Abstract
Aims: The aims of this study were (1) to examine the association between neighborhood alcohol outlet density and individual self-reported alcohol-related health outcomes in the last year—sexually transmitted infections (STI), motor vehicle accidents, injury, liver problems, hypertension and experienced violence; (2) to determine whether the relationship between morbidity and alcohol outlet density is mediated by individual alcohol consumption; and (3) to explore the role of alcohol outlet density in explaining any observed racial and ethnic differences in morbidity. Method: Hierarchical models from a random sample of Los Angeles, CA, and Louisiana residents (N = 2881) from 217 census tracts were utilized. The clustering of health and social outcomes according to neighborhood varied by health problem examined. Results: There was substantial clustering of STI (intraclass correlation coefficient, ICC = 12.8%) and experienced violence (ICC = 13.0%); moderate clustering of liver problems (ICC = 3.5%) and hypertension (ICC = 3.9%); and low clustering of motor vehicle accident (ICC = 1.2%) and injury (ICC = 1.4%). Alcohol outlet density was significantly and positively associated with STI (crude OR = 1.80, 95% CI = 1.10–3.00), liver problems (crude OR = 1.33, 95% CI = 1.02–1.75) and experienced violence (crude OR = 1.31, 95% CI = 1.13–1.51) although not with other morbidity outcomes. Mediation analyses of morbidity outcomes revealed partial mediation of individual alcohol consumption in the relationship between alcohol density and STI and violence, and full mediation for liver problems. Conclusions: Findings support the concept that off-premise alcohol outlets in the neighborhood environment may impact health and social outcomes, either directly or indirectly, through individual alcohol consumption and these associations may be heterogeneous with respect to race and ethnicity.
INTRODUCTION
In ecologic studies at the neighborhood level, alcohol outlet density has been shown to be strongly associated with both alcohol consumption (Gruenewald et al., 1993; Scribner et al., 2000; Gruenewald et al., 2002) and numerous alcohol-related outcomes including fatal and injury traffic crashes (Scribner et al., 1994), drunk driving offenses (Mackinnon et al., 1995; Treno et al., 1996; Gruenewald et al., 2000), cirrhosis mortality (Gruenewald and Ponicki, 1995, Mackinnon et al., 1995), assaultive violence (Scribner et al., 1995, 1999; Gorman et al., 2001), sexually transmitted diseases (Scribner et al., 1998; Cohen et al., 2006) and liquor law violations (Mackinnon et al., 1995). Over the past decade there has been a recognition that the strongest effects emerge at the smaller units of aggregation, i.e. census tracts and blocks groups, often used as units that approximate neighborhoods (Scribner et al., 1999; Gorman et al., 2001).
Multilevel studies have confirmed that the effect of alcohol outlets on health outcomes is independent of individual-level risk factors (Scribner et al., 2000). Despite evidence for a contextual effect at the neighborhood level, the mechanisms of the association between alcohol outlets and health outcomes have not been carefully studied. Various theoretical explanations have been offered, however, including social contextual models, niche theory and assortative drinking (Gruenewald, 2007), the impact of outlets on neighborhood social networks and social capital (Scribner et al., 2007, Theall et al., in press), as well as the role of increased alcohol consumption and its effect on liberalizing social norms (Scribner et al., 2000). Neighborhood alcohol outlet density may be associated with individual alcohol consumption through the frequency of exposure to cues relating to alcohol, including increased availability (Laibson, 2001). In addition to serving as a reminder to drink and supplying alcohol, outlets pose a situational risk in the neighborhood environment. Outlets are often sites where people who engage in high-risk behaviors gather, not just for drinking but sometimes to use and exchange other drugs. Alcohol outlets are also associated with more social disorder, which may be linked to various poor health outcomes.
The objectives of this study were (1) to examine whether neighborhood alcohol outlet density is positively associated with individual self-reported alcohol-related health outcomes in the last year—sexually transmitted infections (STI), motor vehicle accidents, injury, liver problems, hypertension and experienced violence; (2) to determine whether the relationship between morbidity and alcohol outlet density is mediated by individual alcohol consumption; and (3) to explore the role of alcohol outlet density in explaining any observed racial and ethnic differences in morbidity. Given the observed racial and ethnic differences in many of the outcomes examined (Centers for Disease Control and Prevention, 2000; Williams, 2001; Krieger et al., 2003) and the potential impact of alcohol density on certain population subgroups (Parker, 2004; Livingston et al., 2007), we sought to determine whether the impact of alcohol outlets on morbidity may also vary by race and/or ethnicity.
METHODS
Study sites and selection of census tracts
This cross-sectional study was conducted in Louisiana and California, which have different demographics, different retail sales patterns and different cultural attitudes toward alcohol. In Louisiana, there are areas (such as New Orleans) that are very permissive with alcohol, allowing purchases 24 h a day, 7 days per week, and other areas that are ‘dry’ (alcohol sale prohibited) or where the sale of alcohol is limited to certain hours. Los Angeles has more uniform retail sales patterns but a highly diverse population, allowing us to study the impact of alcohol marketing practices on different racial and ethnic groups. The study took place between 4 October 2004 and 28 August 2005 in Louisiana and 19 October 2005 in Los Angeles County. Sampling was limited to urban residential census tracts, with urban defined as having more than 2000 residents per square mile in the 2000 US census. We randomly selected 114 of these census tracts in southeastern Louisiana and 114 census tracts in Los Angeles County, for a total of 228 census tracts. In Louisiana, data collection was suspended when Hurricane Katrina struck, after measurements were collected in 103 census tracts. Those 11 census tracts differed only in population size (they included on average 2000 fewer people per tract) from the other census tracts selected in Louisiana. Furthermore, the sampling procedure was stratified by the region; therefore, the lost neighborhoods were representative of the New Orleans region in terms of SES and racial/ethnic content. Therefore, the representativeness of the remainder of the Louisiana sample was unaffected.
For the purpose of the present study, a census tract was used as a proxy for neighborhood. The resulting sample included 2881 individuals—1578 from Los Angeles County and 1303 from Louisiana. The research was approved by RAND Corporation, Charles R. Drew University of Medicine and Science, the Louisiana State University and Tulane University Institutional Review Boards.
Survey procedures
Sampling employed a two-stage procedure that involved selecting census tracts stratified by location (Los Angeles versus Southern Louisiana) in the first stage and sampling approximately 10 households per census tract in Los Angeles and in Louisiana using a list-based systematic sample in the second stage. A list-based sample was chosen because in addition to the phone numbers, we also required the corresponding addresses for geocoding. Up to 25 contact attempts were made.
