Abstract
Background
Prior studies in urban emergency departments (EDs) have found poor quality of chronic asthma care and identified beliefs and barriers associated with low rates of follow-up with a primary care provider (PCP) after an ED visit.
Objectives
To develop an ED-based intervention including asthma symptom screening, a video developed to impact beliefs about PCP follow-up, and a mailed follow-up reminder; and measure the effect of the intervention on rates of PCP follow-up and asthma-related outcomes.
Methods
This randomized controlled trial enrolled children age 1–18 years who were discharged after asthma treatment in an urban children’s hospital ED. Control subjects received standard instructions to follow up with a PCP within 3–5 days. In addition, intervention subjects: 1. Received a letter to take to their PCP if they screened positive for persistent asthma symptoms, 2. Viewed a video featuring families and providers discussing the importance of asthma control, and 3. Received a mailed reminder to follow up with a PCP. All subjects were contacted by phone at 1, 3, and 6 months after the ED visit, and follow-up was confirmed by PCP record review. Asthma-related quality of life (AQOL), symptoms, and beliefs about asthma
Results
A total of 433 subjects were randomized, and baseline measures of demographics and asthma clinical status were similar between study groups. After the intervention and prior to ED discharge, intervention subjects were more likely to endorse beliefs about the benefits of regular care than controls. However, the percentage following up with a PCP during the 4 weeks after the ED visit (44.5%) was similar to controls (43.8%). AQOL, medication use, and ED visits over the subsequent 6 months were also similar between study groups.
Conclusions
An ED-based intervention influenced short-term beliefs but did not increase PCP follow-up or asthma-related outcomes.
Keywords: asthma, emergency, primary care, children
Introduction
The emergency department (ED) serves an important role in caring for the over 6 million American children with asthma. Children present to EDs at higher rates than adults, and minority children have particularly high visit rates; the rate among black children is more than 2.5 times the rate among whites.1 Concern about the high burden of asthma has led to the development of practice guidelines such as the National Asthma Education Program (NAEPP): Guidelines for the Diagnosis and Management of Asthma published by the NHLBI.2 Central to these guidelines is the importance of ongoing preventive care. After an ED visit, the Guidelines recommend follow-up with a primary care provider (PCP) to provide therapies such as preventive controller medications which have been demonstrated to improve outcomes in multiple studies. 3–6
Although recommendations for follow-up with a PCP are clear, studies have demonstrated poor adherence, particularly among inner-city children for whom reported follow-up rates range from 22% to 52% following an ED visit.7–10 The reasons for poor follow-up are likely multifactorial. Although almost all of the parents in the National Cooperative Inner-City Asthma Study could identify a PCP for their child, more than half reported difficulty in accessing short-term or follow-up care for asthma.11 Prior studies have designed interventions to reduce these health-system barriers but have required substantial resources and had limited effect on subsequent quality of care or outcomes.8–10,12,13 In addition to health-system barriers to follow-up, qualitative research with inner-city families has identified beliefs and misconceptions about preventive care for asthma.14 In a prior study we demonstrated correlation between beliefs expressed by parents in the ED and likelihood of follow-up with a PCP.15 This evidence suggests that ED-based interventions to address beliefs about preventive care would have the potential to improve outcomes by utilizing a “teachable moment” at the time of an ED visit.
The primary goal of this study was to design and test an intervention that could practically be carried out in the ED environment and which would address beliefs and barriers to follow-up asthma care among inner-city families. To address this goal we created a brief video focusing on beliefs reported in prior studies and featuring families and healthcare providers discussing these beliefs and misconceptions. Viewing the video was combined into a three-part intervention along with a letter describing the results of asthma symptom screening for the family to take to their PCP and a mailed reminder to make a follow-up appointment. We then tested the intervention in a randomized trial conducted in an urban children’s hospital ED to determine whether it improved follow-up rates with a PCP during the 4 weeks after an ED visit. Secondary outcomes included satisfaction with the ED visit and subsequent use of asthma controller medications, ED visits, and asthma-related quality of life during the 6 months after enrollment.
