Abstract
Patient participation is increasingly recognized as a key component in the redesign of health care processes and is advocated as a means to improve patient safety. The concept has been successfully applied to various areas of patient care, such as decision making and the management of chronic diseases. We review the origins of patient participation, discuss the published evidence on its efficacy, and summarize the factors influencing its implementation. Patient-related factors, such as acceptance of the new patient role, lack of medical knowledge, lack of confidence, comorbidity, and various sociodemographic parameters, all affect willingness to participate in the health care process. Among health care workers, the acceptance and promotion of patient participation are influenced by other issues, including the desire to maintain control, lack of time, personal beliefs, type of illness, and training in patient-caregiver relationships. Social status, specialty, ethnic origin, and the stakes involved also influence patient and health care worker acceptance. The London Declaration, endorsed by the World Health Organization World Alliance for Patient Safety, calls for a greater role for patients to improve the safety of health care worldwide. Patient participation in hand hygiene promotion among staff to prevent health care—associated infection is discussed as an illustrative example. A conceptual model including key factors that influence participation and invite patients to contribute to error prevention is proposed. Further research is essential to establish key determinants for the success of patient participation in reducing medical errors and in improving patient safety.
Patient participation is a complex concept and arises from the widespread consumer movement of the 1960s that affirmed the consumer's right to safety, the right to be informed, the right to choose, and the right to be heard.1 During the past few years, patient participation has been increasingly recognized as a key component in the redesign of health care processes and successfully applied to some aspects of patient care, notably the decision-making process and the treatment of chronic illness. Recently, increasing patient participation has been recommended to improve patient safety. The World Health Organization (WHO) World Alliance for Patient Safety is actively highlighting the role that patients and their families could play in the improvement of health care.2 However, this field of patient participation has not been widely researched thus far.
We review the underlying principles and the efficacy of patient participation in decision making and self-treatment of chronic illness, as well as the potential obstacles to implementation. Building on these principles, we develop a conceptual framework for patient participation. Finally, we suggest that patient participation could be useful to improve quality of care and prevent medical errors and propose an agenda for research.
LITERATURE SEARCH
A literature search was conducted from January 1966 through December 2008 in English and French of the MEDLINE, Cochrane Library, and Cumulative Index to Nursing and Allied Health Literature databases using the following Medical Subject Headings' keywords in combination: patient participation, patient involvement, patient education, professional-patient relations, decision-making, informed consent, chronic disease, medical errors, infection control, nosocomial infection, and cross infection. Reference lists of relevant articles were hand searched for additional studies. A systematic search of the grey literature was not conducted. Articles retrieved were critically reviewed by the authors and included as appropriate to provide an overview of the literature on the topic. This article is intended to be a comprehensive summary, rather than a systematic review.
DEFINITIONS
The concept of patient participation remains poorly defined despite abundant literature. No single definition exists, and various terms such as patient collaboration, patient involvement, partnership, patient empowerment, or patient-centered care are used interchangeably. Furthermore, patient participation can relate to aspects of health care as diverse as decision making, self-medication, self-monitoring, patient education, goal setting, or taking part in physical care.3 The US National Library of Medicine defines patient participation as “the involvement of the patient in the decision-making process regarding health issues” (www.ncbi.nlm.nih.gov/mesh). However, this focus on the decision-making process does not include the many and varied aspects of health care in which the patient could participate.4 In this review, we make a distinction between participation in decision making and participation in other aspects of care.
A NEW ROLE FOR THE PATIENT
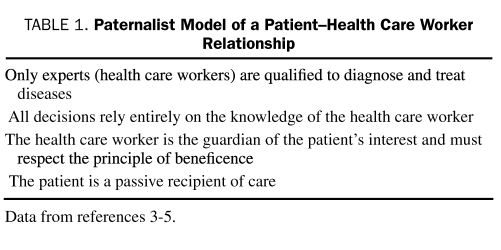
At the center of patient participation resides a redefinition of the patient role. Historically, in many cultures, the relationship between the patient and the health care worker follows a “paternalist” model (Table 1), and the patient has been traditionally a passive spectator in his or her own healing process.5 However, in today's definition of health care, the patient is a key player.5 Several factors have contributed to this change. Humanist considerations state that every human being is endowed with will and with a right to self-determination.6 By participating in the decision-making process, the patient exercises his or her most fundamental rights. Consumerism also contributed to modification of the patient's role in the treatment process.7 Like any consumer, the patient may demand quality services.4,8 By continuously evaluating the service and sometimes lodging complaints toward it, the patient-consumer can improve the health care system.9 This new vision of the patient role is advocated in several official documents of professional medical10,11 and nursing12 bodies and in governmental policies in the United States,13 Australia,14 the Netherlands,15 and the United Kingdom.16,17 In the “Vienna Recommendations on Health Promoting Hospitals” issued in 1997, the WHO recognized the necessity of encouraging an active and participatory role for patients to improve their well-being and increase the efficiency of the health care system.18
TABLE 1.
Paternalist Model of a Patient—Health Care Worker Relationship
PATIENT PARTICIPATION IN DECISION MAKING
Do Patients Want to Participate?
A proportion of patients do not accept the new patient role and refuse to participate in decision making19-21; however, studies diverge as to the exact proportion. In a literature review, it ranged from 48% for women recently diagnosed with breast cancer to 80% for patients with cancer who had been offered an experimental treatment.19 In a representative sample of the US population, 52% of respondents preferred to delegate decision making to their physician.20 However, other studies found a much stronger preference of patients to participate. Among 824 patients waiting to see a general practitioner, 86% expressed the desire to determine the choice of treatment in conjunction with their physician and to establish a therapeutic partnership.22 From these and other studies,23,24 it can be concluded that various factors influence the patient's desire to participate in decision making.
