Abstract
Internalized heterosexism (IH), or the internalization of societal anti-homosexual attitudes, has been consistently linked to depression and low self-esteem among gay men, and inconclusively associated with substance use and sexual risk in gay and bisexual men. Using structural equation modeling, a model framed in Social Action Theory was tested in which IH is associated with HIV transmission risk and poor adherence to HIV antiretroviral therapy (ART) through the mechanisms of negative affect and stimulant use. Data from a sample of 465 gay-identified men interviewed as part of an HIV risk reduction behavioral trial were used to test the fit of the model. Results supported the hypothesized model in which IH was associated with unprotected receptive (but not insertive) anal intercourse with HIV-negative or unknown HIV status partners, and with ART non-adherence indirectly via increased negative affect and more regular stimulant use. The model accounted for 15% of the variance in unprotected receptive anal intercourse (URAI) and 17% of the variance in ART non-adherence. Findings support the potential utility of addressing IH in HIV prevention and treatment with HIV-positive gay men.
Keywords: HIV/AIDS, internalized heterosexism, homophobia, adherence, depression, methamphetamine, HIV transmission risk
Historically, lesbian, gay and bisexual (LGB) individuals report high rates of discrimination, oppression, and physical violence associated with their sexual orientation (Harper & Schneider, 2003; Herek, Chopp, & Strohl, 2007; Huebner & Gerend, 2001). Presumably, as a result of these and other factors, the rates of affective and substance use disorders among LGB individuals are higher than that of the general population (Cochran, Ackerman, Mays, & Ross, 2004; Cochran, Mays, & Sullivan, 2003; Mays & Cochran, 2001; Meyer, 2003). With homosexuality categorized as a mental illness as recent as 1973, it is not surprising that societal stigma and homophobia are pervasive concerns affecting many LGB persons. When Weinberg coined the term “homophobia” to describe the negative societal attitudes and behaviors experienced by LGB persons, this provided an important way for individuals to understand the discrimination they experience across multiple life domains (Weinberg, 1972). The construct of internalized heterosexism (IH), which has also been called internalized homophobia and internalized homonegativity, has been defined as the internalization by gay men and lesbians of these perceived societal anti-homosexual attitudes (see Herek, 2004 for history of IH terminology).
There is evidence that IH is related to a number of psychological and behavioral outcomes, including affective disorders, substance use, and sexual risk taking. In this paper, the literature linking the construct of internalized heterosexism with these outcomes is reviewed and a model based in Social Action Theory (SAT) is tested in which IH, framed as a contextual variable, is linked to HIV sexual transmission risk and treatment adherence via the self-regulatory mechanisms of negative affect and stimulant use among a large sample of HIV-positive gay-identified men living with HIV.
Internalized Heterosexism and Psychological Adjustment
The internalizing of societal negative beliefs about homosexuality has been described by Gonsiornek as a process in which societal “negative attitudes toward homosexuality…are incorporated into self-image, creating various psychological distortions and reactions” (1988, p. 115). In a social-cognitive framework, these beliefs result in negative mood states that can lead to difficulties with managing negative affect, resulting in depression and anxiety disorders. Russell and Bohan (2006) propose that the effects of IH on psychological adjustment can range from overt behaviors such as suicide attempts in response to hatred of one’s identity to more insidious effects such as ongoing tolerance of discrimination. This notion is supported by findings indicating that IH is linked to lower self esteem and greater anxiety and depression (Igartua, Gill, & Montoro, 2003; Ross et al., 2001; Shidlo, 1994) as well as higher rates of suicidal ideation and suicide attempts (Cochran & Mays, 2000; Herrell et al., 1999; Savin-Williams, 2001). There is further evidence that IH is associated with less secure interpersonal attachments (Jellison & McConnell, 2003; Sherry, 2007), which can result in social isolation and can interfere with the acquisition of social support, thereby hindering the positive effects of such support on psychological and physical health.
Among studies focusing exclusively on HIV-positive gay men, Nicholson and Long (1990), in a sample of 89 HIV+ gay men, observed a link between higher levels of IH and increased use of avoidant coping strategies. Although avoidant coping may be an effective means of managing distress in the short-term (Carrico et al., 2006), it has also been associated with increased substance use and poorer adherence to anti-retroviral therapy (ART) among HIV-positive persons (Collins et al., 2001). Wagner studied 142 HIV-positive gay men in New York and found relationships between IH and psychological distress, but no relationship with avoidant coping (Wagner, Brondolo, & Rabkin, 1996). Although not assessing IH directly, one investigation found a relationship between consistent disclosure of sexual orientation (and HIV status) and slower progression of disease as measured by T-helper (CD4+) cell count decline among HIV-positive psychiatric outpatients (Strachan, Bennett, Russo, & Roy-Byrne, 2007). Together, these studies suggest that IH may impair the capacity of individuals to execute effective coping responses and decrease psychological distress. Among HIV-positive persons, this may have important implications for the extent to which individuals are able to effectively manage HIV infection, improve immune status, and delay progression to acquired immune deficiency syndrome.
Internalized Heterosexism and Sexual Risk
The effect of IH can extend directly to sexual satisfaction and behaviors. Shernoff (2006) writes that “internalized homophobia can contribute to barebacking [unprotected intercourse] by creating an unconscious sense that a gay man is unimportant and undervalued, thus increasing his sense that he is expendable, and so too are the men with whom he has sex and from whom he seeks love and validation” (p. 106). In a study of Canadian gay and bisexual men, investigators found an association between higher IH and greater likelihood of engaging in high-risk anal and oral sex (Ratti, Bakeman, & Peterson, 2000). Bearing in mind the association of IH with less secure interpersonal attachments (Jellison & McConnell, 2003; Sherry, 2007), it is plausible that individuals with elevated levels of IH could prefer multiple, brief sexual encounters as opposed to close, intimate relationships. The relationship between IH and increased sexual risk taking behavior may be further exacerbated by avoidance of resources in the gay community such as support services and HIV prevention programs (Huebner, Davis, Nemeroff, & Aiken, 2002) heightening the risk of HIV transmission. Interestingly, IH has also been linked to sexual preferences and sexual satisfaction among gay and bisexual men. Hart and colleagues (2003) observed that men who self-labeled as an exclusively insertive partner (i.e., top) reported elevated levels of IH compared to those who reported that they commonly enjoy both insertive and receptive sex with men (i.e., versatile). It may be that individuals who report a clear preference for being the insertive partner during sex are doing so in part to conform to hetero-normative notions of sex. In another investigation, gay men who were more accepting of their homosexuality reported greater psychosexual adjustment, less concern about sexual image, and lower ratings of sexual impulsivity (Dupras, 1994). Taken together, the internalization of negative views towards one’s sexuality can contribute to the development of less secure interpersonal attachments, social isolation, avoidance of gay venues and resources, and increased sexual impulsivity and risk (Huebner et al., 2002; Meyer & Dean, 1998; Waldo, Kegeles, & Hays, 1998).
Internalized Heterosexism and Substance Use
Given the proposed role of IH in the development and maintenance of psychological distress and sexual problems, it is logical that IH may also lead to the use and abuse of illicit substances. Although not necessarily evidence of a direct causal relationship with IH, there are documented higher rates of substance use and abuse among LGB persons when compared with the general population (Cabaj, 1996; Skinner, 1994). Two possible mechanisms could explain a link between IH and substance use. First, substances can serve as means of self medicating the negative affect experienced from IH, thereby serving as an avoidant coping strategy. Second, substances can lower sexual inhibitions related to IH and thereby allow the fulfillment of sexual urges that are otherwise stigmatized and avoided. A range of specific classes of drugs have been investigated in the context of IH. For instance, a link between IH and alcohol use has been observed but has been more pronounced in lesbian samples than in samples of gay men (Amadio & Chung, 2004). Other studies examining general drug and alcohol use in association with IH have yielded mixed findings with some reporting no association (Ross et al., 2001) and others reporting a link between IH and drug use (Finnegan & Cook, 1984; Meyer & Dean, 1998). In fact, it may be that substance use serves important functions for gay men with elevated IH. One small study of Latino gay men living in San Francisco observed that drug use assisted individuals in coping with negative thoughts and feelings about their sexual orientation, feeling connected with the gay community, and overcoming sexual inhibitions (Bauermeister, 2007).
