Abstract
Objectives
The National Social Life, Health, and Aging Project (NSHAP) data contain multiple indicators of social connectedness, social participation, social support, and loneliness among older adults. We suggest that these indicators can be combined to measure two aspects of social isolation: social disconnectedness (i.e., physical separation from others) and perceived isolation (i.e., feelings of loneliness and a lack of social support). We use the NSHAP data to create scales measuring social disconnectedness and perceived isolation and examine their distribution among older adults.
Methods
We assess the reliability of the scales using Cronbach’s alpha and item-total correlations and perform confirmatory factor analysis to test the model against the data. Finally, we test differences in scale means across subgroups to assess the distribution of social disconnectedness and perceived isolation among older adults.
Results
We find that 17 indicators combine into two reliable scales. The social disconnectedness scale has a two-factor structure, including the restricted social network dimension and the social inactivity dimension. The perceived isolation scale also comprises two dimensions: lack of support and loneliness. We find that social disconnectedness does not vary across age groups, but the oldest old feel more isolated than the young old. Social disconnectedness and perceived isolation are greater among those who have worse health.
Discussion
The creation of scales measuring social disconnectedness and perceived isolation provides one way to utilize the wide variety of indicators of social isolation collected in the NSHAP study. Although individual indicators of social connectedness or isolation are useful in their own right, these scales provide parsimonious, continuous variables that account for a variety of aspects of social isolation, which may be especially useful for inclusion in multivariate analyses predicting health outcomes.
Keywords: Loneliness, Social isolation, Social networks, Social participation, Social support
Previous research has identified social isolation as a risk factor for physical and mental health problems (e.g., Berkman, 1995; Cacioppo & Hawkley, 2003; Cacioppo, Hughes, Waite, Hawkley, & Thisted, 2006; House, 2001). Socially disconnected and lonely individuals tend to suffer higher rates of morbidity and mortality (Taylor, Repetti, & Seeman, 1997; Thoits, 1995) as well as infection (Cohen, Doyle, Skoner, Rabin, & Gwaltney, 1997; Pressman et al., 2005), depression (Heikkinen & Kauppinen, 2004), and cognitive decline (Wilson et al., 2007). The mere presence of another individual can alleviate stress (Cohen & Williamson, 1991; Thoits), whereas feelings of loneliness may exacerbate the physiological effects of stress, resulting in elevated cortisol levels (Hawkley, Burleson, Berntson, & Cacioppo, 2003; Steptoe, Owen, Kunz-Ebrecht, & Brydon, 2004) and blood pressure (Hawkley et al).
The purpose of this article is to demonstrate the development of scales capturing social disconnectedness and perceived isolation using data from the National Social Life, Health, and Aging Project (NSHAP). We use procedures of scale construction to combine multiple indicators of isolation into a scale assessing social disconnectedness and a scale capturing perceived isolation. We then examine the relationship between disconnectedness and perceived isolation and assess their distributions across age, gender, and self-rated health among older adults. Our aim is not to present these scales as definitive measures but to encourage further work toward elucidating the concept, causes, and consequences of social isolation among older adults.
Social Isolation Among Older Adults
The examination of social isolation among older adults is particularly important for a number of reasons. First, there is some evidence that social isolation may become more common with increasing age. Older adults tend to have smaller social networks (McPherson, Smith-Lovin, & Brashears, 2006) and are more likely to experience feelings of loneliness (Dykstra, van Tilburg, & de Jong Gierveld, 2005). This may be due, in part, to older adults’ experiences of bereavement and their greater likelihood of living alone (Kramarow, 1995; Li & Ferraro, 2005). The correspondence of these conditions has led to the assumption that diminishing social networks result in lower levels of perceived social support and increased loneliness.
However, recent research suggests that changes across the life course in social connectedness and satisfaction may be heterogeneous. For example, data from NSHAP indicate that the oldest old have greater participation than the young old (Cornwell, Laumann, & Schumm, 2008), and other research suggests that loneliness may peak in middle age (Carstensen, Isaacowitz, & Charles, 1999). Accordingly, social connectedness, support, and loneliness may not be inextricably linked, especially among older adults. In the face of shrinking social networks, older adults may develop closer relationships and shift expectations so that decreasing connectedness does not necessarily result in the perception of isolation (Lang & Carstensen, 1994; Schnittker, 2007).
Finally, to the extent that social isolation is associated with worse health, it may pose a particularly severe risk for older adults. Older adults are more likely to experience bereavement and develop health problems, both of which may increase their need for social support and companionship. As a result, social isolation may be particularly deleterious for older adults. Indeed, research indicates that older adults who experience one or another aspect of isolation have been found to be at greater risk for all-cause mortality, increased morbidity, depression, and cognitive decline (Brummett et al., 2001; Cacioppo & Hawkley, 2003; House, Landis, & Umberson, 1988; Sherbourne, Meredith, Rogers, & Ware, 1992; Tomaka, Thompson, & Palacios, 2006).
Measuring Social Isolation
The variety of indicators of isolation and loneliness used across research in different disciplines is both a blessing and a curse. This work has captured an enormous number of facets of individuals’ everyday social worlds. Indicators of isolation in previous research include living alone (Dean, Kolody, Wood, & Matt, 1992; Hughes & Gove, 1981; Waite & Hughes, 1999), being unmarried (Lillard & Waite, 1995; Ross, 1995), having a small social network (Berkman & Syme, 1979; Seeman, Berkman, Blazer, & Rowe, 1994), infrequent contact with network members (Brummett et al., 2001), a lack of social network diversity (Barefoot, Gronbaek, Jensen, Schnohr, & Prescott, 2005), a perceived lack of social support (Blazer, 1982; Krause, 1987; Lin, Ye, & Ensel, 1999; Wethington & Kessler, 1986), low participation in social activities (Benjamins, 2004; Ellison & George, 1994; Thoits & Hewitt, 2001), emotionally distant relationships (Uno, Uchino, & Smith, 2002), and feelings of loneliness or not belonging (Cacioppo et al., 2006; Hawkley et al., 2003). However, most of this work has been limited to the examination of only one or two indicators of isolation (or connectedness), or it has focused on only one conceptual area, such as support, participation, or loneliness. As a result, it is difficult to discern whether multiple features of isolation might combine to create particularly severe situations of social isolation among the oldest old. It is also unclear whether feelings of loneliness and a lack of social support do, in fact, follow the loss of social network ties or if more subjective appraisals of isolation are separate from objective features of isolation.