Obstacles to Patient Participation
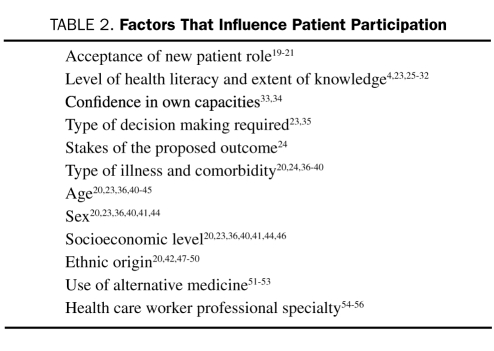
Besides rejection of the new patient role, one of the main obstacles to patient participation is low health literacy and lack of knowledge of the subject (Table 2).4,25 Patients are more likely to be involved in decisions that do not require medical knowledge than those that require clinical expertise.23 Knowledge also confers confidence; patients are more likely to trust their capacity to make decisions when thoroughly informed.33 For example, in a randomized controlled study, participation in therapy for ulcer disease improved with a 20-minute educational session.26 Sessions provided patients with the knowledge necessary for their treatment and encouraged them to actively participate in decision making. They also led to an increased involvement in the patient-physician interaction and fewer limitations imposed by the disease on patients' functional ability. Moreover, patient participation depends on the type of decision to be made. Certain situations (referred to as “problem-solving situations”35) do not present themselves well to patient participation. For example, most patients are not qualified (nor do they desire) to determine whether a radiograph reveals a fracture. In contrast, most “decision-making situations” require an analysis of the value (“utility” in economic parlance) of potential outcomes to the individual, something only the patient can determine, eg, choosing between mastectomy and chemotherapy for breast cancer. Patients instinctively make the distinction between these 2 types of decisions and prefer to be involved in the latter rather than the former.23 The stakes also influence participation. Most patients want to participate in major decision making (eg, whether to undergo coronary bypass) but are less concerned about minor decisions (eg, prescription for bed rest).24
TABLE 2.
Factors That Influence Patient Participation
Disease and comorbidity can limit patient participation. In a study that attempted to measure preferences for participation in decision making, patients were more likely to prefer a passive role compared with their companions.36 The desire to participate in decision making and to be involved in the treatment process is inversely proportional to the patient's disease severity in most,20,37-40 but not all,24 conditions.
Older patients are usually less interested in the decision-making process,20,23,36,40-44 independent of their health status. Nevertheless, evidence shows that even the elderly can participate in their care.45 Studies are divided on the influence of sex on participation; some showed that women wish to participate more,20,36,40,57 but others established no difference.23,24,41
Socioeconomic level influences patient participation, and thus education may play a role.20,23,40,41,44 However, some studies failed to demonstrate such an association.36 In a systematic review of the effect of the socioeconomic level on patient-physician communication,46 physicians modified their interviewing style according to the patient's socioeconomic class. Patients in lower socioeconomic levels were subjected to more directed, less participative medical consultations and were less often invited to build a partnership. Moreover, they were often put at a disadvantage by the practitioner's erroneous belief that they had less need for information and a lower capacity to participate in the decision-making process.
In a study of 2765 patients, African Americans and Hispanic Americans were significantly less inclined to participate in decision making compared with white people.20 Ethnic differences in making end-of-life decisions have been reported. Americans of Korean and Mexican origin were significantly less inclined to believe that the patient should make decisions about the use of life support technology than Americans of European or African origin (28% and 41% vs 60% and 65%, respectively).47 The reason for this disparity is uncertain and may be linked to issues such as language, education, communication style, and autonomy in matters of personal health.42,48-50 Ethnic origin also influences the role that patients will allow their family to have in decision making. Among patients with breast cancer in Los Angeles, 49% of the less culturally adapted Hispanics allowed their family members to determine the final treatment compared with 18% of more acculturated Hispanic patients, and less than 4% of African Americans and white people.58 Japanese and Americans of Japanese origin also tend to leave the decision making to their family.59 Finally, patients who use alternative medicines might be more involved in health care—related decisions,51,52 although these findings lack consistency between studies.53
CAN PATIENTS MODIFY BEHAVIOR OF HEALTH CARE WORKERS?
Evidence shows that patients can be persuasive and substantially modify behavior of health care workers. In an observational study of more than 500 visits to 45 physicians, patients who requested a prescription were almost 3 times more likely to be prescribed a new medication.60 Similarly, those who requested a specialty referral had more than 4 times the odds of receiving a referral. In a randomized trial of patients with major depression, 76% of those who requested an antidepressant received a prescription compared with only 31% of those who did not.57 In obstetrics, 20% of physicians who believed that women have no right to request a cesarean section delivery if not medically required had already allowed the procedure for some patients on direct request.61
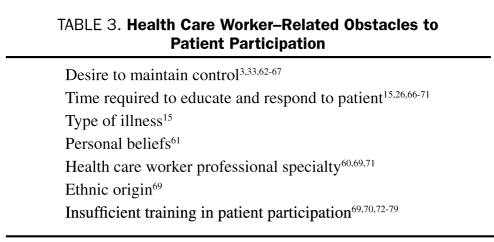
HEALTH CARE WORKERS' OBSTACLES TO PATIENT PARTICIPATION IN DECISION MAKING
Lack of Acceptance of the New Role of Health Care Workers
Health care workers' beliefs, attitudes, and behavior can have a major effect on patient participation (Table 3). One of the main obstacles is refusal of health care workers to abandon their traditional role and to delegate power.3,33 Nurses interviewed by Henderson33 in 1998 conceded unwillingness to share their decision-making power. According to Henderson, many nurses exercise almost absolute power and control over patients and consider them unable to make decisions. This traditional perception is a major barrier to patient participation.62,80 Another example of paternalism is that a significant proportion of nursing students do not consider lying to patients as unprofessional behavior.63 Similarly, physicians are reluctant to encourage patient participation because either they refuse to delegate power or control or they are afraid to lose their identity,64-66 even though they may not be openly negative about the concept.65,67
TABLE 3.
Health Care Worker—Related Obstacles to Patient Participation
Covert Ways to Maintain Control
Health care workers can maintain control through various means. Asking closed-ended questions limits the possibility for discussion and reduces the patient to submissiveness.33 Limiting the depth and amount of information given to the patient reduces his or her autonomy33 and is associated with less participation.15 Health care workers can also establish their power by creating and perpetuating patient uncertainty about his or her illness, as this extract of an interview demonstrates: “Patients don't know what is happening, medical-wise….This way we have the control and it makes our job easier.”33 Moreover, health care workers can limit patient participation by using authoritative language, veiled orders (eg, “you should,” “it is necessary that…”), and condescending terms such as “be good” and “be cooperative.”81
Health Care Workers' Barriers to Patient Participation
Besides the refusal to delegate power, health care workers perceive lack of time as a factor limiting patient input in health care.66-68 Although some studies found that a medical consultation during which the patient participated in decision making was significantly longer,69 others failed to show this relationship.15,26,70,71 Health care workers might allow patient participation to varying degrees according to the type of situation. Physicians are more likely to allow participation when dealing with psychosocial rather than somatic complaints.15 In contrast, patients are less involved when a treatment or a diagnostic procedure is performed.15 Personal beliefs can influence the importance physicians will grant to patient opinion. In a survey of more than 600 obstetricians concerning elective, patient-requested cesarean section, almost all those who thought that patients had the right to ask for such a procedure were ready to carry them out, in contrast to one-quarter who believed that women did not have such a right.61
Primary care physicians have been linked to allowing more patient participation than specialists in most,60,69 but not all,71 studies, and cardiologists allow less patient participation than other specialists.69 Furthermore, nonwhite physicians were less likely to encourage participation, independent of their specialty or the volume of their practice.69 Physician sex15,60,69 and age15,60,61 do not seem to influence patient participation.
