Abstract
Many obese people who try to control body weight experience weight cycling (WC). The present study evaluated the importance of WC in a community-based obesity intervention program. We analyzed the data of 109 Korean participants (86% women) among 177 subjects who had completed a 12-week intervention program at two public health centers in Korea from April to December, 2007. Completion of a self-administrated questionnaire at baseline was used to obtain anthropometric measurements, and laboratory testing was done before and after the program. Differences in body composition change and obesity-related life style between the two groups were compared with respect to WC and non-weight cycling (NWC). After 12 weeks, both groups showed reductions in weight, waist circumference, and body mass index. The group differences were not significant. However, significant differences were evident for the WC group compared to the NWC group in fat percent mass (WC vs. NWC, -3.49±2.31% vs. -4.65±2.59%, P=0.01), fat free mass (WC vs. NWC, -0.95±1.37 kg vs. -0.38±1.05 kg, P=0.01), and total cholesterol (WC vs. NWC, -3.32±14.63 vs. -16.54±32.39, P=0.005). In conducting a community-based weight control program that predominantly targets women, changes of body composition and total cholesterol may be less effective in weight cyclers than in non-weight cyclers.
Keywords: Obesity, Community, Public Health Center, Weight Cycling
INTRODUCTION
According to the 2006 Korea National Health & Nutrition Examination Survey Report, the prevalence of obesity in Korea-defined as a body mass index (BMI) over 25.0-is increasing, with 31.7% of adults over 20 yr being considered obese (1). In addition, as ongoing research has established that obesity is harmful to the body (2-5) and mental health (6-8), and increases the mortality rate related to various diseases (9-11), medical interest in obesity is intense. Furthermore, with increased attention given to beauty and body shape regardless of age and gender, weight control is emerging as a social issue as well as being a health problem (12, 13). For these reasons, many people are currently attempting weight control for health or aesthetic reasons. Attempts at weight control can have ensuing adverse effects that include weight cycling (WC) (14). Although WC does not have clear defining criteria, it refers to the phenomenon where body weight reduction occurs after weight control with subsequent rapid restoration to the initial weight or even more. It is frequently observed among obese subjects who attempt rapid weight control. While WC is widely known among obese subjects, there has been not enough research on the difference after body weight intervention between those who experience WC and those who do not (non-weight cycling, NWC). Therefore, we conducted a preliminary 8-month-long community-based obesity control program at two public health centers that are financially supported by Korea's Gyeonggi Provincial Office, and evaluated the effect and importance of the weight cycling in a 12-week community-based obesity intervention program.
MATERIALS AND METHODS
Subjects
A total of 515 obese subjects enrolled and underwent the 12-week 'Slim Gyeonggi Project' conducted from April to December, 2007 at two public health centers in Gyeonggi Province, Republic of Korea. Participants visited the public health centers weekly or biweekly, and proper obesity programs were administered. They received a program concerning behavior modification, nutrition, and exercise by trained nurses, nutritionists, and exercise trainers at the public health centers. Of the 515 participants, 177 completed the program. We analyzed the data of 109 of these participants who completed a self-administrated questionnaire before and after the 12-week program. The Institutional Review Board of Ajou University Hospital in Suwon City, Republic of Korea, approved this study.
Measurements
Anthropometry, height (cm), and weight (0.1 kg units) measurements were taken while each participant was lightly clothed. BMI was calculated with measured height and weight (kg/m2). Waist circumference was measured at the central part between the twelfth rib and iliac crest by skilled nurses. Body composition analysis was carried out using new In body 7.0 octapolar bioimpedance spectroscopy analyzers (Biospace, Seoul, Korea) (15). Fasting blood sugar, total cholesterol, and triglyceride measurements were recorded using a TBA-200FR apparatus (Toshiba, Tokyo, Japan) at the beginning and end of the 12-week program. Blood pressure of each participant was measured in a sitting position by trained nurses at least 4 min after completion of exercise, beginning at week one of the program and every four weeks thereafter. Regular exercise, alcohol consumption (current, past, non-drinking), tobacco use (current, past, non-smoking), number of breakfasts per week, snack consumption frequency per week, and stress were evaluated through the self-questionnaire.
