Abstract
This study recruited four sociocentric networks (n = 156) of men who have sex with men in Budapest, Hungary, and St. Petersburg, Russia. The sampling approach was based on identifying an initial “seed” in the community for each network, and then recruiting three successive friendship group waves out from the seed. HIV prevalence in the networks was 9%, and the composite rate of other sexually transmitted diseases was 6%. 57% of participants reported both main and casual male partners, and two thirds reported unprotected anal intercourse in the past 3 months. Fifty-five percent of men’s most recent anal intercourse acts were with nonexclusive partners, and 56% of most recent anal intercourse acts were unprotected. Sexual risk predictors were generally consistent with behavioral science theory. In addition, risk was associated with more often talking with friends about AIDS, higher ecstasy use, and less often drinking. Sociocentric social network sampling approaches are feasible and constitute a modality for reaching hidden high-risk populations inaccessible through conventional methods.
Almost unknown during the socialist era, the HIV epidemic in parts of central and eastern Europe quickly accelerated beginning in the mid-1990s. Although HTV primarily first affected injection drug users (IDUs) in post-Soviet countries, transmission has shifted to a predominantly sexual pattern (UNAIDS, 2008). In spite of the rapid emergence of HIV in the region, there has been comparatively little published research on risk behavior as well as HIV/STD prevalence in postsocialist countries. Men who have sex with men (MSM) remain among the world’s most vulnerable populations, and research is needed to identify HIV risk behavior patterns and their determinants among MSM in eastern Europe. In addition, innovative approaches need to be tested that can access those MSM community segments likely to be missed using conventional sampling methods.
The appearance of the HIV epidemic in eastern Europe coincided with massive political, economic, and cultural transitions across the region. These included the breakup of the former Soviet Union and the appearance of new and sometimes fragile democracies in other former socialist countries. These transformations also resulted in fewer authoritarian controls, more personal freedoms including greater travel opportunities, liberalized sexual behaviors and norms, and increased drug use. In the context of these changes and given a weak public health infrastructure, intertwined HIV and sexually transmitted disease (STD) epidemics quickly emerged in many of the region’s countries (Borisenko, Tichonova, & Renton, 1999), Russia and Ukraine are among the countries hardest hit by the HIV epidemic, with a more gradual rise in central Europe. UNAIDS estimates that 940,000 in Russia and 3,000 in Hungary, a much smaller country (UNAIDS, 2008).
During the socialist era, homosexuality was officially proscribed, and there were few public meeting places where gay or bisexual men could openly and freely congregate. Most countries in the region—including both Hungary and Russia—have decriminalized same-sex behavior, and gay-identified venues appeared especially in larger cities. However, gay communities in most postsocialist countries are still relatively new, have little political influence, are neglected by public health authorities, and are inexperienced in dealing with the threat of AIDS. Although several writers pointed out some years ago the high potential HIV/AIDS vulnerability of MSM in post-Soviet countries (Chervyakov & Kon, 1998; Issayev, 1993; Kon, 1995), empirical research documenting levels of risk has been limited. However, past survey studies of community samples of MSM from Russia, Ukraine, Bulgaria, Hungary, and Slovakia have generally revealed high prevalence of unprotected sexual behaviors, frequent multiple sexual partnerships, and condom usage lower than found in studies of gay or bisexual men in the west (Amirkhanian et al., 2001; Amirkhanian et al,, 2006; Csepe et al., 2002; Kobyshcha et al, 1994; Stanekova, Habekova, Wimmerova, & Gramblickova, 2000).
A traditional sampling approach in HIV risk behavior studies among MSM relies on surveys conducted in public venues. Even though venues such as gay bars, clubs, or saunas now exist in eastern Europe, homophobic attitudes and stigma concerning homosexuality remain widespread. A large proportion of MSM in the region are likely to be “closeted,” hidden, and inaccessible through public venues alone. Recruitment strategies in which persons are identified by referral from others who know them can potentially reach these discreet community segments.
The sampling strategies most commonly used for reaching “hidden” community populations in HIV prevention research often focus on recruiting individuals referred by already-recruited participants. For example, the snowball method establishes a chain of recruitment in which a participant recruits someone else from his or her community (Goodman, 1961). In addition, the respondent-driven sampling approach uses snowball-like recruitment but with multiple-branch chains in which a participant is asked to recruit up to three other persons from their community (Heckathorn 1997, 2002). Social network approaches also utilize reference-based sampling modalities but, unlike other reference-based sampling methods, allow one to map all existing ties between individuals in a network. In addition, this permits a determination of whether ties are singular or reciprocal. The egocentric network sampling approach—previously widely utilized in past HIV prevention research (Amirkhanian, Kelly, Kabakchieva, Kirsanov, Vassileva, Takacs et al., 2005; Amirkhanian, Kelly, Kabakchieva, McAuliffe, & Vassileva, 2003; Amirkhanian, Kelly, & McAuliffe, 2005; Kang, Deren, Andia, Colon, & Robles, 2002; Kelly et al., 2006; Kottiri, Friedman, Neaigus, Curtis, & Des Jarlais, 2002; Latkin, Sherman, & Knowlton, 2003; Neaigus et al., 1996)—recruits a single individual from the community and then identifies and engages all members of this reference person’s network. The sociocentric approach is a more integrative method although highly underutilized with respect to HIV prevention research. Instead of recruiting multiple and usually small egocentric networks, the sociocentric approach suggests a modality that identifies, recruits, and determines ties between members of much larger community segments. A study by Friedman et al. (1997) recruited a large network of IDUs to determine associations between HIV serostatus and how individuals are imbedded in the network. However, such approaches have rarely been applied to community populations vulnerable to HIV owing to their sexual risk behavior rather than their injected drug use.
