Abstract
Background
In patients with a major cardiac event, the first priority is to minimize time to treatment. For many patients, first contact with the health system is through emergency medical services (EMS). We set out to identify patient and neighborhood-level factors that were associated with time in EMS.
Methods
A retrospective cohort study was conducted in ten municipalities in Dallas County, Texas from January 1 through December 31, 2004. The dataset included 5,887 calls with a primary complaint that was cardiac in nature. The region was served by 29 hospitals and 98 EMS depots. Multivariate models included measures of distance traveled, time of day, day of week, patient and neighborhood characteristics. The main outcomes were elapsed time in EMS (continuous; in minutes) and delay in EMS (dichotomous; > 15 minutes beyond median time).
Results
We found positive associations between patient characteristics and both average time and serious delay in EMS care. Variation in average time was not large enough to be clinically meaningful. Approximately 11% (n = 647) of patients were delayed 15 minutes or more. Being non-white was associated with delays, but few patients were affected. Women were more likely to be seriously delayed (adjusted odds ratio 1.52; 95% confidence interval: 1.32, 1.74), and this association did not change after adjusting for other characteristics, including neighborhood socio-economic composition.
Conclusions
Compared to otherwise similar men, women have 50% greater odds of being delayed in the EMS setting. The determinants of serious delay should be a special focus of EMS studies where time to treatment is a priority.
Keywords: Patients, population, women, emergency medical services, cardiac care
Background
For patients with a major cardiac event, the first priority is to minimize time to treatment.1, 2 While elapsed time from symptom onset to definitive care is the primary concern, most effort is focused on reducing elapsed time from hospital arrival (“door time”) to treatment.3 Door-to-treatment time is a viable target for reduction because it is reliably recorded in hospital administrative data and is most often managed within a single institution. However, recent developments in emergency medical services (EMS) and new research into pre-hospital delays have made the time segment from 9-1-1 call to hospital arrival an obvious new target for intervention. Approximately a quarter of patients with chest pain 4 and half of patients with heart attack5 arrive at the hospital via EMS. Much could be gained from a new focus on elapsed time in the EMS setting.6
The goal of this study was to identify patient and neighborhood characteristics that were associated with time spent in EMS among patients with cardiac complaints. We evaluated the associations between patient- and neighborhood-level factors and both average time and serious delays in EMS, adjusting for geographic and temporal characteristics.
Methods
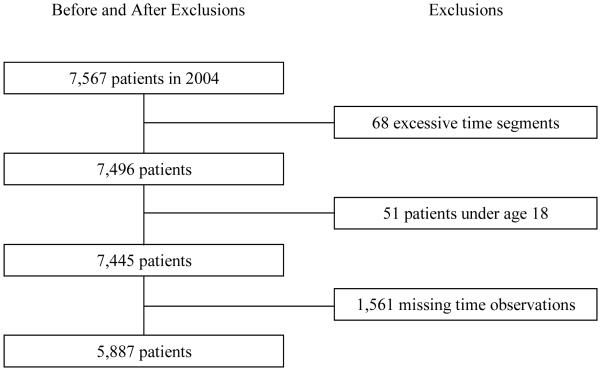
Our study population was comprised of adult residents of ten municipalities within Dallas County, Texas who made a call to 911 with cardiac-related symptoms from January 1 through December 31, 2004. This region (Figure 1) is racially and linguistically diverse, with urban, suburban and rural districts bounded on three sides by sparsely populated counties and on its fourth side by Dallas-Fort Worth airport. These features make the Dallas County EMS system ideal for such an inquiry, because the system and the hospitals it serves are contained within the same boundaries, reducing the potential for confounding from unmeasured geographic, population and health system characteristics lying beyond the system.
Figure 1. Geographic distribution of hospitals, firehouses and patients with cardiac symptoms who called 911 in 2004.
Hospitals are represented by a blue “H”. Firehouses with emergency medical service (EMS) facilities are represented by a red cross. Patient calls (N=5,887) are represented by shaded circles and are scaled in size to represent the number of calls, ranging from 1 to 97 calls from any single Census block group.
The data were compiled from EMS “run sheets” and included patient clinical and demographic characteristics; date, time and location of emergency calls; vehicle response times, on-scene times and transport times; and hospital location and treatment capability. The patient’s point of origin was represented by the geographic centroid of the Census block group from which the call was made. We used geographic information system (GIS) software to construct a model of the population, geography, and provider characteristics of Dallas County. The model incorporated U.S. Census data for each of 1,463 Census block groups within the ten municipalities and the straight-line distance between each block group and all emergency providers. The geographic area under study (Figure 1) is served by 29 hospitals with emergency departments and by 98 fire stations with EMS depots.
