Abstract
Aims
The aim of the study was to find the epidemiology of hip fractures in heart failure. The increasing survival rate for patients with heart failure places them at risk for other diseases of ageing, including osteoporosis.
Methods and results
We included 5613 persons from the Cardiovascular Health Study (CHS) with an average of 11.5 year follow-up. We determined incidence rates and hazard ratios (HRs) in persons with heart failure compared with persons without heart failure and mortality hazards following these fractures. Annualized incidence rates for hip fractures were 14 per 1000 person-years in heart failure and 6.8 per 1000 person-years without heart failure. Unadjusted and multivariable adjusted HRs for hip fracture associated with heart failure in men were 1.87 (95% CI 1.2–2.93) and 1.59 (95% CI 0.93–2.72), respectively. Respective HRs for women were 1.75 (95% CI 1.27–2.4) and 1.41 (95% CI 0.98–2.03). Mortality hazard was ∼2-fold greater in patients with heart failure and hip fracture compared with those having heart failure alone.
Conclusion
Persons with heart failure are at high risk for hip fractures. However, much of the association between hip fractures and heart failure is explained by shared risk factors. Hip fractures are a substantial contributor to mortality in men and women with heart failure.
Keywords: Hip fractures, Heart failure, Mortality
Introduction
Osteoporosis and heart failure are prevalent conditions, particularly among the elderly.1–3 Worldwide, over 1.7 million hip fractures, the most serious fracture related to osteoporosis, occur annually with over 340 000 occurring in the USA alone.1,2 In the USA, heart failure is the most common cause of hospitalization in patients aged >65.3 However, whether hip fracture rates are increased in persons with heart failure compared with healthy persons is a subject of ongoing debate. One report, limited to women, suggested that the odds ratio for hip fractures was increased 2–3-fold in heart failure patients compared with healthy controls matched to the expected hip fracture age distribution.4 In a population-based study in Canada including over 16 000 men and women aged 65 years and older, patients with heart failure had an ∼4-fold increased risk for any fractures and a 6-fold increased risk for hip fractures. However, in this study, the comparator group was patients with cardiovascular disease without heart failure, and not healthy controls.5 Thus, whether there is an increased risk for hip fractures in men and women with heart failure compared with healthy controls and if so, whether the risk of fractures in heart failure is a function of the disease itself, or underlying shared risk factors, is less clear.
There are a number of shared risk factors for hip fractures and heart failure. These include, among others, decreased exercise tolerance,6,7 low levels of 25 hydroxyvitamin D,8,9 advancing age, renal disease,10–12 diabetes10,13,14 and, among women, postmenopausal status.15 In addition, medications used by persons with heart failure, including thiazide diuretics,16 spironolactone,17 angiotensin-converting enzyme (ACE) inhibitors18 and β–blockers,19 have been positively associated with bone metabolism. Conversely, loop diuretics have been associated with loss of bone mineral density (BMD), a risk for fractures in some20 but not all studies.21 Importantly, poor self-reported health status has also been identified to be a risk factor for both heart failure and low BMD.22–24
Theoretically, the pathophysiology of heart failure and osteoporotic fractures may share some common components. Experimental studies suggest that aldosteronism, a key component in heart failure,25 may also be operative in bone loss.26,27 Another potential common pathophysiological mechanism for heart failure and osteoporotic fractures is that of shared matrix proteins.28 Up-regulation of putative cytokines may also underlie the pathogenesis of both heart failure and osteoporosis.28 Finally, one study reported that inflammatory markers are elevated in heart failure,29 and inflammation has been associated with fractures.30,31
No study to date has compared hip fracture rates and mortality rates, following these fractures in those with and without heart failure within the context of a large prospective study of ambulatory, multiethnic, non-institutionalized women and men that uniformly collected data on hip fractures, mortality, and heart failure status. Moreover, no study to date has examined whether any relationship between hip fractures and heart failure is independent of shared risk factors. The primary objective of this study was to examine the association between heart failure and hip fractures and to determine whether this was dependent or independent of shared risk factors. The secondary purposes were to examine the association between heart failure and hip fractures in those with systolic compared with diastolic dysfunction, and to estimate the contribution of hip fractures to mortality in persons with heart failure.
We hypothesized that relative to persons without heart failure, that rates of hip fractures in those with heart failure would be increased. However, we suspected that these increased rates of hip fractures would be explained at least in part by shared risk factors. Finally, since mortality is increased following a hip fracture in healthy persons,32 we hypothesized that there would be a substantial association of hip fractures with mortality in persons with heart failure.
To test these hypotheses, we utilized data from a well-characterized community-based longitudinal cohort study of older men and women, the Cardiovascular Health Study (CHS). We determined the risk for incident hip fractures in men and women with heart failure and by the type of heart failure compared with those without heart failure with and without adjustments for potential covariates. We estimated the mortality due to incident hip fractures in men and women with heart failure.
Methods
Subjects
Cardiovascular Health Study is a longitudinal cohort study of elderly men and women (age ≥65 years) designed to determine the factors that predict development and progression of cardiovascular disease. The main cohort of 5201 participants was enrolled between 10 June 1989 and 30 May 1990. To increase minority representation of African Americans in the study, an additional 687 African Americans were recruited from 17 November 1992 through 11 June 1993. Within four community-based centres (Sacramento County, CA; Forsyth County, NC; Washington County, MD; Allegheny County, PA), a random sample of men and women from Medicare eligibility lists were identified. Participants were excluded if they were institutionalized, required a proxy, were unable to complete informed consent, were planning to move out of the area within 3 years of recruitment, required a wheelchair in the home, were receiving hospice care, or were undergoing radiation or chemotherapy for cancer. Annual examinations and 6 month interim phone calls were performed.
