Abstract
Background
This study examined the racial differences in probabilities of transitioning across three disability levels of walking ½ mile in a community-dwelling population of older women.
Methods
The sample comprised 436 community-dwelling older women who were among the two-third least disabled women in Baltimore, Maryland. The levels of disability status of walking ½ mile included high functioning defined as reporting no difficulty, preclinical disability defined as reports of task modification but no reported difficulty, and disability defined as reported difficulty. First-order Markov transition models were specified to determine whether race influences the types of individual-level transitions between difficulty levels of walking ½ mile.
Results
Among high-functioning women, African Americans were more likely to be disabled at the next round than their White counterparts. African American women who began with preclinical disability were more likely to die before the next round. After adjusting for age, education, and perceived income inadequacy, African American women tended to have an increased risk of becoming disabled if preclinically disabled than White women.
Conclusions
Prevention through identification of individuals at an early phase of decline appears to be key to addressing racial disparities in physical disability even in later life.
Keywords: Racial disparities, Preclinical disability, Mobility disability, Walking
THE elimination of health disparities and the prevention of disability in later life are top public health priorities (1). However, African Americans older adults consistently exhibit higher rates of morbidity, mortality, and disability than White older adults (2,3). African American older adults also experience a higher incidence of mobility disability compared with their White counterparts (4–7). Mobility disability can subsequently lead to disability in activities of daily living and instrumental activities of daily living (8–11), for which there are persistent or increasing gaps in the prevalence and incidence between African American and White older adults (12–15). Given that racial minorities are more likely to experience disadvantages early in life, there is reason to believe that African American older adults experience earlier decline in physical function compared with White older adults. As the older segment of the population is growing larger and becoming more diverse and with the magnitude of the observed race-related differences, it is important to enhance our understanding of race effects at earlier stages in the course of disability.
This report adds to the extant body of literature that examines race differences in disability using data from a longitudinal study that is unique in its measurement of the early course of disability, such as preclinical disability, in older community-dwelling African American and White women. Though it is an area of growing interest, relatively few studies have measures of preclinical disability (8–11,15–18). Unlike previous studies that included measures of preclinical disability, we examined racial differences in the probabilities of transitioning across three disability levels of walking ½ mile and death in a community-dwelling population of older women. Specifically, we hypothesized that among initially high-functioning older women, older African American women experience more unfavorable transitions over the same observation period, compared with their White counterparts.
METHODS
Study Population
The Women's Health and Aging Study II (WHAS II) is a longitudinal cohort designed to understand the onset of disability in 436 high-functioning women aged 70–79 years in eastern Baltimore City and County, Maryland, at baseline (9). WHAS II eligibility criteria included self-reported task difficulty (in ≤1 out of 4 physical domains), Mini-Mental State Examination (MMSE) score ≥24 (19), and ability to participate in a clinical examination. Women were enrolled between 1994 and 1995, with exam every 18 months. Six rounds of data were used in this study. Due to delay in receiving funding, the 54-month follow-up was not performed (therefore, data are from 0, 18, 36, 72, 90, and 108 months). The Johns Hopkins Medical Institutions institutional review board approved all research protocols, and informed consent was obtained from all women. Our analyses included all 436 women.
Outcome Measures
Disability was derived from the following questions, “Have you had difficulty walking ½ mile?” and “Have you changed the way you walk or how often you do this, due to a health or physical condition?” Based on the women’s responses to these questions, they were classified into one of three disability levels. Women who reported no difficulty or task modification in walking ½ mile were considered high functioning (HF). Those who reported no difficulty and modification of walking ½ mile were defined as having preclinical mobility disability (PCD). Women who reported difficulty in walking ½ mile were classified as having disability (DIS).
Main Independent Variables
Women self-reported their race based on the following question, “Which of the following best describes your race?” Responses included: White, African American, and Other.