Study design
Trained nurses collected self-administrated questionnaires that were completed by participants at initial interview. In this process, trained nurses did not know who were in the WC and NWC groups. This study was designed by the principal investigator after the 12-week program was complete, which could eliminate potential blinding in subject selection and measurement. The subjects went through 12 weeks of weekly training and evaluation based on the Protein-Rich Oriental (PRO) Diet Program, a modified protein-enriched diet program that encourages the consumption of low-saturated fat, high protein oriental type foods (such as legumes, soybean curd, soy milk, mushrooms, nuts, seafood, fish, chicken breast, and lean meat) and vegetables, while avoiding foods that contain simple sugars, refined starches, and high saturated fats. In addition, guidance was provided to increase the amount of activity in daily life and approachable type, method, time, and intensity of exercise. At least 40 min of aerobic exercise was done more than 4 days a week and resistance exercise (strength training) was done twice a week. In addition, short message services (SMS, text messaging) delivered twice a week and an Internet-based service (www.prodiet.co.kr) additionally provided information on nutrition, exercise, and behavior modification. WC was defined as a body weight change exceeding 5% of the initial body weight within the previous two years (16).
Statistical analysis
Baseline differences (anthropometric measurements and laboratory tests) and changes of body composition after 12 weeks were compared between the WC and NWC groups using independent t test and ANCOVA after age-adjustment. All significant values were defined by P<0.05 as determined by SPSS version 11.5 (SPSS, Chicago, IL, USA).
RESULTS
Baseline characteristics
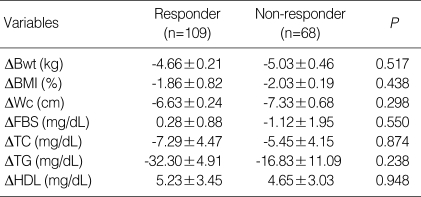
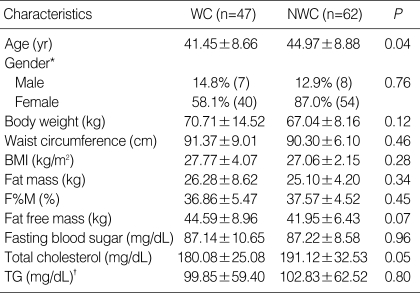
Of the 515 people who initially entered the 12-week obesity control program, 177 subjects (Per Protocol, PP group) who completed the program were selected for study. Of these, 109 participants completed the questionnaire before and upon completion of the program. No significant differences were evident between those who completed the questionnaires (responders) and those who did not (non-responders) in terms of body weight change, BMI, waist circumference, fasting blood sugar, total cholesterol, triglyceride level, and high-density lipoprotein (Table 1). Based on the baseline analysis, the 109 participants were divided into the WC group (n=47) and the NWC group (n=62). The WC group consisted of seven males (14.8%) and 40 females (58%) with a mean age of 41.4 yr and mean BMI of 27.7 kg/m2. The NWC group was comprised of eight males (12.9%) and 54 females (87.0%), with an average age of 44.9 yr, which was significantly older than the WC group (P=0.04). However, no significant difference was observed between the two groups in weight, waist, BMI, body composition analysis and blood test results (with the exception of total cholesterol) (Table 2).
Table 1.
Comparison of weight change between WC and NWC groups after the 12-week obesity control program
All data represents mean±standard error.
P values were from independent t test.
Responder, subjects who filled up self-administrated questionnaire for weight cycling; Non-responder, subjects who did not fill up self-administrated questionnaire for weight cycling; Δ, mean changes after 12 weeks; Bwt, body weight; BMI, body mass index; Wc, waist circumference; FBS, Fasting blood sugar; TC, Total cholesterol; TG, Triglyceride; HDL, High-density lipoprotein cholesterol.
Table 2.
Baseline characteristics between WC and NWC participants
All data represents mean±standard deviation.
*were from χ2 test; †mean±standard error.