In efforts to consolidate multiple measures of social isolation, several authors have previously identified central components of isolation. For example, van Baarsen, Snijders, Smit, and van Duijn (2001) distinguish between social loneliness, as the lack of integration and companionship, and emotional loneliness, as the lack of an attachment figure. De Jong Gierveld and Hagestad (2006) similarly contrast isolation (as the opposite of integration) with loneliness (as the opposite of embeddedness). Following these distinctions and building from the disciplinary approaches of both sociology and psychology, we suggest two distinct aspects of social isolation. Social disconnectedness can be characterized by a lack of contact with others and indicated by situational factors, such as a small social network, infrequent interaction, and a lack of participation in social activities and groups. Perceived isolation, on the other hand, can be characterized by the subjective experience of a shortfall in one’s social resources such as companionship and support. Individuals who are socially disconnected may have small social networks, interact with network members infrequently, and rarely participate in social activities. On the other hand, individuals who perceive themselves to be isolated may report feelings of loneliness and perceive a lack of social support from friends and family members.
Social disconnectedness and perceived isolation are related, but we hypothesize that they are distinct. Some research indicates, for example, that feelings of loneliness are responsive to changes in network size, but other findings indicate only a modest correlation between disconnectedness and perceived isolation (Hawkley et al., 2003; Hughes, Waite, Hawkley, & Cacioppo, 2004; Schnittker, 2007). Although physical separation from others and feelings of loneliness may go hand-in-hand for some individuals, infrequent social interaction may not lead to feelings of loneliness for others. Alternatively, people who are socially active and embedded within an expansive social network may feel socially isolated if their relationships lack emotional closeness and support.
METHODS
We use data from NSHAP, a nationally representative, population-based study of community-residing older adults. From summer 2005 to spring 2006, NSHAP conducted in-person interviews with 3,005 individuals, ages 57–85 years. The study achieved a final weighted response rate of 75.5%. NSHAP used a modularized questionnaire design so that some questions were included in a leave-behind questionnaire for a randomly selected subset of respondents. Detailed information about the NSHAP study design may be found in O’Muircheartaigh, Eckman, and Smith (in press).
NSHAP includes a wide variety of indicators of social connectedness, support, and activity, as well as feelings of loneliness. Measures such as network size, frequency of interaction with network members, participation in social groups, and perceived support can be reversed to indicate the lack of these social resources. We seek to combine all these items into reliable scales of social disconnectedness and perceived isolation. Scale creation is typically used to measure constructs that cannot be adequately or directly assessed using one or two indicators. Therefore, by combining indicators that theoretically covary with objective isolation and subjective isolation, we can create a parsimonious proxy measure for these two constructs (DeVellis, 2003).
Scale Construction
We will begin by selecting items for each scale based on their content validity, determined by previous research suggesting that these items may be indicative of objective or subjective isolation. Assessments of scale reliability indicate how strongly the scale’s items are correlated with each other. Because we assume that the items in the two scales are indicative of objective social isolation and subjective social isolation, we also expect that the items within each respective scale will be interrelated. Two measures indicate the extent of interrelation among scale items. First, item-rest correlations, or the correlations between each item and the set of other items included in the scale, provide a measure of the scale’s internal consistency. Second, the proportion of total variation in the scale that is shared by the included items is indicated by Cronbach’s (1951) alpha coefficient. Alpha coefficients greater than .70 typically connote acceptable overall scale reliability (DeVellis, 2003; Nunnally, 1978). Finally, we examine whether the scales retain acceptable internal consistency reliability across sociodemographic characteristics.
We create the social disconnectedness and perceived isolation scales by retaining items that maximize internal consistency reliability. Scale scores are calculated for each respondent by standardizing the retained items (so that M = 0 and SD = 1) and dividing the sum of the standardized values by the total number of nonmissing items. This method enables the calculation of a valid scale score as long as a respondent has responded to at least one item included in the scale. Scores on each scale may then be interpreted as a standardized variable. A score of zero indicates that the respondent provided the mean response for each of the included items. Positive scores indicate greater-than-average isolation, whereas negative scores indicate lower-than-average isolation.
Confirmatory Factor Analysis
We conduct confirmatory factor analysis to test the factor structures expected to underlie each scale, as described subsequently. We assess the standardized loadings for each factor, which can be interpreted as the correlations between the observed variables and the unobserved variables. We also consider the overall fit of each hypothesized model to the sample using three goodness-of-fit indices. The χ2 statistic compares the tested model with a saturated model, with the null hypothesis that the tested model is a good fit. However, the test is sensitive to sample size (Joreskog, 1969), so this may not be a useful indicator for the present study. The comparative fit index indicates how well the specified model fits compared with a baseline model. Higher values indicate a better fit, and values above 0.90 are generally considered to indicate a good fit (Diamantopoulos & Sigaw, 2000). The root mean square error of approximation (RMSEA) indicates the closeness of the fit of the model in relation to its degrees of freedom. Previous research has suggested that values less than .05 indicate a close fit (Browne & Cudeck, 1993).