Covariates
Covariates were selected based on previous reports and their association with the progression and incidence of mobility disability (8–11,15,20). Demographic characteristics included age (years), formal education (years completed), lives alone (1 = yes; 0 = no), and perceived income inadequacy (1 = not having enough or just enough to make ends meet at the end of each month; 0 = having enough money at the end of the month). A count of prevalent chronic health conditions (osteoarthritis, high blood pressure, angina, congestive heart failure, diabetes, cancer, lung disease, stroke, hip fracture, rheumatoid arthritis, spinal stenosis, degenerative disk disease, peripheral arterial disease, and Parkinson’s disease) was ascertained based on medical record review and adjudication. Body mass index (BMI) was based on measured height and weight and calculated as weight (kg) divided by height (m)2. MMSE was used to assess the women’s cognitive functioning (19). The Geriatric Depression Scale was used to assess depressive symptomatology (21). Usual walking speed was assessed by having the participant walk her normal pace over a 4-m course. Walking aids were permitted. The faster of two trials constituted usual walking speed in meters per second.
Analytic Methods
Means and standard deviations and chi-square tests were used to examine the mean and proportional differences between baseline characteristics by race, respectively. Ninety-five percent confidence intervals (CI) were calculated using the Agresti–Coull method (22). To determine whether race influences the types of individual-level transitions between difficulty levels of walking ½ mile, we applied first-order Markov transition models (23). To illustrate, let Yit be a four-level indicator of difficulty of walking ½ mile for participant i at exam t (t = 1, …, 6), with Yit = 0, 1, 2, and 3 representing HF, PCD, DIS, and death, respectively; the transitions between difficulty level h at exam t − 1 to level k at exam t were modeled as a conditional multinomial logistic regression with HF as reference level for both Yit and Yit − 1: log it(Pr[Yit = k|Yit − 1 = h]) = β0k + β1kI1 + β2kI2 + β3kxi +β4kI1xi+ β5kI2xi + ziβ6k, k = 1, …, 3 and h = 0, 1, 2, where Pr[A|B] is the probability of event A given the occurrence of event B. We incorporated death as an absorbing state by assigning a probability of 0 to any subsequent state but death once death has occurred. The model included as predictors the binary indicators of the previous response (ie, I1 = 1 if h = 1, 0 otherwise; I2 = 1 if h = 2, 0 otherwise), race (x = 1 if African American, 0 if White), other covariates z, as well as the interactions between race and the indicators of the previous response for allowing the transition probabilities to vary by race. The parameters of primary interest include exp(β3k), exp(β3k + β4k), and exp(β3k + β5k), representing the odds ratios of transitioning, respectively, from HF, PCD, or DIS at time t − 1 to difficulty level k at time t comparing African American with White women. The standard multinomial logistic regression algorithm was used for parameter estimation. For ease of interpretation, we calculated crude and adjusted transition probabilities between levels of difficulty in walking ½ mile by race using the parameter estimates. We checked model assumptions and found no significant violations. All analyses were performed using Stata Version 9.2 statistical software (Stata Corp., College Station, TX).
RESULTS
The distribution of demographics by race is displayed in Table 1. Of the 436 older women in our sample, 80 were African American, 355 were White, and 1 reported herself as Other. African American women, on average, were younger, had fewer years of formal education, were more likely to perceive their income as inadequate, have a lower MMSE score, have a slower walking speed, and have a higher BMI than White women. African American women were similar to White women with respect to the average number of prevalent health conditions and their living status.
Table 1.
