Abstract
We have reviewed the clinical presentations, courses, and outcomes of 90 patients seen at Texas Children's Hospital from 1983 through 2008 who had an isolated cleft of the mitral valve without some form of endocardial cushion defect. Additional congenital cardiac defects were present in 61 of the 90 patients, 35 of whom had a congenital syndrome. Seven patients had isolated cleft of the mitral valve without other intracardiac defects, and in these 7 there was a progressive increase in the degree of mitral regurgitation during a median time of 26.5 months from diagnosis to surgery. The patients ranged from a gestational age of approximately 32 weeks to 21.9 years of age. No death was observed among the 39 surgical patients, including 32 who had additional cardiac defects. There was a significant reduction in the degree of mitral regurgitation in all patients who underwent surgery. Among the 51 patients who did not have surgery, the degree of regurgitation did not change significantly over the course of 1 to 27 years' observation.
Isolated cleft of the mitral valve is an uncommon (but not rare) congenital malformation of the mitral valve that can cause all degrees of mitral regurgitation but can be managed medically or surgically.
Key words: Adolescent; child; echocardiography, Doppler; heart defects, congenital/surgery/ultrasonography; infant; mitral valve/abnormalities/ultrasonography; mitral valve insufficiency; retrospective studies
Isolated cleft of the mitral valve, not associated with endocardial cushion defects, is an uncommon congenital anomaly of the mitral valve. Most reports1–4 describe moderate-to-severe regurgitation of the mitral valve, which often requires surgical intervention. We reviewed our experience with this condition at Texas Children's Hospital and found that many patients had only minor clefting of the septal leaflet of the mitral valve, which did not require surgery. With use of high-resolution echocardiography, skilled technicians are able to identify even minor clefts in the mitral valve. This condition is probably more common than previously realized.
Patients and Methods
A search of the clinical and echocardiographic databases at Texas Children's Hospital identified 90 patients seen from 1983 through 2008 who had an isolated cleft of the mitral valve leaflet, not associated with an endocardial cushion defect (complete atrioventricular septal defect, primum atrial septal defect, or left ventricle-to-right atrial defect) or with an inlet ventricular septal defect (VSD). The diagnosis was made primarily by 2-dimensional echocardiography and in some cases by surgical inspection. The degree of mitral regurgitation was evaluated by 2-dimensional echocardiography and graded as none, trace or mild, moderate, or severe.
The patients were divided into 2 groups: surgical patients (39 in number, whose diagnoses were confirmed at surgery), and nonsurgical patients (51 in number). Four of the surgical patients had surgery at other hospitals and later were monitored at Texas Children's Hospital.
Surgical Technique
In preparation for mitral valve repair, patients underwent aorto-bicaval cannulation with cardioplegic arrest at 28 °C. The mitral valve was approached either directly through a left atriotomy or transeptally. After inspection of the intracardiac anatomy, the cleft in the mitral valve was repaired using multiple interrupted 7-0 polypropylene sutures. In the presence of annular dilation (in 13 patients), the repair was buttressed by means of either a Kaye annuloplasty or an annuloplasty band, depending on the age of the patient.
Statistical Analysis
The paired Wilcoxon sum rank test was used to compare the degree of regurgitation from the 1st echocardiogram with the last echocardiogram at follow-up (for the nonsurgical patients); and from the immediate preoperative with the last postoperative echocardiogram (for the surgical patients). A P value of <0.05 was considered to be significant.