Several steps were taken to improve response rates including sending advance letters, providing incentives (a $15 check upon completion), toll-free numbers, and answering machine messages. These channels supplemented and reinforced the work of interviewers, who provided information tailored to respondents’ questions. Advance letters were sent to all unique addresses in the household sample. In the event that multiple phone numbers were matched to the same address, only one letter was sent to that address. The advance letter explained the data collection project and encouraged respondents to participate. It also provided the toll-free telephone number for the participant to call and complete the survey and the number for the Principal Investigator at RAND for the participant to call to get more information about the study. The cooperation rate, the proportion of all cases interviewed of all eligible respondents ever contacted, was 76.2% in Los Angeles and 79.8% in Louisiana for the phone survey. The response rates for Los Angeles County and the state of Louisiana were 34.4% and 37.9%, respectively, based on the method codified by the Council of American Survey Research Organizations (CASRO), which reflects the percentage of completed interviews achieved after fully processing all attempted sample records according to the prescribed sample management rules.
Data sources
Individual-level data were obtained from the phone survey. Counts of alcohol licenses for all years came from the California Department of Alcohol Beverage Control (ABC) and the Louisiana Department Alcohol and Tobacco Control (ATC). Alcohol outlets were classified based on their license to sell alcohol off-premise (liquor stores, grocery stores and convenience stores) using license codes provided by the ABC or ATC (depending on state). Neighborhood-level socio-demographic characteristics were obtained from the 2000 US Census.
All unique address listings for survey respondents and alcohol outlets were geo-coded and mapped to the 2000 Census tract areas, and individual data sources were matched by the census tract. Over 98% of addresses were matched using Arcview GIS software (ESRI Inc, Redlands, CA, USA) along with Los Angeles County and Louisiana TIGER street files from the 2000 Census. Addresses that the computer were unable to match were hand placed with the help of an Internet mapping site (Mapquest) and a Thomas Guide map book.
Measures
The primary outcomes of interest included self-reported STI in the past year, motor vehicle accident in the past year, injury that required an emergency room visit in the last year, history of liver problems, history of hypertension, and heard, witnessed or experienced violence in their neighborhood in the past 6 months. All variables were dichotomous (yes versus no). Outcomes were chosen given their association with alcohol availability and alcohol consumption. Time frames for each morbidity survey items differed to reflect the average frequency of occurrence.
The primary exposure of interest was a contextual neighborhood factor—off-premise alcohol outlet density. Outlet density was measured as (1) the ratio of the number of off-premise outlets to the square mile area in each tract based on 2000 geographic census data; (2) the number of outlets per square mile in a 1.0 mile radius of each respondent's residence; and (3) individual geographic distance to the nearest off-premise outlet. The number of outlets per roadway mile was also calculated and compared for consistency with outlets per square mile. The number of outlets per square mile in distances of 0.1, 0.25 and 0.50 radii was also examined. Results were consistent and therefore we only present data using outlets per square mile and outlets within a 1.0 mile buffer.
Individual alcohol consumption was examined as the primary mediator in the relationship between off-premise neighborhood alcohol outlet density and self-reported morbidity outcomes. Consumption patterns included the number of drinking days per year (measured on a scale from 1–8 or never to daily and recoded to 0, 12, 30, 78, 182, 273 and 365), the number of drinks per day on days when alcohol is consumed, the average estimated daily ethanol consumption in the last 90 days, the average daily ethanol consumption in the last 12 months and heavy episodic drinking (HED) or having at least five or more drinks for men or four or more drinks for women per sitting at least 1 day in the last month (yes/no). The average daily ethanol consumption based on the previous 90 days was computed as follows:
where ‘ethanol’ is the alcohol content of the respondent's most common drink in the last 90 days, ‘ounces’ the size of that drink in ounces, ‘drinks’ the number of drinks per occasion and ‘drinkdays90’ the number of days drinking within the last 90 days.
Race was assessed in the survey as White, Black, Asian, American Indian, Pacific Islander and multi-racial. Due to the limited number of Asian, American Indian, Pacific Islander and multi-racial respondents, these racial categories were combined into one group for primary analyses. Ethnicity was measured as in the survey—Hispanic or non-Hispanic ethnicity.
Additional factors examined as potential predictors of self-reported morbidity or as potential confounding factors in the alcohol density–morbidity relationship included individual- and neighborhood-level socio-demographic characteristics, individual perception of neighborhood characteristics and aggregated neighborhood characteristics, and sexual behavior (primarily for STI outcome). Individual-level socio-demographic characteristics included sex, age, marital status (married versus not married), education (0–5, never attended school to college graduate), employment (employed full-time, legally, versus other) and annual income (0–3, <$20,000, $20,000 to $34,999, $35,000–$74,999 and ≥$75,000). Neighborhood-level socio-demographic characteristics included percentage White, Black and Hispanic, percentage with less than a high school education, percentage below the Federal poverty level (for US 2000 Census) and economic deprivation. Economic deprivation or concentrated disadvantage was measured using a Z-score standardized index of concentrated disadvantage (Sampson and Morenoff, 2004) measuring economic disadvantage in urban neighborhoods and defined by the percent of families below the poverty line, percent of families receiving public assistance, percent of unemployed individuals in the civilian labor force and percent of female-headed families with children (Cronbach's alpha = 0.86).
Sexual behavior included an index of sexual risk, calculated based on the number of sexual partners in the last 12 months and whether a condom was used during the last sexual encounter (yes/no), and ranging from 0 to 4 where 0 = lowest risk (no sex partners), 1 = one sex partner and condom use at last sex, 2 = one sex partner and no condom use, 3 = two or more sex partners and condom use and 4 = two or more sex partners and no condom use.
Statistical analyses
Second-level hierarchical logistic regression models, with individuals (first level, n = 2881) nested within neighborhoods or census tracts (second level, n = 217) were used to examine the contextual effect of alcohol outlet density on self-reported morbidity outcomes. SAS version 9 was used for all analyses, including PROC GLIMMIX for hierarchical models. Such models allow for estimates of variance components at both the individual level and neighborhood level (Bryk and Raudenbush, 1992, Snijders and Boskers, 1999). Partitioning variance in this way accounts for the variance in individual-level outcomes that can be attributed to differences between neighborhoods, expressed as the intraclass correlation coefficient (ICC). The ICC was calculated as follows:
where Vneighborhood = variance between neighborhoods and Vindividual = variance within neighborhoods or between individuals. For all outcomes, which are dichotomous or binary in nature, the ICC was calculated by following the formula of Snijders based on an underlying continuous variable with Vstudent =  2/3 (Snijders and Boskers, 1999).
2/3 (Snijders and Boskers, 1999).
For each outcome variable, the following models were examined: (1) an empty or unconditional means model that is a function of the neighborhood-level random intercept (used to obtain the amount of clustering in morbidity within neighborhood); (2) crude bivariate multi-level models including all individual- and neighborhood-level measures to examine their crude association with morbidity—paying particular attention to the relationship between alcohol outlet density and each outcome; (3) for models with a significant association between density and morbidity, alcohol consumption patterns were added to the crude and adjusted (adjusted for known predictors of morbidity outcomes) models (separately) to examine potential mediation by consumption; and (4) multivariate models were examined to determine the impact of alcohol outlet density on any observed racial or ethnic differences in morbidity, including according to study location.
