Abstract
Objectives
The Multi-Ethnic Study of Atherosclerosis (MESA) is a population-based study of 6,814 men and women. We sought to analyze the relationship between the extent of coronary calcium (CC) at baseline and the severity of coronary stenoses in clinically indicated coronary angiography studies during follow-up.
Background
CC is an established predictor of major cardiovascular events. Yet, the relationship between CC and the distribution and severity of coronary artery stenoses has not been widely explored.
Methods
All MESA participants underwent non-contrast enhanced cardiac CT during enrollment to determine baseline CC. We analyzed 175 consecutive angiography reports from participants who underwent coronary catheterization for clinical indications during a median follow-up period of 18 months. The association between baseline CC and the severity of coronary stenosis detected in coronary angiographies was determined.
Results
Baseline Agatston score was zero in only 7/175 (4%) MESA participants who underwent invasive angiography during follow-up. When coronary arteries were studied separately, 13–18% of coronary arteries with ≥75% stenosis had zero calcium mass scores at baseline. There was close association between baseline calcium mass score and the severity of stenosis in each of the coronary arteries (test for trend, p<0.001). As an example, mean calcium mass scores for <50, 50–74 and ≥75% stenosis in the left anterior descending coronary artery were 105.1 mg, 157.2 mg and 302.2 mg, respectively (p<0.001). Finally, there was a direct relationship between the total Agatston Score at baseline and the number of diseased vessels (test for trend, p<0.001)
Conclusion
The majority of patients with clinically indicated coronary angiography during follow up had detectable coronary calcification at baseline. While there is a significant relationship between the extent of calcification and mean degree of stenosis in individual coronary vessels, 16% of the coronary arteries with significant stenoses had no calcification at baseline.
Background
Most coronary artery disease (CAD) events occur in the population deemed to be at “intermediate risk”1. It is therefore assumed that refined methods of risk prediction may be useful.
The use of computed tomography (CT) imaging to detect coronary calcium has been proposed as a tool to allow improved detection of at-risk individuals2. However, not all coronary events are caused by calcified plaque3;4 and while the relationship between coronary calcium and coronary events on a per-patient basis has been thoroughly studied, little is known about the relationship between calcification of individual coronary arteries and the degree of coronary artery stenosis in invasive coronary angiography.
The extent of calcified plaques has been shown to correlate moderately closely to overall plaque burden in histology5;6. Coronary calcifications measured by CT are usually expressed as the ‘Agatston Score’ 2;7. In numerous trials, coronary calcium has been shown to be predictive of major cardiovascular events, and to modify the cardiovascular risk predicted by the Framingham risk score, especially in the intermediate risk group2;8–13.
The Agatston score has been shown to be related to the severity of coronary artery disease and the number of stenosed vessels determined by coronary angiography7;14–17. However, the association between the extent of coronary calcification to the severity of coronary stenosis in individual coronary beds has not been widely explored.
We studied individuals enrolled in the Multi- Ethnic Study of Atherosclerosis (MESA)18. All MESA participants were asymptomatic for cardiovascular disease at the time of enrollment. At the time of this analysis, six years had elapsed from enrolment and a substantial number of participants had developed symptoms of coronary artery disease (CAD), or were diagnosed to have myocardial ischemia by stress testing. As a result, individuals underwent diagnostic coronary catheterizations, and some proceeded to have surgical or percutaneous coronary revascularization to treat obstructive CAD. The purpose of this study is to report the relationship between the baseline extent of coronary calcium measured by cardiac CT and the anatomic findings in subsequent clinically indicated coronary angiography.
Methods
Study Population
The characteristics of subjects enrolled in MESA have been described elsewhere18. In short, MESA is a multi-center community based study designed to investigate the mechanisms underlying the development and progression of subclinical cardiovascular disease. Individuals with symptoms or a history of cardiovascular disease were excluded. 6,814 men and women, 45–84 years of age, from different ethnic origins (White, African-American, Hispanics and Chinese) were enrolled. As of June 2005, 6 years after enrolment, the reports of clinically driven invasive coronary angiography in 175 participants had been received. Data from these subjects are described in this report. The study protocol had been approved by the institutional review boards in each of the participating centers and informed consent was obtained by each of the participants.
Measurement of coronary calcium
As a part of MESA protocol, all participants underwent measurement of coronary calcium using either Multi-Detector row CT (MDCT) or Electron Beam CT (EBCT) at baseline. Detailed scan protocols have previously been published19. Image settings are described in Supplement A, on line.
Agatston score7 is an important and well established measure of coronary calcium that has been utilized in multiple studies. Therefore, we used this parameter to evaluate the total coronary calcium score per patient. Calcium mass score is less commonly used as an index of coronary calcium, but has been found to be more reproducible in assessing coronary calcium20. In view of the multiple types of CT scanners, including MDCT and EBCT, and the multiple sites participating in the MESA study, and the smaller amounts of calcium in a single coronary vessel as opposed to the entire coronary artery tree, we opted to use calcium mass score as a measure of coronary calcium in individual coronary beds.
Standard calcium scoring software tools were used for calculating the Agatston score and Calcium mass score. For analysis, we used calcium mass scores (mg) determined for each of the coronary arteries and the total Agatston score for the entire coronary bed.
Results obtained from coronary angiography reports
As of June 2005, the MESA coordinating center had received incident coronary angiography reports for 175 individuals. The indications for coronary angiography were clinical and not part of the MESA protocol. All angiographic studies had been performed after baseline CT exams. Only the first catheterization report was utilized for analysis if an individual underwent more than one procedure.