Select Baseline Characteristics by Race Among Women’s Health and Aging Study II Participants
| Characteristics | White (N = 355) | African American (N = 80) | p Value |
| Age, mean ± SD, y | 74.2 ± 2.8 | 73.4 ± 2.7 | .026 |
| Education, mean ± SD, y | 12.9 ± 3.1 | 10.6 ± 3.6 | <.001 |
| Number of prevalent health conditions (0–14), mean ± SD | 1.6 ± 1.1 | 1.5 ± 1.2 | .313 |
| MMSE (24–30), mean ± SD | 28.3 ± 1.7 | 27.3 ± 2.3 | <.001 |
| Body mass index, mean ± SD, kg/m2 | 26.1 ± 4.6 | 29.7 ± 6.5 | <.001 |
| Geriatric depression score (0–30), mean ± SD | 4.0 ± 3.8 | 4.1 ± 3.8 | .843 |
| Perceived income inadequacy, % | 14.5 ± 0.35 | 35.9 ± 0.48 | <.001 |
| Live alone, % | 51.3 ± 0.50 | 50.0 ± 0.50 | .838 |
| Usual walking speed, mean ± SD, m/s | 1.0 ± 0.27 | 0.90 ± 0.25 | <.001 |
Note: One woman reported being neither White nor African American. Tests of significance are for differences in means for continuous variables (ie, t test) and differences in proportions (ie, chi-square test) by race. A MMSE score greater than or equal to 24 was an eligibility criterion for the study. MMSE = Mini-Mental State Examination.
Unadjusted transition probabilities with associated 95% CIs stratified by race and prior disability level in walking ½ mile or death are displayed in Table 2. Relative to White women whose initial disability level of walking ½ mile was HF, African American women were less likely to remain HF (66.9% vs 78.5%) and more likely to be DIS (18.9% vs. 9.8%) at the next round. No racial differences in the probability of transitioning from HF to preclinical disability or death at the next round were observed. Among those women whose initial disability level of walking ½ mile was PCD (Preclinical disability row in Table 2), African American women had a greater probability of being dead at the next round (9.3% vs 2.4%; length of follow-up was 108 months) compared with White women. The probability of transitioning from PCD to DIS or remaining in the PCD level was similar for both African American and White older women. For those women who were initially DIS in walking ½ mile, probabilities of recovering from disability, remaining disabled, or dying was similar for African American and White women. To determine whether disability transitions varied for African American versus White women, we evaluated the −2 log likelihood by including versus not including the interaction between race and previous disability state as predictors in the Markov model (ie, likelihood ratio test), and the difference was not significant (p value = .276). For the specific transitions identified in Table 2 with an asterisk, p values for main and interaction terms from the Markov model were also <.05.
Table 2.
Unadjusted Probabilities of Disability Level in Walking ½ Mile or Death, Conditioned on Prior Disability Status and Race
| Status at Time t-1 | Probability of Disability Level or Death at time t (%) | |||
| High Functioning | Preclinical Disability | Disability | Dead | |
| High functioning | ||||
| African American | 66.9 (59.0–74.0)* | 11.5 (7.2–17.7) | 18.9 (13.4–26.0)* | 2.7 (0.8–7.0) |
| White | 78.5 (75.7–81.0) | 9.2 (7.5–11.3) | 9.8 (8.0–11.9) | 2.6 (1.7–3.8) |
| Preclinical disability | ||||
| African American | 27.9 (16.6–42.8) | 27.9 (16.6–42.8) | 34.9 (22.4–49.9) | 9.3 (12.6–29.5)* |
| White | 40.4 (33.2–48.0) | 27.1 (20.9–34.4) | 30.1 (23.6–37.5) | 2.4 (0.7–6.2) |
| Disability | ||||
| African American | 19.8 (12.6–29.5) | 10.5 (5.4–18.9) | 64.0 (53.4–73.3) | 5.8 (2.2–13.2) |
| White | 19.7 (15.4–24.8) | 10.2 (7.1–14.4) | 63.5 (57.7–69.0) | 6.6 (4.1–10.2) |
Notes: Ninety-five percent confidence intervals were calculated using the Agresti–Coull method.
The 95% confidence intervals do not overlap.
