Abstract
The authors examined pilot data from an attachment-based parenting intervention for substance-abusing mothers of toddlers (ages 12–36 months). The Mothers and Toddlers Program (MTP) is a 20-week individual therapy intervention that aims to help mothers develop more balanced representations of their children and improve their capacity for reflective functioning (i.e., recognition of the intentional nature of children’s behavior). The authors hypothesized that improvement in maternal representational balance and maternal capacity for reflective functioning would correspond with improvements in maternal behavior with toddlers (e.g., sensitivity to cues, responsiveness to distress, and social–emotional growth fostering) and reduction in maternal psychiatric distress and substance abuse. Eight mothers who completed MTP showed moderate improvements in representational balance and reflective functioning, and these changes corresponded with significant improvements in maternal behaviors with toddlers. The authors also compared MTP completers and noncompleters on sociodemographic and psychosocial indexes and examined the validity of the intervention’s proposed mechanisms of change. Preliminary findings support the importance of attachment mechanisms and indicate that attachment-based interventions may strengthen substance-abusing mothers’ capacities to foster their toddlers’ socioemotional development.
Keywords: parenting interventions, substance abuse treatment, family interventions, prevention, parent-child relations
Although not all mothers who seek treatment for their substance abuse have difficulties parenting their children, as a group substance-abusing women are twice as likely as non-substance-using women to lose custody of their children because of reoccurrences of substance abuse and child neglect (U.S. Department of Health & Human Services, 1999). Over the past 20 years, research has shown that although some mothers who use illicit substances are able to provide home environments and parenting that support their children’s development, mothers with substance use disorders are at greater risk for maladaptive parenting practices than mothers who do not have substance use problems (Mayes & Truman, 2002). Problems in maternal interactions with children have been observed during children’s first 3 years of life, including patterns of poor attachment, attunement, involvement, responsiveness, adaptability, and structure, juxtaposed with heightened maternal physical activity, provocation, and intrusiveness (Burns, Chethik, Burns, & Clark, 1997; Hans, Bernstein, & Henson, 1999; Rodning, Beckwith, & Howard, 1991). Studies reporting substance-abusing mothers’ perspectives about parenting have indicated a limited understanding of basic child development issues and ambivalent feelings about having and keeping children (Mayes & Truman, 2002; Murphy & Rosenbaum, 1999).
Only a handful of studies to date have reported findings from clinical trials evaluating interventions for substance-abusing parents of young children (i.e., younger than 5 years of age; for reviews, see Pajulo, Suchman, Kalland, & Mayes, 2006; Suchman, Pajulo, DeCoste, & Mayes, 2006). Although the findings have generally indicated improvement in parental factors such as substance use, psychiatric distress, and knowledge of parenting, very few have shown improvement in parent–child interactions or child adjustment. Intervention approaches have ranged in focus from behavioral skills training to advocacy for needed services to education about early child development; however, very few have emphasized the emotional quality of the parent–child relationship or the social and emotional growth of the child. Given that women with substance use disorders often have developmental histories characterized by emotional neglect (Luthar & Walsh, 1995), it may be that parenting interventions must first focus on emotional deficits in the mother–child relationship to improve parenting interactions and foster optimal child development (see Suchman, Mayes, Conti, Slade, & Rounsaville, 2004).
Attachment Mechanisms of Parenting
Originating with the ideas of John Bowlby (1982), attachment theory emphasizes parental attunement to emotional cues during early caregiving years as a means to promoting optimal social–emotional and cognitive development (for an overview, see Karen, 1994). Attachment research during the past 30 years has generally shown that children whose caregivers accurately perceived and sensitively responded to their emotional cues during early caregiving years have been more likely to express their emotional distress directly to the caregiver and develop greater capacities for self-regulation in response to distress. This self-regulatory capacity is thought to serve as a protective factor, promoting social competence and reducing risk for behavior problems during school-age and adolescent years (Sroufe, Carlson, Levy, & Egeland, 1999). Bowlby proposed that over time, children developed internal “representations” of the caregiving relationship (i.e., enduring perceptions of self and caregiver) based on their experience with early caregivers and that these representations influenced their expectations and guided behavior in subsequent relationships. Children reared by sensitive caregivers are generally thought to develop representations that are balanced in terms of positive and negative affect, whereas children reared by insensitive caregivers are thought more likely to develop mental representations characterized by denial or distortion of painful negative affect (Slade & Cohen, 1996).
In observations of drug-abusing mothers and children, mothers have shown difficulties accurately perceiving and sensitively responding to their children’s signals of emotional distress (Mayes & Truman, 2002). Attachment theorists commonly view these parental misperceptions of children’s emotional distress as a function of parents’ own distorted or denied affect related to their own early experiences (Suchman et al., 2004). According to attachment theory, to accurately perceive her child’s emotional cues, a mother must first have developed the capacity to recognize her own denied or distorted affect about her child and their relationship. Otherwise, the mother is thought to be more likely to misattribute affective states to herself and her child and respond noncontingently or insensitively. For example, a mother who is unable to recognize her child’s fear of separation is thought to be more likely to fail to reassure her child, before departing, that she will return. Likewise, a mother who does not recognize her own feelings of loneliness is thought to be likely to misattribute them to her child and be overly intrusive. Similarly, a mother who does not recognize her own fears for safety is expected to respond with overprotection to her child’s natural bids for independence.
The intergenerational transmission of representations characterized by denial or distortion is thought to be mediated by a caregiver’s inability to recognize the intentionality underlying his or her child’s behavior (i.e., low or absence of “reflective functioning”; Fonagy, Gergely, Jurist, & Target, 2002; Fonagy & Target, 1997). For example, a mother who denies or distorts her own or her child’s painful experiences is thought to be likely to have difficulty recognizing the mental states and emotional needs that underlie her child’s behavior. Instead, the mother is expected to misattribute the behavior to things that are unrelated to her child’s experiences (i.e., distortions of mental states) or to attribute the child’s behavior to global personality characteristics or external factors (i.e., denial of mental states). Without the capacity to recognize mental states that underlie a child’s behavior, a mother is expected to have difficulty making sense of and responding effectively to her child’s behavior. In turn, the child is thought to be more likely to develop a limited understanding of his or her own mental state that may transmit patterns of distorted or denied intentionality to the next generation.
Maternal reflective functioning has been empirically linked with sensitive parenting behavior in at-risk parents (Fonagy et al., 2002; Fonagy & Target, 1997). The absence of or low maternal reflective functioning has been linked with maladaptive parenting behavior (e.g., withdrawal, hostility, or intrusiveness) and with young children’s limited ability to express emotional distress directly (Grienenberger & Slade, 2004; Slade, Grienenberger, Bernbach, Levy, & Locker, 2001). Low maternal reflective functioning has also been found to mediate associations between maternal cocaine use and diminished psychosocial capacities (e.g., attention, social skills, and withdrawal) of young children (Levy & Truman, 2002).
Drug Abuse and Mechanisms of Attachment
Drug abuse has been conceived by Khantzian (1997) as an attempt to self-medicate in the presence of painful or difficult affect that has not otherwise been psychologically contained or regulated. In other words, drug abuse has been understood as an effort to compensate for deficits in emotional regulation. Therefore, it is possible that as a mother’s capacity to contain and regulate her own and her child’s painful affect increases, her desire to return to drug use as a source of emotional comfort may also diminish.
