Abstract
Objective
To compare the estimated prevalence of malnutrition using the World Health Organization’s (WHO) child growth standards versus the National Center for Health Statistics’ (NCHS) growth reference, to examine the relationship between exclusive breastfeeding and malnutrition, and to determine the sensitivity and specificity of nutritional status indicators for predicting death during infancy.
Methods
A secondary analysis of data on 9424 mother–infant pairs in Ghana, India and Peru was conducted. Mothers and infants were enrolled in a trial of vitamin A supplementation during which the infants’ weight, length and feeding practices were assessed regularly. Malnutrition indicators were determined using WHO and NCHS growth standards.
Findings
The prevalence of stunting, wasting and underweight in infants aged < 6 months was higher with WHO than NCHS standards. However, the prevalence of underweight in infants aged 6–12 months was much lower with WHO standards. The duration of exclusive breastfeeding was not associated with malnutrition in the first 6 months of life. In infants aged < 6 months, severe underweight at the first immunization visit as determined using WHO standards had the highest sensitivity (70.2%) and specificity (85.8%) for predicting mortality in India. No indicator was a good predictor in Ghana or Peru. In infants aged 6–12 months, underweight at 6 months had the highest sensitivity and specificity for predicting mortality in Ghana (37.0% and 82.2%, respectively) and Peru (33.3% and 97.9% respectively), while wasting was the best predictor in India (sensitivity: 54.6%; specificity: 85.5%).
Conclusion
Malnutrition indicators determined using WHO standards were better predictors of mortality than those determined using NCHS standards. No association was found between breastfeeding duration and malnutrition at 6 months. Use of WHO child growth standards highlighted the importance of malnutrition in the first 6 months of life.
Résumé
Objectif
Comparer l’estimation de la prévalence de la malnutrition obtenue à partir des normes OMS de croissance de l’enfant avec celle déterminée à partir des valeurs de référence du National Center for Health Statistics (NCHS) en vue d’étudier la relation entre l’allaitement maternel exclusif et la malnutrition et de déterminer la sensibilité et la spécificité des indicateurs d’état nutritionnel dans la prédiction de la mortalité pendant la petite enfance.
Méthodes
Une analyse secondaire des données relatives à 9424 couples mère-enfant a été réalisée au Ghana, en Inde et au Pérou. Des nourrissons et leurs mères ont été recrutés pour participer à un essai de supplémentation en vitamine A, dans le cadre duquel on a évalué régulièrement leur poids, leur taille et leur mode d’alimentation. Les indicateurs de malnutrition ont été déterminés à l’aide des normes de croissance OMS et NCHS.
Résultats
La prévalence du retard de croissance, de l’émaciation et du déficit pondéral chez les nourrissons de moins de 6 mois obtenue avec les normes OMS était supérieure à celle fournie par les normes NCHS. Toutefois, les normes OMS donnaient une valeur nettement plus faible de la prévalence du déficit pondéral chez les enfants de 6 à 12 mois. On n’a pas relevé d’association entre la durée de l’allaitement maternel exclusif et la malnutrition pendant les 6 premiers mois de vie. Chez les nourrissons de moins de 6 mois, la présence d’un déficit pondéral sévère selon les normes OMS lors de la première visite de vaccination était l’indicateur le plus sensible (70,2 %) et le plus spécifique (85,8 %) pour prédire la mortalité en Inde. Aucun indicateur n’a présenté une grande valeur prédictive au Ghana et au Pérou. C’est le déficit pondéral à 6 mois chez les nourrissons de 6 à 12 mois, qui offrait les plus grandes sensibilité et spécificité dans la prédiction de la mortalité au Ghana (37,0 % et 82,2 %, respectivement) et au Pérou (33,3 % et 97,9 %, respectivement), tandis que l’émaciation constituait le meilleur facteur de prédiction en Inde (sensibilité : 54,6 %, spécificité : 85,5 %).
Conclusion
Les indicateurs de malnutrition déterminés en utilisant les normes OMS présentent une meilleure valeur prédictive pour la mortalité que ceux obtenus avec les normes NCHS. Aucune association n’a été relevée entre la durée de l’allaitement au sein et la malnutrition à 6 mois. L’application des normes OMS de croissance de l’enfant fait ressortir l’importance de la malnutrition pendant les 6 premiers mois de vie.
Resumen
Objetivo
Comparar la prevalencia estimada de malnutrición basada en los patrones de crecimiento infantil de la OMS con la basada en los patrones de crecimiento del National Center for Health Statistics (NCHS), estudiar la relación entre lactancia materna exclusiva y malnutrición y determinar la sensibilidad y especificidad de los indicadores del estado nutricional para predecir la mortalidad durante la lactancia.
Métodos
Se llevó a cabo un análisis secundario de datos relativos a 9424 pares de madre y lactante de Ghana, la India y el Perú. Madres y lactantes participaron en un ensayo de administración de suplementos de vitamina A en el que se evaluaron periódicamente el peso, la talla y las prácticas de alimentación de los lactantes. Los indicadores de malnutrición se determinaron aplicando los patrones de crecimiento de la OMS y del NCHS.
Resultados
La prevalencia de retraso del crecimiento, emaciación e insuficiencia ponderal en lactantes de menos de 6 meses fue mayor con los patrones de la OMS que con los del NCHS; sin embargo, la prevalencia de peso inferior al normal en los lactantes de 6 a 12 meses fue mucho menor al aplicar los patrones de la OMS. La duración de la lactancia materna exclusiva no se asoció a malnutrición en los seis primeros meses de vida. En los lactantes de menos de 6 meses, la detección de insuficiencia ponderal grave con los patrones de la OMS en la primera visita de inmunización fue la variable con mayor sensibilidad (70,2%) y especificidad (85,8%) para predecir la mortalidad en la India. Ningún indicador fue un buen factor predictivo en Ghana o el Perú. En los lactantes de 6 a 12 meses, el peso inferior al normal a los 6 meses mostró la máxima sensibilidad y especificidad para predecir la mortalidad en Ghana (37,0% y 82,2%, respectivamente) y el Perú (33,3% y 97,9% respectivamente), mientras que la emaciación fue el mejor factor predictivo en la India (sensibilidad: 54,6%; especificidad: 85,5%).