Health care workers can be educated to improve relationships with patients.72,73 Medical students,74 specialized educators,75 and physicians who have completed their training in general medicine,76 gynecology,70 oncology,77 and pediatrics78 were all able to improve their attitudes with respect to patient participation through structured training sessions. Furthermore, the benefits of training persisted for up to 10 years.69,79 However, some studies failed to show such benefit despite formal training,82 presumably because of difficulties in changing established communication patterns.
SOCIAL INFLUENCE ON PATIENT PARTICIPATION
Some obstacles to patient participation are not within the control of either the patient or the health care worker. Patients' desires reflect societal norms and the permissiveness of the health care environment in which they receive treatment.83 If the culture dictates a passive role, a significant proportion of patients is likely not to “want” to participate. Similarly, patient participation is unlikely if it is clear that health care workers are not interested in receiving patient input. Thus, patient participation reflects societal norms and depends on whether the culture of the organization openly supports it.84,85
PATIENT PARTICIPATION IN THE MANAGEMENT OF CHRONIC ILLNESS
Patient participation originated from the need to improve the decision-making process and has been successfully extended to other areas of patient care, notably the management of chronic illness.4 In a meta-analysis that evaluated interventions used in disease management programs for patients with chronic illness, patient education and the use of “reminders” (prompts given to patients to perform specific tasks related to the care of their condition) were associated with significant improvement in disease control.27 Educational interventions for self-management of asthma in children improved lung function and substantially decreased school absenteeism.28 Training adult patients with type 2 diabetes mellitus was effective in reducing fasting blood glucose levels, glycated hemoglobin levels, and the need for diabetes medication.29 These and other studies30-32 show that patients can be educated to participate in the care of chronic illnesses and that their participation can improve disease control.
SUGGESTIONS FOR THE POTENTIAL ROLE OF PATIENT PARTICIPATION TO PREVENT MEDICAL ERRORS
Because patient participation has been shown to improve decision making and treatment of chronic diseases, it is reasonable to speculate that it could also help prevent medical errors,4,73,86-90 although considerably less evidence exists for this potential application. In addition, a major initiative to enlist patients in error prevention may require that the public be reassured of the legitimacy of such an endeavor, which otherwise could be perceived at first glance as a way to police the health care worker or as putting inappropriate responsibility on an already weakened and vulnerable individual.91
Our general position is supported by the following evidence. A decade ago, the Dana-Farber Cancer Institute completely revised its patient safety program in response to 2 cases of serious medication error extensively covered by the media.92 Among other strategies, patients and their families are now actively invited to contribute to improve the quality of care through participation in developing educational programs for professionals and in establishing institutional policies. Patients are members of quality and safety committees and oversee a quarterly newspaper sent to them and their families. Patients and family members are trained to interview current patients about their perceptions of safe care. During this period, the incidence of medication errors decreased from 3.4 to 1.7 episodes per 10,000 doses.92 Although patients' contribution to this reduction cannot be proven, this experience suggests that their participation can play a role in decreasing medical errors. However, evidence for efficacy is conflicting or requires further testing.93-95
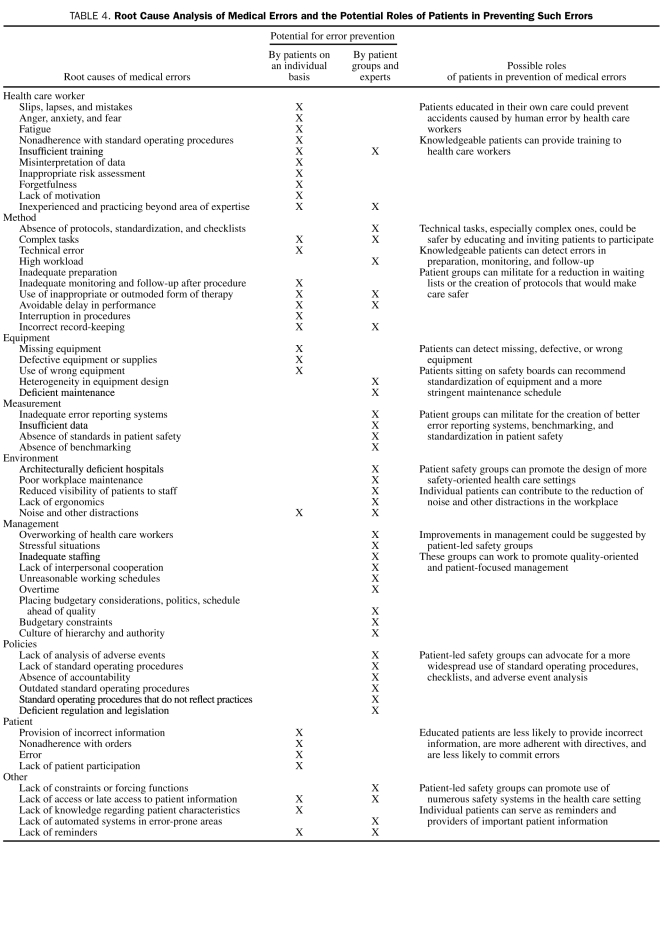
Most medical errors are preventable96 and are due to a convergence of multiple contributing factors,89 such as deficient processes, poor technique, inappropriate environment, failing equipment, and deficient management. Analysis of the various causes of medical errors shows that patients could help prevent many of these by intervening at various levels, and we list some examples in Table 4. Importantly, patients can participate as individuals and by acting as a group or as experts.
TABLE 4.
Root Cause Analysis of Medical Errors and the Potential Roles of Patients in Preventing Such Errors
Patients are ready to have a role in error prevention. Among 2078 questionnaire recipients, 91% thought that they could prevent medical errors occurring in hospitals, and 98% thought that hospitals should educate patients in this regard.97 However, their opinion varied with error types; although 84% would be comfortable asking a nurse to verify patient identity, only 45% felt at ease to ask staff to wash their hands. More innovative error-preventing behaviors, such as questioning health care worker judgment or actions, might be unacceptable to the public.34
Our general position regarding the role patients can play in the prevention of errors is in line with the proposals of WHO. Through its Patients for Patient Safety component, the WHO World Alliance for Patient Safety aims to ensure that patients are at the core of the safety movement worldwide.98 Led by patients, Patients for Patient Safety is convinced that the perspective of patients and families provides a powerful contribution to ensure an authentic and sustainable transformation in patient safety. During the first workshop in 2005,98 patients and patient safety advocates from 20 different countries, representing more than 2000 organizations, endorsed a declaration calling for patients to have a greater role in improving safety of health care worldwide. An international network of patients and consumers is being established to promote patient leadership and participation in patient safety initiatives through advocacy and open dialogue. Action strategies are being developed with a strong emphasis on working in partnership with health care authorities, partners, and professionals.