Mediation by alcohol consumption was assessed by including, separately, each consumption pattern (i.e. drinking days or frequency, drinks per day or quantity, average daily ethanol consumption in last 90 days and year, and HED) in a multivariate model with off-premise outlet density—for morbidity outcomes with a significant relationship between density and morbidity. Removal of the effect of density after inclusion of alcohol consumption patterns, and a significant relationship between consumption and morbidity outcomes, was deemed indicative of mediation.
All of the individual-level variables were centered at their respective means. The effects of any spatial autocorrelation in the data were taken into account in PROC GLIMMIX with repeated measures of spherical clustering, based on the tract centroids and state plane coordinate system in miles, using a 2.5 mile lag distance.
RESULTS
Among the 2881 survey respondents, the prevalence of select morbidities—STI (1.0%), motor vehicle accident (8.1%), injury (11.5%), liver problems (4.9%), hypertension (20.7%) and experienced violence (20.0%)—was within local and national prevalence estimates for these outcomes. For example, with respect to STI, national HIV prevalence is 1.0% (CDC, 2008a) and rates of Chlamydia range from 1.2% to 13.8% and gonorrhea from 0.1% to 3.8% (CDC, 2008b). In the United States, 7% of deaths are injury related and the prevalence of initial physician office and outpatient department visits for injury is 12% (Bergen et al., 2008). The prevalence of hypertension in the United States is 32% (CDC, 2009).
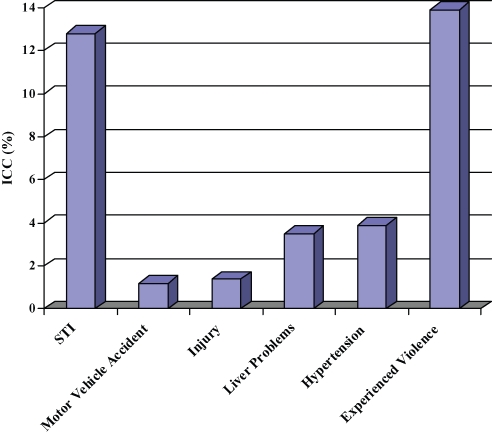
There were no significant differences by study region in morbidity outcomes except for hypertension, which was higher among Louisiana than California respondents (23.8% versus 17.4%, likelihood ratio chi-square = 16.9, P < 0.001). The clustering of morbidity by neighborhood varied by outcome, as shown in Fig. 1. There was strong clustering of STI (ICC = 12.8%) and experienced violence (ICC = 13.0%), moderate clustering of liver problems (ICC = 3.5%) and hypertension (ICC = 3.9%), and low clustering of motor vehicle accident (ICC = 1.2%) and injury (ICC = 1.4%).
Fig. 1.
Clustering of self-reported morbidity outcomes.
Table 1 presents characteristics of survey participants. The majority of respondents were female (63.9%) and substantial proportions were White (46.2%) or Black (25.3%). Approximately one-fifth was Hispanic. Respondents ranged in age from 18 to 65 (mean = 42.9 years). Nearly half (46.9%) indicated they were married and 62.2% were employed full-time. Half of the respondents reported an annual income of $34,999 or less. The average number of years lived in their neighborhood was 11.9 (range = 1–64).
Table 1.
Characteristics of participants
| Number (%) | |
|---|---|
| or mean (SD) | |
| Study location | |
| LA county | 1578 (54.8%) |
| State of LA | 1303 (45.2%) |
| Sex | |
| Male | 1039 (36.1%) |
| Female | 1842 (63.9%) |
| Age (years) | 42.9 (13.2) |
| Race | |
| White | 1330 (46.2%) |
| Black | 731 (25.3%) |
| Other | 820 (28.5%) |
| Hispanic ethnicity (yes) | 663 (23.0%) |
| Married (yes) | 1352 (46.9%) |
| Employed full-time, legally (yes) | 1791 (62.2%) |
| Annual income | |
| < $20,000 | 847 (31.8%) |
| $20,000–$34,999 | 500 (18.8%) |
| $35,000–$74,999 | 704 (26.4%) |
| ≥$75,000 | 612 (23.0%) |
| Years lived in neighborhood | 11.9 (11.1) |
| Distance to nearest off-premise alcohol outlet (miles) | 0.5 (±1.1) |
| Individual off-premise outlet density in 1.0 mile radius | 1.1 (±0.9) |
| Drinking days per year (0–365) | 51.7 (±88.2) |
| Drinks per day on days drink | 1.3 (±1.4) |
| Average daily consumption in last 90 days | 0.10 (±0.5) |
| Average daily consumption in last year | 0.02 (±0.1) |
| Heavy episodic drinking (HED) in the last month (yes) | 512 (17.8%) |
| Level of visible alcohol use in neighborhood | 2.4 (±1.5) |
| Sexual risk behavior (range = 0–4) | 1.6 (±1.1) |
Note. Number and percentages reflect that of non-missing responses.
The average distance to the nearest off-premise outlet was 0.5 mile and the average individual off-premise outlet density in a 1.0 mile radius was 1.1. Respondents drank, on average, 51.7 days out of the year, with an average of 1.3 drinks per day. Approximately 20% were classified as heavy episodic drinkers (HED). The average level of visible alcohol consumption in the neighborhood was between at least once a year and once a month.
Individual-level characteristics associated with morbidity outcomes varied, as shown in Table 2, and included both protective and risk factors for self-reported morbidity. Compared to White respondents, Black respondents were significantly more likely to indicate that they had been injured (crude OR = 1.56, 95% CI = 1.10, 2.20) or had hypertension (crude OR = 2.56, 95% CI = 1.94, 3.38). Respondents of other racial backgrounds were also significantly more likely to report hypertension than White respondents (crude OR = 1.37, 95% CI = 1.05, 1.80). Respondents of Hispanic ethnicity were significantly less likely to report injury and hypertension than were non-Hispanics.
Table 2.
