Abstract
Background
Women with a BRCA1 or BRCA2 genetic mutation have several options for cancer prevention, including prophylactic surgery, chemoprevention and screening. In this study we report on preventive practices used by women with and without breast cancer and examine differences in their selection of preventive practices according to geographic area in Canada.
Methods
Canadian women with a BRCA1 or BRCA2 mutation were followed after genetic testing and questioned about their preventive practices. Women reported on uptake of prophylactic mastectomy, prophylactic oophorectomy, tamoxifen or raloxifene usage and screening practices. We analyzed the uptake of each preventive option and completed a subanalysis according to the geographic area in Canada where genetic testing was provided.
Results
The study included 672 women. Follow-up questionnaires were completed after a mean of 4.0 years (range 1.6–9.1 years). Of the 342 women without breast cancer, 72 (21%) had had a prophylactic bilateral mastectomy. Three hundred and sixty-three women (54%) had had a bilateral prophylactic oophorectomy. Seventeen (6%) of the 270 women without breast cancer who had not had a prophylactic mastectomy took tamoxifen, and 12 (4%) reported taking raloxifene. Of the 342 women without breast cancer, 157 (46%) had not undertaken any cancer prevention option (mastectomy, oophorectomy or treatment with tamoxifen or raloxifene). Sixty-five (39%) of the 167 women from Ontario, 19 (34%) of the 56 women from Western Canada and 73 (62%) of the 119 women from Quebec had not undertaken any preventive procedure.
Conclusion
Significant differences in the uptake of preventive options by women with a BRCA1 or BRCA2 mutation were observed across 3 regions of Canada. Future research is needed to explain why these differences exist.
Introduction
Women with a BRCA1 or BRCA2 genetic mutation have a lifetime risk of breast cancer of between 45% and 87%1, 2. By identifying women at high risk of cancer and by adopting appropriate intervention strategies, it is anticipated that cases of cancer will be prevented. Ultimately, the value of genetic testing for the BRCA1 and BRCA2 mutations depends on the uptake of effective cancer prevention options. The preventive options that are available have varying levels of effectiveness.
Prophylactic mastectomy offers the greatest reduction in breast cancer risk (approximately 95%).3 Prophylactic oophorectomy before 40 years of age in women with a BRCA1 or BRCA2 mutation is associated with a 50% reduction in the risk of breast cancer.4 Tamoxifen usage has been shown to reduce breast cancer risk by 50% in women at high risk of the disease.5 The evidence in favour of tamoxifen usage for primary prevention in carriers of the BRCA1 and BRCA2 mutations is based on the prevention of contralateral breast cancer.6
Some women prefer screening over preventive surgery or chemoprevention. Screening does not prevent breast cancer; the goal is to detect cancer at an early, treatable stage. The superiority of magnetic resonance imaging (MRI) over mammography in detecting small breast cancers in BRCA1 and BRCA2 mutation carriers is becoming evident.7-9
There has been limited previous research examining uptake rates of various preventive options among BRCA1 and BRCA2 carriers. However, there are suggestions that the uptake of preventive procedures differs significantly according to country.10-14 Such differences are likely due to many factors, including patient preferences, physician preferences and access to care. In this study we present data on a Canadian cohort of BRCA1 and BRCA2 carriers who were followed systematically from the time at which they underwent genetic testing. We report on the preventive practices of women with and without breast cancer and examine differences in uptake rates according to geographic area within Canada.
Methods
Study population
Eligible subjects were drawn from a database of carriers of deleterious mutations in either the BRCA1 or the BRCA2 gene. These women had been assessed for genetic risk at 12 Canadian centres between 1995 and 2003. All study subjects provided written informed consent for genetic testing. The study was approved by the ethics committees of all participating centres. In most cases, testing was initially offered to women who had either breast or ovarian cancer. When a mutation in either the BRCA1 or BRCA2 gene was found in a proband or in one of her relatives, testing was offered to other at-risk women in her family. However, in some cases (fewer than 10% of the total) a woman with breast cancer in the family was not available for study and a woman who had not had the disease was the first member of the family to be tested. Mutation detection was performed using a range of techniques, but in every case nucleotide sequences were confirmed with direct sequencing of genomic DNA. A woman was eligible for the study when the molecular analysis established that she was a mutation carrier. We studied both women who had had breast cancer and those who had not.