The current investigation examines drug use in the context of gay men living with HIV in San Francisco. In this setting, there has been a documented increase in the use of stimulants such as methamphetamines that has been convincingly linked to HIV risk and challenges with HIV disease management, including adherence to antiretroviral therapeutic (ART) medications for HIV disease (Carrico et al., 2007; Colfax & Guzman, 2006; Colfax & Shoptaw, 2005; Das-Douglas, Colfax, Moss, Bangsberg, & Hahn, 2007; Hinkin et al., 2007; Reback, Larkins, & Shoptaw, 2003). Evidence of the disinhibting effects of stimulants on sexual behavior is illustrated by findings such as those of Semple and colleagues in which 84% of HIV-positive, methamphetamine-using men who have sex with men reported engaging in sexual marathons, defined as prolonged sexual activity lasting hours or even days (Semple, Zians, Strathdee, & Patterson, In Press). Qualitative and quantitative investigations with gay male stimulant users in New York City have tied stimulant use to men’s efforts to mask feelings of emotional discomfort, allowing a defense against negative affective states and isolation, and creating a sense of sexual disinhibition and dissociation (Halkitis, Fischgrund, & Parsons, 2005; Halkitis, Mukherjee, & Palamar, 2007). Further, patterns of use suggest that chronic stimulant users report higher levels of avoidant coping in which they use stimulants to avoid unpleasant emotions than did gay men who use stimulants less regularly (Halkitis & Shrem, 2006). Although other substances such as alcohol and opiates may contribute to these issues, the usage rates and documented consequences of stimulant use among gay men living with HIV supports the rationale for investigating this class of drugs in relation to IH.
Internalized Heterosexism and the Management of HIV Disease
There have been no direct studies of the potential role of IH in the medical management of HIV disease. There is indirect evidence, however, that a failure to identify as gay is associated with not seeking HIV counseling and testing among men who have sex with men (CDC, 2000). This lack of testing may result in a delayed diagnosis, which may limit treatment options and prognoses for those who present for care later in the disease process (Battegay, Fluckiger, Hirschel, & Furrer, 2007). The advent and widespread availability of advanced HIV pharmacotherapeutics has resulted in dramatic decreases in AIDS-related mortality and morbidity in the developed world (Palella et al., 1998; Riley, Bangsberg, Guzman, Perry, & Moss, 2005). However, the regimen characteristics often require strict adherence to dosing schedules. Non-adherence can result in viral resistance, hastened disease progression, and increased infectivity for transmitting HIV to others. As such, understanding and enhancing ART adherence is a priority. There is a growing body of research identifying predictors of poor HIV medication adherence, including stimulant use and indicators of negative psychological states such as depression (Lima et al., 2007; Reback et al., 2003). HIV stigma, which conceptually may be linked to IH for some, has been proposed as a barrier to seeking care, initiating appropriate treatment, and adhering to medication regimens among HIV-positive persons (Chesney & Smith, 1999; Rao, Kekwaletswe, Hosek, Martinez, & Rodriguez, 2007; Ware, Wyatt, & Tugenberg, 2006). Individuals with elevated IH may be more likely to appraise their unaccepted sexual orientation as the reason they became infected with HIV. Consequently, HIV medications may serve as an ever-present reminder of these negative thoughts and feelings surrounding one’s sexual orientation, resulting in avoidance and potential non-adherence. The current investigation is the first to address this potential IH-non-adherence link.
Across these studies, findings support an important, yet not clearly understood, role of IH in the context of HIV prevention and disease management. Given the evidence to date, IH can be viewed as having pervasive deleterious effects across multiple dimensions of well-being and behavior. Prior work is extended by developing a model with a large sample of HIV-positive, gay-identified men that addresses HIV transmission risk behaviors and adherence to ART, two areas of high importance in HIV primary and secondary prevention.
Social Action Theory
To guide the current analysis, the constructs of interest are framed within SAT (Ewart, 1991, 2004). SAT was developed as an extension of individual level psychological theories to address the broad complexities of public health priorities. In SAT, the self regulatory processes of the individual are positioned within the context of environmental factors in their joined influence on action states or health behaviors. The overarching goal is the detection and manipulation of environmental and self regulatory factors that can promote health and/or hinder healthy behaviors and habits.
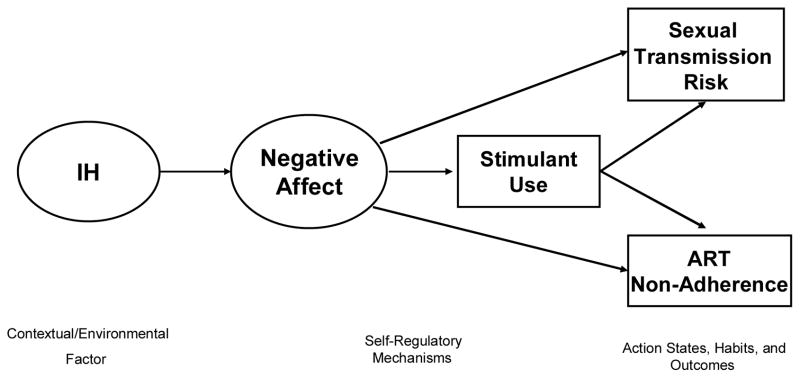
The current application of SAT is illustrated in Figure 1. In this investigation, IH is the identified contextual variable of interest, as it is a product of the environmental atmosphere of discrimination and negative sentiments toward homosexuality. As described previously, IH is linked to two self-regulatory factors: (1) negative affect and (2) substance use, in this case stimulant use. Given the focus on HIV prevention and care in the current investigation, the two action states or outcomes of interest are sexual transmission risk and non-adherence to treatment.
Figure 1.
Conceptual Model based in SAT of the Associations of Internalized Heterosexism with Negative Affect, Stimulant Use, and HIV Transmission and ART Non-Adherence.
The purpose of the current investigation is to examine the hypothesized interrelationships among higher levels of IH and negative affect (i.e., stress, anxiety, depression, and anger/burnout), greater stimulant use (e.g., methamphetamines), poorer ART adherence, and greater risk of transmitting HIV to others (via unprotected sex with HIV-negative or unknown status partners). Specifically, it is hypothesized that: 1) higher IH will be associated with increased negative affect; 2) elevated negative affect will be associated with greater stimulant use; 3) greater stimulant use will, in turn, be independently associated with a greater likelihood of reporting HIV transmission risk acts and ART non-adherence.
Method
Participants
HIV-positive individuals in the San Francisco Bay Area were screened for recruitment into the Healthy Living Project, a behavioral prevention trial of a comprehensive cognitive-behavioral sexual risk reduction intervention (HLP, 2007). Recruitment and screening of potential respondents were undertaken in community agencies and medical clinics serving HIV-positive persons. Respondents were at least 18 years of age, and provided written informed consent and medical documentation of HIV infection. Participants were excluded if they did not complete the interview for any reason. Such reasons included fatigue, voluntary withdrawal, and evidence of substantial confusion or disorientation, consistent with psychosis or severe neuropsychological impairment, as determined subjectively by senior project staff. For the current analysis, only respondents were included who reported homosexual/gay orientation in response to the following assessment item: “Do you now identify as: heterosexual/straight, homosexual/gay, bisexual, not sure, or other (choose one).”
The sample consisted of 465 men with documented HIV infection who identified as exclusively gay/homosexual. The majority of participants were Caucasian (62%), but a substantial minority were African American (17%) or Hispanic/Latino (10%). The mean age was 41.5 (SD = 8.3) years, and participants had been diagnosed with HIV for an average of 9.2 (SD = 5.0) years. The sample was largely well-educated with 76% having completed at least some college. Approximately 71% (n = 328) of participants were currently prescribed ART. Table 1 provides demographic and other relevant descriptive information for this sample.
Table 1.
Participant Characteristics
| Variable | n | % of sample |
|---|---|---|
| Race and Ethnicity | ||
| Black/African American | 81 | 17.5 |
| Hispanic/Latino | 48 | 10.4 |
| Asian/Pacific Islander | 10 | 2.2 |
| Native American/Alaskan Native | 12 | 2.6 |
| Non-Hispanic White | 288 | 62.1 |
| Multi-Racial/Multi-Cultural | 25 | 5.4 |
| Employment Status | ||
| Working (Full-Time or Part-Time) | 222 | 47.7 |
| Not Working | 243 | 52.3 |
| Education | ||
| < High School | 30 | 6.5 |
| High School | 82 | 17.6 |
| Some College | 186 | 40.0 |
| College Graduate or Greater | 167 | 35.9 |
| Currently in a Primary Relationship | 147 | 31.7 |
| Homeless (Past Year) | 41 | 8.8 |
| CD4+ Count < 200 (Self Report) | 80 | 17.2 |
| Undetectable HIV Viral Load (Self Report) | 174 | 37.4 |
| Regular Stimulant Use | 39 | 8.4 |
| URAI with HIV-/unknown partners | 26 | 5.6 |
| UIAI with HIV-/unknown partners | 65 | 14.0 |
| Less than 90% adherence | 94 | 20.2 |
Overview of Assessment Procedures
The data reported in this paper are from the baseline interview that served as screening determination for Healthy Living Project of biological males who reported an exclusively homosexual orientation. All procedures were approved by the University of California, San Francisco Committee on Human Research. Interviews were conducted in private offices over a period of 2–4 hours with regular breaks to minimize respondent fatigue. All data used in these analyses were collected prior to exposure to intervention procedures.