Analysis cohort
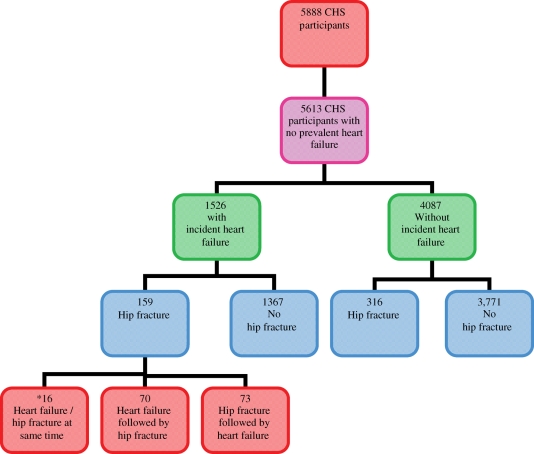
There were 5888 participants in the CHS. Self-report of heart failure at baseline was confirmed by components of the baseline examination, or where necessary, by a validation protocol that included either the review of medical records or surveys of treating physicians (prevalent heart failure).33 After exclusion of the 275 persons with prevalent heart failure at their baseline examination, there remained 5613 persons in our analyses, including 3251 women (58%) and 864 African Americans (15.4%) (Figure 1).
Figure 1.
Cardiovascular Health Study analyses cohort for heart failure and hip fractures. Asterisk denotes patients not included in time-dependent analyses.
Definition of incident heart failure
Participants were queried by telephone interview or during in-clinic visits every 6 months regarding hospitalizations. Diagnoses of incident heart failure were ascertained from obtained hospital records with centralized cardiologist adjudication. Potential incident heart failure was investigated in detail based on initial identification through International Classification of Disease (ICD) diagnostic codes, or mention of this endpoint on the hospital face sheet, discharge summary, or outpatient procedure report. An additional quality-control procedure matched Medicare Part A inpatient data provided by the Health Care Financing Administration (HCFA) to the events database, to ensure ascertainment of all hospitalized heart failure events occurring within the cohort.34 For the purposes of our analyses, among those adjudicated to have incident clinical heart failure, we defined systolic heart failure as an ejection fracture (EF) of <40% and diastolic heart failure as an EF of ≥40% by echocardiograms obtained at the time closest to the diagnosis of incident heart failure (baseline or year 7 of CHS).35
Ascertainment of incident hip fractures
Participants were queried by telephone interview or in-clinic visit every 6 months regarding incident fractures. Diagnoses of incident hip fractures were ascertained from a comprehensive review of hospital records and included those in which there was an International Classification of Diseases, Ninth Revision (ICD-9) code for hip fracture (820.xx). ICD-9 codes for hip fractures that occurred in this cohort included the codes 820.0-820.03, 820.08, 820.09, 820.20, 820.21, 820.22, 820.29, 820.80, and 820.90.
Covariates
We considered as covariates in our models factors previously associated with hip fracture in both the general population,36,37 and in persons with cardiovascular diseases,4 where available in CHS. For one covariate not available in CHS, depth perception,37 we substituted history of visual problems.
Age, body mass index (BMI), age at menopause, number of live births, sex, race, education, income, use of calcium supplements (yes/no), smoking status (never, former, current), frailty status [frail (defined as 3 or more of the following: unintentional loss of >10 pounds in past year, self-reported exhaustion, weak grip strength, slow walking speed, and low physical activity), intermediate (defined as 1 or 2 of the above criteria), or not frail],38 self-described health status (excellent/very good vs. good vs. fair/poor), alcohol use (never, past, current <1 drink/week, current 1 to <7 drink/week, or 7 or more drinks/week),39 history of hypo- or hyperthyroidism, medication use [corticosteroids, oestrogen use (in women only: never, past, current), ACE inhibitors, angiotensin-receptor blockers (ARBs), β-blockers, diuretics),40 physical activity levels (total kcal/week), gait speed (computed from the time to walk 15 ft. test), cystatin C,41 digital symbol substitution test (DSS) (for this test participants were asked to pair nine numbers with nine symbols, and the number correctly completed in 90 s was recorded)],42 and history of cancer, pneumonia, chronic obstructive pulmonary disease and diabetes were considered in the models. No participants were using bisphosphonates or raloxifene at baseline. These covariates were obtained from a participant's baseline visit for all objectives.
Statistical analyses
We computed summary statistics at baseline for all participants and for two subgroups defined by whether ever having an incident heart failure during study follow-up. We report means with standard deviations for continuous variables and counts with percentages for categorical variables. Comparisons were done using t tests for mean values and χ2 tests for percentages. In modelling we used Cox proportional-hazards models estimating hazard ratios (HRs). We used scaled Schoenfeld residuals for both graphical and other tests. We used plots of Schoenfeld residuals against time for each covariate with a smoothing spline fit. We further used them in a correlation test using a χ2 test for each covariate and a global χ2 test, testing a linear trend in the hazard.
To evaluate the association of first hip fracture and heart failure, incident heart failure was modelled as a time-varying exposure. Participants diagnosed with incident heart failure contributed exposure time at risk for hip fractures to the non-heart failure group before their heart failure diagnosis and to the heart failure group after their heart failure diagnosis. Once a participant was diagnosed with incident heart failure, they could not later be categorized as not having heart failure. Each participant's observation time ends at the time of incident hip fracture event, of death, of loss or end to follow-up, whichever occurred first. Covariates at baseline were used as predictors.
To evaluate the association of hip fracture and incident heart failure type (reduced EF vs. preserved EF), we used only participants diagnosed with incident heart failure and without previous hip fracture. We computed time to incident hip fracture event since the incident heart failure and heart failure type was the primary predictor. All covariates were used from the visit closest to the incident heart failure event.
To examine the association of incident heart failure, hip fracture, and mortality, both incident heart failure and incident hip fracture were defined as time-varying covariates. Mortality HRs were determined for those with heart failure alone, those with hip fractures alone, and those with incident heart failure preceded or followed by an incident hip fracture. The reference group was no incident heart failure and no incident hip fracture. We also estimated mortality hazards for those with incident heart failure alone compared with those with incident heart failure and incident hip fracture. A person could contribute his person-time into up to three categories, e.g. a person who has developed a heart failure and then fractured his hip would contribute into the reference group first, then into heart failure alone group and last into the heart failure followed by hip fracture group.