Women were eligible for this study if they were a resident of Canada and had received their genetic testing at a Canadian genetics centre, were known to be a BRCA1 or BRCA2 mutation carrier, were between 25 and 80 years old, and had no previous history of cancer other than breast cancer. Women who were diagnosed with breast cancer during the follow-up period were excluded from the study. In addition, to be included, the women had to have had at least 18 months of follow-up after genetic testing and had to be alive at the date of follow-up.
Women were grouped according to geographic area. Women who received genetic testing in Vancouver (n = 67), Edmonton (n = 20), Saskatoon (n = 8) and Winnipeg (n = 15) were classified as being from Western Canada. Women from Ontario received genetic testing and counselling at 3 centres in Toronto (n = 229), at a centre in London (n = 56) or at a centre in Hamilton (n = 30). Women from Quebec received genetic testing and counseling at 2 centres (n = 247).
Procedures
All subjects completed a baseline questionnaire at the time of genetic testing that assessed cancer history and past use of cancer prevention options and screening tests. Follow-up questionnaires were administered by telephone or by mail. Questions assessed uptake of cancer prevention options, including prophylactic surgery (mastectomy or oophorectomy), chemoprevention (usage of tamoxifen or raloxifene) and MRI of the breast.
Statistical analysis
Chi-square testing was used to compare frequencies of categorical variables, such as different preventive options among regions, and ANOVA was used to compare mean values of continuous variables among regions. All statistical tests were conducted using SAS version 9.1.3 (SAS Institute, Inc., Cary, NC).
Results
We identified 1051 women with a BRCA1 or BRCA2 mutation for this study. Of these, 328 women were ineligible (12 women were less than 25 years of age, 10 women were over 80 years of age, 105 women were deceased at follow-up, 111 women had ovarian cancer, 15 women were followed for less than 18 months, 52 women were diagnosed with breast cancer during the follow-up period and 23 women lived outside of Canada), 29 women refused to complete the follow-up questionnaire and 22 women were lost to follow-up. A total of 672 women were included in the study. Follow-up questionnaires were completed a mean of 4.0 years after genetic testing (range 1.6–9.0 years). Genetic testing and counselling was received by 110 women in Western Canada (from 4 centres), 315 women in Ontario (from 5 centres) and 247 women in Quebec (from 2 centres). Three hundred and thirty women (49%) had had a previous diagnosis of breast cancer and 342 (51%) women had not. Characteristics of the study participants are presented in Table 1. There were no statistical differences in mean ages at the time of genetic testing according to geographic area (p = 0.39).
Table 1.
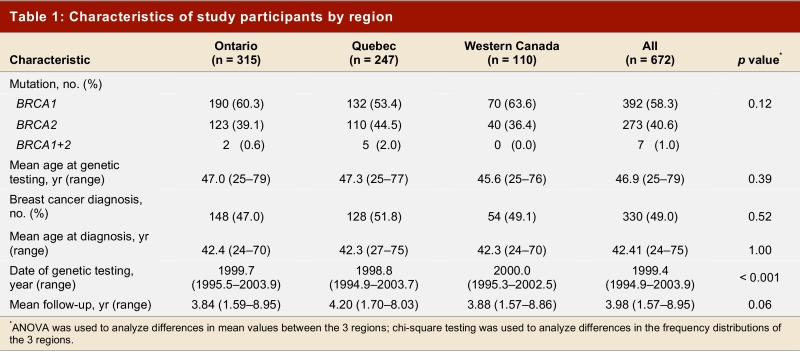
Characteristics of study participants by region
Prophylactic mastectomy
Of the 342 women without breast cancer, 72 (21%) had had a prophylactic bilateral mastectomy (Table 2). Fifty-three of these women (74%) had their surgery after receiving their genetic test result. The other 19 women (26%) had a prophylactic mastectomy before genetic testing, on the basis of their family history alone. All 72 prophylactic mastectomies were performed in women under age 60 (range 26–58 years). Table 3 presents uptake by geographic area.
