Abstract
OBJECTIVES
The aim of this study was to evaluate current American College of Cardiology/American Heart Association (ACC/AHA) hospital percutaneous coronary intervention (PCI) volume minimum recommendations.
BACKGROUND
In order to reduce procedure-associated mortality, ACC/AHA guidelines recommend that hospitals offering PCIs perform at least 400 PCIs annually. It is unclear whether this volume standard applies to current practice.
METHODS
We conducted a retrospective analysis of the Agency for Healthcare Research and Quality’s Nationwide In-patient Sample hospital discharge database to evaluate in-hospital mortality among patients (n = 362,748) who underwent PCI between 1998 and 2000 at low (5 to 199 cases/year), medium (200 to 399 cases/year), high (400 to 999 cases/year), and very high (1,000 cases or more/year) PCI volume hospitals.
RESULTS
Crude in-hospital mortality rates were 2.56% in low-volume hospitals, 1.83% in medium-volume hospitals, 1.64% in high-volume hospitals, and 1.36% in very high-volume hospitals (p < 0.001 for trend). Compared with patients treated in high-volume hospitals (odds ratio [OR] 1.00, referent), patients treated in low-volume hospitals remained at increased risk for mortality after adjustment for patient characteristics (OR 1.21, 95% confidence interval [CI] 1.06 to 1.28). However, patients treated in medium-volume hospitals (OR 1.02, 95% CI 0.92 to 1.14) and patients treated in very high-volume hospitals (OR 0.94, 95% CI 0.85 to 1.03) had a comparable risk of mortality. Findings were similar when high- and very high-volume hospitals were pooled together.
CONCLUSIONS
We found no evidence of higher in-hospital mortality in patients undergoing PCI at medium-volume hospitals compared with patients treated at hospitals with annual PCI volumes of 400 cases of more, suggesting current ACC/AHA PCI hospital volume minimums may merit reevaluation.
There is growing interest in the use of procedure volumes as a means of identifying hospital quality of care (1). At the forefront of this effort is the Leapfrog Group, a collection of large health care purchasers that recommends, as part of a broader safety initiative, using hospital volume as an explicit criterion when contracting for selected procedures (2). Matching current American College of Cardiology/American Heart Association (ACC/AHA) percutaneous coronary intervention (PCI) clinical practice guidelines (3), Leapfrog has established a minimum institutional volume requirement of 400 cases per year for hospitals offering PCI (2,4–6). This volume threshold is based primarily on studies of PCI use in the late 1980s and early 1990s that identified an increased mortality risk for patients treated at hospitals with annual PCI volumes of fewer than 400 cases (7–13). In the past 5 to 10 years, however, there have been notable changes in PCI practice, including the adoption and widespread use of stents, new pharmacologic therapies such as glycoprotein IIb/IIIa inhibitors, and an increase in the overall use of PCI (14,15). These changes in technology and practice patterns raise the possibility that the currently recommended hospital PCI volume threshold of 400 cases may no longer be appropriate. However, no published study, to our knowledge, has assessed national PCI practice patterns after 1997.
To address this issue, we evaluated the association between hospital PCI volume and mortality in a contemporary, national cohort of patients who underwent PCI between 1998 and 2000. We sought to determine specifically whether patients treated at hospitals that conducted fewer PCIs than the current annual PCI volume minimum had higher mortality rates than patients treated at higher volume hospitals. This is particularly important, considering purchasers’ proposed efforts to limit PCI services to hospitals meeting annual PCI volume criteria (2).
METHODS
National In-patient Sample
We utilized data from the National In-patient Sample (NIS), a hospital discharge database created as part of the Agency for Healthcare Research and Quality’s (AHRQ) Health Care Utilization Project (16). The NIS is the largest publicly available all-payer inpatient database in the U.S., consisting of administrative billing records for all hospitalizations that occurred in a national, randomly selected set of acute care, non-governmental hospitals (17). For the year 2000, the NIS contains information on more than 7.5 million discharges occurring at nearly 1,000 hospitals in 28 states (18), or approximately 20% of all community hospitals in the U.S. The AHRQ compiles a public use, de-identified, hospitalization-level data set containing information on primary and secondary diagnoses, demographic characteristics, procedure use, length of stay, payer, total charges, and admission and discharge status from data collected by participating state health data organizations (16). For the purposes of our study, we pooled data from 1998, 1999, and 2000, the three most recent years of the NIS.
Study sample
We restricted our analysis to hospitalizations in which a patient had a primary or secondary procedure code indicating a PCI (International Classification of Diseases-9th Edition-Clinical Modification [ICD-9] procedure codes 36.00 to 36.06 and 36.09). Of the 21 million patient records in the 1998, 1999, and 2000 NIS, 363,155 indicated that a PCI occurred during hospitalization. From this set, we excluded patients under the age of 18 (n = 153) and neonatal or obstetric admissions (n = 23) in order to restrict our evaluation to the use of PCI in a typical adult population. Records missing data for gender (n = 14), age (n = 11), or mortality during hospitalization (n = 26) were also excluded. Of the 362,928 remaining records, we excluded records of patients (n = 180) treated at hospitals with fewer than five PCIs coded in any year in order to limit the influence of administrative data coding errors (12,19– 21). The final study cohort consisted of 362,748 admissions at 457 hospitals.
Hospital PCI volume groups
To assess the validity of the annual hospital PCI volume threshold of 400 cases recommended by current ACC/AHA PCI guidelines (3) and by the Leapfrog Group (2), we divided our cohort into four groups. Hospitals with fewer than 400 annual cases were divided into those with 5 to 199 cases (hereafter referred to as low-volume) and 200 to 399 cases (medium-volume) to distinguish true low providers from mid-volume providers that approached the volume requirement (8,10,12,13,21–26). Hospitals with at least 400 annual cases were divided into those with 400 to 999 cases (high-volume) and those with 1,000 cases or more (very high-volume) to distinguish hospitals with sufficient PCI capability from centers with dedicated, high-volume PCI services (11,27).
