Abstract
The authors examined the joint associations of adiposity (assessed by body mass index (BMI; weight (kg)/height (m)2) and waist circumference) and physical activity with mortality to evaluate whether physical activity protects against the adverse effects of high adiposity. Using data on 185,412 men and women aged 51–72 years participating in the National Institutes of Health-AARP Diet and Health Study, the authors assessed all-cause mortality over 10 years (1996–2006). Overweight (BMI 25–<30), obesity (BMI ≥30), a large waist circumference (men: ≥102 cm; women: ≥88 cm), and low physical activity were each independent predictors of mortality. Compared with normal-weight persons (BMI 18.5–<25) who were physically active (>7 hours/week of moderate physical activity), mortality risks were 1.62 (95% confidence interval (CI): 1.50, 1.75) for inactive normal-weight persons, 1.79 (95% CI: 1.37, 2.33) for active morbidly obese (BMI ≥35) persons, and 3.45 (95% CI: 2.79, 4.00) for inactive morbidly obese persons. Similar results were found for the combined relation of BMI and vigorous physical activity. Inactive persons with a large waist circumference had 2 times’ greater mortality risk than active persons with a normal waist circumference. High physical activity attenuated but did not eliminate the increased mortality risk associated with obesity. Preventing weight gain and promoting physical activity in older persons may lower mortality risk.
Keywords: abdominal fat, adiposity, body fat distribution, body mass index, exercise, mortality, motor activity
High adiposity and physical inactivity are important health risk factors. Recent epidemiologic studies (1–9) of the independent and joint relations of adiposity and physical activity to mortality show that the combination of obesity and physical inactivity or lack of fitness entails a greater mortality risk than does each factor operating alone. Reports from the Aerobics Center Longitudinal Study suggested that a higher cardiorespiratory fitness level eliminated the increased mortality risk in obese persons (2, 6–9), whereas other studies found that physical activity attenuated but did not eliminate the increased mortality risk in obese persons (3–5).
Most previous analyses of adiposity and mortality (1, 2, 4, 5) have focused on body mass index (BMI) as an indicator of overall adiposity, without considering specific measures of body fat distribution. However, anthropometric studies have shown that a high level of abdominal fat is a risk factor for several chronic diseases, independently of total body fat (10–12). Furthermore, studies have demonstrated that a large waist circumference is a strong predictor of mortality (13–15). In a recent study, Katzmarzyk et al. (16) found that physical inactivity and a large waist circumference were independent risk factors for premature mortality among women. Data regarding the joint relations of central adiposity and physical activity to mortality are sparse (7).
Using data from the National Institutes of Health-AARP Diet and Health Study, a large cohort study of older adults, we examined the joint associations of adiposity and physical activity with mortality to evaluate whether physical activity protects against the adverse effects of high adiposity. Few studies have examined the effect of combined associations of adiposity and physical activity on mortality in older adults. We considered both BMI and waist circumference as measures of adiposity.
MATERIALS AND METHODS
Study population
The National Institutes of Health-AARP (formerly known as the American Association of Retired Persons) Diet and Health Study was initiated in 1995–1996 when an extensive baseline questionnaire was mailed to 3.5 million AARP members aged 50–71 years who resided in 1 of 6 US states (California, Florida, Louisiana, New Jersey, North Carolina, and Pennsylvania) or 2 US metropolitan areas (Atlanta, Georgia, and Detroit, Michigan) (17). Out of 617,119 questionnaires returned (17.6%), 567,169 (16.2%) were satisfactorily completed. In 1996–1997, a second questionnaire was sent to participants who successfully completed the baseline questionnaire to collect additional information on diet, family history of cancer, anthropometric factors (including waist circumference and body weight at age 50 years), physical activity, and use of menopausal hormone therapy. A total of 238,866 respondents successfully completed the second questionnaire and had full data on waist circumference, BMI, and physical activity.
Since data on waist circumference and more detailed information on physical activity were first reported on the second questionnaire, respondents to the second questionnaire represented the cohort of eligible study participants for the current analysis. We excluded persons with a waist circumference less than 60 cm (n = 549) and those with a BMI less than 18.5 or higher than 60 (n = 5,336). We further excluded persons who reported cancer, cardiovascular disease, or emphysema (n = 47,569). This resulted in an analytic cohort of 185,412 participants.
The National Institutes of Health-AARP Study was approved by the Special Studies Institutional Review Board of the National Cancer Institute.
Measures
Mortality.
From 1996–1997 through December 31, 2006, vital status was determined by annual linkage of cohort members to the Social Security Administration Death Master File (18) and follow-up searches of the National Death Index. We estimate that follow-up for deaths in our cohort was more than 93% complete (19, 20).
Body mass index.
Current height was reported in feet and inches, and weight at age 50 years was reported to the nearest pound. We used weight at age 50 years as the basis for calculating BMI because previous research in our cohort showed that it was more strongly and more linearly associated with mortality than was BMI derived from current weight (21). BMI was calculated as weight in kilograms divided by height in meters squared and was divided into 4 categories: 18.5–<25 (normal-weight), 25–<30 (overweight), 30–<35 (obese), and ≥35 (morbidly obese).
Waist circumference.
Using a pictured instruction, participants were requested to measure their waist with a tape measure 1 inch (25.4 mm) above the navel while standing and to report values to the nearest quarter inch (6.4 mm). Four categories of waist circumference were created: group 1—men <94 cm, women <80 cm; group 2—men 94–<102 cm, women 80–<88 cm; group 3—men 102–<110 cm, women 88–<96 cm; and group 4—men ≥110 cm, women ≥96 cm. The first 3 categories were in accordance with the previously used “action levels” of waist circumference (10), where category 1 was considered a normal waist circumference, category 2 as action level 1, and category 3 as action level 2. Thirty-one percent of our study population had a waist circumference above action level 2; therefore, we created an additional (fourth) category to classify people with a more extreme waist circumference.