Characteristics of participants and crude association between participant characteristics and self-reported morbidity (N = 2881)
| Crude odds ratio (95% CI) | ||||||
|---|---|---|---|---|---|---|
| Motor vehicle | Experienced | |||||
| STI | accidentc | Injury | Liver problems | Hypertension | violence | |
| Study locationa | ||||||
| State of LA | 1.29 (0.6–2.9) | 1.09(0.8–1.4) | 1.11 (0.9–1.4) | 0.83 (0.6–1.2) | 1.54 (1.26–1.88)‡ | 1.02 (0.8–1.3) |
| LA county | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Sexa | ||||||
| Male | 0.99 (0.4–2.3) | 0.95 (0.7–1.3) | 1.25 (0.99–1.6) | 1.35 (0.96–1.9) | 0.84 (0.7–1.02) | 1.02 (0.8–1.3) |
| Female | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Age (years) | 0.98 (0.9–1.0) | 0.98 (0.97–0.99)‡ | 0.99 (0.98–0.99)‡ | 1.03 (1.02–1.05)† | 1.07 (1.06–1.08)‡ | 0.98 (0.97–0.99)† |
| Racea | ||||||
| White | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Black | 1.18 (0.41, 3.43) | 1.14 (0.77, 1.71) | 1.56 (1.1, 2.2)‡ | 1.06 (0.62, 1.79) | 2.56 (1.94, 3.38)‡ | 1.19 (0.89, 1.59) |
| Other | 0.81 (0.29, 2.23) | 1.15 (0.80, 1.63) | 1.22 (0.89, 1.68) | 1.33 (0.84, 2.09) | 1.37 (1.05, 1.8)‡ | 0.81 (0.62, 1.06) |
| Hispanic ethnicity (yes) | 1.31 (0.5–3.2) | 0.83 (0.6–1.2) | 0.68 (0.5–0.9)‡ | 1.27 (0.86–1.9) | 0.54 (0.42–0.69)‡ | 1.15 (0.9–1.5) |
| Married (yes) | 0.53 (0.2–1.2) | 0.68 (0.50–0.90)‡ | 0.64 (0.5–0.8)‡ | 0.77 (0.55–1.1) | 0.83 (0.77–0.99)† | 0.66 (0.54–0.81)‡ |
| Education, 0 = never attended school to 5 = college graduatea | 0.76 (0.60–0.90)‡ | 1.11 (0.98–1.3) | 0.95 (0.87–1.05) | 0.74 (0.65–0.85)‡ | 0.94 (0.9–1.02) | 0.97 (0.9–1.05) |
| Employed full-time, legally (yes) | 0.56 (0.3–1.2) | 1.24 (0.9–1.7) | 0.73 (0.58–0.92)‡ | 0.41 (0.29–0.59)‡ | 0.57 (0.48–0.69)‡ | 0.93 (0.8–1.13) |
| Annual income | ||||||
| <$20 000 | 12.71 (0.83, 94.04)b | 0.82 (0.56, 1.22) | 1.33 (0.95, 1.85) | 2.04 (1.24, 3.34)‡ | 1.37 (1.04, 1.80)‡ | 1.77 (1.31, 2.41)‡ |
| $20 000–$34 999 | 5.52 (0.39, 76.63)b | 0.90 (0.58, 1.40) | 0.93 (0.62, 1.38) | 1.06 (0.57, 1.96) | 1.29 (0.95, 1.75) | 1.36 (097, 1.91) |
| $35 000–$74 999 | 5.60 (0.40, 79.64)b | 1.04 (0.71, 1.54) | 1.05 (0.74, 1.50) | 0.90 (0.50, 1.61) | 1.06 (0.80, 1.42) | 1.17 (0.85, 1.61) |
| ≥$75 000 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Years lived in neighborhood | 0.96 (0.9–1.0) | 1.00 (0.98–1.0) | 0.98 (0.97–0.99)† | 1.00 (0.99–1.02) | 1.03 (1.02–1.04)‡ | 0.99 (0.98–1.00) |
| Distance to nearest off-premise alcohol outlet (miles) | 0.81 (0.3–1.8) | 1.05 (0.96–1.1) | 1.05 (0.97–1.1) | 0.89 (0.7–1.2) | 1.05 (0.97–1.1) | 0.88 (0.8–1.02) |
| Individual off-premise outlet density in 1.0 mile radius | 1.08 (1.01–1.2)† | 0.86 (0.7–1.0) | 1.04 (0.9–1.2) | 1.30 (1.1–1.5)† | 0.92 (0.8–1.04) | 1.44 (1.25–1.65)‡ |
| Drinking days per year (0–365) | 1.05 (0.9–1.3) | 1.07 (1.01–1.1)† | 1.02 (0.97–1.1) | 0.86 (0.8–0.94)‡ | 0.89 (0.85–0.94)‡ | 1.05 (1.01–1.10)† |
| Drinks per day on days drink | 1.19 (0.9–1.5) | 1.06 (0.97–1.2) | 1.09 (1.01–1.2)† | 0.91 (0.8–1.04) | 0.83 (0.77–0.89)‡ | 1.15 (1.07–1.22)‡ |
| Average daily consumption in the last 90 days | 0.93 (0.3–2.5) | 1.0 (0.9–1.7) | 4.26 (1.4–13.3)‡ | 0.6 (0.2–1.5) | 0.85 (0.7, 0.98)† | 3.39 (1.2–9.8)‡ |
| Average daily consumption in the last year | 1.70 (0.1–3.2) | 1.6 (0.7–2.1) | 1.05 (0.9–1.3) | 1.9 (0.6–6.9) | 0.26 (0.04–1.6) | 0.96 (0.8–1.2) |
| Heavy episodic drinking (HED) in the last month (yes) | 1.15 (0.4–3.1) | 1.31 (0.94–1.8) | 1.50 (1.14–1.98)‡ | 0.93 (0.6–1.5) | 0.55 (0.42–0.72)‡ | 1.43 (1.13–1.81)‡ |
| Level of visible alcohol use in the neighborhood | 1.45 (1.1–1.9)‡ | 1.11 (1.01–1.2)† | 1.15 (1.07–1.24)‡ | 1.20 (1.07–1.34)‡ | 0.97 (0.9–1.03) | 1.62 (1.52–1.73)‡ |
| Sexual risk behavior (range = 0–4) | 1.62 (1.1–1.4)‡ | 1.09 (0.9, 1.2) | 1.10 (0.98, 1.24)† | 0.99 (0.84, 1.17) | 0.70 (0.64, 0.77)‡ | 1.15 (1.05, 1.26)‡ |
P-value: ‡ < 0.01; † < 0.05 based on crude multi-level logistic regression models accounting for spatial autocorrelation.
aComparisons made for: state of LA versus LA county; males versus females; race listed versus White race; lowest versus highest education level.
bExact logistic regression used for STI–income association given the extremely small cell sizes.
cControlling for car ownership.
Similar to neighborhood off-premise outlet density, individual-level outlet density in a 1.0 mile radius was positively and significantly associated with STI (crude OR = 1.08, 95% CI = 1.01–1.20), liver problems (crude OR = 1.30, 95% CI = 1.10–1.50) and experienced violence (crude OR = 1.44, 95% CI = 1.25–1.65). The frequency of alcohol consumption (drinking days) was associated significantly and positively with having a motor vehicle accident and witnessing violence and inversely with liver problems and hypertension. The number of drinks per day and binging were both positively and significantly associated with injury and violence and inversely associated with hypertension.