Statistical analysis
Patient characteristics, including demographics, admission type, comorbidities, and payer, were compared across the four hospital PCI volume groups using global chi-square analyses for categorical variables, and analyses of variance for continuous variables.
The principal study outcome was in-hospital mortality. We compared crude rates of in-hospital mortality across all four hospital PCI volume groups using global chi-square and test of trend analyses. Unadjusted logistic regression analyses were used to evaluate the consistency of the association between hospital PCI volume and mortality when stratifying by gender, age, single-vessel versus multiple-vessel PCI, history of diabetes, myocardial infarction (MI) during admission, admission type, admission source, and year.
Multivariable logistic regressions employing generalized estimating equations were conducted to assess the independent association of hospital PCI volume and patient mortality accounting for the clustered nature of the study sample (admissions within year-specific hospital clusters). Patient characteristics incorporated in the multivariable model were identified on the basis of a review of prior studies of PCI volume and outcomes and clinical judgment. These variables included gender, admission source, urgency of admission, age, year, multiple vessel PCI (ICD-9 procedure code 36.05), stent, MI as a principal diagnosis (ICD-9 diagnosis code 410), MI as a secondary diagnosis, any other non-MI coronary disease diagnosis (ICD-9 diagnosis codes 411 to 414), diabetes (ICD-9 diagnosis code 250), chronic obstructive pulmonary disease (ICD-9 diagnosis codes 490 to 496), hypertension (ICD-9 diagnosis codes 401 to 405), and renal dysfunction (ICD-9 diagnosis codes 580 to 586). Because we specifically sought to examine the value of the current hospital PCI volume minimum of 400 cases, mortality rates and risks among patients treated in medium-volume (200 to 399 cases) and high-volume (400 to 999 cases) hospitals were compared directly. We also compared the experience of patients treated at medium-volume hospitals (200 to 399 cases) with that of patients treated at the combined group of high- and very high-volume hospitals (400 cases and higher).
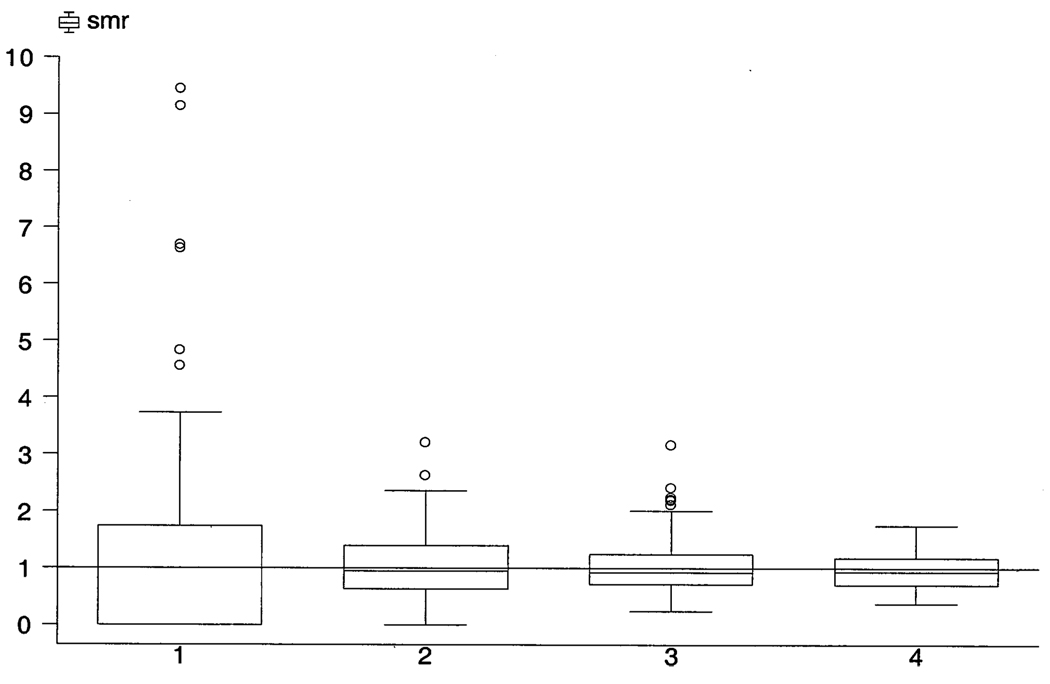
Standardized mortality ratios (SMRs) were calculated for each hospital by dividing the hospital’s observed mortality rate by its expected mortality rate, as predicted by the covariates employed in our multivariable model (excluding hospital PCI volume). Hospitals with SMRs of <1.0 had better outcomes than expected, while hospitals with SMRs >1.0 had worse outcomes than expected. Box and whisker plots were used to present the distribution of hospital SMRs for each of the four hospital PCI volume groups.
This study was approved by the University of Pennsylvania Institutional Review Board. All analyses were conducted using the SAS 8.2 (SAS Institute Inc., Cary, North Carolina) and Stata 7.0 (Stata Corp., College Station, Texas) software packages.
RESULTS
Patient characteristics
Of the 362,748 admissions in the study cohort, 14,575 (4%) were treated at low-volume hospitals, 42,054 (12%) at medium-volume hospitals, 152,500 (42%) at high-volume hospitals, and 153,619 (42%) at very high-volume hospitals (Table 1). Patients treated at lower volume hospitals were on average younger, and larger proportions were female, non-white, and had Medicaid insurance. Lower volume hospitals treated higher risk cases, on average, as reflected by the larger proportion of patients with MI and smaller proportions of elective admissions and patients who arrived by interhospital transfer. The proportions of procedures utilizing stents and involving multiple vessels were greater across successively larger hospital PCI volume groups. The proportions of patients with hypertension, diabetes, and chronic obstructive pulmonary disease were comparable across the four hospital PCI volume groups.