Distribution of Social Isolation
We assess the distributions of social disconnectedness and perceived isolation by comparing mean scale scores across age, gender, and self-rated health among NSHAP respondents. Because previous research has been inconclusive regarding whether social isolation increases with age, differences in the social isolation scales according to age will be of particular interest.
RESULTS
The Social Disconnectedness Scale
We propose that social disconnectedness can be assessed using items capturing two central factors: a lack of social network robustness and a lack of participation in social activities. Based on their content validity, we initially identified 13 items for inclusion in the social disconnectedness scale. The internal consistency of the scale was maximized by removing five items: neighborhood socializing, frequency of attendance at religious services, living alone/household size, partnership status, number of children, and number of grandchildren. Eight variables were retained. Detailed information on their measurement is presented in Table 1.
Table 1.
Summary Statistics for Indicators of Social Isolation Collected in NSHAP
| Measure | M or proportiona | SD | n |
| Social network characteristics | |||
| Social network size (range = 0–5, 6 or more) | 3.57 | 1.59 | 3,001 |
| Social network range (number of types of relationships in the network; range = 0–5) | 2.41 | 1.07 | 3,005 |
| Proportion of social network members who live in the household (range = 0–1) | 0.29 | 0.31 | 2,932 |
| Average frequency of interaction with network members (range = 0–1 where 0 = the respondent does not contact any alters and 1 = respondent contacts all alters every day) | 0.57 | 0.26 | 2,931 |
| Average closeness with network members (average of responses across all alters, where 1 = not very close, 2 = somewhat close, 3 = very close, and 4 = extremely close) | 3.15 | 0.54 | 2,928 |
| Living arrangements | |||
| Household size (range = 1–11) | 2.06 | 1.08 | 2,988 |
| Living alone (1 = respondent lives alone; 0 = all else) | 0.23 | 0.45 | 2,988 |
| Number of friends and family members | |||
| Spouse or current partner (1 = respondent has a spouse or current partner; 0 = all else) | 0.73 | 0.47 | 3,005 |
| Number of friends (How many friends would you say you have? 0 = none, 1 = 1 friend, 2 = 2–3 friends, 3 = 4–9 friends, 4 = 10–20 friends, and 5 = more than 20) | 3.31 | 1.30 | 2,808 |
| Number of children (sum of respondent’s living sons and daughters) | 2.94 | 2.13 | 2,782 |
| Number of grandchildren (respondent’s living grandchildren) | 5.24 | 6.11 | 2,777 |
| Social participation | |||
| Attending religious services (from 0 = never to 6 = several times a week) | 3.27 | 2.11 | 2,990 |
| Attending meetings of an organized group (from 1 = never to 7 = several times a week) | 2.66 | 2.15 | 2,454 |
| Socializing with friends and relatives (from 1 = never to 7 = several times a week) | 4.39 | 1.30 | 2,472 |
| Socializing with neighbors (1 = hardly ever to 5 = daily or almost every day) | 1.35 | 1.28 | 2,370 |
| Volunteering (1 = never to 7 = several times a week) | 2.20 | 2.08 | 2,454 |
| Social support | |||
| How often can you… (1 = often, 2 = some of the time, and 3 = hardly ever [or never]) | |||
| Open up to members of your family? | 1.68 | 0.71 | 2,797 |
| Rely on members of your family? | 1.41 | 0.65 | 2,793 |
| Open up to your friends? | 1.97 | 0.73 | 2,704 |
| Rely on your friends? | 1.68 | 0.71 | 2,860 |
| Open up to your spouse or partner? | 1.27 | 0.54 | 2,012 |
| Rely on your spouse or partner? | 1.16 | 0.45 | 2,007 |
| Loneliness | |||
| How often do you… (1 = hardly ever [or never], 2 = some of the time, and 3 = often) | |||
| Feel that you lack companionship? | 1.41 | 0.61 | 2,415 |
| Feel left out? | 1.32 | 0.54 | 2,409 |
| Feel isolated from others? | 1.26 | 0.51 | 2,416 |
Note: NSHAP, National Social Life, Health, and Aging Project.
Survey adjusted and weighted to account for the probability of selection, with poststratification adjustments for nonresponse.
We include in the social disconnectedness scale four measures from the NSHAP social network module, which was based on the General Social Survey and described in Cornwell, Laumann, Schumm, and Graber (in press). Social network characteristics such as size, range, frequency of interaction, and geographical proximity of network members have been used in previous research to describe the collection of people with whom a given individual interacts and may rely on for social support (Haines & Hurlbert, 1992; Lin et al., 1999). Network measures also, therefore, can be used to reveal relative deficiencies in one’s social connectedness. A small or nonexistent network, a network that is geographically dispersed, or infrequent interaction with one’s network members, for example, may each indicate some level of physical separation from others.
Social network size indicates the number of individuals with whom the respondent can discuss important matters. Social network range captures the extent to which a respondent’s network comprises different types of relationships. Those who have greater network range are less apt to be socially isolated because they have a larger variety of individuals (e.g., a spouse, family member, friend, coworker) with whom they can interact. The proportion of social network members who live in the household provides a rough estimate of the physical proximity of one’s network members. Individuals who have a smaller proportion of their network members residing with them have fewer opportunities for interaction and may experience more objective isolation than those who reside with a larger proportion of their network members. Finally, frequency of contact with network members indicates an individual’s exposure to his network members.
We also incorporate an indicator of the respondent’s number of friends. Respondents indicated how many people they considered to be their “closest friends” and those who were “pretty good friends,” excluding spouses and family members. This provides another assessment of the social connections available to individuals, in addition to the network roster. The number of friends provides a rough indicator of social connectedness with others, regardless of the respondent’s ability and/or willingness to discuss “important matters” with these people. This question was modularized so that a random two thirds of respondents answered the question during the in-person interview and one third responded to the question on the leave-behind questionnaire. Mean response does not differ according to the collection mode.