Procedures involved Audio Computer Assisted Self-Interviewing (ACASI) and Computer Assisted Personal Interviewing (CAPI) using the Questionnaire Development System by Nova Research Company. ACASI allows respondents to listen to items via headphones while reading items on a computer monitor and to enter responses directly into the computer. This approach has been proposed as an effective method of decreasing social desirability and thereby enhancing veracity of self-report (Gribble, Miller, Rogers, & Turner, 1999; Turner et al., 1998). With CAPI, an interviewer reads items from a computer and enters responses directly into the computer. Respondents were compensated US$50 for completing the interview.
Interviewer Training and Quality Assurance
Interviewers were trained with the use of a detailed assessment manual, practice with the computer programs, participation in an intensive 3-day training program, and review and certification of audiotaped interviews with standardized criteria. Interviews were audiotaped and a systematic sample was reviewed for protocol adherence with feedback and correction provided to interviewers on a regular basis.
Measures
Demographics/background
Detailed background and demographic questions assessed respondent age, race/ethnicity, sexual orientation, education, employment status, and self-reported T-helper (CD4+) count and viral load.
Internalized heterosexism (IH)
IH was assessed via four items modified from prior studies of IH (Nungesser, 1983; Shidlo, 1994): “I am glad to be gay” (reverse scored); “I wish I were heterosexual”; “Whenever I think a lot about being gay, I feel critical about myself”; and “Homosexuality is not as satisfying as heterosexuality.” Reponses were selected among 6 Likert-type scale choices ranging from “strongly disagree” to “strongly agree” with higher scores indicating higher internalized heterosexism (current sample alpha = .77).
Substance use
Participants rated the frequency of alcohol and substance use during the past three months using the following responses: never, less than once a month, once a month, 2–3 times a month, once a week, 2–3 times per week, 4–6 times per week, once a day, more than once a day. For the current analysis, the focus is on stimulant use given the prevalence among gay men (Shoptaw, 2006) and the evidence of the role of stimulants in HIV risk behaviors (Schwarcz et al., 2007). Participants who reported using cocaine, crack, or methamphetamine 2–3 times per week or more were categorized as regular users (1) versus those who used once a week or less (0).
Negative Affect
Negative affect describes a broad dimension of affect that is composed of several correlated, yet distinct, negative emotional states (e.g., anger, anxiety, sadness, disgust, contempt, etc.). In the present investigation, an indication of the presence of negative affect was measured using four separate instruments that tapped into discrete, negative emotional states which are consistent with the construct of negative affect.
Cohen’s Perceived Stress Scale (PSS) was administered as an indicator of negative affect (Cohen, Kamarck, & Mermelstein, 1983). The 10 item version, consisting of a series of statements, assesses the degree to which a person describes situations as stressful. A total score was used by summing ratings on a 5-point scale (current sample alpha = .83).
The State form of the State-Trait Anxiety Inventory (STAI) (Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983) is a self-report measure of state and trait anxiety by perceived feelings of tension and apprehension. The STAI includes 20 items rated on 4-point scales. The summary measure is calculated as the sum of the ten positive items minus the sum of the ten negative items plus a value of 50 (current sample alpha = .84 for positive items and alpha = .91 for negative items).
The 21-item Beck Depression Inventory (BDI) assesses the severity of somatic, affective, cognitive, and behavioral symptoms of depression during the past week (Beck & Steer, 1984). The BDI is reliable and has demonstrated good concurrent validity with the Hamilton Rating Scale for Depression. To control for confounds between HIV-related symptoms and somatic symptoms of depression, the 13-item BDI-Affective subscale (current sample alpha = .87) was used for the present investigation (Kalichman, Rompa, & Cage, 2000).
Anger/burnout was assessed by a scale developed in studies of HIV coping (Chesney, Folkman, & Chambers, 1996). This 16 item scale (current sample alpha = .94) is based on the anger and fatigue scales of the Profile of Mood States (McNair, Lorr, & Droppleman, 1981). Respondents are asked to indicate on a five point scale (from not at all to extremely) how much they had been feeling drained, enraged, irritated etc. in the past 30 days. In prior research, HIV+ participants who attended coping intervention programs showed longer decreases in burnout than did control group participants.
Antiretroviral medication adherence
Self-reported ART adherence was assessed over a three-day period using an adherence survey developed for use in AIDS Clinical Trials (Chesney et al., 2000). Respondents indicated how many pills they had missed during each of the previous three days. This measure has been used widely with diverse samples. For the present study, percent adherence was calculated based on number of pills actually taken divided by number of pills prescribed. Respondents were classified as having achieved less than 90% adherence (1) versus 90% or higher adherence (0), consistent with current literature on minimum levels of adherence to achieve HIV viral suppression and clinical benefit (Garcia de Olalla et al., 2002; Paterson et al., 2000).
HIV transmission risk
Participants were asked via ACASI about specific sexual acts and whether condoms were used with each sexual partner over the prior three months. Of particular interest in the current analyses was the occurrence of transmission risk acts: unprotected insertive anal intercourse (UIAI) or receptive anal intercourse (URAI) acts with HIV-negative or status unknown partners in which neither party used a condom. UIAI and URAI were examined separately because prior investigations have highlighted the potential benefit in understanding specific sex risk acts (Schwarcz et al., 2007). Details of the calculation of transmission risk acts are provided elsewhere (HLP, 2007). Participants reporting any UIAI with at risk partners (1) were compared to those who reported none (0). Similarly, individuals reporting any URAI with at risk partners (1) were compared to those who reported none (0).
Statistical Analyses
We began with an exploratory factor analysis (EFA) to determine the structure of the 4 items measuring internalized heterosexism. Because an examination of the distributions for these items indicated that they were positively skewed, we conducted the EFA using MPlus (Muthen & Muthen, 2004b). By using MPlus we were able to treat items as ordered categorical indicators using the weighted least squares-mean and variance-adjusted estimator. We interpreted the results of this EFA by examining the number of eignvalues that were greater than one, the degree to which items loaded strongly (.60 or higher) on a single factor with promax rotation, and whether the root mean residual (RMR) was less than .05 (McDonald, 1985). Finally, we conducted a multiple linear regression analysis to examine race/ethnicity, age, education, and relationship status as correlates of the composite score(s) of IH.
We used structural equation modeling to investigate if poorer affect regulation and increased stimulant use mediated the effect of IH on HIV transmission risk and ART non-adherence. A major strength of structural equation modeling is that it allows one to use latent variables with multiple categorical and/or continuous indicators for constructs to partial out measurement error. Specifying mediating variables as a latent variables also removes any bias in the analysis that arises from lack of perfect reliability of observed mediators, being that measurement error in the mediating variable can weaken statistical power of the tests of the indirect effects (Hoyle & Kenny, 1999). Also, structural equation modeling enables one to examine the associations among multiple independent and dependent variables in the model simultaneously as well as obtain indices of global model fit. For the present investigation, we utilized multiple indices of model fit: comparative fit index (CFI) values greater than .95, root mean square error of approximation (RMSEA) values less than .06, and weighted root-mean-square residual (WRMR) values less than .90 (Hu & Bentler, 1998). Although a non-significant chi-square (χ2) is also generally indicative of better model fit, this statistic may not be as reliable given the large sample size for the present investigation. Thus, we examined if the ratio of the χ2 to degrees of freedom (χ2/df) was less than three (Kline, 1998). Because the present investigation utilized a categorical mediating variable (i.e., stimulant use) and examined categorical outcomes (HIV transmission risk and ART non-adherence), we used the weighted least squares-mean and variance-adjusted estimator with the theta parameterization (Muthen & Muthen, 2004a).