Table 1.
Patient Characteristics Across Hospital PCI Volume Groups
| Hospital Annual PCI Volume Groups (Cases/Year Volume Cut Points) |
||||||
|---|---|---|---|---|---|---|
| Characteristics | Overall | Low (<200) |
Medium (200–399) |
High (400–999) |
Very High (≥1,000) |
Overall p |
| n Patients | 362,748 | 14,575 | 42,054 | 152,500 | 153,619 | — |
| % of Patients | 100.0 | 4.0 | 11.6 | 42.0 | 42.3 | — |
| n Hospitals | 457 | 122 | 98 | 171 | 66 | — |
| % of Hospitals | 100.0 | 26.7 | 21.4 | 37.4 | 14.4 | — |
| n Hospital-year groups* | 659 | 169 | 140 | 251 | 99 | — |
| % of Hospital-year groups* | 100.0 | 25.6 | 21.2 | 38.1 | 15.0 | — |
| Median age | 65 | 64 | 64 | 65 | 65 | <0.001 |
| Age | <0.001 | |||||
| <65 yrs | 49.1 | 51.1 | 50.5 | 49.7 | 47.9 | |
| 65–74 yrs | 29.0 | 27.5 | 28.1 | 28.7 | 29.8 | |
| 75 yrs of age and older | 21.9 | 21.4 | 21.4 | 21.6 | 22.8 | |
| Male | 65.5 | 62.7 | 65.4 | 65.7 | 65.6 | <0.001 |
| Race | <0.001 | |||||
| White | 64.3 | 46.4 | 61.0 | 67.6 | 63.6 | |
| Black | 4.4 | 5.1 | 5.2 | 4.4 | 4.1 | |
| Other | 6.8 | 10.9 | 8.8 | 7.4 | 5.2 | |
| Race not reported/missing | 24.5 | 37.6 | 25 | 20.6 | 27.1 | |
| Primary payer | <0.001 | |||||
| Medicare | 48.5 | 45.6 | 45.9 | 47.0 | 50.9 | |
| Medicaid | 3.8 | 8.1 | 4.3 | 4.2 | 3.0 | |
| Private | 41.7 | 38.7 | 41.6 | 42.5 | 41.2 | |
| Other/missing | 5.9 | 7.6 | 8.2 | 6.2 | 4.9 | |
| Diabetes | 24.4 | 25.3 | 24.2 | 23.7 | 25.0 | <0.001 |
| Hypertension | 52.6 | 51.0 | 51.8 | 51.3 | 54.4 | <0.001 |
| Chronic obstructive pulmonary disease | 11.2 | 11.8 | 11.8 | 11.3 | 10.8 | <0.001 |
| Renal disease | 2.5 | 2.9 | 2.6 | 2.3 | 2.5 | <0.001 |
| Coronary disease | <0.001 | |||||
| Myocardial infarction as primary diagnosis | 31.4 | 42.5 | 36.4 | 33.2 | 27.3 | |
| Myocardial infarction as secondary diagnosis | 4.7 | 4.9 | 5.0 | 4.4 | 5.0 | |
| Other coronary artery disease diagnosis | 60.4 | 47.7 | 55.2 | 59.2 | 64.1 | |
| No coronary artery disease diagnosis | 3.5 | 5.0 | 3.4 | 3.1 | 3.7 | |
| Admission type | <0.001 | |||||
| Emergency | 32.6 | 45.6 | 32.4 | 32.7 | 31.3 | |
| Urgent | 25.6 | 21.3 | 26.9 | 26.1 | 27.4 | |
| Elective | 29.9 | 15.7 | 22.9 | 28.3 | 37.3 | |
| Other/missing | 11.3 | 17.4 | 17.8 | 12.9 | 4.1 | |
| Arrived by interhospital transfer | <0.001 | |||||
| Yes | 17.8 | 7.8 | 10.4 | 16.9 | 21.6 | |
| No | 78.3 | 86.2 | 86.4 | 79.1 | 74.5 | |
| Unknown | 3.9 | 6.0 | 3.2 | 4.0 | 3.9 | |
| Multiple vessel procedure | 14.3 | 11.4 | 13.2 | 13.7 | 15.4 | <0.001 |
| Stent employed | 81.7 | 74.8 | 80.8 | 81.5 | 82.8 | <0.001 |
| Coronary bypass surgery-capable hospital | 98.8 | 75.8 | 98.1 | 100.0 | 100.0 | <0.001 |
| Year | <0.001 | |||||
| 1998 | 29.6 | 34.4 | 33.1 | 33.7 | 24.2 | |
| 1999 | 32.0 | 29.9 | 32.4 | 32.4 | 31.6 | |
| 2000 | 38.4 | 35.7 | 34.6 | 33.9 | 44.2 | |
Unless noted otherwise, findings are expressed as percentages. Percentages may not total 100 due to rounding.
Hospital-year groups refer to the number of hospitals that contributed data in each year of the Nationwide In-patient Sample (NIS). A hospital participating in the NIS over the three-year period would be considered to have contributed three hospital-year groups to the analysis.
PCI = percutaneous coronary intervention.
PCI volume and crude in-hospital mortality
Crude in-hospital morality rates were associated with PCI volume, ranging from 2.56% for patients treated in low-volume hospitals to 1.36% for patients treated in very high-volume hospitals (p < 0.001 for trend). Patients treated in medium-volume hospitals had higher in-hospital mortality rates than patients treated in high-volume hospitals (1.83% vs. 1.64%, p = 0.008) (Table 2).
Table 2.