We initially included several other variables generally assessing the extent of the respondent’s universe of friends and family members and his or her contact with them. First, living alone is one of the most widely used indicators of social isolation, and it typically indicates some degree of physical separation from others. We tested both a dummy variable indicating whether the respondent lived alone and a measure of household size, but the item-rest correlations for both variables were below .20, and the inclusion of either variable decreased the shared variance among the scale items. Our finding that living alone or having a small household do not contribute to objective isolation, as measured here, supports previous findings that living arrangements are not necessarily indicative of social isolation (Waite & Hughes, 1999).
We also began with several variables that provide counts of the respondent’s family members, since being single and having fewer children and grandchildren may be associated with social disconnectedness among older adults. We initially included in the social disconnectedness scale a dummy variable indicating partnership status and counts of the respondent’s number of children and number of grandchildren. However, these items were removed from the scale because their item-total correlations were below .30 and their exclusion increased the overall internal consistency reliability of the scale.
Participation in social activities such as organized group involvement, volunteering, and attendance at religious services has been used by previous research as indicators of social connectedness (Ellison & George, 1994; McIntosh, Sykes, & Kubena, 2002). We selected several items indicating participation in social groups or activities for inclusion in the social disconnectedness scale. NSHAP respondents were asked about their frequency of volunteer work, attending meetings of an organized group, and getting together socially with friends or relatives. We also initially included assessments of the frequency of socializing with neighbors and attending religious services but removed these items to improve the internal consistency reliability of the scale.
The resulting social disconnectedness scale includes the eight items shown in Table 2. These items were standardized and averaged to create the scale, and then the scores were reversed because the variables initially measured connectedness rather than isolation. Scores on the social disconnectedness scale range from −1.30 to 2.34, with a weighted M of −0.02 and SD of 0.63. Social disconnectedness scores above zero are indicative of greater-than-average disconnectedness, whereas scores below zero suggest lower-than-average disconnectedness. In general, higher scores indicate greater isolation.
Table 2.
Reliability of the Social Disconnectedness and Perceived Isolation Scales, by Age Groups and Gender
| Item-rest correlations |
||||||
| Overall | Age groups |
Gender |
||||
| 57–64 | 65–74 | 75–85 | Female | Male | ||
| Social Disconnectedness Scale | ||||||
| Social network size | 0.64 | 0.68 | 0.63 | 0.63 | 0.61 | 0.67 |
| Social network range | 0.49 | 0.54 | 0.49 | 0.47 | 0.42 | 0.55 |
| Frequency of interaction | 0.35 | 0.41 | 0.30 | 0.33 | 0.31 | 0.39 |
| Proportion of alters in the home | 0.45 | 0.52 | 0.48 | 0.35 | 0.34 | 0.53 |
| Number of friends | 0.33 | 0.34 | 0.33 | 0.32 | 0.36 | 0.33 |
| Attending group meetings | 0.43 | 0.43 | 0.43 | 0.41 | 0.47 | 0.37 |
| Socializing with family and friends | 0.32 | 0.32 | 0.33 | 0.30 | 0.35 | 0.27 |
| Volunteering | 0.41 | 0.39 | 0.41 | 0.43 | 0.43 | 0.38 |
| Cronbach’s alpha for scale | 0.73 n = 3,005 | 0.76 n = 1,020 | 0.73 n = 1,092 | 0.71 n = 893 | 0.72 n = 1,550 | 0.74 n = 1,455 |
| Perceived Isolation Scale | ||||||
| Open up to family | 0.31 | 0.33 | 0.31 | 0.29 | 0.33 | 0.29 |
| Rely on family | 0.37 | 0.40 | 0.36 | 0.36 | 0.36 | 0.39 |
| Open up to friends | 0.27 | 0.26 | 0.30 | 0.23 | 0.26 | 0.28 |
| Rely on friends | 0.33 | 0.34 | 0.33 | 0.31 | 0.34 | 0.31 |
| Open up to spouse/partner | 0.39 | 0.35 | 0.39 | 0.44 | 0.45 | 0.35 |
| Rely on spouse/partner | 0.31 | 0.30 | 0.32 | 0.28 | 0.35 | 0.30 |
| Feel that you lack companionship | 0.40 | 0.46 | 0.39 | 0.37 | 0.45 | 0.36 |
| Feel isolated | 0.46 | 0.49 | 0.45 | 0.44 | 0.48 | 0.44 |
| Feel left out | 0.47 | 0.54 | 0.46 | 0.42 | 0.52 | 0.43 |
| Cronbach’s alpha for scale | 0.70 n = 2,939 | 0.71 n = 1,005 | 0.69 n = 1,072 | 0.68 n = 862 | 0.73 n = 1,511 | 0.67 n = 1,428 |
Scale reliability.—
This combination of the eight items retained in the scale maximized the internal consistency reliability with a Cronbach's alpha of .73, and all item-rest correlations were moderate to strong. The Social disconnectedness scale has acceptable reliability across age groups and gender, as shown in Table 2. Item-rest correlations for the scale are also remarkably similar across these subgroups, and nearly all of them are at least moderate in strength. The only exception is the variable indicating (a lack of) socializing with family and friends, for which the item-rest correlation falls to .27 among men.
Confirmatory factor analysis.—
Results from a confirmatory factor analysis indicate that the data support a two-factor structure, with dimensions similar to those we described earlier. The four network items load on a restricted social network dimension, and the three social participation variables load on a social inactivity dimension. One surprise was that the lack of friends is more reflective of social inactivity than a restricted social network. This indicator has a standardized loading of 0.58 on the inactivity dimension. Each of the items has moderate to strong loadings on the corresponding dimension. The correlation between the restricted network dimension and the inactivity dimension is moderate in strength, at .43.
