Abstract
Background
The polypoid form of chronic rhinosinusitis (chronic rhinosinusitis with nasal polyps [CRSwNP]) is a highly prevalent disease that often requires surgical intervention for treatment. Nasal polyps contain large quantities of B lymphocytes and immunoglobulin as well as eosinophils.
Objectives
The objective of this study was to investigate the expression of B cell–activating factor of the TNF family (BAFF), an important regulator of class-switch recombination and immunoglobulin production, in patients with chronic rhinosinusitis (CRS).
Methods
We collected nasal tissue and nasal lavage fluid from patients with CRS and control subjects. We assayed mRNA for BAFF and B-lymphocyte markers, CD20 and transmembrane activator and calcium-modulator and cyclophilin ligand interactor, by using real-time PCR, and assayed BAFF protein by using ELISA and immunohistochemistry.
Results
BAFF mRNA was significantly increased in nasal polyps from patients with CRSwNP (P < .001) compared with inferior turbinate tissue from patients with CRS or healthy subjects. BAFF protein was also elevated in polypoid tissue and nasal lavage from patients with CRSwNP.
Immunohistochemistry showed considerable BAFF staining in mucosal epithelial cells in nasal polyps along with unidentified cells in the lamina propria. Expression of mRNA for BAFF in sinonasal tissue was significantly correlated with CD20 and transmembrane activator and CAML interactor in sinus tissue. IgA, an immunoglobulin isotype known to activate eosinophils, was also significantly elevated in the polypoid tissue.
Conclusion
Overproduction of BAFF in nasal polyps may contribute to the pathogenesis of CRSwNP via the local induction of IgA and activation of eosinophils.
Keywords: Chronic rhinosinusitis, nasal polyps, BAFF, IgA, B cells, eosinophils, epithelial cells
Chronic rhinosinusitis (CRS) is the most common chronic disease in adults in the United States and is estimated to affect 5% to 15% of the urban population.1,2 Primarily on the basis of physical examination, histology, and clinical course, CRS is frequently divided into 2 types: CRS with nasal polyps (CRSwNP) and CRS without nasal polyps (CRSsNP). The etiology and pathogenesis of CRS remain controversial, but recent studies have implicated Alternaria fungi or toxin-secreting staphylococci as key pathogens initiating the symptomatic mucosal inflammation.3,4 Histologic studies have demonstrated significant tissue eosinophilia in a high proportion of CRS cases, most prominently in CRSwNP.5 The ultimate factors inducing this mucosal eosinophilia remain uncertain, but several studies have reported that IL-5 (an eosinophil survival and differentiation factor), eotaxins (eosinophil chemoattractants) and eosinophil cationic protein (an indicator of the presence of eosinophil) are significantly increased in polyp tissue compared with sinonasal tissue from patients with CRSsNP or from healthy subjects.6–8 Taken together, these results point to a prominent role for eosinophils in the pathophysiology of CRSwNP and further suggest that factors triggering eosinophil degranulation may also be associated with polyp formation.
In the case of several diseases of the airways, there are compelling reasons to believe that local proliferation and activation of B cells is of central pathogenic importance.9–14 Local B-cell class-switch recombination and synthesis of IgE and IgA can mediate activation of airway mast cells and eosinophils, respectively, in response to antigen exposure. In the case of CRS, a large proportion of patients with nasal polyps demonstrate the presence of local IgE against aeroallergens without evidence of circulating IgE against the same antigens.12,13 Recent studies have indicated that plasma cell number and antigen-specific IgE concentration are increased in the polypoid sinonasal mucosal tissue from patients with CRSwNP.8,15,16 In contrast with IgE, which is believed to activate mast cells in atopic patients with CRS, the role of IgA in CRS is poorly understood. Interestingly, IgA can serve as a trigger for eosinophil degranulation by binding to surface receptors present on these cells. Although it has become clear that B-cell accumulation and immunoglobulin production at local mucosal sites in the airway are of great importance to airway inflammatory diseases, the mechanism of local immunoglobulin class switching and production is not fully understood.
B cell–activating factor of the TNF family (BAFF; also known as BLyS, TNFSF13B, TALL-1, and THANK) and a proliferation-inducing ligand (APRIL) are recently identified members of the TNF superfamily that play important roles in B-cell survival, proliferation, and maturation.17–19 Although class-switch recombination is generally thought to be highly dependent on ligation of CD40 (on B cells) and CD40 ligand (on activated T cells), it has been reported that BAFF and APRIL also promote T cell–dependent immunoglobulin production as well as CD40-independent, T cell–independent immunoglobulin class switching and production.20–22 BAFF binds to 3 receptors that are selectively expressed on B cells and plasma cells, including BAFF receptor (BAFF-R), transmembrane activator and CAML interactor (TACI), and B-cell maturation antigen. APRIL also binds to TACI and B-cell maturation antigen, but not BAFF-R. BAFF-R is a potent regulator of mature B-cell survival and IgE production by BAFF.23 In contrast, TACI has been considered to suppress B-cell proliferation and survival but is critical for the class-switch recombination and production of IgA in human beings.19,24 Although BAFF has been recognized to be mainly a product of myeloid cells such as monocytes, macrophages, dendritic cells, and neutrophils, nonlymphoid cell types also produce BAFF, including salivary gland epithelial cells and astrocytes.19 Recently we have demonstrated that BAFF is produced by bronchial epithelial cells after stimulation with ligand for Toll-like receptor (TLR)–3, IFNs, and TNF in quantities of the same order of magnitude as produced by myeloid cells.25 In the current study, we investigated whether BAFF and APRIL might be involved in the pathogenesis of CRS. We discovered that resected polyp tissue from patients with CRSwNP had elevated levels of BAFF protein as well as markers of B cells and IgA. These findings imply that upregulation of BAFF inCRSwNP may amplify eosinophilic inflammation via induction of class-switch recombination and production of IgA by B cells in nasal polyps.
METHODS
Patients and biopsies
Patients with CRS were recruited from the allergy clinic and the otolaryngology clinic at Northwestern University and the Northwestern Sinus Center. Sinonasal and polyp tissues were obtained from routine functional endoscopic sinus surgery in the patients with CRS. All subjects met the criteria for CRS as defined by the Sinus and Allergy Health Partnership.1 The presence of sinusitis or bilateral nasal polyps was confirmed by office endoscopy and computed tomography imaging. All patients scheduled for surgery had previously failed to respond to adequate trials of conservative medical therapy (prolonged antibiotic regimens, nasal steroid sprays, oral steroids, saline irrigations, and decongestants) for control of symptoms. Patients with an isolated antrochoanal polyp, cystic fibrosis, or unilateral nasal polyps were excluded from the study. Details of subjects’ characteristics are included in Table I. Disease-free control subjects undergoing procedures to correct anatomical defects without history of CRS or asthma were recruited from the otolaryngology clinic at Northwestern University. All subjects signed informed consent, and the protocol and consent forms governing procedures for this study have been approved by the Institutional Review Board of Northwestern University Feinberg School of Medicine. A portion of each sample for isolation of RNA was transferred in RNAlater (Ambion, Austin, Tex) and stored at −20°C.