Neighborhood-level characteristics and their association with morbidity are presented in Table 3. The average proportion of White, Black and Hispanic residents was ∼30%. The average percentage of residents below poverty was 21.0% and the average concentrated disadvantage was 2.2 (range = −4.6 to 20). The average off-premise alcohol outlet density per square mile was 10.2 (range = 0–100, 25th percentile = 3.0, 75th percentile = 14.0).
Table 3.
Neighborhood-level characteristicsa and crude association between neighborhood characteristics and self-reported morbidity (N = 2881)
| Crude odds ratio (95% CI) | ||||||
|---|---|---|---|---|---|---|
| Motor vehicle | Experienced | |||||
| STI | accidentb | Injury | Liver problems | Hypertension | violence | |
| Mean off-premise outlet density per square mile | 1.80 (1.1–3.0)§ | 0.99 (0.9–1.0) | 1.02 (0.89–1.16) | 1.33 (1.02–1.75)† | 0.98 (0.9–1.1) | 1.31 (1.13–1.51)‡ |
| Mean distance to nearest off-premise outlet | 0.85 (0.4–1.8) | 0.97 (0.8–1.1) | 0.95 (0.82–1.10) | 0.63 (0.38–1.03) | 1.00 (0.9–1.1) | 0.89 (0.8–1.04) |
| Mean visible alcohol use in neighborhood | 1.55 (0.9–2.6) | 0.97 (0.8–1.2) | 1.24 (1.06–1.45)† | 1.60 (1.28–1.99)‡ | 1.09 (0.94–1.3) | 2.09 (1.79–2.44)‡ |
| Mean % White | 0.73 (0.2–3.1) | 1.00 (1.00–1.01) | 1.00 (0.99–1.00) | 0.98 (0.95–1.00) | 0.99 (0.98–1.00) | 0.97 (0.98–0.99)† |
| Mean % Black | 1.01 (0.99–1.02) | 0.97 (0.6–1.5) | 1.50 (1.02–2.22)† | 0.87 (0.47–1.60) | 2.76 (2.02–3.76)‡ | 2.82 (2.10–3.80)‡ |
| Mean % Hispanic | 1.47 (0.4–5.3) | 0.62 (0.4–1.02) | 0.80 (0.5–1.2) | 1.90 (1.10–3.27)† | 0.44 (0.31–0.63)‡ | 1.30 (0.96–1.76) |
| % Neighborhood with < high school education | 1.57 (0.6–4.4) | 0.56 (0.1–2.2) | 1.76 (0.58–5.4) | 0.94 (0.15–5.9) | 9.09 (3.8–21.8)‡ | 14.09 (4.1–8.1)‡ |
| Mean % below poverty | 10.10 (0.6–18.3) | 0.33 (0.1–0.9)† | 2.72 (1.14–6.5)‡ | 8.48 (2.56–28.1)‡ | 1.58 (0.7–3.5) | 37.8 (15.5–91.8)‡ |
| Mean concentrated disadvantage | 1.02 (0.9–1.1) | 0.97 (0.9–1.0) | 1.04 (1.01–1.06)† | 1.04 (1.01–1.08)† | 1.05 (1.02–1.07)† | 1.11 (1.08–1.14)‡ |
P-value: ‡ <0.0001; † <0.01; § <0.05 based on crude multi-level logistic regression models accounting for spatial autocorrelation.
aAggregated individual-level items for all characteristics except outlet density, racial distribution, education, poverty and concentrated disadvantage.
bControlling for car ownership.
The off-premise outlet density was significantly and positively associated with STI (crude OR = 1.80, 95% CI = 1.10–3.00), liver problems (crude OR = 1.33, 95% CI = 1.02–1.75) and experienced violence (crude OR = 1.31, 95% CI = 1.13–1.51) but not with other morbidity outcomes. Additional neighborhood-level factors associated with morbidity varied, as shown in Table 3.
Table 4 presents the result of the hypothesized mediation models for STI, liver problems and experienced violence (i.e. factors that were significantly associated with neighborhood off-premise outlet density). Model 1 presents the adjusted relationship between off-premise outlet density and each morbidity outcome, controlling for study location, age, sex, race, ethnicity, education and income. Models 2–6 add individual alcohol consumption patterns—drinking days, drinks per day, average daily consumption in last 90 days and year, and HED drinking—to Model 1 to examine mediation by consumption.
Table 4.
Mediation by alcohol consumption on neighborhood alcohol outlet density and self-reported morbidity (N = 2881)
| Adjusted odds ratio (95% CI) | |||
|---|---|---|---|
| STI | Liver problems | Experienced violence | |
| Model 1 | |||
| Off-premise outlet density in 1.0 mile radius from home | 1.80 (1.1–3.0)† | 1.33 (1.02–1.75)† | 1.31 (1.13–1.51)‡ |
| Model 2 | |||
| Off-premise outlet density in 1.0 mile radius from home | 1.78 (1.06–2.97)† | 1.27 (0.96–1.67) | 1.03 (1.02–1.04)† |
| Drinking days per year (0–365) | 0.99 (0.80–1.22) | 0.86 (0.79–0.95)‡ | 1.06 (1.01–1.11)† |
| Model 3 | |||
| Off-premise outlet density in 1.0 mile radius from home | 1.78 (1.07–2.96)† | 1.33 (1.01–1.75)† | 1.03 (1.01–1.04)‡ |
| Drinks per day on days drink | 1.09 (0.82–1.44) | 0.91 (0.80–1.04) | 1.15 (1.07–1.22)‡ |
| Model 4 | |||
| Off-premise outlet density in 1.0 mile radius from home | 1.02 (1.00, 1.04)§ | 1.01 (1.00, 1.03)§ | 1.02 (1.01, 1.04)‡ |
| Estimated daily consumption, last 90 days | 0.94 (0.34, 2.56) | 0.59 (0.23, 1.53) | 0.99 (0.81, 1.20) |
| Model 5 | |||
| Off-premise outlet density in 1.0 mile radius from home | 1.02 (1.01, 1.04)§ | 1.02 (1.00, 1.03)§ | 1.02 (1.01, 1.03)‡ |
| Estimated daily consumption, last year | 0.99 (0.81, 1.20) | 1.85 (0.52, 6.59) | 4.23 (1.26, 14.22)§ |
| Model 6 | |||
| Off-premise outlet density in 1.0 mile radius from home | 1.78 (1.07–2.97)† | 1.33 (1.02–1.75)† | 1.03 (1.01–1.04)‡ |
| HED at least one day in the last month | 1.02 (0.34–3.06) | 0.93 (0.59–1.46) | 1.42 (1.12–1.80)‡ |
P-value: ‡ <0.0001; † <0.01; § <0.05 based on adjusted multi-level logistic regression models, adjusted for study location, age, sex, race, ethnicity, education and income.