Many abused substances (e.g., cocaine and heroin) have been shown to affect the dopaminergic pathways in the brain, areas that are associated with initiation of behavior, hedonic reward, and motivation (Koob, 1996; Koob & LeMoal, 1997). These central dopaminergic pathways are also thought to be critically involved in an adult’s capacity to invest in the care of children (Edelman & Tononi, 1995). Drug abuse can therefore be viewed as a co-optation or hijacking of this endogenous value system (Leckman & Mayes, 1998). As a consequence, once this system is co-opted by repeated drug use, competing investments in craving the drug versus caring for the child may reduce the caregiver’s capacity to invest in caring for the child. Conversely, as a caregiver’s desire to invest in her child is enhanced, a concomitant decrease in the reward derived from drug use may also occur.
The Mothers and Toddlers Program: Therapeutic Approach
In an ongoing National Institute on Drug Abuse–funded project, we have been developing the Mothers and Toddlers Program (MTP), an adjunct individual therapy intervention for mothers in outpatient substance abuse treatment who are caring for children 12–36 months of age. Conceptually, the program is based on psychosocial and neurobiological mechanisms of attachment and addiction (Bowlby, 1982). The primary aim of MTP is to foster a large enough shift in maternal representational balance and capacity for reflective functioning to increase maternal capacity for sensitivity and responsiveness to toddler emotional cues.
The therapy follows a developmental progression based on the mechanisms of attachment. The developmental chain of events begins in the early sessions with a focus on building a strong therapeutic alliance in which the patient experiences herself as valued and appreciated by the therapist and comes to view the therapist as a reliable source of assistance and support. The therapist carefully listens to the mother’s concerns about parenting and works to understand the problem as the mother sees it. The therapist accepts (but does not necessarily condone) the mother’s aberrant views about parenting and attempts to learn how the mother is coping with the problem. Strong social mores against substance abuse, particularly regarding women who are caring for children, can make it especially difficult for a mother to trust the therapist’s intentions, increasing the likelihood that the mother will leave treatment prematurely if she perceives the therapist as judgmental. It is therefore imperative that the therapist be attuned to the relationship and encourage the mother’s efforts to openly discuss her concerns.
The therapist offers to assist the mother with whatever is stressing her at the moment, including concrete problems (e.g., need for supplies or services) or other relational issues, to strengthen the mother’s experience of the therapist as a source of help and support for parenting. The program keeps basic supplies on hand (e.g., diapers and healthy snacks) and provides coffee, child care, and transportation when needed. The therapist may help the mother find services, scholarships, or housing and will receive calls for assistance from the mother during the week. Although the therapist may need to endure feelings of being “had” from time to time, assisting the mother provides an opportunity for the therapist to maintain an alliance and also suggest, in a timely way, the need for further work in therapy.
The next step in the developmental progression that begins early in therapy, and continues throughout the intervention as needed, involves ensuring that the mother has adequate support and skills for tolerating and regulating strong affect (both positive and negative) because parenting stress can trigger strong and unregulated affective responses that, in turn, can precipitate a relapse to substance use. The therapist therefore watches and listens carefully for precipitating events and behavioral cues (e.g., restlessness, hyperactivity, defensiveness, opposition, recurring crises, or physical complaints) that indicate that the mother is affectively distressed and brings these observations to the mother’s attention in an effort to help her recognize and contain (and eventually understand) the affect. Particular care is taken to monitor and probe for affective distress in patients who tend to minimize or deny uncomfortable affect or when difficult or stressful circumstances arise.
As the therapist joins with the mother to better understand her point of view about ongoing problems (parenting and other relational issues), the therapist works to clarify for their mutual understanding the mother’s core (although not necessarily conscious) representations of herself in relation to others and to her child. The therapist adopts a naïve and inquisitive stance, seeking opportunities to probe further about these representations (e.g., “When you call [daughter] ‘the devil,’ is this because she does things that seem evil to you or that she does things that scare you?”). The therapist reflects back to the mother her representational world, attempting to place confusing or disparate parts within a logically and emotionally understandable context (e.g., “So most of the time [daughter] seems to be doing things to be mean, but every so often she seems to want your affection and comfort”). The ongoing clarification of the mother’s representational world allows the therapist to identify areas of distortion, harshness, incoherence, and insensitivity that she can then explore with the mother in the interest of developing a more coherent and integrated understanding of herself and her toddler.
Along with exploring and clarifying the mother’s representational world, the therapist encourages the mother to consider the emotional needs, intentions, wishes, and thoughts that might be derived from her representations and that might also be driving her own interactions with others and their interactions with her. This process of “mentalizing” (Fonagy, Target, Steele, & Steele, 1998) is thought to be critical to maintaining a contextualized understanding of behavior and to the process of emotional regulation. In the context of parenting, for example, recognizing that a child’s clinging behavior is often driven by a genuine need for emotional security can help prevent a parent from reacting aggressively or impulsively to the behavior. The therapist is careful not to make assumptions about anyone’s representations or mental states but instead adopts a naïve and inquisitive stance. To do otherwise would risk superimposing the therapist’s perceptions.
Although the ultimate objective is to engage in a mentalizing process about the mother–child relationship, this may not be possible because of the mother’s preoccupation with other relationships (e.g., with family members, the legal system, substances, etc.). The process of examining any stressful relationship from an inquisitive, mentalizing stance is viewed as productive because it provides a regulatory function and a chance to identify representations driving these interactions and can help “free” the mother psychologically to become more available to her child.
When the child becomes the focus of the session, the therapist encourages the mother to explore her own elicited emotions, her assumptions about and expectations for the child, the meaning of the interaction, the child’s capacities at his or her present stage of development, and the child’s underlying emotional needs. The therapist works with the mother to develop a contextual understanding of the interaction and the child’s behavior that can help guide the mother’s chosen response. For example, a mother may mention that her toddler has been very difficult that day—crying even though she, the mother, has been close by. The therapist urges the mother to seriously consider what might have been stressing the child and then underscores the mother’s accurate attributions or realizations (e.g., the child might be stressed because the furniture in the house had been rearranged). During moments when it is evident that the mother is worried about or expecting unrealistic capacities of her toddler (e.g., long attention span, manners, perspective taking, etc.), the therapist will provide realistic guidelines about the child’s capacities.
The therapist and mother will also together observe videotaped play sessions involving the mother and her toddler to learn more about the mother’s interpretations of her child’s behaviors and intentions and to examine their synchronicity. (After each weekly therapy session, there is also often an opportunity for the therapist to witness how the mother and toddler greet each other). The play sessions involve a half hour of free play during which mother and toddler are introduced to various interactive activities that include physical (tent box mats and mesh tunnel), social (kitchen and farm), spatial (wooden and Lego blocks), and quiet (puzzle) play. The therapist watches the play session live on closed-circuit TV to observe how mother and toddler are with each other (e.g., how engaged are they with each other? Does the child visually reference the mother during the play? Does the mother encourage the child to explore or to try a new element of the activity? What is the affective quality of the interaction—joyful? Subdued? Solemn? Agitated? Does the mother use imperatives or give explanations? Is the child paying attention to the mother or playing autonomously? How does the mother respond to the child’s signals to disengage?) The therapist and mother together explore what the mother and toddler might have been thinking during different interaction moments. Moments of the play session when the mother and child seem particularly in sync and moments when the mother and child seem out of sync are noted. The intent here is to join the mother in thinking about underlying thoughts, intentions, and emotions that are driving her own behavior, her child’s behavior, and their interactions.