Physical activity.
Moderate-to-vigorous physical activity was assessed by means of a question on the second questionnaire about the average amount of time spent each week in activities involving at least moderate exertion, with the following response options: weekly but less than 1 hour per week; 1–3 hours per week; 4–7 hours per week; and more than 7 hours per week. Examples of moderate activity were brisk walking/fast dancing, walking during golf, hiking/mountain climbing, cheerleading/drill team, tennis, biking, swimming, aerobics, jogging/running, rowing, basketball/baseball, football/soccer, handball/racquetball, weight lifting, heavy gardening, and heavy housework.
Vigorous physical activity was assessed by means of a question on the baseline questionnaire about how often a person had participated in physical activities at work or at home (including exercise, sports, and activities such as carrying heavy loads for at least 20 minutes) that caused increases in breathing, increases in heart rate, or sweating during a typical month in the past 12 months. Categories of vigorous physical activity were never, rarely, 1–3 times per month, 1–2 times per week, 3–4 times per week, and 5 or more times per week.
Covariates.
Sociodemographic variables included age, sex, and race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, Asian, and Pacific Islander or American Indian). Categories of education were 11 years or less, 12 years or completion of high school, post-high-school study or some college, college graduation, and postgraduate study. Smoking status was categorized in 4 groups as never smoker, former smoker who had stopped smoking 10 or more years previously, former smoker who had stopped smoking less than 10 years previously, and current smoker. Alcohol consumption over the past 12 months was assessed as part of a food frequency questionnaire (17). From total alcohol intake in grams per day, 4 categories were created: 0, >0–<5, 5–<15, and ≥15 g/day.
Statistical analysis
Age-standardized mortality rates were calculated and were standardized to the age distribution of the cohort in men and women using 5-year age categories. We fitted Cox proportional hazards models to estimate individual and joint hazard ratios for the effects of the relation between BMI and physical activity and the relation between waist circumference and physical activity on time to death. Analyses were adjusted for age, sex, race/ethnicity, education, smoking status, and alcohol consumption. The analyses of the joint effects of waist circumference and physical activity were additionally adjusted for BMI. The reference group consisted of men and women with the highest physical activity level and a normal BMI or a normal waist circumference. Because smoking is related to lower body weight and increased mortality, we also examined the joint relations of adiposity and physical activity among never smokers. We investigated the proportional hazards assumption by testing the constancy of the log hazard ratio over time by means of log-minus-log survival plots; according to the test, the proportional hazards assumption was not violated. Analyses were performed using SPSS, version 15.0 (SPSS Inc., Chicago, Illinois).
RESULTS
During 10 years of follow-up, 10,948 men and 4,615 women died. Table 1 shows the baseline characteristics of the study population according to BMI, waist circumference, and moderate and vigorous physical activity. Persons with the highest BMI or the largest waist circumference had a lower educational level, were less physically active, were less likely to currently smoke, and had a lower alcohol intake than persons with a normal BMI (18.5–<25) or a normal waist circumference (category 1). Inactive persons had a lower educational level, were more likely to currently smoke, and had a lower alcohol intake than persons with higher moderate or vigorous physical activity levels.
Table 1.
Baseline Characteristics of Study Participants According to Body Mass Index, Waist Circumference, and Physical Activity Level (n = 185,412), National Institutes of Health-AARP Diet and Health Study, 1996–2006
| No. of Subjects | Mean Age, years | Non-Hispanic White Race/Ethnicity, % | College or Postgraduate Education, % | Mean Body Mass Indexa | Mean Waist Circumference, cm | Inactiveb, % | Current Smoker, % | Alcohol Intake ≥15 g/day, % | |
| Body mass index at age 50 years | |||||||||
| 18.5–<25 | 94,307 | 63.0 (5.2)c | 93.8 | 45.8 | 22.6 (1.5) | 85.5 (10.7) | 4.0 | 11.8 | 23.0 |