Contrary to the conceptualized mediating relationship between individual alcohol consumption on the relationship between neighborhood off-premise density and STI, the addition of alcohol consumption patterns did not reveal any full mediation—density remained significantly and positively associated with STI for each consumption pattern and individual consumption was not associated with STI. The effect estimate was reduced by including any one of the individual consumption items, especially estimated daily ethanol consumption (adjusted OR = 1.80–1.02) which may indicate some partial mediation although none of the consumption items were significantly associated with STI. Results for STI were more consistent with a confounding relationship, i.e. the addition of consumption patterns (separately, Models 2–6) to a model with density did not remove but weakened the effect of density on STI, so that controlling for the amount of individual consumption provides a more valid estimate of the role that neighborhood alcohol outlet density plays on STI.
For liver problems, the number of drinking days per year did appear to mediate the relationship between neighborhood density and consumption (rendering density insignificant and consumption being significantly associated with liver problems); however, this relationship is difficult to determine given the study design and nature of the outcome and its impact on consumption (i.e. liver problems could lead to a decrease in consumption, yet alcohol consumption does lead to liver problems).
The results for experienced violence suggest potential partial mediation and/or confounding of individual alcohol consumption in the relationship between neighborhood outlet density and violence.
Table 5 presents the results of multivariate hierarchical models for the association between outlet density per square mile and density within a 1.0 mile radius of the respondent's home, for each morbidity outcome, stratified by race and ethnicity. The impact of outlet density on morbidity outcomes did differ by race and ethnicity, although in some instances this may have been a result of decreased sample size. Nonetheless, differences were observed and for the majority of outcomes, the magnitude of effect was greater when outlet density in a 1.0 mile radius was considered (versus density per square mile of tract or neighborhood).
Table 5.
Morbidity and the neighborhood alcohol environment—potential modification by race and ethnicity
| Adjusted odds ratio (95% CI) | ||||||
|---|---|---|---|---|---|---|
| Motor vehicle | Experienced | |||||
| STI | accident | Injury | Liver problems | Hypertension | violence | |
| Impact of off-premise outlet density per square mile | ||||||
| Among Whites (n = 1330) | 1.04 (1.01, 1.08)† | 0.99 (0.96, 1.01) | 1.01 (0.99, 1.04) | 1.01 (0.99, 1.04) | 1.00 (0.99, 1.02) | 1.05 (1.03, 1.07)‡ |
| Among Blacks (n = 731) | 1.02 (0.99, 1.05) | 0.99 (0.97, 1.02) | 1.12 (1.02, 1.13)† | 1.02 (1.01, 1.03)† | 1.00 (0.99, 1.01) | 1.01 (0.99, 1.02) |
| Among other racial groups (n = 820) | 0.95 (0.85, 1.05) | 0.97 (0.94, 1.01)§ | 1.02 (1.00, 1.05) | 1.02 (1.00, 1.05) | 0.99 (0.97, 1.01) | 1.02 (1.00, 1.04)† |
| Among Hispanics (n = 657) | 1.03 (1.01, 1.05)† | 0.97 (0.93, 1.00)§ | 1.00 (0.97, 1.02) | 1.01 (0.99, 1.04) | 1.01 (0.99, 1.03) | 1.01 (0.89, 1.03) |
| Among non-Hispanics (n = 2049) | 0.99 (0.93, 1.06) | 0.99 (0.98, 1.01) | 1.01 (1.00, 1.02) | 1.02 (1.01, 1.03)† | 1.00 (0.99, 1.01) | 1.03 (1.01, 1.04)‡ |
| Impact of individual off-premise outlet density in 1.0 mile radius from home | ||||||
| Among Whites (n = 1330) | 1.65 (1.05, 2.90)† | 0.86 (0.67, 1.11) | 1.26 (0.96, 1.64)§ | 1.07 (0.87, 1.32) | 0.99 (0.83, 1.18) | 1.63 (1.34, 1.99)‡ |
| Among Blacks (n = 731) | 1.25 (0.74, 2.13) | 0.84 (0.61, 1.14) | 1.43 (1.12, 1.83)‡ | 1.12 (0.93, 1.36) | 0.87 (0.73, 1.04) | 1.02 (0.83, 1.25) |
| Among other racial groups (n = 820) | 1.41 (0.64, 3.14) | 0.73 (0.50, 1.06)§ | 1.29 (0.85, 1.96) | 0.95 (0.70, 1.28) | 0.84 (0.65, 1.08) | 1.50 (1.20, 1.86)‡ |
| Among Hispanics (n = 657) | 2.08 (1.03, 4.23)‡ | 0.51 (0.33, 0.77)‡ | 1.09 (0.67, 1.21) | 1.19 (0.83, 1.70) | 1.12 (0.88, 1.41) | 1.28 (1.03, 1.59)‡ |
| Among non-Hispanics (n = 2049) | 1.24 (0.80, 1.94) | 0.95 (0.78, 1.14) | 1.16 (1.01, 1.35)† | 1.30 (1.08, 1.57)‡ | 0.93 (0.81, 1.06) | 1.40 (1.18, 1.66)‡ |
P-value: ‡ < 0.01; † < 0.05; § < 0.10 based on adjusted multi-level logistic regression models, adjusted for study location, age, sex, race, ethnicity, education and income.
The association between outlet density and STI was stronger among Whites compared to Blacks or other respondents and stronger among Hispanics compared to non-Hispanic respondents. Greater outlet density was associated with decreased likelihood of motor vehicle accidents among other racial groups and Hispanics. Outlet density was positively associated with injury for all racial and ethnic groups, and significantly so for Whites, Blacks and non-Hispanics when density in a 1.0 mile buffer was considered. Greater density was also associated with a greater likelihood of liver problems among non-Hispanics and a greater likelihood of experienced violence for all racial and ethic groups, although not significantly so for Black respondents. There were no observed associations between density and hypertension once the data were stratified by race and ethnicity.
While not examined in a mediation model, reported visible alcohol use in the respondent's neighborhood was positively and significantly associated with all morbidity outcomes except hypertension. Such visible alcohol use may be a marker for social disorder. Because drug markets, violence and alcohol availability may overlap (Zhu et al., 2004, 2006), social and health problems in areas with increased alcohol availability may be driven more by the overlapping social issues and resulting social disorder than by alcohol availability alone. In this sample, measures of neighborhood alcohol outlet density were significantly (P < 0.001) correlated with visible alcohol use at a magnitude of 0.20–0.30.
DISCUSSION
The neighborhood environment increasingly is being recognized as a key component of individual health. Key findings of our study are that morbidity clusters by neighborhood, alcohol outlet density is associated with several alcohol-related outcomes, (STI, liver problems and experienced violence) and the associations are heterogeneous with respect to race and ethnicity.