Results
The EFA extracted one factor with an eignvalue greater than one. This factor (eignvalue = 2.84) included all four items for IH. All items appeared to load well on this single factor (range: .69 – .86), and there were no cross-loadings for any item. The model appeared to be a good fit for the data (RMR = .02). Using a composite score of all four items, we determined there were no race/ethnic or age differences in IH (p > .20) and individuals in a primary relationship reported similar levels of IH compared to those who were single (p >.10). However, individuals who attended at least some college (M = 7.18; SD = 4.12) reported significantly lower IH when compared to those did not attend college (M = 8.46; SD = 5.00; B = −.12, t = −2.53, p = .012). We then tested the hybrid structural equation model examining the correlates of IH as a single factor with all four items as indicators.
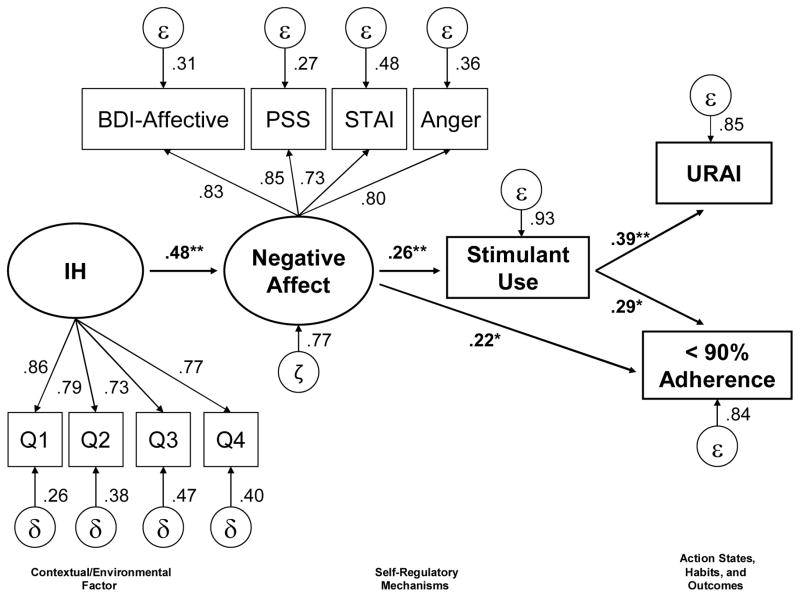
We began by testing the hypothesized model to examine HIV transmission risk as the receptive partner (URAI). The overall fit statistics were within recommended ranges, suggesting good fit (χ2 (20, N = 465) = 33.67, p < .05; χ2/df = 1.68; CFI = .98; RMSEA = .0.38; WRMR = .65). However, we noted that negative affect was not significantly associated with URAI (β = .13, t = 1.16, p > .20). Removing this path did not result in significant changes in model fit (χ2 (19, N = 465) = 31.41, p < .05; χ2/df = 1.65; CFI = .98; RMSEA = .0.37; WRMR = .68). As shown in Figure 2, higher IH was associated with increased negative affect (β = .48, t = 10.26, p < .01). Elevated negative affect was, in turn, associated with an increased likelihood of reporting regular stimulant use (β = .26, t = 3.12, p < .01) and ART non-adherence (β = .22, t = 2.44, p < .05). Regular stimulant use was associated with an increased likelihood of reporting URAI (β= .39, t = 2.85, p < .01) and ART non-adherence (β = .29, t = 2.04, p < .05). Elevated IH was indirectly associated with an increased risk of reporting URAI (Total Indirect Effect: β = .05, t = 2.14, p < .05) and ART non-adherence (Total Indirect Effect: β = .14, t = 3.56, p < .01). When we examined HIV transmission risk as the insertive partner (UIAI), the model continued to be an adequate fit (χ2 (21, N = 465) = 29.46, p > .10;χ2/df = 1.40; CFI = .99; RMSEA = .029; WRMR = .62). However, stimulant use (β = .16, t = 1.11, p > .20) was not associated with UIAI. The total indirect of IH on UIAI was also not significant (β = .02, t =1.02, p > .30). Finally, we examined a model that included education as another important contextual factor that may account for the observed relationships. Including education as a correlate of IH, negative affect, stimulant use, URAI, and ART non-adherence did not change the pattern of results. The more parsimonious model excluding education is reported (See Figure 2).
Figure 2.
Hybrid structural equation model examining the pathways whereby internalized heterosexism (IH) relates to an increased likelihood of HIV transmission risk behavior as the receptive partner (URAI) and non-adherence to anti-retroviral therapy. The model accounted for 15% of the variance in URAI and 17% of the variance in non-adherence to anti-retroviral therapy. (*p< .05 **p<01).
Discussion
The present findings support a model in which internalized heterosexism appears to be linked to greater HIV transmission risk and non-adherence to HIV medications indirectly via increased negative affect and more regular stimulant use. These findings are unique in the focus on identifying potential pathways between IH and an increased risk of infecting others with HIV, and with the increased likelihood of poor disease management through non-adherence to prescribed medications.
The finding that IH is related to increased negative affect is consistent with prior work linking IH and depression. The association of IH with stimulant use is important given the increased rates of methamphetamine use among gay men and the implication of such use in fueling the HIV epidemic in communities of gay and bisexual men (Shoptaw, 2006). There have been mixed findings in the literature investigating the relationship between negative affect and HIV sexual risk behaviors (Crepaz & Marks, 2001; Walch & Rudolph, 2006). The current study identifies substance use, in particular stimulant use, as a potentially important mechanism through which negative affect can indirectly affect HIV transmission risk behavior. Taking into account this indirect effect may help clarify the inconsistency in prior work relating negative affect and sexual risk. Although the current study did not measure avoidant coping, substance use is often framed as a form of avoidant coping in the stress and coping literature (Collins et al., 2001). Stimulant use as a strategy to cope with HIV and IH is consistent with prior findings that linked IH with avoidant coping (Nicholson & Long, 1990). It may be that those with higher levels of IH use stimulants during sex as a means of avoiding negative thoughts and attitudes about their sexual orientation. Such a hypothesis could be examined in future investigations by assessing the rates of stimulant use during sexual encounters versus rates of use in other contexts. The influence of IH may be especially relevant when men seek to engage in sexual activities that are exclusively associated with gay men, possibly increasing the perceived need to use stimulants to engage in receptive anal intercourse. This is supported by the finding that stimulant use was uniquely associated with HIV transmission risk to others when the respondent was the receptive partner.
While the causal effect of the pathways investigated in this study cannot be determined by the present cross-sectional data, the current theoretically-informed model offers possible avenues for intervention. From an intervention development perspective, the current findings identify IH as a contextual issue that may be amenable to psychological treatment. In fact, there is a clear recognition of the importance of social stigmatization and IH in the guidelines for clinical therapeutic work with gay men (APA, 2000). The guidelines suggested by the American Psychological Association include recommendations that “Psychologists strive to understand the ways in which social stigmatization (i.e., prejudice, discrimination, and violence) poses risks to the mental health and well-being of lesbian, gay, and bisexual clients,” (Guideline 3, p. 1442) and that “Psychologists strive to understand how inaccurate or prejudicial views of homosexuality or bisexuality may affect the client’s presentation in treatment and the therapeutic process” (Guideline 4, p. 1443).
In implementing these guidelines, the incorporation of cognitive-behavioral techniques to challenge heterosexist beliefs has been identified as a strategy when working with gay men in psychotherapeutic settings (LaSala, 2006; Safren, Hollander, Hart, & Heimberg, 2001). Other approaches such as Gay Affirmative Therapy (Langdridge, 2007), Affirmative Cognitive-Behavioral Therapy (Balsam, Martell, & Safren, 2006) and Acceptance and Commitment Therapy (Hayes, Luoma, Bond, Masuda, & Lillis, 2006), all of which involve addressing negative beliefs about one’s sexuality, may have a positive impact on HIV transmission and disease self-management among gay men living with HIV. Incorporating intervention content targeting the reduction of IH may further enhance the efficacy of demonstrated coping interventions with HIV-positive gay and bisexual men (Antoni et al., 2006; Carrico et al., 2006; Chesney, Chambers, Taylor, Johnson, & Folkman, 2003). Such intervention content may include problem solving about productive disclosure of sexual orientation and HIV status, identifying and accessing support resources in the gay community, and specific techniques such as identifying and modifying cognitive antecedents related to IH that trigger affective states such as depression. Further, the current findings suggest potential applications for addressing and reducing IH in the context of substance abuse treatment, in particular for the pervasive problem of stimulant abuse in the gay community.