The present study’s purposes were to recruit four sociocentric networks of MSM, to determine the prevalence and predictors of HIV and other STDs in the sample, and to determine HIV risk behavior levels and predictors. In addition to its novel recruitment method, the study investigated levels of substance use and relationships between substance use and sexual risk behavior, an issue heretofore largely unexplored among MSM in central and eastern Europe.
METHODS
ENROLLMENT PROCEDURES
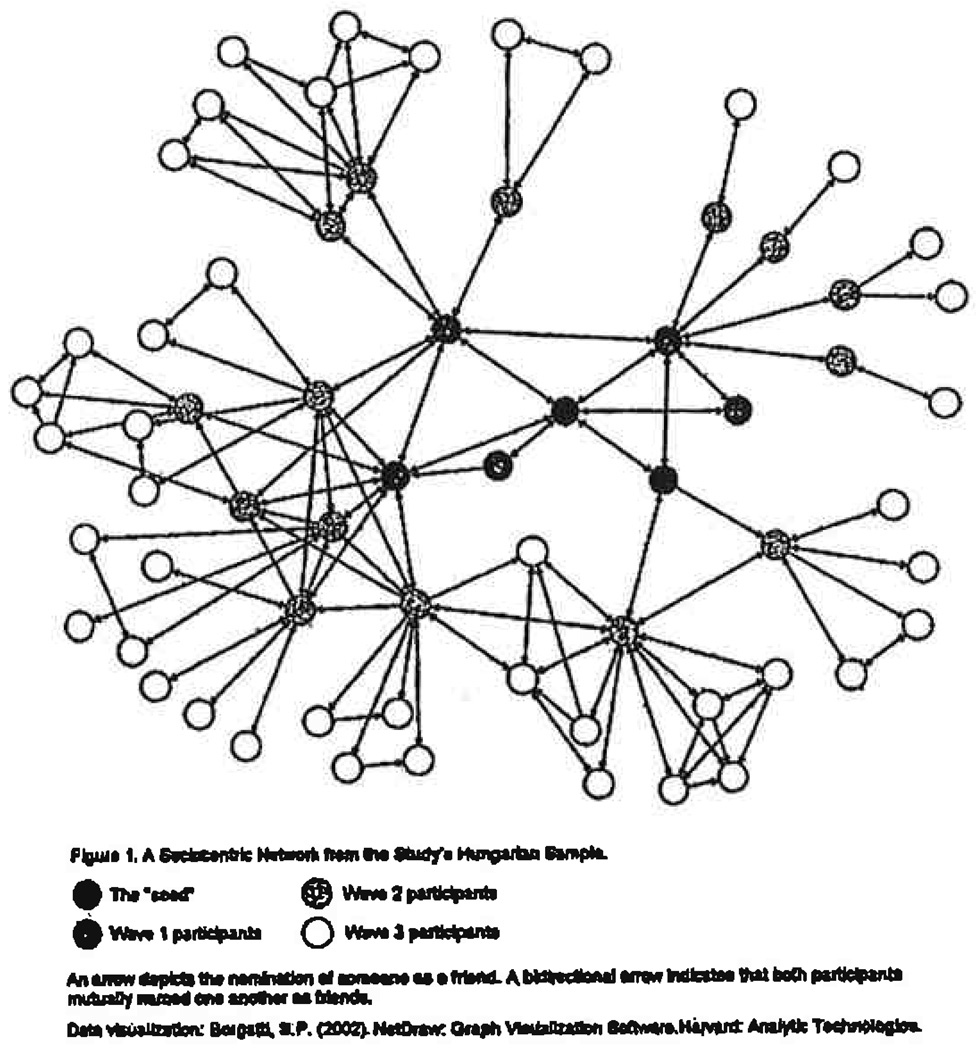
This study was carried out in Budapest, Hungary, and St. Petersburg, Russia, during late 2007, as a part of ongoing randomized, controlled multisite HIV prevention sociocentric network research trial. Both are major metropolitan cities with large gay communities and the highest HIV rates in their respective countries. We sought to recruit as many members as possible of four MSM sociocentric social networks, two networks in each city. Recruitment of each network began with the identification of an initial “seed” in an MSM community venue. The initial seed was an individual who appeared to be the center of attention among others in his social circle based upon systematic ethnographic observation in the venue. The seed was interviewed to identify all members of his immediate friendship group, who were consequently also recruited into the study. This established the first recruitment wave. All willing members of the first wave were interviewed to identify members of their own friendship groups. These individuals were in turn also asked to participate, and became the second recruitment wave. Some individuals from second-wave friendship groups had already been recruited in the first wave and were not reenrolled. The same process was repeated to enroll the third recruitment wave, with a fourth wave added in one Russian network to enhance the sample size. Thus, a sociocentric network was recruited by reaching out three to four waves from an initial seed. Across countries and networks, each participant of Waves 1 and 2 added a mean of 3.2 new participants (range: 0–8) to the overall network. Figure 1 illustrates an example of one of the Hungarian sociocentric networks.
Figure 1.
All network members came to a research office. Following an explanation of the study, willing participants provided written informed consent. They then completed assessment interviews and provided biospecimens for HIV/STD detection. Risk assessment interviews were conducted in private one-on-one sessions with an experienced interviewer that followed a structured protocol. Participants received an incentive payment equivalent to $40. The study was approved by the ethics committee of the Medical College of Wisconsin; Botkin Hospital of Infectious Diseases, St. Petersburg, Russia; and the Hungarian Academy of Sciences, Budapest, Hungary.