The studies were performed in different catheterization laboratories, and quantitative analysis (QCA) of luminal stenosis was not /routinely available. In most cases, the extent of stenosis was assessed using visual assessment. Therefore, the following categories were used to define the degree of stenosis for individual coronaries: 0–49%, 50–74% and ≥75% luminal diameter stenosis to indicate non-significant, intermediate and significant stenosis, respectively. For the analysis of the extent of coronary disease (1, 2 and 3 vessel disease): significant stenosis was defined as: ≥ 50% left main coronary artery and ≥75% in the left anterior descending (LAD), left circumflex (LCX) or right coronary artery (RCA) or their branches.
Definition of risk factors
Hypertension was defined as diastolic blood pressure (DBP) ≥90 mmHg, systolic blood pressure (SBP) ≥140mmHg, or receiving treatment for hypertension. Dyslipidemia was defined as total cholesterol ≥ 240 mg/dl, LDL-cholesterol ≥160 mg/dl, triglycerides ≥150 mg/dl, HDL<45 mg/dl, or receiving treatment for dyslipidemia. Diabetic individuals were defined as either having fasting plasma glucose ≥126 mg/dl or receiving treatment. Smoking status was defined as current smoking, former smoking, or never smoked.
Statistical Analysis
All analyses were performed using STATA-8 software (College Station, TX). To study the association between average baseline calcium scores in each coronary artery and the degree of stenosis (0–49%, 50–74% and ≥75%) in the corresponding vessel or its branches, we used analysis of variance. Due to the skewed distribution of calcium scores, a log-transformation of calcium scores was used when testing trends. Even in this symptomatic subset, a considerable portion of baseline coronary artery calcium plaque (CACP) scores were 0. Hence the value (CACP score+1) was used for log transformation. Chi-squared tests (or Fisher’s Exact tests where indicated) were performed to compare the distribution of stenosis across quartiles of CACP. Significance was defined as p<0.05.
Results
Demographic and clinical characteristics
The demographic characteristics and risk factor profile of the 175 individuals with available angiographic data are shown in Table 1. Compared to the other participants of the MESA cohort, the 175 individuals with available angiographic data were older, more likely to be men, and Caucasian. There were no significant differences between the two groups in socioeconomic parameters including educational status, yearly income and health insurance coverage. (Table A, On-line Supplement).
Table 1.
Demographic characteristics and risk factors in MESA participants who underwent coronary angiography. Percentages are shown in parentheses. Continuous variables are presented as mean ± standard deviation.
| Clinical characteristics | Underwent angiography | Not known to have undergone angiography | P- value* |
|---|---|---|---|
| Number: | 175 | 6,638 | |
| Age (years) | 67±9 | 63±10 | <0.0001 |
| Gender: | |||
| Men (%) | 111 (63) | 3,535 (47) | |
| Women (%) | 64 (37) | 3,103 (53) | <0.001 |
| Ethnic origin | |||
| Caucasian (%) | 83 (48) | 2,536 (38) | |
| Chinese (%) | 12 (7) | 790 (12) | |
| African American (%) | 49 (28) | 1,848 (28) | |
| Hispanics (%) | 31 (18) | 1,464 (22) | 0.030 |
| BMI (Kg/m2) | 28.9±5.2 | 28.3±5.5 | 0.13 |
| Risk factors | |||
| Dyslipidemia† | |||
| Total cholesterol (mg/dl) | 196±38 | 194±36 | 0.39 |
| LDL cholesterol (mg/dl) | 120±31 | 117±32 | 0.23 |
| HDL cholesterol (mg/dl) | 48±16 | 51±15 | 0.006 |
| Treatment for dyslipidemia (%) | 48 (27) | 1,053 (16) | <0.001 |
| Hx of Diabetes Mellitus | 21% | 10% | <0.001 |
| Glucose (mg/dl) | 109.9 | 104.5 | 0.022 |
| Smoking history (%) | |||
| Never smoked | 69 (40) | 3,357 (51) | |
| Former smoker | 74 (43) | 2,391 (36) | |
| Current smoker | 28 (16) | 857 (13) | 0.025 |
| Hypertension | |||
| Hx of Hypertension (%) | 113 (65) | 2,906(44) | <0.001 |
| Treatment for HTN | 85 (48) | 2,182 (33) | <0.001 |
| SBP (mmHg) | 135±21 | 126±21 | <0.0001 |
| DBP (mmHg) | 74±10 | 72±10 | 0.009 |
| CRP (mg/L)† | 3.9±5.0 | 3.8±5.9 | 0.51 |
| Creatinine (mg/dl) | 1.04±0.32 | 0.95±0.28 | <0.0002 |
P value was calculated by t- test for continuous variables and Chi square for categorical variables or Fisher exact test when appropriate.
To convert values for total cholesterol, HDL and LDL- cholesterol to millimoles per liter, multiply by 0.0259; to convert values for glucose to millimoles per liter, multiply by 0.0555; to convert values for triglycerides to millimoles per liter, multiply by 0.0113.
Abbreviations: BMI- body mass index, SBP- systolic blood pressure, DBP- diastolic blood pressure, HTN-hypertension, CRP- C reactive protein, LV - left ventricular.
Compared to those who did not undergo coronary angiography, patients who had invasive angiography performed had lower HDL- cholesterol (p=0.006), were more likely to have a history of hypertension, dyslipidemia, and diabetes mellitus (21% vs 9%, p<0.001).
