Abstract
Purpose: A national quality report card for nursing homes, Nursing Home Compare, has been published since 2002. It has been shown to have some, albeit limited, positive impact on quality of care. The objective of this study was to test empirically the hypothesis that nursing homes have responded to the publication of the report by adopting cream skimming admission policies. Design and Methods: The study included all non-Medicare newly admitted patients to all Medicare- and Medicaid-certified nursing homes nationally during the 2001–2005 period. Using the Minimum Data Set data, we calculated for each quarter several admission cohort characteristics: average number of activity of daily living limitations and percent of residents admitted with pain, with pressure ulcers, with urinary incontinence, with diabetes, and with memory limitations. We tested whether residents admitted in the postpublication period were less frail and sick compared with residents admitted in the prepublication period by estimating fixed facility effects longitudinal regression models. Analyses were stratified by nursing home ownership, occupancy, reported quality ranking, chain affiliation, and region. Results: Evidence for cream skimming was found with respect to pain and, to a lesser degree, with respect to memory limitation but not with respect to the 4 other admission cohort characteristics. Implications: Despite the theoretical expectation, empirical evidence suggests only a limited degree of cream skimming. Further studies are required to investigate this phenomenon with respect to other admission cohort characteristics and with respect to post-acute patients.
Keywords: Nursing homes, Quality, Report cards, Cream skimming
Public report cards have been a common feature of most health care markets in the Untied States since the 1990s (Marshall, Shekelle, Leatherman, & Brook, 2000; Robinowitz & Dudley, 2006). They are designed to provide consumers—patients, their families, and others who make purchasing decisions on their behalf—with information about the performance of the medical providers available in each area, thus enabling referral decisions based on quality (Harrington, O’Meara, Kitchener, Simon, & Schnelle, 2003; Mor, 2005; Mukamel, Weimer, & Mushlin, 2007). Report cards are expected to provide incentives to improve quality of care (Gormley & Weimer, 1999; Mukamel & Mushlin, 2001). They are also one of the four corner stones of the 2006 administration’s Value-Driven Health Care Initiative (US. Department of Health and Human Services, 2007), which calls for measuring, publishing, and using information to improve quality and to promote the efficiency of medical care.
The Centers for Medicare and Medicaid Services (CMS) began publishing the Nursing Home Compare report card in November of 2002 on its Web site, http://www.medicare.gov/NHCompare. As part of CMS’s larger quality initiative, this report card follows other report cards for hospitals and managed care organizations. Studies to date have focused on the impact of Nursing Home Compare on quality. Castle (2005) surveyed nursing home administrators in four states and reported that 33% have used and 51% plan to use the information in quality improvement efforts. In a more representative national survey, Mukamel, Spector, and colleagues (2007) found that, despite being skeptical about the influence the reports have on referral choices, nursing home administrators engage in a variety of actions designed to improve quality. Those nursing homes that had worse published scores were found to be more likely to undertake quality improvement activities. In a follow-up study, Zinn, Spector, Weimer, and Mukamel (2008) found that the propensity of facilities to undertake such quality improvement actions is related to their strategic type, with those that are more innovative, the “prospector” type, being more likely to take such actions. Mukamel, Weimer, Spector, Ladd, and Zinn (2008) also examined trends in 5 of the 10 quality measures (QMs) included in the initial publication of the Nursing Home Compare report card and found improvement in two of them, improvement that was associated with the publication of the report and with the actions undertaken by nursing homes to improve quality. Werner, Konetzka, Stuart, Norton, & Park (2008) similarly found an impact of this report card on the quality of post-acute care. These studies are encouraging, as they indicate that the Nursing Home Compare report card has had at least somewhat of a positive effect on quality of care in nursing homes, similar to the experience with report cards for other health care providers (Robinowitz & Dudley, 2006).
The evaluation of the impact of report cards cannot, however, ignore the possibility that they may also engender dysfunctional responses from providers. In particular, one of the strategies that providers may choose to improve their published scores without actually investing resources in quality improvement is “cream skimming” or “cherry picking”—that is, changing the type of patient they are admitting to patients who are less frail and less sick and thus less likely to experience poor outcomes and consequently less likely to contribute to poor quality scores. The incentives for cream skimming are particularly strong when the QMs included in the published report are not risk adjusted or only minimally risk adjusted. In such cases, avoiding high-risk patients who are more likely to have bad outcomes will indeed improve the provider’s quality score, as has been shown by numerous studies of the importance of risk adjustment (Iezzoni et al., 1996). Cream skimming has been observed in Pennsylvania (Schneider & Epstein, 1996) and in New York State (Narins, Dozier, Ling, & Zareba, 2005), two states that publish physician-level risk-adjusted mortality scores for cardiac procedures. Physicians in these states reported that after report cards were introduced, they were less likely to offer care to the most risky patients because of their concerns about the impact on their published scores.