Table 2.
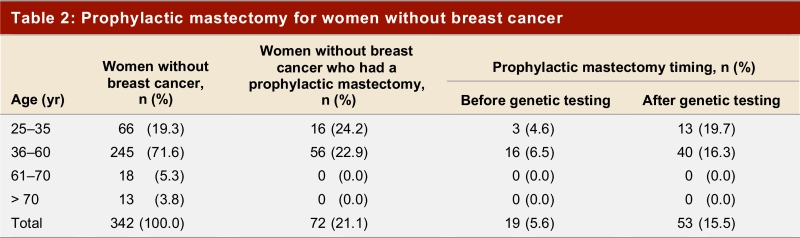
Prophylactic mastectomy for women without breast cancer
Table 3.
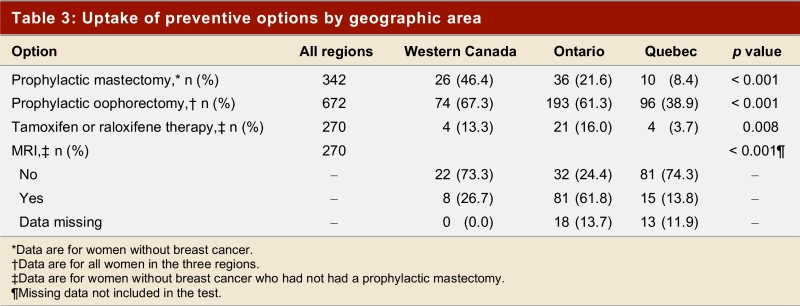
Uptake of preventive options by geographic area
Prophylactic oophorectomy
Three hundred and sixty-three women (54%) had bilateral prophylactic oophorectomy; of these, 215 (59%) had the surgery after receiving their genetic test result (Table 4). We were not able to distinguish between oophorectomies that were done for cancer prophylaxis and those done for other reasons. More women with a history of breast cancer had had a prophylactic oophorectomy (60%) than women without breast cancer (48%)(p = 0.002). Table 3 presents uptake by geographic area.
Table 4.
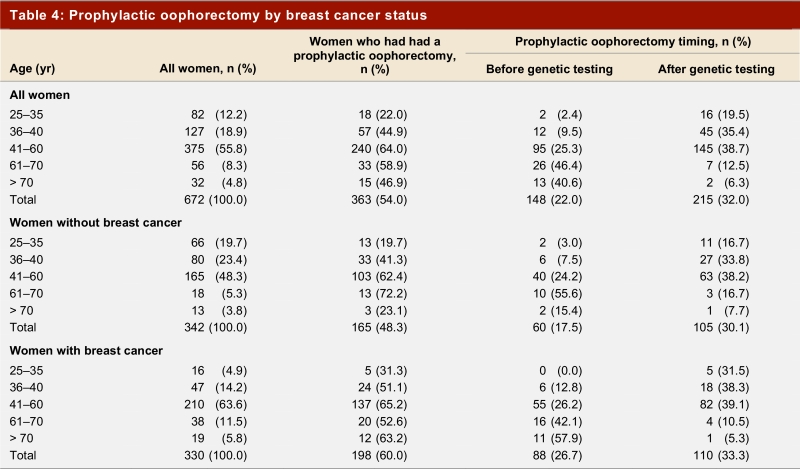
Prophylactic oophorectomy by breast cancer status
Tamoxifen and raloxifene usage
Usage of tamoxifen and raloxifene was examined for women without breast cancer but with both breasts intact (i.e., no prophylactic mastectomy). Seventeen women (6%) took tamoxifen and 12 women (4%) reported having taken raloxifene (Table 5). It is unknown if any of the women took tamoxifen or raloxifene as part of a clinical trial. Table 3 presents uptake by geographic region.
Table 5.