Crude In-Hospital Mortality Rates
| Hospital Annual PCI Volume Groups (Cases/Year Volume Cut Points) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| All Hospitals |
Low (<200) |
Medium (200–399) |
High (400–999) |
Very High (≥1,000) |
Trend p |
Medium vs. High p |
Overall Interaction p |
Medium vs. High Interaction p |
|
| Overall | 1.58 | 2.56 | 1.83 | 1.64 | 1.36 | <0.001 | 0.008 | – | – |
| Gender | 0.649 | 0.580 | |||||||
| Male | 1.27 | 2.15 | 1.50 | 1.31 | 1.08 | <0.001 | 0.020 | ||
| Female | 2.17 | 3.24 | 2.46 | 2.27 | 1.68 | <0.001 | 0.171 | ||
| Age | 0.007 | 0.168 | |||||||
| <65 yrs | 0.72 | 1.37 | 0.93 | 0.76 | 0.72 | <0.001 | 0.012 | ||
| 65–74 yrs | 1.64 | 2.27 | 2.09 | 1.76 | 1.36 | <0.001 | 0.020 | ||
| 75 yrs and older | 3.42 | 5.78 | 3.62 | 3.52 | 3.05 | <0.001 | 0.649 | ||
| Vessels | 0.142 | 0.225 | |||||||
| Single | 1.58 | 2.59 | 1.79 | 1.63 | 1.37 | <0.001 | 0.045 | ||
| Multiple | 1.56 | 2.29 | 2.13 | 1.70 | 1.26 | <0.001 | 0.031 | ||
| Diabetes | 0.242 | 0.902 | |||||||
| Yes | 1.57 | 2.61 | 1.88 | 1.70 | 1.26 | <0.001 | 0.224 | ||
| No | 1.58 | 2.54 | 1.81 | 1.62 | 1.39 | <0.001 | 0.018 | ||
| Acute myocardial infarction | 0.040 | 0.164 | |||||||
| Yes (primary or secondary) | 3.54 | 4.52 | 3.61 | 3.57 | 3.35 | <0.001 | 0.770 | ||
| No | 0.47 | 0.79 | 0.57 | 0.48 | 0.41 | <0.001 | 0.073 | ||
| Admission | 0.091 | 0.142 | |||||||
| Arrived by transfer | 1.83 | 2.20 | 1.93 | 1.98 | 1.70 | 0.057 | 0.837 | ||
| Direct admission | 1.51 | 2.49 | 1.77 | 1.57 | 1.24 | <0.001 | 0.009 | ||
| Unknown | 1.91 | 3.98 | 3.18 | 1.61 | 1.61 | <0.001 | <0.001 | ||
| Type of admission | 0.725 | 0.459 | |||||||
| Emergency | 2.38 | 3.32 | 2.50 | 2.46 | 2.13 | <0.001 | 0.773 | ||
| Urgent | 1.56 | 2.26 | 1.79 | 1.53 | 1.47 | 0.001 | 0.048 | ||
| Elective | 0.72 | 1.26 | 0.75 | 0.78 | 0.64 | 0.001 | 0.732 | ||
| Other/missing | 1.71 | 2.10 | 2.06 | 1.70 | 1.18 | <0.001 | <0.001 | ||
| Year | 0.681 | 0.705 | |||||||
| 1998 | 1.69 | 2.37 | 1.92 | 1.71 | 1.50 | <0.001 | 0.087 | ||
| 1999 | 1.62 | 2.82 | 1.75 | 1.68 | 1.41 | <0.001 | 0.555 | ||
| 2000 | 1.46 | 2.52 | 1.82 | 1.55 | 1.24 | <0.001 | 0.021 | ||
Interaction p values were obtained from a logistic regression model of in-hospital mortality containing terms for each hospital percutaneous coronary intervention (PCI) volume category, the strata of interest, and their interaction. The p values were obtained from multiple partial F-tests assessing whether coefficients for the interaction term were equal to 0.
The association between hospital PCI volume category and crude in-hospital mortality varied by patient age; mortality rates were markedly higher for patients age 75 years and older treated in low-volume hospitals (p = 0.007 for interaction). Differences in in-hospital mortality across hospital volume groups were greater for patients with an MI (low-volume hospital 4.52% vs. very high-volume hospital 3.35%) than for patients who did not have an MI (low-volume hospitals 0.79% vs. very high-volume hospital 0.41%; p = 0.04 for interaction). Crude mortality for patients at medium-, high-, and very high-volume hospitals combined was 1.54%, which was significantly lower than the mortality for patients at low-volume hospitals excluding centers with <100 (2.44%, p < 0.001), <50 (2.44%, p < 0.001), and <25 (2.48%, p < 0.001) cases. The crude association of hospital PCI volume and mortality was otherwise consistent across patient gender, diabetes status, multiple-vessel PCI, arrival by transfer, type of admission, and year. No significant interactions were observed when mortality rates were compared only between patients treated at medium-volume and high-volume hospitals (Table 2).
Adjusted analysis
Patients treated at low-volume hospitals remained at increased risk for in-hospital mortality (odds ratio [OR] 1.21, 95% confidence interval [CI] 1.06 to 1.38) after multivariable adjustment compared with patients treated in high-volume hospitals (referent) (Table 3). However, patients treated at medium-volume hospitals (OR 1.02, 95% CI 0.92 to 1.14) and patients treated at very high-volume hospitals (OR 0.94, 95% CI 0.85 to 1.03) had a mortality risk similar to patients treated in high-volume hospitals after multivariable adjustment. In-hospital mortality risks were also similar when comparing patients treated in medium-volume hospitals with patients treated at very high-volume hospitals (p = 0.29 for test of equality of odds ratios). Patients treated in medium-volume hospitals continued to have a mortality risk comparable to that of patients treated at high- and very high-volume hospitals when those hospitals were pooled together (OR 1.05, 95% CI 0.95 to 1.16). Findings were unchanged when analyses were repeated evaluating interactions for patient gender, age, number of vessels, acute MI admission, history of diabetes, type and urgency of admission, and year.