Conclusión
Los indicadores de malnutrición determinados mediante los patrones de la OMS fueron mejores factores predictivos de la mortalidad que los determinados mediante los patrones del NCHS. No se halló ninguna relación entre la duración de la lactancia materna y la malnutrición a los 6 meses. El uso de los patrones de crecimiento infantil de la OMS puso de relieve la importancia de la malnutrición en los 6 primeros meses de vida.
ملخص
الغرض
مقارنة المعدل التقديري لانتشار سوء التغذية باستخدام المعايير الجديدة لنمو الطفل لمنظمة الصحة العالمية بمعايير النمو المرجعي للمركز الوطني للإحصائيات الصحية، لاستبيان العلاقة بين الرضاعة المقتصرة على الثدي وسوء التغذية، وتحديد حساسية ونوعية مؤشرات الحالة الغذائية في توقع الوفاة أثناء سن الرضاعة.
الطريقة
أُجري تحليل ثانوي للبيانات الخاصة بـ 9424 زوجاً من الأمهات وأطفالهن الرضّع في غانا، والهند، وبيرو. وأُدرجت الأمهات وأطفالهن الرضّع في تجربة لإضافة فيتامين (أ) مع قياس الوزن والطول والممارسات الغذائية للرضع بانتظام. وجرى تحديد مؤشرات سوء التغذية باستخدام كل من معايير النمو الخاصة بمنظمة الصحة العالمية والمركز الوطني للإحصائيات الصحية.
الموجودات
كان انتشار قصر القامة، والهزال، ونقص الوزن بين الرضّع في عمر أقل من 6 شهور أعلى بمعايير منظمة الصحة العالمية مقارنة بمعايير المركز الوطني للإحصائيات الصحية، إلا أن انتشار نقص الوزن بين الرضّع في عمر 6-12 شهراً كان أقل كثيراً بمعايير منظمة الصحة العالمية. ولم ترتبط مدة الرضاعة المقتصرة على الثدي بسوء التغذية خلال الشهور الستة الأولى من العمر. وكان سوء التغذية الوخيم الذي جرى تحديده بمعايير منظمة الصحة العالمية في الرضّع أقل من عمر 6 شهور أثناء أول زيارة للتمنيع أعلى في توقع الوفيات في الهند من حيث الحساسية (70.2%) والنوعية (85.8%). ولم يكن هناك مؤشر جيد للتوقع في غانا أو بيرو. وفي الأطفال في الفئة العمرية 6-12 شهراً، كان سوء التغذية في عمر 6 شهور أعلى حساسية ونوعية في توقع الوفيات في غانا (37.0% و 82.2% بالترتيب) وفي بيرو (33.3% و 97.9% بالترتيب)، بينما كان الهزال أفضل منبئ في الهند (الحساسية: 54.6%؛ والنوعية: 85.5%).
الاستنتاج
إن تحديد مؤشرات سوء التغذية باستخدام معايير منظمة الصحة العالمية كان أفضل منبئ للوفيات مقارنة بمعايير المركز الوطني للإحصائيات الصحية. ولم يوجد ارتباط بين مدة الرضاعة من الثدي وسوء التغذية في عمر 6 شهور. وأظهر استخدام معايير نمو الطفل لمنظمة الصحة العالمية أهمية سوء التغذية في الشهور الستة الأولى من العمر.
Introduction
Malnutrition contributes to about one-third of the 9.7 million child deaths that occur each year.1,2 Recently, the World Health Organization (WHO) introduced new child growth standards for use in deriving indicators of nutritional status, such as stunting, wasting and underweight. These standards are based on the growth of infants from six different regions of the world who were fed according to WHO and United Nations Children’s Fund (UNICEF) feeding recommendations, had a non-smoking mother, had access to primary health care and did not have any serious constraints on health during infancy or early childhood.3–6 It is recommended that these new growth standards replace the previously recommended international growth reference devised by the National Center for Health Statistics (NCHS) in the United States.7
The prevalence of malnutrition estimated using WHO standards is expected to differ from that based on the NCHS growth reference because there are differences in median weight-for-age, height-for-age and weight-for-height between the two.8 Recent studies have investigated the direction and magnitude of these differences.9–12 In children aged 6–59 months, the prevalence of stunting (i.e. low height-for-age) and wasting (i.e. low weight-for-height) were higher when WHO standards were used but that of underweight (i.e. low weight-for-age) was lower.9,11,12 In the first half of infancy (i.e. the period from birth up to the end of the 6th month), the prevalence of stunting, wasting and underweight has been reported to be higher with WHO growth standards.10,12 It is important that the magnitude of these apparent changes in the prevalence of malnutrition are investigated in different settings in order to gain a better understanding of their implications, particularly for child health and nutrition programmes whose progress is monitored through large household surveys.
Another important question connected with growth in the first 6 months of life is its relationship with feeding practices. Exclusive breastfeeding is recommended for infants up to 6 months of age because of its benefits in reducing morbidity and mortality.13 In their systematic review of the optimal duration of exclusive breastfeeding, Kramer and Kakuma14 combined the results of two studies conducted in Honduras and found that exclusively breastfed infants had a lower prevalence of stunting, wasting and underweight, although not significantly so.
Malnourished children are known to be at an increased risk of death.15–20 Nutritional status indicators can be used to identify those infants and children at a higher risk of dying so they can be provided with special care both at a population level in emergency settings and individually following screening. For example, low weight-for-age is used in the UNICEF–WHO Integrated Management of Childhood Illness (IMCI) programme to identify infants whose feeding practices should be assessed and who would benefit from additional counselling on infant feeding.21 It is not yet known whether nutritional status assessed using WHO growth standards or the NCHS growth reference would be a better predictor of death, and answering this question has been proposed as a research priority.12,22
We carried out a secondary analysis of a large data set obtained from a randomized controlled trial of vitamin A supplementation conducted in Ghana, India and Peru23 to determine how using the NCHS growth reference or WHO growth standards influences the calculated prevalence of malnutrition, the relationship between exclusive breastfeeding and malnutrition, and the sensitivity and specificity of nutritional status indicators for predicting the risk of death during infancy.