The total Agatson score was higher in the patients who underwent invasive angiography as compared to controls (528.4±772.2 vs 136.3±339.4, p<0.0001). Similarly, the average calcium mass score was approximately 100 mg higher for each of the coronary arteries (Table 2, p<0.001 for all vessels). The detailed distribution of calcium scores in the MESA participants who underwent angiography is shown in Table B (Online Supplement). As expected, calcium mass score in the LM was lower than the other arteries. Distribution of coronary calcium in the LAD, LCX and RCA was similar, except for a slightly greater percentage of patients with a calcium mass score ≥200 mg in the LAD.
Table 2.
Baseline coronary artery calcium scores in MESA participants who underwent coronary angiography. Variables are presented as mean ± standard deviation.
| CT data | Underwent angiography | Not known to have undergone angiography | P- value* |
|---|---|---|---|
| Coronary calcium score (units)† | |||
| Left main (mg) | 22.9±70.5 | 4.2±30.4 | <0.0001 |
| Left anterior descending (mg) | 190.4±266.5 | 59.1±157.2 | <0.0001 |
| Left circumflex (mg) | 141.9±271.8 | 28.3±111.1 | <0.0001 |
| Right coronary artery (mg) | 145.3±321.1 | 39.9±180.8 | <0.0001 |
| Total score | 528.4±772.2 | 136.3±399.4 | <0.0001 |
Mann-Whitney U test was used to compare CACP scores due to their skewed distribution.
Coronary calcium score: for individual coronary arteries- calcium mass score was used (mg) and for the entire coronary bed (Total score) Agatston score was used (see Methods).
Results of coronary angiography
The indications for coronary angiography and the angiographic findings are shown in Table 3. The majority of participants (73%) underwent coronary angiography because of angina or acute MI. Eight (5%) participants underwent coronary angiography as direct result of the CT study, and 11 (6%) individuals underwent catheterization due to a positive stress test. Indications for catheterization are unknown in three patients. The median time interval between baseline cardiac CT and the clinical angiographic procedure was 18 months (range, <1 to 52 months).
Table 3.
Coronary angiography: Indications, time of angiography and findings.
| Angiographic characteristics | |
|---|---|
| Indications for angiography (n=175) | Number (%) |
| Pre-operative risk stratification | 9 (5) |
| Asymptomatic (positive stress test) | 11 (6) |
| CT results | 8(5) |
| Angina pectoris | 64 (37) |
| Acute myocardial infarction | 63 (36) |
| Congestive heart failure | 13 (7) |
| Other indications | 4 (2) |
| Unknown | 3(2) |
| Time between of baseline CT and angiography, (n=175) | |
| months, median (range) | 18m (<1 to 52) |
| Distribution of time interval, (n=175) | n (%) |
| <12 months | 56 (32) |
| 12–23 months | 63 (36) |
| 24–35 months | 31 (18) |
| ≥ 36 months | 25 (14) |
|
Angiographic Findings, n (%) | |||
|---|---|---|---|
| % stenosis | |||
| Artery | 0–49% | 50–74% | ≥ 75% |
| LAD | 84 (48) | 20 (11) | 71 (41) |
| LCX | 106 (61) | 13 (7) | 56 (32) |
| RCA | 98 (57) | 22 (13) | 53 (31) |
| 0–24% | 25–49% | ≥50% | |
| Lt main disease* | 137 (83) | 9 (5) | 20 (12) |
| Number of Diseased vessels, (n=174) | n (%) | ||
| Non significant CAD | 75 (43) | ||
| 1 vessel disease | 40 (23) | ||
| 2 vessel disease | 24 (14) | ||
| 3 vessel or lt. main disease | 35 (20) | ||
| Dominance, (n=175) | |||
| Right | 147 (84) | ||
| Left | 28 (16) | ||
Among the MESA participants who underwent coronary angiography, 41%, 32% and 31% individuals had ≥75% stenosis in the LAD, LCX and RCA, respectively. Importantly, 20 individuals (12%) had significant LM disease (≥ 50% stenosis) while 21% had either three-vessel or LM disease.
Relationship between baseline calcium scores and obstructive CAD in individual vessels
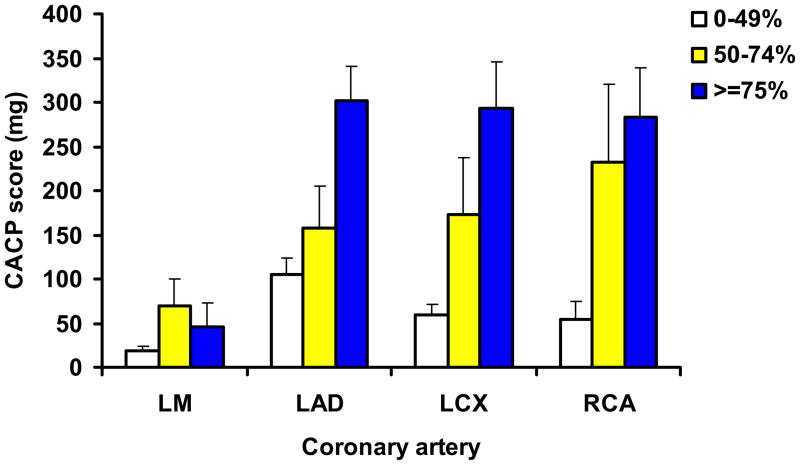
For each of the coronary vessels, there was a significant relationship between baseline calcium scores and the severity of coronary artery stenosis determined by angiography (Figure 1). The baseline score was markedly higher in coronary arteries that were found to be stenotic. For example, in the LAD, baseline calcium mass scores were 105.1 ±167.4 mg (n=83), 157.2±216.6 mg (n=20) and 302.2±329.8 mg (n=71) in the presence of 0–49%, 50–74% and ≥ 75% stenosis, respectively (p<0.001). Similar relationships were noted for the LCX and RCA (p<0.001). (Table C, On-Line Supplement). For the LM, differences were of lower magnitude, yet significant (p<0.05).