Although not available in the current data, it is likely that HIV-related stigma is a construct related to IH that may help understand the current findings. HIV stigma has been shown to be associated with sexual risk (Timberlake & Sigurdson, 2007) and as potentially resulting in poorer adherence to care and poorer psychological well being among HIV-positive samples (Chesney & Smith, 1999; Rao et al., 2007; Ware et al., 2006). The “double stigma” of being gay and HIV-positive creates further challenges for intervention (Grossman, 1991). Future studies that address the relationship between IH and HIV stigma are needed to clarify their relative impact or potentially interactive effects.
In the current sample, IH was linked to unprotected receptive anal intercourse but not unprotected insertive anal intercourse, the behavior with greater associated HIV transmission risk. Prior research by Hart and colleagues (2003) found that men higher in IH were more likely to identify as “tops” or the insertive partner in anal sex rather than “bottoms” (the receptive partner); therefore it is possible that men identifying as tops may engage in insertive anal sex more freely and without self-reproach. It is also plausible that individuals who are high in IH attempt to directly attenuate their inhibitions by using stimulants. This provides sufficient disinhibition such that they can engage in receptive anal sex without experiencing these negative cognitions about the self or negative emotions (e.g., shame).
Other factors may be useful in contextualizing the current findings. Previous work among gay men in the San Francisco area has also found a relationship of URAI and methamphetamine use (Schwarcz et al., 2007), possibly a result of erectile dysfunction that can accompany use of this substance. It is possible that accounting for the use of erectile dysfunction medications, which has been increasing in tandem with stimulant use among gay men, may clarify this relationship. Unfortunately, use of erectile dysfunction medications was not assessed in the current study. Alternatively, this pattern may be a result of sero-sorting (Mao et al., 2006), in which individuals take into account a partner’s likely serostatus when deciding in which sexual behaviors to engage, or sero-positioning, in which individuals select sexual acts or roles (such as receptive) in an attempt to reduce risk of infection/transmission. It is unclear how IH might relate to the stimulant-erectile dysfunction drug connection or to the occurrence of sero-sorting and sero-positioning. Regardless of the explanation, unprotected receptive anal intercourse with an HIV-negative or unknown status partner still carries risk of infection to the uninfected partner, thus creating a public health concern. Further, URAI puts the HIV-positive man at risk of sexually transmitted infections that can speed the progression of HIV disease (Palacios et al., 2007). Finally, because it was indirectly associated with lower levels of ART adherence and increased likelihood of transmission risk, IH may be associated with a heightened risk for transmitting ART-resistant virus, which may limit treatment options for newly infected persons (Colfax et al., 2007).
An SAT framework allowed for the specification of IH as a contextual variable relating to these priority outcomes through the self regulatory mechanisms of negative affect and stimulant use. SAT may be better suited than other individual-level models of health behavior because it allows for the consideration of larger contextual factors and their relation to self-regulatory processes on the outcomes, or health states of interest. The current investigation, with its emphasis on IH is perhaps only a sample of the possible SAT models that could address HIV-related outcomes. For instance, future investigations framed in SAT may also incorporate other societal factors as racism, social class differences, HIV-related stigma, and perceived societal values related to masculinity. Likewise, the SAT framework invites greater exploration of regulatory factors that may mediate the effects of these environmental variables on HIV-related outcomes. For example, the current findings suggest the importance of disinhibition (which was not directly assessed in the current study), which hypothetically is achieved via substance use in the current sample. Such a potential effect requires a more thorough investigation. It is plausible that other regulatory factors may also be at work, such avoidant coping, the seeking of anonymous sexual activities, no-disclosure of HIV-status, and delayed HIV testing and seeking of care. Further, different classes of drugs with different psychoactive effects may have different roles in such models and thus may have varied implications for intervention. Overall, the current analyses demonstrate that an SAT framework offers a broad foundation for exploring multiple facets of health behaviors in HIV and other contexts.
There are limitations of note in the current study. To minimize biases associated with self-report, validated measures of adherence and sexual risk behavior were used via ACASI interviewing, thereby removing the interviewer’s presence and minimizing social desirability bias. Further, because IH was not a primary focus of the parent study from which the data were extracted, the measure was not as comprehensive as that used in other investigations. The study was conducted only with HIV-positive persons, and the IH measure was only administered to men who selected “gay/homosexual” as their sexual orientation. Including HIV-negative men and/or those who identified as bisexual or heterosexual (but reported same sex activity) may have revealed different rates of IH and divergent patterns of findings. The assessment of sexual orientation used in the current study did not take into account the complexity of the construct (Savin-Williams & Ream, 2007), and the assessment of alcohol use did not sufficiently distinguish between moderate, heavy and binge drinking and was not adequate to include in the model. Given that there was no formal evaluation of cognitive functioning, it is also possible that cognitive impairment confounds the results. The specific selection of measures for inclusion in the SEM was guided by prior research, SAT, and the availability and quality of the data. The current analyses combined state and trait indicators of negative affect, which may not fully capture the construct of negative affect. Other models posing alternative causal pathways and including other environmental and regulatory variables may yield disparate results. Finally, the use of cross-sectional data with a non-probability sample precludes causal inferences and limits generalizations that can be made from these findings. Experimental and intervention research designs are clearly needed to examine the potentially causal effects of IH on psychological well-being, substance use, HIV transmission risk, and ART adherence.
Future research efforts should engage in selective, theory-driven investigations of ethnicity, age, HIV-status, and HIV stigma as potential moderators of the effects of IH. In the present study, it was observed that individuals who had at least some college reported significantly lower levels of IH when compared to those who never attended. It could be that attending college provides individuals with an opportunity to explore their sexual identity and challenge negative societal attitudes about LGB persons. However, it is also plausible that higher levels of education are a marker for socio-economic status, which has been shown to confer a variety of health benefits (Adler et al., 1994). This should be examined in future investigations. Although the present findings did not reveal differences in IH by race and ethnicity, such differences have been observed in other samples (O’Leary, Fisher, Purcell, Spikes, & Gomez, 2007) and this provides a rationale for examining group differences in the rates and relationships of IH with outcomes such as sexual risk and treatment adherence.
In summary, the current data support a model framed in SAT in which higher internalized heterosexism may result in greater risk of transmitting HIV to others and in poorer self management of HIV disease via the regulatory mechanisms of increased negative affect and more regular stimulant use. These findings offer potential avenues for intervention and underscore the importance of IH in the HIV epidemic among gay men.
Table 2.
Intercorrelations among indicators of internalized heterosexism, negative affect, stimulant use, HIV transmission risk, and ART adherence.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 IH Q1 | ||||||||||||
| 2. IH Q2 | .57** | |||||||||||
| 3. IH Q3 | .46** | .43** | ||||||||||
| 4. IH Q4 | .50** | .48** | .44** | |||||||||
| 5. BDI-Affective | .27** | .24** | .33** | .24** | ||||||||
| 6. PSS | .23** | .22** | .24** | .22** | .69** | |||||||
| 7. STAI | .25** | .18** | .25** | .27** | .58** | .62** | ||||||
| 8. Anger/Burnout | .23** | .21** | .28** | .18** | .64** | .78** | .60** | |||||
| 9. Stimulant Use | .03 | .05 | .12** | .05 | .12* | .10* | .07 | .07 | ||||
| 10. < 90% Adherence | .07 | .11* | .15** | .04 | .22** | .13* | .16** | .17** | .11* | |||
| 11. URAI | .07 | .06 | .02 | .16** | .07 | .04 | .03 | .08 | .06 | .11* | ||
| 12. UIAI | .01 | .01 | .10* | −.02 | .09* | .03 | .02 | .05 | .03 | −.04 | .25** |
p ≤ .05
p < .01.
IH = internalized heterosexism; PSS = Perceived Stress Scale; STAI = State Trait Anxiety Inventory; URAI = unprotected receptive anal intercourse; UIAI = unprotected insertive anal intercourse.
Acknowledgments
This research was funded by National Institute of Mental Health grants U10-MH57636, U10- MH57631, U10-MH57616, and U10-MH57615; and NIMH center grants P30-MH058107 (Mary Jane Rotheram-Borus, Ph.D., PI), P30-MH57226 (Jeffrey A. Kelly, Ph.D., PI), P30-MH43520 (Anke A. Ehrhardt, Ph.D., PI), and P30-MH062246 (Thomas J. Coates, Ph.D., PI). Additional support was provided by a Ruth L. Kirschstein National Research Service Award (T32-MH019391).