The number of enrolled MSM participants per network ranged from 19 to 65 (mean = 42), reflecting an average participation rate of 78.7%, The combined sample size of the four networks was 166.10 females had been named as members of MSM friendship groups. Because the focus of the study was on risk among MSM and there were too few females for subgroup analysis, they were not included in the study’s analyses. Therefore, the sample consisted of 156 MSM (118 from Budapest networks and 38 from St. Petersburg). We monitored to observe for the potential overlap of the same participant across multiple networks. However, there was no overlap.
STD AND HIV SPECIMEN COLLECTION AND ANALYSIS
HIV testing of blood specimens was performed using HIVenzyme-linked immunosorbent assay (ELISA) followed by a Western blot confirmatory test. Syphilis testing was performed by rapid plasma reagin and confirmed using the Treponema Pallidum particle agglutination test. After not urinating for at least 2 hours, initial-stream urine was collected in sterile polypropylene tubes. Chlamydia trachomatis (CT) and Neisseria gonorrhoeae (NG) DNA were extracted using Amplicor CT/NG specimen preparation kits (Roche Molecular Systems, Inc., USA) and were tested using Amplicor CT/NG polymerase chain reaction (PCR, Roche, Branchburg, NJ, USA). All STDs were treated following U.S. Centers for Disease Control and Prevention or national best-practice guidelines. Most participants who had HIV were aware of their status, and those with newly diagnosed HIV were referred to treatment facilities providing free HAART therapy.
HIV RISK ASSESSMENT INTERVIEW
Study measures, adapted from our previous HIV behavioral epidemiology research studies in eastern Europe (Amirkhanian et al., 2006), were developed, translated from, and back-translated into English. Individual assessment interviews usually lasted less than 1 hour.
Demographic data
Participants were asked about their age, years of education completed, and if they were currently employed or attending school. In addition, participants reported whether they personally knew someone with HIV, whether they had an STD ever and in the past year. Finally, participants used 5-point Likert scale to describe their sexual orientation (from exclusively heterosexual to exclusively homosexual) and whether they had any same-sex activity in the past year.
Psychosocial Scales
The interview included five AIDS-related psychosocial measures. A 15-item scale measured knowledge about AIDS risk and risk reduction steps (sample item: “If a man pulls out before orgasm, it protects from getting AIDS and venereal diseases”). Scores could range from zero to 15, reflecting the number of correct answers. A seven-item scale measured perceptions about safer sex peer norms (sample item: Condom use is accepted by my friends). For each statement, respondents answered yes, somewhat, or no, yielding scores between 0 and 14 (Cronbach’s alpha = .74). The same response options were used to measure attitudes towards condoms and safer sex (10 items, sample item: Using condoms interrupts the pleasure of sex). Scores could range from 0 to 20 (Cronbach’s alpha = .69). A 12-item scale with the same response format measured risk reduction behavioral intentions (sample item: ‘A condom will be used if I have sexual intercourse with a casual partner’), with scores ranging from 0 to 24 (Cronbach’s alpha = .76). Perceived risk reduction self-efficacy was assessed using a nine-item scale with the same response format (sample item: ‘I am sure that I can overcome my partner’s objections to safer sex or condoms’). Scores could range from 0 to 18 (Cronbach’s alpha = .56).
Sexual Risk Background and Sexual Practices During Lifetime, Past Year, Past 3 Months, and Most Recent Anal Intercourse
For both lifetime and the previous year, participants reported their number of male and female sexual partners, number of STD infections, and whether they had given or received money or valuables in exchange for sex. Participants then described specific behaviors occurring during the past 3 months using a partner-by-partner method. A set of questions inquired about sexual practices with up to five males—and up to five females—of participants’ most recent sexual partners during this time period. Respondents indicated whether each partner was main or casual, the number of occurrences of anal and vaginal intercourse with each partner, and the number of times condoms were used. The risk assessment interview elicited information about other sexual practices with male partners (such as oral sex), but the analyses reported here focus only on unprotected anal and vaginal intercourse because of their known and high association with HIV transmission. Participants with more than five partners of a given gender summarized their behavior with all additional partners.
Finally, participants described circumstances that characterized their most recent act of anal intercourse. These included type of sexual partner, whether they were the insertive or receptive partner, and whether or not a condom was used. In addition, participants reported whether they consumed alcohol and the number of alcoholic drinks consumed within 3 hours prior to sex. They also indicated whether or not they used drugs prior to sex and they specified the type of drug. Finally, participants estimated the extent to which they were drunk or high at the time of sex.
Substance Use
Participants reported how many alcohol drinks they had in the past week. In addition, they responded to a battery of questions to specify on how many days in the past month they used any alcohol, alcohol to intoxication, heroin, methadone, other opiates/analgesics, barbiturates, other sedatives/tranquilizers, cocaine, amphetamines, marijuana/hashish, hallucinogens, ecstasy, gamma hydroxybutyrate (GHB), inhaled nitrites (“poppers”), and Viagra. Finally, respondents indicated on how many days in the past month they injected drugs.
STATISTICAL METHODS
Following a description of the demographic backgrounds, substance use, sexual risk behavior, and HIV risk-related attitudes of MSM participants in each country, we examined factors predicting anal intercourse risk and condom use. Because the members of each social network were not selected independently, responses of members within the same social network were correlated. To account for the dependency among these responses, the network identifier was included as a random effect in each regression model. Multivariate generalized mixed-effect regression that incorporated social network as a random effect variable was used to analyze the data. Within this framework, Poisson regression models analyzed counts for the number of UAI occasions and number of UAI partners, as both of these outcomes had highly skewed distributions. A logistic regression model was used to analyze the three dichotomous measures: whether participants had any UAI, had any UAI with a casual partner and had UAI with multiple partners. The percentage of condom-protected anal intercourse was analyzed using a linear regression model because this variable closely satisfied the normal distribution assumption. The statistical program GLIMMIX (SAS Institute) was used for all the multivariate regression analyses. An indicator (0/1) variable for country and demographic variables for age, education and employment status were included in all the regression models. Other variables included in the models were selected from a series of preliminary univariate analyses conducted to evaluate their association with each of the six primary outcomes. Those predictors found in univariate analyses to have a p value less than 0.10 were entered in the multivariate regressions.