TABLE I.
Subject characteristics
| Normal | CRSsNP | CRSwNP | CRSwNP polyp | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total no. of subjects | n = 30 (18 M/12 F) | n = 39 (18 M/21 F) | n = 60 (26 M/34 F) | — | ||||||||
| Age (y), median (range) | 36 (20–77) | 41 (25–64) | 42 (25–77) | — | ||||||||
| Y | N | U | Y | N | U | Y | N | U | — | |||
| Atopy | 8 | 21 | 1 | 18 | 18 | 3 | 31 | 22 | 7 | — | ||
| Asthma | 0 | 30 | 0 | 7 | 30 | 2 | 32 | 27 | 1 | — | ||
| Methodology used | ||||||||||||
| Tissue RNA | n = 12 (10 M/2 F) | n = 12 (6 M/6 F) | n = 9 (4 M/5 F) | n = 15 (10 M/5 F) | ||||||||
| Age (y), median (range) | 36 (20–77) | 34 (27–55) | 44 (28–69) | 44 (28 – 74) | ||||||||
| Tissue extract | n = 13 (9 M/4 F) | n = 17 (9 M/8 F) | n = 8 (2 M/6 F) | n = 23 (6 M/17 F) | ||||||||
| Age (y), median (range) | 36 (27–71) | 40 (27–61) | 47 (27–69) | 41 (26–59) | ||||||||
| Nasal lavage | n = 7 (2 M/5 F) | n = 7 (4 M/3 F) | n = 12 (4 M/8 F) | — | ||||||||
| Age (y), median (range) | 48 (23–60) | 33 (30–59) | 50 (25–77) | — | ||||||||
| Immunohistochemistry | n = 4 (3 M/1 F) | n = 9 (4 M/5 F) | n = 9 (6 M/3 F) | n = 7 (7 M/0 F) | ||||||||
| Age (y), median (range) | 35 (25–42) | 43 (29–64) | 32 (27–74) | 39 (27–74) | ||||||||
F, Female; M, male; N, no; U, unknown; Y, yes.
Cell culture
The methods for primary nasal epithelial cell (PNEC) culture are described in this article’s Online Repository at www.jacionline.org and in Kim et al.26
Real-time PCR
Total RNA from sinus tissue was extracted using QIAzol (Qiagen, Valencia, Calif) and was cleaned and treated with DNase I using RNeasy (Qiagen) according to the manufacturer’s instructions. Quality of total RNA from sinus tissue was assessed with a 2100 Bioanalyzer (Agilent Technologies, Santa Clara, Calif) using a RNA 6000 Nano LabChip (Agilent Technologies). Single-strand cDNA was synthesized with SuperScript II reverse transcriptase (Invitrogen, Carlsbad, Calif) and random primers. Semiquantitative real-time RT-PCR was performed with a TaqMan method using an Applied Biosystems 7500 Sequence Detection System (Applied Biosystems, Foster City, Calif) as described previously.25 Primer and probe sets for 5 genes, BAFF,25 APRIL,25 CD20 (sense, 5′-CACTCTTCAGGAGGATGTCTTCACT-3′; anti-sense, 5′-TCTGGACAGCCCCCAAAGT-3′; minor groove binder-probe, 5′-TCTTCATGAGGGAATCTA-3′), TACI (sense, 5′-AACTCGGGAAGGTACCAAGG-3′; antisense, 5′-GCTGTAGACCAGGGCCACC-3′; 6-carboxyfluorescein/6-carboxytetramethylrhodamine-probe, 5′-CCAGAAGCAAGTC CAGCTCTCCCGG-3′), and β-actin (ACTB; sense, 5′-CTGGCCGGGACCTGACT-3′; antisense, 5′-GCAGCCGTGGCCATCTC-3′;MGB-probe, 5′-CACCACCACGGCCGA-3′) were synthesized by Applied Biosystems or Integrated DNA Technologies (Coralville, Iowa). A primer and probe set for β-glucuronidase (human β-glucuronidase endogenous control, part number 4326320) was purchased from Applied Biosystems. To determine the exact copy number of the target genes, quantified aliquots of purified PCR fragments of the target genes were serially diluted and used as standards in each experiment. Aliquots of cDNA equivalent to 10 ng of total RNA were used for real-time PCR. The mRNA expression levels were normalized to the median expression of housekeeping genes, ACTB for PNEC and β-glucuronidase for nasal tissue.
Measurement of BAFF and IgA in tissue homogenates and nasal lavage fluids
Freshly obtained tissue specimens were weighed, and 1 mL PBS supplemented with 0.05% Tween 20 (Sigma-Aldrich, St Louis, Mo) and 1% protease inhibitor cocktail (PN; P8340, Sigma-Aldrich) was added per every 100 mg tissue. The tissue was then homogenized with an Ultra-Turrax T8 homogenizer (IKA, Wilmington, NC) at setting 3 for 1 minutes on ice. After homogenization, the suspension was centrifuged at 4000 rpm for 20 minutes at 4°C, and the supernatants were stored at −80°C until analyzed.
Nasal lavage was performed by instilling 5mL sterile PBS into each nostril, holding for 5 seconds and then expelling into a sterile container. Samples were concentrated 2-fold by using Centriplus YM-10 (Millipore, Bedford, Mass) and stored at −80°C until analyzed.
The concentrations of BAFF (R&D Systems, Minneapolis, Minn) and IgA (Bethyl Laboratory, Montgomery, Tex) in cell-free supernatants were determined by specific ELISA kits. The minimal detection limits for these kits are 15 pg/mL and 7.8 ng/mL, respectively. The concentration of total protein was measured with a Bradford method–based Bio-Rad protein assay kit (Bio-Rad, Hercules, Calif). Concentrations of BAFF and IgA in the tissue homogenate and nasal lavage were normalized to the concentration of total protein.