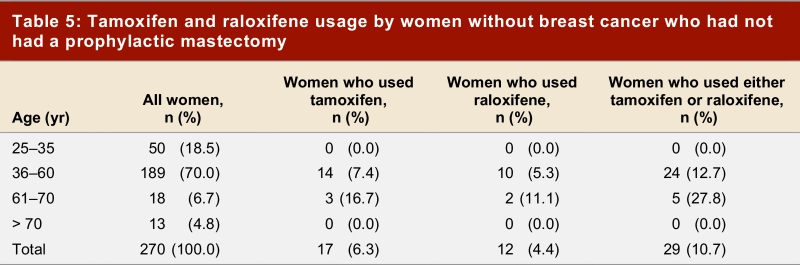
Tamoxifen and raloxifene usage by women without breast cancer who had not had a prophylactic mastectomy
No preventive option
Of the study participants without breast cancer, 157 (46%) had chosen no cancer prevention option (mastectomy, oophorectomy or treatment with tamoxifen or raloxifene). Thirty-nine percent of the women from Ontario (65 of 167), 34% of those from Western Canada (19 of 56), and 62% of those from Quebec (73 of 119) had not undertaken any preventive procedure.
MRI and mammography
Data on uptake of MRI were available for 241 of the 270 women without breast cancer who had not had a prophylactic bilateral mastectomy. One hundred and four women (43%) had been screened for breast cancer with MRI. One hundred of these women (96%) were less than 60 years old. Table 3 presents uptake by geographic area.
In contrast, the majority of women without breast cancer had undergone mammography (96%, 328 of 342). Most of these women (86%, 282 of 328) began mammography screening before genetic testing; however, 14% of the women had had their first mammogram after receiving their genetic test result. Uptake rates were similar across the 3 geographic areas: 99% of the women from Ontario (165 of 167), 93% of the women from Western Canada (52 of 56) and 93% of the women from Quebec (11 of 119) reported undergoing mammography.
Interpretation
We have reported on the rates of uptake of various cancer prevention options among Canadian women with a BRCA1 or BRCA2 mutation. Approximately two-thirds of women from Quebec had not taken up any preventive option, compared with approximately one-third of women from Western Canada and Ontario. The greatest differences in uptake rates were observed with prophylactic mastectomy. Women from Western Canada had the highest uptake of prophylactic mastectomy (46%), followed by women from Ontario (22%), and Quebec (8%). We also observed pronounced differences in rates of uptake of prophylactic oophorectomy. Sixty-seven percent of women from Western Canada and 61% of women from Ontario had undergone preventive oophorectomy. Again, fewer women from Quebec elected to have this preventive surgery (39%). Overall, the uptake rates of various preventive modalities were similar to those reported in other countries.[11,12,14–18] The surprising result was the great difference in uptake of preventive options depending on where a woman received her genetic counselling and testing.
Our results, and those of others, suggest that there are wide variations in the uptake of preventive options among BRCA1 and BRCA2 mutation carriers. The differences in uptake could be due to a number of factors, including health care professionals’ acceptance and recommendation of the procedures, cultural differences that influence patient preferences, and access (including cost and availability).
Health care professionals’ acceptance and recommendations clearly influence uptake. There is evidence that physicians have differing opinions on the various preventive options available to women with a BRCA1 or BRCA2 mutation. In the United States, a greater proportion of plastic surgeons (84.6%) than general surgeons (47.0%) or gynecologists (38.3%) in Maryland agreed that bilateral prophylactic mastectomy has a role in the care of women at high risk of developing breast cancer.19 In France, only 11% of physicians found it acceptable to propose prophylactic mastectomy to women with a BRCA mutation.20 Peshkin and colleagues surveyed physicians regarding recommendations for tamoxifen for primary breast cancer prevention and reported that physicians were more likely to recommend tamoxifen to BRCA2 carriers (73%) than to BRCA1 carriers (57%)(p < 0.0001).21 They concluded that physicians were not convinced of the benefits of tamoxifen in BRCA1 and BRCA2 mutation carriers. Although this research did not examine women’s uptake of preventive options with respect to their physician’s preference, it is expected that physicians would influence their patients’ choices.