Table 3.
Hospital Annual PCI Volume and Odds of In-Hospital Mortality
| Hospital Annual PCI Volume Groups (Cases/Year Volume Cut Points) |
Unadjusted | Adjusted* |
|---|---|---|
| Low (<200) | 1.58 (1.39–1.80) | 1.21 (1.06–1.38) |
| Medium (200–399) | 1.12 (1.00–1.25) | 1.02 (0.92–1.14) |
| High (400–999) | 1.00 (referent) | 1.00 (referent) |
| Very high (≥1,000) | 0.84 (0.76–0.93) | 0.94 (0.85–1.03) |
| P comparing medium and very high volume hospitals | <0.0001 | 0.16 |
| P comparing medium, high, very high volume hospitals | <0.0001 | 0.29 |
| Low (<200) | 1.68 (1.47–1.90) | 1.24 (1.09–1.41) |
| Medium (200–399) | 1.18 (1.06–1.32) | 1.05 (0.95–1.16) |
| High and very high (≥400) | 1.00 (referent) | 1.00 (referent) |
Data are presented as odds ratios with 95% confidence intervals.
Analyses adjusted for age, gender, race, payer, myocardial infarction, coronary artery disease, diabetes, hypertension, chronic obstructive pulmonary disease, admission acuity, interhospital transfer, stent use, single versus multiple vessel procedure, and renal disease.
PCI = percutaneous coronary intervention.
The box and whisker plot showed large variation in the distribution of hospital SMRs within and across the four hospital PCI volume groups (Fig. 1). The median hospital SMR ranged from 0.99 for low-volume hospitals down to 0.92 for high-volume hospitals. A sizeable proportion of hospitals in each PCI volume group had SMRs above 1.0, indicating higher mortality rates than predicted.
Figure 1.
Box and whisker plot of hospitals’ standardized mortality ratios by percutaneous coronary intervention (PCI) volume groups. X-axis: hospital PCI volume groups (1 = low-volume, 2 = medium-volume, 3 = high-volume, 4 = very high-volume). Y-axis: standardized mortality ratio. smr = standardized mortality ratio.
DISCUSSION
Our evaluation of patients undergoing PCI in a national, random sample of hospitals between 1998 and 2000 demonstrates that patients treated at medium-volume hospitals (200 to 399 cases annually) and patients treated at hospitals with 400 or more PCI cases had statistically comparable mortality rates. These findings challenge earlier reports of poorer outcomes for patients undergoing PCI at middle-volume centers (7–13,19,21,24,26). Our results further suggest that efforts by the Leapfrog Group advocating a minimum annual hospital PCI volume of 400 cases are unlikely to achieve sizable reductions in PCI-related patient mortality (4–6). Moreover, our findings do not support current ACC/AHA PCI clinical practice guidelines recommending hospitals maintain a minimum annual PCI volume of 400 cases (3).
Our findings should not be interpreted as evidence that there is no association between hospital PCI volume and mortality. Indeed, we found that patients treated at hospitals that performed fewer than 200 PCI procedures annually had a higher risk of mortality than patients at hospitals in any other PCI volume group. At the same time, we noted substantial heterogeneity in hospital SMRs within each of the hospital PCI volume groups, and failed to find a statistically significant difference in mortality risks among patients treated in medium, high, or very high PCI volume hospitals. Given that we evaluated over 360,000 admissions at 457 hospitals throughout the U.S. over a three-year period, we believe this analysis, unlike previous reports of a neutral volume-outcome association (22,28), was sufficiently powered to detect even a modest difference between hospital PCI volume groups (3). If our analysis failed to detect a volume-mortality association, the magnitude of any such effect would have been so small as to be virtually meaningless from either a clinical or policy perspective. Finally, the similarity in mortality rates between medium, high, and very high hospitals across a variety of clinical strata suggests these results are robust and not limited to selected patient groups.
There are several potential explanations for the comparable mortality rates among patients treated in medium, high, and very high PCI volume hospitals. Percutaneous coronary intervention technology has changed markedly since the first studies of hospital PCI volume and outcomes (14,29,30). Although the adoption of coronary stents during the mid-1990s improved patient outcomes (13,14,30–32), previous studies indicated that patients undergoing PCIs involving stents at higher volume centers continued to have lower mortality rates than patients undergoing PCIs involving stents at lower volume centers (13,19,23,32,33). However, these studies evaluated procedure use before 1998. Stents may have attenuated the hospital PCI volume-mortality difference between medium-, high-, and very high-volume hospitals in subsequent years as additional operators were trained in their use, operators became more experienced, and newer stent designs were incorporated into practice. In addition, the increased use of new adjunctive pharmacologic therapies in the late 1990s, including glycoprotein IIb/IIIa receptor inhibitors (34) may have reduced the mortality difference between medium, high, and very high PCI volume hospitals. As in the case of stents, the full beneficial effect of these therapies may not have been observed in previous studies (13,19,23,32,33).
Technological improvements in PCI have been accompanied by significant changes in PCI practice patterns in the past decade (14,15,24,26,29). The substantial increase in the number of PCIs performed reflects a rise not only in the number of providers performing PCIs (i.e., diffusion), but also in the total number of procedures ever performed by each provider (i.e., accumulated experience) (26). This cumulative gain in provider experience may explain why mortality rates are now similar across medium, high, and very high PCI volume hospital groups. Additionally, the clinical threshold for PCI use has changed over time (14,24,30). To the extent that increases in PCI volume have occurred as a result of the treatment of a lower risk patient pool, any mortality difference between hospital PCI volume groups would have become smaller as the overall absolute mortality rate decreased. Alternatively, data from California indicate that some smaller PCI volume hospitals stopped providing PCIs during the 1990s (24,25). The lack of a difference in this study in mortality rates between medium, high, and very high PCI volume hospitals may be because medium-volume hospitals that stopped providing PCI were, on average, hospitals with higher mortality rates. Finally, differences in mortality between hospital PCI volume groups may be both smaller and less well established than commonly acknowledged. A recent literature review noted that nearly half of the published studies evaluating hospital PCI volume and outcomes had reported no association with in-hospital mortality, while the remainder suggested only a modest mortality difference (35).