Immunohistochemistry
Nasal tissue was dehydrated, infiltrated, and embedded with paraffin, and tissue was sectioned at 3 µm by using a Leica RM2245 Cryostat (Leica Microsystems Inc, Bannockburn, Ill). Sections were rehydrated and blocked for endogenous peroxidase activity with 3% H2O2/methanol. After rinsing, tissue sections were blocked for nonspecific binding with 1% goat serum/0.3% Tween-20/PBS. Tissue sections were then incubated with 0.125 µg/mL rat antihuman BAFF mAb (clone: Buffy 2, IgM; Abcam, Cambridge, Mass) or 0.125 µg/mL rat IgM antibody (clone: RTK2118; Abcam) for 1 hour at room temperature. Sections were rinsed and then incubated in biotinylated secondary goat antirat antibody (Jackson ImmunoResearch Laboratories, West Grove, Pa) at a 1:500 dilution for 1 hour at room temperature. After another rinse, sections were incubated in ABC reagent (avidin–biotin–horseradish peroxidase complex; Vector Laboratories, Burlingame, Calif) for 1 hour at room temperature. Sections were rinsed again and incubated in diaminobenzidine reagent (Invitrogen) for 10 minutes at room temperature. They were then rinsed in deionized H2O, counterstained with hematoxylin, dehydrated, cleared, mounted, and coverslipped by using Cytoseal 60 (Richard-Allan Scientific, Kalamazoo, Mich) in preparation for microscopic analysis.
The number of BAFF positive cells in epithelium, glands, and submucosae was counted by using a magnification of × 400. Each section was randomly selected, and diagnosis was unknown to the observer. The tissue area counted was determined using the National Institutes of Health–issued Image J software.
Statistics
All data are reported as the means ± SEMs unless otherwise noted. Differences between groups were analyzed by using the Wilcoxon signed-rank test or the Mann-Whitney U test. Correlations were assessed by using the Spearman rank correlation. A P value less than .05 was considered significant.
RESULTS
BAFF expression in CRS
To determine the relevance of BAFF and APRIL expression in chronic rhinosinusitis, sinonasal and polyp tissues were collected from 39 subjects with CRSsNP, 60 subjects with CRSwNP, and 30 control subjects. Subject characteristics are shown in Table I. Subjects in the various groups were of similar age and sex. None of the patients had Churg-Strauss syndrome or allergic fungal sinusitis, and 1 patient with CRSwNP had aspirin sensitivity (but not asthma) in this study. Historically, approximately 80% of nasal polyps have eosinophilia (ie, greater than 5 eosinophils per high power field) in our clinic.
It has been reported that mRNA expression of housekeeping genes, including ACTB, is elevated in the nasal mucosa of patients with CRS compared with control subjects.27 We therefore first screened the expression of housekeeping genes in the inferior turbinate (IT) from patients with CRS and in nasal polyp tissue by using the TaqMan Human Endogenous Control Plate (Applied Biosystems), which included 11 housekeeping genes and an internal positive control. We found that the level of mRNA expression of 3 housekeeping genes, 18S rRNA, acidic ribosomal protein, and β-glucuronidase, was not significantly different between IT and nasal polyp tissue and that the level of mRNA expression of the 8 other genes, including ACTB, was elevated in the nasal polyps (n = 4; data not shown). We thus selected β-glucuronidase as the housekeeping gene for normalization in the current report.
We assessed the expression of BAFF and APRIL in IT tissue from patients with CRSsNP and CRSwNP and controls, as well as in polyp tissue from patients with CRSwNP. Expression of β-glucuronidase was not significantly different between the 4 groups (data not shown). BAFF mRNA was significantly increased in polyp tissue from patients with CRSwNP (P <.001) in comparison with IT tissue from either patients with CRS or control subjects (Fig 1, A). In contrast, expression of mRNA for APRIL was not different in the same groups (data not shown). To confirm this observation at the protein level, we made detergent extracts from homogenates of IT and nasal polyp tissues and then measured the concentration of BAFF by using ELISA. BAFF protein was significantly increased in polyp tissue (P <.05) compared with IT tissue from either patients with CRS or control subjects (Fig 1, B). BAFF was detected in 11 of 23 nasal polyp extracts from patients with CRSwNP and in 2 of 17 IT extracts from patients with CRSsNP, but it was not detected in IT extracts from either patients with CRSwNP (n = 8) or control subjects (n = 13; Fig 1, B). We also determined BAFF protein expression in nasal lavage fluids collected from separate groups of subjects. BAFF protein was detected in 5 of 12 nasal lavage fluids from patients with CRSwNP (P < .05) but was not detected in nasal lavage from patients with CRSsNP (n = 7) or from control subjects (n = 7; Fig 1, C). These data suggest that BAFF is locally produced in the nasal mucosa of 40% to 50% of patients with CRSwNP.
FIG 1.
Detection of BAFF in patients with CRSwNP. A, Total RNA was extracted from IT and nasal polyps (Polyp), and expression of BAFF was analyzed by using real-time PCR. The concentration of BAFF in tissue homogenates of IT and polyp (B) and nasal lavage (C) was measured by using ELISA. BAFF concentration was normalized to the concentration of total protein.
To examine the BAFF-producing cells in nasal mucosa, we used immunohistochemistry to detect BAFF in uncinate tissue and nasal polyp tissue. As shown in Fig 2, BAFF staining was observed in the mucosal and the glandular epithelium as well as in submucosal cells. Elevated submucosal staining was found in tissue from patients with CRSwNP. Similar data were obtained by using a different clone of antihuman BAFF mAb (a kind gift from Drs Fabienne Mackay and Charles Mackay, Garvan Institute of Medical Research, Darlinghurst, Australia). We also counted the number of BAFF-positive cells by using a semiquantitative method. Perhaps because BAFF was highly expressed by epithelial cells in all subject groups, we did not observe a significant difference in the number of BAFF-positive cells in the epithelium and glands among the 3 groups of subjects (Table II). However, BAFF-positive cells were significantly elevated in the submucosal region of uncinate and nasal polyp tissues from the patients with CRSwNP (Fig 2, D– F; Table II).
FIG 2.
Immunohistochemistry of BAFF was performed by using antihuman BAFF mAb (clone: Buffy 2). A, Negative control antibody staining in uncinate tissue (UT) from a patient with CRSsNP. B–F, Representative immunostaining for BAFF in UT from a control subject (B), a patient with CRSsNP (C), and a patient with CRSwNP (D) and in nasal polyp tissue (E and F). Arrow, Eosinophil-like cells. Magnification ×200 (A–E); ×400 (F).
TABLE II.
BAFF-positive cells in nasal mucosal tissue from normal subjects and patients with CRS
| Normal UT | CRSsNP UT | CRSwNP UT | CRSwNP polyp | |
|---|---|---|---|---|
| Epithelium | n = 4 | n = 7 | n = 6 | n = 6 |
| BAFF+ cells (102 cells/mm2) | 8.6 ± 3.2 | 12.4 ± 6.1 (NS) | 6.0 ± 1.6 (NS) | 7.7 ± 3.3 (NS) |
| Glands | n = 4 | n = 7 | n = 8 | n = 5 |
| BAFF+ cells (102 cells/mm2) | 7.3 ± 3.5 | 3.7 ± 0.9 (NS) | 5.7 ± 1.9 (NS) | 6.0 ± 2.9 (NS) |
| Submucosa | n = 4 | n = 9 | n = 9 | n = 7 |
| BAFF+ cells (102 cells/mm2) | 2.8 ± 0.7 | 7.4 ± 2.2 (NS) | 7.0 ± 0.6 (P = .003) | 6.5 ± 1.0 (P = .024) |
UT, Uncinate tissue; NS, not significant.