Research Design
The goals of the completed first phase of this therapy development study were to (a) develop a therapist’s manual for the MTP, (b) conduct a pilot study with a small sample of mothers with all assessments that will be used to evaluate MTP efficacy in an upcoming randomized trial pilot study, and (c) develop a therapist adherence rating scale and coding procedures for measuring treatment integrity. Using data collected during this first phase, we were interested in (a) examining the preliminary efficacy of MTP for maternal caregiving, (b) comparing the demographic and psychosocial characteristics of treatment completers versus noncompleters, and (c) testing the attachment treatment model’s proposed mechanisms of change. Our research hypotheses were as follows:
Hypothesis 1
Mothers who complete the MTP intervention will show meaningful improvement in targeted domains—representational balance and reflective functioning—that will co-occur with meaningful improvement in indirectly targeted domains—maternal sensitivity and responsiveness to child cues during mother–child interactions. Mothers who complete the MTP intervention will also show a reduction in symptoms of psychiatric distress—depression, anxiety, and global psychiatric distress—as well as a reduction in the frequency of illicit drug use.
Hypothesis 2
In comparison with treatment completers, treatment noncompleters are more likely to come from disadvantaged or disenfranchised demographic backgrounds and to be at greater risk for psychosocial maladjustment.
Hypothesis 3
Improvement in maternal representational balance will be associated with improvement in maternal behavior with children, and this association will be mediated by improvement in maternal capacity for reflective functioning.
Method
Recruitment, Consent, and Assessment Procedures
Women were recruited via referrals from their primary substance abuse clinicians at two outpatient clinics (a methadone maintenance program and a women’s outpatient program) run by the APT Foundation, a private nonprofit organization and major provider of outpatient substance abuse treatment in the Greater New Haven, Connecticut, area. Women were eligible to participate if they were (a) caring for a toddler between 12 to 36 months of age who did not exhibit any serious developmental delays; (b) enrolled in outpatient treatment at the APT Foundation for their substance abuse; (c) not currently suicidal, homicidal, in crisis, or cognitively impaired; and (d) English speaking. Interested and eligible mothers were invited to complete informed consent procedures during which a research assistant explained the parenting program and research procedures and the extent and limits of confidentiality. Consenting mothers were scheduled for their baseline assessment visits, which took place across the following 4 weeks.
During the baseline phase, mothers completed a psychosocial intake interview, two videotaped attachment interviews, two play sessions with their toddler, and a series of brief psychosocial adjustment questionnaires. During the first visit, mothers also met with their individual therapist for an introductory session. On the days when attachment interviews were conducted, the mothers met with their therapist (Nancy E. Suchman or Nancy Legow) before and after each interview for preparation, support, and debriefing, and the therapist viewed each interview on a closed-circuit TV. All narrative interviews were conducted by the study’s project director (Cindy DeCoste), and all study questionnaires were administered by the study research assistant (Nicole Schmitt).
After completing the baseline assessments and during the subsequent 12 weeks, mothers continued to meet with their individual therapist for weekly 1-hr sessions. These sessions were provided in addition to the mothers’ ongoing substance abuse treatment at the referring clinic. Child care was provided for the mothers’ children during weekly visits. Following each therapy session, mothers completed several questionnaires about therapeutic alliance, mood, and knowledge about child development and child temperament, for which they were compensated.
After 12 weeks of MTP, mothers completed the posttreatment assessments (approximately 4 weeks) and were given the option to continue in MTP for an additional 12 weeks or to enter a 4-week follow-up period of no parenting treatment followed by a final 4-week assessment period. Mothers who chose to continue in MTP completed posttreatment assessments again after 12 weeks and follow-up assessments after 4 weeks of no parenting treatment. Posttreatment results collected after the first 12 weeks of treatment were analyzed for this report.
Sample
Fourteen women (8 from the women’s outpatient program and 6 from the methadone clinic) were referred by their primary substance abuse clinicians and found eligible to participate. Mothers’ mean age was 32 years (range = 21–43, SD = 6.4). A majority of mothers (57%) had completed high school or the equivalent, 29% had completed some college, and the remaining 14% had not completed high school. Seventy-one percent were unemployed at the time of enrollment. A majority (64%) of mothers were either married or cohabiting with a partner, 21% were separated or divorced, and the remaining 15% had never been married. A majority of the mothers were Caucasian (72%), 14% were Hispanic, and 14% were African American. Mothers had an average of 2.4 biological children (range = 1 – 6, SD = 1.5). Their participating toddlers ranged from 12 to 36 months in age (M = 26.4, SD = 8.02).
Of the 14 women who completed consent procedures, 8 completed 12 weeks of individual therapy and 4 chose to continue in MTP for an additional 12 weeks. Of the 6 women who dropped MTP prematurely, 4 left the program before completing baseline assessments (1 mother dropped out after baseline Week 3 after learning she was pregnant with twins and an onset of severe morning sickness; 1 mother disclosed suspicion about being filmed during interviews and did not return after Week 1, and 2 mothers did not return to MTP or to the women’s substance abuse program after baseline Week 1). Two mothers left the program after their second individual therapy session (1 mother was close to completing her mandated substance abuse treatment episode and did not wish to receive any additional treatment, and 1 mother relapsed to cocaine use after her second individual therapy session and dropped out of MTP and the women’s outpatient program).
Assessments and Measures
Psychosocial intake evaluation
On enrollment in the study, each mother completed a structured 1.5-hr intake interview during which she was asked about her demographic background, personal and family psychiatric and substance abuse history, problems related to substance abuse (e.g., unemployment, legal issues, and medical history), family and personal relationships, trauma history and posttraumatic stress disorder symptoms, and goals for treatment. The interview was used to establish preliminary diagnoses based on Diagnostic and Statistical Manual of Mental Disorders (4th ed.; American Psychiatric Association, 1994) diagnostic criteria. The research assistant, Nicole Schmitt, was trained and supervised by Nancy E. Suchman and Cindy DeCoste to conduct all intake interviews.
Working Model of the Child Interview (WMCI; Zeanah & Benoit, 1993)
The WMCI was used to assess the mother’s mental representation of her toddler. During the 1.5-hr interview, the mother is asked to describe her pregnancy and her child’s birth, reactions of family members to the birth, the child’s developmental milestones and personality, and the mother’s relationship with the child. The mother is also asked to describe recent instances when the toddler was upset, physically or emotionally hurt, or exhibiting difficult behaviors and times when the mother and toddler were separated, as these are times that the child’s attachment needs are likely to be activated. The purpose of the interview is to determine how the mother mentally represents her child and their relationship, particularly during moments of emotional distress (i.e., when the child’s attachment needs are activated).
Each interview was videotaped and reviewed by a team of five clinical psychology students and trainees who were trained by Nancy E. Suchman to code the interviews on a series of 5-point Likert subscales originally developed by Zeanah and Benoit (1993). Although Zeanah and colleagues have used these subscales to determine overall classifications of parents’ working models of the child as “balanced,” “disengaged,” or “distorted,” these classifications were considered unlikely to detect nuanced shifts in representation in response to the MTP intervention. We therefore developed a composite scale—the Representational Balance Composite Scale—to measure subtle changes in maternal representation. The following six subscales were used to calculate the Representational Balance Composite Scale: Richness (elaboration and detail used to describe the child’s unique personality), Openness (acceptance of change in the child and relationship over the course of development), Coherence (organization and credibility of the narrative), Caregiving Sensitivity (recognition of and responsiveness to child’s emotional needs), Acceptance (adoption of a parental stance and the creation of psychological “room” for the child and his or her unique personality), and Overall Balance (coder’s overall rating of representational balance). The Representational Balance Composite Scale was conceived theoretically and examined statistically in terms of its internal validity: All items were first entered together in an exploratory factor analysis. A one-factor solution best fit the data, and factor loadings for the scale were above .60. Cronbach’s coefficient alpha was .93 for the Representational Balance Composite Scale. The five raters achieved interclass correlations of .60 for the Representational Balance Composite Scale score, indicating substantial reliability (Garson, 2006).