| 25–<30 | 71,131 | 62.4 (5.3) | 93.2 | 44.4 | 26.9 (1.4) | 97.6 (9.9) | 5.0 | 8.8 | 24.9 |
| 30–<35 | 15,415 | 61.0 (5.4) | 92.7 | 39.1 | 31.9 (1.4) | 106.9 (11.8) | 8.4 | 8.6 | 18.4 |
| ≥35 | 4,559 | 59.8 (5.3) | 91.5 | 35.0 | 38.9 (4.0) | 115.2 (15.6) | 15.0 | 7.6 | 10.4 |
| Waist circumference categoryd | |||||||||
| 1 | 78,582 | 62.2 (5.4) | 92.7 | 47.8 | 23.4 (2.5) | 82.7 (8.8) | 3.2 | 11.7 | 24.1 |
| 2 | 49,414 | 62.9 (5.3) | 93.8 | 44.2 | 25.4 (2.9) | 93.0 (7.4) | 4.3 | 9.5 | 24.2 |
| 3 | 29,722 | 63.0 (5.2) | 94.2 | 42.3 | 26.8 (3.3) | 100.4 (7.4) | 6.0 | 9.0 | 23.0 |
| 4 | 27,694 | 62.5 (5.3) | 94.0 | 37.6 | 29.7 (5.0) | 111.8 (10.5) | 10.3 | 9.0 | 18.3 |
| Moderate physical activity, hours/week | |||||||||
| >7 | 47,708 | 63.0 (5.2) | 94.3 | 42.9 | 24.8 (3.4) | 89.7 (12.3) | 8.7 | 25.5 | |
| 4–7 | 49,826 | 62.6 (5.3) | 94.1 | 47.6 | 25.1 (3.5) | 91.3 (12.7) | 9.1 | 23.8 | |
| 1–3 | 46,867 | 62.3 (5.4) | 93.4 | 45.6 | 25.6 (3.9) | 93.4 (13.2) | 10.6 | 21.9 | |
| <1 | 18,669 | 62.1 (5.4) | 92.1 | 42.7 | 26.1 (4.3) | 95.6 (13.9) | 11.9 | 20.7 | |
| Inactive | 22,342 | 62.4 (5.4) | 91.4 | 39.3 | 26.6 (4.8) | 97.4 (14.9) | 14.2 | 20.6 | |
| Vigorous physical activity, times/week | |||||||||
| ≥5 | 39,378 | 63.0 (5.2) | 93.9 | 47.9 | 24.9 (3.5) | 90.1 (12.4) | 6.7 | 25.4 | |
| 3–4 | 53,819 | 62.8 (5.3) | 93.5 | 48.2 | 25.1 (3.5) | 91.5 (12.7) | 7.6 | 23.9 | |
| 1–2 | 41,513 | 62.2 (5.3) | 93.9 | 45.2 | 25.5 (3.8) | 93.5 (13.2) | 11.1 | 22.8 | |
| <1 | 24,466 | 61.9 (5.4) | 93.7 | 41.9 | 25.9 (4.1) | 94.7 (13.9) | 13.6 | 21.4 | |
| Inactive | 26,236 | 62.5 (5.3) | 91.6 | 32.6 | 26.2 (4.8) | 95.4 (15.0) | 16.7 | 19.8 |
Weight (kg)/height (m)2.
Inactive for both moderate and vigorous physical activity.
Numbers in parentheses, standard deviation.
Group 1: men <94 cm, women <80 cm; group 2: men 94–<102 cm, women 80–<88 cm; group 3: men 102–<110 cm, women 88–<96 cm; group 4: men ≥110 cm, women ≥96 cm.
In comparison with a normal weight, overweight (BMI 25–<30; hazard ratio (HR) = 1.08, 95% confidence interval (CI): 1.05, 1.12), obesity (BMI 30–<35; HR = 1.48, 95% CI: 1.40, 1.57), and morbid obesity (BMI ≥35; HR = 2.08, 95% CI: 1.91, 2.27) were associated with significantly greater mortality risk (Table 2). Persons with a waist circumference in the third (HR = 1.09, 95% CI: 1.04, 1.14) or fourth (HR = 1.47, 95% CI: 1.40, 1.53) category had a significantly greater mortality risk than persons with a normal waist circumference. Low moderate and vigorous physical activity levels were independent risk factors for mortality. Inactive persons had a more than 50% greater mortality risk than the most active persons.
Table 2.
Mortality Ratesa and Hazard Ratiosb for Mortality According to Body Mass Index, Waist Circumference, and Physical Activity (n = 185,412), National Institutes of Health-AARP Diet and Health Study, 1996–2006
| Person-Years of Follow-Up | No. of Deaths | Mortality Rate | Hazard Ratio | 95% Confidence Interval | P Value From Trend Test | |
| Body mass indexc at age 50 yearsd | <0.01 | |||||
| 18.5–<25 | 919,713 | 7,302 | 792 | 1.00 | Referent | |
| 25–<30 | 690,634 | 6,110 | 932 | 1.08 | 1.05, 1.12 | |
| 30–<35 | 148,482 | 1,598 | 1,287 | 1.48 | 1.40, 1.57 | |
| ≥35 | 43,620 | 553 | 1,676 | 2.08 | 1.91, 2.27 | |
| Waist circumference categoryde | <0.01 | |||||
| 1 | 767,082 | 5,845 | 812 | 1.00 | Referent | |
| 2 | 480,615 | 3,981 | 839 | 1.02 | 0.98, 1.06 | |
| 3 | 288,497 | 2,615 | 912 | 1.09 | 1.04, 1.14 | |
| 4 | 266,254 | 3,122 | 1,220 | 1.47 | 1.40, 1.53 | |
| Moderate physical activity, hours/weekf | <0.01 | |||||
| ≥7 | 466,369 | 3,445 | 741 | 1.00 | Referent | |
| 4–7 | 485,946 | 3,839 | 822 | 1.11 | 1.06, 1.16 | |
| 1–3 | 455,798 | 3,869 | 905 | 1.18 | 1.13, 1.24 | |
| <1 | 180,796 | 1,727 | 1,042 | 1.30 | 1.22, 1.37 | |
| Inactive | 213,540 | 2,683 | 1,327 | 1.54 | 1.46, 1.62 | |
| Vigorous physical activity, times/weekf | <0.01 | |||||
| ≥5 | 384,706 | 2,852 | 746 | 1.00 | Referent | |
| 3–4 | 525,965 | 4,005 | 775 | 1.04 | 0.99, 1.09 | |
| 1–2 | 403,721 | 3,413 | 907 | 1.15 | 1.09, 1.21 | |
| <1 | 237,415 | 2,135 | 997 | 1.21 | 1.14, 1.28 | |
| Inactive | 250,641 | 3,158 | 1,323 | 1.55 | 1.47, 1.63 |
Age-standardized mortality rate per 100,000 person-years, standardized to the age distribution of the cohort in men and women.
Adjusted for age, race/ethnicity, education, smoking status, physical activity, and alcohol consumption.
Weight (kg)/height (m)2.