Figure 1. Relationship between calcium score and the severity of coronary artery stenosis.
Calcium mass score as a measure of coronary calcification in each of the coronary arteries with different levels of stenosis. White bars indicate 0–49% stenosis, yellow bars 50–74% and blue bars indicate ≥75% stenosis. (Exception: for the left main artery the corresponding categories are 0–24%, 25–49% and ≥50% stenosis). Standard error bars are shown. Test for trend across the different stenosis categories were significant for each artery (p<0.05 for the LM, p<0.001 in each of the other arteries). Analysis of variance on the log- transformed values of CACP scores was used to test for trend. LM- left main, LAD- left anterior descending, LCX- left circumflex, RCA- right coronary artery.
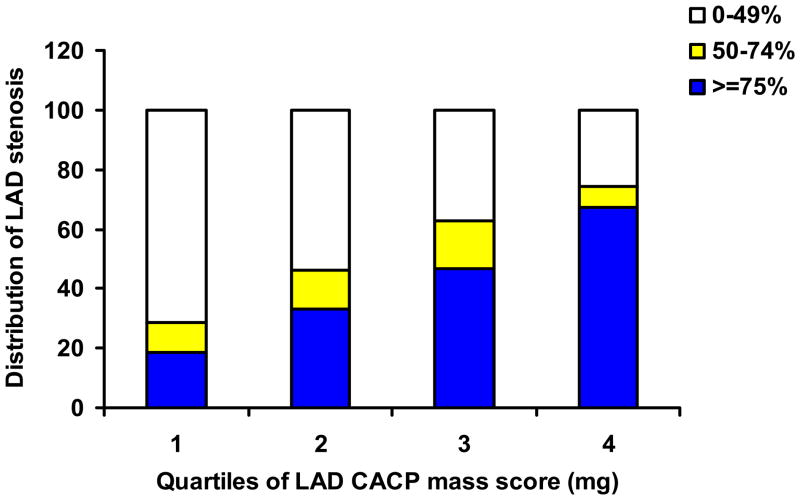
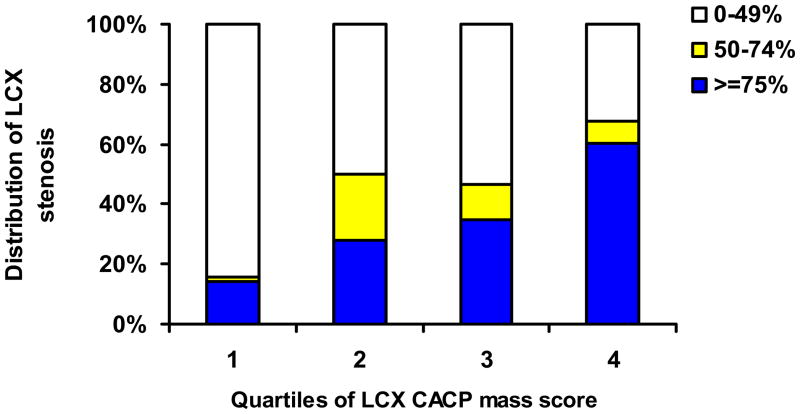
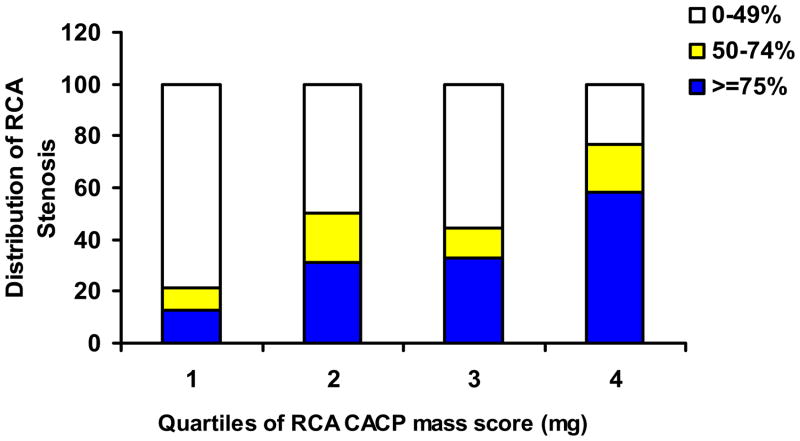
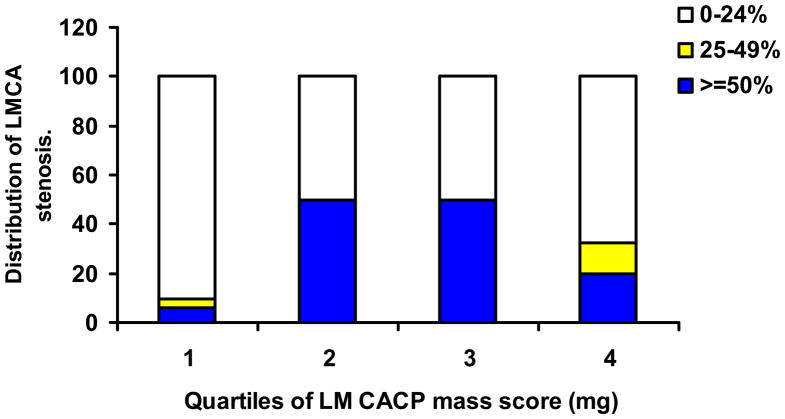
When the distribution of stenotic segments in each of the coronary arteries was studied using calcium score quartiles, there was a gradual increase in the severity of stenosis among those who had greater calcium scores at baseline (Figure 2). This pattern was seen in each of the coronary arteries except for the LM (p<0.001 for each of the coronaries).