Data are presented as means ± SEMs. P value is determined compared with normal.
Nasal polyps from patients with CRSwNP have long been known to be characterized by eosinophilic inflammation.1,5 Immunohistochemical staining showed that some of the BAFF-positive cells in polyp tissue may be eosinophils (Fig 2, F, arrow).We therefore tested whether eosinophils were able to produce BAFF. Purified human eosinophils from peripheral blood were stimulated with IL-5, GM-CSF, plate-bound secretory IgA, IFN-β, and IFN-γ. However, we could not find detectable amounts of BAFF in supernatants of eosinophils stimulated as long as 72 hours (data not shown).
BAFF and APRIL expression in nasal epithelial cells
Although we have reported that bronchial epithelial cells are capable of producing BAFF,25 it is not known whether nasal epithelial cells also produce BAFF. To test the possible role of the expression of BAFF and APRIL in nasal epithelial cells, PNECs were treated for 6 hours with various stimuli including TLR ligands and cytokines. In resting PNECs, expression of BAFF and APRIL was minimal. However, mRNA for BAFF was significantly upregulated by stimulation with double-stranded RNA (dsRNA) (TLR-3 ligand; 213-fold: n = 7, P < .05), IFN-β (22-fold; n = 8; P < .05), IFN-γ (6-fold; n = 9; P < .05), and IFN-λ1 (6-fold; n = 5; P <.05), and was not affected by peptidoglycan (TLR-2 ligand), LPS (TLR-4 ligand), flagellin (TLR-5 ligand), TNF, IL-1β, IL-4, IL-6, IL-10, IL-13, IL-17, oncostatin M, and TGF-β in PNEC (see this article’s Fig E1, A, in the Online Repository at www.jacionline.org; data not shown). In contrast, mRNA for APRIL was significantly but weakly upregulated by stimulation with dsRNA (2-fold; n = 7; P < .05), IL-4 (2-fold; n = 7; P < .05), IFN-β (2-fold; n = 8; P < .05) and IFN-γ (2-fold; n = 9; P <.05; Fig E1, A). To examine further the details of the induction of mRNA for BAFF, we determined the time dependence of the responses in PNECs. Expression of mRNA for BAFF induced by dsRNA peaked at 24 hours, and elevated expression of BAFF persisted as long as 72 hours (Fig E1, B). In contrast, expression of mRNA for BAFF induced by IFN-β peaked at 6 hours, then returned to baseline at 72 hours (Fig E1, B). These data imply that the mechanism of dsRNA-dependent BAFF expression in PNECs may be the same as in bronchial epithelial cells, in which we identified an autocrine/paracrine loop involving IFN-β. 25 To confirm these findings at the protein level, we measured the production of BAFF by using ELISA. Significant levels of BAFF were detected in the supernatant after stimulation with dsRNA and IFN-β for 72 hours (control, undetectable; dsRNA-treated, 64 ± 10 pg/mL, n = 7; IFN-β–treated, 20 ± 5 pg/mL, n = 4; Fig E1, C).
CD20 and IgA expression in nasal polyps
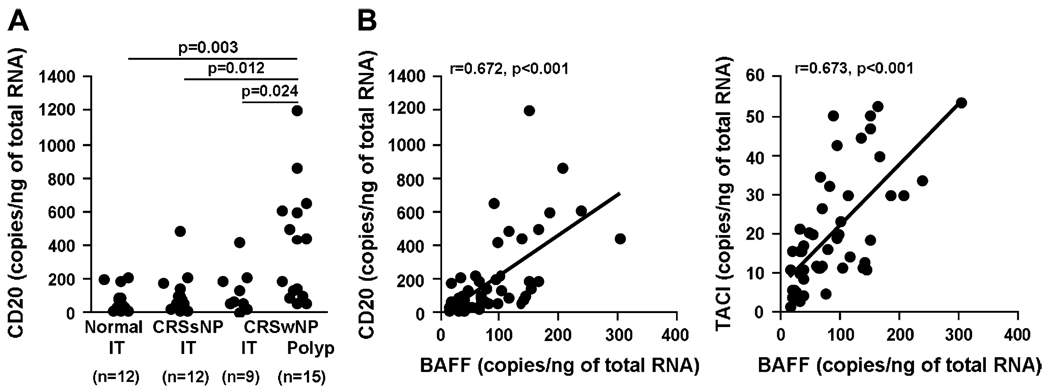
Because BAFF is known to be an important factor in the generation, maintenance, and activation of B lymphocytes, we next assessed the level of expression of mRNA for the B-cell marker CD20 and for TACI (a receptor for BAFF expressed on B cells and plasma cells) in IT tissue from patients with CRS and control subjects, and in polyp tissue from patients with CRSwNP. The expression of CD20 (and TACI) was highly elevated in nasal polyps from patients with CRSwNP compared with IT tissue from patients with CRS and control subjects (Fig 3, A; data not shown; P < .05). The levels of expression of CD20 and TACI were significantly correlated with the expression of BAFF (CD20, r = 0.672, P < .001; TACI, r = 0.673, P < .001; Fig 3, B), suggesting that locally produced BAFF may be involved in the elevation of B cells. As a monitor of local B-cell responses, we examined the concentration of IgA and IgE in tissue extracts. The level of IgA was significantly increased in polyp tissue from patients with CRSwNP (25.7 ± 3.6 µg/mg; n = 10; P < .001) compared with IT tissue from patients with CRSsNP (7.4 ± 1.9 µg/mg; n = 11), patients with CRSwNP (6.6 ± 1.3 µg/mg; n = 9), or healthy subjects (5.2 ± 1.1 µg/mg; n = 9; Fig 4). In contrast, we did not observe a significant difference in the levels of total IgE in the tissue homogenates from these groups of subjects (data not shown).
FIG 3.
B-cell accumulation in nasal polyps. A, Total RNA was extracted from IT and nasal polyps (Polyp), and expression of CD20 was analyzed by using real-time PCR. B, Relationship of expression of BAFF and the B-cell marker CD20 or the BAFF receptor TACI in the nasal tissue was evaluated by using real-time PCR. Correlations were assessed by using the Spearman rank correlation.
FIG 4.
Elevated expression of IgA in nasal polyps. Measurement of IgA in tissue homogenates of IT from control subjects, from patients with CRSsNP and CRSwNP, and in nasal polyps was measured by using ELISA. IgA concentration was normalized to the concentration of total protein.