Fit statistics generally indicate a good fit of the model to the data. The χ2 statistic is significant (χ2 = 35.14, p < .001), indicating that we cannot reject the null hypothesis that the model does not fit the data. However, this statistic is likely inflated by the large sample size (Joreskog, 1969). The comparative fit index of 1.00 is well above the threshold of 0.90 for indication of a good fit compared with the baseline mode (Diamantopoulos & Sigaw, 2000). The RMSEA of 0.035 indicates that the model is a close fit to the data because it is lower than the typical cutoff of 0.05 (Browne & Cudeck, 1993).
The Perceived Isolation Scale
We also constructed a scale of subjective, or perceived, isolation. Based on their content validity, we began scale construction with 10 items from the NSHAP data indicating one’s perception of the supportiveness, closeness, adequacy, and companionship provided by one's social relationships. We retained nine items, which fall into two general categories: a perceived lack of support and loneliness. Descriptions of these items are presented in Table 1.
Six of the nine items in the perceived isolation scale capture the respondent’s assessment of social support available from family, friends, and one’s spouse or current partner. These questions are drawn from the 2002 Health and Retirement Study. Respondents were asked how often they can open up to their spouse or current partner, family members, and friends and how often they can rely on people from these three groups. The perception that one can rarely access emotional and instrumental support from friends and family may contribute to perceived isolation.
Because loneliness is based on the perception of having fewer (or less close) interpersonal relationships than one would like (van Baarsen et al., 2001), we consider it here as a facet of subjective social isolation. We incorporate responses to the three-item loneliness scale developed by Hughes and colleagues (2004) and examined in Shiovitz-Ezra, Leitsch, Graber, and Karraker (in press). The loneliness scale includes items assessing the respondent’s perceived lack of companionship and frequency of feeling left out and isolated (Hughes et al.).
We also examined the possibility of including a variable assessing average emotional closeness with one’s network members. We expected that low emotional closeness with network members would indicate perceived isolation. However, this item had a low item-rest correlation (.22) and its removal increased the scale’s overall internal consistency (although the improvement was marginal, from .69 to .70). We therefore removed this item from the scale. Most respondents indicated that their relationships with network members were quite close, so a lack of cases at the low end of this variable may have reduced its fit with the scale. More importantly, the item’s lack of fit with the scale indicates that the quality of one’s relationships may be conceptually distinct from the perception of isolation.
Table 2 lists the nine items retained in the perceived isolation scale. The items were standardized and their values were averaged to arrive at a score for perceived isolation. The scale ranges from −0.98 to 3.63, with a weighted M of −0.01 and SD of 0.59. Higher scores indicate greater perceived isolation.
Scale reliability—
The resulting scale has a Cronbach’s alpha of .70, indicating acceptable internal consistency. Each of the item-rest correlations exceeds the cutoff of .20 for satisfactory reliability (Kline, 1986). With the exception of the item assessing one’s ability to open up to his or her friends, all the item-rest correlations are above .30. The scale also demonstrates acceptable reliability across age groups and gender, as shown in Table 2. Although the Cronbach's alpha coefficients drop slightly below .70 for the middle-old and oldest-old age groups, as well as for males, the differences across subgroups are small. Item-rest correlations across the age and gender subgroups range from .23 to .30, with the vast majority of these correlations being above .30.
Confirmatory factor analysis—
Results from a confirmatory factor analysis indicate that six items assessing social support load on a perceived lack of support dimension, and the three items from the short loneliness scale load on a loneliness dimension. Standardized loadings exceed 0.60, with the exception of the item regarding reliance on one’s spouse, which has a standardized loading of 0.32 on the perceived lack of support dimension. The correlation between the perceived lack of support dimension and the loneliness dimension (.19) is weak to moderate in strength.
Fit statistics generally indicate an acceptable fit of the model to the data. The χ2 statistic is significant (χ2 = 52.60, p < .001), indicating that we cannot reject the null hypothesis that the model does not fit the data. This statistic should be used with caution, however, because it is likely inflated by the large sample size (Joreskog, 1969). Both the comparative fit index (0.99) and the RMSEA (0.040) exceed conventional thresholds (Browne & Cudeck, 1993; Diamantopoulos & Sigaw, 2000), thereby indicating that the model has an acceptably close fit to the data.
Social Disconnectedness and Perceived Isolation Among Older Adults
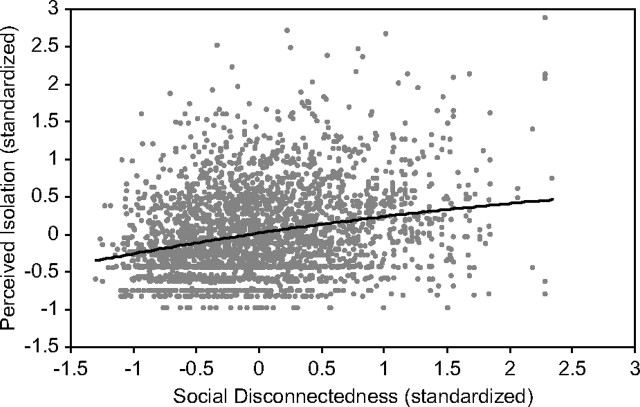
Most previous research has found only a modest correlation between aspects of disconnectedness and perceived isolation (Hawkley et al., 2003; Hughes et al., 2004; Mirowsky & Ross, 1986). As depicted in Figure 1, the social disconnectedness and perceived isolation scales are positively correlated, but the correlation is weak to moderate in strength (r = .25, p < .001). Individuals who lack social connections are more likely to feel isolated. However, some people who have many social connections still feel lonely, whereas others who have very few social connections do not feel lonely at all.
Figure 1.
Scatter plot of social disconnectedness and perceived isolation.
What is the distribution of the experience and perception of social isolation within a population-based sample of older adults? We provide a brief examination of this by considering mean scores for the social disconnectedness and perceived isolation scales across age, gender, and self-rated health of the older adults in our sample.