RESULTS
PARTICIPANT CHARACTERISTICS
The mean age of participants was 28.1 years, with a mean education level of 15.3 years. Among the participants, 72.4% (n = 113) were permanently employed, and 40.4% (n = 63) were students. Of men in the sample, 96.8% (n = 151) reported same-sex activity in the past year. With respect to sexual orientation, 75.4% (n = 89) of Hungarian participants but only 34.2% (n = 13) of the Russian sample identified themselves as exclusively homosexual. The percentage of participants who reported ever having had an STD was 29.5% (n = 46), and 7.7% (n = 12) reported having an STD in the past year. Fifty-eight (49.2%) of Hungarian participants and 11 (20.9%) of Russian men said they personally knew someone with HIV.
STD AND HIV PREVALENCE
Excluding three participants who declined HIV testing, 9.2% (n = 14) of the study sample had positive laboratory HIV test results, 5.3% (n = 2) in Russia and 10.4% (n = 12) in Hungary. All but one of the individuals already knew of their HIV-positive status before testing performed in the study. In addition, 5.9% (n = 9) of participants had positive laboratory results for one of the other STDs, 10.5% (n = 4) in Russia and 4.3% (n = 5) in Hungary. STDs were predominantly chlamydia (3.3%, n = 5) but also gonorrhea (1.3%, n = 2) and syphilis (0.7%, n = 1). The two countries’ samples did not significantly differ in the prevalence of any disease.
SEXUAL RISK BEHAVIOR LEVELS AND SUBSTANCE USE
Almost all participants in the sample reported a history of having sex with men in their lifetimes (96.8%, n = 151), in the past year (96.2%, n = 150), and during the past 3 months (93.0%, n = 145). Russian men in the sample were more likely than Hungarians to be behaviorally bisexual; 23.7% (n = 9) of Russian MSM had both male and female partners during the past year compared with only 1.7% (n = 2) of Hungarian MSM (p < .001).
Table 1 summarizes sexual risk behaviors reported by participants during the past 3 months. As the table shows, the most common pattern of sexual partnership was having both a main and also additional partners, reported by 57.1% of men in the past 3 months. Although participants had an average of only one main partner during this period, they also had z mean of 4.7 (median = 3) other male partners. Sexual behaviors were generally safer with casual partners than with main partners, including less frequent UAI and greater levels of condom use in the past 3 months. However, recent UAI was reported by approximately two thirds of men in the sample, with a mean of 18.5 (median = 10) unprotected acts in the past 3 months. Although 54.5% of men engaged in UAI with their main partners, 25.0% reported UAI with a casual partner and 22.4% did so with multiple partners during the same time period.
TABLE 1.
HIV Risk-Related Scales and Sexual Risk Practices During the Past 3 Months by MSM in Hungary and Russia
| Variable | Total (N=156) | Hungary (n = 118) | Russia (n= 38) |
|---|---|---|---|
| HIV risk-related scales, mean (median) | |||
| AIDS risk behavior knowledge | 13.5(14) | 13.7(14) | 12.8(13) |
| Safer sex peer norms | 10.5(11) | 10.6(11) | 10.1(11) |
| Attituides toward condoms and safer sex | 12.0(12) | 12.0(12) | 12.1(12) |
| Risk reduction behavioral intentions | 16.4(17) | 16.9(17) | 14.8(16) |
| Perceived risk reduction self-efficacy | 14.8(15) | 14.7(15) | 15.2(16) |
| Types of sexual relationships during the past 3 months, % (n) | |||
| None | 3.8%(6) | 3.4%(4) | 5.3%(2) |
| Single main partner | 19.9%(31) | 17.8%(21) | 26.3%(10) |
| Single non-main partner | 1.9%(4) | 2.5%(3) | 0.0%(0) |
| Both main and non-main partners | 57.1%(89) | 56.8%(67) | 57.9%(22) |
| Multiple non-main partners | 17.3%(27) | 19.5%(23) | 10.5%(4) |
| Number of sexual partners in the past 3 months, mean (median) | |||
| Number of male partners | 4.7(3) | 4.9(3) | 3.9(2) |
| Number of main male partners | 0.9(1) | 0.9(1) | 1.0(1) |
| Proportion of participants reporting in the past 3 months, % (n) | |||
| Any UAI | 67.3%(105) | 72.0%(85) | 52.6%(20) |
| UAI with main partner | 54.5%(85) | 57.6%(68) | 44.7%(17) |
| UAI with non-main partners | 25.0%(39) | 28.0%(33) | 15.8%(6) |
| UAI with multiple partners | 22.4%(35) | 24.6%(29) | 15.8% (6) |
| Frequency of UAI act in the past 3 months, mean (median)b | |||
| With any partner | 18.5(10) | 16.3(9) | 27.8(10.5) |
| With a main partner | 14.9(8) | 14.3(8) | 17.2(8.5) |
| With non-main partners | 1.3(0) | 1.3(0) | 1.4(0) |
| Proportion of condom use for anal intercourse in the past 3 months, mean % (median)c | |||
| With any partner | 50.1%(100) | 49.6%(100) | 51.5%(100) |
| With a main partner | 37.6%(10) | 35.3%(7.9) | 44.8%(16.7) |
| With non-main partners | 73.7%(100) | 74.0%(100) | 72.0%(100) |
Note. MSM = men who have sex with men; UAI = unprotected anal intercourse.