Methods
Prior to conducting the study, the Institutional Review Board approved the protocol. The video used in the intervention was developed by a multidisciplinary group of institutional experts. Development of the video began with a literature review of prior research on beliefs and barriers regarding asthma care in urban children. Interviews were filmed with three physician experts and three families of children with well-controlled asthma. Excerpts from these interviews were used to produce a draft video that was shown to a focus group of 15 urban parents who were attending an asthma education class. Feedback from the focus group was used to revise the video and produce a final 12-minute version. The video was structured around three questions: “What is asthma?”; “How can asthma be controlled?”; and What are the benefits of controlling asthma?” (see Table 1).
Table 1.
Components of the Study Intervention.
|
Study staff were present in the ED between the hours of 8 AM and midnight, 7 days per week. Families were approached for enrollment based on the following inclusion criteria: 1) age 1–18 years; 2) residing within city limits; 3) history of asthma defined as 2 or more prior medical visits at which bronchodilators were prescribed; 4) acute respiratory symptoms requiring ED treatment with bronchodilators; 5) treating physician had decided to discharge the patient. Children with a history of cystic fibrosis or congenital cardiac disease were excluded. Because of the need for ED and phone interviews and consent for PCP medical record review, patients were excluded if no English-speaking guardian was present or if the family could not be reached for telephone follow-up. A patient log was kept during the study period to document patients screened and the reasons for exclusion. Patients were not eligible for repeat enrollment.
After obtaining written informed consent, study staff surveyed subjects about demographic characteristics, asthma history, site of primary care, and current therapies. Using a previously validated instrument based on the NAEPP guidelines, subjects were categorized as having persistent asthma if they reported baseline symptoms (cough, wheeze, shortness of breath, trouble breathing or chest tightness) more than twice weekly for daytime symptoms or twice monthly for nighttime symptoms.16 Subjects completed the Integrated Therapeutics Group (ITG) Child Asthma Short Form, an 8-item instrument which has been previously validated to measure asthma-related quality of life.17 Study staff then assigned patients to intervention or control groups using a series of numbered, opaque envelopes that had been pre-randomized in blocks of eight. Control group patients received standard discharge instructions to follow-up with their PCP within 3–5 days. In the ED, all intervention group participants viewed the intervention video; the subgroup who screened positive for persistent asthma, received a letter regarding the results to give to their PCP. All participants completed the Parental Impressions of the Benefits (Pros) and Barriers (Cons) of Follow-up Care Scale at the end of the visit (after the intervention for subjects in that group).18 This scale is a validated 24-item instrument that measures perceived benefits and barriers to follow-up after an ED visit. For the last 252 subjects enrolled in the study we asked about satisfaction with the ED visit using the same 5-point scale Likert scale as the Pros and Cons survey.
After the visit, all intervention participants received a mailed reminder (a self-addressed postcard completed during the ED visit) to schedule a follow-up appointment with their PCP. Copies of ED medical records for both control and intervention groups were faxed to PCPs, as per standard procedure in this ED separate from the study protocol. Initiating controller medications at ED discharge was not part of routine practice during the study.
All study subjects were contacted by phone one, three, and six months following the ED visit; phone interviewers were unaware of group assignment. A standardized phone survey was administered which inquired about the patient’s symptoms since the visit, date of follow-up, return ED visits, and interventions that had taken place. We measured asthma-related quality of life and asthma symptoms using the same instruments as at the baseline visit and re-administered the Pros survey. At study conclusion, we contacted PCP offices and reviewed medical records to verify dates of subsequent visits and outcomes.
Sample size was estimated based on a predicted follow-up rate among controls of 45%. Assuming 10% loss to follow-up alpha1=0.05, 440 subjects were needed to provide 90% power to detect an increase of 15% (i.e. from 45% to 60%) in the follow-up rate. Statistical analysis was carried out using SPSS Version 10.1 (Chicago, IL) and STATA Version 7.0 (College Station, TX). Group differences were determined using chi-square for categorical variables, independent sample t-test for comparison of means of continuous variables, and Mann-Whitney U test for comparison of medians.
