Abstract
Background
Intimate partner violence against women is prevalent and is associated with poor health outcomes. Understanding indicators of exposure to intimate partner violence can assist health care professionals to identify and respond to abused women. This study was undertaken to determine the strength of association between selected evidence-based risk indicators and exposure to intimate partner violence.
Methods
In this cross-sectional study of 768 English-speaking women aged 18–64 years who presented to 2 emergency departments in Ontario, Canada, participants answered questions about risk indicators and completed the Composite Abuse Scale to determine their exposure to intimate partner violence in the past year.
Results
Intimate partner violence was significantly associated with being separated, in a common-law relationship or single (odds ratio [OR] = 2.08, 95% confidence interval [CI] 1.17–3.71); scoring positive for depression (OR = 4.26, 95% CI 2.11–8.60) or somatic symptoms (OR = 4.09, 95% CI 2.18–7.67); having a male partner who was employed less than part time (OR = 5.12, 95% CI 2.46–10.64), or having a partner with an alcohol (OR = 4.36, 95% CI 2.16–8.81) or drug problem (OR = 4.63, 95% CI 1.89–11.38). Each unit increase in the number of indicators corresponded to a four-fold increase in the risk of intimate partner violence (OR = 3.92, 95% CI 3.06–5.02); women with 3 or more indicators had a greater than 50% probability of a positive score on the Composite Abuse Scale. Intimate partner violence was not associated with pregnancy status.
Conclusion
Specific characteristics of male partners, relationships and women’s mental health are significantly related to exposure to intimate partner violence in the past year. Identification of these indicators has implications for the clinical care of women who present to health care settings.
Introduction
Despite its identification over a decade ago as a serious public health problem,1 statistics on the prevalence,2-4 consequences5-8 and costs9-11 of intimate partner violence (IPV) against women attest to its persistent and devastating impact on families and society today. As many as 37% of women who present to emergency departments (EDs) in the United States report having been victims of emotional or physical abuse at some point during their lives; 2.2% present with acute physical trauma resulting from partner abuse; and 14.4% report abuse in the past year.12
The best approach to the identification, in health care settings, of women exposed to IPV remains unclear. Several recent systematic reviews,13-15 including one that examined the ED context,16 found no evidence for the effectiveness of IPV screening in improving outcomes for women. Two evidence-based practice guidelines have concluded that there is insufficient evidence to support routine screening for IPV, primarily because of the lack of evidence for effective IPV interventions to which women identified as abused can be referred.17, 18
The absence of evidence for the effectiveness of routine screening requires that clinicians be especially aware of the signs and symptoms of abuse to facilitate appropriate case identification of women experiencing violence who may wish to discuss the issue but may not self-disclose.19,20,21 Similarly, the absence of evidence for effective interventions puts an additional burden on clinicians to understand the woman’s context and develop a treatment or referral plan suited to her situation. Therefore, knowledge of the risk indicators for IPV can assist in the “diagnostic” or “case-finding” approach to identification of abused women.19,20,21
The purpose of this study was to examine the relationship between IPV and factors posited to correlate with IPV among female ED patients. For this study we selected risk indicators that could be assessed using information elicited during a routine patient interview; the selection was also based on the results of a systematic review of prior evidence22 and an unpublished meta-analysis of risk indicators for IPV (available from the authors).
Methods
Study setting, participants and procedures
The study was conducted from May 2004 to February 2005 (data were analyzed in January and February 2006). Participants were the subgroup of women from a larger trial23 that evaluated approaches to IPV screening who presented to 1 of 2 EDs in southwestern Ontario. The EDs were in communities of 15,000 (“town,” also serving a large rural area) and 122,000 (“city”) people and had 32,000 and 39,000 annual ED visits, respectively.
Sample size was determined by the requirements of the larger trial. All women who presented for care at each ED during the study period were invited to participate if they met the following criteria: 18 to 64 years old; at the ED for their own health care visit; able to be interviewed away from individuals accompanying them, including dependent children other than those less than 18 months old; able to speak and read English; not too ill to participate (as defined by a score of 3 to 5 (on a scale of 5) on the Canadian Emergency Department Triage and Acuity Scale (CTAS), that is “urgent,” “less urgent” and “non urgent”); and able to provide informed consent. For safety reasons no reference to abuse or violence was made until the women were taken to a private area where informed consent was obtained. Following informed consent, the women were asked to complete all of the measures described below.
Ethical and safety issues
All participants were advised before enrollment that the ED staff would not be informed of their responses to any of the questions asked but were available to discuss any concerns. The women were provided with information about resources in the community and were given the option to have shredded any study material that they felt might put them at risk. All women answered the risk indicator questions on paper forms provided by the study’s recruitment staff. According to the requirements of the larger trial, approximately two-thirds of the women were provided with the questions by the trial recruiter before being seen by the health care provider. Women who were randomly assigned, for the randomized trial, to the face-to-face screening condition answered the risk indicator and demographic questions after the clinical visit and before leaving the ED. Health care providers at each site were given specialized training in responding to IPV. Led by clinical experts in the field, the training included information on the causes and consequences of IPV and local resources to which providers could refer women (for the 2 settings discussed in the present report, this included on-site resources, such as a Sexual Assault Domestic Violence Care Centre, and community-based services, including advocacy agencies and shelters). The study was approved by the McMaster University / Hamilton Health Sciences Research Ethics Board and the research ethics committees of the participating hospitals.