We believe our findings have important implications concerning the use of hospital volume as a proxy for PCI quality. Our findings, along with evidence of the benefits of hospital competition (36), the economic consequences of restricting PCI provision (37), and patients’ documented willingness to tolerate increased mortality rates at local hospitals rather than travel to lower mortality rate regional hospitals for treatment (38) challenge the benefit of a hospital PCI volume standard of 400 annual cases (4). Further, the current PCI volume minimum criterion would unfairly affect the majority of hospitals in the medium-volume group with outcomes that are better than or comparable to what would be expected given their patient case-mix (i.e., SMR ≤1).
Our findings also underscore the importance of periodic reevaluation of the volume-outcome association in order to allow for changes in technology and practice patterns. Recent data supporting the increased use of interventional strategies in the management of unstable angina (39), benefits provided by new pharmacologic therapies (40), and the promise of drug-eluting stents (41) make it apparent that PCI practice is continuously evolving. This is consistent with the pattern of decreasing differences in mortality between hospital PCI volume groups (24,26). Thus, the suggestion that there is sufficient evidence to “move ahead” with existing volume standards (42) may, in the case of PCI, be premature given the dated information upon which those standards are based. Future studies of the PCI volume-outcome association will be needed to identify and test new volume thresholds, and ultimately to determine the process(es) through which volume and outcomes are linked.
There are four potential limitations of our evaluation that merit specific consideration. First, our analysis used administrative data, and thus may not have captured the full clinical detail of a patient’s risk profile. However, it is unclear whether having additional clinical data would have led us to uncover a meaningful difference in mortality between medium- and high-volume PCI hospitals. Given that patients treated at low- and medium-volume hospitals had a higher risk profile based on this administrative data, it is likely that more detailed clinical risk adjustment would have further narrowed any putative hospital PCI volume-associated mortality difference.
Second, we evaluated in-hospital mortality alone and could not assess other patient outcomes, including periprocedural complications, repeat revascularization rates, or longer-term outcomes. However, current ACC/AHA PCI clinical practice guidelines recommend hospital PCI volume minimums primarily on the basis of prior studies demonstrating a reduction in procedure-related mortality (3). Similarly, the Leapfrog Group explicitly justifies hospital PCI volume minimums as a means of reducing mortality (4). In addition, long-term outcomes are reportedly comparable for patients treated at different PCI volume hospitals, suggesting that any differences in outcomes between PCI volume hospitals are observed during hospitalization (22,43).
Third, the NIS does not track the experience of individual physicians. Thus, we cannot account for the influence of individual operator PCI volume on the association between hospital PCI volume and mortality. Physician PCI volume may modify the association between hospital PCI volume and outcomes, particularly if physicians at low-volume hospitals practice at more than one hospital. However, prior studies suggest both volume measures influence patient outcomes independently (9,11,19), and current ACC/AHA guidelines recommend separate operator and hospital annual PCI volume minimums (3). More importantly, if individual physician PCI volumes account primarily for the association between hospital PCI volume and outcomes, then efforts to reduce PCI mortality should focus on operator, and not hospital, volume. In addition, patients undergoing PCI who did not require hospitalization would not be represented in our sample, although it is uncertain what proportion of patients are in this group and how they are distributed across hospital PCI volume groups.
Finally, the NIS database does not contain unique patient identifiers. The inclusion of multiple patient admissions in our cohort may violate the statistical assumption of independence of observations. However, patient readmissions would alter our findings substantively only if readmissions were not randomly distributed across hospital PCI volume groups, and if readmission constituted an independent mortality risk beyond that measured by our current covariates.
Conclusions
Our evaluation of more than 360,000 PCIs from a national random sample of U.S. hospitals between 1998 and 2000 found no difference in mortality rates for patients treated at medium (200 to 399 cases/year), high (400 to 999 cases/year), and very high (≥1,000 cases/year) PCI volume hospitals after accounting for differences in case-mix. Moreover, within each of the hospital PCI volume groups, we detected substantial heterogeneity in hospital mortality. These results contradict current ACC/AHA clinical practice guidelines recommending all hospitals perform 400 PCIs each year. Our findings also question the usefulness of efforts by the Leapfrog Group to adopt PCI hospital volume minimums as a means of improving quality of care. Future evaluations of hospital PCI volume thresholds will be needed to assess recent and pending changes in PCI technology and practice.
Acknowledgments
Mr. Epstein is supported by a National Research Service Award (T32-HS00009) from the Agency for Healthcare Research and Quality, Rockville, Maryland. Mr. Rathore was supported by NIH/National Institute of General Medical Sciences Medical Scientist Training Grant GM07205.
Abbreviations and Acronyms
- ACC/AHA
American College of Cardiology/American Heart Association
- AHRQ
Agency for Healthcare Research and Quality
- CI
confidence interval
- ICD-9-CM
International Classification of Diseases-9th Revision-Clinical Modification
- MI
myocardial infarction
- NIS
Nationwide In-patient Sample
- OR
odds ratio
- PCI
percutaneous coronary intervention
- SMR
standard mortality ratio
Footnotes
Presented, in part, at the 2003 American College of Cardiology Scientific Sessions, Chicago, Illinois, April 2, 2003.