Figure 2.
2A: Distribution of LAD stenosis with increasing LAD CACP mass quartiles
2B: Distribution of LCX stenosis with increasing LCX CACP mass quartiles.
2C: Distribution of RCA stenosis with increasing RCA CACP mass quartiles
2D: Distribution of LM stenosis with increasing LM CACP mass quartiles.
The distribution of the severity of coronary stenosis across quartiles of the coronary calcium score in the LAD (2A), LCX (Figure 2B), RCA (2C) and left main coronary artery (2D). In figures 2A-C, the blue portion indicates ≥75% stenosis, yellow indicates 50–74% stenosis and the white part of the bars indicates 0–49% stenosis. In Figure 2D, the blue portion indicates ≥50% stenosis, the yellow portion 25–49% stenosis and the white part of the bars 0–24% stenosis. For all arteries, the Chi square test for association between CACP quartile and % stenosis group was significant (p<0.001 for each).
Ranges of CACP scores for each quartile:
LAD: I 0 to 0; II. 0.9 to 86.7; III 87.2 to 287.8; IV 290.7 yo 1368.4
LCX: I 0 to 0; II 1.6 to 19.7; III 24.5 to 174.8; IV 176.0 to 1884.8
RCA: I 0 to 0; II 1.2 to 13.6; III 13.6 to 121.3; IV 127.5 to 1799.4
LM: I. 0 to 0; II 0 to 0.78; III 0.78 to 3.7; IV. 4.7 to 543.5.
Seven of 176 participants (4%) with significant flow limiting coronary artery disease (≥ 75% stenosis in at least one of the coronary beds) had zero calcium mass scores at baseline. Similarly, 11 of 176 participants (6.25%) with at least one stenosis ≥50% had a zero mass calcium score. Importantly, when analyzing individual arteries, the rate of zero calcium mass scores in spite of the presence of a ≥75% stenosis was 12.7% (9/71) for the LAD, 17.9% (10/56) for the LCX, and 17% (9/53) for the RCA. Of vessels with ≥50% stenoses, 16.3% (15/92), 15.7% (11/70) and 21.8% (17/78) had zero baseline calcium mass scores in the LAD, LCX and RCA territories, respectively. Moreover, among 20 patients with ≥50% stenosis in the LM, 8 individuals (35%) had a zero mass score in the LM at baseline and 2 patients had a total zero Agatston score.
Finally, results for patients who underwent coronary angiography earlier than the median time interval (18 months after enrollment) were similar to patients whose angiographic studies were performed later (data not shown).
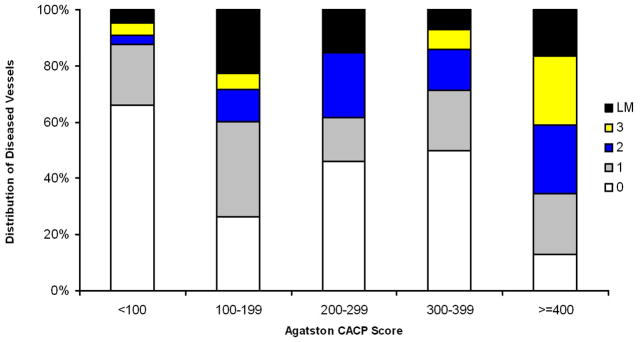
Relationship between baseline calcium scores and the number of diseased coronary vessels
There was a direct relationship between the total Agatston score at baseline and the number of diseased vessels (Figure 3). For patients without significant stenosis, as well as for patients with 1-, 2-, 3-vessel disease and LM disease, average Agatston scores were 161.3±268.2, 462.7±608.5, 961.7±986.9, 1351.4±1180.1 and 658.3±607.4 units, respectively (p<0.001). The relationship between the number of diseased vessels and the categories of the Agatston score is displayed in Figure 4. Notably, 66% of patients with scores <100 Agatston units at baseline did not have significant coronary stenoses, whereas only 13% of the participants with baseline scores ≥400 had no coronary arery stenoses.
Figure 3. Relationship between number of diseased coronaries and Agatston score.
Agatston calcium score (phantom adjusted) in individuals with non-significant coronary artery disease and in those with one, two, three vessel disease and left main coronary artery disease. Significant vessel disease is defined as ≥ 50% stenosis in the left main artery or ≥ 75 stenosis in the LAD, LCX or RCA coronary arteries. Standard error bars are shown.
The test for trend (ANOVA on log transformed CACP) among the four different groups was highly significant (p<0.001).
Figure 4. Distribution of diseased coronaries with increasing Agatston score.
The distribution of coronary artery disease among individuals with different Agatston Scores (<100, 100–199, 200–299, 300–399 and ≥400 units). The white portions indicate non-significant CAD, while the gray, blue, yellow and black portions indicate one, two, three vessel disease and left main disease, respectively. The Chi square test for association between calcium score category and extent of disease was highly significant (p<0.001).