Maternal Attribution Scale–Toddler Version (MAS-T; DeCastro & Mayes, 2006)
The Toddler Version of the MAS-T is a 35-item measure used to assess positive and negative intentional stances attributed by mothers to their toddlers. Because children under 3 years of age are usually not thought to be capable of intentional stances, the measure captures the mother’s projections about the toddler’s intentions, wishes, thoughts, and emotions. The Negative Attribution Scale has 21 items rated on a 5-point Likert scale (e.g., “I feel that my child cries just to upset me”). The Positive Attribution Scale has 14 items rated on a 5-point Likert scale (e.g., “I feel that my child thinks good things about me”). Cronbach’s coefficient alphas were .95 and .60, respectively, for the negative and positive scales.
Parent Development Interview (PDI; Slade, Aber, Berger, Bresgi, & Kaplan, 2002)
The PDI was used to measure maternal capacity for reflective functioning. During the 1.5-hr interview, the mother is asked to describe recent times when she felt she and her child were getting along; times when they were not getting along; times when the mother felt angry, needy, and guilty as a parent; times when the child needed the mother’s attention; and times when the mother and child were separated. The interviewer asks the mother to describe her own and her child’s responses to situations to capture the mother’s capacity to mentalize for herself and her child. Each of the mother’s transcribed responses is then coded item by item on a scale ranging from − 1 to 9 for its level of reflective functioning, using methods originally developed by Fonagy and colleagues (1998) for use with the Adult Attachment Interview (Main & Goldwyn, 1985) and then adapted by Slade and colleagues (2004) for use with the PDI. A score of 5 on the Reflective Functioning scale indicates the presence of a rudimentary capacity for reflective functioning—or a basic understanding of how mental states work together and influence behavior. A score of 3 indicates a limited capacity to acknowledge mental states without any understanding of how mental states function. A score of 1 indicates a complete absence of any mental state recognition (e.g., reference is made only to behavior and global personality characteristics). Scores above 5 indicate increasingly elaborate and sophisticated understanding of how mental states function and influence behavior. After each narrative passage is coded for reflective functioning, an overall score on a scale ranging from − 1 to 9 is assigned on the basis of the mother’s typical mode of response. The PDI protocols for this study were coded by a clinical psychology doctoral student who was trained to reliability by Nancy E. Suchman (i.e., achieved an interclass correlation of .63 with trainers on practice protocols) and was unaware of the interview dates and other information about participants.
Nursing Child Assessment Satellite Training (NCAST) Teaching Scales (Barnard & Eyres, 1979)
The NCAST Teaching Scales are a 73 binary-item tool used to observe and rate caregiver–child interactions with children ages birth to 36 months. Mothers are asked to choose one task to teach the child (e.g., stringing beads, drawing shapes, or grouping blocks by color) from a list of tasks that are organized in increasing order of difficulty. The session is videotaped and coded for four types of maternal behaviors (i.e., two adaptive types—sensitivity to toddler’s cues and response to the toddler’s potent disengagement cues—and two types that rely more on maternal initiative and less on maternal response to the child—social–emotional and cognitive growth fostering). Two types of child behaviors are also coded (i.e., clarity of cues and responsiveness to caregiver) and will be discussed in a forthcoming report. The 11-item Sensitivity to Cues Subscale measures the mother’s responsiveness to her toddler’s behavioral cues (e.g., “Caregiver positions child so that child can reach and handle teaching materials”). The 11-item Response to Distress Subscale measures the mother’s effectiveness in relieving the toddler’s distress (e.g., when the toddler signals to the mother a desire to disengage from the task, the mother “avoids using abrupt movements or rough handling”). The 11-item Social-Emotional Growth Fostering Subscale measures maternal ability to play affectionately with the child, engage in social interactions, and provide appropriate social reinforcement of desired behaviors (e.g., “Caregiver laughs or smiles at child during the teaching interaction”). The 17-item Cognitive Growth Fostering Subscale measures maternal ability to provide stimulation that is just above her child’s current level of understanding (e.g., “Caregiver uses explanatory verbal style more than imperative style in teaching the child”).
Maternal psychosocial adjustment and illicit drug use
All measures of maternal psychosocial adjustment were administered at 8-week intervals beginning at baseline and ending at the follow-up assessment. The Beck Depression Inventory (BDI; Beck, Steer, & Brown, 1996), a widely used 21-item questionnaire rated on a 4-point scale, was used to assess maternal symptoms of depression. The BDI yields a total score between 0 and 63. Scores between 13 and 19 indicate mild depression, scores between 20 and 28 indicate moderate levels of depression, and scores between 29 and 63 indicate severe levels of depression (Beck et al., 1996). The Brief Symptom Inventory (BSI; Derogatis, 1993), a widely used standardized 90-item self-report measure of psychopathology, was used to measure levels of maternal global psychiatric distress. The BSI yields a composite Global Severity Index of current overall symptomatology across multiple domains that has demonstrated good reliability and validity (Derogatis, 1993). Maternal illicit drug use was monitored twice weekly at the women’s outpatient program and twice monthly at the methadone program using urine toxicology screens that tested for presence of cocaine, heroin, opiate, cannabis, benzodiazepine, and methamphetamine metabolites in urine specimens. All mothers were asked for permission to release results of laboratory drug screens to the research team during informed consent procedures. The presence of metabolites for any drug in urine specimens during a given month served as an indication of a reoccurrence of substance use for that month of the mothers’ study enrollment.
Data Analysis
Because a sample size of 14 may be too small to provide sufficient power for testing statistical significance (see Cohen, 1988), we examined both statistical significance and effect sizes (the latter are not affected by sample size). Data analytic strategies used for examining (a) treatment completer outcomes, (b) baseline differences between treatment completers and noncompleters, and (c) validity of the proposed treatment model are described below.
Treatment outcomes
To test the hypothesis that mothers completing 12 weeks of MTP will show meaningful improvement in all primary (i.e., maternal representational balance, maternal reflective functioning, and maternal attributions of toddlers) and secondary (i.e., maternal behavior with toddlers, maternal psychosocial adjustment, and maternal drug use) targeted domains, a series of paired-sample t tests were conducted, and effect sizes (d) were computed to determine the magnitude of effect (see Cohen, 1988).
Comparison of treatment completers with treatment noncompleters
To test the hypothesis that treatment noncompleters have more disadvantaged socioeconomic backgrounds and higher levels of psychosocial maladjustment at baseline, a series of t tests for independent samples (continuous variables) and chi-square tests (categorical variables) were conducted, and effect sizes (d and w, respectively) were computed to determine the magnitude of effects.