P values were from independent t test.
WC, weight cycler; NWC, non-weight cycler; BMI, body mass index; TG, triglyceride; F%M, fat % mass.
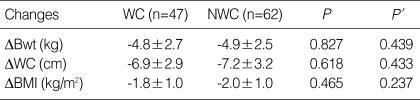
Changes of anthropometry and laboratory test results after 12 weeks of intervention
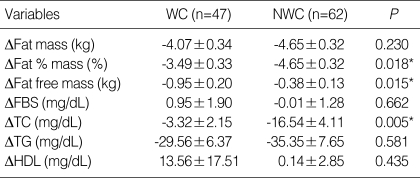
After the 12-week program, weight, waist circumference, BMI, body composition analysis, and blood testing were performed in both groups and the results were compared with the baseline data gathered at the beginning of week one. Both groups showed a decrease in weight, waist circumference, and BMI (Table 3). In the WC group, the respective changes averaged -4.8 kg, -6.9 cm and -1.8 kg/m2, while larger decreases (-4.9 kg, -7.2 cm and -2.0 kg/m2, respectively) were evident in the NWC group. These decreases were not statistically significant (Table 3). Concerning body composition changes, the WC group displayed decreases of body fat mass, body fat percentage, and fat-free mass of -4.07 kg, -3.49%, and -0.95 kg, respectively, while the NWC group displayed respective decreases of -4.65 kg, -4.65%, and -0.38 kg (Table 4). The difference between reductions in body fat percentage (P=0.018) and fat-free mass (P=0.015) was statistically significant, before and after age adjustment. Laboratory analyses revealed a mean change in fasting blood sugar in the WC and NWC groups of 0.95 mg/dL and -0.01 mg/dL, respectively; the difference was statistically insignificant. Furthermore, the mean change of triglycerides was -29.5 mg/dL for the WC group and -35.3 mg/dL for the NWC group, which were not statistically significant. The mean change in total cholesterol was -3.3 mg/dL for the WC group and -16.5 mg/dL for NWC group, which represented a significant difference (P=0.005), before and after age adjustment.
Table 3.
Comparison of weight change between WC and the NWC participants after the 12-week obesity control program
All data represents mean±standard deviation
P values were from independent t test, P' values were from general linear model after age, fat free mass adjustment, presence of regular menstruation, female hormone use, and removal of uterus surgically.
WC, weight cycler; NWC, non-weight cycler; Δ, mean changes after 12 weeks; Bwt, body weight; BMI, body mass index.
Table 4.
Comparison of body composition and laboratory changes between the WC and NWC participants after the 12-week obesity control program
All data represents mean±standard error.
P values were from independent t test.
Values marked* were also from ANCOVA test with age-adjustment.
FBS, fasting blood sugar; TC, total cholesterol; TG, triglyceride; HDL, high-density lipoprotein cholesterol.
DISCUSSION
Obesity is drawing a great deal of attention not only for the health of individuals but also for that of families, societies, and even whole nations. Many obese people experience WC when attempting weight control with various methods. Recent studies have indicated that repeated WC is related to an escalation of weight gain and frequency of overeating (17), and that WC related excess weight gain is predictable in men and women who have previous experience of weight loss (18). People with excessive changes in body weight show an even greater increase in body weight during the follow-up period than those whose weight has not cycled (19). Also, women who have experienced WC tend to display abdominal obesity rather than typical lower body obesity, putting them at increased risk of adult diseases such as metabolic syndrome (20). Many obesity patients who experience WC also struggle with eating disorders such as overeating and can experience diminished mental health (8, 21). WC has also been related with increased mortality of all reasons (22, 23), although other studies have not reported mortality rate influences (24-27) and no harm to the health of young, healthy women (28).