The Nursing Home Compare report card may not be immune to cream skimming. A recent study suggests that the minimal risk adjustment of the QMs in the Nursing Home Compare report leads to substantial differences in quality ranking of providers compared with more extensive risk-adjusted measures (Mukamel, Glance, et al., 2008), and nursing home administrators seem to be aware of this (Mukamel, Spector, et al., 2007). Thus, incentives for cream skimming may exist.
In this study, we examine whether there is empirical evidence for cream skimming behavior among nursing homes in response to the publication of the Nursing Home Compare report card. We define cream skimming as a change in the health status characteristics of the admission cohort in the postpublication era toward healthier and less frail patients. We operationalize this by examining changes in the average number of activities of daily living (ADLs) limitations of admission cohorts and in the percent of each admission cohort with pain, diabetes, incontinence, pressure ulcers, and memory loss.
Conceptual Framework
Adopting a neoclassical economic paradigm, we assume that for-profit nursing homes maximize profits, whereas nonprofit, private, or government nursing homes, maximize a different objective, possibly quality of care or providing access to those with the most need (Weisbrod, 1988). All are subject to constraints, including the local demand for their services. Higher demand for their services allows for-profit facilities to realize higher profits and allows nonprofit facilities to achieve their own objectives by increasing revenues. The demand each nursing home faces (its residual demand), in turn, depends on how its consumers perceive its quality and hence is influenced, among other factors, by the quality scores as reported in the Nursing Home Compare report card. Thus, all nursing home types benefit from higher demand and, therefore, have incentives to improve their reported QMs.
Improving reported QMs can be achieved by investing in quality improvements such as increased staffing, enhanced training, or improved equipment. Alternatively, nursing homes can turn away the sickest patients who are the most likely to experience bad health outcomes. To the degree that patient risks are not accounted for in the reported QMs, changing the mix of residents in the facility toward a healthier population, that is, cream skimming, would improve average outcomes and hence reported quality, without requiring costly investment.
This conceptual framework leads to several hypotheses regarding the potential association between nursing home characteristics and cream skimming behavior, as discussed in the following.
Ownership
The incentive to cream skim exists for all nursing homes, but its magnitude may differ by ownership. One may expect to see the most cream skimming among for-profit nursing homes and less among nonprofit nursing homes, especially if the objectives of the latter type include providing high-quality care or providing access to the sick and frail who need nursing home services the most.
Occupancy
Cream skimming can be a costly action if the alternative to turning a high-risk patient away is keeping a bed empty. This opportunity cost is higher for nursing homes that have low occupancies than for those that have high occupancies and face a waiting list. Therefore, we would expect that nursing homes with very high occupancies would be more likely to exhibit cream skimming.
Relatively Poor Reported QM Scores
The incentive to improve quality scores depends on the facility’s position relative to its competitors. Nursing homes with the worst QMs have the strongest incentive to improve their scores because they are the ones most likely to lose admissions and face declining demand once the report card reveals their poor quality (Mukamel, Spector, et al., 2007). We further hypothesize that nursing homes with poor scores on a specific QM may selectively cream skim on those health status characteristics that are associated with that QM. For example, we expect that admission of patients with pain will decline more among nursing homes with poor scores on the pain QM.
Chain Affiliation
Management practices, as well as the resources available for coping and responding to the report cards, might be different among chain-affiliated facilities than among freestanding facilities. Although we do not propose a directional hypothesis, we explore the possibility that chain-affiliated facilities responded differently than freestanding facilities.
Regional Differences
We also investigate the hypothesis that cream skimming behavior differs by region of the country. The environment that the nursing homes are facing, and in particular the regulation of quality by states and regional CMS offices, may vary, prompting nursing homes to react differently.
To summarize, we investigate the potential for cream skimming by examining changes in six health status characteristics of admission cohorts following publication of the Nursing Home Compare report card with respect to ownership, facility occupancy, relative quality status, chain affiliation, and region of the country.
Methods
Sample
The study included all Medicare- and Medicaid-certified nursing homes nationally (16,745), focusing on those residents admitted for long-term rather than post-acute care, those identified as non-Medicare admissions, and those aged 65 years and older. Minimum Data Set (MDS) admission assessments were used to calculate the six admission cohort characteristics (described subsequently) for each quarter, beginning in 2001 and ending in 2005 for a total of 20 observations for each facility. Facilities missing data for 10% or more of their admission records for the quarter were excluded from the sample for that quarter. However, all their data for other quarters were included. The percent of nursing homes excluded in any quarter for any QM did not exceed 0.20%.