All models were stratified by sex because of previous reports, albeit in populations without heart failure, of sex differences in hip fracture incidence and in mortality following these fractures.43 This approach allows not only for different HRs but also for different baseline hazards for men and women.
The original plan was to adjust models for all proposed covariates, regardless of the statistical significance of their association with the outcome. However, a proportion of participants had missing values for at least one covariate. The approach of excluding participants with at least one missing covariate was not taken to avoid selection bias. Multiple imputation techniques could also easily bias the results. Instead, backwards stepwise regression was used to eliminate covariates that were not statistically significant (defined as P ≥ 0.10), recognizing that backwards elimination does not solve the problem of missingness, but may reduce missingness by eliminating covariates from the model that do not significantly improve the fit of the model but may reduce the usable sample size. An additional analysis was performed in which missing covariates (Table I) were substituted with their gender-specific medians.
Table 1.
Baseline characteristics of population by heart failure status
| Total (n = 5613) | No heart failure (n = 4087) | Incident heart failure (n = 1526) | P-value | |
|---|---|---|---|---|
| Age (years) (missing data n = 0) | 72.74 ± 5.57 | 72.29 ± 5.45 | 73.95 ± 5.71 | <0.001 |
| BMI (kg/m2) (missing data n = 19) | 26.65 ± 4.67 | 26.38 ± 4.5 | 27.38 ± 5.02 | <0.001 |
| Age at meno (women) (missing data n = 247) | 47.04 ± 6.72 | 47.24 ± 6.54 | 46.42 ± 7.22 | 0.01 |
| Male (missing data n = 0) | 2362 (42) | 1636 (40) | 726 (48) | <0.01 |
| African American (missing data n = 0) | 864 (15) | 645 (16) | 219 (14) | 0.2 |
| Education (≥12 years) (missing data n = 16) | 3975 (71) | 2938 (72) | 1037 (68) | <0.001 |
| Income(≥25 000 USD/year) (missing data n = 364) | 2047 (39) | 1558 (41) | 489 (34) | <0.001 |
| Live birth (women) (missing data n = 848) | 2339 (97) | 1761 (97) | 578 (98) | 0.51 |
| Calcium supplement intake (missing data n = 56) | 1093 (20) | 802 (20) | 291 (19) | 0.67 |
| Smoking status (missing data n = 6) | ||||
| Never | 2602 (46) | 1908 (47) | 694 (45) | 0.55 |
| Former | 2331 (42) | 1679 (41) | 652 (43) | |
| Current | 674 (12) | 495 (12) | 179 (12) | |
| Glucose status (missing data n = 58) | ||||
| Normal | 3935 (71) | 2955 (73) | 980 (65) | <0.001 |
| IFG | 752 (13) | 552 (14) | 200 (13) | |
| Diabetes | 868 (16) | 528 (13) | 340 (22) | |
| Frailty status (missing data n = 556) | ||||
| Not frail | 2402 (47) | 1826 (49) | 576 (43) | <0.001 |
| Intermediate | 2342 (46) | 1688 (46) | 654 (48) | |
| Frail | 313 (6) | 190 (5) | 123 (9) | |
| Health status, self-reported (missing data n = 13) | ||||
| Excellent | 783 (14) | 640 (16) | 143 (9) | <0.001 |
| Very good | 1399 (25) | 1084 (27) | 315 (21) | |
| Good | 2100 (37) | 1491 (36) | 609 (40) | |
| Fair | 1124 (20) | 743 (18) | 381 (25) | |
| Poor | 194 (4) | 122 (3) | 72 (5) | |
| Oestrogen use (women) (missing data n = 0) | ||||
| Never | 2003 (62) | 1466 (60) | 537 (67) | <0.001 |
| Past | 874 (27) | 685 (28) | 189 (24) | |
| Current | 374 (12) | 300 (12) | 74 (9) | |
| Alcohol use (drinks/week) (missing data n = 51) | ||||
| None | 2248 (40) | 1585 (39) | 663 (44) | <0.001 |
| Previous | 484 (9) | 316 (8) | 168 (11) | |
| <1 | 1073 (19) | 795 (20) | 278 (18) | |
| 1 to <7 | 973 (17) | 737 (18) | 236 (16) | |
| 7 and more | 784 (14) | 612 (15) | 172 (11) | |
| Kcal/day of physical activity (missing data n = 18) | 1738 ± 2045 | 1793 ± 2084 | 1591 ± 1930 | <0.001 |
| Digital symbol substitution (DSS) (in s) (missing data n = 264) | 37 ± 13.4 | 37.4 ± 13.7 | 34.8 ± 12.5 | <0.001 |
| Cystatin C (mg/L) (missing data n = 676) | 1.0 ± 0.3 | 1.02 ± 0.28 | 1.12 ± 0.38 | <0.001 |
| Gait speed (m/s) (missing data n = 79) | 1.1 ± 0.3 | 1.13 ± 0.28 | 1.08 ± 0.28 | <0.001 |
| Pneumonia (missing data n = 63) | 1510 (27) | 1073 (26) | 437 (29) | 0.08 |
| Use of thyroid medications (missing data n = 7) | 488 (9) | 362 (9) | 126 (8) | 0.51 |
| Cancer (missing data n = 9) | 808 (14) | 590 (14) | 218 (14) | 0.92 |
| Chronic obstructive pulmonary disease (missing data n = 199) | 698 (13) | 483 (12) | 215 (15) | 0.02 |
| Vision problems (missing data n = 230) | 362 (7) | 239 (6) | 123 (9) | <0.001 |
| Current oral corticosteroid (missing data n = 7) | 116 (2) | 69 (2) | 47 (3) | <0.001 |
| Use of cardiac medications (missing data n = 0) | 2101 (37) | 1398 (34) | 703 (46) | <0.01 |
Means ± standard deviations or counts (by percentages).