Development of risk indicator questions
Indicators were selected according to the results of a systematic review22 and an unpublished meta-analysis conducted by the authors to assess the strength of association between risk indicators and abuse status. The likelihood that a given risk indicator could be assessed using information elicited during a routine patient interview was another factor in the selection process. The following indicators (described below) were selected for assessment: type of relationship; employment status of the male partner (women were asked the sex of their partner: 97.4% indicated that they had a male partner, resulting in too small a sample (n = 19) to make meaningful statements about risk indicators in same-sex relationships; therefore, the data are presented for female-male relationships only); current pregnancy status; alcohol or drug abuse by the partner; depressive and somatic symptoms in the woman; and specific demographic characteristics identified in the literature. The psychometric properties of the indicator questions are provided below where available; we do not have these data for the demographic and de novo questions (e.g., alcohol and drug use). Development of the questions was iterative and included input from pilot testing with IPV and questionnaire design experts and from women residing in a shelter for abused women and in the community. There were 12 parts to the questionnaire, the last 2 being scales for depression (9 items) and somatic complaints (15 items): in total, there were 34 items. Although we did not time the study participants, pilot testing with women indicated a mean completion time of 15 minutes (standard deviation = 5 minutes).
Measures
In addition to answering standard demographic questions, participants completed items on the following variables.
Type of relationship
A single question asked about type of relationship: single and never married; married; common-law (referring to 2 people of the same or opposite sex who live together but are not legally married); separated; divorced; or widowed. This variable was dichotomized as “separated or common-law or single” versus “divorced or married or widowed” according to the associations between these categories and IPV risk in this data set and based on previous literature indicating that recent separation is associated with stalking and other forms of harassment.
Male partner’s employment status
The woman was asked to describe her male partner’s employment status using 1 of 5 options: full-time job; part-time job; works once in a while, e.g., as a day labourer; unemployed in the last 6 months; or unemployed for more than 6 months. The category associated with risk for IPV was employment less than part-time (options other than full-time job or part-time job), and so categories were collapsed for subsequent analyses.
Male partner’s alcohol and drug use
Single-item, dichotomized (yes/no) questions were created for this study that asked each woman if her partner had, in her opinion or that of family, friends or professionals, an alcohol problem (1 question) or a drug problem (1 question).
Pregnancy
A single item asked if the respondent was pregnant (yes/no).
Depression
Depression was assessed using the self-report version of the depression subscale from the PRIME-MD Patient Health Questionnaire (PHQ-9),24 which has been extensively validated against clinician-administered approaches and has good psychometric properties (kappa = 0.65, sensitivity = 75%, specificity = 90%. accuracy = 85%).24 The PHQ-9 has 9 items that range in frequency from 0 (“not at all”) to 3 (“nearly every day”) with a range in total scores of 0 to 27. Scoring was performed according to the instruction manual, and this variable was dichotomized as “with symptoms of major depressive disorder” versus “without symptoms of major depressive disorder.”
Somatic symptoms
Somatization was assessed using the self-report version of the 15-item somatic complaints subscale from the PRIME-MD Patient Health Questionnaire (PHQ-15),25 a valid and reliable assessment tool (construct validity as assessed against 3 other somatic complaints instruments and Cronbach’s alpha >> 0.80 for reliability). The items were scored from 0 (“not bothered at all”) to 2 (“bothered a lot”), for a total score range of 0–30, with cut-off points for somatic symptom severity of < 5 (none or minimal), 5–9 (low), 10–14 (medium) and ≥ 15 (high).25 This variable was dichotomized as a score of ≥ 15 (high) versus 0–14 (low or moderate).
IPV exposure
The Composite Abuse Scale (CAS)26, 27 was completed by all women and served as the reference standard to assess abuse exposure. The CAS is a validated 30-item instrument developed for research purposes that assesses physical, sexual and emotional abuse, harassment and severe combined abuse. Women were asked to consider their exposure in the past 12 months to such items as “[My partner] slapped me”; “forced me to have sex”; “harassed me over the telephone”; “told me I wasn’t good enough.” The CAS has a total possible score of 150; each of the 30 items is measured according to frequency, from 0 (“never”) to 5 (“daily”). A CAS score of ≥ 7 was deemed positive for IPV.26
Women’s perceptions of the risk indicator questions
Women completed 8 questions about the experience of responding to the risk indicator questions, including the ease of understanding them, their emotional responses to them (anger, upset, discomfort), and whether the questions were embarrassing, offensive, too harsh or too personal. Questions were scaled 1 to 5, anchored by 1 (“not at all”) and 5 (“very”).
Statistical analysis
Analyses were run in SPSS version 11.0.1 (SPSS Inc., Chicago, Ill.). Descriptive statistics were determined for each variable of interest. Logistic regressions provided odds ratios (ORs) and 95% confidence intervals (CIs) for the bivariate relationships between each indicator and IPV exposure, and between the woman’s age (in years) and IPV, and the partner’s age (in years) and IPV. To determine whether risk indicators performed differently in the 2 settings, a term for site and a term for the interaction of site and the indicator variable were included in each regression. Indicators with significant bivariate associations with IPV exposure were entered into a multiple logistic regression. The positive and negative predictive values, sensitivity, specificity and efficiency of the risk indicators in predicting abuse status were also calculated.