For numerical measures, the Mann-Whitney U test was used to evaluate statistical significance of country differences. For categorical variables, Pearson’s chi-square was used.
The analyses included 105 men who had had any UAI in the past 3 months.
The analyses included 139 men who bad had any anal intercourse in the put 3 months.
One hundred forty-eight participants completed interview questions concerning their most recent anal intercourse with a male partner. Presumably, the other eight men in the sample had never engaged in anal sex. With respect to their last anal intercourse with a male, 44.6% (n = 68) of participants reported that the act was with an exclusive partner, but 55.4% (n = 82) said it was with either a regular but nonexclusive, casual, or new partner. Insertive (42.7%, n = 61) and receptive roles (55.2%, n = 79) were relatively balanced. Condoms were used in only 44.2% (n = 65) of participants’ most recent anal intercourse, and 55.8% (n = 82) of men’s most recent anal intercourse occasions were unprotected.
Approximately 3% (n = 5) of participants said that they had received money or valuables in exchange for sex during the past year. Paying for sex was more common. 7.7% (n = 12) of men paid someone for sex during the past year, with rates higher (p < .04) among Russian MSM (15.8%, n = 6) than among Hungarians (5.1%, n = 6). 9.6% (n = 15) of participants had either bought or sold sex during the past year.
The portion of the interview assessing substance use inquired about behavior during the past 30 days. Alcohol was a substance most commonly used, reported by 96.2% (n = 150) of participants. Men drank alcohol on a mean of 6.6 days (median = 5), and 41% (n = 64) said they had been drunk during this time period. Poppers were used by 21.2% (n = 33) of men and GHB was used by 10.3% (n = 16), primarily among MSM in Hungary; marijuana or hashish by 15.4% (n = 24) of men; and amphetamines by 3.8% (n = 6) of men. Other substances including injected drugs were used by smaller numbers of men (<1.0%) in the past month.
MULTIVARIATE REGRESSION PREDICTORS OF ENGAGING IN HIV SEXUAL RISK PRACTICES
Table 2 depicts predictors of frequencies of several HIV risk behaviors reported by participants and percent of condom-protected anal intercourse occasions. The data show that measures of safer sex behavioral intentions, attitudes, and self-efficacy—in various combinations—consistently predicted lower numbers of unprotected intercourse occasions and partners and higher rates of condom use. In addition, cofactors in the multivariate analysis often also included substance use. For example, the use of ecstasy in the past month was strongly associated with greater numbers of UAI partners. However, more frequent use of alcohol in the past month predicted fewer UAI occasions and a higher percentage of condom use for anal intercourse. Surprisingly, higher frequency of talk with friends about AIDS in the past 3 months predicted both higher number of UAI occasions and UAI partners.
TABLE 2.
Multivariate Regression Models Predicting Number of Unprotected Anal Intercourse (UAI) Acts Number of UAI partners, and percent of Condom Use for Anal intercourse in the Past 3 Months Within Sociocentric Networks of MSM in Hungary and Russia
| Outcome Variable |
||||||
|---|---|---|---|---|---|---|
| Number of UAI Occasionsb |
Number UAI Partnerb |
Percent of condom Use for UAI |
||||
| Predictorsa | Coefficient | P | Coefficient | P | Coefficient | P |
| Country (Hungary = 1) | n.s. | n.s. | n.s. | |||
| Age (in years) | n.s. | −.022 | .070 | n.s. | ||
| Education (in years) | −.085 | .067 | n.s. | n.s. | ||
| Currently employed (0/1) | n.s. | n.s. | n.s. | |||
| Ever tested for HIV prior to the study (0/1) | .639 | .083 | n.s. | n.s. | ||
| Number of days of alcohol use, past month | −.095 | .004 | n.s. | 1.727 | .012 | |
| Used any ecstasy in the past month (0/1) | n.s. | 0.852 | <.001 | n.s. | ||
| Number of talks with friends about AIDS, past 3 months | .023 | <.001 | .014 | .004 | n.s. | |
| HIV/AIDS risk knowledge | n.s. | .190 | <.001 | n.s. | ||
| Safer sex intentions | n.s. | −.060 | .002 | 3.150 | <.001 | |
| Condom and safer sex attitudes | −.068 | .094 | −.044 | .057 | 2.268 | .021 |
| Safer sex self-efficacy | n.s. | −.063 | .044 | n.s. | ||
Note
All analyses included data on 156 participants. The indicator for country (research site) and demographic variables for participants’ age, education, and employment status were included in each of the models. Additional predictors were chosen from a preliminary series of bivariate regressions for each of the outcome variables. Those predictors that achieved a p-value <0.10 in one of these analyses were included all three multivariate models. Variables that did not quality for inclusion based on this criterion included: knowing an HIV-positive person; number of discussions with friends about safer sex in the past 3 months; safer sex peer norms; number of days one got drunk from alcohol in the past month; used any marijuana or hashish in die past month; used any amphetamines in the past month; used any GHB in the past month; used any poppers in the past month; and used any Viagra in the past month.
The model was estimated using Poisson regression for this outcome variable. n.s.= not significant (p > .10)
Table 3 presents predictors of whether participants had any UAI, and also whether they had UAI with a casual partner or with multiple partners in the past 3 months. Positive safer sex attitudes were associated with lower odds of unprotected anal sex. Predictors of engaging in unprotected anal sex with multiple or casual partners during the past 3 months included lower intentions to practice safer sex and weaker risk reduction self-efficacy.
TABLE 3.