DISCUSSION
B cell–activating factor of the TNF family is an important regulator of immunoglobulin class-switch recombination and production in B lymphocytes, independent of T-cell help. BAFF also enhances T cell–dependent immunoglobulin class switching and production. This study provides the first demonstration that BAFF is significantly increased in polypoid tissue from patients with CRSwNP (Fig 1 and Fig 2). Significant levels of BAFF protein were found in both polypoid tissue and nasal lavage taken from patients with CRSwNP (Fig 1). BAFF-positive cells were elevated in the submucosal tissue of uncinate and nasal polyps from patients with CRSwNP (Fig 2; Table II). We also demonstrate that IgA was significantly elevated in polyp tissue from patients with CRSwNP (Fig 4).
It has been reported that B cells, plasma cells, and antigen-specific IgE accumulate in the nasal mucosa of patients with CRSwNP, although the mechanism is not fully understood.8,12,13,15,16 In the current study, we demonstrate that mRNA encoding BAFF was significantly increased in polyp tissue (Fig 1, A). BAFF protein was detected in 40% to 50% of polyp tissue extracts and was also detected in nasal lavage from a distinct cohort of patients with CRSwNP (Fig 1, B and C), reinforcing this finding. Although BAFF protein was found to be elevated in only half of the CRSwNP extracts and nasal lavage samples, elevated BAFF mRNA was detected in nearly all polyp tissues. This difference may reflect the detection limit of the ELISA and the relatively dilute extracts that were used. Importantly, expression of BAFF was correlated with expression of CD20 in nasal tissue and with levels of TACI, a receptor for BAFF and APRIL found on B cells and plasma cells (Fig 3, B). These data suggest that increased levels of BAFF may play a role in local proliferation and activation of B cells and plasma cells in nasal polyp tissue. It is possible that other B-cell activators such as IL-6 and/or B-cell chemokines may be involved in B-cell accumulation and activation in nasal polyps.
Our in vitro data showed that nasal epithelial cells were able to make BAFF (Fig E1), prompting us to search for BAFF-producing cells in nasal mucosa by using immunohistochemistry. In this experiment, we selected uncinate tissue instead of IT because uncinate tissue is in proximity to the region where nasal polyps generally form. We found that mucosal epithelial cells and glandular epithelial cells were both a major source of BAFF in the nasal mucosa (Fig 2). Surprisingly, BAFF was constitutively expressed in the epithelium of all subjects, and the level of expression was not significantly different in uncinate tissue from patients with CRS and control subjects or in nasal polyps despite the fact that BAFF mRNA was elevated only in nasal polyp tissue (Fig 1 and Fig 2; Table II). There are several possible explanations for why results from experiments evaluating epithelial BAFF staining and experiments assessing levels of BAFF protein may not agree. We previously showed that airway epithelial cells produce BAFF protein on both the apical and basolateral sides of the monolayer after stimulation.25 The current study showed that BAFF protein was detected only in the nasal lavage of patients with CRSwNP (Fig 1, C). These data suggest that BAFF protein production may be elevated in the epithelium of patients with CRSwNP, and activated epithelial cells may constitutively secrete BAFF into the lumen and submucosa. BAFF, like other members of the TNF superfamily, must be cleaved from the cell surface by furin convertase enzymes 17,28 to be liberated into the nasal lavage and, presumably, the tissue extracts. Although the total number of epithelial cells expressing BAFF on their surface may not differ between patients and controls, the process by which it is liberated may occur only in patients with CRSwNP. Alternatively, it is possible that the BAFF, that we have detected in nasal lavage fluid from patients with CRSwNP, might have been produced by cells in the lamina propria of the nasal polyp tissue. Data from immunohistochemistry clearly showed that BAFF-positive cells were elevated in the submucosal tissue of patients with CRSwNP (Fig 2; Table II). Interestingly, BAFF-positive cells were elevated in the submucosal region of both uncinate tissue and nasal polyps (Table II). This result suggests that elevated BAFF production may not occur exclusively in nasal polyp tissue and that elevations of BAFF may not be sufficient to lead to the generation of a nasal polyp.
Nasal polyps are characterized by eosinophilic inflammation. We therefore considered the possibility that BAFF is made by infiltrating eosinophils in the submucosa of nasal polyps. Data from immunohistochemistry showed that some eosinophil-like cells from patients with CRSwNP stained for BAFF (Fig 2, F). However, we could not obtain evidence indicating that either resting or primed eosinophils purified from peripheral blood make BAFF by using an in vitro culture system (data not shown). Previous studies have shown that eosinophils isolated from bronchoalveolar lavage are phenotypically distinct from those primed by cytokines in vitro.29,30 For example, tissue eosinophils in lung from patients with asthma expressed reduced IL-5 receptor and are relatively resistant to anti–IL-5 antibody treatment, in contrast with eosinophils in the blood.31,32 Although further experiments will be required to determine the identity of the BAFF-producing cells in the submucosa, data from immunohistochemistry suggest that 1 type may be lymphocytes (Fig 2). Several groups have reported that BAFF is expressed by T cells, although the level of expression is rather weak compared with that of myeloid cells.19,33 BAFF expression in T cells has been suggested to be elevated in autoimmune diseases such as SLE.34 It has also been reported that malignant B cells and salivary gland B cells in Sjögren syndrome synthesize BAFF, although normal B cells do not usually make BAFF.19,35 Although B cells have only trace levels of membrane-bound BAFF, recent studies show that blood B cells can have receptor-bound BAFF that can be detected as surface BAFF by using flow cytometry.36 In the same studies, germinal center B cells did not have receptor-bound BAFF, possibly because germinal centers contain low levels of soluble BAFF.36 Future studies will be required to determine whether infiltrating eosinophils, T cells, B cells, or other cell types in nasal polyps synthesize BAFF or have receptor-bound BAFF.
We also examined expression of APRIL in CRS. APRIL was not elevated in nasal mucosa of patients with CRS, and APRIL was not strongly induced by most stimuli tested in PNECs (Fig E1, A; data not shown). He et al22 recently reported that baseline expression of APRIL is much higher in intestinal epithelial cells than epithelial cells from the epidermis, lung, and mouth. APRIL is strongly induced by flagellin and LPS in intestinal epithelial cells,22 whereas we observed that flagellin and LPS did not affect the expression of APRIL in PNEC (Fig E1, A; data not shown). It has been reported that TLR-4 and TLR-5 are highly expressed in intestinal epithelial cells, possibly because the surface of the human intestine is densely colonized by a variety of largely commensal microbial species, and intestinal epithelial cells need to detect these bacteria to prevent invasion.22,37 In contrast, the most prominently expressed TLRs in airway epithelial cells are TLR-2 and TLR-3.38–40 The differences in BAFF and APRIL expression between intestinal and airway epithelial cells may suggest that APRIL is an important regulator of induction of class switching and production of IgA for protection from commensal bacteria in the intestine, whereas airway epithelial BAFF may trigger the induction of immunoglobulin class-switch recombination and production induced by infection with viruses and bacteria in the airways.