Logistic regression was used to determine the relationship between the number of positive risk indicators and IPV status, as well as for combinations (interactions) of indicators specified a priori to be strongly associated with IPV status. These combinations, based on the literature, were as follows: partner alcohol problem plus partner underemployment; partner drug problem plus partner underemployment; and partner drug problem plus partner alcohol problem.
Results
Descriptive data
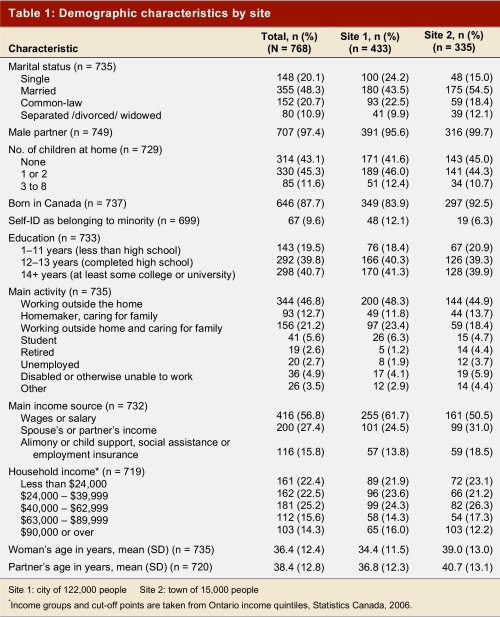
Of the 798 eligible women who entered the 2 EDs during the study period, 768 provided informed consent, for a refusal rate of 3.8%. Table 1 presents the demographic characteristics of the 768 women in the sample, overall and by site.
Table 1.
Demographic characteristics by site
Examination of demographic characteristics indicated some differences between sites. Women in the larger, urban ED were younger and less likely to be married. They were also more likely to self-identify as being a member of a minority group and to have been born outside Canada. Women in the more urban site were also more likely to work outside the home or be students and less likely to be homemakers, retired, unemployed or disabled. More women in the urban site relied on their own wages or salary and fewer on their partners’ income or other form of support or social assistance. Analysis by site revealed no statistically significant differences in the nondemographic risk indicators and no difference in IPV rates; therefore, subsequent inferential analyses were conducted on the grouped sample.
Presence of risk indicators and relationship with IPV status
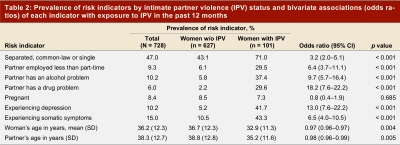
Of the 768 women who provided informed consent and were included in the sample, 40 women (5.2%) did not provide sufficient data on the CAS to allow a determination of their IPV status. These cases were excluded from the regression analyses, leaving 728 cases for these analyses. CAS scores indicated that 13.9% (101/728) of these women reported being exposed to IPV in the previous 12 months. Table 2 presents the percentage of women in the sample who were positive for each risk indicator, stratified by IPV status, and the bivariate associations between risk indicators and reports of IPV. Since no significant interactions between site and any indicator were found, simple bivariate associations are presented. Those women who reported IPV were significantly more likely to be separated, living in a common-law relationship or single, to have a male partner employed less than part time, to have a partner with an alcohol or drug problem, and to be experiencing depression or somatization. They were also significantly younger, as were their partners. Being pregnant was not significantly associated with IPV status.
Table 2.
Prevalence of risk indicators by intimate partner violence (IPV) status and bivariate associations (odds ratios) of each indicator with exposure to IPV in the past 12 months
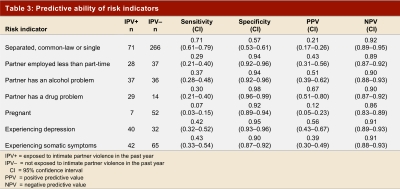
Table 3 presents the positive and negative predictive values, sensitivity, specificity and efficiency of the risk indicators as predictors of abuse status, singly and in groups. Although the absence of indicators is quite predictive of no abuse exposure (as seen in the specificity values of > 90% and the negative predictive values of > 86%), the sensitivity and positive predictive values are low to moderate. Generally, the questions are reasonably efficient in predicting abuse status, although this is driven by the negative predictive values.
Table 3.
Predictive ability of risk indicators
Overall relationship between risk indicators and IPV
In the full regression model (Table 4), with the exception of marital status and the 2 age variables, all indicators that were significantly related to IPV in the bivariate analyses remained so. Each indicator was associated with an OR of at least 4.0. Overall, the model accounts for 22% of the variance in IPV status. None of the hypothesized interaction effects was significant.
Table 4.