Methods
Data collection
Between 1995 and 1997, 9424 mother–infant pairs were enrolled in a randomized controlled trial of vitamin A supplementation linked to the WHO Expanded Programme on Immunization (EPI): 2919 mother–infant pairs were from 37 villages in the Kintampo district of Ghana, 4000 were from two urban slums in New Delhi, India, and 2505 were from a periurban shanty town in Lima, Peru. Child morbidity, mainly diarrhoea and respiratory infection, was high at all study sites. Breastfeeding was almost universal and more than 94% of infants were still consuming breast milk after 9 months. Full details of the original study are described elsewhere.23 In this paper, we present only the information essential for the secondary analysis.
Mothers and infants were enrolled 21–42 days after childbirth in Ghana and 18–28 days after childbirth in India and Peru. Information on each infant’s age, sex and breastfeeding status and on several family characteristics was collected by fieldworkers, who visited participants’ homes after enrolment.23
During the first follow-up visit at 6 weeks in Ghana and India and at 10 weeks in Peru, the first doses of diphtheria, tetanus and pertussis vaccine and oral poliomyelitis vaccine were administered and the infants’ weight and length were measured. Weights and lengths were also measured when the infants were 6, 9 and 12 months of age. However, of the 9424 enrolled infants, 983 from either Ghana or Peru were followed up only to 6 months of age to enable the study to be completed in the intended time period.23 Standard procedures were followed for measuring weight and length. Field workers were extensively trained and standardization exercises were conducted before data collection to ensure high levels of reproducibility and validity. Length measurements were taken three times and the median was used to calculate the z-score, which is the number of standard deviations an observation is above or below the mean. Weight was measured only once. A length board with a sliding foot scale and a precision of 0.1 cm was used to measure length and a hanging spring scale accurate to 100 g and calibrated daily was used to measure weight.
Information on each infant’s vital status and feeding mode was collected at follow-up visits which took place every 4 weeks until the infant was 12 months of age. Infants were divided into subgroups by feeding history using data collected at 6 (Ghana and India only), 10, 14, 18 and 22 weeks. At each visit, mothers were asked what they had offered their child to eat or drink during the past week. After the mother’s unprompted response was documented, she was asked whether she had offered her own breast milk, breast milk from a wet nurse, animal milk, infant formula, other fluids or solid food at any time during the week. An exclusively breastfed infant was one who received only breast milk from his mother or a wet nurse and who took no other liquids or solids, except vitamins, mineral supplements or medication.
The study was approved by the ethics review committees of all the participating institutions and by WHO’s ethics review board.23
Secondary data analysis
The nutritional survey option in WHO Anthro 2005 software (WHO, Geneva, Switzerland) for assessing growth and development was used to calculate weight-for-age, length-for-age and weight-for-length z-scores on the basis of both WHO standards and the NCHS growth reference. An infant was defined as stunted, wasted or underweight if his or her length-for-age, weight-for-length or weight-for-age z-score, respectively, was less than –2. Severe stunting, severe wasting or severe underweight corresponded to a length-for-age, weight-for-length or weight-for-age z-score, respectively, less than –3.
Weight and length measurements were considered valid at 6 or 10 weeks if measured within 2 weeks of the target date and valid at 6, 9 and 12 months if measured within 4 weeks of the target date. Data were checked to exclude extreme outliers (only one outlier from Ghana was excluded from the analysis) and missing or unknown values. The length of a small number of infants could not be measured, for example, because the parents refused permission or because of deformity. Consequently their length-for-age and weight-for-length could not be calculated. In addition, the weight-for-length of infants whose length was under a certain value (i.e. 49 cm for the NCHS growth reference and 45 cm for WHO standards) was not calculated. The analysis only included data on infants whose z-scores could be calculated using both the NCHS growth reference and WHO standards. Weight could not be adjusted for oedema as its presence was not recorded.
The duration of exclusive breastfeeding was defined as the age of the infant at the follow-up visit when exclusive breastfeeding was last reported. Detailed feeding information was available only after the first immunization visit, at 6 weeks in Ghana and India and at 10 weeks in Peru. We categorized the duration of exclusive breastfeeding as < 10 weeks, 10 to < 18 weeks or ≥ 18 weeks. The prevalences of malnutrition in infants aged 6 months in these three categories were compared using Cuzick’s nonparametric statistical test for the trend across ordered groups. Logistic regression analysis was used to adjust for potential confounding factors, which included the infant’s weight, age at enrolment, sex and birth order, the mother’s education, whether there was a multiple or single birth, and the death of a previous child from the same mother.
The risk of death among malnourished and adequately nourished infants was compared. The sensitivity and specificity of nutritional status indicators (i.e. stunting, wasting and underweight) at 6 weeks and 6 months for predicting death in the subsequent periods of 6 weeks to 6 months and 6 months to 12 months, respectively, were calculated. If a malnutrition indicator had a high sensitivity but a low specificity, we also calculated the sensitivity and specificity of the corresponding indicator of severe malnutrition. For example, as underweight had a high sensitivity and low specificity in India, we additionally calculated the sensitivity and specificity of severe underweight in the country.
The area under the receiver operating characteristic curve (AUC) and its 95% confidence interval (CI) were used to assess the performance of nutritional status indicators for identifying those at risk of death. An AUC of 0.5 means the indicator is no better than chance; the closer the AUC is to 1, the better the performance of the indicator.
The statistical analysis was performed using Intercooled Stata 8.0 (Stata Corp LP, College Station, TX, United States of America). Baseline characteristics and results are summarized by country.