Adjusted for moderate physical activity.
Group 1: men <94 cm, women <80 cm; group 2: men 94–<102 cm, women 80–<88 cm; group 3: men 102–<110 cm, women 88–<96 cm; group 4: men ≥110 cm, women ≥96 cm.
Adjusted for body mass index.
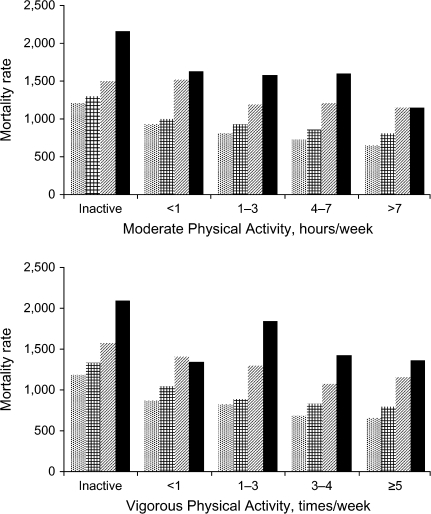
The increased risks of mortality conferred by excess adiposity were similar among both physically active and inactive persons; no significant interactions were observed (all P’s > 0.10). The joint relations of BMI and physical activity and waist circumference and physical activity are shown in Tables 3 and 4 and Figures 1 and 2. Interactions with sex were not statistically significant (all P’s > 0.10); therefore, all results are shown for men and women combined. In each BMI group, mortality rates increased with decreasing levels of physical activity. Likewise, in each physical activity group, mortality rates rose with increasing BMI levels (Figure 1), and we did not see an attenuation of the effect of obesity by physical activity. Compared with persons with a combination of normal BMI and more than 7 hours per week of moderate physical activity, mortality risk was significantly increased in groups with lower physical activity levels within the same BMI range (Table 3). The greatest risk was observed in inactive persons (HR = 1.62, 95% CI: 1.50, 1.75). In the most active group (>7 hours/week), mortality risks were significantly higher in overweight and obese persons, with the highest risk being seen in morbidly obese persons (BMI ≥35; HR = 1.79, 95% CI: 1.37, 2.33). Inactive morbidly obese persons had a particularly high mortality risk (HR = 3.45, 95% CI: 2.97, 4.00).
Table 3.
Mortality Ratesa and Hazard Ratiosb for Mortality According to the Combination of Body Mass Index and Moderate Physical Activity and the Combination of Waist Circumference and Moderate Physical Activity (n = 185,412), National Institutes of Health-AARP Diet and Health Study, 1996–2006
| Moderate Physical Activity, hours/week |
|||||||||||||||
| >7 |
4–7 |
1–3 |
<1 |
Inactive |
|||||||||||
| MR | HR | 95% CI | MR | HR | 95% CI | MR | HR | 95% CI | MR | HR | 95% CI | MR | HR | 95% CI | |
| Body mass indexc at age 50 years | |||||||||||||||
| 18.5–<25 | 653 | 1.00 | Referent | 735 | 1.14 | 1.07, 1.21 | 815 | 1.22 | 1.14, 1.30 | 935 | 1.33 | 1.22, 1.45 | 1,206 | 1.62 | 1.50, 1.75 |
| 25–<30 | 806 | 1.15 | 1.07, 1.23 | 864 | 1.23 | 1.15, 1.32 | 928 | 1.31 | 1.22, 1.40 | 996 | 1.39 | 1.27, 1.52 | 1,303 | 1.71 | 1.58, 1.85 |
| 30–<35 | 1,151 | 1.62 | 1.42, 1.84 | 1,211 | 1.73 | 1.53, 1.95 | 1,187 | 1.76 | 1.57, 1.96 | 1,523 | 2.16 | 1.89, 2.47 | 1,505 | 2.12 | 1.89, 2.38 |
| ≥35 | 1,149 | 1.79 | 1.37, 2.33 | 1,601 | 2.45 | 1.98, 3.04 | 1,583 | 2.49 | 2.08, 2.98 | 1,631 | 2.75 | 2.20, 3.44 | 2,158 | 3.45 | 2.97, 4.00 |
| Waist circumference categoryd | |||||||||||||||
| 1 | 684 | 1.00 | Referent | 756 | 1.11 | 1.04, 1.19 | 853 | 1.20 | 1.12, 1.29 | 977 | 1.28 | 1.16, 1.42 | 1,303 | 1.61 | 1.48, 1.76 |
| 2 | 734 | 1.10 | 1.00, 1.21 | 759 | 1.15 | 1.05, 1.27 | 828 | 1.22 | 1.11, 1.35 | 961 | 1.36 | 1.21, 1.54 | 1,225 | 1.64 | 1.47, 1.83 |
| 3 | 782 | 1.15 | 1.00, 1.32 | 888 | 1.33 | 1.17, 1.51 | 885 | 1.31 | 1.16, 1.49 | 990 | 1.44 | 1.24, 1.67 | 1,154 | 1.59 | 1.39, 1.83 |
| 4 | 999 | 1.44 | 1.23, 1.68 | 1,097 | 1.55 | 1.34, 1.80 | 1,156 | 1.62 | 1.41, 1.87 | 1,283 | 1.75 | 1.50, 2.04 | 1,561 | 2.01 | 1.74, 2.32 |
Abbreviations: CI, confidence interval; HR, hazard ratio; MR, mortality rate.
Age-standardized mortality rate per 100,000 person-years, standardized to the age distribution of the cohort in men and women.
Adjusted for sex, age, race/ethnicity, education, smoking status, and alcohol consumption.
Weight (kg)/height (m)2.