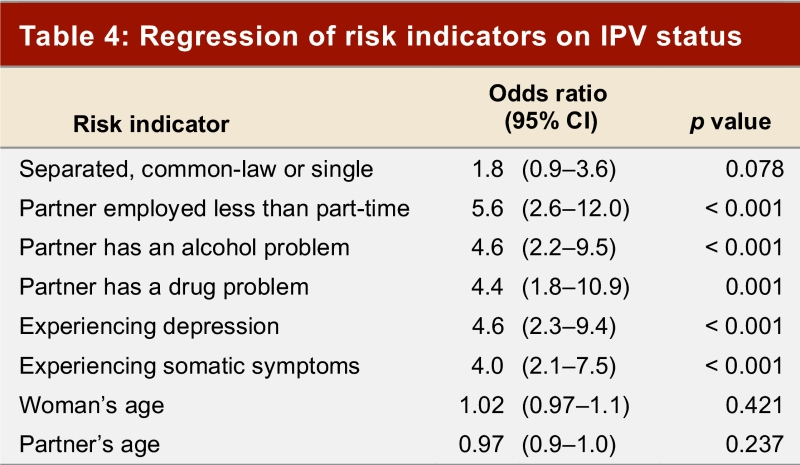
Regression of risk indicators on IPV status
Regarding the number of risk indicators, the majority of women had no (40.1%) or 1 (38.3%) indicator; 21.6% had 2 or more indicators; and 8.9% had 3 or more. The number of risk indicators present was significantly related to IPV status, with each unit increase in number of indicators corresponding to a nearly four-fold increase in IPV risk (OR = 3.92, 95% CI 3.06–5.02, p < 0.001). Figure 1 shows the receiver operating characteristic (ROC) curve describing the predictive value of the number of risk indicators; the area under the curve was 0.839 (95% CI 0.793–0.885, p < 0.001).
Figure 1.
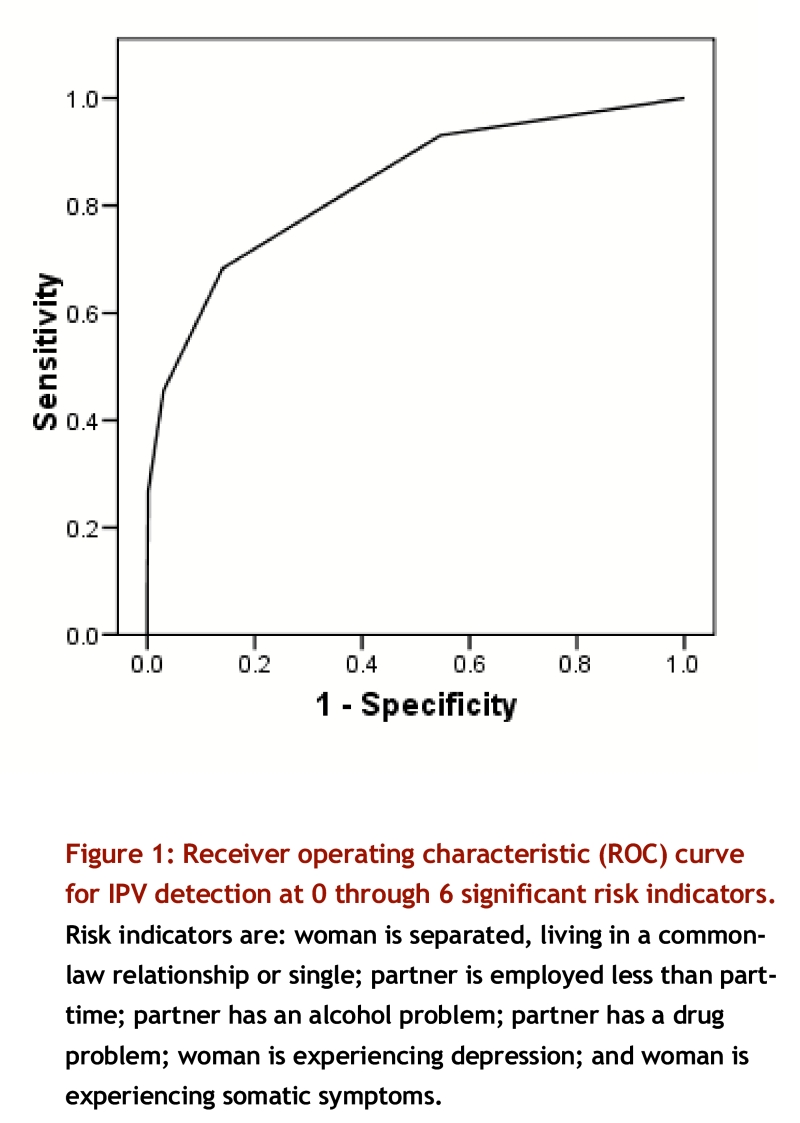
Receiver operating characteristic (ROC) curve for IPV detection at 0 through 6 significant risk indicators. Risk indicators are: woman is separated, living in a common-law relationship or single; partner is employed less than part-time; partner has an alcohol problem; partner has a drug problem; woman is experiencing depression; and woman is experiencing somatic symptoms
Evaluation of risk indicator questions by participants
Most women found the risk indicator questions acceptable. The percentage of women who indicated “not at all” to the items were as follows: hard to understand, 93.4; make you feel uncomfortable, 87.7; make you feel upset, 89.5; make you feel angry, 93.4; embarrassing, 90.1; offensive, 95.5; too harsh, 95.3; too personal, 88.8.