Data Sources
Individual-level data for all newly admitted nursing home residents were obtained from the MDS. The MDS contains health assessments recorded by nursing home personnel and submitted to the CMS by all Medicare- and Medicaid-certified nursing homes in the United States. Assessments are performed at admissions, at regular intervals following that admission (i.e., annually for full assessments, quarterly for long-term care patients, and at 5, 14, and 30 days for Medicare post-acute patients), and when there is a significant change in the resident’s health status. The MDS includes information about the patient’s sociodemographics, physical and mental health status, and specific diagnoses and treatments. These data are used by the CMS both for reimbursement purposes and for calculating the QMs included in the public report card, Nursing Home Compare, suggesting that nursing homes have an incentive to ensure high data quality. Several prior studies have reported on the reliability and validity of the MDS data (Hawes, Phillips, Mor, Fries, & Morris, 1992; Hawes et al., 1995).
Facility characteristics were obtained from the Online Survey, Certification, and Reporting (OSCAR) system. OSCAR is a data set maintained by the CMS. It includes information from the annual surveys conducted by state surveyors as part of the Medicare/Medicaid recertification process mandated by CMS. OSCAR reports on aggregate resident characteristics as well as other facility characteristics such as number of beds, occupancy, and ownership.
Variables
We examined the cream skimming hypotheses with respect to six characteristics of patients admitted to nursing homes. These admission cohort characteristics included (a) ADL limitations defined as the average number of self-performance limitations in the following categories: bed mobility, transfer, walking in room, walking in corridor, locomotion on unit, locomotion off unit, dressing, eating, toilet use, personal hygiene, and bathing; (b) percent admitted with diabetes; (c) percent admitted who are frequently or always incontinent; (d) percent admitted with at least one pressure ulcer of Stage 2 or higher; (e) percent admitted with excruciating pain or daily moderate pain; and (f) percent admitted with memory loss, either short term or long term, or diagnosis of dementia or Alzheimer’s disease. These characteristics were chosen either because they were directly related to a QM included in the report card, that is, ADLs, pain, pressure ulcers, and incontinence, or because they are an important risk factor for a QM, that is, diabetes, which is associated with greater risk for pressure ulcers (Mukamel, 1997) and memory loss, which is a risk factor for urinary incontinence (Mukamel, Watson, Meng, & Spector, 2003).
These data were obtained from the MDS admission assessment and therefore include only new admissions and “true” readmissions to the facility (i.e., patients returning after a hospital stay whose return to the facility was anticipated will not have an MDS admission assessment). Thus, these cohort characteristics reflect only the characteristics of the newly admitted patients at the time of their admission to the facility and are not diluted by the characteristics of those individuals already residing in the nursing home. As such, they capture the full impact of any admission policies that nursing homes may institute.
These admission cohort characteristics were measured for each quarter starting with the first quarter of 2001, through the end of 2005. These time periods include the first publication of the report card, in the fourth quarter of 2002 and the changes made to the report card (i.e., increase in number of QMs and some changes in QM definitions), which occurred in the first quarter of 2004.
Several nursing home characteristics were included in the analyses. Full occupancy facilities were defined as facilities operating at full occupancy (100%) for each year during the 2001–2005 period, based on the OSCAR data. As it was unclear a priori what might be an empirically relevant level of full capacity, we performed sensitivity analyses with full capacity defined at 99% and 95% occupancy levels as well. Other characteristics included ownership (for-profit, nonprofit, and government owned, chain affiliation), census region, and facility ranking in the Nursing Home Compare report card within the bottom 20th percentile of its state distribution for each of the QMs. All these were determined at the time of the first publication of the report card, in November of 2002.
Analyses
We performed longitudinal analyses to test the hypothesis that there was a change in the admission cohort characteristics following publication of the report card. The analysis was repeated separately for each of the six characteristics. We first describe the basic analysis and then describe the variants and sensitivity analyses that were performed.
The basic model we estimated was of the form:
 |
Where ADMCHARi,t is the admission cohort characteristic (e.g., average ADLs or percent with diabetes) in facility i at quarter t. Quarter 8, the quarter of the first publication, which is a mixed pre/postpublication quarter, was omitted from the analysis. Q is an indicator variable that takes the value 1 for the quarter and is 0 otherwise, and D is an indicator variable for each of the N facilities that captures facility time-invariant fixed effects, such as a propensity to admit more frail residents. The 18 estimated βs capture the sample average cohort characteristics over time, adjusted for the facility time-invariant fixed effects.