One hallmark feature of CRS is upper airway inflammation. The mucosal lining in patients with CRSsNP is characterized by basement membrane thickening, goblet cell hyperplasia, glandular hyperplasia, limited subepithelial edema, mononuclear cell infiltration, and a predominantly neutrophilic inflammation, with a diminished contribution of eosinophils compared with CRSwNP.1,2 CRSwNP reveals frequent epithelial damage and a thickened basement membrane, and a prominent feature is edematous and occasionally fibrotic stromal tissue.1,2 CRSwNP is usually characterized by intense eosinophilic inflammation. Importantly, EG2+ activated eosinophils are found in about 80% of nasal polyp tissue from patients with CRSwNP.5,41 In the middle and inferior turbinate, EG2+ eosinophils are also found in patients with CRSwNP, whereas no EG2+ eosinophils are detected in control subjects, although some resting eosinophils are found.5 The mechanisms of eosinophil accumulation in CRSwNP are well studied. Overproduction of eotaxins and RANTES in nasal polyp epithelium might be important in promoting the local chemotaxis of eosinophils.7,42 Upregulation of the endothelial adhesion molecules vascular cell adhesion molecule 1 and P-selectin regulates eosinophil migration into nasal polyps.42–44 Local production of IL-5 and GM-CSF contributes to the local survival and differentiation of eosinophils.41,45 Despite ample information on the mechanisms of eosinophil accumulation in CRSwNP, the mechanism of activation of eosinophils in nasal polyp is not fully understood, although locally produced IL-5 and GMCSF are thought to contribute to the activation of eosinophils in polyps.
The current finding, that BAFF is elevated in CRSwNP, has considerable implications for the local activation of immunoglobulin production and class switching, as has been proposed to occur in allergic diseases of the upper airways.9,14,46,47 Production of IgA is of particular interest in patients with CRSwNP because nasal polyps are characterized by intense eosinophilic inflammation. One of the most potent stimulators of eosinophil degranulation is IgA, which is abundant on mucosal surfaces. In the current study, we showed that IgA was significantly elevated in nasal polyp tissue (Fig 4). This finding confirms very recent results from Van Zele et al,48 who reported that levels of IgA are much higher in nasal polyp homogenates compared with homogenates of tissue from control subjects or patients with CRSsNP. Van Zele et al48 also showed that total IgE was elevated in the nasal polyp. The mechanism of the elevation of local IgA in nasal polyps is unknown. In the current report, we show that expression of BAFF was highly correlated with expression of both the B-cell marker CD20 and TACI, which is a critical receptor expressed on both B cells and plasma cells that mediates class-switch recombination for IgA induced by BAFF (Fig 3). Thus, it is tempting to speculate that local elevations of BAFF play an important role in activating B cells in nasal polyp tissue to undergo class-switch recombination and to express IgA, and that disruption of BAFF production or signaling might diminish local B-cell responses. Elevated local production of IgA could in turn contribute directly to activation of eosinophils in nasal polyp tissue, an event that would be expected to promote the impressive edema observed in CRSwNP. Interestingly, polypoid CRS in China has been reported to have a lesser eosinophilic phenotype than in Western countries.49 These polyps still contain high levels of B cells and immunoglobulins.49 It would be of interest to determine whether BAFF elevation exists in this form of polypoid CRS.
In summary, we report here that nasal epithelial cells produce the B cell–activating factor BAFF, and that patients with CRSwNP have elevated levels of BAFF, B cells, and IgA in polypoid tissue. Our findings indicate that overproduction of BAFF in nasal polyps may contribute to the pathogenesis of CRSwNP, perhaps via expansion and activation of B cells. The associated increased in production of IgA may contribute to the local activation of eosinophils.
Supplementary Material
Acknowledgments
We thank Drs Fabienne Mackay and Charles Mackay (Garvan Institute of Medical Research, Darlinghurst, Australia) for the kind gift of antihuman BAFF mAb.
Supported in part by National Institutes of Health grants R01 HL068546, R01 HL078860, and 1R01 AI072570 and by a grant from the Ernest S. Bazley Trust.
Abbreviations
- APRIL
A proliferation-inducing ligand
- BAFF
B cell–activating factor of the TNF family
- BAFF-R
B cell–activating factor of the TNF family receptor
- CRS
Chronic rhinosinusitis
- CRSsNP
Chronic rhinosinusitis without nasal polyps
- CRSwNP
Chronic rhinosinusitis with nasal polyps
- IT
Inferior turbinate
- PNEC
Human primary nasal epithelial cell
- TACI
Transmembrane activator and CAML interactor
- TLR
Toll-like receptor
Footnotes
Disclosure of potential conflict of interest: A. Peters has served as a member of the American Academy of Allergy, Asthma & Immunology. D. Conley has received research support from Acclarent. L. C. Grammer has served as an expert witness on reaction during hemodialysis litigation. R. Kern has served as a member of the American Rhinologic Society. The rest of the authors have declared that they have no conflict of interest.
Clinical implications: Expression or function of BAFF in nasal polyps may have a pathogenic role in CRSwNP.