Discussion
The present study took a clinically oriented approach to examining the relationship between intimate partner violence and the specific characteristics of women, their partners and their relationships to provide information about the potential risk indicators for IPV that are both clinically relevant and detectable during history-taking and diagnostic assessment.
The annual prevalence rate of 13.9% in the present study included all forms of abuse by an intimate partner (physical, sexual and emotional/psychological), and falls within the range of annual rates reported in studies conducted in clinical samples in the United States and Canada,12, 28, 29 although the largest US study using an ED sample measured only physical and sexual abuse, finding a prevalence of 14.4%.12 In addition, the results regarding relationship and partner characteristics are consistent with existing data, including type of union30, 31 and the significant impact of the male partner’s alcohol or drug abuse30-36 and underemployment.33, 36 Finally, the significant bivariate association between both the woman’s age and IPV and the partner’s age and IPV is consistent with previous research,12, 30 women reporting IPV being significantly younger and having younger partners. However, these age variables, as well as the marital status variable, were not significant in the multivariate model, indicating that the significant bivariate relationships result from the correlation of these variables with other variables in the model. For example, younger women are more likely to have younger partners. Younger males are more likely to be aggressive and to perpetrate more severe violence30, 37 and are more likely to be underemployed.38
In terms of specific characteristics of women and their clinical utility in predicting IPV exposure, the 2 indicators of mental health are of particular interest. Recent guidelines suggest that screening adults for depression and linking the results to a diagnostic and treatment plan are effective in reducing depression and its health-related outcomes.39, 40 The present results and those of others5, 6 suggest that the presence of depression is an important risk indicator for IPV; therefore, any woman with suspected depression should be asked about IPV, as this could be a critical factor in determining treatment options. Similarly, the finding that 15% of the current sample scored “high” on the questions concerning somatic symptoms is of note. Of these women, 43% also reported IPV, a finding consistent with that of Glass and colleagues,41 who found that 20% of women disclosing in the ED physical or sexual abuse in the past year were presenting for pain-related, non-injury complaints. This finding suggests that women presenting with high levels of somatic symptoms should be asked about exposure to IPV; such inquiry has the potential to limit the need for additional diagnostic investigations.
Of particular note is the additive effect of risk indicators: for each additional indicator present, the woman’s odds of reporting IPV in the past year increased almost four-fold. More than 50% of the women with 3 indicators reported IPV in the past year, and this percentage approached 100% for women with 4–6 indicators, although the subsamples in the latter group were small. The data on the predictive value of multiple indicators provide further support for this observation: the presence of 4 or more indicators predicts abuse status with 96% accuracy.
The sole indicator that was not significantly associated with abuse was pregnancy, a finding consistent with the current literature. Although unintended pregnancy has been linked to abuse,42 most studies find either no significant difference in rates of abuse during the pre-, peri- and post-natal periods or a trend toward a decrease in abuse when a woman is pregnant.43,44,45 Abuse that occurs earlier in the time span between the pre- and post-natal periods (rather than the pregnancy itself) is by far the strongest predictor of abuse later in this time span; that is, pre-natal abuse predicts peri- and post-natal abuse, and peri-natal abuse predicts post-natal abuse.44 The potential consequences of abuse during pregnancy are, however, severe,46, 47 and clinicians should maintain a high degree of suspicion when pregnant women present with clinical indicators of abuse.
There were demographic differences between the two EDs from which participants were recruited, but because these differences were consistent with the urban versus semi-urban/rural characters of the 2 sites, the overall sample was representative of the broader population.48
Information not collected for this study, but that should be considered for future research, included whether the woman’s reason for presenting to the ED (chief complaint) was directly related to IPV and whether she was currently experiencing post-traumatic stress disorder. These data would be useful to help understand not only the relationships between and among the current set of indicators, IPV and post-traumatic stress disorder, but whether the visits to the ED by women disclosing abuse was directly or indirectly related to violence.
Clinical implications
In the absence of clear evidence about whether routine screening for IPV does more good than harm,14, 17, 18 awareness by health care providers of the types of indicators significantly associated with IPV can assist with assessing and responding appropriately to the patient (for example, being sensitive to the need to interview a woman away from any family members). Women in this study found the risk indicator questions to be acceptable and did not indicate concerns regarding being asked about violence. The relatively poor performance of the indicators as positive predictors of abuse, however, precludes recommending that these be used as a form of “risk-based screening”; rather, their utility lies in signaling to the clinician that violence may be a concern, especially when more than 1 risk indicator is present. There may be some conditions (such as depression) or symptoms (such as a high level of somatic complaints) for which identifying IPV exposure can assist with diagnosis and treatment. For example, developing a treatment plan for depression that includes antidepressants or cognitive behavior therapy or both without taking into account exposure to violence could reduce the effectiveness of the management strategy. Ultimately, these findings might serve as the basis for the derivation of a clinical prediction rule to be used by ED staff in the identification of IPV victims; however, additional research is needed to determine the right combination of indicators to ask about to improve the predictive value of this approach. An important yet unanswered question is, Once a woman is identified as a victim of violence, how can clinicians best care for her? This question remains a pressing research gap.