Group 1: men <94 cm, women <80 cm; group 2: men 94–<102 cm, women 80–<88 cm; group 3: men 102–<110 cm, women 88–<96 cm; group 4: men ≥110 cm, women ≥96 cm. Results were additionally adjusted for body mass index.
Table 4.
Mortality Ratesa and Hazard Ratiosb for Mortality According to the Combination of Body Mass Index and Vigorous Physical Activity and the Combination of Waist Circumference and Vigorous Physical Activity (n = 185,412), National Institutes of Health-AARP Diet and Health Study, 1996–2006
| Vigorous Physical Activity, times/week |
|||||||||||||||
| ≥5 |
3–4 |
1–2 |
<1 |
Inactive |
|||||||||||
| MR | HR | 95% CI | MR | HR | 95% CI | MR | HR | 95% CI | MR | HR | 95% CI | MR | HR | 95% CI | |
| Body mass indexc at age 50 years | |||||||||||||||
| 18.5–<25 | 658 | 1.00 | Referent | 684 | 1.04 | 0.97, 1.11 | 826 | 1.18 | 1.10, 1.27 | 870 | 1.20 | 1.10, 1.30 | 1,189 | 1.56 | 1.45, 1.68 |
| 25–<30 | 794 | 1.09 | 1.01, 1.18 | 831 | 1.15 | 1.07, 1.23 | 893 | 1.21 | 1.12, 1.30 | 1,042 | 1.34 | 1.23, 1.46 | 1,334 | 1.73 | 1.60, 1.87 |
| 30–<35 | 1,155 | 1.59 | 1.39, 1.83 | 1,072 | 1.53 | 1.35, 1.72 | 1,294 | 1.79 | 1.59, 2.00 | 1,403 | 1.89 | 1.66, 2.15 | 1,571 | 2.12 | 1.89, 2.37 |
| ≥35 | 1,358 | 2.00 | 1.55, 2.59 | 1,426 | 2.14 | 1.74, 2.64 | 1,839 | 2.76 | 2.30, 3.32 | 1,347 | 2.09 | 1.64, 2.65 | 2,093 | 3.38 | 2.91, 3.91 |
| Waist circumference categoryd | |||||||||||||||
| 1 | 684 | 1.00 | Referent | 705 | 1.03 | 0.96, 1.11 | 869 | 1.18 | 1.09, 1.27 | 917 | 1.19 | 1.09, 1.31 | 1,315 | 1.60 | 1.47, 1.74 |
| 2 | 707 | 1.04 | 0.95, 1.14 | 746 | 1.11 | 1.02, 1.20 | 830 | 1.19 | 1.09, 1.30 | 976 | 1.34 | 1.21, 1.48 | 1,176 | 1.58 | 1.44, 1.73 |
| 3 | 819 | 1.19 | 1.06, 1.33 | 806 | 1.19 | 1.08, 1.31 | 889 | 1.27 | 1.15, 1.41 | 948 | 1.32 | 1.18, 1.49 | 1,197 | 1.66 | 1.49, 1.84 |
| 4 | 1,085 | 1.50 | 1.33, 1.70 | 1,049 | 1.48 | 1.33, 1.64 | 1,141 | 1.56 | 1.41, 1.73 | 1,183 | 1.54 | 1.37, 1.72 | 1,557 | 2.03 | 1.85, 2.24 |
Abbreviations: CI, confidence interval; HR, hazard ratio; MR, mortality rate.
Age-standardized mortality rate per 100,000 person-years, standardized to the age distribution of the cohort in men and women.
Adjusted for sex, age, race/ethnicity, education, smoking status, and alcohol consumption.
Weight (kg)/height (m)2.
Group 1: men <94 cm, women <80 cm; group 2: men 94–<102 cm, women 80–<88 cm; group 3: men 102–<110 cm, women 88–<96 cm; group 4: men ≥110 cm, women ≥96 cm. Results were additionally adjusted for body mass index.
Figure 1.
Age-standardized mortality rate per 100,000 person-years (standardized to the age distribution of the cohort in men and women) according to the combination of body mass index (weight (kg)/height (m)2) and moderate and vigorous physical activity, National Institutes of Health-AARP Diet and Health Study, 1996–2006. Body mass index categories:  , 18.5–<25 (normal-weight);
, 18.5–<25 (normal-weight);  , 25–<30 (overweight);
, 25–<30 (overweight);  , 30–<35 (obese);
, 30–<35 (obese);  , ≥35 (morbidly obese).
, ≥35 (morbidly obese).
Figure 2.
Age-standardized mortality rate per 100,000 person-years (standardized to the age distribution of the cohort in men and women) according to the combination of waist circumference and moderate and vigorous physical activity, National Institutes of Health-AARP Diet and Health Study, 1996–2006. Waist circumference categories:  , group 1 (men <94 cm, women <80 cm);
, group 1 (men <94 cm, women <80 cm);  , group 2 (men 94–<102 cm, women 80–<88 cm);
, group 2 (men 94–<102 cm, women 80–<88 cm);  , group 3 (men 102–<110 cm, women 88–<96 cm);
, group 3 (men 102–<110 cm, women 88–<96 cm);  , group 4 (men ≥110 cm, women ≥96 cm).
, group 4 (men ≥110 cm, women ≥96 cm).
We also examined the joint relations of adiposity and physical activity among never smokers (data not tabulated). In never smokers, the BMI gradient among the most active persons was particularly strong. Compared with active normal-weight persons, active obese persons had a 2 times’ higher mortality risk (HR = 2.05, 95% CI: 1.61, 2.60) and active morbidly obese persons had a more than 3 times’ greater mortality risk (HR = 3.25, 95% CI: 2.16, 4.94). A similar pattern was found for the combination of BMI and vigorous physical activity in relation to risk of mortality.