In contrast, 9% of the participants with Agatston score <100 had 3-vessel or LM disease, compared to 41% of those with a baseline score ≥400 units (p<0.001).
Discussion
The main purpose of the present study was to explore the relationship between the extent of coronary calcification detected by cardiac CT and the severity of coronary stenosis documented in clinically indicated coronary angiography. The study population consisted of 175 individuals who were asymptomatic enrolment, but subsequently developed symptoms of CAD or had positive stress tests requiring coronary angiography.
We could demonstrate that on a per-patient basis, the severity of coronary calcification was directly related to the extent of obstructive CAD in those individuals who underwent coronary angiography due to clinical indications after a median time interval of 18 months following enrolment. Only 4% of individuals who had significant stenosis in angiography had a baseline coronary score of zero.
Importantly, this does not indicate the likelihood of an individual with a zero calcium score to develop stenoses or a coronary event during follow-up. Out of the entire group of 3,563 MESA participants who had baseline calcium score of zero, only 11 individuals (0.3%), were referred for coronary angiography due to clinical indications and were found to have significant stenosis after a median of 18 months.
Similar to the relationship on a per-patient level, calcium scores in each of the major coronary beds (except for the left main coronary artery) predicted the severity of coronary stenosis as well as the extent and distribution of coronary artery disease among those MESA participants who underwent clinically driven coronary angiography. However, and as expected, calcium was less predictive on a per-vessel than on a per-patient level: between 13% and 18% of individual coronary arteries demonstrated stenoses ≥75% in spite of the absence of coronary calcium at baseline. For left main stenoses ≥ 50%, absence of calcium was noted in 35% of cases.
In previous studies, coronary calcium has been shown to closely correlate to the severity of coronary stenosis and number of vessels with significant stenoses as determined by coronary angiography14;15;17. Budoff et al evaluated 1,851 patients who underwent both EBCT and coronary angiography due to suspected CAD. The overall sensitivity for coronary calcium to predict obstructive disease on angiography was 95% and the specificity was 66%15. A strong correlation (r= 0.92) has been demonstrated between the amount of coronary calcium detected by CT, as well as the extent of calcium deposits and the severity of coronary stenosis determined by histomorphometry5;6. However, coronary plaque area was approximately five times greater than the area of calcium. While calcium is correlated to the amount of plaque, it is not necessarily correlated to the degree of stenosis of individual plaques. Similarly, the relationship between plaque calcification and the risk plaque rupture is not well established. Recurrent subclinical episodes of plaque rupture with repeated hemorrhage and healing may constitute an important mechanism of plaque growth and worsening of luminal stenosis and may predispose plaques to calcification21. However, plaques can rupture in the absence of calcium. A recent study used CT to demonstrate that in patients presenting with suspected acute coronary syndromes, there is a relatively high prevalence of non-calcified plaques. Moreover, 33% of the patients had a zero calcium score. This study, though relatively small (n=40), clearly demonstrated that the absence of calcium does not absolutely exclude the existence of a vulnerable plaque22.
However, in asymptomatic individuals and on a per-patient level, coronary calcification remains an excellent predictor of future CAD events. Coronary calcium has been found to predict major coronary events independently of standard risk factors and CRP, and has been found to be superior to Framingham risk score in predicting events8;10;23. As mentioned above, of the 3,563 MESA participants who had total zero calcium score, only 11 individuals (0.3%), were referred for coronary angiography due to clinical indications and were found to have significant stenosis (≥50%) after a median of 18 months. These findings are consistent with previous large studies including the overall results of the MESA trial, indicating that a zero score is associated with a low incidence of future cardiovascular events. 9;10;24;25
In summary, while the calcium score is a useful surrogate of the total atherosclerosis burden in the coronary vessels, only a small portion of the atherosclerotic plaque is calcified, and the relationship to the severity of stenosis substantially less close.
Limitations
The main limitation of the study is the availability of data in only 175 individuals who underwent coronary angiography for clinical indications. This number constitutes less than 3% of the MESA cohort. Moreover, the database includes only catheterization reports received by the MESA coordinating center, and does not represent complete ascertainment of all the angiography procedures despite extensive efforts dedicated to track all clinical events.
The indications for performance of coronary angiography were entirely clinical. It is possible that individuals who were aware of their positive CACP scores were more likely to seek medical attention when becoming symptomatic. As can be seen in Table 2, 5% of individuals underwent angiography as a result of the CT results. Therefore, ascertainment bias is a possibility and might have affected the findings. As a result, any conclusions about the predictive value or the performance of baseline cardiac CT (e.g sensitivity and specificity) cannot be made. These factors might have been more important in individuals of a higher socio-economic status and better access to medical care. No differences were observed in various socioeconomic parameters, implying that access to medical care was probably not a major factor distinguishing between individuals who did and those who did not undergo catheterization.
Angiographic studies have been performed in different laboratories, and thus, quantification of coronary luminal area (QCA) was not performed. Therefore, it was necessary to express stenoses using a categorial scale. Finally, the time between the baseline CT study and angiography was dictated by clinical indications and was not uniform (ranging from 1 to 52 months).
We opted to define 75% percent stenosis in the major coronary arteries and 50% stenosis in theleft main coronary artery as significant stenoses since these are routinely used for the performance of either percutaneous or surgical coronary interventions. Similar results were obtained if 50% were chosen to define significant luminal stenosis.