Multivariate Logistic Regression Models Predicting Occurrences of Unprotected Anal Intercourse (UAI), UAI with a Casual Partner and UAI with Multiple Partners in the Past 3 Months Within Sociocentric Networks of MSM in Hungary and Russia
| Outcome Variable |
||||||
|---|---|---|---|---|---|---|
| Had Any UAI |
Had UAI With a Casual Partner |
Had UAI With Multiple Partners |
||||
| Predictorsa | OR | 95% Cl | OR | 95% Cl | OR | 95% Cl |
| Country (Hungary=1) | n.s | n.s | n.s | |||
| Age (in years) | n.s | n.s | n.s | |||
| Education (in years) | n.s | 1.17 | 0.99, 1.37† | n.s | ||
| Currently employed (0/1) | n.s | n.s | n.s | |||
| Used any marijuana/hashish in past month (0/1) | n.s | n.s | n.s | |||
| Used any poppers in the past month (0/1) | n.s | n.s | n.s | |||
| HIV/AIDS risk knowledge | n.s | n.s | n.s | |||
| Safer sex intentions | 0.91 | 0.82, 1.01* | 0.90 | 0.99, 1.37* | 0.85 | 0.75, 0.97** |
| Condom and safer sex Attitudes | 0.86 | 0.76, 0.97** | n.s | n.s | ||
| Safer sex self-efficacy | n.s | 0.77 | 0.63, 0.93*** | 0.64 | 0.50, 0.83**** | |
Note. OR = odds ratio; CI = confidence interval; n.s. = not significant (p > .10).
All analyses included data on 156 participants. The indicator for country (research site) and demographic variables for participants’ age, education, and employment status were included in each of the models. Additional predictors were chosen from a preliminary series of bivariate regression for each of the outcome variables. Those predictors that achieved a p-value < 0.10 in one of these analyses were included all three multivariate models. Variables that did not qualify for inclusion based on this criterion included: knowing an HIV-positive person; number of discussion with friends about AIDS, and number of discussion about safer sex. in the past 3 months; safer in peer norms; number of day of alcohol use in the past month; number of days one got drunk from alcohol in the past month; used any amphetamines in the past month; used any ecstasy in the past month; used any GHB in past month; and used any Viagra in the past month.
p < .10,
p < .05,
p < .01,
p < .001.
Not included in the tables, we also examined multivariate predictors condom use during participants’ most recent anal intercourse with a male partner (147 participants who responded on this outcome were included in the analysis). The mixed logistic regression model again controlled for group effects by entering network as a random factor. Use of a condom during anal intercourse on this occasion was predicted by having sex with a casual or new partner (odds ratio [OR] = 15.03, 95% confidence interval [CI] = 5.66, 39.96, p < .0001), stronger risk reduction behavioral intentions (OR = 1.23,95% CI = 1.08, 1.39, p < .01), and personally knowing someone with HIV (Partial OR = 5.48, 95% CI = 1.95, 15.40, p < .01).
DISCUSSION
This is the first study to utilize a sociocentric network sampling approach with respect to determining sexual HIV risk levels and prevention needs. Traditionally, community-based research studies often utilize social venues frequented by target community members to recruit participants. This has also been predominantly the case in research among MSM. However, venue-based MSM samples are likely to underrepresent the community. Many locations, including in eastern Europe, lack openly accessible gay-identified venues, and existing venues such as gay bars or nightclubs—widely utilized by many MSM in the past to find new sexual partners—are less likely to represent the community. This is because Internet Web sites provide alternative methods to find a partner (Benotsch, Kalichman, & Cage, 2002; Elford, Bolding, & Sherr, 2001; Ross, Tikkanen, & Mansson, 2000) and this might reduce attendance at venues by sex or partner seekers. In addition, high levels of stigma characterize many at-risk populations and lead vulnerable persons to remain hidden. These circumstances raise the likelihood that venues may no longer be the primary gates for accessing the most risky MSM community segments and methods for more effectively sampling MSM may include referral by other participants.
In this light, the sociocentric network sampling methodology used in the current study allows one to recruit successive waves of individuals from a community by beginning with a single or with a very few “seeds” even in circumstances where there exist very few community recruitment venues. The study demonstrated the feasibility of using a sociocentric approach to recruit a sample—characterized by high HIV sexual risk and substance use levels—with a relatively high response rate.
There have been few past HIV seroprevalence studies of MSM in Russia or Hungary. Although this research used a social network rather than venue-based or representative community sampling method, the overall HIV prevalence rate of 9% is consistent with or is greater than found in some prior community samples in the region (Kolpakova, 2008; Sergeev, 2008). This may reflect increasing HIV trends or could be due to our recruitment of high-risk community clusters.
With respect to behavioral risk, several findings are especially noteworthy. First, the modal sexual pattern observed in the sample reflected sexual partner concurrency, with most men reporting both main and also multiple casual partners in the past 3 months. MSM in Russia have been previously shown to often report both male and female partners (Amirkhanian, 2001), a pattern also found in the present study. Although UAI was more common during sex with main partners than non-main partners during the past 3 months, a substantial proportion of men reported at least some occurrences of UAI during sexual encounters with males who were not their main partners. This was especially borne out by the profile of factors present during participants’ most recent act of anal intercourse. These acts most frequently occurred with partners who were not usually exclusive boyfriends but instead were nonexclusive regular, casual, or new partners. Further, condoms were not used a majority of the time. Collectively, these findings underscore the high disease vulnerability of gay or bisexual men in these countries.
