusted Norwegian scabies induced by use of topical steroids. Arch Dermatol. 1998;134:143–145. doi: 10.1001/archderm.134.2.143. [DOI] [PubMed] [Google Scholar]
- 10.Cestarri FT, Martignago FB. Scabies, pediculosis, bedbegs, and stinkbugs: uncommon presentations. Clin Dermatol. 2005;23:545–554. doi: 10.1016/j.clindermatol.2005.01.013. [DOI] [PubMed] [Google Scholar]
- 11.Kim KJ, Roh KH, Choi JH, Sung KJ, Moon KC, Koh JK. Scabies incognito presenting as urticaria pigmentosa in an infant. Pediatr Dermatol. 2002;19:409–411. doi: 10.1046/j.1525-1470.2002.00115.x. [DOI] [PubMed] [Google Scholar]
- 12.Hengge UR, Currie BJ, Jager G, Lupi O, Schwartz RA. Scabies: a ubiquitous neglected skin disease. Lancet Infect Dis. 2006;6:769–779. doi: 10.1016/S1473-3099(06)70654-5. [DOI] [PubMed] [Google Scholar]
- 13.Guldbakke KK, Khachemoune A. Crusted scabies: a clinical review. J Drugs Dermatol. 2006;5:221–227. [PubMed] [Google Scholar]
- 14.Marliere V, Roul S, Labreze C, Taieb A. Crusted (Norwegian) scabies induced by use of topical corticosteroids and treated successfully with ivermectin. J Pediatr. 1999;135:122–124. doi: 10.1016/s0022-3476(99)70342-2. [DOI] [PubMed] [Google Scholar]
- 15.Roberts LJ, Huff am SE, Walton SF, Currie BJ. Crusted scabies: clinical and immunological findings in seventy-eight patients and a review of the literature. J Infect. 2005;50:375–381. doi: 10.1016/j.jinf.2004.08.033. [DOI] [PubMed] [Google Scholar]
- 16.Gladstone HB, Darmstadt GL. Crusted scabies in an immunocompetent child;treatment with ivermectin. Pediatr Dermatol. 2000;17:144–148. doi: 10.1046/j.1525-1470.2000.01736.x. [DOI] [PubMed] [Google Scholar]
- 17.Arya V, Molinaro MJ, Majewski SS, Schwartz R. Pediatric scabies. Cutis. 2003;71:193–196. [PubMed] [Google Scholar]
- 18.Sugimoto T, Kashiwagi A. A case of scabies masquerading as drug eruption. Eur J Intern Med. 2007;18:445–446. doi: 10.1016/j.ejim.2007.04.003. [DOI] [PubMed] [Google Scholar]