Agatston score7 is an important and well-established indicator of coronary calcification, and has been used in multiple studies. Therefore we used this parameter for assessing the total calcium score. Calcium mass score is less commonly used to assess coronary calcium. However, mass score has been found to be a more reproducible in assessing coronary calcium20, and in view of the multiple centers, and the use of different CT scanners, we opted to use the mass score for individual arteries.
In a previous study, also based on MESA, Brown et al26, underscore the importance of the spatial distribution of calcified plaque. They show that ‘calcium coverage score’, was a better predictor of cardiovascular events than calcium mass or the “Agatston Score”. Such an analysis was beyond the scope of our study, and we could not obtain exact per-segment correlations between calcium deposits and the stenotic lesions determined by angiography.
In conclusion, the extent of coronary calcification in individual coronary arteries is correlated to the severity of coronary stenosis in these vessels. All the same, a considerable number of arteries present with significant stenosis despite having no calcification at baseline. On a per-patient level, the presence of significant stenoses in the absence of calcium is rare.
Supplementary Material
Acknowledgments
This study was supported by the National Heart, Lung, and Blood Institute grant (RO1-HL66075-01) and the Multi-Ethnic Study of Atherosclerosis study contracts (NO1-HC-95162, NO1-HC-95168, and NO1-HC-95169). Dr. Lima is also supported by the Johns Hopkins
This research was supported by MESA contracts (N01-HC-95159 through N01-HC-95166 and N01-HC-95168) from the National Heart, Lung, and Blood Institute, and by an NHLBI grant (RO1-HL6607-01). Dr. Lima is also supported by the Reynolds Foundation. The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org
Abbreviations
- DBP
Diastolic Blood Pressure
- HDL cholesterol
High Density Lipoprotein- Cholesterol
- LAD
Left Anterior Descending
- LCX
Left Circumflex
- LDL cholesterol
Low Density Lipoprotein
- LMCA
Left Main Coronary Artery
- LV
Left Ventricle
- MESA
Multi-Ethnic Study of Atherosclerosis
- RCA
Right Coronary Artery
- SBP
Systolic Blood Pressure
Footnotes
Reynolds Center. There are no conflicts of interest.
Reference List
- 1.Naghavi M, Falk E, Hecht HS, Jamieson MJ, Kaul S, Berman D, Fayad Z, Budoff MJ, Rumberger J, Naqvi TZ, Shaw LJ, Faergeman O, Cohn J, Bahr R, Koenig W, Demirovic J, Arking D, Herrera VL, Badimon J, Goldstein JA, Rudy Y, Airaksinen J, Schwartz RS, Riley WA, Mendes RA, Douglas P, Shah PK. From vulnerable plaque to vulnerable patient--Part III: Executive summary of the Screening for Heart Attack Prevention and Education (SHAPE) Task Force report. Am J Cardiol. 2006;98:2H–15H. doi: 10.1016/j.amjcard.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 2.Greenland P, Bonow RO, Brundage BH, Budoff MJ, Eisenberg MJ, Grundy SM, Lauer MS, Post WS, Raggi P, Redberg RF, Rodgers GP, Shaw LJ, Taylor AJ, Weintraub WS. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) developed in collaboration with the Society of Atherosclerosis Imaging and Prevention and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol. 2007;49:378–402. doi: 10.1016/j.jacc.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 3.Forrester JS. Prevention of plaque rupture: a new paradigm of therapy. Ann Intern Med. 2002;137:823–833. doi: 10.7326/0003-4819-137-10-200211190-00012. [DOI] [PubMed] [Google Scholar]
- 4.Schmermund A, Erbel R. Unstable coronary plaque and its relation to coronary calcium. Circulation. 2001;104:1682–1687. doi: 10.1161/hc3901.093339. [DOI] [PubMed] [Google Scholar]
- 5.Mautner GC, Mautner SL, Froehlich J, Feuerstein IM, Proschan MA, Roberts WC, Doppman JL. Coronary artery calcification: assessment with electron beam CT and histomorphometric correlation. Radiology. 1994;192:619–623. doi: 10.1148/radiology.192.3.8058924. [DOI] [PubMed] [Google Scholar]
- 6.Rumberger JA, Simons DB, Fitzpatrick LA, Sheedy PF, Schwartz RS. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area. A histopathologic correlative study. Circulation. 1995;92:2157–2162. doi: 10.1161/01.cir.92.8.2157. [DOI] [PubMed] [Google Scholar]
- 7.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 8.Arad Y, Goodman KJ, Roth M, Newstein D, Guerci AD. Coronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events: the St. Francis Heart Study. J Am Coll Cardiol. 2005;46:158–165. doi: 10.1016/j.jacc.2005.02.088. [DOI] [PubMed] [Google Scholar]
- 9.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, Liu K, Shea S, Szklo M, Bluemke DA, O’Leary DH, Tracy R, Watson K, Wong ND, Kronmal RA. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 10.Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA. 2004;291:210–215. doi: 10.1001/jama.291.2.210. [DOI] [PubMed] [Google Scholar]