REFERENCES
- 1.Phillips KA, Luft HS. The policy implications of using hospital and physician volumes as ‘indicators’ of quality of care in a changing health care environment. Intl J Quality Health Care. 1997;9:341–348. doi: 10.1093/intqhc/9.5.341. [DOI] [PubMed] [Google Scholar]
- 2.Milstein A, Galvin RS, Delbanco SF, Salber K, Buck CRJ. Improving the safety of health care: the Leapfrog initiative. Eff Clin Pract. 2000;6:313–316. [PubMed] [Google Scholar]
- 3.Smith SC, Dove JT, Jacobs AK, et al. ACC/AHA guidelines for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1993 Guidelines for Percutaneous Transluminal Coronary Angioplasty) J Am Coll Cardiol. 2001;37:2239i. doi: 10.1016/s0735-1097(01)01344-4. lxvi. [DOI] [PubMed] [Google Scholar]
- 4.The Leapfrog Group. 2002. [Accessed October 2]. Evidence-based hospital referral: the Leapfrog Group. Available at http://www.leapfroggroup.org/FactSheets/EHR_FactSheet.PDF. [Google Scholar]
- 5.Dudley RA, Johansen KL, Brand R, Rennie DJ, Milstein A. Selective referral to high-volume hospitals: estimating potentially avoidable deaths. JAMA. 2000;283:1159–1166. doi: 10.1001/jama.283.9.1159. [DOI] [PubMed] [Google Scholar]
- 6.Birkmeyer JD, Finlayson EVA, Birkmeyer CM. Volume standards for high-risk surgical procedures: potential benefits of the Leapfrog initiative. Surgery. 2001;130:415–422. doi: 10.1067/msy.2001.117139. [DOI] [PubMed] [Google Scholar]
- 7.Jollis JG, Peterson ED, DeLong ER, et al. The relation between the volume of coronary angioplasty procedures at hospitals treating Medicare beneficiaries and short-term mortality. N Engl J Med. 1994;331:1625–1629. doi: 10.1056/NEJM199412153312406. [DOI] [PubMed] [Google Scholar]
- 8.Kimmel SE, Berlin JA, Laskey WK. The relationship between coronary angioplasty procedure volume and major complications. JAMA. 1995;274:1137–1142. [PubMed] [Google Scholar]
- 9.Jollis JG, Peterson ED, Nelson CL, et al. Relationship between physician and hospital coronary angioplasty volume and outcome in elderly patients. Circulation. 1997;95:2485–2491. doi: 10.1161/01.cir.95.11.2485. [DOI] [PubMed] [Google Scholar]
- 10.Phillips KA, Luft HS, Ritchie JL. The association of hospital volumes of percutaneous transluminal coronary angioplasty with adverse outcomes, length of stay, and charges in California. Med Care. 1995;33:502–514. doi: 10.1097/00005650-199505000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Hannan EL, Racz M, Ryan TJ, et al. Coronary angioplasty volume-outcome relationships for hospitals and cardiologists. JAMA. 1997;279:892–898. [PubMed] [Google Scholar]
- 12.Ritchie JL, Phillips KA, Luft HS. Coronary angioplasty: statewide experience in California. Circulation. 1993;88:2735–2743. doi: 10.1161/01.cir.88.6.2735. [DOI] [PubMed] [Google Scholar]
- 13.Rill V, Brown DL. Practice of coronary angioplasty in California in 1995: comparison to 1989 and impact of coronary stenting. Circulation. 1999;99:e12. doi: 10.1161/01.cir.99.21.e12. [DOI] [PubMed] [Google Scholar]
- 14.Srinivas VS, Brooks MM, Detre KM, et al. Contemporary percutaneous coronary intervention versus balloon angioplasty for multivessel coronary artery disease: a comparison of the National Heart, Lung and Blood Institute Dynamic Registry and the Bypass Angioplasty Revascularization (BARI) study. Circulation. 2002;106:1627–1633. doi: 10.1161/01.cir.0000031570.27023.79. [DOI] [PubMed] [Google Scholar]
- 15.American Heart Association. 2002 Heart and Stroke Statistical Update. Dallas, TX: 2002. [Google Scholar]
- 16.Steiner C, Elixhauser A, Schnaier J. The Healthcare Cost and Utilization Project: an overview. Eff Clin Pract. 2002;5:143–151. [PubMed] [Google Scholar]
- 17.Best AE. Secondary databases and their use in outcomes research: a review of the Area Resource File and the Healthcare Cost and Utilization Project. J Med Syst. 1999;23:175–181. doi: 10.1023/a:1020515419714. [DOI] [PubMed] [Google Scholar]
- 18.Agency for Healthcare Research and Quality. [Accessed October 2];Nationwide in-patient sample. 2002 Available at http://www.ahrq.gov/data/hcup/hcupnis.htm. [Google Scholar]
- 19.McGrath PD, Wennberg DE, Dickens JDJ, et al. Relation between operator and hospital volume and outcomes following percutaneous coronary interventions in the era of the coronary stent. JAMA. 2000;284:3139–3144. doi: 10.1001/jama.284.24.3139. [DOI] [PubMed] [Google Scholar]
- 20.Maynard C, Chapko MK, Every NR, Ritchie JL. Coronary angioplasty outcomes in the Healthcare Cost and Utilization Project, 1993–1994. Am J Cardiol. 1998;81:848–852. doi: 10.1016/s0002-9149(98)00017-4. [DOI] [PubMed] [Google Scholar]
- 21.Ritchie JL, Maynard C, Chapko MK, Every NR, Martin DC. Association between percutaneous transluminal coronary angioplasty volume and outcomes in the Healthcare Cost and Utilization Project, 1993–1994. Am J Cardiol. 1999;83:493–497. doi: 10.1016/s0002-9149(98)00901-1. [DOI] [PubMed] [Google Scholar]