In comparison with the most active persons with a normal waist circumference, mortality risk rose with increasing waist circumference as well as with decreasing physical activity levels (Tables 3 and 4, Figure 2). Inactive persons with a normal waist circumference had a similarly increased mortality risk (HR = 1.61, 95% CI: 1.48, 1.76) as the most active persons with the largest waist circumference (HR = 1.44, 95% CI: 1.23, 1.68) (Table 3). The highest mortality risk was found among persons with the largest waist circumference who were physically inactive (HR = 2.01, 95% CI: 1.74, 2.32), as compared with active persons with a normal waist circumference. Similar patterns were found in never smokers and for the combined relations of waist circumference and vigorous physical activity.
DISCUSSION
In this large prospective cohort study of older adults, overweight (BMI 25–<30), obesity (BMI ≥30), a large waist circumference, and low physical activity levels were each independent predictors of mortality. The increased risks of mortality conferred by excess weight or a large waist circumference were similar among both physically active and inactive persons. Compared with active normal-weight persons, inactive normal-weight persons had a similarly high mortality risk as active obese persons. The highest mortality risks were found among inactive morbidly obese persons, who had a 3.5 times’ higher mortality risk. Inactive persons with a large waist circumference had a mortality risk 2 times higher than that of active persons with a normal waist circumference.
In the Aerobics Center Longitudinal Study, greater cardiorespiratory fitness was a more important predictor of mortality than was BMI, suggesting that higher fitness eliminates the increased mortality risk in obese persons (2, 6–9). In other studies, however, investigators reported that high physical activity levels attenuated but did not eliminate the increased mortality risk associated with obesity. For example, in a large cohort of women aged 30–55 years participating in the Nurses’ Health Study, increased adiposity and reduced physical activity were strong independent predictors of death, and high levels of physical activity did not eliminate the excess mortality associated with obesity (3). In another study, Stevens et al. (5) did not find a significant interaction between fitness and fatness in Russian or American men for all-cause mortality. A large study in middle-aged Finnish men and women showed that regular physical activity and normal weight were both important indicators for decreased risk of mortality (4).
To our knowledge, our study is by far the largest study to have examined the joint relations of adiposity and physical activity with mortality risk in both men and women, and it does not support the hypothesis that physical activity protects against the apparent adverse effects of obesity. Cardiorespiratory fitness was not assessed in the present study. However, physical activity is the primary determinant of fitness that is modifiable. Persons who regularly engage in moderate physical activity can attain a fitness level sufficient to result in important and substantial health benefits (22). We found a strong mortality gradient with increasing BMI in all physical activity groups. Morbidly obese people who were physically active had an approximately 2 times’ higher mortality risk than their normal-weight counterparts. Additionally, equally high mortality risks were found in active obese persons and inactive normal-weight persons.
The joint relations of waist circumference and physical activity with mortality risk have not been studied extensively (7). We previously showed that a large waist circumference was associated with increased mortality risk, independently of BMI (15). In the present study we also adjusted for BMI, so the effect of waist circumference across physical activity groups was independent of total adiposity. This suggests that a large waist circumference should be considered a risk factor for mortality, in addition to BMI. We excluded persons with chronic disease at baseline in order to minimize the potential effect of disease on adiposity and physical activity levels. Because smoking is associated with lower body weight and an increased mortality risk, we also examined the results in never smokers only. In never smokers, the BMI gradient was stronger in the more physically active groups.
Promoting regular physical activity may lower all-cause mortality rates in both obese and nonobese older adults. The finding that mortality risks were greater in obese persons than in normal-weight persons regardless of physical activity level suggests that preventing weight gain or weight loss may also lower mortality risk. However, losing weight may also have unintended negative health consequences, such as the loss of muscle mass or loss of bone (23, 24). While involuntary weight loss has been associated with increased mortality risk in older persons, voluntary weight loss has been associated with positive effects on physical functioning, cardiovascular disease risk, and diabetes risk (25–27). Rather than focusing only on weight loss, interventions focusing on weight loss through the promotion of physical activity may be an effective strategy for lowering mortality risk. An additional beneficial effect of increasing physical activity levels in obese and overweight persons might be the conservation of muscle mass and strength (28, 29).
Some limitations of this study should be considered. Height and weight were self-reported. Self-reported height and weight are generally known to be accurate, although heavy persons are more likely to underreport their weight (30). We used BMI at age 50 years; therefore, we may not have captured acute effects of BMI on mortality. Waist circumference was self-measured by participants. Self-reported waist circumference has been found to be a valid approximation of measured waist circumference (30, 31). For example, in a study carried out among 123 men aged 40–75 years and 140 women aged 41–65 years, Rimm et al. (31) reported crude Pearson coefficients for correlation between self-reported and measured waist circumference of 0.95 for men and 0.89 for women. Physical activity was also assessed by self-report, which may have led to misclassification (32). Validation studies comparing physical activity questionnaires with referent methods suggested that physical activity assessment by questionnaires was reasonably valid and reliable (33).
In conclusion, we found high adiposity and low physical activity to be independent and important risk factors for mortality. High physical activity attenuated but did not eliminate the increased mortality risk associated with obesity. The combination of high adiposity with physical inactivity particularly increased mortality risk. Preventing weight gain and promoting physical activity in both obese and nonobese older persons may lower the risk of death.