The authors thank those at NIMH: Ellen Stover, Ph.D, and Willo Pequegnat, Ph.D., for their technical assistance in developing the study and Christopher M. Gordon, Ph.D., and Dianne Rausch, Ph.D., for their support of this research. Gratitude is also given to Susan Tross, Ph.D. and Gary Dowsett, Ph.D. for methodological guidance; to the assessors in each city who conducted the interviews, to our clinic and community based organization collaborators, to all other support staff involved in the project, and to the men and women who participated in the interviews. We would also like to thank Torsten Neilands for his input and review of the analyses presented in this paper.
This study was conducted by the NIMH Healthy Living Trial Group. Research Steering Committee (site principal investigators and NIMH staff collaborator): Margaret A. Chesney, Ph.D.1, Anke A. Ehrhardt, Ph.D.2, Jeffrey A. Kelly, Ph.D.3, Willo Pequegnat, Ph.D.4, Mary Jane Rotheram-Borus, Ph.D.5 Collaborating Scientists, Co-Principal Investigators, and Investigators: Eric G. Benotsch, Ph.D.3, Michael J. Brondino, Ph.D.3, Sheryl L. Catz, Ph.D.3, Edwin D. Charlebois, Ph.D., M.P.H.1, Don C. DesJarlais, Ph.D. 6, Naihua Duan, Ph.D. 5, Theresa M. Exner, Ph.D. 2, Rise B. Goldstein, Ph.D., M.P.H.5, Cheryl Gore-Felton, Ph.D.3, A. Elizabeth Hirky, Ph.D.2, Mallory O. Johnson, Ph.D.1, Robert M. Kertzner, M.D. 2, Sheri B. Kirshenbaum, Ph.D.2, Lauren E. Kittel, Psy.D. 2, Robert Klitzman, M.D. 2, Martha Lee, Ph.D.5, Bruce Levin, Ph.D. 2, Marguerita Lightfoot, Ph.D.5, Stephen F. Morin, Ph.D.1, Steven D. Pinkerton, Ph.D.3, Robert H. Remien, Ph.D.2, Fen Rhodes, Ph.D. 5, Susan Tross, Ph.D.2, Lance S. Weinhardt, Ph.D.3, Robert Weiss, Ph.D. 5, Hannah Wolfe, Ph.D. 7, Rachel Wolfe, Ph.D. 7, Lennie Wong, Ph.D.5 Data Management and Analytic Support: Philip Batterham, M.A.5, Tyson Rogers, M.A.5 Site Project Coordinators: Kristin Hackl, M.S.W.3, Daniel Hong, M.A.5, Karen Huchting, B.A.5, Joanne D. Mickalian, M.A.1, Margaret Peterson, M.S.W.3 NIMH: Christopher M. Gordon, Ph.D.4, Dianne Rausch, Ph.D.4, Ellen Stover, Ph.D.4
University of California, San Francisco
New York State Psychiatric Institute/Columbia University, New York
Medical College of Wisconsin, Milwaukee
National Institute of Mental Health, Bethesda, Maryland
University of California, Los Angeles
Beth Israel Medical Center, New York
St. Luke’s-Roosevelt Medical Center, New York
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/journals/ccp.
References
- Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn RL, et al. Socioeconomic status and health. The challenge of the gradient. American Psychologist. 1994;49:15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- Amadio DM, Chung YB. Internalized homophobia and substance use among lesbian, gay, and bisexual persons. Journal of Gay & Lesbian Social Services: Issues in Practice, Policy & Research. 2004;17:83–101. [Google Scholar]
- Antoni MH, Carrico AW, Duran RE, Spitzer S, Penedo F, Ironson G, et al. Randomized clinical trial of cognitive behavioral stress management on human immunodeficiency virus viral load in gay men treated with highly active antiretroviral therapy. Psychosomatic Medicine. 2006;68:143–151. doi: 10.1097/01.psy.0000195749.60049.63. [DOI] [PubMed] [Google Scholar]
- APA. Guidelines for psychotherapy with lesbian, gay, and bisexual clients. American Psychologist. 2000;55:1440–1451. doi: 10.1037/0003-066x.55.12.1440. [DOI] [PubMed] [Google Scholar]
- Balsam KF, Martell CR, Safren SA. Affirmative cognitive-behavioral therapy with lesbian, gay, and bisexual people. In: Hays P, Imawasa G, editors. Cognitive behavioral therapy with diverse populations. Washington, D.C: American Psychological Association Press; 2006. [Google Scholar]
- Battegay M, Fluckiger U, Hirschel B, Furrer H. Late presentation of HIV-infected individuals. Antiviral Therapy. 2007;12:841–851. [PubMed] [Google Scholar]
- Bauermeister JA. It’s all about “connecting”: Reasons for drug use among Latino gay men living in the San Francisco Bay area. Journal of Ethnicity in Substance Abuse. 2007;6:109–129. doi: 10.1300/J233v06n01_07. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Internal consistencies of the original and revised Beck Depression Inventory. Journal of Clinical Psychology. 1984;40:1365–1367. doi: 10.1002/1097-4679(198411)40:6<1365::aid-jclp2270400615>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Cabaj RP. Substance abuse in gay men, lesbians, and bisexuals. In: Cabaj RP, Stein TS, editors. Textbook of Homosexuality and Mental Health. Washington, D.C: American Psychiatric Press, Inc; 1996. pp. 783–799. [Google Scholar]
- Carrico AW, Antoni MH, Duran RE, Ironson G, Penedo F, Fletcher MA, et al. Reductions in depressed mood and denial coping during cognitive behavioral stress management with HIV-positive gay men treated with HAART. Annals of Behavioral Medicine. 2006;31:155–164. doi: 10.1207/s15324796abm3102_7. [DOI] [PubMed] [Google Scholar]
- Carrico AW, Johnson MO, Moskowitz JT, Neilands TB, Morin SF, Charlebois ED, et al. Affect regulation, stimulant use, and viral load among HIV-positive persons on anti-retroviral therapy. Psychosomatic Medicine. 2007;69:785–792. doi: 10.1097/PSY.0b013e318157b142. [DOI] [PubMed] [Google Scholar]
- CDC. HIV-related knowledge and stigma--United States, 2000. MMWR Morbidity and Mortality Weekly Report. 2000;49:1062–1064. [PubMed] [Google Scholar]
- Chesney M, Chambers DB, Taylor J, Johnson L, Folkman S. Coping effectiveness training for men living with HIV: Results from a randomized clinical trial testing a group-based intervention. Psychosomatic Medicine. 2003;65:1038–1046. doi: 10.1097/01.psy.0000097344.78697.ed. [DOI] [PubMed] [Google Scholar]
- Chesney M, Folkman S, Chambers D. Coping effectiveness training for men living with HIV: Preliminary findings. International Journal of STDs & AIDS. 1996;7:75–82. doi: 10.1258/0956462961917690. [DOI] [PubMed] [Google Scholar]
- Chesney MA, Ickovics JR, Chambers DB, Gifford AL, Neidig J, Zwickl B, et al. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: The AACTG adherence instruments. Patient Care Committee & Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG) AIDS Care. 2000;12:255–266. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- Chesney MA, Smith AW. Critical delays in HIV testing and care: The potential role of stigma. American Behavioral Scientist. 1999;42 [Google Scholar]
- Cochran SD, Ackerman D, Mays VM, Ross MW. Prevalence of non-medical drug use and dependence among homosexually active men and women in the US population. Addiction. 2004;99:989–998. doi: 10.1111/j.1360-0443.2004.00759.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran SD, Mays VM. Lifetime prevalence of suicide symptoms and affective disorders among men reporting same-sex sexual partners: Results from NHANES III. American Journal of Public Health. 2000;90:573–578. doi: 10.2105/ajph.90.4.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran SD, Mays VM, Sullivan JG. Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. Journal of Consulting and Clinical Psychology. 2003;71:53–61. doi: 10.1037//0022-006x.71.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health & Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Colfax G, Guzman R. Club drugs and HIV infection: A review. Clinical Infectious Diseases. 2006;42:1463–1469. doi: 10.1086/503259. [DOI] [PubMed] [Google Scholar]
- Colfax G, Shoptaw S. The methamphetamine epidemic: Implications for HIV prevention and treatment. Current HIV/AIDS Reports. 2005;2:194–199. doi: 10.1007/s11904-005-0016-4. [DOI] [PubMed] [Google Scholar]
- Colfax GN, Vittinghoff E, Grant R, Lum P, Spotts G, Hecht FM. Frequent methamphetamine use is associated with primary non-nucleoside reverse transcriptase inhibitor resistance. AIDS. 2007;21:239–241. doi: 10.1097/QAD.0b013e3280114a29. [DOI] [PubMed] [Google Scholar]