With the definition of the cohort characteristics as measures of frailty or disease severity, a cream skimming response by nursing homes to the report card would result in a decrease in these characteristics following its publication. Therefore, if nursing homes have engaged in cream skimming, we would expect to observe a decreasing trend in the βs following publication. Hence, we performed two tests: (a) we tested whether each β postpublication was significantly less than the last β prior to publication and (b) we tested whether each of the β’s postpublication was less than the average of all the β‘ s prior to publications. The latter set of tests was motivated by the possibility that the last quarter prior to publication might have been an outlier, with an unusually high or low value, leading to an artificially significant or insignificant finding.
Based on inspection of the data, it seemed that for memory limitations a cream skimming response may not have occurred following the first publication of the report card, in November of 2002, but rather after changes were made to the report card in the beginning of 2004. Therefore, for this characteristic, we used the last quarter of 2003, Quarter 12, as the reference quarter for testing response and omitted the first quarter of 2004 from the analyses.
We also note that in six states, publication of the report card occurred 6 months prior to the national rollout, as part of the CMS demonstration pilot for Nursing Home Compare. Therefore, these states were excluded from the analyses for all cohort characteristics, except for memory limitations.
The first set of analyses was at the aggregate level, pooling data for all facilities. We then repeated the analyses for different subsets of nursing homes, stratified by the facility characteristics discussed in the Conceptual Framework section and that might have led to different cream skimming behavior. We stratified the sample rather than introducing these facility characteristics as covariates in the aggregate sample to allow for interaction between the time trend and the facility characteristics.
Results
Table 1 presents descriptive statistics for the admission cohort characteristics and the nursing home characteristics used in the analyses. Admission cohort characteristics were highly variable, with standard deviations ranging from about 30% of the mean for memory limitations and ADLs to more than 150% for pressure ulcers.
Table 1.
Descriptive Statistics
| Admission cohort characteristics | M | SD |
| Average number of ADLs | 23.5 | 8.2 |
| % with diabetes | 21.4 | 21.0 |
| % who are frequently or always incontinent | 34.8 | 27.8 |
| % with at least a Stage 2 pressure sore | 9.6 | 15.3 |
| % with excruciating or daily moderate pain | 18.0 | 21.0 |
| % with short/long-term memory loss, dementia, or Alzheimer’s diagnosis | 60.7 | 24.1 |
| Facility characteristics | No. of facilities | % of sample |
| Ownership | ||
| For profit | 8,864 | 63 |
| Nonprofit | 3,813 | 27 |
| Full occupancy | ||
| 100% occupancy | 62 | <1 |
| 99% occupancy | 111 | 1 |
| 95% occupancy | 1,164 | 8 |
| Have low quality (bottom 20th percentile of the state quality measure distribution based on the Nursing Home Compare November 2002 publication) | ||
| ADLs | 2,501 | 18 |
| Pain | 2,529 | 18 |
| Pressure ulcers | 2,689 | 19 |
| Low-risk incontinence (February 2004 publication) | 2,092 | 15 |
| Chain affiliation | 7,240 | 51 |
| Region | ||
| New England | 1,030 | 7 |
| Middle Atlantic | 1,821 | 13 |
| East North Central | 2,261 | 16 |
| West North Central | 2,259 | 16 |
| South Atlantic | 1,436 | 10 |
| East South Central | 1,075 | 8 |
| West South Central | 2,116 | 15 |
| Mountain | 591 | 4 |
| Pacific | 1,556 | 11 |
Note: Sample includes 14,149 nursing homes in non-demonstration states. ADLs = activities of daily living.
Aggregate Analyses
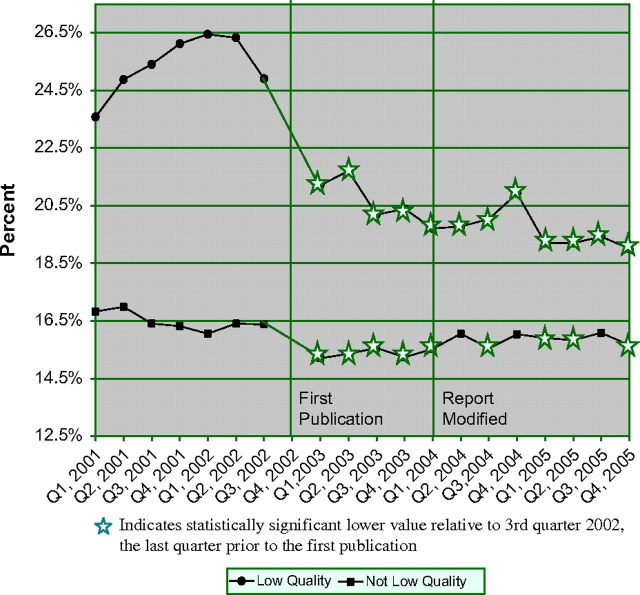
Figure 1 presents the trends in admission cohort characteristics adjusted for facility fixed effects for the aggregate sample. The figure also indicates which quarters had significantly lower levels relative to the last quarter prior to the first publication of the report (third quarter in 2002), that is, exhibiting cream skimming behavior. The only exception is memory limitation, for which the reference quarter is the last quarter before the report card was modified (fourth quarter in 2003).