Cultural influences may also be responsible for some of the discrepancies that we observed. Other authors have examined the differences in uptake of preventive options in various countries. Bouchard and colleagues surveyed women from Canada (Quebec), France and Great Britain about their medical decisions related to BRCA1 and BRCA2 mutation testing and found differences in the uptake of preventive procedures in the 3 countries, which they attributed to cultural differences.22 Previous single-country follow-up studies of BRCA1 and BRCA2 mutation carriers have reported various rates of uptake of all of the preventive options.11, 12, 14-18 When the single-country uptake rates are compared across countries, noticeable differences in uptake are observed. This suggests that variations between countries could be due to cultural influences.
Access to services may also contribute to the observed differences, particularly in the case of uptake of MRI screening. To date, screening MRI is offered on a research basis and is not widely available as a clinical service. Women with access to research studies are more likely to have MRI for screening. The differences in tamoxifen uptake may also be due to access issues, including cost. Currently, tamoxifen costs approximately $25 per month. Some women may not have drug coverage and therefore may not be able to afford this drug. The differences in surgical uptake that we observed are probably not due to differences in access across the country. Canadian women have coverage for prophylactic surgeries, including breast reconstruction, without cost. This would not be the case in the United States, where differences in uptake of preventive procedures have been attributed to financial constraints. For example, Schwartz and colleagues attributed the low rate of prophylactic oophorectomy they observed to the constrained financial resources of their study subjects.23
Study limitations
The study participants were women who had been found to carry a BRCA1 or BRCA2 mutation at one of 12 specialized genetic counseling centres in Canada between 1995 and 2003. Although ours is a relatively large sample (672 women), it may not be representative of all women who have received a positive genetic test result in Canada. Canadian women may have undergone genetic testing in centres other than the ones included here and we do not have any information on their uptake of cancer prevention options. Patterns of practice have evolved since 1999, the average time at which our study subjects received their genetic testing. We believe that genetic services are now better integrated with surgical care and that physician attitudes may have changed with regard to specific preventive measures. It is our intention to repeat this survey in 5 years to evaluate trends in clinical practice.
We have described the significant differences in uptake of preventive options by women with a BRCA1 or BRCA2 mutation who have received genetic testing in different areas of one country. The differences cannot be explained by differing health care systems because Canada has a universal health care system: all of the women in this study had similar access to health care (with the exception of MRI), and therefore no woman would be denied any of the preventive procedures because of lack of health insurance. We have speculated that the differences exist because of health care professionals’ acceptance and recommendation of the preventive procedures; cultural differences across Canada; and access (including cost and availability). In this study we could not ascertain the specific reason for the discrepancies across Canada, but future research will address this important question.
Biographies
Kelly A. Metcalfe is an assistant professor at the Lawrence S. Bloomberg Faculty of Nursing, University of Toronto, Toronto, Ont., and an adjunct scientist at Women’s College Research Institute, Toronto, Ont.
Parviz Ghadirian is an epidemiologist at the Epidemiology Research Unit, Centre hospitalier de l’Université de Montréal, Hôtel-Dieu, Université de Montréal, Montréal, Que.
Barry Rosen is a gynecologic oncologist in the Division of Gynecologic Oncology, Princess Margaret Hospital and University of Toronto, Toronto, Ont.
William Foulkes is a cancer geneticist with the Program in Cancer Genetics, Department of Oncology and Human Genetics, McGill University, Montréal, Que.
Charmaine Kim-Sing is a medical oncologist at the BC Cancer Agency, Vancouver, BC.
Andrea Eisen is a medical oncologist at the Toronto Sunnybrook Regional Cancer Centre, Toronto, Ont.
Peter Ainsworth is a geneticist at the London Health Sciences Centre, University of Western Ontario, London, Ont.
Doug Horsman is a cytogeneticist at the BC Cancer Agency, Vancouver, BC.
Christine Maugard is a clinical geneticist at Hôpital Notre-Dame, Montréal, QC.
Diane Provencher is a gynecologic oncologist at Hôpital Notre-Dame, Montréal, QC.
André Robidoux is a surgeon at the Epidemiology Research Unit, Centre hospitalier de l’Université de Montréal, Hôtel-Dieu, Université de Montréal, Montréal, Que.