Previous research indicates that loneliness increases with age (Dykstra et al., 2005) and social connectedness may decline with age (McPherson et al., 2006), although other work has suggested that older adults may adjust their social networks and expectations so that they are no more isolated or lonely than their younger counterparts (Lang & Carstensen, 1994; Schnittker, 2007). As shown in Table 3, we find very little difference in social disconnectedness across age groups. The oldest old do not have fewer connections than the younger old, on average, but the perception of isolation does increase with age. The oldest old have significantly higher scores for perceived isolation than the youngest old (p < .01).
Table 3.
Means and Standard Deviations for Social Disconnectedness and Perceived Isolation, by Age Groups, Gender, and Self-Rated Health
| Social disconnectedness |
Perceived isolation |
|||
| Ma | SD | Ma | SD | |
| Overall | –0.02 | 0.63 | –0.01 | 0.59 |
| Age groups | ||||
| 57–64 (reference) | –0.01 | 0.65 | –0.04 | 0.59 |
| 65–74 | –0.04 | 0.62 | –0.03 | 0.58 |
| 75–85 | –0.01 | 0.62 | 0.08** | 0.61 |
| Gender | ||||
| Female (reference) | –0.10 | 0.60 | –0.06 | 0.60 |
| Male | 0.06*** | 0.66 | 0.05*** | 0.58 |
| Self-rated health | ||||
| Excellent/very good (reference) | –0.14 | 0.61 | –0.09 | 0.53 |
| Good | 0.03*** | 0.63 | –0.01** | 0.61 |
| Fair/poor | 0.13*** | 0.63 | 0.16*** | 0.64 |
Means are survey adjusted and weighted to account for the probability of selection, with poststratification adjustments for nonresponse. Significance levels from Wald tests of differences in means are presented for subgroups.
**p < .01; ***p < .001.
With respect to gender, previous research suggests that social network size does not significantly differ for men and women (McPherson et al., 2006). However, women are more likely to participate in social activities and voluntary associations (Sherkat & Ellison, 1999; Wilson, 2000), and they tend to experience less loneliness than men (Borys & Perlman, 1985). But this previous work has not focused specifically on late adulthood, when widowhood, retirement, health changes, and other factors may shift individuals’ opportunities for social engagement (Ferraro, 1984; Li & Ferraro, 2005). As indicated in Table 3, we find that women have significantly lower scores for both social disconnectedness and perceived isolation (p < .001), on average. Older women, therefore, are less likely than men to suffer social disconnectedness or perceived isolation than older men.
Finally, nearly all the indicators of isolation that we have combined in these two scales have associated with worse health in previous research (see, e.g., Berkman, 1995; Cacioppo & Hawkley, 2003; House, 2001; House et al., 1988). We therefore expect that both social disconnectedness and perceived isolation will be negatively related to self-rated health. Indeed, we find higher levels of social disconnectedness and perceived isolation among older adults who have worse health. More specifically, older adults who rated their health as “very good” or “excellent” had below average levels of both social disconnectedness and perceived isolation. But those who have “good,” “fair,” or “poor” health also have significantly greater scores on the social isolation scales. The gradient observed here—where both social disconnectedness and perceived isolation increase as self-rated health decreases—suggests a broad relationship between social isolation and health. Further research is needed to elucidate the causal order in the relationships between health and various aspects of social isolation and to assess the relative effects of social disconnectedness and perceived isolation on particular health outcomes.
DISCUSSION
By combining multiple indicators of social isolation collected in the NSHAP study, we have developed two reliable scales assessing social disconnectedness and perceived isolation. Our results indicate that these two dimensions of isolation are related but distinct. Individuals who have small social networks or rarely participate in social activities do not necessarily feel lonely. Furthermore, one may be surrounded by friends and family but perceive a lack of social support and feel left out.
Because so many different aspects of social isolation have been separately examined in previous research, this work has been inconclusive regarding whether social isolation increases with age. Our findings show that social disconnectedness is not more marked among the oldest old compared with the young old. However, the oldest old are more likely to perceive themselves as isolated than the young old. Further research is needed to understand the source of the greater feelings of loneliness and the perceived lack of social support that are more common among oldest adults.
The creation of scales measuring social disconnectedness and perceived isolation provides one way to use the wide variety of indicators of social isolation collected in the NSHAP study. These scales also recognize an important fact about the complexity of individuals’ everyday social lives: No single indicator of perceived or actual social isolation can fully assess the degree to which an individual lacks social resources or outlets for socializing, feels that emotional and material support are unavailable in times of need, or yearns for companionship. Further research is needed to assess the validity of these scales and refine the measurement of social disconnectedness and perceived isolation. At the most basic level, we argue that the combination of multiple measures is imperative for the assessment of social isolation.
The social disconnectedness and perceived isolation scales available in the NSHAP data bring a number of benefits for future research. First, because the scales are continuous variables, they enable analysis of the functional form of the relationship between disconnectedness and perceived isolation and specific health outcomes. We can assess, for example, whether social isolation exerts a gradual or threshold effect on health. The scales also allow researchers to take into account a number of aspects of isolation using a parsimonious indicator, which is especially useful for inclusion in multivariate analyses predicting health outcomes. Most importantly, the scales will enable comparison of the specific health risks brought by a lack of social connections versus perceived isolation. We hope that these analyses will move us closer to understanding the mechanisms through which each form of isolation may threaten health and well-being among the growing population of community-residing older adults.
FUNDING
We are grateful for comments and suggestions from Benjamin Cornwell, Louise Hawkley, Edward Laumann, Martha McClintock, Sanyu Mojola, and Phil Schumm.
Acknowledgments
The NSHAP is supported by the National Institute on Aging, Office of Women's Health Research, Office of AIDS Research, and the Office of Behavioral and Social Science Research (5R01AG021487).