Figure 1.
Admission cohort characteristics adjusted for facility fixed effects.
Four of the characteristics we examined, ADLs, diabetes, incontinence, and pressure ulcers, did not exhibit any significant (at the .05 one-tailed test) decline following publication, suggesting no evidence for cream skimming (see Figure 1). There was, however, a significant decline in the percent of patients entering with pain and memory limitations. For pain, there was a decline around the time of first publication of about 2.5 percentage points, which is equivalent to about 13% fewer admissions with excruciating pain or daily moderate pain. All postpublication quarters were significantly below the last prepublication quarter as well as the average for the whole prepublication period. For memory limitations, there did not seem to be a trend following the first publication, in the fourth quarter of 2002, but there seemed to be a decline following the change in the report card in the first quarter of 2004. The decline, of about 0.4 percentage point, which is equivalent to about 0.7% of new admissions, was a much smaller response than the response observed for pain. Five of the seven post-report modification quarters showed a significant decline in the percent residents admitted with memory limitations relative to the last quarter prior to the modifications, and when compared with the average for the whole period prior, all but one quarter showed a significant lower percent.
These analyses suggest that nursing homes have not engaged in cream skimming with respect to four of the six characteristics that we examined. However, there is evidence of cream skimming with respect to pain and to a lesser degree with respect to memory limitations.
Stratified Analyses
The aforementioned analyses were repeated for subsets of nursing homes stratified by ownership, full occupancy status, having a low QM reported in the first publication, chain affiliation, and region. As shown in Table 2, the four characteristics that showed no cream skimming in the aggregate analysis—ADLs, diabetes, incontinence, and pressure ulcers—showed no evidence of cream skimming in the subsamples either, suggesting that the aggregation across types did not mask such behavior, if it existed.
Table 2.
Number of Quarter’s Postpublication in Which the Admission Cohort Is Significantly Lower Than the Last Quarter Prior to Publication
| Facility characteristics | % in pain | No. of ADLs | % with diabetes | % with incontinence | % with pressure ulcers | % with memory loss |
| Ownership | ||||||
| For profit | 12 | 0 | 0 | 0 | 0 | 6 |
| Nonprofit | 12 | 0 | 0 | 0 | 0 | 0 |
| Government | 0 | 0 | 0 | 0 | 0 | 0 |
| Full occupancy | ||||||
| 100% occupancy | 0 | 1 | 0 | 0 | 0 | 0 |
| 99% occupancy | 0 | 0 | 0 | 0 | 0 | 0 |
| 95% occupancy | 6 | 0 | 0 | 0 | 0 | 0 |
| Have low quality (bottom 20th percentile of the state quality measure distribution based on the November 2002 publication) | ||||||
| ADLs | NA | NA | NA | NA | NA | |
| Low quality | 0 | |||||
| Not low quality | 0 | |||||
| Pain | NA | NA | NA | NA | NA | |
| Low quality | 12 | |||||
| Not low quality | 9 | |||||
| Pressure ulcers | NA | NA | NA | |||
| Low quality | 0 | 0 | 0 | |||
| Not low quality | 0 | 0 | 0 | |||
| Low-risk incontinence (February 2004 publication) | NA | NA | NA | NA | NA | |
| Low quality | 1 | |||||
| Not low quality | 0 | |||||
| Chain affiliation | ||||||
| Part of a chain | 12 | 0 | 0 | 0 | 0 | 7 |
| Not part of a chain | 12 | 0 | 0 | 0 | 0 | 0 |
| Region | ||||||
| New England | 6 | 0 | 0 | 6 | 0 | 3 |
| Middle Atlantic | 11 | 0 | 0 | 3 | 0 | 0 |
| East North Central | 10 | 0 | 0 | 0 | 0 | 0 |
| West North Central | 10 | 0 | 0 | 1 | 0 | 0 |
| South Atlantic | 8 | 0 | 0 | 0 | 0 | 2 |
| East South Central | 1 | 1 | 0 | 0 | 0 | 1 |
| West South Central | 11 | 0 | 0 | 0 | 0 | 1 |
| Mountain | 12 | 0 | 0 | 0 | 0 | 0 |
| Pacific | 8 | 0 | 0 | 0 | 0 | 3 |
Note: ADLs = activities of daily living; NA = not applicable.