The first outcome of interest was time in EMS, measured in three segments and rounded to the nearest minute: 1) response time, or elapsed time from patient call to scene arrival, 2) on-scene time, or elapsed time from scene arrival to scene departure, and 3) transport time, or elapsed time from scene departure to hospital arrival. The main analysis combined all three segments. A second outcome of interest was delays of 15 minutes beyond median total time in EMS care. In patients with myocardial infarction, starting reperfusion treatment within 60 minutes of symptom onset is known to prevent irreversible damage to the myocardium,1 and additional increments of 15 minutes up to five hours have been shown to be predictive of the size of infarct.2 In the EMS setting, unnecessary delays of 15 minutes or more could be harmful to patients with an existing or evolving major cardiac event. We therefore evaluated the group of patients who were in EMS care at least 15 minutes longer than the median patient.
Patient-Level Data
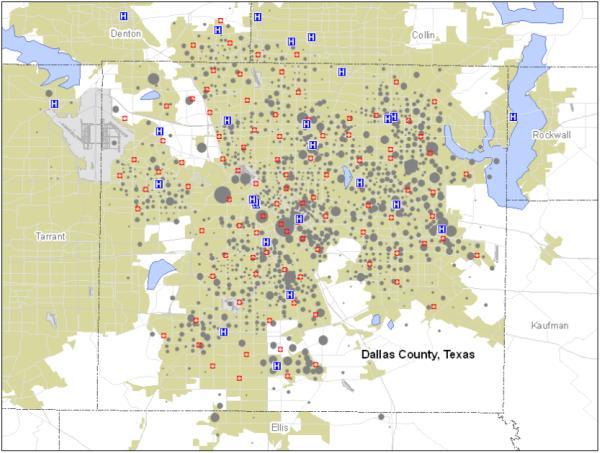
The initial dataset included 7,567 calls. We excluded patients with excessive elapsed time measurements (more than one hour from firehouse to scene; more than two hours on scene or more than two hours from scene to hospital) because of the probability that such measurements were made in error (n=68). We also excluded patients under age 18 (n=51) because of the low probability that they experienced an acute coronary syndrome. Additional observations were excluded for missing a measure of total elapsed time in any one of the three segments (n=1,561), most of which (82.2%) were patients who were seen by EMS personnel but had no record of delivery to a hospital. The final dataset included 5,887 patients (Figure 2).
Figure 2. Exclusions.
During 2004 in Dallas County, Texas, 7,567 patients with cardiac complaints called 911 for assistance. Patients were excluded for elapsed time over two hours in any measured time segment (N=68), age under 18 (N=51), and missing time observations (N=1,561)
Prior to the analysis, we adjusted for typical shortcomings in observational data by employing two widely accepted procedures. First, we imputed values for missing observations of age in 16% of patients. Following the approach detailed by Rubin (1987) and adapted by Schafer (1997), we used a Markov-Chain Monte-Carlo simulation for non-monotone missing variables to multiply impute the missing values.7,8 Ten complete datasets were created. Second, we used an inverse propensity score weighting procedure described by Lunceford and Davidian (2004)9 to correct for baseline imbalances between racial and ethnic groups. We estimated a propensity score model of the probability that the patient was of white race, conditional on all measured patient and neighborhood characteristics, excluding the outcomes of interest. The inverse of this propensity score was applied as a weight to make racial and ethnic groups similar in baseline measures. To confirm weighted balance on these measures, we ran chi-square tests on categorical variables and a standardized difference estimate (Cohen’s d) on continuous variables.
Neighborhood-Level Data
Neighborhood socio-economic data were drawn from the 2000 U.S. Census at the block group level. We included the percent of residents who were white, percent foreign born, percent living under 200% of the federal poverty level, and population density.
Distance traveled in the first segment - from firehouse to scene - was estimated along a straight line from the nearest firehouse to the geographic centroid of the patient’s block group. Distance estimates in the third segment were computed along the straight line from the patient’s block group to the observed arrival hospital. Both straight-line and rectilinear distances are highly correlated with road network distances in urban, semi-urban and suburban areas; however, straight-line estimates are better as population density approaches rurality,10 as it does in parts of Dallas County.
Analytic Models
To identify predictors of average time in EMS, we fit four successive linear regression models for each time segment and for total elapsed time. The initial model for each elapsed time measure included travel distance alone. In successive models, we added day of the week and time of day, patient characteristics, and neighborhood characteristics. To identify predictors of delay, we estimated an additional multiple logistic regression with 15-minute delay as the outcome of interest. We adjusted for distance, onset time, patient vitals, age, race and neighborhood socio-economic composition. We also included a dummy variable for bypassing a close hospital in favor of a distant hospital with a cardiac catheterization lab that was open and staffed at the time of hospital arrival.