With increased clustering indicative of a stronger area-based (in this case, census tract) influence, results suggest that, in the present sample, the neighborhood influence is strongest for STI and experienced violence, and lowest for motor vehicle accident and injury. STIs were mainly reported in females who typically are infected from sexual relations with males. The reason why the association with alcohol outlet density may not be mediated by individual drinking is because the male partner may be the one who drinks, while the female recipient of the STI may be abstinent from alcohol. Similarly, an abstinent resident in a neighborhood with high alcohol outlet density will be just as likely to experience violence as the residents who drink. Contextually determined outcomes may not be mediated by individuals’ drinking behaviors. In contrast, liver problems only occur as a consequence of individual drinking, so mediation would be expected. Motor vehicle accidents, on the other hand, are very individually isolated outcomes that typically occur when traveling outside of the neighborhood, for which a car is needed. While the environment is expected to have a greater impact on injury, the question did not limit responses to injuries occurring in or near home, but could have occurred at work or elsewhere.
Furthermore, only density in a radius (e.g. 1.0 mile) from the respondent's home and density per square mile of the census tract (rather than distance to travel to nearest outlet) were associated with STI, liver problems and experienced violence. We have shown in these data that alcohol density impacts on alcohol consumption rather than nearness of the closest outlet (Schonlau et al., 2008) and we showed the same in a previous study (Scribner et al., 2000).
In addition to variation in the associations between alcohol outlet density measures and morbidity outcomes, there were inconsistencies in the association between individual consumption patterns and morbidity outcomes. Individual consumption was positively associated with experienced violence. The inverse relationship between individual ethanol consumption and hypertension may reflect that patients with some medical conditions or taking medication avoid alcohol.
Despite few observed racial and ethnic differences in self-reported morbidity outcomes, we examined the contribution of alcohol outlet density to all outcomes within each racial and ethnic group. Although the decreased sample size and therefore power may have influenced some of the results of the stratified analysis, significant associations with outlet density were observed and for the majority of outcomes, the magnitude of effect was greater when outlet density in a 1.0 mile radius was considered (versus density per square mile of tract or neighborhood). Outlet density appears, in our sample, to have had a stronger impact on STI among White and Hispanic respondents, and on injury among Black respondents. Furthermore, Black respondents were the only group within whom outlet density did not impact their likelihood of experienced violence. This may also be a result of limited variation in alcohol outlet density among Black respondents, with more clustering of Black respondents in neighborhoods that also have high rates of alcohol availability.
Limitations of this study include a cross-sectional design, survey sampling methodology, self-reported alcohol consumption and morbidity outcomes, and inclusion of only off-premise outlets. Because the sampling was based on listed landline numbers, the response rate was likely impacted. Furthermore, the self-reported nature of the study's surveys and the resulting data on alcohol use and alcohol-related health incidence may have resulted in under-reporting by respondents. Therefore, one of this study's strengths of utilizing respondent information may also have been a limitation; however, the use of self-reporting surveys among the general public is a vital tool that may be the only way to obtain data from individuals who are not currently seeking treatment for their alcohol-related health conditions.
The computing of alcohol-outlet density was based only on off-premise locations. Many of the examined outcomes may also be greatly influenced by on-premise environments (e.g. violence, STI). As mentioned, respondents’ reporting of alcohol consumption was not restricted to what they consumed from off-premise purchases, while on-premise locations may clearly play a large role in alcohol consumption. Furthermore, there may be substantial variations within the two geographic locations in the number of on-premise outlets and their impact on alcohol access, consumption and alcohol-related morbidity. However, study location was controlled for in all analyses to minimize this effect. Analyses were limited to off-premise outlets due to data availability but also because we wished to examine the unique impact of off-premise outlets.
Another limitation is that we examined variations in the density and morbidity relationships only by race and ethnicity, but such differences by class, income, age and other demographics are also important and may be examined in future studies.
Furthermore, the only off-premise parameter examined was density measures and therefore we did not account for differences in the availability by outlet type (e.g. liquor stores versus grocery stores), the impact of alcohol advertising and promotion within or near outlets, or alcohol pricing (Bluthenthal et al., 2008). Additionally, while density per square mile is a widely used measure of alcohol density, density per capita is also commonly used and has the advantage of accounting for population density. As an additional sensitivity analysis, we calculated a per capita (per 1000 population) measure and compared it with the per square mile measure. Results were similar, which was expected given the more urban nature of the sampled tracts (Scribner et al., 1999).
In conclusion, our findings support the notion that alcohol outlets are likely to play a significant role in health outcomes at the neighborhood level, irrespective of individual consumption patterns. Alcohol availability may have a different influence on individuals according to race or ethnicity, although additional research is needed to confirm and further understand this possibility. To address the impact of alcohol availability and other contextual factor on health outcomes, knowledge not only of its association with health outcomes but also on why and how these environments may influence health is required (Morenoff, 2003). Observed results presented here suggest that, with respect to neighborhood alcohol availability, changing this environment may prove effective at reducing certain alcohol-related morbidity outcomes.
Acknowledgments
This research was supported by grants from the Centers for Disease Control and Prevention, CDC (1K01SH000002-01 to K.P.T.); the National Cancer Institute, NCI (1 R03 CA103484-01 to D.C.); and the National Institute on Alcohol Abuse and Alcoholism, NIAAA (R01AA013749 to R.S.). The authors wish to thank Paul Robinson, Adrian Overton, Diane Schoeff, Heather Guentzel, Kamua Williams, Michael Murrley, Erica Alacrcon, Catherine Haywood, Kellie Trombacco and all of the study participants. The views presented in this paper are those of the authors and do not represent those of the funding agencies.