REFERENCES
- 1.Meltzer EO, Hamilos DL, Hadley JA, Lanza DC, Marple BF, Nicklas RA, et al. Rhinosinusitis: establishing definitions for clinical research and patient care. J Allergy Clin Immunol. 2004;114:155–212. doi: 10.1016/j.jaci.2004.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hamilos DL. Chronic rhinosinusitis patterns of illness. Clin Allergy Immunol. 2007;20:1–13. [PubMed] [Google Scholar]
- 3.Bachert C, Gevaert P, van Cauwenberge P. Staphylococcus aureus superantigens and airway disease. Curr Allergy Asthma Rep. 2002;2:252–258. doi: 10.1007/s11882-002-0027-9. [DOI] [PubMed] [Google Scholar]
- 4.Shin SH, Ponikau JU, Sherris DA, Congdon D, Frigas E, Homburger HA, et al. Chronic rhinosinusitis: an enhanced immune response to ubiquitous airborne fungi. J Allergy Clin Immunol. 2004;114:1369–1375. doi: 10.1016/j.jaci.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 5.Stoop AE, van der Heijden HA, Biewenga J, van der Baan S. Eosinophils in nasal polyps and nasal mucosa: an immunohistochemical study. J Allergy Clin Immunol. 1993;91:616–622. doi: 10.1016/0091-6749(93)90267-j. [DOI] [PubMed] [Google Scholar]
- 6.Bachert C, Wagenmann M, Hauser U, Rudack C. IL-5 synthesis is upregulated in human nasal polyp tissue. J Allergy Clin Immunol. 1997;99:837–842. doi: 10.1016/s0091-6749(97)80019-x. [DOI] [PubMed] [Google Scholar]
- 7.Olze H, Forster U, Zuberbier T, Morawietz L, Luger EO. Eosinophilic nasal polyps are a rich source of eotaxin, eotaxin-2 and eotaxin-3. Rhinology. 2006;44:145–150. [PubMed] [Google Scholar]
- 8.Van Zele T, Claeys S, Gevaert P, Van Maele G, Holtappels G, Van Cauwenberge P, et al. Differentiation of chronic sinus diseases by measurement of inflammatory mediators. Allergy. 2006;61:1280–1289. doi: 10.1111/j.1398-9995.2006.01225.x. [DOI] [PubMed] [Google Scholar]
- 9.Takhar P, Smurthwaite L, Coker HA, Fear DJ, Banfield GK, Carr VA, et al. Allergen drives class switching to IgE in the nasal mucosa in allergic rhinitis. J Immunol. 2005;174:5024–5032. doi: 10.4049/jimmunol.174.8.5024. [DOI] [PubMed] [Google Scholar]
- 10.Nakajima S, Gillespie DN, Gleich GJ. Differences between IgA and IgE as secretory proteins. Clin Exp Immunol. 1975;21:306–317. [PMC free article] [PubMed] [Google Scholar]
- 11.Merrett TG, Houri M, Mayer AL, Merrett J. Measurement of specific IgE antibodies in nasal secretion: evidence for local production. Clin Allergy. 1976;6:69–73. doi: 10.1111/j.1365-2222.1976.tb01413.x. [DOI] [PubMed] [Google Scholar]
- 12.Small P, Barrett D, Frenkiel S, Rochon L, Cohen C, Black M. Local specific IgE production in nasal polyps associated with negative skin tests and serum RAST. Ann Allergy. 1985;55:736–739. [PubMed] [Google Scholar]
- 13.Shatkin JS, Delsupehe KG, Thisted RA, Corey JP. Mucosal allergy in the absence of systemic allergy in nasal polyposis and rhinitis: a meta-analysis. Otolaryngol Head Neck Surg. 1994;111:553–556. doi: 10.1177/019459989411100503. [DOI] [PubMed] [Google Scholar]
- 14.Takhar P, Corrigan CJ, Smurthwaite L, O'Connor BJ, Durham SR, Lee TH, et al. Class switch recombination to IgE in the bronchial mucosa of atopic and nonatopic patients with asthma. J Allergy Clin Immunol. 2007;119:213–218. doi: 10.1016/j.jaci.2006.09.045. [DOI] [PubMed] [Google Scholar]
- 15.Van Zele T, Gevaert P, Watelet JB, Claeys G, Holtappels G, Claeys C, et al. Staphylococcus aureus colonization and IgE antibody formation to enterotoxins is increased in nasal polyposis. J Allergy Clin Immunol. 2004;114:981–983. doi: 10.1016/j.jaci.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 16.Polzehl D, Moeller P, Riechelmann H, Perner S. Distinct features of chronic rhino-sinusitis with and without nasal polyps. Allergy. 2006;61:1275–1279. doi: 10.1111/j.1398-9995.2006.01132.x. [DOI] [PubMed] [Google Scholar]
- 17.Schneider P, MacKay F, Steiner V, Hofmann K, Bodmer JL, Holler N, et al. BAFF, a novel ligand of the tumor necrosis factor family, stimulates B cell growth. J Exp Med. 1999;189:1747–1756. doi: 10.1084/jem.189.11.1747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hahne M, Kataoka T, Schroter M, Hofmann K, Irmler M, Bodmer JL, et al. APRIL, a new ligand of the tumor necrosis factor family, stimulates tumor cell growth. J Exp Med. 1998;188:1185–1190. doi: 10.1084/jem.188.6.1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mackay F, Silveira PA, Brink R. B cells and the BAFF/APRIL axis: fast-forward on autoimmunity and signaling. Curr Opin Immunol. 2007;19:327–336. doi: 10.1016/j.coi.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 20.Litinskiy MB, Nardelli B, Hilbert DM, He B, Schaffer A, Casali P, et al. DCs induce CD40-independent immunoglobulin class switching through BLyS and APRIL. Nat Immunol. 2002;3:822–829. doi: 10.1038/ni829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu W, He B, Chiu A, Chadburn A, Shan M, Buldys M, et al. Epithelial cells trigger frontline immunoglobulin class switching through a pathway regulated by the inhibitor SLPI. Nat Immunol. 2007;8:294–303. doi: 10.1038/ni1434. [DOI] [PubMed] [Google Scholar]
- 22.He B, Xu W, Santini PA, Polydorides AD, Chiu A, Estrella J, et al. Intestinal bacteria trigger T cell-independent immunoglobulin A(2) class switching by inducing epithelial-cell secretion of the cytokine APRIL. Immunity. 2007;26:812–826. doi: 10.1016/j.immuni.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 23.Castigli E, Wilson SA, Scott S, Dedeoglu F, Xu S, Lam KP, et al. TACI and BAFFR mediate isotype switching in B cells. J Exp Med. 2005;201:35–39. doi: 10.1084/jem.20032000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Castigli E, Wilson SA, Garibyan L, Rachid R, Bonilla F, Schneider L, et al. TACI is mutant in common variable immunodeficiency and IgA deficiency. Nat Genet. 2005;37:829–834. doi: 10.1038/ng1601. [DOI] [PubMed] [Google Scholar]
- 25.Kato A, Truong-Tran AQ, Scott AL, Matsumoto K, Schleimer RP. Airway epithelial cells produce B cell-activating factor of TNF family by an IFN-beta-dependent mechanism. J Immunol. 2006;177:7164–7172. doi: 10.4049/jimmunol.177.10.7164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim J, Myers AC, Chen L, Pardoll DM, Truong-Tran QA, Lane AP, et al. Constitutive and inducible expression of B7 family of ligands by human airway epithelial cells. Am J Respir Cell Mol Biol. 2005;33:280–289. doi: 10.1165/rcmb.2004-0129OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lane AP, Truong-Tran QA, Schleimer RP. Altered expression of genes associated with innate immunity and inflammation in recalcitrant rhinosinusitis with polyps. Am J Rhinol. 2006;20:138–144. [PMC free article] [PubMed] [Google Scholar]