- Collins RL, Kanouse DE, Gifford AL, Senterfitt JW, Schuster MA, McCaffrey DF, et al. Changes in health-promoting behavior following diagnosis with HIV: Prevalence and correlates in a national probability sample. Health Psychology. 2001;20:351–360. [PubMed] [Google Scholar]
- Crepaz N, Marks G. Are negative affective states associated with HIV sexual risk behaviors? A meta-analytic review. Health Psychology. 2001;20:291–299. doi: 10.1037//0278-6133.20.4.291. [DOI] [PubMed] [Google Scholar]
- Das-Douglas M, Colfax G, Moss AR, Bangsberg DR, Hahn JA. Tripling of methamphetamine/amphetamine use among homeless and marginally housed persons, 1996–2003. Journal of Urban Health. doi: 10.1007/s11524-007-9249-4. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupras A. Internalized homophobia and psychosexual adjustment among gay men. Psychological Reports. 1994;75:23–28. doi: 10.2466/pr0.1994.75.1.23. [DOI] [PubMed] [Google Scholar]
- Ewart CK. Social action theory for a public health psychology. American Psychologist. 1991;46:931–946. doi: 10.1037//0003-066x.46.9.931. [DOI] [PubMed] [Google Scholar]
- Ewart CK. How integrative behavioral theory can improve health promotion and disease prevention. In: Boll TJ, editor. Handbook of Clinical Health Psychology. Vol. 3. Washington, D.C: American Psychological Association; 2004. pp. 249–289. [Google Scholar]
- Finnegan D, Cook D. Special issues affecting the treatment of gay men and lesbian alcoholics. Alcoholism Treatment Quarterly. 1984;1:85–98. [Google Scholar]
- Garcia de Olalla P, Knobel H, Carmona A, Guelar A, Lopez-Colomes JL, Cayla JA. Impact of adherence and highly active antiretroviral therapy on survival in HIV-infected patients. Journal of Acquirred Immune Deficiciency Syndromes. 2002;30:105–110. doi: 10.1097/00042560-200205010-00014. [DOI] [PubMed] [Google Scholar]
- Gonsiorek JC. Mental health issues of gay and lesbian adolescents. Journal of Adolescent Health Care. 1988;9:114–122. doi: 10.1016/0197-0070(88)90057-5. [DOI] [PubMed] [Google Scholar]
- Gribble JN, Miller HG, Rogers SM, Turner CF. Interview mode and measurement of sexual behaviors: Methodological issues. Journal of Sex Research. 1999;36:16–24. doi: 10.1080/00224499909551963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman AH. Gay men and HIV/AIDS: Understanding the double stigma. Journal of the Association of Nurses in AIDS Care. 1991;2:28–32. [PubMed] [Google Scholar]
- Halkitis PN, Fischgrund BN, Parsons JT. Explanations for methamphetamine use among gay and bisexual men in New York City. Substance Use & Misuse. Special Issue: Club Drug Epidemiology. 2005;40:1331–1345. doi: 10.1081/JA-200066900. [DOI] [PubMed] [Google Scholar]
- Halkitis PN, Mukherjee PP, Palamar JJ. Multi-level modeling to explain methamphetamine use among gay and bisexual men. Addiction. 2007;102:76–83. doi: 10.1111/j.1360-0443.2007.01769.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halkitis PN, Shrem MT. Psychological differences between binge and chronic methamphetamine using gay and bisexual men. Addictive Behaviors. 2006;31:549–552. doi: 10.1016/j.addbeh.2005.05.040. [DOI] [PubMed] [Google Scholar]
- Harper GW, Schneider M. Oppression and discrimination among lesbian, gay, bisexual, and transgendered people and communities: A challenge for community psychology. American Journal of Community Psychology. 2003;31:243–252. doi: 10.1023/a:1023906620085. [DOI] [PubMed] [Google Scholar]
- Hart TA, Wolitski RJ, Purcell DW, Gomez C, Halkitis P the Seropositive Urban Men’s Study Team. Sexual behavior among HIV-positive men who have sex with men: What’s in a label? Journal of Sex Research. 2003;40:179–188. doi: 10.1080/00224490309552179. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy. 2006;44:1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Herek GM. Beyond “homophobia”: Thinking about sexual prejudice and stigma in the twenty-first century. Sexuality Research & Social Policy: A Journal of the NSRC. 2004;1:6–24. [Google Scholar]
- Herek GM, Chopp R, Strohl D. Sexual stigma: Putting sexual minority health issues in context. In: Meyer I, Northridge M, editors. The health of sexual minorities: Public health perspectives on lesbian, gay, bisexual, and transgender populations. New York: Springer; 2007. pp. 171–208. [Google Scholar]
- Herrell R, Goldberg J, True WR, Ramakrishnan V, Lyons M, Eisen S, et al. Sexual orientation and suicidality: A co-twin control study in adult men. Archives of General Psychiatry. 1999;56:867–874. doi: 10.1001/archpsyc.56.10.867. [DOI] [PubMed] [Google Scholar]
- Hinkin CH, Barclay TR, Castellon SA, Levine AJ, Durvasula RS, Marion SD, et al. Drug use and medication adherence among HIV-1 infected individuals. AIDS and Behavior. 2007;11:185–194. doi: 10.1007/s10461-006-9152-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HLP. Effects of a behavioral intervention to reduce risk of transmission among people living with HIV: The Healthy Living Project randomized controlled study. Journal of Acquired Immune Deficiency Syndromes. 2007;44:213–221. doi: 10.1097/QAI.0b013e31802c0cae. [DOI] [PubMed] [Google Scholar]
- Hoyle RH, Kenny DA. Sample size, reliability, and tests of statistical mediation. In: Hoyle RH, editor. Statistical strategies for small sample research, [pages needed?] Thousand Oaks, CA: Sage Publications; 1999. [Google Scholar]
- Hu L, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998:424–453. [Google Scholar]
- Huebner D, Gerend M. The relation between beliefs about drug treatments for HIV and sexual risk behavior among gay and bisexual men. Annals of Behavioral Medicine. 2001;23:304–312. doi: 10.1207/S15324796ABM2304_10. [DOI] [PubMed] [Google Scholar]
- Huebner DM, Davis MC, Nemeroff CJ, Aiken LS. The impact of internalized homophobia on HIV preventive interventions. American Journal of Community Psychology. 2002;30:327–348. doi: 10.1023/A:1015325303002. [DOI] [PubMed] [Google Scholar]
- Igartua KJ, Gill K, Montoro R. Internalized homophobia: a factor in depression, anxiety, and suicide in the gay and lesbian population. Canadian Journal of Community Mental Health. 2003;22:15–30. doi: 10.7870/cjcmh-2003-0011. [DOI] [PubMed] [Google Scholar]
- Jellison WA, McConnell AR. The mediating effects of attitudes toward homosexuality between secure attachment and disclosure outcomes among gay men. Journal of Homosexuality. 2003;46:159–177. doi: 10.1300/j082v46n01_05. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D, Cage M. Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV-AIDS. Journal of Nervous & Mental Disease. 2000;188:662–670. doi: 10.1097/00005053-200010000-00004. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York: Guilford; 1998. [Google Scholar]
- Langdridge D. Gay affirmative therapy: A theoretical framework and defence. Journal of Gay & Lesbian Psychotherapy. 2007;11:27–43. [Google Scholar]
- LaSala MC. Cognitive and environmental interventions for gay males: Addressing stigma and its consequences. Families in Society. 2006;87:181–189. [Google Scholar]
- Lima VD, Geller J, Bangsberg DR, Patterson TL, Daniel M, Kerr T, et al. The effect of adherence on the association between depressive symptoms and mortality among HIV-infected individuals first initiating HAART. AIDS. 2007;21:1175–1183. doi: 10.1097/QAD.0b013e32811ebf57. [DOI] [PubMed] [Google Scholar]
- Mao L, Crawford JM, Hospers HJ, Prestage GP, Grulich AE, Kaldor JM, et al. “Serosorting” in casual anal sex of HIV-negative gay men is noteworthy and is increasing in Sydney, Australia. AIDS. 2006;20:1204–1206. doi: 10.1097/01.aids.0000226964.17966.75. [DOI] [PubMed] [Google Scholar]