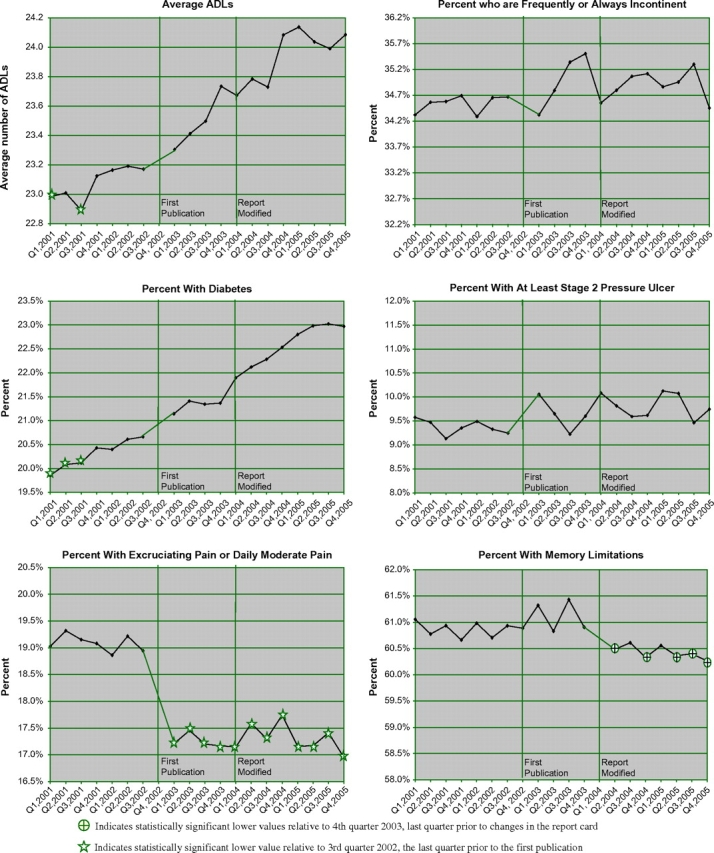
The evidence we found for cream skimming with respect to pain was also observed in the subsamples (Table 2), with partial support for the hypotheses we offered earlier. We found a tendency to cream skim among for-profit and nonprofit facilities but not among government-owned facilities. We found the same tendency to cream skim irrespective of chain affiliation but no uniformity across regions of the country. We did not find strong evidence for the hypothesized relationship between high occupancy and cream skimming possibly because of the small number of facilities with high occupancy, resulting in low power to detect significant effects. The most interesting finding is with respect to the published pain QM, as shown in Figure 2. Nursing homes with scores at the bottom 20th percentile of the state distribution for this QM exhibited a much stronger and sustained decline in the admission of patients with pain compared with facilities that had better scores for this QM.
Figure 2.
Percent of the admission cohort with excruciating or daily moderate pain stratified by the facility’s quality ranking based on the pain quality measure.
The aggregate analysis also indicated cream skimming (albeit to a lesser degree) with respect to memory loss, for five of the seven quarters after the modification of the report card. The stratified analyses (Table 2) found similar evidence of cream skimming among for-profit facilities, chain-affiliated facilities, and for one quarter among those with a low score on the incontinence QM, for which dementia and memory loss are considered a risk factor.
Discussion
The objective of this study was to investigate the possibility that nursing homes may have reacted to the publication of the Nursing Home Compare report card by adopting cream skimming admission policies. Adoption of such policies would not only have frustrated the intent of the report cards to promote quality improvement but also have in fact led to an unintended adverse outcome by limiting access to patients who need nursing home care the most. Despite the theoretical reasons for expecting nursing homes to engage in cream skimming, we found little evidence that they do. For only two of the six cohort characteristics we examined did we find any evidence that nursing homes have begun to admit healthier patients following the publication of the report card, and even for these two characteristics, the effect is not very large.
We also found very little evidence for cream skimming in the stratified analyses. It is particularly surprising that we found no evidence for cream skimming among the high-occupancy facilities, as they were predicted to be the most likely to engage in this behavior. It is possible that due to the small sample size, we did not have sufficient power to detect a response in this group.
We should note that the measures of cream skimming that we studied are not comprehensive, and nursing homes may have changed their admission policies in ways not captured in our study. However, we did include some of the most important characteristics that determine the health status and quality of life of long-term care patients. We should also note that we did not examine admissions of post-acute patients. These are typically Medicare patients who enter the nursing home following a hospital discharge for a short (several days to several weeks) stay for rehabilitation care and then are typically discharged home. Nursing Home Compare includes specific QMs reflecting the quality of care that these patients receive. There are, therefore, incentives for cream skimming for this patient population as well. Our findings may not necessarily generalize to this patient population because the Medicare market is different and the incentives might be different. A separate study would have to address this issue in the context of post-acute care.