Acknowledgments
Author affiliations: Laboratory of Epidemiology, Demography, and Biometry, National Institute on Aging, Bethesda, Maryland (Annemarie Koster, Tamara B. Harris); Faculty of Health, Medicine and Life Sciences, Universiteit Maastricht, Maastricht, the Netherlands (Annemarie Koster, Jacques Th. M. van Eijk); Nutritional Epidemiology Branch, Division of Cancer Epidemiology and Genetics, National Cancer Institute, Bethesda, Maryland (Steven C. Moore, Arthur Schatzkin, Michael F. Leitzmann); Institute of Epidemiology and Preventive Medicine, University of Regensburg, Regensburg, Germany (Michael F. Leitzmann); and AARP, Washington, DC (Albert R. Hollenbeck).
This research was supported partly by the Intramural Research Program of the National Institutes of Health, National Cancer Institute, and partly by the Intramural Research Program of the National Institutes of Health, National Institute on Aging.
Cancer incidence data from the Atlanta, Georgia, metropolitan area were collected by the Georgia Center for Cancer Statistics, Department of Epidemiology, Rollins School of Public Health, Emory University. Cancer incidence data from California were collected by the California Department of Health Services, Cancer Surveillance Section. Cancer incidence data from the Detroit, Michigan, metropolitan area were collected by the Michigan Cancer Surveillance Program, Community Health Administration, State of Michigan. The Florida cancer incidence data used in this report were collected by the Florida Cancer Data System under contract with the Department of Health. (The views expressed herein are solely those of the authors and do not necessarily reflect those of the contractor or the Florida Department of Health.) Cancer incidence data from Louisiana were collected by the Louisiana Tumor Registry, Louisiana State University Medical Center in New Orleans. Cancer incidence data from New Jersey were collected by the New Jersey State Cancer Registry, Cancer Epidemiology Services, New Jersey State Department of Health and Senior Services. Cancer incidence data from North Carolina were collected by the North Carolina Central Cancer Registry. Cancer incidence data from Pennsylvania were supplied by the Division of Health Statistics and Research, Pennsylvania Department of Health. (The Pennsylvania Department of Health specifically disclaims responsibility for any analyses, interpretations, or conclusions.)
Conflict of interest: none declared.
Glossary
Abbreviations
- BMI
body mass index
- CI
confidence interval
- HR
hazard ratio
References
- 1.Katzmarzyk PT, Church TS, Janssen I, et al. Metabolic syndrome, obesity, and mortality: impact of cardiorespiratory fitness. Diabetes Care. 2005;28(2):391–397. doi: 10.2337/diacare.28.2.391. [DOI] [PubMed] [Google Scholar]
- 2.Church TS, LaMonte MJ, Barlow CE, et al. Cardiorespiratory fitness and body mass index as predictors of cardiovascular disease mortality among men with diabetes. Arch Intern Med. 2005;165(18):2114–2120. doi: 10.1001/archinte.165.18.2114. [DOI] [PubMed] [Google Scholar]
- 3.Hu FB, Willett WC, Li T, et al. Adiposity as compared with physical activity in predicting mortality among women. N Engl J Med. 2004;351(26):2694–2703. doi: 10.1056/NEJMoa042135. [DOI] [PubMed] [Google Scholar]
- 4.Hu G, Tuomilehto J, Silventoinen K, et al. The effects of physical activity and body mass index on cardiovascular, cancer and all-cause mortality among 47 212 middle-aged Finnish men and women. Int J Obes (Lond) 2005;29(8):894–902. doi: 10.1038/sj.ijo.0802870. [DOI] [PubMed] [Google Scholar]
- 5.Stevens J, Evenson KR, Thomas O, et al. Associations of fitness and fatness with mortality in Russian and American men in the Lipids Research Clinics Study. Int J Obes Relat Metab Disord. 2004;28(11):1463–1470. doi: 10.1038/sj.ijo.0802770. [DOI] [PubMed] [Google Scholar]
- 6.Lee CD, Blair SN, Jackson AS. Cardiorespiratory fitness, body composition, and all-cause and cardiovascular disease mortality in men. Am J Clin Nutr. 1999;69(3):373–380. doi: 10.1093/ajcn/69.3.373. [DOI] [PubMed] [Google Scholar]
- 7.Sui X, LaMonte MJ, Laditka JN, et al. Cardiorespiratory fitness and adiposity as mortality predictors in older adults. JAMA. 2007;298(21):2507–2516. doi: 10.1001/jama.298.21.2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wei M, Kampert JB, Barlow CE, et al. Relationship between low cardiorespiratory fitness and mortality in normal-weight, overweight, and obese men. JAMA. 1999;282(16):1547–1553. doi: 10.1001/jama.282.16.1547. [DOI] [PubMed] [Google Scholar]
- 9.Farrell SW, Braun L, Barlow CE, et al. The relation of body mass index, cardiorespiratory fitness, and all-cause mortality in women. Obes Res. 2002;10(6):417–423. doi: 10.1038/oby.2002.58. [DOI] [PubMed] [Google Scholar]
- 10.Lean ME, Han TS, Morrison CE. Waist circumference as a measure for indicating need for weight management. BMJ. 1995;311(6998):158–161. doi: 10.1136/bmj.311.6998.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutr. 2004;79(3):379–384. doi: 10.1093/ajcn/79.3.379. [DOI] [PubMed] [Google Scholar]