Test of proposed mechanisms of change
Cohen and Cohen (1983) have noted that the intuitive approach to measuring change, subtracting a prescore from a postscore, is problematic because the resulting “change” score contains variance because of the prescore that is likely to cause distortion in correlations with other variables (for a complete discussion, see Cohen & Cohen, 1983, pp. 413–427). Change was therefore measured as the residual (remaining variance) after variance because the prescore was removed from the postscore.
To test the hypothesis that associations between improvement in maternal representational balance and improvements in maternal behavior with toddlers are mediated by improvement in the maternal capacity for reflective functioning, a series of standard linear regressions were conducted to test for meaningful associations between (a) improvement in representational balance and improvement in reflective functioning and maternal behavior and (b) improvement in reflective functioning and maternal behavior (see Baron & Kenny, 1986). Then, in a hierarchical linear regression, we examined whether the magnitude of association between improvement in maternal representations and improvement in maternal behavior was reduced when variance due to improvement in maternal reflective functioning was first removed.
Results
Treatment Outcomes
Maternal representations of the toddler
Baseline mean scores for the Representational Balance Composite Scale (M = 2.13, SD = 0.78) corresponded with representations characterized by general versus detailed accounts of the child’s personality, static versus developmental perspectives of the child’s behavior, disorganized or distorted versus coherent or contextual understanding of the child’s personality and behavior, limited recognition of the child’s underlying emotional needs, and limited acceptance of the child’s unique personality characteristics (see Table 1). After 12 weeks of weekly individual therapy in MTP, the mean score for treatment completers (n = 8) increased significantly (M = 2.46, SD = 0.82, t[7] = − 2.91, p = .02, d = 0.29) in the direction of balance.
Table 1.
Results of Paired-Sample t-Tests Comparing Mean Scores of Mothers and Toddlers Program Completers at Baseline and Week 12
| Measure | N | Normative score or cut-off | Baseline mean (SD) | Week 12 mean (SD) | t (df) | p | da | |
|---|---|---|---|---|---|---|---|---|
| Maternal representations of the toddler | WMCI | 8 | ||||||
| Representational balance | 3.00 | 2.13 (.78) | 2.46 (0.82) | −2.91 (7) | .02 | 0.29 | ||
| Maternal attributions of the toddler | MAS-T | 8 | ||||||
| Negative | n/a | 0.86 (0.99) | .53 (0.98) | 1.35 (7) | .23 | 0.24 | ||
| Positive | n/a | 3.06 (0.37) | 3.21 (0.34) | −1.76 (7) | .43 | 0.30 | ||
| Maternal reflective functioning | PDI | 8 | ||||||
| Overall level | 4.00 | 3.38 (0.96) | 3.91 (0.55) | −1.89 (7) | .10 | 0.48 | ||
| Maternal behavior with toddler | NCAST | 7 | ||||||
| Sensitivity to cues | 9.16 (1.62) | 9.29 (1.11) | 10.00 (0.58) | −1.99 (6) | .09 | 0.57 | ||
| Response to distress | 10.04 (1.78) | 7.86 (0.90) | 8.75 (0.68) | −1.74 (6) | .13 | 0.79 | ||
| Social–emotional growth fostering | 8.99 (1.83) | 8.00 (1.16) | 9.55 (0.35) | −2.74 (6) | .03 | 1.03 | ||
| Cognitive growth fostering | 12.51 (3.39) | 12.57 (1.81) | 14.75 (0.35) | −3.53 (6) | .01 | 1.18 | ||
| Mother total teaching score | 40.69 (6.85) | 37.71 (2.81) | 42.75 (1.57) | −6.71 (6) | .001 | 1.57 | ||
| Mother contingency | 16.09 (3.64) | 15.29 (1.11) | 16.50 (0.91) | −1.66 (6) | .15 | 0.84 | ||
| Maternal psychological adjustment | ||||||||
| Maternal depression | BDI | 8 | 13.00 | 14.13 (3.56) | 7.50 (1.37) | 1.85 (7) | .11 | −1.74 |
| Maternal psychiatric distress | BSI | 8 | 50.00 (10.00) | 56.4 (8.75)b | 53.80 (2.89) | 1.16 (7) | .29 | −0.28 |
| Maternal anxiety | STAI | 7 | ||||||
| State anxiety | 50.00 (10.00) | 48.11 (9.08) | 51.50 (8.35) | −1.25 (6) | .26 | 0.27 | ||
| Trait anxiety | 50.00 (10.00) | 56.44 (11.58) | 52.25 (6.24) | 0.94 (6) | .39 | −0.32 | ||
| Maternal drug abuse | ||||||||
| % positive urine toxicology screens | UTOX | 8 | n/a | 63 | 13 | 2.65 (7) | .03 | 1.13 |
Note. N = 8. Italicized scores represent T Scores or percentiles where normative M = 50. df = degrees of freedom; WMCI = Working Model of the Child Interview; MAS-T = Maternal Attribution Scale–Toddler version; PDI = Parent Development Interview; NCAST = Nursing Child Assessment Satellite Training Teaching Scales; BDI = Beck Depression Inventory; BSI = Brief Symptom Inventory; STAI = State–Trait Anxiety Inventory; UTOX = urine toxicology screen.
Effect size d computed for t-tests was computed as follows: Mean1 − Mean0(SD1)2 + SD0)2]; effect size of 0.20 is considered small; 0.50, medium; and 0.80, large (Cohen, 1988). The use of paired t-test values to compute effect sizes was considered less optimal because of the likelihood that effect sizes would be overestimated (see Dunlap, Cortina, Vaslow, & Burke, 1996).
Maternal attributions of the toddler
At baseline, mothers’ mean score on the Negative Attributions Scale of the MAS-T was 0.86 (SD = 0.99), which corresponds to a response of “almost never” on a Likert scale ranging from 0 to 4. Mothers’ mean score on the Positive Attributions Scale at baseline was 3.06 (SD = 0.37), which corresponds to a response of “sometimes” on a Likert scale ranging from 0 to 4. After 12 weeks of individual therapy in MTP, the mean score on the Negative Attributions scale decreased to 0.53 (SD = 0.98, t[7] = 1.35, p = .23, d = − 0.24), which corresponds to the midpoint between a response of “never” and “almost never” on a Likert scale ranging from 0 to 4. At 12 weeks, the mean score for Positive Attributions increased to 3.21 (SD = 0.34, p = .43, d = 0.30), which corresponds to a response of “sometimes” on a Likert scale ranging from 0 to 4. Neither change was statistically significant, and effect sizes representing change in each case were small.
Maternal reflective functioning
The baseline mean score for overall maternal reflective functioning (M = 3.38, SD = 0.96) indicated that mothers generally recognized their own and their children’s mental states (e.g., thoughts, intentions, wishes, and emotions) but did not understand their own or their children’s behaviors in terms of mental states. After 12 weeks of individual therapy in MTP, mothers’ overall level of reflective functioning increased to 3.91 (SD = 0.55). This increase was marginally significant (t[7] = − 1.89, p = .10, d = 0.48), and the effect size was medium-large.
Maternal behavior with the toddler
The baseline mean maternal scores on the Sensitivity to Cues, Cognitive Growth Fostering, and Mother Contingency subscales approximated the NCAST Teaching Scales normative scores for Caucasian mothers. Mean scores at baseline on Maternal Response to Distress, Social-Emotional Growth Fostering, and Mother Total Teaching Subscales ranged from 0.5 to 2 standard deviations below the normative mean.