Dawna Gilchrist is a clinical geneticist in the Departments of Medicine and Medical Genetics, University of Alberta, Edmonton, Alta.
Albert Chudley is a clinical geneticist at the Children’s Hospital, University of Manitoba, Winnipeg, Man.
Edmond G. Lemire is a clinical geneticist in the Division of Medical Genetics, Department of Pediatrics, University of Saskatchewan, Saskatoon, Sask.
Susan Armel is a genetic counsellor in the Division of Gynecologic Oncology, Princess Margaret Hospital and University of Toronto, Toronto, Ont.
Amy Finch is a genetic counsellor in the Division of Gynecologic Oncology, Princess Margaret Hospital and University of Toronto, Toronto, Ont.
Ping Sun is a statistician at the Women’s College Research Institute, Toronto, Ont.
Steven A. Narod is a geneticist at the Women’s College Research Institute, Toronto, Ont.
Footnotes
Competing interests: None declared.
References
- 1.Ford D, Easton D F, Stratton M, Narod S, Goldgar D, Devilee P, Bishop D T, Weber B, Lenoir G, Chang-Claude J, Sobol H, Teare M D, Struewing J, Arason A, Scherneck S, Peto J, Rebbeck T R, Tonin P, Neuhausen S, Barkardottir R, Eyfjord J, Lynch H, Ponder B A, Gayther S A, Zelada-Hedman M. Genetic heterogeneity and penetrance analysis of the BRCA1 and BRCA2 genes in breast cancer families. The Breast Cancer Linkage Consortium. Am J Hum Genet. 1998 Mar;62(3):676–689. doi: 10.1086/301749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Antoniou A, Pharoah P D P, Narod S, Risch H A, Eyfjord J E, Hopper J L, Loman N, Olsson H, Johannsson O, Borg A, Pasini B, Radice P, Manoukian S, Eccles D M, Tang N, Olah E, Anton-Culver H, Warner E, Lubinski J, Gronwald J, Gorski B, Tulinius H, Thorlacius S, Eerola H, Nevanlinna H, Syrjäkoski K, Kallioniemi O-P, Thompson D, Evans C, Peto J, Lalloo F, Evans D G, Easton D F. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case Series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet. 2003 May;72(5):1117–1130. doi: 10.1086/375033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hartmann L C, Sellers T A, Schaid D J, Frank T S, Soderberg C L, Sitta D L, Frost M H, Grant C S, Donohue J H, Woods J E, McDonnell S K, Vockley C W, Deffenbaugh A, Couch F J, Jenkins R B. Efficacy of bilateral prophylactic mastectomy in BRCA1 and BRCA2 gene mutation carriers. J Natl Cancer Inst. 2001 Nov 7;93(21):1633–1637. doi: 10.1093/jnci/93.21.1633. [DOI] [PubMed] [Google Scholar]
- 4.Eisen Andrea, Lubinski Jan, Klijn Jan, Moller Pal, Lynch Henry T, Offit Kenneth, Weber Barbara, Rebbeck Tim, Neuhausen Susan L, Ghadirian Parviz, Foulkes William D, Gershoni-Baruch Ruth, Friedman Eitan, Rennert Gadi, Wagner Teresa, Isaacs Claudine, Kim-Sing Charmaine, Ainsworth Peter, Sun Ping, Narod Steven A. Breast cancer risk following bilateral oophorectomy in BRCA1 and BRCA2 mutation carriers: an international case-control study. J Clin Oncol. 2005 Oct 20;23(30):7491–7496. doi: 10.1200/JCO.2004.00.7138. [DOI] [PubMed] [Google Scholar]
- 5.Fisher B, Costantino J P, Wickerham D L, Redmond C K, Kavanah M, Cronin W M, Vogel V, Robidoux A, Dimitrov N, Atkins J, Daly M, Wieand S, Tan-Chiu E, Ford L, Wolmark N. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998 Sep 16;90(18):1371–1388. doi: 10.1093/jnci/90.18.1371. [DOI] [PubMed] [Google Scholar]