Results
Study Enrollment
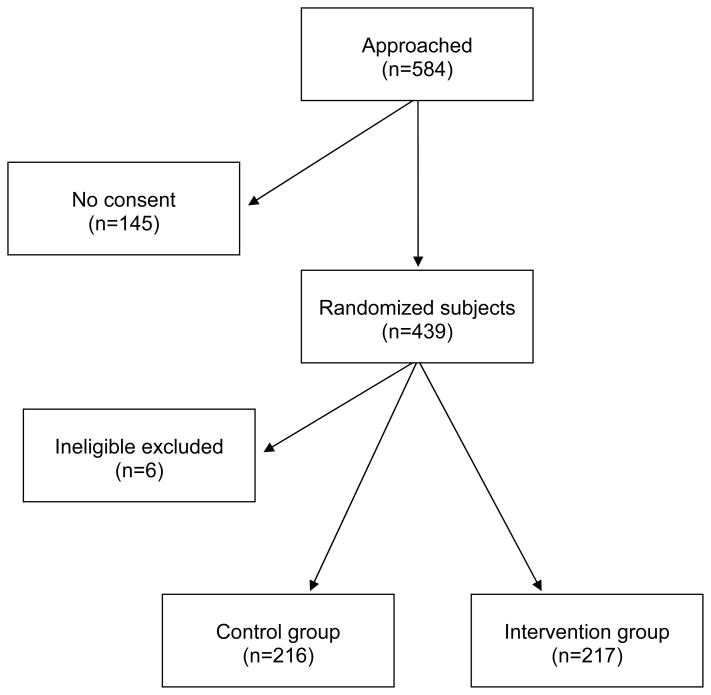
Between March and December 2005, a total of 2292 asthmatic children between the ages of 1 and 18 were screened by study staff. Of these, exclusions were made for the following reasons: clinical decision to admit to the hospital (857) or discharge when study staff were not present (97), non-urban residence (277), no guardian present to give consent (48), not English-speaking (8), or prior study enrollment (93). Of the 912 potentially eligible subjects, 584 were approached for enrollment. Of those approached, 439 subjects (70%) gave informed consent (Figure 1). Randomization assigned 220 subjects to the control group and 219 to the intervention group. Six subjects were excluded due to prior enrollment in the study (5), or inadequate documentation of guardian consent (1). Thirteen other subjects (9 intervention and 4 control) subsequently were found not to meet eligibility criteria because of the clinical team’s decision to admit after enrollment in the study (10) or living outside of city limits (3); these subjects were included in the analysis.
Figure 1.
Study enrollment diagram.
Baseline characteristics are presented in Table 2 and were similar between control and intervention groups. Similar to prior studies in this population, a majority of the study subjects were of black race, enrolled in Medical Assistance, and had high use of the ED for asthma care, with 58% of subjects reporting 2 or more ED asthma visits during the prior year.9 Running out of medications was reported frequently at the time of the ED visit, with 27% for albuterol, and 28% of those using inhaled corticosteroids running out during the week prior to the ED visit. A total of 32 subjects (16 in each study group) had a prescription for inhaled corticosteroids initiated at the time of the ED visit as part of care not defined by the study protocol. When asked about satisfaction with the information received during the ED visit on a 5-point Likert scale, more intervention subjects chose 5 (Extremely satisfied) compared to controls (73% vs. 65%) although this difference was not statistically significant (8%, 95% confidence interval −4%, 19%)
Table 2.
Baseline characteristics of control and intervention groups.