After 12 weeks of individual therapy in MTP, the mean maternal Sensitivity to Cues score increased to 0.5 standard deviations above the normative mean. This increase was marginally significant (t[6] = − 1.99, p = .09), and its effect size (d = 0.57) was medium. The mean Maternal Response to Distress score increased to 0.5 standard deviations below the normative mean. This increase was not quite marginally significant (t[6] = − 1.74, p = .13), but its effect size (d = 0.79) was large. The mean score for Social-Emotional Growth Fostering increased significantly (t[6] = − 2.74, p = .03, d = 1.80) to 1 standard deviation above the normative mean. The mean Cognitive Growth Fostering score increased significantly (t[6] = − 3.53, p = .01, d = 1.03) to 0.75 standard deviations above the normative mean. The mean Mother’s Total Teaching Subscales score increased significantly (t[6] = − 6.71, p = .001, d = 1.57) to 1.5 standard deviations below the normative mean, and the mean Mother Contingency score increased to approximate the normative mean. Although this increase was not significant (t[6] = − 1.66, p = .15), the corresponding effect size (d = 0.84) was large.
Maternal psychosocial adjustment and illicit drug use
At baseline, the mean BDI score for maternal depression was above the clinical cut-off corresponding to mild depression, the mean score for maternal global psychiatric distress was 0.6 standard deviations above the normative mean, and the mean scores for maternal state and trait anxiety, respectively, were 0.2 standard deviations below and 0.6 standard deviations above the normative mean.
After 12 weeks in MTP, maternal depression decreased to 5.5 points below the clinical cut-off. Although this decrease was not quite marginally significant (t[7] = 1.85, p = .11) the corresponding effect size (d = − 1.74) was large. Maternal global psychiatric distress decreased to 0.4 standard deviations above the normative mean. Although this decrease was not statistically significant (t[7] = 1.16, p = .29), the corresponding effect size (d = − 0.28) was small. The mean score for maternal state anxiety increased to 0.1 standard deviation above the normative mean, and maternal trait anxiety decreased to 0.2 standard deviation above the normative mean. Although these score differences were not statistically significant, the corresponding effect sizes were both medium. Finally, during the month before the baseline assessment, 63% (5) of the mothers had at least one positive urine toxicology screen for cocaine or heroin. During the 3rd month of the intervention, 13% (1) of the mothers had a positive toxicology screen for cocaine or heroin (t[7] = 2.65, p = .03, d = 1.13).
Comparison of Treatment Completers With Noncompleters
As shown in Table 2, meaningful differences in background characteristics of MTP completers in comparison with noncompleters were found. Sociodemographically, in comparison with noncompleters, MTP completers were, on average, 5 years older and their participating toddlers were, on average, 5.9 months older. Completers were also more likely to be Caucasian, to be employed, and to have been married. In terms of their substance abuse histories, treatment completers were more likely to have initiated their substance use 1 year earlier (age 14 vs. 15) and to have initiated cocaine use 4 years earlier (age 20 vs. 24) and heroin use 3.5 years later (age 25 vs. 21.5). Treatment completers were also more likely to be enrolled in methadone maintenance and to report fewer symptoms of drug withdrawal and dependence. Psychiatrically, treatment noncompleters reported more exposure to more traumatic events and more symptoms of depression and anxiety (state and trait).
Table 2.
Descriptive Data for Full Sample
|
M (SD) or % |
|||||
|---|---|---|---|---|---|
| Variable | Noncompleters (n = 6) | Completers (n = 8) | t(df) or χ2a | p | wb or dc |
| Maternal age | 29.00 (7.72) | 34.63 (4.07) | −1.77 (13) | .10 | .91 |
| Ethnicity | 16 | .23 | .49 | ||
| Caucasian | 50.0 | 87.5 | |||
| African American | 33.4 | 00.0 | |||
| Hispanic or Latino | 16.7 | 12.5 | |||
| Marital status | 16 | .19 | .48 | ||
| Never married | 33.3 | 0.00 | |||
| Separated/divorced | 16.7 | 25.0 | |||
| Married/cohabitating | 50.0 | 75.0 | |||
| Education | 23 | .89 | .38 | ||
| College | 33.3 | 25.0 | |||
| High school | 50.0 | 62.5 | |||
| Less than high school | 16.7 | 12.5 | |||
| Employment | 16.7 | 37.5 | 19 | .41 | .21 |
| Dependents | |||||
| No. of dependents | 3.2 (0.84) | 3.25 (1.75) | −0.06 (13) | .95 | .04 |
| No. of children | 2.67 (1.03) | 2.25 (1.83) | 0.50 (13) | .63 | .28 |
| Toddler’s age (months) | 23.00 (6.26) | 28.90 (8.63) | −4.10 (13) | .19 | .78 |
| Substance use history | |||||
| Referring clinic | 9 | .02 | .91 | ||
| Methadone | 0 | 62.5 | |||
| Outpatient | 100 | 37.5 | |||
| Age first used | |||||
| Cocaine/crack | 24.00 (3.2) | 20.00 (5.4) | 0.90 (8) | .40 | .90 |
| Heroin/opiates | 21.5 (.5) | 25.0 (7.0) | −0.51 (6) | .57 | .71 |
| Alcohol | 15.67 (1.37) | 14.43 (2.70) | 1.01 (13) | .33 | .58 |
| Cannabis | 15.50 (1.38) | 15.13 (1.96) | 0.40 (12) | .70 | .22 |
| Withdrawal symptoms | 7.5 (4.51) | 5.5 (4.72) | 0.75 (11) | .47 | .43 |
| Dependence symptoms | 6.5 (2.51) | 5.8 (2.96) | 0.50 (13) | .63 | .26 |
| Psychiatric symptoms | |||||
| Depression (BDI) | 17.67 (10.25) | 11.71 (8.02) | 1.18 (13) | .26 | .65 |
| State anxiety (STAI) | 54 (1.4)d | 47 (10.5) | 0.93 (11) | .39 | .96 |
| Trait anxiety (STAI) | 68 (12.8) | 52.5 (10.48) | 1.78 (11) | .13 | 1.36 |
| Trauma exposure | 4.3 (2.5) | 3.1 (2.0) | 1.25 (13) | .29 | .53 |
| PTSD symptoms | 2.83 (1.6) | 2.14 (1.9) | 0.70 (13) | .42 | .39 |
Note. N = 14. df = degrees of freedom; BDI = Beck Depression Inventory; STAI = State–Trait Inventory; PTSD = posttraumatic stress disorder.
t-test results are reported for continuous and chi-square results for categorical variables.
Effect size w computed for chi-square tests where 0.10 is considered small; 0.30, medium; and 0.50, large.
Effect size d computed for t tests where 0.20 is considered small; 0.50, medium; and 0.80, large (Cohen, 1988).
Italicized scores represent T scores or percentiles.