Biographies
C. Nadine Wathen, PhD, is an Assistant Professor in the Faculty of Information and Media Studies, The University of Western Ontario, London, Ont.
Ellen Jamieson, MEd, is a Research Associate in the Department of Psychiatry and Behavioural Neurosciences, McMaster University, Hamilton, Ont.
Margo Wilson, PhD, is a Professor in the Department of Psychology, McMaster University, Hamilton, Ont.
Martin Daly, PhD, is a Professor in the Department of Psychology, McMaster University, Hamilton, Ont.
Andrew Worster, MD, MSc, is an Associate Professor in the Department of Medicine, McMaster University, Hamilton, Ont.
Harriet L. MacMillan, MD, MSc, is a Professor in the Departments of Psychiatry and Behavioural Neurosciences and of Pediatrics, McMaster University, Hamilton, Ont.
Appendix 1.
Members of the McMaster University Violence Against Women Research Group
Footnotes
Competing interests: None declared.
Funding Source: This study was funded by the Ontario Women’s Health Council, Ontario Ministry of Health and Long-Term Care, as part of the McMaster University Violence Against Women Research Program. The sponsor had no role in study design, data collection or analysis, data interpretation or writing the manuscript. The authors are solely responsible for the design, implementation, interpretation and reporting of this study. Dr. Wathen held a Canadian Institutes of Health Research–Ontario Women’s Health Council Fellowship. Dr. MacMillan holds a Canadian Institutes of Health Research New Emerging Team Grant from the Institutes of Gender and Health; Aging; Human Development, Child and Youth Health; Neurosciences, Mental Health and Addiction; and Population and Public Health.
References
- 1.Violence against women: relevance for medical practitioners. JAMA. 1992;267(23):3184–9. [PubMed] [Google Scholar]
- 2.Tjaden P, Thoennes N. Full report of the prevalence, incidence and consequences of violence against women: research report. NCJ 183781. 2000. http://www.ncjrs.gov/pdffiles1/nij/183781.pdf. [Google Scholar]
- 3.Canadian Centre for Justice Statistics . Family violence in Canada: a statistical profile 2002. Cat no 85-224-XIE. 2002. http://www.statcan.ca/english/freepub/85-224-XIE/85-224-XIE00002.pdf. [Google Scholar]
- 4.Krug EG, Dahlberg LL, Mercy JA, et al., editors. Geneva (Switzerland): World Health Organization; 2002. World report on violence and health. http://www.who.int/violence_injury_prevention/violence/world_report/en/full_en.pdf. [DOI] [PubMed] [Google Scholar]
- 5.Campbell Jacquelyn, Jones Alison Snow, Dienemann Jacqueline, Kub Joan, Schollenberger Janet, O'Campo Patricia, Gielen Andrea Carlson, Wynne Clifford. Intimate partner violence and physical health consequences. Arch Intern Med. 2002 May 27;162(10):1157–1163. doi: 10.1001/archinte.162.10.1157. [DOI] [PubMed] [Google Scholar]
- 6.Golding JM. Intimate partner violence as a risk factor for mental disorders: a meta-analysis. J Fam Violence. 1999;14(2):99–132. [Google Scholar]
- 7.Cokkinides V E, Coker A L, Sanderson M, Addy C, Bethea L. Physical violence during pregnancy: maternal complications and birth outcomes. Obstet Gynecol. 1999 May;93(5 Pt 1):661–666. doi: 10.1016/S0029-7844(98)00486-4. [DOI] [PubMed] [Google Scholar]
- 8.Murphy C C, Schei B, Myhr T L, Du Mont J. Abuse: a risk factor for low birth weight? A systematic review and meta-analysis. CMAJ. 2001 May 29;164(11):1567–1572. [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention . 2003. [accessed 2007 Jul 24]. Costs of IPV against women in the United States. http://www.cdc.gov/ncipc/pub-res/ipv_cost/ipv.htm. [Google Scholar]
- 10.Ulrich Yvonne C, Cain Kevin C, Sugg Nancy K, Rivara Frederick P, Rubanowice David M, Thompson Robert S. Medical care utilization patterns in women with diagnosed domestic violence. Am J Prev Med. 2003 Jan;24(1):9–15. doi: 10.1016/S0749-3797(02)00577-9. [DOI] [PubMed] [Google Scholar]
- 11.Wisner C L, Gilmer T P, Saltzman L E, Zink T M. Intimate partner violence against women: do victims cost health plans more? J Fam Pract. 1999 Jun;48(6):439–443. [PubMed] [Google Scholar]
- 12.Dearwater S R, Coben J H, Campbell J C, Nah G, Glass N, McLoughlin E, Bekemeier B. Prevalence of intimate partner abuse in women treated at community hospital emergency departments. JAMA. 1998 Aug 5;280(5):433–438. doi: 10.1001/jama.280.5.433. [DOI] [PubMed] [Google Scholar]
- 13.Nelson Heidi D, Nygren Peggy, McInerney Yasmin, Klein Jonathan. Screening women and elderly adults for family and intimate partner violence: a review of the evidence for the U. S. Preventive Services Task Force. Ann Intern Med. 2004 Mar 2;140(5):387–396. doi: 10.7326/0003-4819-140-5-200403020-00015. [DOI] [PubMed] [Google Scholar]
- 14.Ramsay Jean, Richardson Jo, Carter Yvonne H, Davidson Leslie L, Feder Gene. Should health professionals screen women for domestic violence? Systematic review. BMJ. 2002 Aug 10;325(7359):314. doi: 10.1136/bmj.325.7359.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wathen C Nadine, MacMillan Harriet L. Interventions for violence against women: scientific review. JAMA. 2003 Feb 5;289(5):589–600. doi: 10.1001/jama.289.5.589. [DOI] [PubMed] [Google Scholar]
- 16.Anglin Deirdre, Sachs Carolyn. Preventive care in the emergency department: screening for domestic violence in the emergency department. Acad Emerg Med. 2003 Oct;10(10):1118–1127. doi: 10.1197/S1069-6563(03)00371-3. [DOI] [PubMed] [Google Scholar]