Seventeen models were thus estimated within each of the ten imputed datasets. For every model, observations were weighted using the inverse propensity for being of white race, continuous variables were centered on their means, and neighborhood characteristics were adjusted to account for differences of one standard deviation. We combined models across the ten datasets by taking the average of coefficients and standard errors and inflating the errors with between-model variation.7
The authors had full access to the data and take responsibility for its integrity. All authors have read and agree to the manuscript as written. The research protocol was deemed exempt by Institutional Review Boards at Tufts Medical Center and University of Texas-Southwestern.
Results
After exclusions, 5,887 calls were included (Figure 2). Table 1 presents baseline characteristics of the cohort. Average age was 57.9 (standard deviation 17.7) years. Women comprised 50.8% of the cohort and people of white race comprised 49.9%. After weights were applied (c=0.76), there were no significant differences between white and non-white patients on measured covariates.
Table 1. Baseline Characteristics of the Cohort.
| Covariates | N | Value* |
|---|---|---|
| Distance Characteristics | ||
| Distance: EMS Depot to scene (miles) | 5650 | 0.9 (0.45) |
| Distance: Scene to hospital (miles) | 5321 | 4.05 (3.3) |
| Time Characteristics | ||
| Rush hour, morning (%) | 5887 | 8.7 |
| Rush hour, evening (%) | 5887 | 8.5 |
| Weekday (%) | 5887 | 75.3 |
| Patient characteristics | ||
| Age (yrs.) | 4556 | 57.9 (17.7) |
| Female (%) | 5887 | 50.8 |
| Race/Ethnicity | 5887 | - |
| White | - | 49.9 |
| Black | - | 32.1 |
| Latin/Hispanic | - | 8.8 |
| Asian/Pacific Islander | - | 2.6 |
| Native American | - | 2.4 |
| Other | - | 1.2 |
| Unknown | - | 3.0 |
| Diastolic blood pressure (mmHg) | 5166 | 89.3 (21.3) |
| Systolic Blood Pressure (mmHg) | 5370 | 148.9 (34.2) |
| Pulse (beats/min.) | 5824 | 87.1 (41.1) |
| Respiratory rate (breaths/min.) | 5716 | 18.0 (6.7) |
| Neighborhood Characteristics | ||
| Population density (1,000 residents/square mile.) | 5865 | 5.3 (2.8) |
| Race (% white) | 5865 | 43.9 (30.4) |
| Birthplace (% Foreign-born) | 5865 | 16.4 (15.5) |
| Income (%households < 200% FPL) | 5865 | 35.6 (22.7) |
Values are given in %, or mean (standard deviation)
The average patient
Our “as the crow flies” estimate of travel distance in segment one (firehouse to scene) averaged 0.9 miles (inter-quartile range: 0.6, 1.2) and the average elapsed time was 5.7 minutes (4.0, 6.0). Average time spent in segment two (on-scene) was 19.9 minutes (15.0, 24.0). In time segment three (scene to hospital), average distance was 4.1 miles (1.9, 5.4) and average elapsed time was 10.3 minutes (5.0, 13.0). Total distance was 5.0 miles (2.7 3, 6.4) and average time was 35.9 minutes (28.0, 41.0). Median time in EMS was 34 minutes.
Table 2 presents the results of the most comprehensive analytic model, including all distance, time, patient and neighborhood characteristics. Over total elapsed time, each mile traveled to and from the scene contributed 1.3 minutes. Patients who were transported during evening rush hour spent a little over 2 additional minutes in EMS care. Blacks and whites, the two largest race groups, had nearly identical transport times on average. Asian/Pacific Islanders and Native Americans spent 2.9 and 3.0 minutes longer, respectively, than did whites. Women were delivered to the hospital 2.3 minutes slower on average than men. Characteristics of the neighborhood from which a patient called did not make a statistically significant contribution to total time.
Table 2. Time Spent in EMS Transport, in Minutes.