HAND HYGIENE
Health care—associated infection is a major issue in patient safety. Hand hygiene is the primary measure to prevent health care—associated infection and limit the spread of antimicrobial resistance.99-102 However, adherence by health care workers to good practice is extremely low. Studies in many countries worldwide show that nurses and physicians wash their hands less than half the time.2,99,100 Improving hand hygiene adherence has been the major focus of the WHO First Global Patient Safety Challenge “Clean Care is Safer Care.”2,103 New guidelines for hand hygiene were developed together with a multimodal implementation strategy to promote system changes and modification of health care workers' behavior.100 These are currently undergoing testing worldwide in both developed and developing countries.103-105
Patient participation is among the critical elements in hand hygiene promotion. McGuckin et al54-56 were among the first to study the possible effect of patient education to increase staff adherence with handwashing. When patients were educated on admission to ask staff to wash their hands, soap consumption increased by 34% to 94%.54,56 In surveys after discharge, 90% to 100%54,55 of patients confirmed having asked a nurse, and 31% to 35%55,56 a physician. However, some patients (up to 60% of those eligible in 1 study55) did not wish to participate. Some of these refusals may represent a rejection of the concept by patients. Among a number of scenarios to reduce medical errors, the one in which the patient asked health care workers if they had washed their hands was perceived as the least popular and the least likely to be undertaken by patients.34
In a recent survey, 80% of Americans indicated their readiness to ask health care workers to wash their hands.106 Because this rate can vary substantially according to how the question is framed, this proportion could be an overestimate. In a survey during the CleanyourHands nationwide campaign in the United Kingdom, the proportion of respondents who supported patient participation diminished from 71% to 38% when the question was changed from theoretical (eg, “Should patients be involved in helping staff improve hand hygiene?”) to concrete (eg, “What would you do if you thought a staff member had not washed their hands?”).107 Additional factors known to influence participation in decision making, eg, an extrovert personality and younger age,108 may affect patients' intentions to ask health care workers to perform hand hygiene. Patients' perception of the sincerity of the invitation to ask may be even more important. As an example, health care workers wearing badges with an explicit invitation increased the challenge rate.108 Despite repeated observations that reveal lower hand hygiene adherence among physicians compared with nurses,101,109,110 request rates to physicians are lower,54-56 suggesting reluctance to contradict authority figures. Thus, despite their strong desire to contribute to diminishing medical errors and the documented positive effect they can have on behavior of health care workers, patients might refuse to ask some staff to wash their hands.
PROPOSAL FOR A MODEL OF PATIENT PARTICIPATION TO IMPROVE PATIENT SAFETY
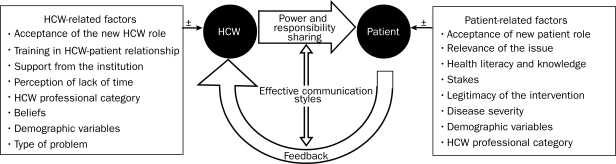
Drawing on the previous review of factors that influence patient participation in decision making and in the treatment of chronic disease, we outline the main elements of a strategy aimed at encouraging patients to participate in improving patient safety (Figure). Given that support from health care workers is crucial for success, the first and most important step is to enlist their full and enthusiastic support. A major educational campaign, using articulate patients when possible, may be needed to convince physicians and nurses of the value of patient participation. The objective is to help health care workers recognize the contribution of patients and their families to the healing process and to be receptive to patient input. This campaign must be designed to take into account the numerous health care worker—related obstacles to patient participation (eg, perception of lack of time and their level of training in the patient-caregiver relationship). Once health care workers are “on board,” educational programs for patients must be offered so that they have the knowledge required to participate. The strategy must also educate patients so that they understand the legitimacy and relevance of their interventions and are convinced of their effectiveness. To do so, numerous patient-related factors shown to influence patient participation must be addressed and overcome. Although they are not modifiable, sociodemographic factors (eg, age, disease severity, and ethnicity) must also be taken into account. When both health care worker and patient support are secured, positive feedback will emerge from the patients and contribute to the safety of health care.
FIGURE.
Conceptual model of factors that influence patient participation in preventing errors. HCW = health care worker.
RESEARCH AGENDA
Many aspects of patient participation remain unexplored, particularly concerning patient safety and error prevention. Studies of health care workers' views on patient participation in this area are lacking. There is a need to determine the possibility of redrawing the border between health care worker and patient responsibilities without the former considering patient involvement intrusive and to identify the model of patient-physician relationship best suited to achieve this objective.5 The paucity of convincing data on the effect of patient participation in error prevention and the methodologic limitations of the few published studies have shed some doubt about its possible efficacy.111-113 Inviting families to participate deserves investigation. The possible effect of an information campaign on patient satisfaction is unknown. Revelation of low staff performance with some practices could cause anxiety to patients and compromise their participation in an improvement strategy. The effect of participation on health care worker behavior remains to be determined. For example, in hand hygiene promotion, the efficiency of patient participation in institutions where adherence with hand hygiene practices is already reasonably high is unknown. Staff who do not respect the rules of hand hygiene will also possibly refuse to participate in a campaign involving patient participation. The level of knowledge of the importance of hand hygiene needed to encourage patients to participate remains unknown. Similarly, the way in which patient participation contributes to increase staff adherence with hand hygiene should be determined. Alternatively, organizing a campaign that encourages patients to ask health care workers about hand hygiene could draw health care workers' attention to its importance and raise their adherence without patients having to intervene. Moreover, such a campaign could act through normative pressure, meaning that the health care worker will feel “observed” by the patients and therefore adhere with directives. Many questions remain about how to structure a hand hygiene promotional campaign, in particular the optimal way to establish an atmosphere favorable to collaboration between patients and health care workers. Finally, cost-effectiveness and the role of patient participation in the sustainability of promotion campaigns need to be assessed. The latter holds great promise according to international experts.97
LIMITATIONS
The level of evidence for many of the concepts presented in this review is from uncontrolled or observational studies, and few included studies would qualify as a high quality of evidence. Because this review is narrative, some studies may have been missed. A systematic review was not undertaken because of the paucity of methodologically sound research on patient participation in error prevention. Moreover, a narrative review was more appropriate to better illustrate the origins of patient participation and describe its evolution leading to a potential use to improve patient safety.114,115 Furthermore, it allows one to analogize the principles of patient participation in decision making to prevention of medical errors and to foresee obstacles to its implementation.