In this study, mean changes of body weight, waist circumference, and BMI in all subjects showed significant reductions after 12 weeks of the weight control program. However, the WC group experienced less reduction of body fat percentage with more reduction in fat-free mass compared to the NWC group. This may suggest that body fat utilization decreases and more muscle wasting can occur in those who experience WC, even though in the present case the same weight control program was applied to the both groups. Therefore, it is conceivable that weight cyclers have a lower basal metabolic rate, which makes it difficult to control long term stable body weight, thereby provoking weight regain and even recurrent WC (29, 30). In this study, we used new octapolar bioimpedance spectroscopy analyzers, which represent a simple and relatively accurate method to evaluate body composition in a community-based situation. Although bioimpedance analysis was comparable with dual energy radiography absorptiometry, it is not yet a standard method to evaluate body composition, which could affect the values of measurements. In our study, fat-free mass and fat percent mass showed statistically significant differences between the two groups, however, these differences might be in the range of error of measurement. Nevertheless, because the reproducibility of this analyzer has been approved by the Korea Food & Drug Administration (KFDA), we should scrutinize these differences carefully.
Although statistically not significant, the WC group had small changes of body weight, waist circumference, BMI, and body fat mass compared to the NWC group. Concerning laboratory results, the WC group showed less reduction of total cholesterol than the NWC group. The cholesterol level, however, was different at the beginning of the study in the two groups, making it difficult to confirm this statistical difference. Even though statistically insignificant, a lesser reduction of triglycerides was evident in the WC group, showing that improvement of blood lipid levels was also less in the WC group as compared to the NWC group. In our study, those who were obese and exhibited WC also displayed a higher prevalence of alcohol use and reported more environmental stress than obese NWC participants (data not shown). This suggests that WC could be related to a detrimental life style including overuse of alcohol as a means of coping with environmental stress.
The present study has several limitations. The 109 subjects (47 WC and 62 NWC) is a small number. Especially, data were analyzed with no consideration of gender, because few males took part. We did not adjust the data for menopausal status, although most subjects were women, but we failed to discern any differences in the results after adjustment for regular menstruation, female hormone usage, and surgical uterus removal, which could minimize the bias of menopause. Another limitation is that selected subjects were the Per Protocol (PP) group with self-administrated questionnaire, which might introduce bias. However, except for age, initial body weight and numbers of female were not different between the ITT (Intention To Treat) group and the PP group (data not shown). We surmise that the reason why the younger subjects had more WC events is that they tried weight control more often than older subjects. The mean age of subjects in the present study was 41 yr for the WC group and 44 yr for the NWC group; further studies will help clarify the relationship between WC and obesity in younger or older age groups. Since this study targeted residents from only two cities within Gyeonggi-do, there might have been some errors due to different individual environments such as socio-economic status. In addition, as the WC experience of subjects was classified in a self-administrated questionnaire, informational bias is a possibility. Besides WC, we gathered data on exercise, cigarette smoking, alcohol consumption, presence of stress, and snack food consumption. Among these variables, alcohol consumption and presence of stress were significantly different in the two groups. However, the data was not quantitative.
In conclusion, the present study conducted with Korean participants (mainly women) has found a lower reduction of body fat percentage and total cholesterol, and greater reduction of fat-free mass in weight cyclers who attempted weight control. Therefore, when conducting an obesity control program, special attention should be given to weight control that does not involve WC.