References
- Bergen G, Chen LH, Warner M, et al. Injury in the United States: 2007 Chartbook. Hyattsville, MD: National Center for Health Statistics; 2008. [Google Scholar]
- Bluthenthal R, Cohen D, Farley T, et al. Alcohol availability and neighborhood characteristics in Los Angeles, California, and Southern Louisiana. J Urban Health. 2008;85:191–205. doi: 10.1007/s11524-008-9255-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryk AS, Raudenbush SW. Hierarchical Linear Models: Applications and Data Analysis Methods. Newbury Park, CA: Sage; 1992. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) State-specific prevalence of selected health behaviors, by race and ethnicity: Behavioral Risk Factor Surveillance System, 1997. Morb Mortal Wkly Rep. 2000;49:1–60. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) 2008a;19 HIV/AIDS Surveillance Report. Year-end 2007 Edition. Atlanta, GA: U.S. Department of Health and Human Services. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Sexually Transmitted Disease Surveillance, 2007. Atlanta, GA: U.S. Department of Health and Human Services; 2008b. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Health, United States, 2008 with Chartbook. Hyattsville, MD: National Center for Health Statistics.; 2009. [Google Scholar]
- Cohen DA, Ghosh-Dastidar B, Scribner R, et al. Alcohol outlets, gonorrhea, and the Los Angeles civil unrest: a longitudinal analysis. 2006;62:3062–71. doi: 10.1016/j.socscimed.2005.11.060. Social Science and Medicine 2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorman DM, Speer PW, Gruenewald PJ, et al. Spatial dynamics of alcohol availability, neighborhood structure and violent crime. J Stud Alcohol. 2001;62:628–36. doi: 10.15288/jsa.2001.62.628. [DOI] [PubMed] [Google Scholar]
- Gruenewald PJ. The spatial ecology of alcohol problems: niche theory and assortative drinking. Addiction. 2007;102:870–8. doi: 10.1111/j.1360-0443.2007.01856.x. [DOI] [PubMed] [Google Scholar]
- Gruenewald PJ, Johnson FW, Millar A, et al. Drinking and driving: explaining beverage-specific risks. J Stud Alcohol. 2000;61:515–23. doi: 10.15288/jsa.2000.61.515. [DOI] [PubMed] [Google Scholar]
- Gruenewald PJ, Johnson FW, Treno AJ. Outlets, drinking and driving: a multilevel analysis of availability. J Stud Alcohol. 2002;63:460–8. doi: 10.15288/jsa.2002.63.460. [DOI] [PubMed] [Google Scholar]
- Gruenewald PJ, Ponicki WR. The relationship of alcohol sales to cirrhosis mortality. J Stud Alcohol. 1995;56:635–41. doi: 10.15288/jsa.1995.56.635. [DOI] [PubMed] [Google Scholar]
- Gruenewald PJ, Ponicki WR, Holder HD. The relationship of outlet densities to alcohol consumption: a time series cross-sectional analysis. Alcohol Clin Exp Res. 1993;17:38–47. doi: 10.1111/j.1530-0277.1993.tb00723.x. [DOI] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, et al. Race/ethnicity, gender, and monitoring socioeconomic gradients in health: a comparison of area-based socioeconomic measures—the public health disparities geocoding project. Am J Public Health. 2003;93:1655–71. doi: 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laibson D. A cue-theory of consumption. Quart J Econ. 2001;116:81–119. [Google Scholar]
- Livingston M, Chikritzhs T, Room R. Changing the density of alcohol outlets to reduce alcohol-related problems. Drug Alcohol Rev. 2007;26:557–66. doi: 10.1080/09595230701499191. [DOI] [PubMed] [Google Scholar]
- Mackinnon DP, Scribner R, Taft KA. Development and applications of a city-level alcohol availability and alcohol problems database. Stat Med. 1995;14:591–604. doi: 10.1002/sim.4780140517. [DOI] [PubMed] [Google Scholar]
- Morenoff J. Neighborhood mechanisms and the spatial dynamics of birth weight. Am J Sociol. 2003;108:976–1017. doi: 10.1086/374405. [DOI] [PubMed] [Google Scholar]
- Parker RN. Alcohol and violence: connections, evidence and possibilities for prevention. J Psychoactive Drugs. 2004;157:157–63. doi: 10.1080/02791072.2004.10400051. [DOI] [PubMed] [Google Scholar]
- Sampson R, Morenoff J. Spatial (Dis) advantage and homicide in Chicago neighborhoods. In: Goodchild M, Janelle D, editors. Spatially Integrated Social Science. New York, NY: Oxford University Press; 2004. [Google Scholar]
- Schonlau M, Scribner R, Farley TA, et al. Alcohol outlet density and alcohol consumption in Los Angeles County and Southern Louisiana. GeoSpatial Health. 2008;3:91–101. doi: 10.4081/gh.2008.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scribner RA, Cohen DA, Farley TA. A geographic relation between alcohol availability and gonorrhea rates. Sex Transm Dis. 1998;25:544–8. doi: 10.1097/00007435-199811000-00009. [DOI] [PubMed] [Google Scholar]
- Scribner RA, Cohen DA, Fisher W. Evidence of a structural effect for alcohol outlet density: a multilevel analysis. Alcohol Clin Exp Res. 2000;24:188–95. [PubMed] [Google Scholar]
- Scribner RA, Cohen DA, Kaplan S. Alcohol availability and homicide in New Orleans: conceptual considerations for small area analysis of the effect of alcohol outlet density. J Stud Alcohol. 1999;60:310–6. doi: 10.15288/jsa.1999.60.310. [DOI] [PubMed] [Google Scholar]
- Scribner RA, Mackinnon DP, Dwyer JH. Alcohol outlet density and motor vehicle crashes in Los Angeles County cities. J Stud Alcohol. 1994;55:447–53. doi: 10.15288/jsa.1994.55.447. [DOI] [PubMed] [Google Scholar]
- Scribner RA, Mackinnon DP, Dwyer JH. The risk of assaultive violence and alcohol availability in Los Angeles County. Am J Public Health. 1995;85:335–40. doi: 10.2105/ajph.85.3.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scribner R, Theall KP, Ghosh-Dastidar B, et al. Structural determinants of social capital at the neighborhood level: a longitudinal analysis of loss of alcohol outlets and voting. J Stud Alcohol Drugs. 2007;68:934–43. doi: 10.15288/jsad.2007.68.934. [DOI] [PubMed] [Google Scholar]
- Snijders T, Boskers R. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. London: Sage; 1999. [Google Scholar]
- Theall K, Scribner R, Cohen D, et al. Social capital and the neighborhood alcohol environment. Health Place. 2009;15:323–32. doi: 10.1016/j.healthplace.2008.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treno AJ, Gruenewald PJ, Ponicki WR. Use of ICD-9-CM codes in the estimation of alcohol-involved injury: search for a surrogate II. Alcohol Clin Exp Res. 1996;20:320–6. doi: 10.1111/j.1530-0277.1996.tb01646.x. [DOI] [PubMed] [Google Scholar]
- Williams DR. Smelser NJ, Wilson WJ, Mitchell F, editors. Racial variations in adult health status: patterns, paradoxes, and prospects. America Becoming: Racial Trends and Their Consequences. 2001 National Research Council (U.S.). Commission on Behavioral and Social Sciences and Education. [Google Scholar]
- Zhu L, Gorman DM, Horel S. Alcohol outlet density and violence: a geospatial analysis. Alcohol Alcohol. 2004;39:369–75. doi: 10.1093/alcalc/agh062. [DOI] [PubMed] [Google Scholar]
- Zhu L, Gorman DM, Horel S. Hierarchical Bayesian spatial models for alcohol availability, drug “hot spots” and violent crime. Int J Health Geogr. 2006;5:54. doi: 10.1186/1476-072X-5-54. [DOI] [PMC free article] [PubMed] [Google Scholar]