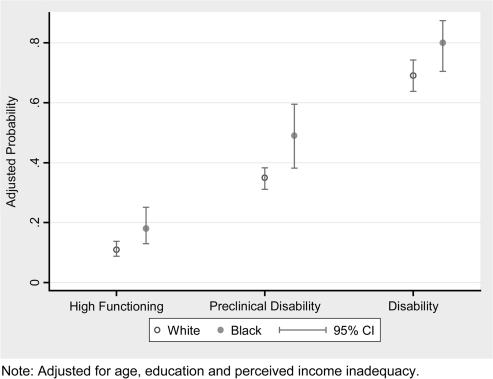
Adjusted probabilities for becoming or staying disabled in walking ½ mile are shown in Figure 1. After adjusting for age, education, and perceived income inadequacy, African American and White women had similar probabilities of becoming disabled in walking ½ mile, although African American women had a higher probability of transitioning to becoming disabled regardless of their previous disability status. Among women who started in a preclinical state (Preclinical disability in Figure 1), 48.7% (95% CI = 38.2–57.5) of African American women versus 34.6% (95% CI = 31.1–38.3) of White women became disabled by the next round. This increase in probability of becoming disabled reached borderline statistical significance (p = .08).
Figure 1.
Adjusted probabilities of incident (if high functioning or preclinically disabled) or persistent (if disabled) disability walking ½ mile, by previous disability status and race. Adjusted for age, education, and perceived income inadequacy.
DISCUSSION
In this study, we examined the racial differences in probabilities of transitioning across three disability levels of walking ½ mile and death in a community-dwelling population of older women. We found that African American women were associated with a higher probability of progressing to disability in walking ½ mile and death from the preclinical disability level. Accounting for age, education, and perceived income inadequacy, African American women were associated with a higher probability of becoming disabled in walking ½ mile, and this reached marginal significance for an interaction among African American women who were preclinically disabled at the prior round. Our findings suggest that PCD in walking ½ mile may be an important stage in understanding racial disparities in disability in late life.
Previous work demonstrated that preclinical disability is associated with a number of health outcomes including the mortality, nursing home admissions, hospitalizations, and the onset of disability (8–11). Furthermore, initial findings in this same cohort indicated that PCD predicted incident mobility disability (9). More recently, Miller and colleagues (15) found that both disability and PCD occur 10 years earlier in an inner-city African American men and women. This study adds to the literature by examining race differences in transitions in preclinical disability. The baseline prevalence of preclinical disability in this sample of older women was 40.3% in African American women and 28.9% in White women, which was higher than in a study of middle-aged African Americans by Miller and colleagues (15). The excess loss to mortality from PCD in African American women has several implications. Perhaps most importantly, it suggests that estimates of health disparities in disability may be lowered by prevalence bias, such that shorter cases of disability in African American women are less likely to be ascertained (24). Future studies examining racial disparities in disability should consider onset and duration of preclinical disability.
A recent review considered epidemiological criteria for screening as applied to preclinical disability (25). These findings provide further support to the idea that clinicians should screen high-functioning older patients for an increased risk of mobility decline by asking them if they have changed the method or frequency of walking. In individuals who respond in the affirmative, the next step is to perform a comprehensive assessment for medical causes of the change. Individuals who are not found to have a specific disease barrier, such as arthritis, nor a specific deficit, such as imbalance, should generally then be encouraged to participate in a walking, or similar, exercise program.
The similarities and differences observed in recovery are another important aspect of this study. Consistent with prior literature (6,7), we found that African American and White women had similar rates of recovery after developing difficulty in walking ½ mile. For example, in the middle section in Table 2, African American women were more likely to have difficulty or be dead at 18 months (44.2%) than to recover (27.9%), whereas White women were less likely to be worse (32.5%) than to recover (40.4%). This suggests that either recovery is less malleable after a person has reached disability than it is during preclinical disability or the factors that promote decline may differ by race, resulting in different effects for recovery and disablement.