CONCLUSION
This review suggests that patient participation can improve the decision-making process and the care of chronic illness. However, many patient and health care worker—related factors can influence its efficacy and implementation. Its use to decrease medical errors and to increase staff adherence with optimal practices is promising and deserves further study, but several potential obstacles can be foreseen at patient, health care worker, and health care center levels. Given the controversial nature of this subject, it will be essential to conduct rigorous studies to answer the inherent questioning of the concept.
Acknowledgments
We thank all members of the Infection Control Program, University of Geneva Hospitals, in particular Rosemary Sudan for expert editorial assistance, and members of the WHO Global Patient Safety Challenge “Clean Care is Safer Care” core group: John Boyce, MD; Barry Cookson, BDS, MBBS; Nizam Damani, MD; Don Goldmann, MD; Lindsay Grayson, MD; Elaine Larson, RN, PhD; Geeta Mehta, MD; Ziad Memish, MD; Hervé Richet, MD; Manfred Rotter, MD; Syed Sattar, PhD; Hugo Sax, MD; Wing Hong Seto, MD; Andreas Voss, MD; and Andreas Widmer, MD. They thank the members of the WHO Task Force on Patients for Patient Safety for their participation in the discussion on this topic, in particular, Benedetta Allegranzi, MD, Maryanne McGuckin, DrScED, and Julie Storr, MBA.
Footnotes
The World Health Organization takes no responsibility for the information provided or the views expressed in this article.
REFERENCES
- 1.Kennedy JF. Special message to the Congress on protecting the consumer interest. In: Public Papers of the Presidents of the United States March15, 1962 Washington, DC: US Government Printing Office; 1962:93:236 http://www.jfklink.com/speeches/jfk/publicpapers/1962/jfk93_62.html Accessed July 1, 2009 [Google Scholar]
- 2.World Health Organisation World Alliance for Patient Safety. Global Patient Safety Challenge 2005-2006: Clean Care is Safer Care Geneva, Switzerland: World Health Organisation; 2005:1-25 http://www.who.int/patientsafety/events/05/GPSC_Launch_ENGLISH_FINAL.pdf Accessed July 1, 2009 [Google Scholar]
- 3.Cahill J. Patient participation—a review of the literature. J Clin Nurs 1998;7(2):119-128 [PubMed] [Google Scholar]
- 4.Coulter A, Ellins J. Patient-Focused Interventions: A Review of the Evidence London, England: The Health Foundation and Picker Institute Europe; 2006:7-20 [Google Scholar]
- 5.Emanuel EJ, Emanuel LL. Four models of the physician-patient relationship. JAMA 1992;267(16):2221-2226 [PubMed] [Google Scholar]
- 6.Gillon R. Medical ethics: four principles plus attention to scope. BMJ 1994;309(6948):184-188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kizer KW. Establishing health care performance standards in an era of consumerism. JAMA 2001;286(10):1213-1217 [DOI] [PubMed] [Google Scholar]
- 8.Advisory Commission on Consumer Protection and Quality in the Health Care Industry Consumer bill of rights and responsibilities: executive summary Published November 1997 Revised July 17, 1998 Washington, DC;1997. http://www.hcqualitycommission.gov/cborr/ Accessed July 1, 2009 [Google Scholar]
- 9.Will consumerism lead to better health [editorial]? Lancet 2005;366(9483):343 [PubMed] [Google Scholar]
- 10.ACOG Committee on Quality Improvement and Patient Safety ACOG Committee Opinion #320: partnering with patients to improve safety. Obstet Gynecol 2005;106(5, pt 1):1123-1125 [DOI] [PubMed] [Google Scholar]
- 11.General Medical Council Good medical practice: the duties of a doctor registered with the General Medical Council London, England: General Medical Council; 2006. http://www.gmc-uk.org/guidance/good_medical_practice/GMC_GMP.pdf Accessed July 1, 2009 [Google Scholar]
- 12.Nursing and Midwifery Council The NMC code of professional conduct: standards for conduct, performance and ethics: protecting the public through professional standards London: Nursing and Midwifery Council; 2004. http://www.nmc-uk.org/aDisplayDocument.aspx?DocumentID=338 Accessed July 1, 2009 [Google Scholar]
- 13.Patient Self-Determination Act, 42 USC §§1395cc 1396a (1994).
- 14.State of Queensland Queensland Health Public Patient's Charter Brisbane, Queensland, Australia: Queensland Health; 2002. http://www.health.qld.gov.au/qhppc/docs/booklet.pdf Accessed July 1, 2009 [Google Scholar]
- 15.van den Brink-Muinen A, van Dulmen SM, de Haes HC, Visser AP, Schellevis FG, Bensing JM. Has patients' involvement in the decision-making process changed over time? Health Expect 2006;9(4):333-342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Department of Health The Patient's Charter London, England: Her Majesty's Stationery Office; 1991. [Google Scholar]
- 17.Department of Health Patient and Public Involvement in the New NHS London, England: The Stationery Office; 1999. http://www.dh.gov.uk/en/Publicationsandstatistics/Lettersandcirculars/Healthservicecirculars/DH_4004176 Accessed July 1, 2009 [Google Scholar]
- 18.National/Regional Health Promoting Hospitals Network Coordinators Vienna Recommendations on Health Promoting Hospitals Geneva, Switzerland: World Health Organisation; 1997. http://www.euro.who.int/document/IHB/hphviennarecom.pdf Acccessed April 1, 2009 [Google Scholar]
- 19.Guadagnoli E, Ward P. Patient participation in decision-making. Soc Sci Med 1998;47(3):329-339 [DOI] [PubMed] [Google Scholar]
- 20.Levinson W, Kao A, Kuby A, Thisted RA. Not all patients want to participate in decision making: a national study of public preferences. J Gen Intern Med 2005;20(6):531-535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Strull WM, Lo B, Charles G. Do patients want to participate in medical decision making? JAMA 1984;252(21):2990-2994 [PubMed] [Google Scholar]
- 22.Little P, Everitt H, Williamson I, et al. Preferences of patients for patient centred approach to consultation in primary care: observational study. BMJ 2001;322(7284):468-472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thompson SC, Pitts JS, Schwankovsky L. Preferences for involvement in medical decision-making: situational and demographic influences. Patient Educ Couns 1993;22(3):133-140 [DOI] [PubMed] [Google Scholar]