- 17.U.S. Preventive Services Task Force Screening for family and intimate partner violence: recommendation statement. Ann Intern Med. 2004;140(5):382–386. doi: 10.7326/0003-4819-140-5-200403020-00014. http://www.ncbi.nlm.nih.gov/entrez/utils/fref.fcgi?PrId=3051&itool=AbstractPlus-def&uid=14996680&db=pubmed&url=http://www.annals.org/cgi/pmidlookup?view=reprint&pmid=14996680. [DOI] [PubMed] [Google Scholar]
- 18.Wathen C Nadine, MacMillan Harriet L. Prevention of violence against women: recommendation statement from the Canadian Task Force on Preventive Health Care. CMAJ. 2003 Sep 16;169(6):582–584. [PMC free article] [PubMed] [Google Scholar]
- 19.Rhodes Karin V, Levinson Wendy. Interventions for intimate partner violence against women: clinical applications. JAMA. 2003 Feb 5;289(5):601–605. doi: 10.1001/jama.289.5.601. [DOI] [PubMed] [Google Scholar]
- 20.Ferris Lorraine E. Intimate partner violence. BMJ. 2004 Mar 13;328(7440):595–596. doi: 10.1136/bmj.328.7440.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.MacMillan Harriet L, Wathen C Nadine. Violence against women: integrating the evidence into clinical practice. CMAJ. 2003 Sep 16;169(6):570–571. [PMC free article] [PubMed] [Google Scholar]
- 22.MacMillan HL, Wathen CN. 2001. [accessed 2007 Jul 24]. Canadian Task Force on Preventive Health Care. Prevention and treatment of violence against women: systematic review and recommendations. http://www.ctfphc.org/Full_Text/CTF_DV_TR_final.pdf. [Google Scholar]
- 23.MacMillan Harriet L, Wathen C Nadine, Jamieson Ellen, Boyle Michael, McNutt Louise-Anne, Worster Andrew, Lent Barbara, Webb Michelle. Approaches to screening for intimate partner violence in health care settings: a randomized trial. JAMA. 2006 Aug 2;296(5):530–536. doi: 10.1001/jama.296.5.530. [DOI] [PubMed] [Google Scholar]
- 24.Spitzer R L, Kroenke K, Williams J B. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999 Nov 10;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 25.Kroenke Kurt, Spitzer Robert L, Williams Janet B W. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64(2):258–266. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Hegarty K, Sheehan M, Schonfeld C. A multidimensional definition of partner abuse: development and preliminary validation of the Composite Abuse Scale. J Fam Violence. 1999;14(4):399–415. [Google Scholar]
- 27.Hegarty Kelsey, Fracgp, Bush Robert, Sheehan Mary. The composite abuse scale: further development and assessment of reliability and validity of a multidimensional partner abuse measure in clinical settings. Violence Vict. 2005 Oct;20(5):529–547. [PubMed] [Google Scholar]
- 28.Jones AS, Carlson Gielen A, Campbell JC. Annual and lifetime prevalence of partner abuse in a sample of female HMO enrollees. Womens Health Issues. 1999;9(6):295–305. [Google Scholar]
- 29.Clark Jocalyn P, Du Mont Janice. Intimate partner violence and health: a critique of Canadian prevalence studies. Can J Public Health. 2003;94(1):52–58. doi: 10.1007/BF03405053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Canadian Centre for Justice Statistics . Family violence in Canada: a statistical profile 2000. Cat no 85-224-XIE. 2000. Family violence in Canada: a statistical profile 2000. Cat no 85-224-XIE. http://www.statcan.ca/english/freepub/85-224-XIE/0000085-224-XIE.pdf. [Google Scholar]
- 31.Hotaling G T, Sugarman D B. An analysis of risk markers in husband to wife violence: the current state of knowledge. Violence Vict. 1986;1(2):101–124. [PubMed] [Google Scholar]
- 32.Holtzworth-Munroe A, Meehan J C, Herron K, Rehman U, Stuart G L. Testing the Holtzworth-Munroe and Stuart (1994) batterer typology. J Consult Clin Psychol. 2000 Dec;68(6):1000–1019. doi: 10.1037/0022-006X.68.6.1000. [DOI] [PubMed] [Google Scholar]
- 33.Kyriacou D N, Anglin D, Taliaferro E, Stone S, Tubb T, Linden J A, Muelleman R, Barton E, Kraus J F. Risk factors for injury to women from domestic violence against women. N Engl J Med. 1999 Dec 16;341(25):1892–1898. doi: 10.1056/NEJM199912163412505. [DOI] [PubMed] [Google Scholar]
- 34.Pan H S, Neidig P H, O'Leary K D. Predicting mild and severe husband-to-wife physical aggression. J Consult Clin Psychol. 1994 Oct;62(5):975–981. doi: 10.1037/0022-006X.62.5.975. [DOI] [PubMed] [Google Scholar]
- 35.Goldkamp JS, Weiland D, Collins M. The role of drug and alcohol abuse in domestic violence and its treatment: Dade County’s Domestic Violence Court experiment. Final report. 1999. The role of drug and alcohol abuse in domestic violence and its treatment: Dade County’s Domestic Violence Court experiment. Final report. [Google Scholar]
- 36.Coker A L, Smith P H, McKeown R E, King M J. Frequency and correlates of intimate partner violence by type: physical, sexual, and psychological battering. Am J Public Health. 2000 Apr;90(4):553–559. doi: 10.2105/ajph.90.4.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wilson M, Johnson H, Daly M. Lethal and nonlethal violence against wives. Can J Criminol. 1995;37:331–61. [Google Scholar]
- 38.Statistics Canada CANSIM table 282-0002. Labour force survey estimates (LFS), by sex and detailed age group, annual. 2007. [accessed 2007 Jul 24]. http://www40.statcan.ca/l01/cst01/labor05.htm.