References
- Barefoot JC, Gronbaek M, Jensen G, Schnohr P, Prescott E. Social network diversity and risks of ischemic heart disease and total mortality: Findings from the Copenhagen City Heart Study. American Journal of Epidemiology. 2005;161:960–967. doi: 10.1093/aje/kwi128. [DOI] [PubMed] [Google Scholar]
- Benjamins MR. Religion and functional health among the elderly: Is there a relationship and is it constant? Journal of Aging and Health. 2004;16:355–374. doi: 10.1177/0898264304264204. [DOI] [PubMed] [Google Scholar]
- Berkman LF. The role of social relations in health promotion. Psychosomatic Medicine. 1995;57:245–254. doi: 10.1097/00006842-199505000-00006. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Syme L. Social networks, host resistance, and mortality: A nine-year follow-up study of Alameda County residents. American Journal of Epidemiology. 1979;109:186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- Blazer DG. Social support and mortality in an elderly community population. American Journal of Epidemiology. 1982;115:684–694. doi: 10.1093/oxfordjournals.aje.a113351. [DOI] [PubMed] [Google Scholar]
- Borys S, Perlman D. Gender differences in loneliness. Personality and Social Psychology Bulletin. 1985;11:63–74. [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage Publications; 1993. [Google Scholar]
- Brummett BH, Barefoot JC, Siegler IC, Clapp-Channing NE, Lytle BL, Bosworth HB, Williams RB, Mark DB. Characteristics of socially isolated patients with coronary artery disease who are at elevated risk for mortality. Psychosomatic Medicine. 2001;63:267–272. doi: 10.1097/00006842-200103000-00010. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC. Social isolation and health, with an emphasis on underlying mechanisms. Perspectives in Biology and Medicine. 2003;46:S39–S52. [PubMed] [Google Scholar]
- Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychology and Aging. 2006;21:140–151. doi: 10.1037/0882-7974.21.1.140. [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Isaacowitz DM, Charles ST. Taking time seriously: A theory of socioemotional selectivity. American Psychologist. 1999;54:165–181. doi: 10.1037//0003-066x.54.3.165. [DOI] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM., Jr. Social ties and susceptibility to the common cold. Journal of the American Medical Association. 1997;277:1940–1944. [PubMed] [Google Scholar]
- Cohen S, Williamson GM. Stress and infectious disease in humans. Psychological Bulletin. 1991;109:5–24. doi: 10.1037/0033-2909.109.1.5. [DOI] [PubMed] [Google Scholar]
- Cornwell B, Laumann E, Schumm P. The social connectedness of older adults: A national profile. American Sociological Review. 2008;73:185–203. doi: 10.1177/000312240807300201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell B, Laumann E, Schumm LP, Graber J. The social networks of older adults: Network members in health and medical matters. Journals of Gerontology: Social Sciences. in press [Google Scholar]
- Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- de Jong Gierveld J, Hagestad GO. Perspectives on the integration of older men and women. Research on Aging. 2006;28:627–637. [Google Scholar]
- Dean A, Kolody B, Wood P, Matt GE. The influence of living alone on depression in elderly persons. Journal of Aging and Health. 1992;4:3–18. [Google Scholar]
- DeVellis RF. Thousand Oaks, CA: Sage Publications; 2003. Scale development: Theory and applications. [Google Scholar]
- Diamantopoulos A, Sigaw J. Introducing LISREL. London: Sage; 2000. [Google Scholar]
- Dykstra PA, van Tilburg TG, de Jong Gierveld J. Changes in older adult loneliness: Results from a seven-year longitudinal study. Research on Aging. 2005;27:725–747. [Google Scholar]
- Ellison CG, George LK. Religious involvement, social ties, and social support in a southeastern community. Journal for the Scientific Study of Religion. 1994;33:46–61. [Google Scholar]
- Ferraro KF. Widowhood and social participation in later life: Isolation or compensation? Research on Aging. 1984;6:451–468. [Google Scholar]
- Haines VA, Hurlbert JS. Network range and health. Journal of Health and Social Behavior. 1992;33:254–266. [PubMed] [Google Scholar]
- Hawkley LC, Burleson MH, Berntson GG, Cacioppo JT. Loneliness in everyday life: Cardiovascular activity, psychosocial context, and health behaviors. Journal of Personality and Social Psychology. 2003;85:105–120. doi: 10.1037/0022-3514.85.1.105. [DOI] [PubMed] [Google Scholar]
- Heikkinen R, Kauppinen M. Depressive symptoms in late life: A 10-year follow-up. Archives of Gerontology and Geriatrics. 2004;38:239–250. doi: 10.1016/j.archger.2003.10.004. [DOI] [PubMed] [Google Scholar]
- House JS. Social isolation kills, but how and why? Psychosomatic Medicine. 2001;63:273–274. doi: 10.1097/00006842-200103000-00011. [DOI] [PubMed] [Google Scholar]
- House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241:540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Hughes M, Gove WR. Living alone, social integration, and mental health. American Journal of Sociology. 1981;87:48–74. doi: 10.1086/227419. [DOI] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging. 2004;26:655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joreskog KG. A general approach to confirmatory maximum likelihood factor analysis. Psychometrika. 1969;34:183–202. [Google Scholar]
- Kline P. A handbook of test construction: Introduction to psychometric design. New York: Methuen; 1986. [Google Scholar]
- Kramarow EA. The elderly who live alone in the United States: Historical perspectives on household change. Demography. 1995;32:335–352. [PubMed] [Google Scholar]