- 24.Mansell D, Poses RM, Kazis L, Duefield CA. Clinical factors that influence patients' desire for participation in decisions about illness. Arch Intern Med 2000;160(19):2991-2996 [DOI] [PubMed] [Google Scholar]
- 25.Katz MG, Jacobson TA, Veledar E, Kripalani S. Patient literacy and question-asking behavior during the medical encounter: a mixed-methods analysis. J Gen Intern Med 2007June;22(6):782-786 Epub 2007 Apr 12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Greenfield S, Kaplan S, Ware JE., Jr Expanding patient involvement in care: effects on patient outcomes. Ann Intern Med 1985;102(4):520-528 [DOI] [PubMed] [Google Scholar]
- 27.Weingarten SR, Henning JM, Badamgarav E, et al. Interventions used in disease management programmes for patients with chronic illness—which ones work? Meta-analysis of published reports. BMJ 2002;325(7370):925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Guevara JP, Wolf FM, Grum CM, Clark NM. Effects of educational interventions for self management of asthma in children and adolescents: systematic review and meta-analysis. BMJ 2003;326(7402):1308-1309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Deakin T, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005;(2):CD003417 [DOI] [PubMed] [Google Scholar]
- 30.Fitzmaurice DA, Murray ET, McCahon D, et al. Self management of oral anticoagulation: randomised trial [published correction appears in BMJ. 2005;331(7528):1330] BMJ 2005November;331(7524):1057 Epub 2005 Oct 10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Murray E, Davis H, Tai SS, Coulter A, Gray A, Haines A. Randomised controlled trial of an interactive multimedia decision aid on benign prostatic hypertrophy in primary care. BMJ 2001;323(7311):493-496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Murray E, Davis H, Tai SS, Coulter A, Gray A, Haines A. Randomised controlled trial of an interactive multimedia decision aid on hormone replacement therapy in primary care. BMJ 2001;323(7311):490-493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Henderson S. Power imbalance between nurses and patients: a potential inhibitor of partnership in care. J Clin Nurs 2003;12(4):501-508 [DOI] [PubMed] [Google Scholar]
- 34.Hibbard JH, Peters E, Slovic P, Tusler M. Can patients be part of the solution? Views on their role in preventing medical errors. Med Care Res Rev 2005;62(5):601-616 [DOI] [PubMed] [Google Scholar]
- 35.Kraetschmer N, Sharpe N, Urowitz S, Deber RB. How does trust affect patient preferences for participation in decision-making? Health Expect 2004;7(4):317-326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stiggelbout AM, Kiebert GM. A role for the sick role: patient preferences regarding information and participation in clinical decision-making. CMAJ 1997;157(4):383-389 [PMC free article] [PubMed] [Google Scholar]
- 37.Arora NK, McHorney CA. Patient preferences for medical decision making: who really wants to participate? Med Care 2000;38(3):335-341 [DOI] [PubMed] [Google Scholar]
- 38.Sekimoto M, Asai A, Ohnishi M, et al. Patients' preferences for involvement in treatment decision making in Japan. BMC Fam Pract 2004March;5:1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ende J, Kazis L, Ash A, Moskowitz MA. Measuring patients' desire for autonomy: decision making and information-seeking preferences among medical patients. J Gen Intern Med 1989;4(1):23-30 [DOI] [PubMed] [Google Scholar]
- 40.Gaston CM, Mitchell G. Information giving and decision-making in patients with advanced cancer: a systematic review. Soc Sci Med 2005;61(10):2252-2264 [DOI] [PubMed] [Google Scholar]
- 41.McKinstry B. Do patients wish to be involved in decision making in the consultation? a cross sectional survey with video vignettes. BMJ 2000;321(7265):867-871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rosén P, Anell A, Hjortsberg C. Patient views on choice and participation in primary health care. Health Policy 2001;55(2):121-128 [DOI] [PubMed] [Google Scholar]
- 43.Cassileth BR, Zupkis RV, Sutton-Smith K, March V. Information and participation preferences among cancer patients. Ann Intern Med 1980;92(6):832-836 [DOI] [PubMed] [Google Scholar]
- 44.Rothenbacher D, Lutz MP, Porzsolt F. Treatment decisions in palliative cancer care: patients' preferences for involvement and doctors' knowledge about it. Eur J Cancer 1997;33(8):1184-1189 [DOI] [PubMed] [Google Scholar]
- 45.Wetzels R, Harmsen M, Van Weel C, Grol R, Wensing M. Interventions for improving older patients' involvement in primary care episodes. Cochrane Database Syst Rev. 2007;(1):CD004273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Willems S, De Maesschalck S, Deveugele M, Derese A, De Maeseneer J. Socio-economic status of the patient and doctor-patient communication: does it make a difference? Patient Educ Couns 2005;56(2):139-146 [DOI] [PubMed] [Google Scholar]
- 47.Blackhall LJ, Murphy ST, Frank G, Michel V, Azen S. Ethnicity and attitudes toward patient autonomy. JAMA 1995;274(10):820-825 [PubMed] [Google Scholar]
- 48.Gordon HS, Street RL, Jr, Sharf BF, Souchek J. Racial differences in doctors' information-giving and patients' participation. Cancer 2006;107(6):1313-1320 [DOI] [PubMed] [Google Scholar]
- 49.van Ryn M, Burgess D, Malat J, Griffin J. Physicians' perceptions of patients' social and behavioral characteristics and race disparities in treatment recommendations for men with coronary artery disease. Am J Public Health 2006February;96(2):351-357 Epub 2005 Dec 27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA 1999;282(6):583-589 [DOI] [PubMed] [Google Scholar]
- 51.Vincent C, Furnham A. Complementary medicine: state of the evidence. J R Soc Med 1999;92(4):170-177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Montbriand MJ. Freedom of choice: an issue concerning alternate therapies chosen by patients with cancer. Oncol Nurs Forum 1993;20(8):1195-1201 [PubMed] [Google Scholar]
- 53.Boon H, Westlake K, Deber R, Moineddin R. Problem-solving and decision-making preferences: no difference between complementary and alternative medicine users and non-users. Complement Ther Med 2005;13(3):213-216 [DOI] [PubMed] [Google Scholar]
- 54.McGuckin M, Waterman R, Porten L, et al. Patient education model for increasing handwashing compliance. Am J Infect Control 1999;27(4):309-314 [DOI] [PubMed] [Google Scholar]