Results
Baseline characteristics
For this secondary analysis, 8787 of the 9424 infants (93.2%) enrolled in the study were included at the first immunization visit, 7964 (84.5%) were included at 6 months and 5890 (62.5%), at 12 months. Fig. 1 summarizes the reasons for infants being lost to follow-up.
Fig. 1.
Number of infants included at different times in the study of infant malnutrition in Ghana, India and Peru, 1995–1997
a Of the 9424 infants overall, 983 from Ghana or Peru were followed up only to 6 months of age to enable the study to be completed in the intended time period.
The baseline characteristics of the mothers and infants enrolled in the randomized controlled trial and aspects of their living environment are summarized in Table 1. The sites in the three countries were similar with regard to the infants’ age at enrolment, sex and breastfeeding status. The proportion of twins was much higher in Ghana. Peru had the highest parental educational level and the lowest proportion of mothers who reported a previous child death, followed sequentially by India and Ghana.
Table 1. Baseline characteristics and aspects of the living environment of mothers and infants enrolled in the study of infant malnutrition in Ghana, India and Peru, 1995–1997.
| Characteristics | Ghana | India | Peru |
|---|---|---|---|
| (n = 2919) | (n = 4000) | (n = 2505) | |
| Mean age at enrolment in days (SD) | 24.8 (3.9) | 23.0 (2.5) | 22.8 (3.2) |
| No. of males (%) | 1438.0 (49.3) | 2068.0 (51.7) | 1274.0 (50.9) |
| No. of twins (%) | 123.0 (4.2) | 25.0 (0.6) | 34.0 (1.4) |
| No. breastfed in the 48 hours before enrolment (%) | 2906.0 (99.6) | 3948.0 (98.7) | 2494.0 (99.6) |
| Mean weight at enrolment in kg (SD) | 3.6 (0.6) | 3.2 (0.6) | 3.9 (0.5) |
| Median maternal education in years (IQR) | 0 (0 to 6.0) | 3.0 (0 to 8.0) | 8.0 (6 to 11.0) |
| Median paternal education in years (IQR) | 0 (0 to 10.0) | 8.0 (5 to 10.0) | 11.0 (8 to 11.0) |
| No. of mothers reporting a previous child death (%) | 1099.0 (37.6) | 730.0 (18.3) | 241.0 (9.6) |
| Mean total number of births including the enrolled child (SD) | 4.0 (2.5) | 2.8 (1.6) | 2.7 (1.7) |
| No. dwelling with a piped water source (%) | 2.0 (0.1) | 2190.0 (54.8) | 1349.0 (53.9) |
| No. of flush latrines as a place of defecation for the mother (%) | 3.0 (0.1) | 2932.0 (73.3) | 1066.0 (42.6) |
| No. with dirt, mud or clay flooring in the home (%) | 533.0 (18.3) | 173.0 (4.3) | 1397.0 (55.8) |
SD, standard deviation; IQR, interquartile range.
Prevalence of malnutrition
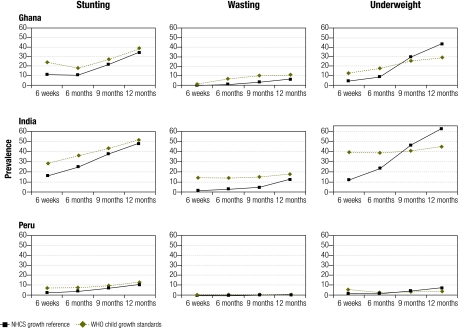
The prevalence of malnutrition in infancy was high, particularly in India and Ghana (Fig. 2). As expected, the prevalence of stunting, wasting and underweight in infants in the first half of infancy (i.e. before 6 months of age) was lower at all study sites when the NCHS growth reference was used. When infants were 1 year of age, the prevalence of stunting and wasting continued to be lower with the NCHS growth reference, while that of underweight was much higher. Consequently, there appeared to be a sharp increase in the prevalence of malnutrition during the second half of infancy when the NCHS growth reference was used. In contrast, a more gradual increase in the prevalence of malnutrition was observed throughout infancy when WHO standards were used (Fig. 2).
Fig. 2.
Prevalence of stunting, wasting and underweight in infants during the first year of life in Ghana, India and Peru as determined using WHO child growth standards and the NCHS growth reference, 1995–1997
NCHS, National Center for Health Statistics; WHO, World Health Organization.
There appeared to be an association between a longer duration of exclusive breastfeeding and a lower prevalence of malnutrition in 6-month-old infants at all study sites, particularly when judged by the proportion of underweight infants (Table 2). This association was no longer statistically significant for most indicators after adjustment for potential confounding factors, except for wasting in Peru determined using WHO standards and underweight in India determined using the NCHS growth reference.
Table 2. Duration of exclusive breastfeeding and prevalence of stunting, wasting and underweight in 6-month-old infants as determined using WHO child growth standards and the NCHS growth reference, Ghana, India and Peru, 1995–1997.