Proposed Mechanisms of Change
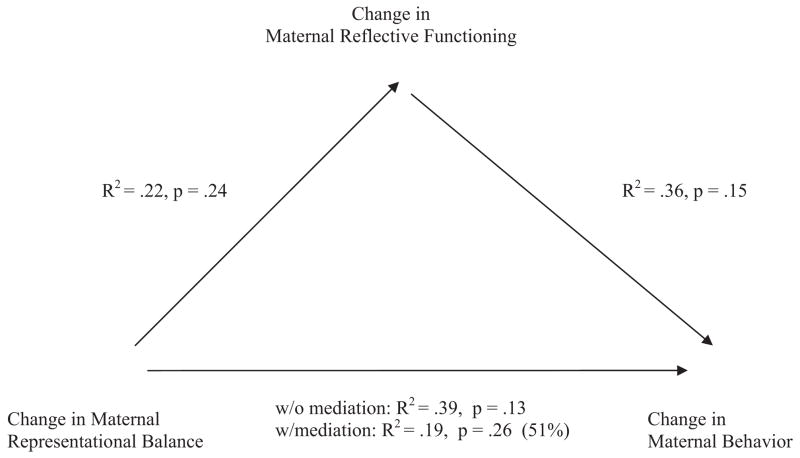
As shown in Table 3 and Figure 1, improvement in representational balance was meaningfully associated with improvement in reflective functioning (R2 = .22) and improvement in maternal behavior (R2 = .39). Improvement in reflective functioning was meaningfully associated with maternal behavior (R2 = .36). The magnitude of association between improvement in maternal representations and improvement in maternal behavior was reduced by 51% when variance resulting from improvement in maternal reflective functioning was first removed (ΔR2 = .19), indicating a partial mediation effect.
Table 3.
Hierarchical Regressions With and Without Test of Change in Maternal Reflective Functioning as Mediator of Associations Between Change in Maternal Representational Balance and Change in Maternal Caregiving Behavior
| Change in maternal behavior |
|||||
|---|---|---|---|---|---|
| Without mediation test | With mediation test | ||||
| Change in | Step | βa | ΔR2b | β | ΔR2 |
| Maternal reflective functioning | 1 | — | — | .60 | .36 |
| Maternal representational balance | 2 | .62 | .39 | .47 | .19 |
| Total R2 | .39 | .55 | |||
Note. N = 8.
Standardized beta weights.
Effect size criteria (Cohen, 1988) for R2 are as follows: .01 = small, .09 = medium, and .25 = large.
Figure 1.
Test of Mothers and Toddlers Program (MTP) treatment model: Change in maternal reflective functioning mediates effects of change in maternal representational balance on change in maternal behavior with toddler.
Discussion
The aim of this investigation was to examine preliminary treatment outcomes for the MTP, a 20-week parenting intervention for mothers enrolled in outpatient treatment for their substance abuse who are caring for toddlers ages 12 to 36 months. Differences in sociodemographic background and psychosocial adjustment between mothers who completed MTP and mothers who did not were also examined. Finally, the efficacy of the proposed attachment mechanisms on which the intervention is based was tested. Findings and limitations are discussed below.
Treatment Outcomes
Overall, mothers’ response to MTP on targeted representational outcomes showed meaningful shifts toward more balanced representations of caregiving and an increased capacity for reflective functioning. Mothers’ behavior with toddlers showed corresponding improvement in sensitivity to child cues, response to child distress, social–emotional growth fostering, cognitive growth fostering, and contingency of response. Together, these findings suggest that individual therapy for substance-abusing mothers that targets change at the representational level shows promise for bringing about changes at the behavioral level that have previously been resistant to change (see Suchman et al., 2004, 2006). During the 12-week episode of treatment, as a group, mothers’ psychosocial adjustment also improved and illicit drug use decreased. These changes may reflect an increased capacity for emotional regulation resulting from improvements in the mother’s representational world and reflective functioning capacity. No definitive conclusions can be drawn, though, about the temporal order of changes (e.g., whether improvement in representation preceded improvement in maternal behavior or maternal psychosocial adjustment) because posttreatment data were collected concurrently. Likewise, without data from a randomized control group, effects of substance abuse treatment and maturation cannot be ruled out as contributors to post-MTP improvements. A randomized pilot study in which mothers are randomly assigned to MTP versus a parent education control condition is currently under way to test the efficacy of MTP while controlling for confounding factors (e.g., maturation and other treatment effects).
Comparison of Treatment Completers With Noncompleters
As expected, mothers who completed treatment were generally at lower risk in terms of their sociodemographic characteristics and psychosocial adjustment. Treatment completers presented with a number of sociodemographic advantages including being older, Caucasian, employed, and married. Treatment completers also presented at intake having had less exposure to traumatic events, fewer psychiatric symptoms, and fewer symptoms of substance withdrawal and dependence. They were also more likely to be enrolled in methadone maintenance. Together, these findings suggest a need for more intensive outreach efforts and ancillary services to hold more disenfranchised and psychosocially at-risk mothers in the parenting program. For example, adapting MTP to accommodate programs for younger, first-time mothers and for the African American culture may increase its appeal and relevance to these special populations. Likewise, adapting MTP to be offered in conjunction with more intensive substance abuse and psychiatric treatment (e.g., intensive outpatient, partial hospital, inpatient, and residential settings) might address psychiatric vulnerabilities more quickly and increase retention. It is also possible that the more intensive treatment environment of methadone clinics and/or mothers’ neurophysiological responses to methadone treatment support more optimal responses to adjunct parenting interventions).
Proposed Mechanisms of Change
As predicted, improvement in maternal representational balance was meaningfully associated with improvement in maternal behavior with children (e.g., maternal sensitivity and responsiveness to cues and maternal social–emotional and cognitive growth fostering). Moreover, there is evidence that this association was partially mediated by improvement in maternal reflective functioning. These findings provide preliminary support for the proposed intervention model that improvement in representational balance supports the development of a greater capacity for understanding the intentional nature of behavior, which, in turn, promotes more optimal parenting (e.g., more sensitivity, responsiveness, and growth-fostering behavior) among mothers. However, because temporal sequences cannot be determined using cross-sectional data, the mediation model has not yet been fully tested. In the ongoing randomized pilot, we are conducting four waves of repeated measures with a subsample of mothers who have requested additional sessions in MTP. These data will be used to examine the temporal relations of changes in representation, reflective functioning, and maternal behavior in response to ongoing treatment.
Limitations not withstanding, the present study provides preliminary evidence that attachment-based parenting interventions with substance-abusing mothers are both feasible and potentially beneficial for improving maternal sensitivity and responsiveness to toddlers, behavioral indicators that are likely to promote children’s optimal social and emotional developmental. Moreover, preliminary findings from this study are consistent with the attachment theoretical framework on which the MTP intervention is based. There are many remaining questions, including (a) whether the intervention alone accounts for change in maternal representations and behavior and, if so, which elements of the intervention are the therapeutic ingredients; (b) whether changes in maternal representations and behaviors will last beyond the initial involvement period; (c) what the short- and long-term implications for children’s development are; and (d) whether longer or earlier involvement (e.g., starting at pregnancy or during infancy) will increase the magnitude of effects. There is also a need for parallel investigations of attachment-based interventions for substance-abusing parents that target mother–toddler dyads and caregiving fathers and that are delivered in diverse treatment settings (e.g., intensive outpatient and residential) by a range of clinicians (e.g., substance abuse clinicians, nurse practitioners, and para-professionals) to identify the most durable, efficient, and cost-effective approaches to preventing transgenerational cycles of substance abuse and maladaptive parenting.
Acknowledgments
Preparation of the manuscript was funded by Grants R01DA017294 and K23DA14606 from the National Institutes of Health. We thank Bruce Rounsaville, Kathy Carroll, Thomas McMahon, Arietta Slade, Elaine Fagan, Carolyn Parler-McCrae, Jean Larson, Carol Weber, Andy Campbell, Christine Lozano, Julie Scott, Jessie Borelli, Daryn David, and the APT Foundation for their contributions and support on this project.