- 6.Metcalfe Kelly, Lynch Henry T, Ghadirian Parviz, Tung Nadine, Olivotto Ivo, Warner Ellen, Olopade Olufunmilayo I, Eisen Andrea, Weber Barbara, McLennan Jane, Sun Ping, Foulkes William D, Narod Steven A. Contralateral breast cancer in BRCA1 and BRCA2 mutation carriers. J Clin Oncol. 2004 Jun 15;22(12):2328–2335. doi: 10.1200/JCO.2004.04.033. [DOI] [PubMed] [Google Scholar]
- 7.Warner Ellen, Plewes Donald B, Hill Kimberley A, Causer Petrina A, Zubovits Judit T, Jong Roberta A, Cutrara Margaret R, DeBoer Gerrit, Yaffe Martin J, Messner Sandra J, Meschino Wendy S, Piron Cameron A, Narod Steven A. Surveillance of BRCA1 and BRCA2 mutation carriers with magnetic resonance imaging, ultrasound, mammography, and clinical breast examination. JAMA. 2004 Sep 15;292(11):1317–1325. doi: 10.1001/jama.292.11.1317. [DOI] [PubMed] [Google Scholar]
- 8.Kriege Mieke, Brekelmans Cecile T M, Boetes Carla, Besnard Peter E, Zonderland Harmine M, Obdeijn Inge Marie, Manoliu Radu A, Kok Theo, Peterse Hans, Tilanus-Linthorst Madeleine M A, Muller Sara H, Meijer Sybren, Oosterwijk Jan C, Beex Louk V A M, Tollenaar Rob A E M, de Koning Harry J, Rutgers Emiel J T, Klijn Jan G M. Efficacy of MRI and mammography for breast-cancer screening in women with a familial or genetic predisposition. N Engl J Med. 2004 Jul 29;351(5):427–437. doi: 10.1056/NEJMoa031759. [DOI] [PubMed] [Google Scholar]
- 9.Tilanus-Linthorst Madeleine M, Obdeijn Inge-Marie, Bartels Karina C M. MARIBS study. Lancet. 2005;366(9482):291–292. doi: 10.1016/S0140-6736(05)66980-2. [DOI] [PubMed] [Google Scholar]
- 10.Lynch H T, Lemon S J, Durham C, Tinley S T, Connolly C, Lynch J F, Surdam J, Orinion E, Slominski-Caster S, Watson P, Lerman C, Tonin P, Lenoir G, Serova O, Narod S. A descriptive study of BRCA1 testing and reactions to disclosure of test results. Cancer. 1997 Jun 1;79(11):2219–2228. doi: 10.1002/(SICI)1097-0142(19970601)79:11<2219::AID-CNCR21>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 11.Metcalfe K A, Liede A, Hoodfar E, Scott A, Foulkes W D, Narod S A. An evaluation of needs of female BRCA1 and BRCA2 carriers undergoing genetic counselling. J Med Genet. 2000 Nov;37(11):866–874. doi: 10.1136/jmg.37.11.866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lodder Litanja N, Frets Petra G, Trijsburg R Willem, Meijers-Heijboer E Johanna, Klijn Jan G M, Seynaeve Caroline, van Geel Albertus N, Tilanus Madeleine M A, Bartels Carina C M, Verhoog Leon C, Brekelmans Cecile T M, Burger Curt W, Niermeijer Martinus F. One year follow-up of women opting for presymptomatic testing for BRCA1 and BRCA2: emotional impact of the test outcome and decisions on risk management (surveillance or prophylactic surgery). Breast Cancer Res Treat. 2002 May;73(2):97–9112. doi: 10.1023/A:1015269620265. [DOI] [PubMed] [Google Scholar]