Our study findings should be considered within the context of the following limitations. First, these results were obtained from mostly urban, community-dwelling women 70–79 years of age who represented the two-third least disabled women at study inception. Because it is not known if our results would differ in nonurban or noncommunity-dwelling environments, the external validity of our findings may be limited to this segment of the older population. Second, our measures of disability are based on reports that may be subject to response bias. We calculated the agreement between objectively measured physical function (ie, walking speed) and self-reported disability status of walking ½ mile in White women compared with that in African American women by calculating kappa coefficients (comparing slowest half walking speed or walking speed <1.0 m/s with self-report) and Spearman’s rho (comparing walking speed tertiles with self-report). Also we compared the average change in walking speed associated with a change in self-report using linear regression in White and African American women. In both instances, we failed to find a substantive or statistical difference in agreement between objective and self-reported physical function between the two groups.
In summary, among this community-dwelling population of high-functioning older women, our findings indicate that when African American women begin to decline in physical function (indicated by walking ½ mile), they decline quicker than White women, particularly among those women in the PCD stage. That is, over the same time interval, African American women had more progress from high functioning to disabled and from preclinically disabled to death than White women. Prevention through identification of individuals at an early phase of decline appears to be a key to addressing disparities in physical disability in later life. Preclinical disability may identify an important window in which recovery is more modifiable.
FUNDING
This research was supported by the National Institute on Aging (NIA) grant R01 AG11703 and by the National Institutes of Health-National Center for Research Resources grant M01-RR000052 at the Johns Hopkins School of Medicine. The first author was supported by a training grant from the NIA (T32AG000120). The second author is supported by Robert Wood Johnson Harold Amos Medical Faculty Development Program, and NIA P30 AG021334-04
References
- 1.Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. 1st ed. Washington, DC: National Academies Press; 2002. [PubMed] [Google Scholar]
- 2.US Department of Health and Human Services. Healthy People 2010. Washington, DC: US Department of Health and Human Services; 2001. [Google Scholar]
- 3.US Department of Health and Human Services. Tracking Healthy People 2010. Washington, DC: US Department of Health and Human Services: 2000. [Google Scholar]
- 4.Freedman VA, Martin LG, Schoeni RF. Recent trends in disability and functioning among older adults in the United States: a systematic review. JAMA. 2002;288(24):3137–3146. doi: 10.1001/jama.288.24.3137. [DOI] [PubMed] [Google Scholar]
- 5.Song J, Chang HJ, Tirodkar M, Chang RW, Manheim LM, Dunlop DD. Racial/ethnic differences in activities of daily living disability in older adults with arthritis: a longitudinal study. Arthritis Rheum. 2007;57(6):1058–1066. doi: 10.1002/art.22906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Melzer D, Izmirlian G, Leveille SG, Guralnik JM. Educational differences in the prevalence of mobility disability in old age: the dynamics of incidence, mortality, and recovery. J Gerontol B Psychol Sci Soc Sci. 2001;56(5):S294–S301. doi: 10.1093/geronb/56.5.s294. [DOI] [PubMed] [Google Scholar]
- 7.Clark DO, Stump TE, Wolinsky FD. Predictors of onset of and recovery from mobility difficulty among adults aged 51-61 years. Am J Epidemiol. 1998;148(1):63–71. doi: 10.1093/oxfordjournals.aje.a009561. [DOI] [PubMed] [Google Scholar]