All statistical analyses were carried out using R version 2.5.1.44
Results
A total of 5613 participants without prevalent heart failure at baseline were included. Of these, 1526 persons developed incident heart failure during a mean follow-up of 11.5 years. A total of 475 participants had an incident hip fracture during the follow-up period; 159 (33%) of these also had incident heart failure during follow-up, whereas 316 (67%) did not. Among the 159 participants who had both an incident hip fracture and incident heart failure during CHS follow-up, 73 participants experienced a hip fracture before their incident heart failure diagnosis and 70 participants had a hip fracture after their incident heart failure diagnosis. Sixteen participants who had a hip fracture at the same time as their incident heart failure diagnosis were excluded from all subsequent time-dependent analyses. A total of 33 persons died in the same day as they were diagnosed with heart failure; these persons are included in the analyses (Figure 1).
Baseline characteristics
Compared with those without incident heart failure during follow-up, those with incident heart failure were significantly more likely to be older, to have a higher BMI, to be male, to have diabetes, to be frail, to have poorer health status, to not use oestrogen (women), and to consume less alcohol. They were also significantly less likely to have an education level of ≥12 years, an income >25 000 USD/year and to be current users of oestrogen (women) (P < 0.01 for all) (Table 1). Race, the number of live births (women), use of calcium supplements (yes/no), and smoking status did not differ significantly between the groups (P ≥ 0.51 for all). Persons with heart failure had significantly lower kcal/day of physical activity, DSS and gait speed, significantly higher levels of cystatin C, and more use of oral corticosteroids (P < 0.02 for all); frailty and a poorer health status were also more common among those with incident heart failure (P < 0.01). Persons with incident heart failure were also more likely to have chronic obstructive pulmonary disease and vision problems (P < 0.02 for both) and to use cardiac medications (ACE, ARBs, β-blockers, diuretics (loop, thiazide, potassium sparing)) (P < 0.01). There were no significant differences between the groups with respect to history of pneumonia, cancer, or use of thyroid medications (P ≥ 0.08 for all) (Table 1).
Risk of incident hip fracture by heart failure status
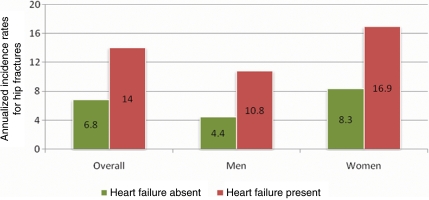
In persons without heart failure, including both men and women, a total of 389 hip fractures (98 in men and 291 in women) occurred over a follow-up of 57 335 person-years (22 173 person-years in men and 35 161 person-years in women). The annualized incidence rate for hip fractures in those with no heart failure over a follow-up of 57 335 person-years was 6.8 per 1000 person-years (95% CI 6.1–7.5); 4.4 per 1000 person-years (95% CI 3.6–5.4) in men and 8.3 per 1000 person-years (95% CI 7.4–9.3) person-years in women. In persons with incident heart failure, including men and women, 70 hip fractures (25 in men and 45 in women) occurred over a follow-up of 4991 person-years (2322 person-years in men and 2668 person-years in women). The overall annualized incidence rate for hip fractures in those with incident heart failure, over a follow-up of 4991 years, was 14 per 1000 person-years (95% CI 10.9–17.7), 10.8 per 1000 person-years (95% CI 7.0–15.9) in men and 16.9 per 1000 person-years (95% CI 12.3–22.5) in women (Figure 2).
Figure 2.
Annualized incidence rates for hip fractures by gender and heart failure status.
Heart failure was significantly associated with subsequent hip fracture in both men [unadjusted HR 1.87 (95% CI 1.2–2.93) and women (unadjusted HR 1.75 (95% CI 1.27–2.4)]. After adjustment for covariates, the association between heart failure and incident hip fractures was still in the same direction but was attenuated and marginally lost statistical significance in both men [HR 1.59 (95% CI 0.93–2.72)] and women [HR 1.41 (95% CI 0.98–2.32)] (Table 2). When missing values of covariates were substituted with their gender-specific medians, the estimates of HRs and their significance did not change in any of the considered models (data not shown).
Table 2.
Unadjusted and adjusted hazard ratios for hip fracture in persons with heart failure by gender
| Gender | Unadjusted HR | Unadjusted 95% CI | Unadjusted P-value | Adjusted HRa | Adjusted 95% CIa | Adjusted P-valuea |
|---|---|---|---|---|---|---|
| Men | 1.87 | 1.20–2.93 | <0.01 | 1.59 | 0.93–2.72 | 0.09 |
| Women | 1.75 | 1.27–2.40 | <0.01 | 1.41 | 0.98–2.03 | 0.06 |
Reference group is persons without heart failure.
aAdjusted for age, race, education, income, BMI, health status, smoking, oestrogen use, age at menopause, diabetes, physical activity, DSS, cystatin C, cancer, chronic obstructive pulmonary disease, walking speed, oral corticosteroids, cardiac medications.
Of the 1526 persons who developed heart failure during study follow-up, 1437 did not previously have a hip fracture. Echocardiograms were available for 1107 of the 1437 persons (77%). This included 895 participants with systolic heart failure and 212 participants with diastolic heart failure. In unadjusted and adjusted models, for men and women with incident heart failure, no differences could be shown in the hazard for incident hip fractures in those with systolic heart failure (EF ≤40%) compared with those with diastolic heart failure (EF > 40%) [unadjusted HR (men) 0.93 (95% CI 0.34–2.52); P = 0.89 and adjusted HR (men) 0.80 (95% CI 0.25–2.58); P = 0.72) and unadjusted HR (women) 0.81 (95% CI 0.25–2.6); P = 0.38 and adjusted HR (women) 0.45 (95% CI 0.13–1.85); P = 0.27]. Setting the threshold for the diagnosis of diastolic heart failure to an EF of >55% did not materially change the results. In sensitivity analyses, in which the 330 persons with missing echocardiogram data were included as first having systolic heart failure and then diastolic heart failure, the results were not changed (data not shown).