- 22.Doucet M, Eisenberg M, Joseph L, Pilote L. Effects of hospital volume on long-term outcomes after percutaneous transluminal coronary angioplasty after acute myocardial infarction. Am Heart J. 2002;144:144–150. doi: 10.1067/mhj.2002.123571. [DOI] [PubMed] [Google Scholar]
- 23.Maynard C, Every NR, Chapko MK, Ritchie JL. Institutional volumes and coronary angioplasty outcomes before and after the introduction of stenting. Eff Clin Pract. 1999;2:108–113. [PubMed] [Google Scholar]
- 24.Ho V. Evolution of the volume-outcome relation for hospitals performing coronary angioplasty. Circulation. 2000;101:1806–1811. doi: 10.1161/01.cir.101.15.1806. [DOI] [PubMed] [Google Scholar]
- 25.Maynard C, Every NR, Chapko MK, Ritchie JL. Decline in the number of low-volume hospitals performing coronary angioplasty in California, 1989 to 1996. Am J Cardiol. 2000;85:1026–1027. doi: 10.1016/s0002-9149(99)00925-x. [DOI] [PubMed] [Google Scholar]
- 26.Ho V. Learning and the evolution of medical technologies: the diffusion of coronary angioplasty. J Health Econ. 2002;21:873–885. doi: 10.1016/s0167-6296(02)00057-7. [DOI] [PubMed] [Google Scholar]
- 27.Ellis SG, Weintraub WS, Holmes D, Shaw R, Block PC, King SB. Relation of operator volume and experience to procedural outcome of percutaneous coronary revascularization at hospitals with high interventional volumes. Circulation. 1997;96:2479–2484. doi: 10.1161/01.cir.95.11.2479. [DOI] [PubMed] [Google Scholar]
- 28.Hartz AJ, Kuhn EM, Kayser KL, Pryor DB, Green R, Rimm AA. Assessing providers of coronary revascularization: a method for peer review organizations. Am J Public Health. 1992;82:1631–1640. doi: 10.2105/ajph.82.12.1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Popma JJ, Kuntz RE, Baim DS. A decade of improvement in the clinical outcomes of percutaneous coronary intervention for multivessel coronary artery disease. Circulation. 2002;106:1592–1594. doi: 10.1161/01.cir.0000033309.35425.a6. [DOI] [PubMed] [Google Scholar]
- 30.Hasdai D, Berger PB, Bell MR, Rihal CS, Garratt KN, Holmes DRJ. The changing face of coronary interventional practice. Arch Intern Med. 1997;157:677–682. [PubMed] [Google Scholar]
- 31.Kimmel SE, Localio AR, Krone RJ, Laskey WK for the Registry Committee of the Society for Cardiac Angiography and Interventions. The effects of contemporary use of coronary stents on in-hospital mortality. J Am Coll Cardiol. 2001;37:499–504. doi: 10.1016/s0735-1097(00)01115-3. [DOI] [PubMed] [Google Scholar]
- 32.Ritchie JL, Maynard C, Every NR, Chapko MK. Coronary artery stent outcomes in a Medicare population: less emergency bypass surgery and lower mortality rates in patients with stents. Am Heart J. 1999;138:437–440. doi: 10.1016/s0002-8703(99)70144-4. [DOI] [PubMed] [Google Scholar]
- 33.Watanabe CT, Maynard C, Ritchie JL. Short-term outcomes after percutaneous coronary intervention: effects of stenting and institutional volume shifts. Am Heart J. 2002;144:309–314. [PubMed] [Google Scholar]
- 34.The EPILOG Investigators. Platelet glycoprotein IIb/IIIa receptor blockade and low-dose heparin during percutaneous coronary revascularization. N Engl J Med. 1997;336:1689–1697. doi: 10.1056/NEJM199706123362401. [DOI] [PubMed] [Google Scholar]
- 35.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med. 2002;137:511–520. doi: 10.7326/0003-4819-137-6-200209170-00012. [DOI] [PubMed] [Google Scholar]
- 36.Kessler DP, McClellan MB. Is hospital: competition socially wasteful? Q J Econ. 2000;115:577–615. [Google Scholar]
- 37.Birkmeyer CM, Skinner JS, Wennberg DE. Will volume-based referral strategies reduce costs or just save lives? Health Aff. 2002;21:234–241. doi: 10.1377/hlthaff.21.5.234. [DOI] [PubMed] [Google Scholar]
- 38.Finlayson SRG, Birkmeyer CM, Tosteson ANA, Nease RFJ. Patient preferences for location of care: implications for regionalization. Med Care. 1999;37:204–209. doi: 10.1097/00005650-199902000-00010. [DOI] [PubMed] [Google Scholar]
- 39.Cannon CP, Weintruab WS, Demopoulos LA, et al. Comparison of early invasive and conservative strategies in patients with unstable coronary syndromes treated with the glyocoprotein IIb/IIIa inhibitor tirofiban. N Engl J Med. 2001;344:1879–1887. doi: 10.1056/NEJM200106213442501. [DOI] [PubMed] [Google Scholar]
- 40.Mehta SR, Yusuf S, Peters RJ, et al. Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet. 2001;358:527–533. doi: 10.1016/s0140-6736(01)05701-4. [DOI] [PubMed] [Google Scholar]
- 41.Morice M-C, Serruys PW, Sousa JE, et al. A randomized study of a sirolimus-eluting stent with a standard stent for coronary revascularization. N Engl J Med. 2002;346:1773–1780. doi: 10.1056/NEJMoa012843. [DOI] [PubMed] [Google Scholar]
- 42.Epstein AM. Volume and outcome—it is time to move ahead (editorial) N Engl J Med. 2002;346:1161–1164. doi: 10.1056/NEJM200204113461512. [DOI] [PubMed] [Google Scholar]
- 43.Kimmel SE, Sauer WH, Brensinger C, Hirshfield J, Haber HL, Localio AR. Relationship between coronary angioplasty laboratory volume and outcomes after hospital discharge. Am Heart J. 2002;143:833–840. doi: 10.1067/mhj.2002.122116. [DOI] [PubMed] [Google Scholar]