| Control | Intervention | |
|---|---|---|
| n=216 (%) | n=217 (%) | |
| Male | 133 (62) | 135 (62) |
| Black race | 199 (92) | 206 (95) |
| Age, mean years ± sd | 6.7 ± 4.5 | 6.6 ± 4.4 |
| Insurance type | ||
| Medical Assistance | 150 (69) | 145 (67) |
| Commercial | 58 (27) | 63 (29) |
| None | 8 (4) | 9 (4) |
| Primary care provider (PCP) type | ||
| Teaching hospital | 143 (66) | 130 (60) |
| Private office | 48 (22) | 60 (28) |
| Public health clinic | 25 (12) | 27 (12) |
| Has an asthma specialist | 40 (18) | 27 (12) |
| Had a PCP asthma visit in past year | 123 (57) | 136 (63) |
| Had an ED asthma visit in past year | 164 (76) | 159 (73) |
| Asthma hospitalization in past year | 74 (34) | 67 (31) |
| Persistent asthma symptoms (per NAEPP) | 108 (50) | 109 (50) |
| Using controller medication daily | 98 (45) | 93 (43) |
| Triage category for ED visit | ||
| Non-urgent or Urgent | 113 (52) | 124 (57) |
| Emergent or Critical | 88 (41) | 83 (38) |
| Unknown | 15 (7) | 10 (5) |
Study Outcomes
Research staff successfully completed phone interviews with 385 (89%) families 4–6 weeks after the ED visit and data on completion rates for subsequent calls are presented in Table 3. Review of PCP medical records was completed for 365 (84%) subjects; the PCPs treating the remaining 68 (16%) subjects either did not respond to the investigator’s request for PCP medical record review or did not have any record of the patients. As has been described in prior studies, overall PCP follow-up rates as reported by the family were higher than those determined by objective PCP record review (56% vs. 41%);9 agreement where both were available was 72% (kappa=0.45). To determine an overall outcome for follow-up with a PCP, PCP record review was considered the primary source, with family report used when PCP review was not available. This method provided an outcome for 425 (89%) of subjects.
Table 3.
Study outcomes for control and intervention groups.
| Control n=216 | Intervention n=217 | Difference [95% CI] | |
|---|---|---|---|
| PCP Follow-up during 4 weeks after ED visit | |||
| By PCP record review, % | 39 | 42 | 3 [−7, 13] |
| By Phone interview, % | 56 | 57 | 1 [− 9, 11] |
| Combination of PCP and phone, % | 46 | 47 | 1 [−8, 11] |
| 1-month phone interview completed, % | 87 | 90 | 3 [−3, 9] |
| Return visit to ED (%) | 14 | 9 | −5 [−12, 1] |
| Patient schooldays missed, median [IQ range] | 2 [0,6] | 1 [0,4] | 1 |
| Guardian workdays missed, median [IQ range] | 0 [0,3] | 0 [0,2] | 0 |
| Using controller medication daily, % of complete | 64 | 66 | 2 [−8, 12] |
| Mean asthma-related quality of life [sd], 0–100 | 70 [22] | 69 [24] | −1 [4, −6] |
| 3-month phone interview completed, % | 78 | 83 | 5 [−3, 12] |
| Using controller medication daily, % of complete | 55 | 50 | −5 [−16, 5] |
| Mean asthma-related quality of life [sd], (0–100) | 70 [25] | 71 [23] | 1 [7, −4] |
| 6-month phone interview completed (%) | 75 | 75 | 0 [−9, 7] |
| Using controller medication daily, % of complete | 58 | 54 | −4 [−15, 7] |
| Mean asthma-related quality of life [sd], (0–100) | 70 [24] | 71 [25] | 1 [−5, 6] |
| PCP record review completed | 83 | 85 | 2 [−5, 9] |
| 6 month healthcare utilization for asthma | |||
| ED visit, % | 31 | 29 | −2 [−11, 6] |
| Hospitalization, % | 10 | 11 | 1 [−5, 7] |