Mortality after hip fracture by incident heart failure status
Within the overall analysis cohort of 5613 subjects, 3226 (57.5%) died by the end of follow-up. Participants who developed a hip fracture during follow-up had a greater mortality risk than those who did not develop a hip fracture; 353 of 475 (74.3%) participants with an incident hip fracture died, whereas 2873 of 5138 (55.9%) participants with no incident hip fracture died (P < 0.01). Similarly, participants who developed heart failure during follow-up had a greater mortality risk than those who did not develop heart failure; 1132 of 1526 (74.2%) with incident heart failure died whereas 2094 of 4087 (51.2%) participants with no incident heart failure died (P < 0.01). Among these 1132 participants with incident heart failure who died during follow-up, 135 (12%) had an incident hip fracture, on average 3 years before death (range 0–14 years). In 76 of these 135 persons, the incident hip fracture occurred following the diagnosis of incident heart failure, and 59 sustained a hip fracture prior to the diagnosis of incident heart failure.
Compared with having neither incident heart failure nor an incident hip fracture, mortality hazards were significantly increased in unadjusted and adjusted (adjusted for same covariates as in Table 2) models, respectively, in both men HR 4.08 (95% CI 3.16–5.27) and HR 3.46 (95% CI 2.52–4.74) and women HR 3.38 (95% CI 2.84–4.01) and HR 2.5 (95% CI 2.01–3.11) with hip fractures alone, those with heart failure alone [men HR 3.96 (95% CI 3.53–4.44) and HR 3.22 (95% CI 2.78–3.72)] and [women HR 5.04 (95% CI 4.5–5.63) and HR 3.69 (95% CI 3.21–4.25)] and those with heart failure followed [men HR 11.35 (95% CI 7.95–16.20) and HR 6.15 (95% CI 3.90–9.71)] and [women HR 10.31 (95% CI 7.61–13.98) and HR 6.8 (95% CI 4.48–10.32)] or preceded by a hip fracture [men HR 5.85 (95% CI 3.37–10.15) and HR 4.68 (95% CI 2.05–10.69)] and women [HR 9.85 (95% CI 7.29–13.32) and HR 4.38 (95% CI 3.02–6.35)]. In men, in unadjusted models, relative to having heart failure alone, the mortality HR for heart failure followed by an incident hip fracture was 2.87 (95% CI 2.27–6.63). In unadjusted models in women, the mortality HR for heart failure followed by an incident hip fracture was 2.05 (95% CI 1.68–2.49). In adjusted models in men, relative to having heart failure alone, the mortality HR for heart failure followed by an incident hip fracture was 1.91 (95% CI 1.57–2.32) and, in women, it was 1.84 (95% CI 1.52–2.24).
Discussion
In this large, community-based study of elderly men and women, the annualized incidence rates for hip fractures after a diagnosis of heart failure were 10.8 per 1000 person-years in men and 16.9 per 1000 persons-years in women. Although the multivariable-adjusted association between heart failure and incident hip fracture was attenuated and marginally lost significance, the overall direction of the association remained in the same direction as in the unadjusted association in both men and women. No differences could be shown in the hazards for hip fracture in systolic, compared with diastolic, heart failure. Mortality following hip fractures was markedly increased (∼2-fold) in both men and women with heart failure and a hip fracture, compared with those persons with heart failure who did not sustain a hip fracture.
There is limited information relative to the epidemiology of hip fractures in heart failure, and our study substantially contributes to this body of knowledge. One report has suggested an increased risk for hip fractures of 5-fold in women with heart failure compared with population-based controls in Sweden.4 More recently, a 6-fold increased risk of hip fractures in the first year following a diagnosis of heart failure compared with controls with cardiovascular disease without heart failure was reported in Canada.5 Uniquely, our study is the first to document the long-term risks, over more than a decade of follow-up, of hip fractures following a diagnosis of incident heart failure in an elderly, community dwelling population of African American and Caucasian men and women. Another major strength of our study, which has not previously been addressed,4,5 was our careful consideration and adjustment for potential confounders of the relationship between heart failure and hip fracture including indices of frailty.45–47 In our study, the association between heart failure and hip fracture was attenuated after adjusting for these covariates Other reports have suggested a significant association between heart failure and osteoporosis, but did not adjust for frailty indices5 or included BMD without hip fracture data.48 Our study suggests a number of important points. First, that, in clinical practice, heart failure is an important marker for hip fracture risk. Secondly, that the association of hip fractures with heart failure is likely partially, although not completely, a function of shared risk factors. Finally, that attention to shared risk factors for heart failure and osteoporosis merits further study.
There are a number of limitations to our study. Our finding that the association between heart failure and hip fractures was attenuated after adjustment for covariates could have been due to the loss of power inherent in adding the adjusters with some missing values. However, our analysis to address the impact of these missing covariates on our results by substituting gender-specific medians for these values did not change the significance of our findings. Additionally, importantly, a potentially important risk factor for both heart failure8 and fractures,9 that of hypovitaminosis D, was not considered in this study as vitamin D measurements are not yet available in CHS.
With the rise in diagnoses of diastolic heart failure, particularly in women,49 our findings that both systolic and diastolic heart failure are a risk for hip fracture underscore the importance of screening measures for osteoporosis in this population. In contrast with our study, an EF of ≤49% has been reported to predict osteoporosis.50 However, this study,50 in contrast to our work, examined the relationship of EF to BMD measurements of osteoporosis, not fractures. Our analysis of the relationship of EF to hip fractures was limited in several ways. First, we may have been underpowered to detect differences in hip fractures between those with systolic compared with diastolic dysfunction as there were only 218 persons with diastolic dysfunction in our analysis using a cut point EF of 40%. However, using an EF cut point of 55% included 435 persons with diastolic dysfunction, and did not materially change our conclusion. In addition, ascertainment of EFs in our study was limited to estimations from 2-D echocardiograms, and this may have limited our ability to accurately classify systolic vs. diastolic dysfunction and, as a result, to detect meaningful differences between the groups.