References
- 1.Korean Ministry of Health and Welfare. Report on National Health and Nutrition Survey 2005. Seoul: Korean Ministry of Health and Welfare; 2006. [Google Scholar]
- 2.Thompson D, Edelsberg J, Colditz GA, Bird AP, Oster G. Lifetime health and economic consequences of obesity. Arch Intern Med. 1999;159:2177–2183. doi: 10.1001/archinte.159.18.2177. [DOI] [PubMed] [Google Scholar]
- 3.National Task Force on the Prevention and Treatment of Obesity. Overweight, obesity, and health Risk. Arch Intern Med. 2000;160:898–904. doi: 10.1001/archinte.160.7.898. [DOI] [PubMed] [Google Scholar]
- 4.Pischon N, Heng N, Bernimoulin JP, Kleber BM, Willich SN, Pischon T. Obesity, inflammation, and periodontal disease. J Dent Res. 2007;86:400–409. doi: 10.1177/154405910708600503. [DOI] [PubMed] [Google Scholar]
- 5.Dunai A, Mucsi I, Juhász J, Novák M. Obstructive sleep apnea and cardiovascular disease. Orv Hetil. 2006;147:2303–2311. [PubMed] [Google Scholar]
- 6.Hach I, Ruhl UE, Klose M, Klotsche J, Kirch W, Jacobi F. Obesity and the risk for mental disorders in a representative German adult sample. Eur J Public Health. 2007;17:297–305. doi: 10.1093/eurpub/ckl227. [DOI] [PubMed] [Google Scholar]
- 7.Wyshak G. Weight change, obesity, mental health, and health perception: self-reports of college-educated women. Prim Care Companion J Clin Psychiatry. 2007;9:48–54. doi: 10.4088/pcc.v09n0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Petroni ML, Villanova N, Avagnina S, Fusco MA, Fatati G, Compare A, Marchesini G QUOVADIS Study Group. Psychological distress in morbid obesity in relation to weight history. Obes Surg. 2007;17:391–399. doi: 10.1007/s11695-007-9069-3. [DOI] [PubMed] [Google Scholar]
- 9.Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R, Hollenbenk A, Leitzmann MF. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355:763–778. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- 10.Gu D, He J, Duan X, Reynolds K, Wu X, Chen J, Huang G, Chen CS, Whelton PK. Body weight and mortality among men and women in China. JAMA. 2006;295:776–783. doi: 10.1001/jama.295.7.776. [DOI] [PubMed] [Google Scholar]
- 11.Corrada MM, Kawas CH, Mozaffar F, Paganini-Hill A. Association of body mass index and weight change with all-cause mortality in the elderly. Am J Epidemiol. 2006;163:938–949. doi: 10.1093/aje/kwj114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perman JA, Young TL, Stines E, Hamon J, Turner LM, Rowe MG. A community-driven obesity prevention and intervention in an elementary school. J Ky Med Assoc. 2008;106:104–108. [PubMed] [Google Scholar]
- 13.Roux L, Kuntz KM, Donaldson C, Goldie SJ. Economic evaluation of weight loss interventions in overweight and obese women. Obesity. 2006;14:1093–1106. doi: 10.1038/oby.2006.125. [DOI] [PubMed] [Google Scholar]
- 14.Lee JS, Kawakubo K, Kobayashi Y, Mori K, Kashihara H, Tamura M. Effects of ten year body weight variability on cardiovascular risk factors in Japanese middle-aged men and women. Int J Obes Relat Metab Disord. 2001;25:1063–1067. doi: 10.1038/sj.ijo.0801633. [DOI] [PubMed] [Google Scholar]
- 15.Gibson AL, Holmes JC, Desautels RL, Edmonds LB, Nuudi L. Ability of new octapolar bioimpedance spectroscopy analyzers to predict 4-component-model percentage body fat in Hispanic, black, and white adults. Am J Clin Nutr. 2008;87:332–338. doi: 10.1093/ajcn/87.2.332. [DOI] [PubMed] [Google Scholar]
- 16.Benini ZL, Camilloni MA, Scordato C, Lezzi G, Oriani G, Bertoli S, Balzola F, Liuzzi A, Petroni ML. Contribution of weight cycling to serum leptin in human obesity. Int J Obes Relat Metab Disord. 2001;25:721–726. doi: 10.1038/sj.ijo.0801587. [DOI] [PubMed] [Google Scholar]