- 12.Zhu S, Wang Z, Heshka S, et al. Waist circumference and obesity-associated risk factors among whites in the third National Health and Nutrition Examination Survey: clinical action thresholds. Am J Clin Nutr. 2002;76(4):743–749. doi: 10.1093/ajcn/76.4.743. [DOI] [PubMed] [Google Scholar]
- 13.Bigaard J, Tjønneland A, Thomsen BL, et al. Waist circumference, BMI, smoking, and mortality in middle-aged men and women. Obes Res. 2003;11(7):895–903. doi: 10.1038/oby.2003.123. [DOI] [PubMed] [Google Scholar]
- 14.Visscher TL, Seidell JC, Molarius A, et al. A comparison of body mass index, waist-hip ratio and waist circumference as predictors of all-cause mortality among the elderly: The Rotterdam Study. Int J Obes Relat Metab Disord. 2001;25(11):1730–1735. doi: 10.1038/sj.ijo.0801787. [DOI] [PubMed] [Google Scholar]
- 15.Koster A, Leitzmann MF, Schatzkin A, et al. Waist circumference and mortality. Am J Epidemiol. 2008;167(12):1465–1475. doi: 10.1093/aje/kwn079. [DOI] [PubMed] [Google Scholar]
- 16.Katzmarzyk PT, Craig CL. Independent effects of waist circumference and physical activity on all-cause mortality in Canadian women. Appl Physiol Nutr Metab. 2006;31(3):271–276. doi: 10.1139/h05-038. [DOI] [PubMed] [Google Scholar]
- 17.Schatzkin A, Subar AF, Thompson FE, et al. Design and serendipity in establishing a large cohort with wide dietary intake distributions: The National Institutes of Health-American Association of Retired Persons Diet and Health Study. Am J Epidemiol. 2001;154(12):1119–1125. doi: 10.1093/aje/154.12.1119. [DOI] [PubMed] [Google Scholar]
- 18.Hauser TH, Ho KK. Accuracy of on-line databases in determining vital status. J Clin Epidemiol. 2001;54(12):1267–1270. doi: 10.1016/s0895-4356(01)00421-8. [DOI] [PubMed] [Google Scholar]
- 19.Hill ME, Rosenwaike I. The Social Security Administration's Death Master File: the completeness of death reporting at older ages. Soc Secur Bull. 2001-2002;64(1):45–51. [PubMed] [Google Scholar]
- 20.Rich-Edwards JW, Corsano KA, Stampfer MJ. Test of the National Death Index and Equifax Nationwide Death Search. Am J Epidemiol. 1994;140(11):1016–1019. doi: 10.1093/oxfordjournals.aje.a117191. [DOI] [PubMed] [Google Scholar]
- 21.Adams KF, Schatzkin A, Harris TB, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355(8):763–778. doi: 10.1056/NEJMoa055643. [DOI] [PubMed] [Google Scholar]
- 22.Stofan JR, DiPietro L, Davis D, et al. Physical activity patterns associated with cardiorespiratory fitness and reduced mortality: The Aerobics Center Longitudinal Study. Am J Public Health. 1998;88(12):1807–1813. doi: 10.2105/ajph.88.12.1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Newman AB, Lee JS, Visser M, et al. Weight change and the conservation of lean mass in old age: The Health, Aging and Body Composition Study. Am J Clin Nutr. 2005;82(4):872–878. doi: 10.1093/ajcn/82.4.872. [DOI] [PubMed] [Google Scholar]
- 24.Ensrud KE, Ewing SK, Stone KL, et al. Intentional and unintentional weight loss increase bone loss and hip fracture risk in older women. J Am Geriatr Soc. 2003;51(12):1740–1747. doi: 10.1046/j.1532-5415.2003.51558.x. [DOI] [PubMed] [Google Scholar]
- 25.Villareal DT, Apovian CM, Kushner RF, et al. Obesity in older adults: technical review and position statement of the American Society for Nutrition and NAASO, The Obesity Society. Am J Clin Nutr. 2005;82(5):923–934. doi: 10.1093/ajcn/82.5.923. [DOI] [PubMed] [Google Scholar]
- 26.Nicklas BJ, Dennis KE, Berman DM, et al. Lifestyle intervention of hypocaloric dieting and walking reduces abdominal obesity and improves coronary heart disease risk factors in obese, postmenopausal, African-American and Caucasian women. J Gerontol A Biol Sci Med Sci. 2003;58(2):181–189. doi: 10.1093/gerona/58.2.m181. [DOI] [PubMed] [Google Scholar]
- 27.Hamman RF, Wing RR, Edelstein SL, et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care. 2006;29(9):2102–2107. doi: 10.2337/dc06-0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Raguso CA, Kyle U, Kossovsky MP, et al. A 3-year longitudinal study on body composition changes in the elderly: role of physical exercise. Clin Nutr. 2006;25(4):573–580. doi: 10.1016/j.clnu.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 29.Goodpaster BH, Chomentowski P, Ward BK, et al. Effects of physical activity on strength and skeletal muscle fat infiltration in older adults: a randomized controlled trial. J Appl Physiol. 2008;105(5):1498–1503. doi: 10.1152/japplphysiol.90425.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stevens J, Keil JE, Waid LR, et al. Accuracy of current, 4-year, and 28-year self-reported body weight in an elderly population. Am J Epidemiol. 1990;132(6):1156–1163. doi: 10.1093/oxfordjournals.aje.a115758. [DOI] [PubMed] [Google Scholar]
- 31.Rimm EB, Stampfer MJ, Colditz GA, et al. Validity of self-reported waist and hip circumferences in men and women. Epidemiology. 1990;1(6):466–473. doi: 10.1097/00001648-199011000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport. 2000;71(2 suppl):S1–S14. [PubMed] [Google Scholar]
- 33.Pereira MA, FitzerGerald SJ, Gregg EW, et al. A collection of physical activity questionnaires for health-related research. Med Sci Sports Exerc. 1997;29(6 suppl):S1–S205. [PubMed] [Google Scholar]