| Malnutrition indicator | Infants who received exclusive breastfeeding; n (%) |
Unadjusted P-value | Adjusted P-valuea | ||||
|---|---|---|---|---|---|---|---|
| < 10 weeks | 10 to < 18 weeks | ≥ 18 weeks | |||||
| WHO child growth standards | |||||||
| Ghanab | 1967 | 274 | 163 | ||||
| Stunted | 364 (18.5) | 42 (15.3) | 25 (15.3) | 0.144 | 0.481 | ||
| Wasted | 139 (7.1) | 16 (5.8) | 7 (4.3) | 0.135 | 0.268 | ||
| Underweight | 362 (18.4) | 37 (13.5) | 21 (12.9) | 0.015* | 0.057 | ||
| Indiac | 2870 | 408 | 185 | ||||
| Stunted | 1048 (36.6) | 138 (33.8) | 60 (32.4) | 0.132 | 0.421 | ||
| Wasted | 415 (14.5) | 65 (15.9) | 14 (7.6) | 0.096 | 0.152 | ||
| Underweight | 1119 (39.0) | 155 (38.0) | 58 (31.4) | 0.063 | 0.139 | ||
| Perud | 882 | 383 | 821 | ||||
| Stunted | 75 (8.5) | 29 (7.6) | 48 (5.9) | 0.035* | 0.424 | ||
| Wasted | 13 (1.5) | 2 (0.5) | 1 (0.1) | 0.006* | 0.031* | ||
| Underweight | 31 (3.5) | 7 (1.8) | 8 (1.0) | 0.001* | 0.052 | ||
| NCHS growth reference | |||||||
| Ghanab | 1967 | 274 | 163 | ||||
| Stunted | 218 (11.1) | 22 (8.0) | 12 (7.4) | 0.049* | 0.210 | ||
| Wasted | 14 (0.7) | 2 (0.7) | 2 (1.2) | 0.535 | 0.312 | ||
| Underweight | 180 (9.2) | 20 (7.3) | 9 (5.5) | 0.073 | 0.269 | ||
| Indiac | 2870 | 408 | 185 | ||||
| Stunted | 730 (25.5) | 97 (23.8) | 41 (22.2) | 0.224 | 0.733 | ||
| Wasted | 78 (2.7) | 8 (2.0) | 3 (2.6) | 0.225 | 0.266 | ||
| Underweight | 688 (24.0) | 94 (23.0) | 28 (15.1) | 0.016* | 0.045* | ||
| Perud | 882 | 383 | 821 | ||||
| Stunted | 36 (4.1) | 14 (3.7) | 26 (3.2) | 0.311 | 0.192 | ||
| Wasted | 2 (0.2) | 0 (0.0) | 0 (0.0) | 0.13 | – | ||
| Underweight | 14 (1.6) | 2 (0.5) | 4 (0.5) | 0.026* | 0.268 | ||
* P < 0.05. NCHS, National Center for Health Statistics; WHO, World Health Organization. a Adjusted for mother’s education, previous child deaths, birth order, infant’s sex, multiple or single birth, and infant’s age and weight at enrolment. b Stunting could not be assessed for 2 infants and wasting could not be assessed for 4 infants in Ghana. c Stunting could not be assessed for 8 infants and wasting could not be assessed for 8 infants in India. d Stunting could not be assessed for 6 infants and wasting could not be assessed for 6 infants in Peru.
Prediction of infant mortality
The relationship between malnutrition at the first immunization visit (at 6 weeks in Ghana and India and 10 weeks in Peru) and the risk of death between then and the age of 6 months is presented in Table 3. The presence of stunting, wasting or underweight, as determined using WHO child growth standards or the NCHS growth reference, did not identify infants at risk of death in either Ghana or Peru. However, in India, malnutrition at 6 weeks of age was associated with an increased risk of death before 6 months of age, and the indicator that had the best performance was severe underweight determined using the WHO child growth standard (sensitivity: 70.2%; specificity: 85.8%; AUC: 0.78, 95% CI: 0.72–0.84), followed by underweight determined using the NCHS reference chart.
Table 3. Infant malnutrition at the first immunization visita as a predictor of death between then and 6 months of age, Ghana, India and Peru, 1995–1997.
| Malnutrition indicator at first immunization visitb | No. of deaths |
Sensitivity | Specificity | AUC (95% CI) | |||
|---|---|---|---|---|---|---|---|
| among malnourished | among non-malnourished | ||||||
| Ghana (n = 2637) | |||||||
| WHO child growth standards | |||||||
| Stuntingc | 9 of 627 | 21 of 2007 | 30.0 | 76.3 | 0.53 (0.45–0.62) | ||
| Wastingd | 0 of 21 | 29 of 2587 | 0.0 | 98.9 | 0.50 (0.49–0.50) | ||
| Underweight | 7 of 331 | 23 of 2306 | 23.3 | 87.6 | 0.55 (0.48–0.63) | ||
| NCHS growth reference | |||||||
| Stuntingc | 5 of 288 | 25 of 2346 | 16.7 | 89.1 | 0.53 (0.46–0.60) | ||
| Wastingd | 0 of 3 | 27 of 2523 | 0.0 | 99.9 | 0.50 (0.50–0.50) | ||
| Underweight | 3 of 99 | 27 of 2538 | 10.0 | 96.3 | 0.53 (0.48–0.58) | ||
| India (n = 3718) | |||||||
| WHO child growth standards | |||||||
| Stuntingc | 31 of 1 049 | 16 of 2638 | 66.0 | 72.0 | 0.69 (0.62–0.76) | ||
| Wastingd | 23 of 486 | 22 of 3114 | 51.1 | 85.0 | 0.65 (0.56–0.74) | ||
| Underweight | 47 of 1458 | 10 of 2260 | 82.5 | 61.5 | 0.72 (0.67–0.77) | ||
| Severe underweighte | 40 of 561 | 17 of 3157 | 70.2 | 85.8 | 0.78 (0.72–0.84) | ||
| NCHS growth reference | |||||||
| Stuntingc | 24 of 599 | 23 of 3088 | 51.1 | 84.2 | 0.68 (0.60–0.75) | ||
| Wastingd | 7 of 50 | 23 of 3426 | 23.3 | 98.8 | 0.61 (0.53–0.69) | ||
| Underweight | 37 of 446 | 20 of 3272 | 64.9 | 88.8 | 0.77 (0.7–0.83) | ||
| Peru (n = 2251) | |||||||
| WHO child growth standards | |||||||
| Stuntingc | 1 of 149 | 12 of 2098 | 7.7 | 93.4 | 0.51 (0.43–0.58) | ||
| Wastingd | 0 of 16 | 13 of 2230 | 0.0 | 99.2 | 0.5 (0.5–0.5) | ||
| Underweight | 1 of 112 | 12 of 2139 | 7.7 | 95.0 | 0.51 (0.44–0.59) | ||
| NCHS growth reference | |||||||
| Stuntingc | 0 of 46 | 13 of 2201 | 0.0 | 97.9 | 0.49 (0.49–0.49) | ||
| Wastingd | 0 of 0 | 13 of 2241 | 0.0 | 100.0 | 0.5 (0.5–0.5) | ||
| Underweight | 0 of 21 | 13 of 2230 | 0.0 | 99.1 | 0.5 (0.49–0.5) | ||
AUC, area under the receiver operating characteristic curve; CI, confidence interval; NCHS, National Center for Health Statistics; WHO, World Health Organization. a The first immunization visit took place at 6 weeks in Ghana and India and at 10 weeks in Peru. b Malnutrition indicators were determined using either WHO child growth standards or the NCHS growth reference. c Stunting could not be assessed for 3, 31 and 4 infants in Ghana, India and Peru, respectively. d Wasting could not be assessed for 29, 118 and 5 infants in Ghana, India and Peru, respectively. e Figures for the severe malnutrition indicator were calculated only when the malnutrition indicator had a high sensitivity and a low specificity.