- 13.Wagner T M, Möslinger R, Langbauer G, Ahner R, Fleischmann E, Auterith A, Friedmann A, Helbich T, Zielinski C, Pittermann E, Seifert M, Oefner P. Attitude towards prophylactic surgery and effects of genetic counselling in families with BRCA mutations. Austrian Hereditary Breast and Ovarian Cancer Group. Br J Cancer. 2000 Apr;82(7):1249–1253. doi: 10.1054/bjoc.1999.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lerman C, Hughes C, Croyle R T, Main D, Durham C, Snyder C, Bonney A, Lynch J F, Narod S A, Lynch H T. Prophylactic surgery decisions and surveillance practices one year following BRCA1/2 testing. Prev Med. 2000 Jul;31(1):75–80. doi: 10.1006/pmed.2000.0684. [DOI] [PubMed] [Google Scholar]
- 15.Botkin JR, Smith KR, Croyle RT, Baty BJ, Wylie JE, Dutson D. Genetic testing for a BRCA1 mutation: prophylactic surgery and screening behavior in women 2 years post testing. Am J Med Genet. 2003;118A(3):201–9. doi: 10.1002/ajmg.a.10102. [DOI] [PubMed] [Google Scholar]
- 16.Metcalfe Kelly A, Snyder Carrie, Seidel Jennifer, Hanna Danielle, Lynch Henry T, Narod Steven. The use of preventive measures among healthy women who carry a BRCA1 or BRCA2 mutation. Fam Cancer. 2005;4(2):97–9103. doi: 10.1007/s10689-005-4215-3. [DOI] [PubMed] [Google Scholar]
- 17.Meijers-Heijboer E J, Verhoog L C, Brekelmans C T, Seynaeve C, Tilanus-Linthorst M M, Wagner A, Dukel L, Devilee P, van den Ouweland A M, van Geel A N, Klijn J G. Presymptomatic DNA testing and prophylactic surgery in families with a BRCA1 or BRCA2 mutation. Lancet. 2000 Jun 10;355(9220):2015–2020. doi: 10.1016/S0140-6736(00)02347-3. [DOI] [PubMed] [Google Scholar]
- 18.Phillips K-A, Jenkins M A, Lindeman G J, McLachlan S A, McKinley J M, Weideman P C, Hopper J L, Friedlander M L. Risk-reducing surgery, screening and chemoprevention practices of BRCA1 and BRCA2 mutation carriers: a prospective cohort study. Clin Genet. 2006 Sep;70(3):198–206. doi: 10.1111/j.1399-0004.2006.00665.x. [DOI] [PubMed] [Google Scholar]
- 19.Houn F, Helzlsouer K J, Friedman N B, Stefanek M E. The practice of prophylactic mastectomy: a survey of Maryland surgeons. Am J Public Health. 1995 Jun;85(6):801–805. doi: 10.2105/ajph.85.6.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Julian-Reynier C, Eisinger F, Moatti J P, Sobol H. Physicians' attitudes towards mammography and prophylactic surgery for hereditary breast/ovarian cancer risk and subsequently published guidelines. Eur J Hum Genet. 2000 Mar;8(3):204–208. doi: 10.1038/sj.ejhg.5200418. [DOI] [PubMed] [Google Scholar]
- 21.Peshkin Beth N, Isaacs Claudine, Finch Clinton, Kent Sheryl, Schwartz Marc D. Tamoxifen as chemoprevention in BRCA1 and BRCA2 mutation carriers with breast cancer: a pilot survey of physicians. J Clin Oncol. 2003 Dec 1;21(23):4322–4328. doi: 10.1200/JCO.2003.02.107. [DOI] [PubMed] [Google Scholar]
- 22.Bouchard Louise, Blancquaert I, Eisinger F, Foulkes W D, Evans G, Sobol H, Julian-Reynier C. Prevention and genetic testing for breast cancer: variations in medical decisions. Soc Sci Med. 2004 Mar;58(6):1085–1096. doi: 10.1016/S0277-9536(03)00263-6. [DOI] [PubMed] [Google Scholar]
- 23.Schwartz Marc D, Kaufman Elizabeth, Peshkin Beth N, Isaacs Claudine, Hughes Chanita, DeMarco Tiffani, Finch Clinton, Lerman Caryn. Bilateral prophylactic oophorectomy and ovarian cancer screening following BRCA1/BRCA2 mutation testing. J Clin Oncol. 2003 Nov 1;21(21):4034–4041. doi: 10.1200/JCO.2003.01.088. [DOI] [PubMed] [Google Scholar]