This review was carried out under the Institutional Review Board protocol of Baylor College of Medicine and Texas Children's Hospital
Results
Among the 90 patients found to have an isolated cleft of the septal leaflet of the mitral valve, not associated with any form of endocardial cushion defect or inlet VSD, we identified additional cardiac malformations in 61 patients (some of whom had multiple malformations): VSD (32 patients), left ventricular outflow tract (LVOT) obstruction (12), subaortic stenosis (9), aortic valve stenosis (3), secundum atrial septal defect (14), patent ductus arteriosus (13), tetralogy of Fallot (2), transposition of the great arteries, VSD, and pulmonary stenosis (2), congenitally corrected transposition (1), tricuspid atresia (1), and Shone's anomaly (1). Thirty-five patients had syndromes: trisomy 21 (26 patients), CHARGE syndrome (2), heterotaxy syndrome (2), other chromosome defects (2), Holt-Oram syndrome (1), Williams syndrome (1), and Noonan's syndrome (1).
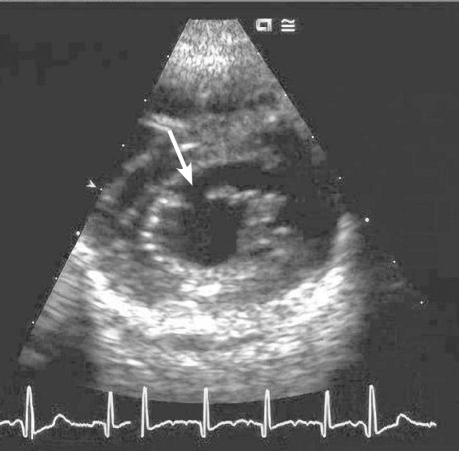
The median age at the 1st echocardiogram was 2 years, ranging from a gestational age of approximately 32 weeks (in a fetus with trisomy 21) to 21.9 years. The presence of mitral regurgitation was evaluated on the 1st echocardiogram in 86 patients and was classified as none (7 patients), trace or mild (44), moderate (27), and severe (8). The cleft was in the septal leaflet of the mitral valve in all patients and was oriented towards the LVOT (Figs. 1 and 2) rather than towards the ventricular septum, as in patients with some form of endocardial cushion defect.
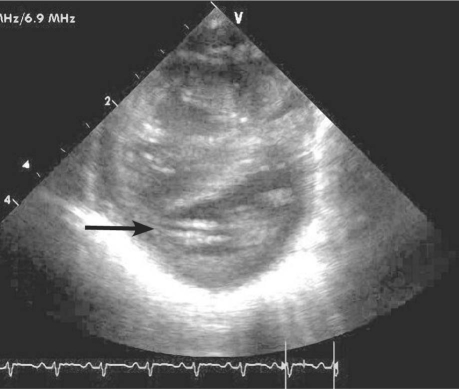
Fig. 1. This short-axis echocardiographic view of the left ventricle in a patient with a complete atrioventricular septal defect shows the “cleft” between the anterior and posterior bridging atrioventricular valve leaflets in systole. The cleft “points” towards the inlet septum (arrow).
Fig. 2. This short-axis view of the left ventricle in diastole shows an isolated cleft of the septal leaflet of the mitral valve. The cleft “points” towards the left ventricular outflow tract (arrow).
Additional anomalies of the mitral valve were present in 58 patients: thickening of the leaflets (23 patients), prolapse of the anterior leaflet (12), and papillary muscle anomalies (5)—including fusion of the muscles in 2 patients and single papillary muscle in 1. Anomalous insertion of the anterior leaflet chordae, usually towards the LVOT, was present in 16 patients. Left ventricular outflow tract obstruction occurred in 12 patients but was not associated with the anomalous chordal insertion.
Surgical Results
Cleft closure was performed in 39 patients at a median age of 5.4 years (range, 1 mo–21.4 yr). The median time to surgical intervention from the initial diagnosis was 15.7 months (range, 1 wk–16.5 yr). There were no operative deaths. One patient, a 13-year-old with aortic insufficiency and a VSD, required mitral valve replacement.
Follow-Up
A follow-up echocardiogram was obtained in 87 patients, 37 of whom had undergone surgical repair of the mitral valve 1 month to 20.4 years previously (median, 2.78 yr).