- 55.McGuckin M, Waterman R, Storr IJ, et al. Evaluation of a patient-empowering hand hygiene programme in the UK. J Hosp Infect 2001;48(3):222-227 [DOI] [PubMed] [Google Scholar]
- 56.McGuckin M, Taylor A, Martin V, Porten L, Salcido R. Evaluation of a patient education model for increasing hand hygiene compliance in an inpatient rehabilitation unit. Am J Infect Control 2004;32(4):235-238 [DOI] [PubMed] [Google Scholar]
- 57.Kravitz RL, Epstein RM, Feldman MD, et al. Influence of patients' requests for direct-to-consumer advertised antidepressants: a randomized controlled trial [published correction appears in JAMA. 2005;294(19):2436] JAMA 2005;293(16):1995-2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Maly RC, Umezawa Y, Ratliff CT, Leake B. Racial/ethnic group differences in treatment decision-making and treatment received among older breast carcinoma patients. Cancer 2006;106(4):957-965 [DOI] [PubMed] [Google Scholar]
- 59.Kagawa-Singer M, Blackhall LJ. Negotiating cross-cultural issues at the end of life: “You got to go where he lives.” JAMA 2001;286(23):2993-3001 [DOI] [PubMed] [Google Scholar]
- 60.Kravitz RL, Bell RA, Azari R, Kelly-Reif S, Krupat E, Thom DH. Direct observation of requests for clinical services in office practice: what do patients want and do they get it? Arch Intern Med 2003;163(14):1673-1681 [DOI] [PubMed] [Google Scholar]
- 61.Bettes BA, Coleman VH, Zinberg S, et al. Cesarean delivery on maternal request: obstetrician-gynecologists' knowledge, perception, and practice patterns. Obstet Gynecol 2007;109(1):57-66 [DOI] [PubMed] [Google Scholar]
- 62.Hewison A. Nurses' power in interactions with patients. J Adv Nurs 1995;21(1):75-82 [DOI] [PubMed] [Google Scholar]
- 63.Johnson M, Haigh C, Yates-Bolton N. Valuing of altruism and honesty in nursing students: a two-decade replication study. J Adv Nurs 2007;57(4):366-374 [DOI] [PubMed] [Google Scholar]
- 64.Brody DS. The patient's role in clinical decision-making. Ann Intern Med 1980;93(5):718-722 [DOI] [PubMed] [Google Scholar]
- 65.O'Flynn N, Britten N. Does the achievement of medical identity limit the ability of primary care practitioners to be patient-centred? a qualitative study. Patient Educ Couns 2006January;60(1):49-56 Epub 2005 Jan 19 [DOI] [PubMed] [Google Scholar]
- 66.Ford S, Schofield T, Hope T. Barriers to the evidence-based patient choice (EBPC) consultation. Patient Educ Couns 2002;47(2):179-185 [DOI] [PubMed] [Google Scholar]
- 67.Stevenson FA. General practitioners' views on shared decision making: a qualitative analysis. Patient Educ Couns 2003;50(3):291-293 [DOI] [PubMed] [Google Scholar]
- 68.Anderson RM, Funnell MM. Patient empowerment: reflections on the challenge of fostering the adoption of a new paradigm. Patient Educ Couns 2005;57(2):153-157 [DOI] [PubMed] [Google Scholar]
- 69.Kaplan SH, Greenfield S, Gandek B, Rogers WH, Ware JE., Jr Characteristics of physicians with participatory decision-making styles. Ann Intern Med 1996;124(5):497-504 [DOI] [PubMed] [Google Scholar]
- 70.van Dulmen AM, van Weert JC. Effects of gynaecological education on interpersonal communication skills. BJOG 2001;108(5):485-491 [DOI] [PubMed] [Google Scholar]
- 71.Braddock CH, III, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. Informed decision making in outpatient practice: time to get back to basics. JAMA 1999;282(24):2313-2320 [DOI] [PubMed] [Google Scholar]
- 72.Lewin SA, Skea ZC, Entwistle V, Zwarenstein M, Dick J. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev 2001;(4):CD003267 [DOI] [PubMed] [Google Scholar]
- 73.Bergeson SC, Dean JD. A systems approach to patient-centered care. JAMA 2006;296(23):2848-2851 [DOI] [PubMed] [Google Scholar]
- 74.Anderson RM, Donnelly MB, Gorenflo DW, Funnell MM, Sheets KJ. Influencing the attitudes of medical students toward diabetes: results of a controlled study. Diabetes Care 1993;16(2):503-505 [DOI] [PubMed] [Google Scholar]
- 75.Anderson RM, Funnell MM, Barr PA, Dedrick RF, Davis WK. Learning to empower patients: results of professional education program for diabetes [published correction appears in Diabetes Care. 1991;14(10):933] Diabetes Care 1991;14(7):584-590 [DOI] [PubMed] [Google Scholar]
- 76.Roter DL, Hall JA, Kern DE, Barker LR, Cole KA, Roca RP. Improving physicians' interviewing skills and reducing patients' emotional distress: a randomized clinical trial. Arch Intern Med 1995;155(17):1877-1884 [PubMed] [Google Scholar]
- 77.Fellowes D, Wilkinson S, Moore P. Communication skills training for health care professionals working with cancer patients, their families and/or carers. Cochrane Database Syst Rev. 2004;(2):CD003751 [DOI] [PubMed] [Google Scholar]
- 78.van Dulmen AM, Holl RA. Effects of continuing paediatric education in interpersonal communication skills. Eur J Pediatr 2000;159(7):489-495 [DOI] [PubMed] [Google Scholar]
- 79.Maguire P, Fairbairn S, Fletcher C. Consultation skills of young doctors, I: benefits of feedback training in interviewing as students persist [published correction appears in Br Med J (Clin Res Ed). 1986;293(6538):26] Br Med J (Clin Res Ed) 1986;292(6535):1573-1576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Saunders P. Encouraging patients to take part in their own care. Nurs Times 1995;91(9):42-43 [PubMed] [Google Scholar]
- 81.Moore KN. Compliance or collaboration? the meaning for the patient. Nurs Ethics 1995;2(1):71-77 [DOI] [PubMed] [Google Scholar]
- 82.Towle A, Godolphin W, Grams G, Lamarre A. Putting informed and shared decision making into practice. Health Expect 2006;9(4):321-332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Belcher VN, Fried TR, Agostini JV, Tinetti ME. Views of older adults on patient participation in medication-related decision making. J Gen Intern Med 2006;21(4):298-303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Balint J, Shelton W. Regaining the initiative: forging a new model of the patient-physician relationship. JAMA 1996;275(11):887-891 [DOI] [PubMed] [Google Scholar]
- 85.Novack DH, Suchman AL, Clark W, Epstein RM, Najberg E, Kaplan C, Working Group on Promoting Physician Personal Awareness. American Academy on Physician and Patient Calibrating the physician: personal awareness and effective patient care. JAMA 1997;278(6):502-509 [DOI] [PubMed] [Google Scholar]