Although mortality following a diagnosis of heart failure is substantial,51 recent trends suggest that survival rates for persons with heart failure are improving.52,53 Our findings of a striking, more than double increased mortality among men and women with heart failure who then sustain a hip fracture compared to those with heart failure alone, suggests that hip fractures may be an important cause of death in persons with heart failure. In support of this, a study of Medicare beneficiaries reported heart failure to be an independent risk factor for 30-day mortality following a hip fracture.54 Our mortality assessments are limited in that they included any death that occurred during CHS follow-up after the diagnosis of incident heart failure but did not stratify by time of death relative to date of diagnosis of incident heart failure.
In conclusion, men and women with heart failure should be considered a high-risk population for hip fractures. However, the association between heart failure and hip fractures is at least partially explained by shared risk factors. Hip fracture is a substantial contributor to mortality in heart failure. Future studies should address strategies for fracture prevention in persons with heart failure.
Funding
This work was supported by contract numbers N01-HC-85079 through N01-HC-85086, N01-HC-35129, N01 HC-15103, N01 HC-55222, N01-HC-75150, N01-HC-45133, grant number U01 HL080295 from the National Heart, Lung, and Blood Institute, with additional contribution from the National Institute of Neurological Disorders and Stroke. Supported in part by program directed funds from the Department of Veterans Affairs.
Conflict of interest: L.C. has received honorarium from Merck, Novartis, P&G, and Aventis.
References
- 1.Keen RW. Burden of osteoporosis and fractures. Curr Osteoporos Rep. 2003;1:66–70. doi: 10.1007/s11914-003-0011-x. [DOI] [PubMed] [Google Scholar]
- 2.Jiang HX, Majumdar SR, Dick DA, Moreau M, Raso J, Otto DD, Johnston DW. Development and initial validation of a risk score for predicting in-hospital and 1-year mortality in patients with hip fractures. J Bone Miner Res. 2005;20:494–500. doi: 10.1359/JBMR.041133. [DOI] [PubMed] [Google Scholar]
- 3.Aronow WS. Heart disease and aging. Med Clin North Am. 2006;90:849–862. doi: 10.1016/j.mcna.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 4.Sennerby U, Farahmand B, Ahlbom A, Ljunghall S, Michaelsson K. Cardiovascular diseases and future risk of hip fracture in women. Osteoporos Int. 2007;18:1355–1362. doi: 10.1007/s00198-007-0386-0. [DOI] [PubMed] [Google Scholar]
- 5.van Diepen S, Majumdar SR, Bakal JA, McAlister FA, Ezekowitz JA. Heart failure is a risk factor for orthopedic fracture: a population-based analysis of 16,294 patients. Circulation. 2008;118:1946–1952. doi: 10.1161/CIRCULATIONAHA.108.784009. [DOI] [PubMed] [Google Scholar]
- 6.Kenchaiah S, Sesso HD, Gaziano JM. Body mass index and vigorous physical activity and the risk of heart failure among men. Circulation. 2009;119:44–52. doi: 10.1161/CIRCULATIONAHA.108.807289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gregg EW, Pereira MA, Caspersen CJ. Physical activity, falls, and fractures among older adults: a review of the epidemiologic evidence. J Am Geriatr Soc. 2000;48:883–893. doi: 10.1111/j.1532-5415.2000.tb06884.x. [DOI] [PubMed] [Google Scholar]
- 8.Shane E, Mancini D, Aaronson K, Silverberg SJ, Seibel MJ, Addesso V, McMahon DJ. Bone mass, vitamin D deficiency, and hyperparathyroidism in congestive heart failure. Am J Med. 1997;103:197–207. doi: 10.1016/s0002-9343(97)00142-3. [DOI] [PubMed] [Google Scholar]
- 9.van Schoor NM, Visser M, Pluijm SM, Kuchuk N, Smit JH, Lips P. Vitamin D deficiency as a risk factor for osteoporotic fractures. Bone. 2008;42:260–266. doi: 10.1016/j.bone.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 10.Ahmed A, Campbell RC. Epidemiology of chronic kidney disease in heart failure. Heart Fail Clin. 2008;4:387–399. doi: 10.1016/j.hfc.2008.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.LaCroix AZ, Lee JS, Wu L, Cauley JA, Shlipak MG, Ott SM, Robbins J, Curb JD, Leboff M, Bauer DC, Jackson RD, Kooperberg CL, Cummings SR. Cystatin-C, renal function, and incidence of hip fracture in postmenopausal women. J Am Geriatr Soc. 2008;56:1434–1441. doi: 10.1111/j.1532-5415.2008.01807.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int. 2005;16(Suppl. 2):S3–S7. doi: 10.1007/s00198-004-1702-6. [DOI] [PubMed] [Google Scholar]
- 13.Hofbauer LC, Brueck CC, Singh SK, Dobnig H. Osteoporosis in patients with diabetes mellitus. J Bone Miner Res. 2007;22:1317–1328. doi: 10.1359/jbmr.070510. [DOI] [PubMed] [Google Scholar]
- 14.Koro CE, Bowlin SJ, Weiss SR. Antidiabetic therapy and the risk of heart failure in type 2 diabetic patients: an independent effect or confounding by indication. Pharmacoepidemiol Drug Saf. 2005;14:697–703. doi: 10.1002/pds.1069. [DOI] [PubMed] [Google Scholar]