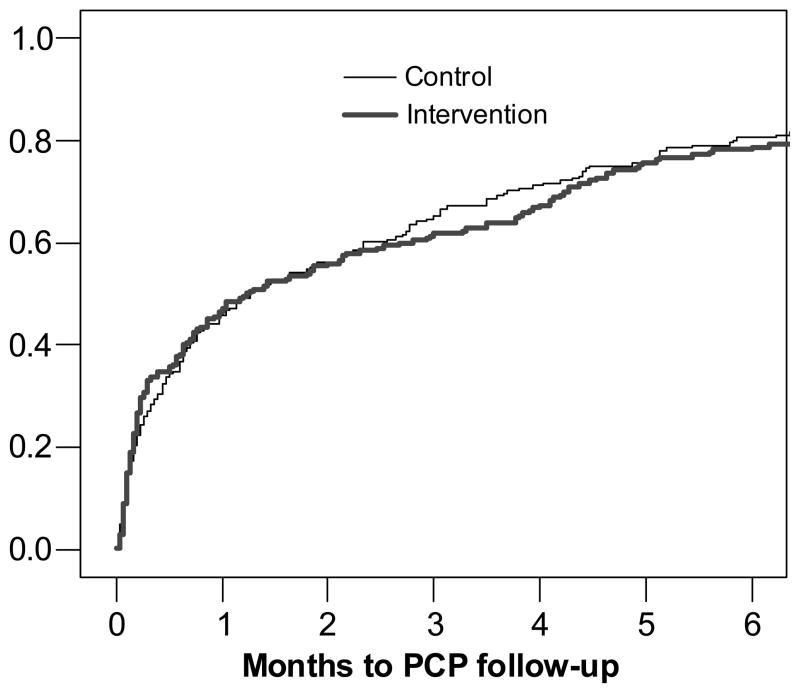
Primary and secondary outcomes are presented in Table 3 and Figure 2. PCP follow-up rates were similar between groups with a median time to follow up of 38 days in both groups, and over a third of subjects not seeing a PCP within the 3 months after the ED visit. Symptoms, asthma-related quality of life and subsequent ED visits were all similar between study groups. Over half (58.1%) of subjects making a return ED visit within 6 months had seen their PCP within the month following the initial ED visit. Daily controller medication use was highest at one month after the ED visit, with 65% of families reporting daily use; another 12% had a prescription for a controller medication but used it less frequently than daily. We conducted additional analysis to evaluate the primary outcome in subgroups categorized by: presence or absence of persistent asthma symptoms, controller medication use prior to the ED visit, and type of primary care site. Intervention and control groups had similar outcomes across these subgroups (data not shown).
Figure 2.
Proportion of subjects following up with a PCP over time after the initial ED visit
Beliefs about Asthma follow-up
Results of the Pros and Cons survey administered at the end of the ED visit are presented in Table 4. Although both intervention and control groups generally endorsed positive beliefs about the need for follow-up, they differed on several items, including beliefs about whether children with asthma who see their doctor regularly have fewer ED visits, miss less school, or have fewer asthma symptoms; intervention subjects had higher median values for these items than controls. When the Pros survey was repeated at the 3-month phone interview, no significant differences were observed between the groups (data not shown).
Table 4.
Responses to the Parental Impressions of the Benefits (Pros) and Barriers (Cons) of Follow-up Care Scale conducted at the end of the ED visit.
| Going to a follow-up visit… | Not (%) | Slightly (%) | Moderately (%) | Very (%) | Extremely (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| C | I | C | I | C | I | C | I | C | I | p-value | |
| Pros: | |||||||||||
| 1. …allows me to ask the doctor questions. | 3 | 1 | 4 | 4 | 8 | 7 | 30 | 27 | 56 | 62 | 0.2 |
| 2. …allows me to find out if my child is better. | 1 | 1 | 2 | 2 | 7 | 8 | 21 | 24 | 69 | 65 | 0.4 |
| 3. …allows me to ask about triggers or things that worsen asthma. | 3 | 3 | 2 | 3 | 9 | 9 | 26 | 26 | 60 | 60 | 0.9 |
| 4. …makes me feel that I have done my best. | 3 | 1 | 1 | 2 | 6 | 7 | 24 | 23 | 66 | 67 | 0.9 |
| 5. …allows me to get my child’s medication checked. | 3 | 2 | 2 | 0 | 5 | 6 | 18 | 20 | 72 | 72 | 0.8 |
| 6. …allows my child’s siblings and other family to learn about asthma. | 16 | 10 | 5 | 6 | 16 | 9 | 23 | 24 | 40 | 52 | 0.003 |
| 7. …allows me to get asthma medication for my child at school. | 13 | 11 | 5 | 2 | 6 | 7 | 19 | 18 | 57 | 62 | 0.2 |
| 8. …allows me to get asthma information for my child’s school. | 20 | 13 | 6 | 4 | 9 | 8 | 18 | 20 | 48 | 56 | 0.04 |
| 9. …allows my child to be sent to a specialist. | 18 | 9 | 7 | 5 | 6 | 13 | 23 | 19 | 47 | 54 | 0.06 |
| 10. Children with asthma are healthier if they see their doctor regularly. | 5 | 2 | 4 | 1 | 7 | 7 | 15 | 20 | 70 | 70 | 0.6 |