The largest cream skimming effect we found was with respect to pain. Unlike the other admission characteristics we examined, pain is more likely to be subject to ascertainment bias and measurement error (Morris et al., 2003). It is, therefore, possible that the decline in the percent of admissions with pain that we found is a decline in the percent of recorded admissions with pain, rather than actual change in the type of patients being admitted. With the data we had, we are unable to rule out this possibility.
We also note that the type of study we present cannot separate out admission decisions made by nursing homes from those made by prospective patients and their families. One might wonder if the changes we observe are a reaction of consumers to the publication of the report card, rather than a cream skimming response by nursing homes. However, because we have examined aggregate changes in admission characteristics, it is likely that they reflect providers’ response. Consumers’ response is most likely to manifest itself in shifts in market shares and redistribution across nursing homes, as consumers are choosing the best among the nursing homes available to them in their local markets. It is much less likely to result in changes in the average characteristics across all nursing homes. Consumers’ response would lead to the aggregate results we observe only if (a) the published results reveal conditions in nursing homes considered to be so horrendous that patients prefer to avoid nursing home admission altogether or (b) the nursing homes with acceptable levels of quality are operating at full capacity and cannot accommodate any increase in demand and thus prospective patients who would have sought admission to these facilities prefer to stay at home. The latter is not likely as occupancies have been in the 80% range throughout the period we study.
The limited evidence for cream skimming that we observe suggests that the CMS initiative to report nursing home quality publicly has, by and large, avoided this adverse outcome to date. What might be the reasons for this and can we expect this to continue in the future? Several factors might be at play. First, financial incentives in some states may counteract the incentives to cream skim. Some state Medicaid reimbursement systems, which pay for the majority of the long-term care residents, are based on case mix, offering higher rates to nursing homes caring for sicker and frailer patients. If these rates are such that the profit margin is also higher for these patients, then nursing homes have a financial incentive to preferentially admit these patients, incentives that may overshadow the incentive to cream skim. Second, to engage in cream skimming, nursing homes have to view the report cards as very important in influencing their residual demand. A national survey conducted a year following the first publication (in 2004) found that less than 1% of nursing home administrators thought that the Nursing Home Compare report was a major factor influencing admission decisions by prospective patients (Mukamel, Spector, et al., 2007), indicating that perhaps the report card is not viewed as having sufficient influence on residual demand to provide strong incentives to cream skim. Third, nursing homes are constrained by the supply of patients they face, both in terms of number of patients and the type of patients seeking admission. Although they may wish to admit only patients who are relatively healthy, they may be faced with a clientele composed of mostly high-severity and frail patients. The increasing availability of assisted living and home care alternatives in long-term care markets have siphoned off demand by potential low–care need residents, leaving nursing home with a population that is increasingly sicker, making it difficult to cream skim. Finally, cream skimming, especially when prospective patients are becoming more severely ill and frail, may entail the opportunity cost of forgoing admissions that result in beds being empty for prolonged periods of time while waiting for a more desirable patient. Decreasing occupancies and increased competition between nursing homes (Mukamel, Spector, et al., 2007) increase these opportunity costs, making cream skimming less attractive. If these trends were to continue, then it is unlikely that nursing homes will revert to cream skimming strategies on a large scale in the coming years.
Funding
The authors gratefully acknowledge funding from the National Institutes on Aging, Grant AG023177.