- 15.Tanko LB, Christiansen C, Cox DA, Geiger MJ, McNabb MA, Cummings SR. Relationship between osteoporosis and cardiovascular disease in postmenopausal women. J Bone Miner Res. 2005;20:1912–1920. doi: 10.1359/JBMR.050711. [DOI] [PubMed] [Google Scholar]
- 16.Bolland MJ, Ames RW, Horne AM, Orr-Walker BJ, Gamble GD, Reid IR. The effect of treatment with a thiazide diuretic for 4 years on bone density in normal postmenopausal women. Osteoporos Int. 2007;18:479–486. doi: 10.1007/s00198-006-0259-y. [DOI] [PubMed] [Google Scholar]
- 17.Carbone LD, Cross JD, Raza SH, Bush AJ, Sepanski RJ, Dhawan S, Khan BQ, Gupta M, Ahmad K, Khouzam RN, Dishmon DA, Nesheiwat JP, Hajjar MA, Chishti WA, Nasser W, Khan M, Womack CR, Cho T, Haskin AR, Weber KT. Fracture risk in men with congestive heart failure risk reduction with spironolactone. J Am Coll Cardiol. 2008;52:135–138. doi: 10.1016/j.jacc.2008.03.039. [DOI] [PubMed] [Google Scholar]
- 18.Lynn H, Kwok T, Wong SY, Woo J, Leung PC. Angiotensin converting enzyme inhibitor use is associated with higher bone mineral density in elderly Chinese. Bone. 2006;38:584–588. doi: 10.1016/j.bone.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 19.Schlienger RG, Kraenzlin ME, Jick SS, Meier CR. Use of beta-blockers and risk of fractures. J Am Med Assoc. 2004;292:1326–1332. doi: 10.1001/jama.292.11.1326. [DOI] [PubMed] [Google Scholar]
- 20.Lim LS, Fink HA, Kuskowski MA, Taylor BC, Schousboe JT, Ensrud KE. Loop diuretic use and increased rates of hip bone loss in older men: the Osteoporotic Fractures in Men Study. Arch Intern Med. 2008;168:735–740. doi: 10.1001/archinte.168.7.735. [DOI] [PubMed] [Google Scholar]
- 21.Carbone LD, Johnson KC, Bush AJ, Robbins J, Larson JC, Thomas A, LaCroix AZ. Loop diuretic use and fracture in postmenopausal women: findings from the Women's Health Initiative. Arch Intern Med. 2009;169:132–140. doi: 10.1001/archinternmed.2008.526. [DOI] [PubMed] [Google Scholar]
- 22.Magnus JH, Broussard DL. Can self-rated health identify US women and men with low bone mineral density? A cross-sectional population study. Gend Med. 2008;5:246–258. doi: 10.1016/j.genm.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 23.Sullivan MD, O'Meara ES. Heart failure at the end of life: symptoms, function, and medical care in the Cardiovascular Health Study. Am J Geriatr Cardiol. 2006;15:217–225. doi: 10.1111/j.1076-7460.2006.05196.x. [DOI] [PubMed] [Google Scholar]
- 24.Ensrud KE, Ewing SK, Cawthon PM, Fink HA, Taylor BC, Cauley JA, Dam TT, Marshall LM, Orwoll ES, Cummings SR. A comparison of frailty indexes for the prediction of falls, disability, fractures, and mortality in older men. J Am Geriatr Soc. 2009;57:492–498. doi: 10.1111/j.1532-5415.2009.02137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Weber KT. Aldosterone in congestive heart failure. N Engl J Med. 2001;345:1689–1697. doi: 10.1056/NEJMra000050. [DOI] [PubMed] [Google Scholar]
- 26.Chhokar VS, Sun Y, Bhattacharya SK, Ahokas RA, Myers LK, Xing Z, Smith RA, Gerling IC, Weber KT. Hyperparathyroidism and the calcium paradox of aldosteronism. Circulation. 2005;111:871–878. doi: 10.1161/01.CIR.0000155621.10213.06. [DOI] [PubMed] [Google Scholar]
- 27.Law PH, Sun Y, Bhattacharya SK, Chhokar VS, Weber KT. Diuretics and bone loss in rats with aldosteronism. J Am Coll Cardiol. 2005;46:142–146. doi: 10.1016/j.jacc.2005.03.055. [DOI] [PubMed] [Google Scholar]
- 28.Baldini V, Mastropasqua M, Francucci CM, D'Erasmo E. Cardiovascular disease and osteoporosis. J Endocrinol Invest. 2005;28(Suppl. 10):69–72. [PubMed] [Google Scholar]
- 29.Wisniacki N, Taylor W, Lye M, Wilding JP. Insulin resistance and inflammatory activation in older patients with systolic and diastolic heart failure. Heart. 2005;91:32–37. doi: 10.1136/hrt.2003.029652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cauley JA, Danielson ME, Boudreau RM, Forrest KY, Zmuda JM, Pahor M, Tylavsky FA, Cummings SR, Harris TB, Newman AB. Inflammatory markers and incident fracture risk in older men and women: the Health Aging and Body Composition Study. J Bone Miner Res. 2007;22:1088–1095. doi: 10.1359/jbmr.070409. [DOI] [PubMed] [Google Scholar]
- 31.Schett G, Kiechl S, Weger S, Pederiva A, Mayr A, Petrangeli M, Oberhollenzer F, Lorenzini R, Redlich K, Axmann R, Zwerina J, Willeit J. High-sensitivity C-reactive protein and risk of nontraumatic fractures in the Bruneck study. Arch Intern Med. 2006;166:2495–2501. doi: 10.1001/archinte.166.22.2495. [DOI] [PubMed] [Google Scholar]
- 32.Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet. 1999;353:878–882. doi: 10.1016/S0140-6736(98)09075-8. [DOI] [PubMed] [Google Scholar]
- 33.Psaty BM, Kuller LH, Bild D, Burke GL, Kittner SJ, Mittelmark M, Price TR, Rautaharju PM, Robbins J. Methods of assessing prevalent cardiovascular disease in the Cardiovascular Health Study. Ann Epidemiol. 1995;5:270–277. doi: 10.1016/1047-2797(94)00092-8. [DOI] [PubMed] [Google Scholar]