| 11. …helps me feel that next time I might be able to prevent the ED visit. | 7 | 6 | 4 | 4 | 8 | 9 | 23 | 22 | 58 | 60 | 0.6 |
| 12. Children with asthma have fewer ED visits if they see their doctor regularly. | 16 | 8 | 11 | 11 | 18 | 14 | 17 | 24 | 38 | 43 | 0.03 |
| 13. Children with asthma miss less school if they see their doctor regularly. | 21 | 10 | 11 | 9 | 17 | 10 | 18 | 27 | 34 | 44 | 0.001 |
| 14. Children with asthma have fewer symptoms if they see their doctor regularly. | 22 | 13 | 10 | 11 | 20 | 14 | 17 | 26 | 31 | 36 | 0.02 |
| Cons: | |||||||||||
| 15. …means I have to find transportation to get there. | 58 | 56 | 7 | 5 | 6 | 4 | 11 | 11 | 19 | 24 | 0.5 |
| 16. …forces me to take time off from work. | 43 | 44 | 9 | 9 | 9 | 12 | 10 | 9 | 29 | 26 | 0.6 |
| 17. …means I have to get a family member or friend to sit with the other kids. | 68 | 67 | 5 | 6 | 4 | 6 | 8 | 8 | 16 | 13 | 1.0 |
| 18. …means I have to find a babysitter for the other children. | 69 | 69 | 4 | 7 | 3 | 4 | 7 | 8 | 16 | 13 | 0.9 |
| 19. …means I have to pay for transportation. | 53 | 47 | 9 | 12 | 7 | 6 | 9 | 8 | 23 | 27 | 0.2 |
| 20. …is hard because my family doesn’t want to spend the time. | 87 | 86 | 4 | 2 | 5 | 3 | 2 | 3 | 3 | 5 | 0.8 |
| 21. I don’t need to see the doctor unless my child is sick. | 71 | 74 | 6 | 2 | 13 | 10 | 4 | 6 | 7 | 8 | 0.8 |
| 22. …is hard because my family doesn’t think my child has asthma. | 96 | 94 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 0.4 |
| 23. …is hard because my family doesn’t want to spend the money. | 96 | 95 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 0.6 |
| 24. My family and friends can give me good advice about asthma so I don’t need a follow-up visit. | 94 | 95 | 2 | 2 | 2 | 2 | 1 | 0 | 2 | 1 | 0.4 |
Discussion
Overall, this study assessed a three-part intervention to improve PCP follow-up after an ED visit for asthma in an urban population. Intervention subjects who viewed an educational video showed some differences in beliefs on a standardized instrument administered during the ED visit, although not at the time of a phone survey 3 months later. The primary outcome of follow-up with a PCP was similar between groups, with most subjects not visiting a PCP within the month following the ED visit, and a substantial proportion experiencing ED visits and hospitalizations during the next 6-months.
Our results are consistent with the limited success of prior attempts to improve long-term care after an ED asthma visit in urban populations. Some of these studies focused on reducing financial barriers to follow-up by providing interventions such as transportation vouchers or direct monetary incentives.8,12 Others focused on improving linkage to primary care by scheduling a follow-up appointment or providing access to a case manager to assist the family.9,10,13 Some of these studies were able to improve short-term PCP follow-up rates, for example a prior study in this population increased follow-up within 4 weeks from 46% to 64%, but none had a lasting effect on outcomes such as quality of life or return ED visits.9 In addition, many of these interventions required substantial resources that would not be generalizable to a routine environment. Although the current intervention was designed to be feasible, it appears not to have improved PCP follow-up.