The relationship between infant malnutrition at 6 months of age and the risk of death between 6 and 12 months of age is presented in Table 4. In Ghana, being underweight at 6 months of age as determined using WHO child growth standards had the highest sensitivity and specificity for death: 37.0% and 82.2%, respectively, with an AUC of 0.60 (95% CI: 0.50–0.69). In Peru, the same indicator was the most predictive (sensitivity: 33.3%; specificity: 97.9%; AUC: 0.66, 95% CI: 0.45–0.86). In India, wasting at 6 months as determined using WHO child growth standards gave the best performance (sensitivity: 54.6%; specificity: 85.5%; AUC: 0.70, 95% CI: 0.61–0.79), closely followed by severe underweight as determined using WHO child growth standards (sensitivity: 50.0%; specificity: 86.3%; AUC: 0.68, 95% CI: 0.60–0.77) and underweight determined using the NCHS growth reference (sensitivity: 58.8%; specificity: 76.6%; AUC: 0.68, 95% CI: 0.59–0.76).
Table 4. Infant malnutrition at 6 months of age as a predictor of death between 6 and 12 months of age, Ghana, India and Peru, 1995–1997.
| Malnutrition indicator at 6 months of agea | No. of deaths |
Sensitivity | Specificity | AUC (95% CI) | |||
|---|---|---|---|---|---|---|---|
| among malnourished | among non-malnourished | ||||||
| Ghana (n = 1558) | |||||||
| WHO child growth standards | |||||||
| Stuntingb | 8 of 274 | 19 of 1282 | 29.6 | 82.6 | 0.56 (0.47–0.65) | ||
| Wastingc | 5 of 113 | 22 of 1441 | 18.5 | 92.9 | 0.56 (0.48–0.63) | ||
| Underweight | 10 of 283 | 17 of 1275 | 37.0 | 82.2 | 0.60 (0.50–0.69) | ||
| NCHS growth reference | |||||||
| Stuntingb | 7 of 153 | 20 of 1403 | 25.9 | 90.5 | 0.58 (0.50–0.67) | ||
| Wastingc | 0 of 14 | 27 of 1540 | 0.0 | 99.1 | 0.5 (0.49–0.50) | ||
| Underweight | 5 of 144 | 22 of 1414 | 18.5 | 90.9 | 0.55 (0.47–0.62) | ||
| India (n = 1702) | |||||||
| WHO child growth standards | |||||||
| Stuntingb | 19 of 631 | 14 of 1065 | 57.6 | 63.2 | 0.60 (0.52–0.69) | ||
| Wastingc | 18 of 260 | 15 of 1436 | 54.6 | 85.5 | 0.70 (0.61–0.79) | ||
| Underweight | 22 of 660 | 12 of 1042 | 64.7 | 61.8 | 0.63 (0.55–0.71) | ||
| Severe underweightd | 17 of 246 | 17 of 1456 | 50.0 | 86.3 | 0.68 (0.60–0.77) | ||
| NCHS growth reference | |||||||
| Stuntingb | 18 of 443 | 15 of 1253 | 54.6 | 74.4 | 0.64 (0.56–0.73) | ||
| Wastingc | 8 of 53 | 25 of 1643 | 24.2 | 97.3 | 0.61 (0.53–0.68) | ||
| Underweight | 20 of 410 | 14 of 1292 | 58.8 | 76.6 | 0.68 (0.59–0.76) | ||
| Peru (n = 1734) | |||||||
| WHO child growth standards | |||||||
| Stuntingb | 2 of 129 | 4 of 1599 | 33.3 | 92.6 | 0.63 (0.42–0.84) | ||
| Wastingc | 1 of 13 | 5 of 1715 | 16.7 | 99.3 | 0.58 (0.42–0.74) | ||
| Underweight | 2 of 38 | 4 of 1696 | 33.3 | 97.9 | 0.66 (0.45–0.86) | ||
| NCHS growth reference | |||||||
| Stuntingb | 1 of 70 | 5 of 1658 | 16.7 | 96.0 | 0.56 (0.40–0.73) | ||
| Wastingc | 0 of 2 | 6 of 1726 | 0.0 | 99.9 | 0.50 (0.50–0.50) | ||
| Underweight | 1 of 14 | 5 of 1720 | 16.7 | 99.3 | 0.58 (0.42–0.74) | ||
AUC, area under the receiver operating characteristic curve; CI, confidence interval; NCHS, National Center for Health Statistics; WHO, World Health Organization. a Malnutrition indicators were derived using either WHO child growth standards or the NCHS growth reference. b Stunting could not be assessed for 2, 6 and 6 infants in Ghana, India and Peru, respectively. c Wasting could not be assessed for 4, 6 and 6 infants in Ghana, India and Peru, respectively. d Figures for the severe malnutrition indicator were calculated only when the malnutrition indicator had a high sensitivity and a low specificity.