- 34.Ives DG, Fitzpatrick AL, Bild DE, Psaty BM, Kuller LH, Crowley PM, Cruise RG, Theroux S. Surveillance and ascertainment of cardiovascular events. The Cardiovascular Health Study. Ann Epidemiol. 1995;5:278–285. doi: 10.1016/1047-2797(94)00093-9. [DOI] [PubMed] [Google Scholar]
- 35.Smith GL, Masoudi FA, Vaccarino V, Radford MJ, Krumholz HM. Outcomes in heart failure patients with preserved ejection fraction: mortality, readmission, and functional decline. J Am Coll Cardiol. 2003;41:1510–1518. doi: 10.1016/s0735-1097(03)00185-2. [DOI] [PubMed] [Google Scholar]
- 36.De Laet CE, Van Hout BA, Burger H, Weel AE, Hofman A, Pols HA. Hip fracture prediction in elderly men and women: validation in the Rotterdam study. J Bone Miner Res. 1998;13:1587–1593. doi: 10.1359/jbmr.1998.13.10.1587. [DOI] [PubMed] [Google Scholar]
- 37.Taylor BC, Schreiner PJ, Stone KL, Fink HA, Cummings SR, Nevitt MC, Bowman PJ, Ensrud KE. Long-term prediction of incident hip fracture risk in elderly white women: study of osteoporotic fractures. J Am Geriatr Soc. 2004;52:1479–1486. doi: 10.1111/j.1532-5415.2004.52410.x. [DOI] [PubMed] [Google Scholar]
- 38.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 39.Mukamal KJ, Chung H, Jenny NS, Kuller LH, Longstreth WT, Jr, Mittleman MA, Burke GL, Cushman M, Psaty BM, Siscovick DS. Alcohol consumption and risk of coronary heart disease in older adults: the Cardiovascular Health Study. J Am Geriatr Soc. 2006;54:30–37. doi: 10.1111/j.1532-5415.2005.00561.x. [DOI] [PubMed] [Google Scholar]
- 40.Psaty BM, Lee M, Savage PJ, Rutan GH, German PS, Lyles M. Assessing the use of medications in the elderly: methods and initial experience in the Cardiovascular Health Study. The Cardiovascular Health Study Collaborative Research Group. J Clin Epidemiol. 1992;45:683–692. doi: 10.1016/0895-4356(92)90143-b. [DOI] [PubMed] [Google Scholar]
- 41.Shlipak MG, Sarnak MJ, Katz R, Fried LF, Seliger SL, Newman AB, Siscovick DS, Stehman-Breen C. Cystatin C and the risk of death and cardiovascular events among elderly persons. N Engl J Med. 2005;352:2049–2060. doi: 10.1056/NEJMoa043161. [DOI] [PubMed] [Google Scholar]
- 42.Salthouse TA. What do adult age differences in the Digit Symbol Substitution Test reflect? J Gerontol. 1992;47:P121–P128. doi: 10.1093/geronj/47.3.p121. [DOI] [PubMed] [Google Scholar]
- 43.Forsen L, Sogaard AJ, Meyer HE, Edna T, Kopjar B. Survival after hip fracture: short- and long-term excess mortality according to age and gender. Osteoporos Int. 1999;10:73–78. doi: 10.1007/s001980050197. [DOI] [PubMed] [Google Scholar]
- 44.R Development Core Team. A Language and Environment for Statistical Computing. 2.5.1 ed. Vienna, Austria: R–Foundation for Statistical Computing; 2004. [Google Scholar]
- 45.Burns RB, McCarthy EP, Moskowitz MA, Ash A, Kane RL, Finch M. Outcomes for older men and women with congestive heart failure. J Am Geriatr Soc. 1997;45:276–280. doi: 10.1111/j.1532-5415.1997.tb00940.x. [DOI] [PubMed] [Google Scholar]
- 46.Newman AB, Gottdiener JS, McBurnie MA, Hirsch CH, Kop WJ, Tracy R, Walston JD, Fried LP. Associations of subclinical cardiovascular disease with frailty. J Gerontol A Biol Sci Med Sci. 2001;56:M158–M166. doi: 10.1093/gerona/56.3.m158. [DOI] [PubMed] [Google Scholar]
- 47.Rich MW. Epidemiology, pathophysiology, and etiology of congestive heart failure in older adults. J Am Geriatr Soc. 1997;45:968–974. doi: 10.1111/j.1532-5415.1997.tb02968.x. [DOI] [PubMed] [Google Scholar]
- 48.Farhat GN, Newman AB, Sutton-Tyrrell K, Matthews KA, Boudreau R, Schwartz AV, Harris T, Tylavsky F, Visser M, Cauley JA. The association of bone mineral density measures with incident cardiovascular disease in older adults. Osteoporos Int. 2007;18:999–1008. doi: 10.1007/s00198-007-0338-8. [DOI] [PubMed] [Google Scholar]
- 49.Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355:251–259. doi: 10.1056/NEJMoa052256. [DOI] [PubMed] [Google Scholar]
- 50.Abou-Raya S, Abou-Raya A. Osteoporosis and congestive heart failure (CHF) in the elderly patient: double disease burden. Arch Gerontol Geriatr. 2008;49:250–254. doi: 10.1016/j.archger.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 51.Senni M, Tribouilloy CM, Rodeheffer RJ, Jacobsen SJ, Evans JM, Bailey KR, Redfield MM. Congestive heart failure in the community: trends in incidence and survival in a 10-year period. Arch Intern Med. 1999;159:29–34. doi: 10.1001/archinte.159.1.29. [DOI] [PubMed] [Google Scholar]
- 52.Ni H, Nauman DJ, Hershberger RE. Analysis of trends in hospitalizations for heart failure. J Card Fail. 1999;5:79–84. doi: 10.1016/s1071-9164(99)90029-5. [DOI] [PubMed] [Google Scholar]
- 53.Shahar E, Lee S. Historical trends in survival of hospitalized heart failure patients: 2000 versus 1995. BMC Cardiovasc Disord. 2007;7:2. doi: 10.1186/1471-2261-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nettleman MD, Alsip J, Schrader M, Schulte M. Predictors of mortality after acute hip fracture. J Gen Intern Med. 1996;11:765–767. doi: 10.1007/BF02598997. [DOI] [PubMed] [Google Scholar]