- 39.U.S. Preventive Services Task Force Screening for depression: recommendations and rationale. Ann Intern Med. 2002;136(10):760–4. doi: 10.7326/0003-4819-136-10-200205210-00012. http://www.ncbi.nlm.nih.gov/entrez/utils/fref.fcgi?PrId=3051&itool=AbstractPlus-def&uid=12020145&db=pubmed&url=http://www.annals.org/cgi/pmidlookup?view=reprint&pmid=12020145. [DOI] [PubMed] [Google Scholar]
- 40.MacMillan Harriet L, Patterson Christopher J S, Wathen C Nadine, Feightner John W, Bessette Paul, Elford R Wayne, Feig Denice S, Langley Joanne, Palda Valerie A, Patterson Christopher, Reeder Bruce A, Walton Ruth. Screening for depression in primary care: recommendation statement from the Canadian Task Force on Preventive Health Care. CMAJ. 2005 Jan 4;172(1):33–35. doi: 10.1503/cmaj.1030823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Glass N, Dearwater S, Campbell J. Intimate partner violence screening and intervention: data from eleven Pennsylvania and California community hospital emergency departments. J Emerg Nurs. 2001 Apr;27(2):141–149. doi: 10.1067/men.2001.114387. [DOI] [PubMed] [Google Scholar]
- 42.Goodwin M M, Gazmararian J A, Johnson C H, Gilbert B C, Saltzman L E. Pregnancy intendedness and physical abuse around the time of pregnancy: findings from the pregnancy risk assessment monitoring system, 1996-1997. PRAMS Working Group. Pregnancy Risk Assessment Monitoring System. Matern Child Health J. 2000 Jun;4(2):85–92. doi: 10.1023/A:1009566103493. [DOI] [PubMed] [Google Scholar]
- 43.Saltzman Linda E, Johnson Christopher H, Gilbert Brenda Colley, Goodwin Mary M. Physical abuse around the time of pregnancy: an examination of prevalence and risk factors in 16 states. Matern Child Health J. 2003 Mar;7(1):31–43. doi: 10.1023/A:1022589501039. [DOI] [PubMed] [Google Scholar]
- 44.Martin S L, Mackie L, Kupper L L, Buescher P A, Moracco K E. Physical abuse of women before, during, and after pregnancy. JAMA. 2001 Mar 28;285(12):1581–1584. doi: 10.1001/jama.285.12.1581. [DOI] [PubMed] [Google Scholar]
- 45.Stewart D E, Cecutti A. Physical abuse in pregnancy. CMAJ. 1993 Nov 1;149(9):1257–1263. [PMC free article] [PubMed] [Google Scholar]
- 46.Cokkinides V, Coker A. Experiencing physical violence during pregnancy: prevalence and correlates. Fam Community Health. 1998;20(4):19–37. [Google Scholar]
- 47.Campbell Jacquelyn C, Webster Daniel, Koziol-McLain Jane, Block Carolyn, Campbell Doris, Curry Mary Ann, Gary Faye, Glass Nancy, McFarlane Judith, Sachs Carolyn, Sharps Phyllis, Ulrich Yvonne, Wilt Susan A, Manganello Jennifer, Xu Xiao, Schollenberger Janet, Frye Victoria, Laughon Kathryn. Risk factors for femicide in abusive relationships: results from a multisite case control study. Am J Public Health. 2003 Jul;93(7):1089–1097. doi: 10.2105/ajph.93.7.1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Statistics Canada Census 2001: data tables. 2002. [accessed 2007 Jul 24]. http://www12.statcan.ca/english/census01/Products/standard/themes/DataProducts.cfm?S=1&T=37&ALEVEL=2&FREE=0.