- Mays VM, Cochran SD. Mental health correlates of perceived discrimination among lesbian, gay, and bisexual adults in the United States. American Journal of Public Health. 2001;91:1869–1876. doi: 10.2105/ajph.91.11.1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald RP. Factor analysis and related methods. Hillsdale, New Jersey: Lawrence Erlbaum and Associates; 1985. [Google Scholar]
- McNair DM, Lorr M, Droppleman LF. Profile of mood states. San Diego: Educational and Industrial Testing Service; 1981. [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129:674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, Dean L. Internalized homophobia, intimacy, and sexual behavior among gay and bisexual men. In: Herek G, editor. Stigma and sexual orientation: Understanding prejudice against lesbians, gay men and bisexuals, [pages needed?] Thousand Oaks, CA: Sage Publications; 1998. [Google Scholar]
- Muthén L, Muthen B. MPlus: Statistical analysis with latent variables. Los Angeles: Muthén and Muthén; 2004a. [Google Scholar]
- Muthén LK, Muthén B. Mplus user’s guide. Los Angeles, CA: Muthen and Muthen, Inc; 2004b. [Google Scholar]
- Nicholson WD, Long BC. Self-esteem, social support, internalized homophobia, and coping strategies of HIV+ gay men. Journal of Consulting and Clinical Psychology. 1990;58:873–876. doi: 10.1037//0022-006x.58.6.873. [DOI] [PubMed] [Google Scholar]
- Nungesser LG. Homosexual acts, actors, and identities. New York: Praeger; 1983. [Google Scholar]
- O’Leary A, Fisher HH, Purcell DW, Spikes PS, Gomez CA. Correlates of risk patterns and race/ethnicity among HIV-positive men who have sex with men. AIDS and Behavior, [vol and pages needed] 2007 doi: 10.1007/s10461-006-9205-4. [DOI] [PubMed] [Google Scholar]
- Palacios R, Jimenez-Onate F, Aguilar M, Galindo MJ, Rivas P, Ocampo A, et al. Impact of syphilis infection on HIV viral load and CD4 cell counts in HIV-infected patients. Journal of Acquired Immune Deficiency Syndromes. 2007;44:356–359. doi: 10.1097/QAI.0b013e31802ea4c6. [DOI] [PubMed] [Google Scholar]
- Palella FJ, Jr, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. New England Journal of Medicine. 1998;338:853–860. doi: 10.1056/NEJM199803263381301. [DOI] [PubMed] [Google Scholar]
- Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Annals of Internal Medicine. 2000;133:21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- Rao D, Kekwaletswe TC, Hosek S, Martinez J, Rodriguez F. Stigma and social barriers to medication adherence with urban youth living with HIV. AIDS Care. 2007;19:28–33. doi: 10.1080/09540120600652303. [DOI] [PubMed] [Google Scholar]
- Ratti R, Bakeman R, Peterson JL. Correlates of high-risk sexual behaviour among Canadian men of South Asian and European origin who have sex with men. AIDS Care. 2000;12:193–202. doi: 10.1080/09540120050001878. [DOI] [PubMed] [Google Scholar]
- Reback CJ, Larkins S, Shoptaw S. Methamphetamine abuse as a barrier to HIV medication adherence among gay and bisexual men. AIDS Care. 2003;15:775–785. doi: 10.1080/09540120310001618621. [DOI] [PubMed] [Google Scholar]
- Riley ED, Bangsberg DR, Guzman D, Perry S, Moss AR. Antiretroviral therapy, hepatitis C virus, and AIDS mortality among San Francisco’s homeless and marginally housed. Journal of Acquired Immune Deficiciency Syndromes. 2005;38:191–195. doi: 10.1097/00126334-200502010-00010. [DOI] [PubMed] [Google Scholar]
- Ross MW, Rosser BR, Bauer GR, Bockting WO, Robinson BE, Rugg DL, et al. Drug use, unsafe sexual behavior, and internalized homonegativity in men who have sex with men. AIDS & Behavior. 2001;5:97–103. [Google Scholar]
- Russell GM, Bohan JS. The case of internalized homophobia: Theory and practice. Theory & Psychology. 2006;16:343–366. [Google Scholar]
- Safren SA, Hollander G, Hart TA, Heimberg RG. Cognitive-behavioral therapy with lesbian, gay, and bisexual youth. Cognitive and Behavioral Practice. 2001;8:215–223. [Google Scholar]
- Savin-Williams RC. Suicide attempts among sexual-minority youths: Population and measurement issues. Journal of Consulting and Clinical Psychology. 2001;69:983–991. doi: 10.1037//0022-006x.69.6.983. [DOI] [PubMed] [Google Scholar]
- Savin-Williams RC, Ream GL. Prevalence and stability of sexual orientation components during adolescence and young adulthood. Archives of Sexual Behavior. 2007;36:385–394. doi: 10.1007/s10508-006-9088-5. [DOI] [PubMed] [Google Scholar]
- Schwarcz S, Scheer S, McFarland W, Katz M, Valleroy L, Chen S, et al. Prevalence of HIV infection and predictors of high-transmission sexual risk behaviors among men who have sex with men. American Journal of Public Health. 2007;97:1067–1075. doi: 10.2105/AJPH.2005.072249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semple SJ, Zians J, Strathdee SA, Patterson TL. Sexual marathons and methamphetamine use among HIV-positive men who have sex with men. Archives of Sexual Behavior. doi: 10.1007/s10508-007-9292-y. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shernoff M. Condomless sex: Gay men, barebacking, and harm reduction. Social Work. 2006;51:106–113. doi: 10.1093/sw/51.2.106. [DOI] [PubMed] [Google Scholar]
- Sherry A. Internalized homophobia and adult attachment: Implications for clinical practice. Psychotherapy: Theory, Research, Practice, Training. 2007;44:219–225. doi: 10.1037/0033-3204.44.2.219. [DOI] [PubMed] [Google Scholar]
- Shidlo A. Internalized homophobia: Conceptual and empirical issues in measurement. In: Beverly Greene GMHE, editor. Lesbian and gay psychology: Theory, research, and clinical applications. Psychological perspectives on lesbian and gay issues. Vol. 1. Thousand Oaks, CA: Sage Publications; 1994. pp. 176–205. [Google Scholar]
- Shoptaw S. Methamphetamine use in urban gay and bisexual populations. Topics in HIV Medicine. 2006;14:84–87. [PubMed] [Google Scholar]
- Skinner WF. The prevalence and demographic predictors of illicit and licit drug use among lesbians and gay men. American Journal of Public Health. 1994;84:1307–1310. doi: 10.2105/ajph.84.8.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory (Form Y) Palo Alto, California: Consulting Psychologists Press, Inc; 1983. [Google Scholar]
- Strachan ED, Bennett WR, Russo J, Roy-Byrne PP. Disclosure of HIV status and sexual orientation independently predicts increased absolute CD4 cell counts over time for psychiatric patients. Psychosomatic Medicine. 2007;69:74–80. doi: 10.1097/01.psy.0000249900.34885.46. [DOI] [PubMed] [Google Scholar]
- Timberlake S, Sigurdson J. HIV, stigma, and rates of infection: a human rights and public health imperative. PLoS Med. 2007;4:e52. doi: 10.1371/journal.pmed.0040052. author reply e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: Increased reporting with computer survey technology. Science. 1998;280:867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- Wagner G, Brondolo E, Rabkin J. Internalized homophobia in a sample of HIV+ gay men, and its relationship to psychological distress, coping, and illness progression. Journal of Homosexuality. 1996;32:91–106. doi: 10.1300/j082v32n02_06. [DOI] [PubMed] [Google Scholar]
- Walch SE, Rudolph SM. Negative affect and risk for Human Immunodeficiency Virus: One size may not fit all. American Journal of Health Promotion. 2006;20:324–333. doi: 10.4278/0890-1171-20.5.324. [DOI] [PubMed] [Google Scholar]
- Waldo CM, Kegeles SM, Hays RB. Self-Acceptance of gay identity decreases sexual risk behavior and increases psychological health in U.S. gay men; Paper presented at the International AIDS Conference; Geneva. 1998. [Google Scholar]
- Ware NC, Wyatt MA, Tugenberg T. Social relationships, stigma and adherence to antiretroviral therapy for HIV/AIDS. AIDS Care. 2006;18:904–910. doi: 10.1080/09540120500330554. [DOI] [PubMed] [Google Scholar]
- Weinberg G. Society and the Healthy Homosexual. New York: St. Martin’s Press; 1972. [Google Scholar]