| Elapsed Time (in minutes) |
||||
|---|---|---|---|---|
| Covariates | Segment 1: Response (s.e.) |
Segment 2: On-scene (s.e.) |
Segment 3: Transport (s.e.) |
Total: EMS Depot to Hospital (s.e.) |
| Distance | ||||
| Distance: EMS Depot to scene (miles) |
0.92 (0.11)‡ | -- | -- | 1.33 (0.34) ‡ |
| Distance: Scene to hospital (miles) |
-- | -- | 1.21 (0.03) ‡ | 1.33 (0.05) ‡ |
| Time | ||||
| Rush hour (morning) | 0.40 (0.17)* | -- | -0.15 (0.35) | 0.57 (0.48) |
| Rush hour (evening) | 0.01 (0.17) | -- | 1.37 (0.34) ‡ | 2.01 (0.50) ‡ |
| Weekday | 0.04 (0.11) | 0.33 (0.23) | 0.31 (0.23) | 0.56 (0.33) |
| Patient Characteristics | ||||
| Black | -0.01 (0.11) | -0.25 (0.24) | 0.38 (0.24) | 0.08 (0.34) |
| Latin/Hispanic | 0.65 (0.17) ‡ | -0.60 (0.35) | -0.05 (0.33) | 0.10 (0.48) |
| Asian/Pacific Islander | -0.95 (0.32)† | 2.76 (0.67) ‡ | -0.97 (0.64) | 2.88 (0.91)† |
| Native American | -0.48 (0.29) | 2.36 (0.61) ‡ | 1.17 (0.58)* | 3.03 (0.84) ‡ |
| Other Race (not white/other) |
-1.05 (0.35)† | -0.25 (0.78) | -0.37 (0.79) | -1.72 (1.16) |
| Unknown Race | -0.40 (0.22) | 3.44 (0.48) ‡ | 0.52 (0.49) | 0.03 (0.01) ‡ |
| Age (yrs.) | -0.01 (0.00)* | 0.03 (0.01) ‡ | 0.01 (0.01) | 0.03 (0.01)* |
| Female | -0.23 (0.10)* | -1.51 (0.20) ‡ | 0.57 (0.20) | -2.30 (0.28) ‡ |
| Neighborhood Characteristics | ||||
| Population density (residents/sq.mi.) |
-0.10 (0.05)* | 0.27 (0.11)* | -0.07 (0.10) | 0.26 (0.15) |
| Race (% white) | 0.02 (0.07) | 0.68 (0.16) ‡ | -0.45 (0.16)† | 0.36 (0.22) |
| Birthplace (% Foreign-born) |
-0.01 (0.06) | 0.16 (0.12) | -0.16 (0.11) | 0.01 (0.17) |
| Income (% households under 200% FPL) |
0.18 (0.07)* | -0.21 (0.15) | -0.18 (0.15) | -0.10 (0.21) |
p < 0.05
p < 0.01
p < 0.001
All estimates are adjusted for patient vital statistics, including blood pressure, pulse and respiratory rate. White race and male are reference categories. Continuous variables were centered on their mean value. Coefficients on neighborhood level covariates represent the change in outcome per one standard deviation from the mean
Delayed Patients
Of 5,887 patient calls, 647 (11.0%) resulted in delays of 15 minutes or more (≥49 minutes) beyond median time (34 minutes). Of these 647, average time was 58.6 minutes and average distance was 7.8 miles. In segment one, delayed patients traveled one mile in 6.5 minutes, roughly the same as the average patient. EMS personnel spent 28.3 minutes on scene, approximately 9 minutes longer than average. In segment three, patients traveled nearly seven miles in 27.7 minutes, or 13.4 minutes longer than average.
Table 3 presents ratios for the odds of delay. Women had significantly higher odds [OR 1.52 (95% CI: 1.32, 1.74)] of being in the delay group. Each additional mile traveled gave patients 9-46% greater odds of being in the delay group. Traveling during evening rush hour, bypassing a local hospital, being Asian/Pacific Islander, Native American or of unknown race also increased the odds of being delayed while being of “other” race decreased the odds.
Table 3. Odds of Being Delayed in EMS Care.
| Covariates | Odds of Delay (95% CI) (> median time + 15 minutes) |
|---|---|
| Distance Characteristics | |
| Distance: EMS Depot to scene (miles) | 1.26 (1.09, 1.46) |
| Distance: Scene to hospital (miles) | 1.22 (1.20, 1.25) |
| Bypass | 1.81 (1.53, 2.15) |
| Time Characteristics | |
| Rush hour (morning) | 1.18 (0.93, 1.49) |
| Rush hour (evening) | 1.97 (1.59, 2.43) |
| Weekday | 1.04 (0.87, 1.24) |
| Patient Characteristics | |
| Black | 1.15 (0.97, 1.35) |
| Latin/Hispanic | 1.02 (0.81, 1.31) |
| Asian/Pacific Islander | 1.89 (1.29, 2.78) |
| Native American | 1.60 (1.11, 2.29) |
| Other Race (not white/other) | 0.35 (0.15, 0.79) |
| Unknown Race | 1.74 (1.29, 2.35) |
| Age (yrs.) | 1.00 (1.00, 1.01) |
| Female | 1.52 (1.32, 1.74) |
| Neighborhood Characteristics | |
| Population density (thousand residents/square mile.) |
1.11 (1.03, 1.19) |
| Race (% white) | 1.16 (1.04, 1.29) |
| Birthplace (% Foreign-born) | 0.95 (0.88, 1.04) |
| Income (%households < 200% FPL) | 1.04 (0.93, 1.15) |
All estimates are adjusted for patient vital statistics, including blood pressure, pulse and respiratory rate. White race and male are reference categories. Continuous variables were centered on their mean value. Coefficients on neighborhood level covariates represent the change in outcome per one standard deviation from the mean
Being from a more densely populated neighborhood modestly increased the odds of delay. Being from a white neighborhood appeared at first to contribute to delay, but this effect was not monotonic. We separately assessed the adjusted odds of delay for patients from the four quartiles of white concentration. Neighborhoods in the 3rd quartile were more likely than all others to be delayed, and this effect was strong enough to persist over the continuous measure.