- 28.Thomas G. Furin at the cutting edge: from protein traffic to embryogenesis and disease. Nat Rev Mol Cell Biol. 2002;3:753–766. doi: 10.1038/nrm934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sedgwick JB, Calhoun WJ, Vrtis RF, Bates ME, McAllister PK, Busse WW. Comparison of airway and blood eosinophil function after in vivo antigen challenge. J Immunol. 1992;149:3710–3718. [PubMed] [Google Scholar]
- 30.Kroegel C, Liu MC, Hubbard WC, Lichtenstein LM, Bochner BS. Blood and bronchoalveolar eosinophils in allergic subjects after segmental antigen challenge: surface phenotype, density heterogeneity, and prostanoid production. J Allergy Clin Immunol. 1994;93:725–734. doi: 10.1016/0091-6749(94)90252-6. [DOI] [PubMed] [Google Scholar]
- 31.Leckie MJ, ten Brinke A, Khan J, Diamant Z, O'Connor BJ, Walls CM, et al. Effects of an interleukin-5 blocking monoclonal antibody on eosinophils, airway hyper-responsiveness, and the late asthmatic response. Lancet. 2000;356:2144–2148. doi: 10.1016/s0140-6736(00)03496-6. [DOI] [PubMed] [Google Scholar]
- 32.Liu LY, Sedgwick JB, Bates ME, Vrtis RF, Gern JE, Kita H, et al. Decreased expression of membrane IL-5 receptor alpha on human eosinophils, II: IL-5 down-modulates its receptor via a proteinase-mediated process. J Immunol. 2002;169:6459–6466. doi: 10.4049/jimmunol.169.11.6459. [DOI] [PubMed] [Google Scholar]
- 33.Huard B, Arlettaz L, Ambrose C, Kindler V, Mauri D, Roosnek E, et al. BAFF production by antigen-presenting cells provides T cell co-stimulation. Int Immunol. 2004;16:467–475. doi: 10.1093/intimm/dxh043. [DOI] [PubMed] [Google Scholar]
- 34.Yoshimoto K, Takahashi Y, Ogasawara M, Setoyama Y, Suzuki K, Tsuzaka K, et al. Aberrant expression of BAFF in T cells of systemic lupus erythematosus, which is recapitulated by a human T cell line, Loucy. Int Immunol. 2006;18:1189–1196. doi: 10.1093/intimm/dxl053. [DOI] [PubMed] [Google Scholar]
- 35.Daridon C, Devauchelle V, Hutin P, Le Berre R, Martins-Carvalho C, Bendaoud B, et al. Aberrant expression of BAFF by B lymphocytes infiltrating the salivary glands of patients with primary Sjogren's syndrome. Arthritis Rheum. 2007;56:1134–1144. doi: 10.1002/art.22458. [DOI] [PubMed] [Google Scholar]
- 36.Darce JR, Arendt BK, Chang SK, Jelinek DF. Divergent effects of BAFF on human memory B cell differentiation into Ig-secreting cells. J Immunol. 2007;178:5612–5622. doi: 10.4049/jimmunol.178.9.5612. [DOI] [PubMed] [Google Scholar]
- 37.Gewirtz AT, Navas TA, Lyons S, Godowski PJ, Madara JL. Cutting edge: bacterial flagellin activates basolaterally expressed TLR5 to induce epithelial proinflammatory gene expression. J Immunol. 2001;167:1882–1885. doi: 10.4049/jimmunol.167.4.1882. [DOI] [PubMed] [Google Scholar]
- 38.Sha Q, Truong-Tran AQ, Plitt JR, Beck LA, Schleimer RP. Activation of airway epithelial cells by toll-like receptor agonists. Am J Respir Cell Mol Biol. 2004;31:358–364. doi: 10.1165/rcmb.2003-0388OC. [DOI] [PubMed] [Google Scholar]
- 39.Homma T, Kato A, Hashimoto N, Batchelor J, Yoshikawa M, Imai S, et al. Corticosteroid and cytokines synergistically enhance toll-like receptor 2 expression in respiratory epithelial cells. Am J Respir Cell Mol Biol. 2004;31:463–469. doi: 10.1165/rcmb.2004-0161OC. [DOI] [PubMed] [Google Scholar]
- 40.Kato A, Schleimer RP. Beyond inflammation: airway epithelial cells are at the interface of innate and adaptive immunity. Curr Opin Immunol. 2007;19:711–720. doi: 10.1016/j.coi.2007.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hamilos DL, Leung DY, Wood R, Meyers A, Stephens JK, Barkans J, et al. Chronic hyperplastic sinusitis: association of tissue eosinophilia with mRNA expression of granulocyte-macrophage colony-stimulating factor and interleukin-3. J Allergy Clin Immunol. 1993;92:39–48. doi: 10.1016/0091-6749(93)90035-e. [DOI] [PubMed] [Google Scholar]
- 42.Beck LA, Stellato C, Beall LD, Schall TJ, Leopold D, Bickel CA, et al. Detection of the chemokine RANTES and endothelial adhesion molecules in nasal polyps. J Allergy Clin Immunol. 1996;98:766–780. doi: 10.1016/s0091-6749(96)70126-4. [DOI] [PubMed] [Google Scholar]
- 43.Jahnsen FL, Haraldsen G, Aanesen JP, Haye R, Brandtzaeg P. Eosinophil infiltration is related to increased expression of vascular cell adhesion molecule-1 in nasal polyps. Am J Respir Cell Mol Biol. 1995;12:624–632. doi: 10.1165/ajrcmb.12.6.7539273. [DOI] [PubMed] [Google Scholar]
- 44.Symon FA, Walsh GM, Watson SR, Wardlaw AJ. Eosinophil adhesion to nasal polyp endothelium is P-selectin-dependent. J Exp Med. 1994;180:371–376. doi: 10.1084/jem.180.1.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Simon HU, Yousefi S, Schranz C, Schapowal A, Bachert C, Blaser K. Direct demonstration of delayed eosinophil apoptosis as a mechanism causing tissue eosinophilia. J Immunol. 1997;158:3902–3908. [PubMed] [Google Scholar]
- 46.Diaz-Sanchez D, Dotson AR, Takenaka H, Saxon A. Diesel exhaust particles induce local IgE production in vivo and alter the pattern of IgE messenger RNA isoforms. J Clin Invest. 1994;94:1417–1425. doi: 10.1172/JCI117478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cameron L, Hamid Q, Wright E, Nakamura Y, Christodoulopoulos P, Muro S, et al. Local synthesis of epsilon germline gene transcripts, IL-4, and IL-13 in allergic nasal mucosa after ex vivo allergen exposure. J Allergy Clin Immunol. 2000;106:46–52. doi: 10.1067/mai.2000.107398. [DOI] [PubMed] [Google Scholar]
- 48.Van Zele T, Gevaert P, Holtappels G, van Cauwenberge P, Bachert C. Local immunoglobulin production in nasal polyposis is modulated by superantigens. Clin Exp Allergy. 2007;37:1840–1847. doi: 10.1111/j.1365-2222.2007.02838.x. [DOI] [PubMed] [Google Scholar]
- 49.Zhang N, Holtappels G, Claeys C, Huang G, van Cauwenberge P, Bachert C. Pattern of inflammation and impact of Staphylococcus aureus enterotoxins in nasal polyps from southern China. Am J Rhinol. 2006;20:445–450. doi: 10.2500/ajr.2006.20.2887. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.