- 86.Howe A. Can the patient be on our team? an operational approach to patient involvement in interprofessional approaches to safe care. J Interprof Care 2006;20(5):527-534 [DOI] [PubMed] [Google Scholar]
- 87.Awé C, Lin SJ. A patient empowerment model to prevent medication errors. J Med Syst 2003;27(6):503-517 [DOI] [PubMed] [Google Scholar]
- 88.Shaw JM, Letts M, Dickinson D. Adverse events reporting in English hospital statistics: patients should be involved as partners [letter]. BMJ 2004;329(7470):857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Institute of Medicine. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System Washington, DC: National Academy Press; 1999. [PubMed] [Google Scholar]
- 90.The Committee on Identifying and Preventing Medication Errors. Institute of Medicine. Aspden P, Wolcott J, Bootman JL, Cronenwett LR, eds. Preventing Medication Errors Washington, DC: National Academies Press; 2006. [Google Scholar]
- 91.Entwistle VA, Mello MM, Brennan TA. Advising patients about patient safety: current initiatives risk shifting responsibility. Jt Comm J Qual Patient Saf. 2005;31(9):483-494 [DOI] [PubMed] [Google Scholar]
- 92.Conway J, Nathan D, Benz E, et al. Key Learning from the Dana-Farber Cancer Institute's 10-year patient safety journey. In: American Society of Clinical Oncology 2006 Educational Book. 42nd Annual Meeting, June 2-6, 2006 Atlanta, GA: 2006:615-619 [Google Scholar]
- 93.DiGiovanni CW, Kang L, Manuel J. Patient compliance in avoiding wrong-site surgery. J Bone Joint Surg Am 2003;85-A(5):815-819 [DOI] [PubMed] [Google Scholar]
- 94.Weingart SN, Toth M, Eneman J, et al. Lessons from a patient partnership intervention to prevent adverse drug events. Int J Qual Health Care 2004;16(6):499-507 [DOI] [PubMed] [Google Scholar]
- 95.Møller T, Borregaard N, Tvede M, Adamsen L. Patient education—a strategy for prevention of infections caused by permanent central venous catheters in patients with haematological malignancies: a randomized clinical trial. J Hosp Infect 2005December;61(4):330-341 Epub 2005 Jul 6 [DOI] [PubMed] [Google Scholar]
- 96.Leape LL, Brennan TA, Laird N, et al. The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II. N Engl J Med 1991;324(6):377-384 [DOI] [PubMed] [Google Scholar]
- 97.Waterman AD, Gallagher TH, Garbutt J, Waterman BM, Fraser V, Burroughs TE. Brief report: hospitalized patients' attitudes about and participation in error prevention. J Gen Intern Med 2006;21(4):367-370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.World Health Organisation London Declaration: Patients for Patient Safety Published March 29, 2006 Geneva, Switzerland: World Health Organisation; http://www.who.int/patientsafety/patients_for_patient/London_Declaration_EN.pdf Accessed July 15 [Google Scholar]
- 99.Pittet D, Mourouga P, Perneger TV. Compliance with handwashing in a teaching hospital: infection control program. Ann Intern Med 1999;130(2):126-130 [DOI] [PubMed] [Google Scholar]
- 100.World Health Organisation WHO Guidelines on Hand Hygiene in Health Care Geneva, Switzerland: World Health Organisation; 2009. http://whqlibdoc.who.int/publications/2009/9789241597906_eng.pdf Accessed July 15, 2009 [Google Scholar]
- 101.Pittet D, Hugonnet S, Harbarth S, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene: infection control programme [published correction appears in Lancet. 2000;356(9248):2196] Lancet 2000;356(9238):1307-1312 [DOI] [PubMed] [Google Scholar]
- 102.Sax H, Allegranzi B, Uçkay I, Larson E, Boyce J, Pittet D. ‘My five moments for hand hygiene’: a user-centred design approach to understand, train, monitor and report hand hygiene. J Hosp Infect 2007September;67(1):9-21 Epub 2007 Aug 27 [DOI] [PubMed] [Google Scholar]
- 103.Pittet D, Donaldson L. Clean Care is Safer Care: a worldwide priority. Lancet 2005;366(9493):1246-1247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Allegranzi B, Pittet D. Healthcare-associated infection in developing countries: simple solutions to meet complex challenges. Infect Control Hosp Epidemiol 2007December;28(12):1323-1327 Epub 2007 Oct 22 [DOI] [PubMed] [Google Scholar]
- 105.Pittet D, Donaldson L. Challenging the world: patient safety and health care-associated infection. Int J Qual Health Care 2006February;18(1):4-8 Epub 2006 Jan 5 [DOI] [PubMed] [Google Scholar]
- 106.McGuckin M, Waterman R, Shubin A. Consumer attitudes about health care-acquired infections and hand hygiene. Am J Med Qual 2006;21(5):342-346 [DOI] [PubMed] [Google Scholar]
- 107.National Patient Safety Agency Achieving Our Aims: Evaluating the Results of the Pilot CleanyourHands Campaign London, England: NPSA; 2004. [Google Scholar]
- 108.Duncanson V, Pearson LS. A study of the factors affecting the likelihood of patients participating in a campaign to improve staff hand hygiene. Br J Infect Control. 2005;6(4):26-30 [Google Scholar]
- 109.Pittet D, Simon A, Hugonnet S, Pessoa-Silva CL, Sauvan V, Perneger TV. Hand hygiene among physicians: performance, beliefs, and perceptions. Ann Intern Med 2004;141(1):1-8 [DOI] [PubMed] [Google Scholar]
- 110.Larson E, Killien M. Factors influencing handwashing behavior of patient care personnel. Am J Infect Control 1982;10(3):93-99 [DOI] [PubMed] [Google Scholar]
- 111.Gould DJ, Hewitt-Taylor J, Drey NS, Gammon J, Chudleigh J, Weinberg JR. The CleanYourHandsCampaign: critiquing policy and evidence base. J Hosp Infect 2007February;65(2):95-101 Epub 2006 Dec 14 [DOI] [PubMed] [Google Scholar]
- 112.Pearson L. Gimmicks are not the way to combat infection NursingTimes.net Web site. Published December 20, 2006 http://www.nursingtimes.net/nursing-practice-clinical-research/comment-gimmicks-are-not-the-way-to-combat-infection/201637.article Accessed July 15, 2009
- 113.Lyons M. Should patients have a role in patient safety? a safety engineering view. Qual Saf Health Care 2007;16(2):140-142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Cook DJ, Mulrow CD, Haynes RB. Systematic reviews: synthesis of best evidence for clinical decisions. Ann Intern Med 1997;126(5):376-380 [DOI] [PubMed] [Google Scholar]
- 115.Reviews: making sense of an often tangled skein of evidence [editorial]. Ann Intern Med 2005;142(12, pt 1):1019-1020 [DOI] [PubMed] [Google Scholar]