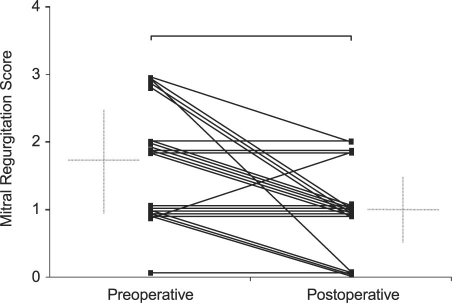
Follow-Up of Surgical Patients. Of the 39 patients who underwent surgery to repair the mitral valve, 37 had preoperative echocardiograms available for review: 2 patients had no preoperative regurgitation, 11 had mild, 16 had moderate, and 8 had severe. Postoperatively, 38 patients had echocardiograms available for review; these tests had been performed at a median of 3.2 postoperative years (range, 1 mo–16.5 yr). Four patients had no postoperative regurgitation, 29 had mild, and 5 had moderate; no patient had severe postoperative regurgitation (Fig. 3). The difference between preoperative and postoperative echocardiographic results is highly significant (P = 0.00005).
Fig. 3. A plot of the mitral regurgitation scores in 39 surgical patients, from the immediate preoperative echocardiogram to the last follow-up echocardiogram.
Six patients underwent repair of an isolated mitral cleft without other cardiac defects. All 6 had moderate-to-severe preoperative mitral regurgitation, and in 1 patient the regurgitation had progressed from mild to severe before surgery. After surgery, all of these patients displayed only mild regurgitation.
At 3 to 9 postoperative years, 4 patients developed mild-to-moderate mitral stenosis. The age at corrective surgery was 13 to 21 years, and all received a mitral ring as part of the annuloplasty procedure. The postoperative mitral gradients ranged from 4 to 14 mmHg. None of these patients has had further surgery.
Follow-Up of Nonsurgical Patients. Of the 50 patients who did not have mitral valve surgery, at initial presentation 6 had no regurgitation, 33 had mild, 11 had moderate, and none had severe.
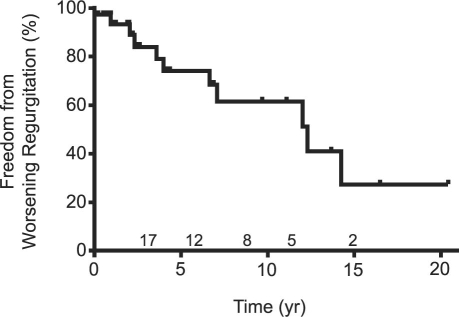
At last follow-up in the 50 nonsurgical patients (range, 0 to 27.7 years [median, 1.6 yr] after the initial echocardiogram), 4 patients had no regurgitation, 32 had mild, 14 had moderate, and none had severe. The difference between echocardiographic results at initial presentation and last follow-up is not significant (P = 0.18). A Kaplan-Meier curve (Fig. 4) depicts the freedom from worsening mitral regurgitation in 37 nonsurgical patients who had at least 2 follow-up echocardiograms during the study period.
Fig. 4. Kaplan-Meier plot of the freedom from worsening mitral regurgitation from the 1st echocardiogram to the last follow-up echocardiogram, in 37 nonsurgical patients who had at least 2 echocardiograms. The numbers above the X axis are the numbers of patients available for follow-up at 3, 6, 9, 12, and 15 years.
Two premature infants who did not undergo surgery died of unrelated causes 1 and 2 months after diagnosis.