Across a variety of risk indicators including any occurrence of UAI, frequency of UAI, and levels of condom use in the past 3 months, scales measuring psychosocial factors including condom attitudes, risk reduction behavioral intentions, and self-efficacy generally predicted riskiness of sexual behavior in a manner consistent with reasoned action and social cognitive theories (Bandura, 1986; Fishbein & Ajzen, 1975). Conceptual formulations shown to predict risk behavior in western populations were generally borne out in this sample of Russian and Hungarian MSM. However the positive association of frequency of talk with friends about AIDS with higher sexual behavioral risk levels was surprising. However, we do not know whether this talk was about the disease, whether the information exchanged was accurate, or whether it was about prevention. Further research is needed to explore the content of AIDS communication that occurs among friends and to establish ways to increase the effectiveness of informal AIDS prevention communication in reducing risk, particularly because information coming from friends is likely to be trusted.
The role of substance use was also identified in the sample. Unexpectedly, the greater the number of days on which any alcohol was used either did not predict risk or else showed a protective effect. Relationships between risky sex and alcohol use are complex, and involve the interplay of both global- and event-level associations (Leigh & Stall, 1993). More research on relationships between alcohol use and high-risk sex in eastern European MSM samples is needed. The findings also show the emergence of recreational or “club” drug use in the eastern European sample and the association of ecstasy with indicators of sexual risk behavior. This association is well known in research conducted with samples of gay and bisexual men in the west. The emergence of similar patterns has not been previously documented among MSM in postsocialist countries.
This research has several limitations. Sociocentric methods may not reach socially isolated at-risk persons who have no friendship connections with other MSM. The sample size in the current study was modest and consisted of members of only four sociocentric networks. The statistical analysis for this paper included an effect for sociocentric social network. However, it did not include information resulting from individual friendship links within a network. Not all members of the networks participated. In addition, social networks are not necessarily a representative community sample, and these findings may not generalize to a larger community. Finally, self-reports of sexual and substance use behaviors are subject to bias, recall inaccuracy, stigma, or drug illegality.
Although this study was not a test of an intervention, it establishes a foundation for developing HIV prevention interventions that may utilize network leadership and information flow channels to reduce risk behaviors. Social network methods are culturally relevant for work with populations in eastern European postsocialist countries where personal networks have historically played—and continue to play—an important role for mutual assistance and the exchange of resources and reliable information (Rona-Tas, 1999). The same patterns are also true of populations elsewhere that experience severe underdevelopment and economic hardships (Cook, 1993). African American MSM in the United States constitute another population that may be hard-to-reach except through other members of their own social networks. Future research is needed to test sociocentric network sampling approaches to address HTV risk in other populations, to examine sociocentric network research opportunities related to other public health concerns, and to identify network-based attributes responsible for both risk taking by network members and how network attributes can serve to support risk reduction behavior changes.
Acknowledgments
This research was supported by Grant R01-DA023854 from the National Institute on Drug Abuse and Grant P30-MH52776 from the National Institute of Mental Health. The authors thank Dmitry G. Pirogov, Maria N. Donskaya, Victoria N. Rozmanova, Alexander Y, Komarovsky in Russia and Ferenc Szabo and Andras Szell in Hungary for their assistance.
Footnotes
Notice: This material may be protected by copyright law (Title 17 U.S. Code)
REFERENCES
- Amirkhanian YA, Kelly JA, Kabakchieva E, Kirsanova AV, Vassileva S, Takacs J, et al. A randomized social network HIV prevention trial with young men who have sex with men in Russia and Bulgaria. AIDS. 2005;19:1897–1905. doi: 10.1097/01.aids.0000189867.74806.fb. [DOI] [PubMed] [Google Scholar]
- Amirkhanian YA, Kelly JA, Kabakchieva E, McAuliffe TL, Vassileva S. Evaluation of a social network HIV prevention intervention program for young men who have sex with men in Russia and Bulgaria. AIDS Education and Prevention. 2003;15:205–220. doi: 10.1521/aeap.15.4.205.23832. [DOI] [PubMed] [Google Scholar]
- Amirkhanian YA, Kelly JA, Kirsanova AV, DiFranceisco WJ, Khoursine RA, Semenov AV, Rozmanova VN. HIV risk behavior patterns, predictors, and STD prevalence in young MSM social networks in St, Petersburg, Russia. International Journal of STD & AIDS. 2006;17:50–56. doi: 10.1258/095646206775220504. [a] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amirkhanian YA, Kelly JA, Kukharsky AA, Borodkina OI, Granskaya JV, Dyatlov RV, et al. Patterns and predictors of HIV risk behavior in a large community sample of Russian men who have sex with men: Evidence of a new emerging epidemic in eastern Europe. AIDS. 2001;15:407–412. doi: 10.1097/00002030-200102160-00014. [DOI] [PubMed] [Google Scholar]