Discussion
Our study of patient and neighborhood characteristics associated with time in EMS in ten municipalities in Dallas County, Texas, including 29 hospitals and 98 EMS stations over a one-year period, showed that women were 50% more likely than men to be seriously delayed while in EMS care. This difference remained even after adjusting for day of week and time of day of symptom onset, EMS transport distance, age, race, vital signs as an indicator of clinical severity, and neighborhood socio-economic composition.
Our primary conclusion is consistent with a large body of research into gender disparities in acute coronary syndromes. Women with heart attack are more likely to delay seeking emergency medical care.11, 12 They present with higher risk,13 are less likely to receive percutaneous coronary intervention (PCI),14 have longer door-to-balloon times15 and are more likely to die before discharge, even after controlling for older age and higher severity.16 Whether gender differences in presentation, care, and outcomes are the result of bias or biology, further explanation of their causes is needed.17 Our results suggest that this need may extend to the EMS setting.
Though our analysis does not reveal why women were more likely to be delayed, previous research suggests a plausible explanation: symptom presentation in women with cardiac disease differs from that of men18 and a coronary event may not be recognized as readily by the patient19 or by EMS personnel. Inappropriate delays may occur because there is less certainty of cardiac involvement, because more time is spent diagnosing the condition, because the patient’s condition may not be seen as emergent, or as the result of some combination of these factors.
The results also suggest that other patient characteristics (race and age) influenced average elapsed time and delays, while neighborhood socio-economic composition had no meaningful effect. In all cases, however, variation in average time was too small to be clinically meaningful. This may be explained in part by the relatively brief time from emergency call to hospital delivery in this region. In regions that manage similarly brief transport, we would not expect to find meaningful average variation by patient or neighborhood characteristics. In all variables other than gender, variation in the odds of delay involved very few individuals. For Asian/Pacific Islanders, Native Americans and people of unknown race, the odds of being delayed were statistically significant but the number of patients affected was small (20, 18 and 22 individuals, respectively, were delayed for reasons other than bypassing a hospital).
Our second conclusion is that long delays should be a special focus of research in the EMS setting. In our study, women arrived at the hospital on average just over 2.3 minutes later than men, not long enough to be clinically meaningful. However, women were also 50% more likely to be seriously delayed. By dichotomizing the time variable and looking at the extreme of the distribution, we were able to identify variables that had an important effect on serious delays. Had we concentrated only on average elapsed time and to the exclusion of delays, our study could have obscured a significant and meaningful gender disparity. A previous study of time in EMS for patients with stroke,20 for example, found variation in average time to hospital arrival, including a 5 minute lag for black compared to white patients after adjusting for age, distance traveled and area poverty. As in our study, this lag was not large enough to be clinically meaningful. However, there was evidence of potentially hazardous delay for some patients in the study. Median and maximum time from 9-1-1 to hospital arrival were 28 and >90 minutes, respectively, representing at least a 62 minute gap between the typical and most delayed patients, but this study did not evaluate the gap for evidence of disparities, despite the signal of slower average time for patients of black race. We suggest that the determinants of serious delay should be included in all EMS studies where time to treatment is a priority.
Our findings have several implications for future research. Our primary finding - that women with cardiac related complaints are at greater risk for delay in EMS than are men - should be tested in a range of geographic settings. Similarly, elapsed time in EMS should be studied in other clinical domains. As already discussed, the determinants of serious delay should be a special focus of EMS studies where time to treatment is a priority. Finally, qualitative research should be directed at understanding why delays occur. To make such research possible, EMS systems must continue to make improvements in the collection, maintenance and reporting of patient data. Both qualitative and quantitative data are needed on patient experiences from 911 through hospital discharge. Efforts to improve EMS “run sheet” documentation according to national standards should be a top priority. Toward this end, considerable progress has already been made through the National EMS Information System (NEMSIS) and its Technical Assistance Center.21 EMS systems must also continue to test and evaluate methods to improve quality and reduce time to hospital arrival. Results from several regional EMS pilot projects around the US suggest there is unmet potential in both of these domains. These have included the introduction of electrocardiograms (ECG) and hospital pre-notification into the EMS setting.22-26 Decision aids for triage of patients with acute cardiac ischemia (ACI) and ST-elevation myocardial infarction (STEMI) have been implemented safely and effectively in the emergency department setting, 27-29 and calls have been growing for their use in EMS.24, 30 The American Heart Association’s nascent Mission: Lifeline program is designed to assess and improve EMS effectiveness as part of a system-wide quality improvement program for the care of patients with STEMI.31
This study faced some limitations. Compared to US Census data, Latin/Hispanic ethnicity was underrepresented and white race was overrepresented in our dataset, probably as a result of misclassification. Improved methods of collecting patient data in the EMS setting might lead to new observations about the interaction of race and time to treatment. Second, we studied time in EMS in only one region. We selected Dallas County for its size, diversity, and composition of urban, suburban and rural districts, but the primary advantage of this setting was its self-contained EMS and hospital systems, allowing us to estimate effects in an area with little confounding at the borders. Third, our analytic models tested for multiple potential associations with delay, increasing the probability of a spurious false positive result. However, the association between gender and delay was both robust to adjustment and monotonic across the distribution of elapsed time. Furthermore, it is consistent with a large body of previous research on gender in cardiac care. We believe our analysis and results make a strong case for the existence of a gender disparity in the EMS setting.