- 17.Field AE, Manson JE, Taylor CB, Willett WC, Colditz GA. Association of weight change, weight control practices, and weight cycling among women in the Nurses' Health Study II. Int J Obes Relat Metab Disord. 2004;28:1134–1142. doi: 10.1038/sj.ijo.0802728. [DOI] [PubMed] [Google Scholar]
- 18.Kroke A, Liese AD, Schulz M, Bergmann MM, Klipstein-Grobusch K, Hoffmann K, Boeing H. Recent weight changes and weight cycling as predictors of subsequent two year weight change in a middle-aged cohort. Int J Obes Relat Metab Disord. 2002;26:403–409. doi: 10.1038/sj.ijo.0801920. [DOI] [PubMed] [Google Scholar]
- 19.Field AE, Byers T, Hunter DJ, Laird NM, Manson JE, Williamson DF, Colditz GA. Weight cycling, weight gain, and risk of hypertension in women. Am J Epidemiol. 1999;150:573–579. doi: 10.1093/oxfordjournals.aje.a010055. [DOI] [PubMed] [Google Scholar]
- 20.Wallner SJ, Luschnigg N, Schnedl WJ, Lahousen T, Sudi K, Crailsheim K, Möller R, Tafeit E, Horejsi R. Body fat distribution of overweight females with a history of weight cycling. Int J Obes Relat Metab Disord. 2004;28:1143–1148. doi: 10.1038/sj.ijo.0802736. [DOI] [PubMed] [Google Scholar]
- 21.Marchesini G, Cuzzolaro M, Mannucci E, Dalle Grave R, Gennaro M, Tomasi F, Barantani EG, Melchionda N QUOVADIS Study Group. Weight cycling in treatment-seeking obese persons: data from the QUOVADIS study. Int J Obes Relat Metab Disord. 2004;28:1456–1462. doi: 10.1038/sj.ijo.0802741. [DOI] [PubMed] [Google Scholar]
- 22.Lissner L, Odell PM, D'Agostino RB, Stokes J, 3rd, Kreger BE, Belanger AJ, Brownell KD. Variability of body weight and health outcomes in the Framingham population. N Engl J Med. 1991;324:1839–1844. doi: 10.1056/NEJM199106273242602. [DOI] [PubMed] [Google Scholar]
- 23.Blair SN, Shaten J, Brownell K, Collins G, Lissner L. Body weight change, all-cause mortality, and cause-specific mortality in the Multiple Risk Factor Intervention Trial. Ann Intern Med. 1993;119:749–757. doi: 10.7326/0003-4819-119-7_part_2-199310011-00024. [DOI] [PubMed] [Google Scholar]
- 24.Rzehak P, Meisinger C, Woelke G, Brasche S, Strube G, Heinrich J. Weight change, weight cycling and mortality in the ERFORT Male Cohort Study. Eur J Epidemiol. 2007;22:665–673. doi: 10.1007/s10654-007-9167-5. [DOI] [PubMed] [Google Scholar]
- 25.Sullivan DH, Liu L, Roberson PK, Bopp MM, Rees JC. Body weight change and mortality in a cohort of elderly patients recently discharged from the hospital. J Am Geriatr Soc. 2004;52:1696–1701. doi: 10.1111/j.1532-5415.2004.52463.x. [DOI] [PubMed] [Google Scholar]
- 26.Wannamethee SG, Shaper AG, Walker M. Weight change, weight fluctuation, and mortality. Arch Intern Med. 2002;162:2575–2580. doi: 10.1001/archinte.162.22.2575. [DOI] [PubMed] [Google Scholar]
- 27.Gregg EW, Gerzoff RB, Thompson TJ, Williamson DF. Intentional weight loss and death in overweight and obese U.S. adults 35 years of age and older. Ann Intern Med. 2003;138:383–389. doi: 10.7326/0003-4819-138-5-200303040-00007. [DOI] [PubMed] [Google Scholar]
- 28.Rebuffe-Serive M, Hendler R, Bracero N, Cummunings N, McCarthy S, Rodin J. Biobehavioral effects of weight cycling. Int J Obes Relat Metab disord. 1994;18:651–658. [PubMed] [Google Scholar]
- 29.Richelsen B, Vrang N. Why is weight loss so often followed by weight regain? Basal biological response as a possible explanation. Ugeskr Laeger. 2006;168:159–163. [PubMed] [Google Scholar]
- 30.Horswill CA. Weight loss and weight cycling in amateur wrestlers: implications for performance and resting metabolic rate. Int J Sport Nutr. 1993;3:245–260. doi: 10.1123/ijsn.3.3.245. [DOI] [PubMed] [Google Scholar]