- Amirkhanian YA, Kelly JS, McAuliffe TL. Identifying, recruiting, and assessing social networks at high risk (or HIV/AIDS: Methodology, practice, and a case study in St. Petersburg, Russia. AIDS Care. 2005;17:58–75. doi: 10.1080/09540120412331305133. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social foundation of thought and action: A social cognitive theory. Engle-wood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- Benotsch EG, Kalichman SC, Cage M. Men who have sex partners via the Internet: Prevalence, predictors, and implications for HIV prevention. Archives of Sexual Behavior. 2002;31:177–183. doi: 10.1023/a:1014739203657. [DOI] [PubMed] [Google Scholar]
- Borisenko KK, Tichonova LI, Renton AM. Syphilis and other sexually transmitted infections in the Russian Federation. International Journal of STD and AIDS. 1999;10:665–668. doi: 10.1258/0956462991913240. [DOI] [PubMed] [Google Scholar]
- Chervyakov V, Kon IS. Sex education and HIV prevention in the context of Russian politics. In: Rosenbrock R, editor. Politics behind AIDS politics: case studies from India, Russia, and South Africa. Berlin: Wissen schaftszentrum Berlin for Sozialforschung; 1998. [Google Scholar]
- Cook HBK. Antropológica. Caracas, Venezuela: Institute Caribe de Antropología y Sociología. Fundación La Salle de Ciencias Naturales; 1993. Small town, big hell. An ethnographic study of aggression in a Mar-gariteño community. [Google Scholar]
- Csepe R, Amirkhanian YA, Kelly JA, McAuliffe TL, Mocsonaki L. HIV risk behaviour among gay and bisexual men in Budapest, Hungary. International Journal of STD and AIDS. 2002;13:192–200. doi: 10.1258/0956462021924785. [DOI] [PubMed] [Google Scholar]
- Elford J, Bolding G, Sherr L. Seeking sex on the Internet and sexual risk behaviour among gay men using London gyms. AIDS. 2001;15:1409–1419. doi: 10.1097/00002030-200107270-00010. [DOI] [PubMed] [Google Scholar]
- Fishbein M, Ajzen I. Attitude, intention, and behavior: An introduction to theory and research. Reading, MA: Addison-Wesley; 1975. [Google Scholar]
- Friedman SR, Neaigus A, Jose B, Curtis R, Goldstein M, Ildefonso G, et al. Sociometric risk networks and risk for HIV infection. American Journal of Public Health. 1997;87:1289–1296. doi: 10.2105/ajph.87.8.1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman LA. “Snowball sampling”. Annals of Mathematical Statistics. 1961;32:148–170. [Google Scholar]
- Heckathorn DD. ’Respondent-driven sampling: A new approach to the study of hidden populations. Social Problems. 1997;44:174–199. [Google Scholar]
- Heckathorn DD. Respondent-driven sampling II: Deriving valid estimates from chain-referral samples of hidden populations. Social Problems. 2002;49:11–34. [Google Scholar]
- Issayev DD. Survey of the sexual behaviour of gay men in Russia. International Lesbian and Gay Association Bulletin. 1993;3:12. [Google Scholar]
- Kang SY, Deren S, Andia J, Colon HM, Robles RR. Egocentric HIV risk networks among Puerto Rican crack users in New York and Puerto Rico: Impact on sex risk behaviors over time. AIDS Education and Prevention. 2005;17:53–67. doi: 10.1521/aeap.17.1.53.58684. [DOI] [PubMed] [Google Scholar]
- Kelly JA, Amirkhanian YA, Kabakchieva E, Vassileva S, McAuliffe TL, DiFranceisco WJ, et al. Prevention of HIV and sexually transmitted diseases in high-risk social networks of young Roma (Gypsy) men in Bulgaria: Randomised controlled trial. British Medical Journal. 2006;333:1098–1101. doi: 10.1136/bmj.38992.478299.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobyshcha Y, Kruglov Y, Secheiko H, Schebinskaya A, Morosov V, Stoyan H. HIV risk-related sexual behaviour of homo- and bisexual men and STD patients m Ukraine; Paper presented at the International Conference on AIDS; Yokahama, Japan. 1994. Aug, Abstract PC0101. [Google Scholar]
- Kolpakova O. Second generation surveillance study among MSM in St. Petersburg; Paper presented at the Second eastern Europe and Central Asia AIDS Conference; Moscow, Russia. 2008. may, [Google Scholar]
- Kon IS. The sexual revolution in Russia: From the age of the czars to today. New York: The Free Press; 1995. [Google Scholar]
- Kottiri BJ, Friedman SR, Neaigus A, Curtis R, Des Jarlais DC. Risk networks and racial/ethnic differences in the prevalence of HIV infection among injection drug users. Journal of Acquired Immune Deficiency Syndromes. 2002;30:95–104. doi: 10.1097/00042560-200205010-00013. [DOI] [PubMed] [Google Scholar]
- Latkin CA, Sherman S, Knowlton A. HIV prevention among drug users: Outcome of a network-oriented peer outreach intervention. Health Psychology. 2003;22:332–339. doi: 10.1037/0278-6133.22.4.332. [DOI] [PubMed] [Google Scholar]
- Leigh BV, Stall R. Substance use and risky sexual behavior for exposure to HIV: Issues in methodology, interpretation, and prevention. American Psychologist. 1993;48:1035–1045. doi: 10.1037//0003-066x.48.10.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neaigus A, Friedman S, Jose B, Goldstein M, Curtis R, Ildefonso G, et al. High-risk personal networks and syringe sharing as risk factors for HIV infection among new drug injectors. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 1996;11:499–509. doi: 10.1097/00042560-199604150-00011. [DOI] [PubMed] [Google Scholar]
- Rona-Tas A. Ustoychivost’ sotsial’nykhsetey v postkommunisticheskoy transformatsii: Vostochnoy Evropy [Sustainability of social networks in the eastern European postcommunist transformation. In: Sahanin T, editor. Informal economy, Russia, and the world. Moscow: Logos (in Russian); 1999. pp. 396–411. [Google Scholar]
- Ross MW, Tikkanen R, Manssion S. Differences between Internet samples and conventional samples of men who have sex with men; Implications for research and HIV interventions. Social Science and Medicine. 2000;51:749–758. doi: 10.1016/s0277-9536(99)00493-1. [DOI] [PubMed] [Google Scholar]
- Sergeev B. Results of the MSM polls; Paper presented at the Second eastern Europe and Central Asia AIDS Conference; Moscow, Russia. 2008. May, [Google Scholar]
- Stanekova D, Habekova M, Wimmerova S, Gramblickova I. HIV infection and sexual behaviour among homosexual and bisexual men in Bratislava. Central European Journal of Public Health. 2000;8:172–175. [PubMed] [Google Scholar]
- UNAIDS. 2008 Report on the global AIDS epidemic. Geneva, Switzerland: Author; 2008. [Google Scholar]