In summary, we found that women with cardiac complaints were more likely to be delayed in EMS, even after adjusting for distance, onset time, patient vitals, age, race and neighborhood. This result would have been missed if we focused solely on average elapsed time, to the exclusion of delays. Serious delays should be a special focus of research in the EMS setting. Future research should examine delay in other geographic settings and clinical domains, explore why delay occurs, and evaluate interventions for eliminating unnecessary delay. Continued efforts to improve the collection, maintenance and reporting of EMS data; to improve quality; and to reduce elapsed time from 9-1-1 to hospital arrival should be a top priority.
Acknowledgements
Dr. Concannon was supported by Grants RO1 HS010282 and T32 HS00060-12 from the Agency for Healthcare Research and Quality (AHRQ), and by the Tufts Medical Center - Pfizer Career Development Award. The funding organizations had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Disclosures
The authors have no conflicts of interest or other financial disclosures to report.
References
- 1.Boersma E, Maas AC, Deckers JW, Simoons ML. Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet. 1996;348:771–775. doi: 10.1016/S0140-6736(96)02514-7. [DOI] [PubMed] [Google Scholar]
- 2.Weaver WD. Time to thrombolytic treatment: factors affecting delay and their influence on outcome. J Am Coll Cardiol. 1995;25:3S–9S. doi: 10.1016/0735-1097(95)00108-g. [DOI] [PubMed] [Google Scholar]
- 3.Bradley EH, Herrin J, Wang Y, Barton BA, Webster TR, Mattera JA, Roumanis SA, Curtis JP, Nallamothu BK, Magid DJ, McNamara RL, Parkosewich J, Loeb JM, Krumholz HM. Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med. 2006;355:2308–2320. doi: 10.1056/NEJMsa063117. [DOI] [PubMed] [Google Scholar]
- 4.Hutchings CB, Mann NC, Daya M, Jui J, Goldberg R, Cooper L, Goff DC, Jr, Cornell C. Patients with chest pain calling 9-1-1 or self-transporting to reach definitive care: which mode is quicker? Am Heart J. 2004;147:35–41. doi: 10.1016/s0002-8703(03)00510-6. [DOI] [PubMed] [Google Scholar]
- 5.Canto JG, Zalenski RJ, Ornato JP, Rogers WJ, Kiefe CI, Magid D, Shlipak MG, Frederick PD, Lambrew CG, Littrell KA, Barron HV. Use of Emergency Medical Services in Acute Myocardial Infarction and Subsequent Quality of Care: Observations From the National Registry of Myocardial Infarction 2. Circulation. 2002;106:3018–3023. doi: 10.1161/01.cir.0000041246.20352.03. [DOI] [PubMed] [Google Scholar]
- 6.Concannon TW, Kent DM, Normand SL, Newhouse JP, Griffith JL, Ruthazer R, Beshansky JR, Wong JB, Aversano T, Selker HP. A Geospatial Analysis of Emergency Transport and Inter-Hospital Transfer in ST-Segment Elevation Myocardial Infarction. Am J Cardiol. 2008;101:69–74. doi: 10.1016/j.amjcard.2007.07.050. [DOI] [PubMed] [Google Scholar]
- 7.Little RJA, Rubin DB. Statistical Analysis with Missing Data. J. Wiley & Sons; New York: 1987. [Google Scholar]
- 8.Schafer JL. Analysis of Incomplete Multivariate Data. Chapman & Hall; London: 1997. [Google Scholar]
- 9.Lunceford JK, Davidian M. Stratification and weighting via the propensity score in estimation of causal treatment effects: a comparative study. Stat Med. 2004;23:2937–2960. doi: 10.1002/sim.1903. [DOI] [PubMed] [Google Scholar]
- 10.Apparecio P, Shearmur R, Brochu M, Dussault G. The Measure of Distance in a Social Science Policy Context: Advantages and Costs of using Network Distances in Eight Canadian Metropolitan Areas. Journal of Geographic Information and Decision Analysis. 2003;7:105–131. [Google Scholar]