References
- Castle NG. Nursing home administrators’ opinions of the nursing home compare web site. The Gerontologist. 2005;45:299–308. doi: 10.1093/geront/45.3.299. [DOI] [PubMed] [Google Scholar]
- Gormley WT, Weimer DL. Organizational report cards. Cambridge, MA: Harvard University Press; 1999. [Google Scholar]
- Harrington C, O’Meara J, Kitchener M, Simon LP, Schnelle JF. Designing a report card for nursing facilities: What information is needed and why. The Gerontologist. 2003;43:47–57. doi: 10.1093/geront/43.suppl_2.47. Spec No. 2. [DOI] [PubMed] [Google Scholar]
- Hawes C, Morris JN, Phillips CD, Mor V, Fries BE, Nonemaker S. Reliability estimates for the minimum data set for nursing home resident assessment and care screening (MDS) The Gerontologist. 1995;35:172. doi: 10.1093/geront/35.2.172. [DOI] [PubMed] [Google Scholar]
- Hawes C, Phillips CD, Mor V, Fries BE, Morris JN. MDS data should be used for research. The Gerontologist. 1992;32:563–564. doi: 10.1093/geront/32.4.563b. [DOI] [PubMed] [Google Scholar]
- Iezzoni LI, Ash AS, Shwartz M, Daley J, Hughes JS, Mackiernan YD. Judging hospitals by severity-adjusted mortality rates: The influence of the severity-adjustment method. American Journal of Public Health. 1996;86:1379–1387. doi: 10.2105/ajph.86.10.1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall MN, Shekelle PG, Leatherman S, Brook RH. The public release of performance data; what do we expect to gain? A review of the evidence. Journal of the American Medical Association. 2000;283:1866–1874. doi: 10.1001/jama.283.14.1866. [DOI] [PubMed] [Google Scholar]
- Mor V. Improving the quality of long-term care with better information. Milbank Quarterly. 2005;83:333–364. doi: 10.1111/j.1468-0009.2005.00405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris JN, Moore T, Jones R, Mor V, Angelelli J, Berg K, et al. Validation of long-term and post-acute care quality indicators. Cambridge, MA: Abt; 2003. No. CMS Contract No: 500-95-0062/T.O.#4. [Google Scholar]
- Mukamel DB. Risk adjusted outcome measures and quality of care in nursing homes. Medical Care. 1997;35:367–385. doi: 10.1097/00005650-199704000-00007. [DOI] [PubMed] [Google Scholar]
- Mukamel DB, Glance LG, Li Y, Weimer D, Spector WD, Zinn JS, et al. Does risk adjustment of the CMS quality measures for nursing homes matter? Medical Care. 2008;46:532–541. doi: 10.1097/MLR.0b013e31816099c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukamel DB, Mushlin AI. The impact of quality report cards on choice of physicians, hospitals and HMOs: A midcourse evaluation. Joint Commission Journal on Quality Improvement. 2001;27:20–27. doi: 10.1016/s1070-3241(01)27003-5. [DOI] [PubMed] [Google Scholar]
- Mukamel DB, Spector WD, Zinn JS, Huang L, Weimer D, Dozier A. Nursing homes’ response to the nursing home compare report card. Journal of Gerontology: Psychology Sciences and Social Sciences. 2007;62:S218–225. doi: 10.1093/geronb/62.4.s218. [DOI] [PubMed] [Google Scholar]
- Mukamel DB, Watson NM, Meng H, Spector WD, et al. Development of a risk-adjusted urinary incontinence outcome measure of quality for nursing homes. Medical Care. 2003;41:467–478. doi: 10.1097/01.MLR.0000053227.95476.02. [DOI] [PubMed] [Google Scholar]
- Mukamel DB, Weimer D, Mushlin A. Interpreting market share changes as evidence for effectiveness of quality report cards. Medical Care. 2007;45:1227–1232. doi: 10.1097/MLR.0b013e31812f56bb. [DOI] [PubMed] [Google Scholar]
- Mukamel DB, Weimer D, Spector WD, Ladd H, Zinn JS. Publication of the nursing home compare quality report card & trends in reported quality measures. Health Services Research. 2008;43:1244–1262. doi: 10.1111/j.1475-6773.2007.00829.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narins CR, Dozier AM, Ling FS, Zareba W. The influence of public reporting of outcome data on medical decision making by physicians. Archives of Internal Medicine. 2005;165:83. doi: 10.1001/archinte.165.1.83. [DOI] [PubMed] [Google Scholar]
- Robinowitz DL, Dudley RA. Public reporting of provider performance: Can its impact be made greater? Annual Review of Public Health. 2006;27:517–536. doi: 10.1146/annurev.publhealth.27.021405.102210. [DOI] [PubMed] [Google Scholar]
- Schneider EC, Epstein AM. Influence of cardiac-surgery performance reports on referral practices and access to care. New England Journal of Medicine. 1996;335:251. doi: 10.1056/NEJM199607253350406. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Value-driven health care. 2007. Retrieved August 15, 2007. [Google Scholar]
- Weisbrod BA. The nonprofit economy. 1st ed. Cambridge, MA: Harvard University Press; 1988. [Google Scholar]
- Werner RM, Konetzka RT, Stuart E, Norton EC, Park J. The impact of public reporting on quality of post-acute care. Washington, DC: AcademyHealth; 2008. [Google Scholar]
- Zinn JS, Spector WD, Weimer D, Mukamel D. Strategic orientation and nursing home response to public reporting of quality measures: An application of the miles and snow typology. Health Services Research. 2008;43:598–615. doi: 10.1111/j.1475-6773.2007.00781.x. [DOI] [PMC free article] [PubMed] [Google Scholar]