- Krause N. Satisfaction with social support and self-rated health in older adults. The Gerontologist. 1987;27:301–308. doi: 10.1093/geront/27.3.301. [DOI] [PubMed] [Google Scholar]
- Lang FR, Carstensen LL. Close emotional relationships in late life: Further support for proactive aging in the social domain. Psychology and Aging. 1994;9:315–324. doi: 10.1037//0882-7974.9.2.315. [DOI] [PubMed] [Google Scholar]
- Li Y, Ferraro KF. Volunteering and depression in later life: Social benefit or selection processes? Journal of Health and Social Behavior. 2005;46:68–84. doi: 10.1177/002214650504600106. [DOI] [PubMed] [Google Scholar]
- Lillard LA, Waite LJ. ‘Til death do us part:’ Marital disruption and mortality. American Journal of Sociology. 1995;100:1131–1156. [Google Scholar]
- Lin N, Ye X, Ensel WM. Social support and depressed mood: A structural analysis. Journal of Health and Social Behavior. 1999;40:344–359. [PubMed] [Google Scholar]
- McIntosh WA, Sykes D, Kubena KS. Religion and community among the elderly: The relationship between the religious and secular characteristics of their social networks. Review of Religious Research. 2002;44:109–125. [Google Scholar]
- McPherson M, Smith-Lovin L, Brashears ME. Social isolation in America: Changes in core discussion networks over two decades. American Sociological Review. 2006;71:353–375. [Google Scholar]
- Mirowsky J, Ross CE. Social patterns of distress. Annual Review of Sociology. 1986;12:23–45. [Google Scholar]
- Nunnally JC. Psychometric theory. 2nd ed. New York: McGraw-Hill; 1978. [Google Scholar]
- O’Muircheartaigh C, Eckman S, Smith S. Statistical design and estimation for the National Social Life, Health, and Aging Project (NSHAP) Journals of Gerontology: Social Sciences. in press doi: 10.1093/geronb/gbp045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pressman SD, Cohen S, Miller GE, Barkin A, Rabin BS, Treanor JJ. Loneliness, social network size, and immune response to influenza vaccination in college freshmen. Health Psychology. 2005;24:297–306. doi: 10.1037/0278-6133.24.3.297. [DOI] [PubMed] [Google Scholar]
- Ross CE. Reconceptualizing marital status as a continuum of social attachment. Journal of Marriage and the Family. 1995;57:129–140. [Google Scholar]
- Schnittker J. Look (closely) at all the lonely people: Age and the social psychology of social support. Journal of Aging and Health. 2007;19:659–682. doi: 10.1177/0898264307301178. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Berkman LF, Blazer DG, Rowe JW. Social ties and support and neuroendocrine function: The MacArthur studies of successful aging. Annals of Behavioral Medicine. 1994;16:95–106. [Google Scholar]
- Sherbourne CD, Meredith LS, Rogers W, Ware JE., Jr. Social support and stressful life events: Age differences in their effects on health-related quality of life among the chronically ill. Quality of Life Research. 1992;1:235–246. doi: 10.1007/BF00435632. [DOI] [PubMed] [Google Scholar]
- Sherkat DE, Ellison CG. Recent developments and current controversies in the sociology of religion. Annual Review of Sociology. 1999;25:363–394. [Google Scholar]
- Shiovitz-Ezra S, Leitsch S, Graber J, Karraker A. Quality of Life and Psychological Health Indicators in the National Social Life, Health, and Aging Project. Journals of Gerontology: Social Sciences. in press doi: 10.1093/geronb/gbn020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Owen N, Kunz-Ebrecht SR, Brydon L. Loneliness and neuroendocrine, cardiovascular, and inflammatory stress responses in middle-aged men and women. Psychoneuroendocrinology. 2004;29:593–611. doi: 10.1016/S0306-4530(03)00086-6. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Repetti RL, Seeman TE. Health psychology: What is an unhealthy environment and how does it get under the skin? Annual Review of Psychology. 1997;48:411–447. doi: 10.1146/annurev.psych.48.1.411. [DOI] [PubMed] [Google Scholar]
- Thoits P. Stress, coping, and social support processes: Where are we? What next? Journal of Health and Social Behavior. 1995;35:53–79. (Extra Issue) [PubMed] [Google Scholar]
- Thoits PA, Hewitt LN. Volunteer work and well-being. Journal of Health and Social Behavior. 2001;42:115–131. [PubMed] [Google Scholar]
- Tomaka J, Thompson S, Palacios R. The relation of social isolation, loneliness, and social support to disease outcomes among the elderly. Journal of Aging and Health. 2006;18:359–384. doi: 10.1177/0898264305280993. [DOI] [PubMed] [Google Scholar]
- Uno D, Uchino BN, Smith TW. Relationship quality moderates the effect of social support given by close friends on cardiovascular reactivity in women. International Journal of Behavioral Medicine. 2002;9:243–262. doi: 10.1207/s15327558ijbm0903_06. [DOI] [PubMed] [Google Scholar]
- van Baarsen B, Snijders TAB, Smit JH, van Duijn MA. Lonely but not alone: Emotional isolation and social isolation as two distinct dimensions of loneliness in older people. Educational and Psychological Measurement. 2001;61:119–135. [Google Scholar]
- Waite LJ, Hughes ME. At risk on the cusp of old age: Living arrangements and functional status among Black, White, and Hispanic adults. Journal of Gerontology. 1999;54B:S136–S144. doi: 10.1093/geronb/54b.3.s136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wethington E, Kessler RC. Perceived support, received support, and adjustment to stressful life events. Journal of Health and Social Behavior. 1986;27:78–89. [PubMed] [Google Scholar]
- Wilson J. Volunteering. Annual Review of Sociology. 2000;26:215–240. [Google Scholar]
- Wilson RS, Krueger KR, Arnold SE, Schneider JA, Kelly JF, Barnes LL, Tang Y, Bennett DA. Loneliness and risk of Alzheimer disease. Archives of General Psychiatry. 2007;64:234–240. doi: 10.1001/archpsyc.64.2.234. [DOI] [PubMed] [Google Scholar]