- 11.Goldberg RJ, Gurwitz JH, Gore JM. Duration of, and temporal trends (1994-1997) in, prehospital delay in patients with acute myocardial infarction: the second National Registry of Myocardial Infarction. Arch Intern Med. 1999;159:2141–2147. doi: 10.1001/archinte.159.18.2141. [DOI] [PubMed] [Google Scholar]
- 12.Zijlstra F, Patel A, Jones M, Grines CL, Ellis S, Garcia E, Grinfeld L, Gibbons RJ, Ribeiro EE, Ribichini F, Granger C, Akhras F, Weaver WD, Simes RJ. Clinical characteristics and outcome of patients with early (<2 h), intermediate (2-4 h) and late (>4 h) presentation treated by primary coronary angioplasty or thrombolytic therapy for acute myocardial infarction. Eur Heart J. 2002;23:550–557. doi: 10.1053/euhj.2001.2901. [DOI] [PubMed] [Google Scholar]
- 13.Mehilli J, Ndrepepa G, Kastrati A, Nekolla SG, Markwardt C, Bollwein H, Pache J, Martinoff S, Dirschinger J, Schwaiger M, Schömig A. Gender and myocardial salvage after reperfusion treatment in acute myocardial infarction. J Am Coll Cardiol. 2005;45:828–831. doi: 10.1016/j.jacc.2004.11.054. [DOI] [PubMed] [Google Scholar]
- 14.Blomkalns AL, Chen AY, Hochman JS, Peterson ED, Trynosky K, Diercks DB, Brogan GX, Jr, Boden WE, Roe MT, Ohman EM, Gibler WB, Newby LK. Gender disparities in the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: large-scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative. J Am Coll Cardiol. 2005;45:832–837. doi: 10.1016/j.jacc.2004.11.055. [DOI] [PubMed] [Google Scholar]
- 15.Angeja BG, Gibson CM, Chin R, Frederick PD, Every NR, Ross AM, Stone GW, Barron HV. Predictors of door-to-balloon delay in primary angioplasty. Am J Cardiol. 2002;89:1156–1161. doi: 10.1016/s0002-9149(02)02296-8. [DOI] [PubMed] [Google Scholar]
- 16.Milcent C, Dormont B, Durand-Zaleski I, Steg PG. Gender Differences in Hospital Mortality and Use of Percutaneous Coronary Intervention in Acute Myocardial Infarction: Microsimulation Analysis of the 1999 Nationwide French Hospitals Database. Circulation. 2007;115:833–839. doi: 10.1161/CIRCULATIONAHA.106.664979. [DOI] [PubMed] [Google Scholar]
- 17.Anderson RD, Pepine CJ. Gender Differences in the Treatment for Acute Myocardial Infarction: Bias or Biology? Circulation. 2007;115:823–826. doi: 10.1161/CIRCULATIONAHA.106.685859. [DOI] [PubMed] [Google Scholar]
- 18.Zucker DR, Griffith JL, Beshansky JR, Selker HP. Presentations of acute myocardial infarction in men and women. J Gen Intern Med. 1997;12(2):79–87. doi: 10.1046/j.1525-1497.1997.00011.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Finnegan JR, Jr, Meischke H, Zapka JG, Leviton L, Meshack A, Benjamin-Garner R, Estabrook B, Hall NJ, Schaeffer S, Smith C, Weitzman ER, Raczynski J, Stone E. Patient Delay in Seeking Care for Heart Attack Symptoms: Findings from Focus Groups Conducted in Five U.S. Regions. Preventive Medicine. 2000;31:205–213. doi: 10.1006/pmed.2000.0702. [DOI] [PubMed] [Google Scholar]
- 20.Kleindorfer DO, Lindsell CJ, Broderick JP, et al. Community Socioeconomic Status and Prehospital Times in Acute Stroke and Transient Ischemic Attack: Do Poorer Patients Have Longer Delays From 911 Call to the Emergency Department? Stroke. 2006;37:1508–1513. doi: 10.1161/01.STR.0000222933.94460.dd. [DOI] [PubMed] [Google Scholar]
- 21.National EMS Information System (NEMSIS) Update; Joint National EMS Teleconference; 2007; http://www.nemsis.org/media/ppt/JointNationalEMSLeadershipPresentation.ppt. [Google Scholar]
- 22.Jacobs AK, Antman EM, Ellrodt G, Faxon DP, Gregory T, Mensah GA, Moyer P, Ornato J, Peterson ED, Sadwin L, Smith SC. Recommendation to develop strategies to increase the number of ST-segment-elevation myocardial infarction patients with timely access to primary percutaneous coronary intervention. Circulation. 2006;113:2152–2163. doi: 10.1161/CIRCULATIONAHA.106.174477. [DOI] [PubMed] [Google Scholar]