Discussion
This analysis shows the prevalence of stunting, wasting and underweight in the first half of infancy was higher when determined using WHO child growth standards rather than the NCHS growth reference. In contrast, the prevalence of underweight was lower at 1 year of age. Nutritional status indicators determined using WHO standards were better predictors of mortality during infancy than those determined using the NCHS growth reference.
Our analysis was based on data collected on large samples taken from sites on three continents, namely Africa, Asia and Latin America. Well-standardized anthropometric measurements were available for a large proportion of enrolled infants at four time points during their first year of life. This analysis is the first to examine the relative merits of WHO child growth standards and the NCHS growth reference for predicting mortality during infancy.
The analysis has a number of potential limitations related to the characteristics of the study population and how they were followed up. Infants were not enrolled at birth and, therefore, birth weights and lengths were not available. While around 85% of the cohort was followed up to 6 months, the proportion fell to 63% at 12 months, largely because a shorter follow-up was planned. However, the baseline characteristics of those with a short follow-up did not differ from that of those who were followed up to 1 year of age (data not shown). In addition, the weight-for-length z-score at 6 weeks of age could not be estimated for infants whose length was too short (i.e. < 49 cm for the NCHS growth reference and < 45 cm for WHO standards). Because information on feeding involved 7-day recall at intervals of 4 weeks, it is possible that the feeding practices recorded may differ from those in the intervals between follow-up visits. Finally, the number of deaths in Peru was small, which makes it difficult to draw conclusions about the performance of the different malnutrition indicators in predicting subsequent mortality.
This analysis confirms the findings of previous studies10,12 which also showed that the prevalence of malnutrition during the first half of infancy was higher when WHO child growth standards rather than the NCHS growth reference were used and that the difference became less marked thereafter. At 1 year of age, the prevalence of wasting continued to be higher when WHO growth standards were used and the prevalence of stunting was similar, but the prevalence of underweight was lower. Thus, a gradual increase in the prevalence of malnutrition was observed throughout infancy when WHO standards were used, which contrasts with the steep rise in the prevalence observed after 6 months when the NCHS growth reference was used. The high prevalence of malnutrition in the first half of infancy observed using WHO standards is more consistent with the prevailing prevalence of low birth weight for the three study sites as calculated using available data:24 30% in India and 11% in Ghana and Peru.
The differences found in the prevalence of malnutrition are due to differences between the median growth curves derived using WHO standards and the NCHS growth reference. This can be explained by two characteristics of the WHO standards. First, they are based on the growth of breastfed infants only while the NCHS growth reference is based predominantly on the growth of formula-fed infants. Second, the WHO standards are based on more frequent measurements (i.e. every 2 weeks in the first 2 months and monthly thereafter) than the NCHS growth reference (i.e. every 3 months).8
The apparent association observed between the duration of exclusive breastfeeding and most nutritional status indicators at 6 months was not significant after adjustment for confounding factors. Although the association remained significant for two indicators, residual confounding cannot be ruled out. While exclusive breastfeeding has been associated with lower mortality and morbidity in previous studies,13 no clear association with a growth benefit has been reported.25
Anthropometric status, particularly underweight and wasting, has been shown to be a good predictor of subsequent mortality in previous studies.15,17–20 Our findings for the second half of infancy are consistent with these previous results. However, no such association was observed between the first immunization visit and 6 months of age in Ghana or Peru, which indicates that adequately nourished infants are exposed to other significant causes of death during this period in these countries. While there are clear guidelines for providing additional feeding counselling for underweight infants beyond 6 months of life, recommendations for underweight infants aged under 6 months are the same as those for the general population of infants, namely to promote exclusive breastfeeding.21
Malnutrition indicators calculated using WHO growth standards had higher AUCs, indicating that their performance may be better for predicting subsequent mortality than those calculated using the NCHS growth reference.
These findings have important implications. The higher prevalence of malnutrition between birth and 6 months of age found using the new WHO child growth standards challenges the traditionally held belief that malnutrition largely begins during the period of complementary feeding between 6 and 24 months of age. Our results add to the limited body of evidence on the relationship between the duration of exclusive breastfeeding and growth during the first 6 months of life. There appears to be little, if any, evidence in this study that exclusive breastfeeding is associated with better growth. However, previous studies provide clear evidence that exclusive breastfeeding reduces the risk of death and illness. Finally, our analysis shows that being judged underweight on the basis of WHO child growth standards may be a better predictor of the risk of death than other indicators or being judged underweight on the basis of the NCHS growth reference. This finding provides an additional reason for countries to implement WHO child growth standards as soon as possible. ■
Acknowledgements
We thank Dr Mercedes de Onis, Department of Nutrition for Health and Development, WHO, Geneva, Switzerland, for reviewing this paper and providing very helpful comments. We also thank members of the WHO Division of Child Health and Development Immunization-Linked Vitamin A Group: P Arthur, Kintampo Health Research Centre, Ghana and London School of Hygiene and Tropical Medicine, London, United Kingdom; S Morris, London School of Hygiene and Tropical Medicine, London, United Kingdom; S Amenga–Etego, C Zandoh and O Boahen, Kintampo Health Research Centre, Ghana; N Bhandari and MK Bhan, All India Institute of Medical Sciences, New Delhi, India; MA Wahed, International Center for Diarrhoeal Disease Research, Bangladesh; CF Lanata, B Butron, AR Huapaya and KB Rivera, Instituto de Investigacion Nutricional, Lima, Peru; for data management, LH Moulton, M Ram, CL Kjolhede and L Propper, Department of International Health, Johns Hopkins University, Baltimore, MA, USA; and for coordination, J Martines and B Underwood, WHO, Geneva, Switzerland.
Footnotes
Competing interests: None declared.