Contributor Information
Nancy Suchman, Department of Psychiatry and Child Study Center, Yale University.
Cindy DeCoste, Department of Psychiatry, Yale University School of Medicine.
Nicole Castiglioni, Department of Psychiatry, Yale University School of Medicine.
Nancy Legow, Project Reward, Family and Childrens Agency Inc, Norwalk, CT.
Linda Mayes, Yale Child Study Center.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Barnard KE, Eyres SJ. Child health assessment, Pt. 2: The first year of life (Pub. No. DHEW No. HRA 79–25) Washington, DC: U.S. Government Printing Office; 1979. [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory Manual. 2. New York: Psychological Corporation; 1996. [Google Scholar]
- Bowlby J. Attachment and loss: Vol. 1. Attachment. 2. New York: Basic Books; 1982. [Google Scholar]
- Burns KA, Chethik L, Burns WJ, Clark R. The early relationship of drug abusing mothers and their infants: An assessment at eight to twelve months of age. Journal of Clinical Psychology. 1997;53:279–287. doi: 10.1002/(sici)1097-4679(199704)53:3<279::aid-jclp11>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. 2. Hillsdale, NJ: Erlbaum; 1983. [Google Scholar]
- DeCastro F, Mayes L. Maternal Attribution Scale. Yale Child Study Center; 2006. Unpublished manuscript. [Google Scholar]
- Derogatis LR. Brief Symptom Inventory: Administration, scoring, and procedures manual. 3. Minneapolis, MN: National Computer Systems; 1993. [Google Scholar]
- Dunlap WP, Cortina, Jose M, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychological Methods. 1996;1:170–177. [Google Scholar]
- Edelman GM, Tononi G. Neural Darwinism: The brain as a selectional system. In: Cornwell J, editor. Nature’s imagination: The frontiers of scientific vision. New York: Oxford University Press; 1995. pp. 78–100. [Google Scholar]
- Fonagy P, Gergely G, Jurist EL, Target M. Affect regulation, metallization, and the development of the self. New York: Other Press; 2002. [Google Scholar]
- Fonagy P, Target M. Attachment and reflective function: Their role in self-organization. Development & Psychopathology. 1997;9:679–700. doi: 10.1017/s0954579497001399. [DOI] [PubMed] [Google Scholar]
- Fonagy P, Target M, Steele H, Steele M. Reflective-Functioning Manual, Version 5. University College; London: 1998. Unpublished manuscript. [Google Scholar]
- Garson D. Reliability analysis. 2006 Retrieved January 21, 2007, from the North Carolina State University, College of Humanities and Social Sciences, Web site: http://www2.chass.ncsu.edu/garson/pa765/reliab.htm.
- Grienenberger J, Slade A. Maternal reflective functioning, mother-infant affective communication, and infant attachment: Exploring the link between mental states and observed care giving behavior. 2004 doi: 10.1080/14616730500245963. Manuscript in preparation. [DOI] [PubMed] [Google Scholar]
- Hans LL, Bernstein VJ, Henson LG. The role of psychopathology in the parenting of drug-dependent women. Development and Psychopathology. 1999;11:957–977. doi: 10.1017/s0954579499002400. [DOI] [PubMed] [Google Scholar]
- Karen R. Becoming attached. New York: Oxford University Press; 1994. [Google Scholar]
- Khantzian E. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry. 1997;4:231–244. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Koob GF. Hedonic valence, dopamine and motivation. Molecular Psychiatry. 1996;1:186–189. [PubMed] [Google Scholar]
- Koob GF, LeMoal M. Drug abuse: Hedonic homeostatic dysregulation. Science. 1997 October 3;278:52–58. doi: 10.1126/science.278.5335.52. [DOI] [PubMed] [Google Scholar]
- Leckman JF, Mayes LC. Understanding developmental psychopathology: How useful are evolutionary accounts? Child and Adolescent Psychiatry. 1998;37:1011–1021. doi: 10.1097/00004583-199810000-00010. [DOI] [PubMed] [Google Scholar]
- Levy DW, Truman S. Reflective functioning as mediator between drug use, parenting stress, and child behavior. Paper presented at the College on Problems of Drug Dependence Annual Meeting; Quebec City, Quebec, Canada. 2002. Jun, [Google Scholar]
- Luthar SS, Walsh KG. Treatment needs of drug-addicted mothers: Integrated parenting psychotherapy interventions. Journal of Substance Abuse Treatment. 1995;12:341–348. doi: 10.1016/0740-5472(95)02010-1. [DOI] [PubMed] [Google Scholar]
- Main M, Goldwyn R. Adult Attachment Classification System. University of California; Berkeley: 1985. Unpublished manuscript. [Google Scholar]
- Mayes L, Truman S. Substance abuse and parenting. In: Bornstein M, editor. Handbook of parenting: Vol. 4. Social conditions and applied parenting. 2. Mahwah, NJ: Erlbaum; 2002. pp. 329–359. [Google Scholar]
- Murphy S, Rosenbaum M. Pregnant women on drugs: Combating stereotypes and stigma. New Brunswick, NJ: Rutgers University Press; 1999. [Google Scholar]
- Pajulo M, Suchman NE, Kalland M, Mayes LC. Enhancing the effectiveness of residential treatment for substance abusing pregnant and parenting women: Focus on maternal reflective functioning and mother-child relationship. Infant Mental Health Journal. 2006;27:448–465. doi: 10.1002/imhj.20100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodning C, Beckwith L, Howard J. Quality of attachment and home environments in children prenatally exposed to PCP and cocaine. Development and Psychopathology. 1991;3:351–366. [Google Scholar]
- Slade A, Aber JL, Berger B, Bresgi I, Kaplan M. The Parent Development Interview—Revised. Yale Child Study Center; 2002. Unpublished manuscript. [Google Scholar]
- Slade A, Cohen LJ. The process of parenting and the remembrance of things past. Infant Mental Health Journal. 1996;17:217–222. [Google Scholar]
- Slade A, Grienenberger J, Bernbach E, Levy D, Locker A. Maternal reflective functioning and attachment: Considering the transmission gap. Paper presented at the biennial meeting of the Society for Research on Child Development; Minneapolis, MN. 2001. Apr, [Google Scholar]
- Sroufe LA, Carlson EA, Levy AK, Egeland B. Implications of attachment theory for developmental psychopathology. Development and Psychopathology. 1999;11:1–13. doi: 10.1017/s0954579499001923. [DOI] [PubMed] [Google Scholar]
- Suchman NE, Mayes L, Conti J, Slade A, Rounsaville B. Rethinking parenting interventions for drug dependent mothers: Fostering maternal responsiveness to children’s emotional needs. Journal of Substance Abuse Treatment. 2004;27:179–185. doi: 10.1016/j.jsat.2004.06.008. [DOI] [PubMed] [Google Scholar]
- Suchman NE, Pajulo M, DeCoste C, Mayes LC. Parenting interventions for drug dependent mothers and their young children: The case for an attachment-based approach. Family Relations. 2006;55:211–226. doi: 10.1111/j.1741-3729.2006.00371.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health & Human Services. Blending perspectives and building common ground: A report to Congress on substance abuse and child protection. Washington, DC: U.S. Government Printing Office.; 1999. [Google Scholar]
- Zeanah CH, Benoit D. Clinical applications of a parent perception interview in infant mental health. Infant Psychiatry. 1993;3:539–554. [Google Scholar]