- 23.Moyer P, Ornato JP, Brady WJ, Jr, Davis LL, Ghaemmaghami CA, Gibler WB, Mears G, Mosesso VN, Jr, Zane RD, The Emergency Medical Services. Emergency Department Perspective Development of Systems of Care for ST-Elevation Myocardial Infarction Patients. Circulation. 2007;116:e43–e48. doi: 10.1161/CIRCULATIONAHA.107.184047. [DOI] [PubMed] [Google Scholar]
- 24.Garvey JL, MacLeod BA, Sopko G, Hand MM, National Heart, Lung, and Blood Institute (NHLBI) National Institutes of Health Pre-Hospital 12-Lead Electrocardiography Programs: A Call for Implementation by Emergency Medical Services Systems Providing Advanced Life Support--National Heart Attack Alert Program (NHAAP) Coordinating Committee. J Am Coll Cardiol. 2006;47:485–491. doi: 10.1016/j.jacc.2005.08.072. [DOI] [PubMed] [Google Scholar]
- 25.Jollis JG, Roettig ML, Aluko AO, Anstrom KJ, Applegate RJ, Babb JD, Berger PB, Bohle DJ, Fletcher SM, Garvey JL, Hathaway WR, Hoekstra JW, Kelly RV, Maddox WT, Jr, Shiber JR, Valeri FS, Watling BA, Wilson BH, Granger CB. Implementation of a Statewide System for Coronary Reperfusion for ST-Segment Elevation Myocardial Infarction. JAMA. 2007;298:2371–2380. doi: 10.1001/jama.298.20.joc70124. [DOI] [PubMed] [Google Scholar]
- 26.Henry TD, Sharkey SW, Burke MN, Chavez IJ, Graham KJ, Henry CR, Lips DL, Madison JD, Menssen KM, Mooney MR, Newell MC, Pedersen WR, Poulose AK, Traverse JH, Unger BT, Wang YL, Larson DM. A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation. 2007;116:721–728. doi: 10.1161/CIRCULATIONAHA.107.694141. [DOI] [PubMed] [Google Scholar]
- 27.Selker HP, Griffith JL, D’Agostino RB. A time-insensitive predictive instrument for acute myocardial infarction mortality: a multicenter study. Med Care. 1991;29:1196–1211. doi: 10.1097/00005650-199112000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Selker HP, Beshansky JR, Griffith JL, Aufderheide TP, Ballin DS, Bernard SA, Crespo SG, Feldman JA, Fish SS, Gibler WB, Kiez DA, McNutt RA, Moulton AW, Ornato JP, Podrid PJ, Pope JH, Salem DN, Sayre MR, Woolard RH. Use of the acute cardiac ischemia time-insensitive predictive instrument (ACI-TIPI) to assist with triage of patients with chest pain or other symptoms suggestive of acute cardiac ischemia. A multicenter, controlled clinical trial. Ann Intern Med. 1998;129:845–855. doi: 10.7326/0003-4819-129-11_part_1-199812010-00002. [DOI] [PubMed] [Google Scholar]
- 29.Selker HP, Beshansky JR, Griffith JL. Use of the electrocardiograph-based thrombolytic predictive instrument to assist thrombolytic and reperfusion therapy for acute myocardial infarction. A multicenter, randomized, controlled, clinical effectiveness trial. Ann Intern Med. 2002;137:87–95. doi: 10.7326/0003-4819-137-2-200207160-00006. [DOI] [PubMed] [Google Scholar]
- 30.Moyer P, Levine J, Beshansky J, Selker HP, Barnewolt B, Brown DFM, Cardoza JP, Jr., Grossman SA, Jacobs A, Kerman B, Kimmelstein C, Larson R, Losordo D, Perlmutter M, Pozner C, Ramirez A, Rosenfield K, Ryan TJ, Zane RD, Cannon CP. Implications of the Mechanical (PCI) vs. thrombolytic controversy for ST segment elevation myocardial infarction on the organization of emergency medical services: the Boston EMS experience. Crit Pat Cardiol. 2004;3:53–61. doi: 10.1097/01.hpc.0000128714.35330.6d. FJ. [DOI] [PubMed] [Google Scholar]
- 31.Jacobs AK, Antman EM, Faxon DP, Gregory T, Solis P. Development of Systems of Care for ST-Elevation Myocardial Infarction Patients. Executive Summary. Circulation. 2007;116:217–230. doi: 10.1161/CIRCULATIONAHA.107.184043. [DOI] [PubMed] [Google Scholar]