Discussion
An isolated cleft of the mitral valve, not associated with some form of endocardial cushion defect, is a very uncommon (but not rare) congenital malformation of the septal leaflet and sometimes of the posterior leaflet. This condition was first described in 1987 by Petitalot and colleagues,1 and most subsequent reports haveconcerned cases of 1 to 5 patients who have displayed severe regurgitation. The morphology of the mitral valve and the cleft in the septal leaflet have been well delineated both by echocardiographic and gross pathologic studies.2,3 This cleft can be wide and extend to the mitral annulus, but it can be only a few millimeters deep and display minimal regurgitation. A similar cleft has been described in the posterior leaflet of the mitral valve.4 The edges of the mitral valve tend to be thicker and more retracted in older patients. The isolated mitral cleft is oriented towards the LVOT rather than towards the inlet septum, as is seen in the “cleft” between the anterior and posterior bridging mitral leaflets of patients who have endocardial cushion defects.5,6
Repair of the mitral cleft is usually straightforward. Our method of repair involves the use of an interrupted suture technique and fine monofilament suture. The repair is buttressed with an annuloplasty in patients who have a dilated mitral annulus. The surgical results in our series have been excellent. Most patients display mild postoperative regurgitation, a significant reduction in grade.7,8
An isolated cleft can be diagnosed adequately by means of 2-dimensional echocardiography with Doppler interrogation or by means of 3-dimensional echocardiography.9 Because the mitral septal leaflet is often thickened and distorted, the investigator must rule out mitral regurgitation due to rheumatic fever or endocarditis. The high incidence of associated congenital cardiac defects has an unlooked-for benefit: often, a significant cleft can be repaired at the time of repair of the other cardiac lesions. When the cleft mitral valve is the only defect, repair must be initiated on the basis of the usual clinical and echocardiographic criteria. If the degree of regurgitation is only mild-to-moderate, surgical repair is not urgent, because the regurgitation does not progress over the intermediate term.
Footnotes
Address for reprints: Michael R. Nihill, MD, Section of Pediatric Cardiology, Texas Children's Hospital, WT 19345-C, 6621 Fannin St., Houston, TX 77030
E-mail: nihill@bcm.tmc.edu
References
- 1.Petitalot JP, Chaix AF, Bonneau G, Rousseau G, Barraine R. Latent congenital mitral insufficiency caused by an isolated mitral cleft. Diagnosis by two-dimensional echocardiography and pulsed Doppler [in French]. Ann Cardiol Angeiol (Paris) 1987;36(7):347–50. [PubMed]
- 2.Di Segni E, Kaplinsky E, Klein HO. Color Doppler echocardiography of isolated cleft mitral valve. Roles of the cleft and the accessory chordae. Chest 1992;101(1):12–5. [DOI] [PubMed]
- 3.Van Praagh S, Porras D, Oppido G, Geva T, Van Praagh R. Cleft mitral valve without ostium primum defect: anatomic data and surgical considerations based on 41 cases. Ann Thorac Surg 2003;75(6):1752–62. [DOI] [PubMed]
- 4.McDonald RW, Ott GY, Pantely GA. Cleft in the anterior and posterior leaflet of the mitral valve: a rare anomaly. J Am Soc Echocardiogr 1994;7(4):422–4. [DOI] [PubMed]
- 5.Sulafa AK, Tamimi O, Najm HK, Godman MJ. Echocardiographic differentiation of atrioventricular septal defects from inlet ventricular septal defects and mitral valve clefts. Am J Cardiol 2005;95(5):607–10. [DOI] [PubMed]
- 6.Kohl T, Silverman NH. Comparison of cleft and papillary muscle position in cleft mitral valve and atrioventricular septal defect. Am J Cardiol 1996;77(2):164–9. [DOI] [PubMed]
- 7.Perier P, Clausnizer B. Isolated cleft mitral valve: valve reconstruction techniques. Ann Thorac Surg 1995;59(1):56–9. [DOI] [PubMed]
- 8.Tamura M, Menahem S, Brizard C. Clinical features and management of isolated cleft mitral valve in childhood. J Am Coll Cardiol 2000;35(3):764–70. [DOI] [PubMed]
- 9.Kuperstein R, Feinberg MS, Carasso S, Gilman S, Dror Z, Di Segni E. The added value of real-time 3-dimensional echocardiography in the diagnosis of isolated cleft mitral valve in adults. J Am Soc Echocardiogr 2006;19(6):811–4. [DOI] [PubMed]