- 8.Wolinsky FD, Miller DK, Andresen EM, Malmstrom TK, Miller JP, Miller TR. Effect of subclinical status in functional limitation and disability on adverse health outcomes 3 years later. J Gerontol A Biol Sci Med Sci. 2007;62(1):101–106. doi: 10.1093/gerona/62.1.101. [DOI] [PubMed] [Google Scholar]
- 9.Fried LP, Bandeen-Roche K, Chaves PH, Johnson BA. Preclinical mobility disability predicts incident mobility disability in older women. J Gerontol A Biol Sci Med Sci. 2000;55(1):M43–M52. doi: 10.1093/gerona/55.1.m43. [DOI] [PubMed] [Google Scholar]
- 10.Fried LP, Young Y, Rubin G, Bandeen-Roche K. WHAS II Collaborative Research Group. Self-reported preclinical disability identifies older women with early declines in performance and early disease. J Clin Epidemiol. 2001;54(9):889–901. doi: 10.1016/s0895-4356(01)00357-2. [DOI] [PubMed] [Google Scholar]
- 11.Wolinsky FD, Miller DK, Andresen EM, Malmstrom TK, Miller JP. Further evidence for the importance of subclinical functional limitation and subclinical disability assessment in gerontology and geriatrics. J Gerontol B Psychol Sci Soc Sci. 2005;60(3):S146–S151. doi: 10.1093/geronb/60.3.s146. [DOI] [PubMed] [Google Scholar]
- 12.Clark DO. US trends in disability and institutionalization among older blacks and whites. Am J Public Health. 1997;87(3):438–440. doi: 10.2105/ajph.87.3.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kelley-Moore JA, Ferraro KF. The black/white disability gap: persistent inequality in later life? J Gerontol B Psychol Sci Soc Sci. 2004;59(1):S34–S43. doi: 10.1093/geronb/59.1.s34. [DOI] [PubMed] [Google Scholar]
- 14.Mendes de Leon CF, Barnes LL, Bienias JL, Skarupski KA, Evans DA. Racial disparities in disability: recent evidence from self-reported and performance-based disability measures in a population-based study of older adults. J Gerontol B Psychol Sci Soc Sci. 2005;60(5):S263–S271. doi: 10.1093/geronb/60.5.s263. [DOI] [PubMed] [Google Scholar]
- 15.Miller DK, Wolinsky FD, Malmstrom TK, Andresen EM, Miller JP. Inner city, middle-aged African Americans have excess frank and subclinical disability. J Gerontol A Biol Sci Med Sci. 2005;60(2):207–212. doi: 10.1093/gerona/60.2.207. [DOI] [PubMed] [Google Scholar]
- 16.Fried LP, Guralnik JM. Disability in older adults: evidence regarding significance, etiology, and risk. J Am Geriatr Soc. 1997;45(1):92–100. doi: 10.1111/j.1532-5415.1997.tb00986.x. [DOI] [PubMed] [Google Scholar]
- 17.Fried LP, Bandeen-Roche K, Williamson JD, et al. Functional decline in older adults: expanding methods of ascertainment. J Gerontol A Biol Sci Med Sci. 1996;51(5):M206–M214. doi: 10.1093/gerona/51a.5.m206. [DOI] [PubMed] [Google Scholar]
- 18.West SK, Munoz B, Rubin GS, Bandeen-Roche K, Broman AT, Turano KA. Compensatory strategy use identifies risk of incident disability for the visually impaired. Arch Ophthalmol. 2005;123(9):1242–1247. doi: 10.1001/archopht.123.9.1242. [DOI] [PubMed] [Google Scholar]
- 19.Folstein MF, Folstein SE, McHugh PR. Mini-Mental State.” A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 20.Thorpe RJ, Kasper JD, Szanton SL, Frick KD, Fried LP, Simonsick EM. Relationship of race and poverty to lower extremity function and decline: findings from the Women’s Health and Aging Study. Soc Sci Med. 2008;66(4):811–821. doi: 10.1016/j.socscimed.2007.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1983;17(1):37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 22.Brown L, Cai TT, DasGupta A. Interval estimation for a binomial proportion. Stat Sci. 2001;16(2):101–133. [Google Scholar]
- 23.Diggle PJ, Lian KY, Zeger SL. Analysis of Longitudinal Data. Oxford, England: Oxford University Press; 1994. [Google Scholar]
- 24.Gill TM, Hardy SE, Williams CS. Underestimation of disability in community-living older persons. J Am Geriatr Soc. 2002;50(9):1492–1497. doi: 10.1046/j.1532-5415.2002.50403.x. [DOI] [PubMed] [Google Scholar]
- 25.Weiss CO, Hoenig HM, Fried LP. Compensatory strategies used by older adults facing mobility disability. Arch Phys Med Rehabil. 2007;88(9):1217–1220. doi: 10.1016/j.apmr.2007.07.007. [DOI] [PubMed] [Google Scholar]