- 11.Lamont DH, Budoff MJ, Shavelle DM, Shavelle R, Brundage BH, Hagar JM. Coronary calcium scanning adds incremental value to patients with positive stress tests. Am Heart J. 2002;143:861–867. doi: 10.1067/mhj.2002.120972. [DOI] [PubMed] [Google Scholar]
- 12.Raggi P, Callister TQ, Cooil B, He ZX, Lippolis NJ, Russo DJ, Zelinger A, Mahmarian JJ. Identification of patients at increased risk of first unheralded acute myocardial infarction by electron-beam computed tomography. Circulation. 2000;101:850–855. doi: 10.1161/01.cir.101.8.850. [DOI] [PubMed] [Google Scholar]
- 13.Shemesh J, Morag-Koren N, Goldbourt U, Grossman E, Tenenbaum A, Fisman EZ, Apter S, Itzchak Y, Motro M. Coronary calcium by spiral computed tomography predicts cardiovascular events in high-risk hypertensive patients. J Hypertens. 2004;22:605–610. doi: 10.1097/00004872-200403000-00024. [DOI] [PubMed] [Google Scholar]
- 14.Budoff MJ, Georgiou D, Brody A, Agatston AS, Kennedy J, Wolfkiel C, Stanford W, Shields P, Lewis RJ, Janowitz WR, Rich S, Brundage BH. Ultrafast computed tomography as a diagnostic modality in the detection of coronary artery disease: a multicenter study. Circulation. 1996;93:898–904. doi: 10.1161/01.cir.93.5.898. [DOI] [PubMed] [Google Scholar]
- 15.Budoff MJ, Diamond GA, Raggi P, Arad Y, Guerci AD, Callister TQ, Berman D. Continuous probabilistic prediction of angiographically significant coronary artery disease using electron beam tomography. Circulation. 2002;105:1791–1796. doi: 10.1161/01.cir.0000014483.43921.8c. [DOI] [PubMed] [Google Scholar]
- 16.Kaufmann RB, Peyser PA, Sheedy PF, Rumberger JA, Schwartz RS. Quantification of coronary artery calcium by electron beam computed tomography for determination of severity of angiographic coronary artery disease in younger patients. J Am Coll Cardiol. 1995;25:626–632. doi: 10.1016/0735-1097(94)00435-S. [DOI] [PubMed] [Google Scholar]
- 17.Rumberger JA, Sheedy PF, III, Breen JF, Schwartz RS. Coronary calcium, as determined by electron beam computed tomography, and coronary disease on arteriogram. Effect of patient’s sex on diagnosis. Circulation. 1995;91:1363–1367. doi: 10.1161/01.cir.91.5.1363. [DOI] [PubMed] [Google Scholar]
- 18.Bild DE, Bluemke DA, Burke GL, Detrano R, Diez Roux AV, Folsom AR, Greenland P, Jacob DR, Jr, Kronmal R, Liu K, Nelson JC, O’Leary D, Saad MF, Shea S, Szklo M, Tracy RP. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol. 2002;156:871–881. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 19.Carr JJ, Nelson JC, Wong ND, McNitt-Gray M, Arad Y, Jacobs DR, Jr, Sidney S, Bild DE, Williams OD, Detrano RC. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology. 2005;234:35–43. doi: 10.1148/radiol.2341040439. [DOI] [PubMed] [Google Scholar]
- 20.McCollough CH, Ulzheimer S, Halliburton SS, Shanneik K, White RD, Kalender WA. Coronary artery calcium: a multi-institutional, multimanufacturer international standard for quantification at cardiac CT. Radiology. 2007;243:527–538. doi: 10.1148/radiol.2432050808. [DOI] [PubMed] [Google Scholar]
- 21.Burke AP, Kolodgie FD, Farb A, Weber DK, Malcom GT, Smialek J, Virmani R. Healed plaque ruptures and sudden coronary death: evidence that subclinical rupture has a role in plaque progression. Circulation. 2001;103:934–940. doi: 10.1161/01.cir.103.7.934. [DOI] [PubMed] [Google Scholar]
- 22.Henneman MM, Schuijf JD, Pundziute G, van Werkhoven JM, van der Wall EE, Jukema JW, Bax JJ. Noninvasive evaluation with multislice computed tomography in suspected acute coronary syndrome: plaque morphology on multislice computed tomography versus coronary calcium score. J Am Coll Cardiol. 2008;52:216–222. doi: 10.1016/j.jacc.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 23.Guerci AD, Spadaro LA, Goodman KJ, Lledo-Perez A, Newstein D, Lerner G, Arad Y. Comparison of electron beam computed tomography scanning and conventional risk factor assessment for the prediction of angiographic coronary artery disease. J Am Coll Cardiol. 1998;32:673–679. doi: 10.1016/s0735-1097(98)00299-x. [DOI] [PubMed] [Google Scholar]
- 24.Church TS, Levine BD, McGuire DK, Lamonte MJ, Fitzgerald SJ, Cheng YJ, Kimball TE, Blair SN, Gibbons LW, Nichaman MZ. Coronary artery calcium score, risk factors, and incident coronary heart disease events. Atherosclerosis. 2007;190:224–231. doi: 10.1016/j.atherosclerosis.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 25.Lamonte MJ, Fitzgerald SJ, Church TS, Barlow CE, Radford NB, Levine BD, Pippin JJ, Gibbons LW, Blair SN, Nichaman MZ. Coronary artery calcium score and coronary heart disease events in a large cohort of asymptomatic men and women. Am J Epidemiol. 2005;162:421–429. doi: 10.1093/aje/kwi228. [DOI] [PubMed] [Google Scholar]
- 26.Brown ER, Kronmal RA, Bluemke DA, Guerci AD, Carr JJ, Goldin J, Detrano R. Coronary calcium coverage score: determination, correlates, and predictive accuracy in the Multi-Ethnic Study of Atherosclerosis. Radiology. 2008;247:669–675. doi: 10.1148/radiol.2473071469. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.