References
- 1.Global strategy for infant and young child feeding Geneva: WHO; 2003. Available from: http://www.who.int/child_adolescent_health/documents/9241562218/en/ [accessed on 21 September 2009]
- 2.United Nations Children’s Fund. The state of the world’s children 2008 New York, NY: UNICEF; 2007. [Google Scholar]
- 3.de Onis M, Garza C. A new international growth reference for young children. Am J Clin Nutr. 1999;70(suppl):169S–72S. [PubMed] [Google Scholar]
- 4.de Onis M, Garza C, Victoria CG, Bhan MK, Norum KR.editorsWHO Multicentre Growth Reference Study (MGRS): rationale, planning and implementation. Food Nutr Bull 2004Suppl 1S1–89. [Google Scholar]
- 5.WHO Multicentre Growth Reference Study Group WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr. 2006;450:76–85. doi: 10.1111/j.1651-2227.2006.tb02378.x. [DOI] [PubMed] [Google Scholar]
- 6.de Onis M, Garza C, Victoria CG, Onyango AW, Frongillo EA, Martines J. The WHO Multicentre Growth Reference Study: planning, study design and methodology. Food Nutr Bull. 2004;25(Suppl 1):S15–26. doi: 10.1177/15648265040251S103. [DOI] [PubMed] [Google Scholar]
- 7.United Nations Standing Committee on Nutrition. Use of the new WHO Child Growth Standards in emergency nutrition programmes [Draft Statement v 4. SCN Working Group on Nutrition in Emergencies]. Geneva: World Health Organization; 2007. Available from: http://www.unscn.org/en/statements/ [accessed on 21 September 2009].
- 8.WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age. Geneva: World Health Organization; 2006. [Google Scholar]
- 9.Seal A, Kerac M. Operational Implications of using 2006 World Health Organization growth standards in nutrition programmes: secondary data analysis. BMJ. 2007;334:733. doi: 10.1136/bmj.39101.664109.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Onis M, Onyango AW, Borghi E, Cuberto G, Yang H, WHO Multicentre Growth Reference Study Group. Comparison of the World Health Organization (WHO) child growth standards and the National Center for Health Statistics/WHO international growth reference: implications for child health programmes. Public Health Nutr. 2006;9:942–7. doi: 10.1017/PHN20062005. [DOI] [PubMed] [Google Scholar]
- 11.Fenn B, Penny ME. Using the new World Health Organisation growth standards: differences from 3 countries. J Pediatr Gastroenterol Nutr. 2008;46:316–21. doi: 10.1097/MPG.0b013e31815d6968. [DOI] [PubMed] [Google Scholar]
- 12.Prost M-A, Jahn A, Floyd SA, Mvula H, Mwaiyeghele E, Mwinuka V, et al. Implication of new WHO growth standards on identification of risk factors and estimated prevalence of malnutrition in rural Malawian infants. PLoS One. 2008;3:e2684. doi: 10.1371/journal.pone.0002684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS, Bellagio Child Survival Study Group. How many child deaths can we prevent this year? Lancet. 2003;362:65–71. doi: 10.1016/S0140-6736(03)13811-1. [DOI] [PubMed] [Google Scholar]
- 14.Kramer MS, Kakuma R. Optimal duration of exclusive breastfeeding. Cochrane Database Syst Rev. 2002;CD003517(Issue 1) doi: 10.1002/14651858.CD003517. [DOI] [PubMed] [Google Scholar]
- 15.Pelletier DL. The relationship between child anthropometry and mortality in developing countries: implications for policy, programs and future research. J Nutr. 1994;124:2047S–81S. doi: 10.1093/jn/124.suppl_10.2047S. [DOI] [PubMed] [Google Scholar]
- 16.Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371:243–60. doi: 10.1016/S0140-6736(07)61690-0. [DOI] [PubMed] [Google Scholar]
- 17.Fawzi WW, Herrera MG, Spiegelman FL, el Amin A, Nestel P, Mohamed KA. A prospective study of malnutrition in relation to child mortality in the Sudan. Am J Clin Nutr. 1997;65:1062–9. doi: 10.1093/ajcn/65.4.1062. [DOI] [PubMed] [Google Scholar]
- 18.Villamor E, Misegades L, Fataki MR, Mbise RL, Fawzi WW. Child mortality in relation to HIV infection, nutritional status, and socio-economic background. Int J Epidemiol. 2005;34:61–8. doi: 10.1093/ije/dyh378. [DOI] [PubMed] [Google Scholar]
- 19.Bairagi R, Koenig MA, Mazumder KA. Mortality-discriminating power of some nutritional, sociodemographic, and diarrheal disease indices. Am J Epidemiol. 1993;138:310–7. doi: 10.1093/oxfordjournals.aje.a116860. [DOI] [PubMed] [Google Scholar]
- 20.Bairagi R, Chowdhury MK. Socioeconomic and anthropometric status, and mortality of young children in rural Bangladesh. Int J Epidemiol. 1994;23:1179–84. doi: 10.1093/ije/23.6.1179. [DOI] [PubMed] [Google Scholar]
- 21.Integrated management of childhood illness chart booklet World Health Organization and United Nations Children’s Fund. 2008. Available from: http://www.who.int/child_adolescent_health/documents/IMCI_chartbooklet/en/index.html [accessed on 9 September 2009].
- 22.Van den Broeck J, Willie D, Younger N. The World Health Organization child growth standards: expected implications for clinical and epidemiological research. Eur J Pediatr. 2009;168:247–51. doi: 10.1007/s00431-008-0796-9. [editorial] [DOI] [PubMed] [Google Scholar]
- 23.WHO/CHD Immunisation-Linked Vitamin A Supplementation Study Group Randomised trial to assess benefits and safety of vitamin A supplementation linked to immunization in early infancy. Lancet. 1998;352:1257–63. doi: 10.1016/S0140-6736(98)02487-8. [DOI] [PubMed] [Google Scholar]
- 24.Low birth weight: country, regional and global estimates New York, NY: United Nations Children’s Fund and World Health Organization; 2004. [Google Scholar]
- 25.Bhutta ZA, Ahmed T, Black RE, Cousens S, Dewey K, Giugliani E, et al. What works? Interventions for maternal and child undernutrition and survival. Lancet. 2008;371:417–40. doi: 10.1016/S0140-6736(07)61693-6. [DOI] [PubMed] [Google Scholar]