Our study was innovative in its attempt to address beliefs about long-term care of asthma at the time of the ED visit. Prior research has documented beliefs in inner-city families that may negatively impact subsequent preventive care.7,11,14 For example, Mansour et al. conducted focus groups of inner-city parents and found consistent misperceptions about the value of preventive medications such as concerns about dependence and safety. Parents often limited the activity of their child and reported a high impact of their child’s asthma on quality of life for the entire family. Our video was designed to address these misconceptions and stress the positive benefit of asthma control on the child and family. Other urban families were included in the content and design of the video to increase relevance to the intended audience. Viewing the video during the ED visit was well-accepted by families as evidenced by high satisfaction scores. In addition we observed some improvement in items on the Pros and Cons Survey relating to the ability of parents to prevent future asthma morbidity. It is possible that intervention at a single visit is ineffective but cumulative reinforcement over time may have more benefit. In addition, the format of the intervention may need to be reconsidered. Our intervention was a passively viewed video; Sockrider et al. recently designed a computer-based resource which used video clips and other tools chosen for the family by an asthma educator in the ED.19 Preliminary results from a study of this resource in an urban ED report a reduction in subsequent ED visits. Future work on educational interventions should be tailored to the family but also designed for a routine clinical setting, perhaps through web-based approaches or other technologies.
Recently, investigators have gone beyond facilitation of PCP follow-up or addressing beliefs and studied more substantial interventions to improve long-term asthma care. Lehman et al. described initiating a two week course of inhaled corticosteroids at the time of an ED visit in a series of 47 children; of the 28 who followed up with a PCP, the majority (21) of ED prescriptions were continued at that visit and 13 families reported continued adherence in a later phone interview.20 Teach et al. implemented a much more comprehensive intervention that involved bringing families back to the ED on a subsequent day for a follow-up asthma visit that included education, initiating controller medications, and scheduling a follow-up visit with a PCP.21 In a randomized trial, 70% of those randomized to the intervention attended the ED follow-up visit, and this group had improved use of controller medications, fewer unscheduled asthma visits and improved quality of life as compared to controls. Although linkage back to a PCP was a goal of the study, no improvement was observed in this outcome. The success of these studies suggests that initiating controller medications may be an appropriate role for the ED; in fact the most recent NAEPP Guidelines recommend that ED physicians consider doing this, while noting the limited available data.2 The challenge for future studies will be to devise effective and generalizable ways to do this in the ED setting in a way that improves outcomes and supports a long-term relationship with a PCP.
There were a number of limitations to this study. The study was conducted in a single center in a predominantly African-American population and may not be generalizable to other settings. A majority of the patients were followed in hospital-affiliated teaching clinics. Patients followed by both residents or faculty in our institution use a nurse-based, after-hours call system with physician back-up and acute visits reserved in the schedule; the impact of the study intervention might be different in other systems of care. In addition, coincident to the study there were several quality improvement programs relating to asthma occurring within and outside our institution. These programs have increased use of controller medications across our population and may have limited the effectiveness of further intervention. Overall rates of daily controller medication use were higher than in a prior study in our population (44% vs. 38%), although presence of persistent asthma symptoms remained common (50% vs 70%).9 We excluded non-English-speaking families (although only 8 were excluded for this reason) and did not enroll between midnight and 8AM; families seeking care overnight may differ from other families. Although we were well-powered to detect outcomes in the overall study group, power was limited in subgroups and it is possible that the intervention may have benefits we were unable to detect in selected patients.
In summary, we found that a three-part ED-based intervention including asthma symptom screening, a mailed reminder, and viewing an educational video did not improve follow-up or other outcomes. The intervention was well accepted by families and appeared to impact beliefs at the time of the visit, but not at a subsequent phone call. Future research should evaluate interactive forms of education that can be implemented in the ED and combine education with initiation of preventive medications to assess impact on long-term care outcomes.
Acknowledgments
National Heart, Lung and Blood Institute Award 5K23HL074250-05
Abbreviations
- AQOL
Asthma-related quality of life
- ED
Emergency Department
- NAEPP
National Asthma Education and Prevention Program
- PCP
Primary care provider
Footnotes
Clinicaltrials.gov number: NCT00113633
References
- 1.Akinbami LJ. The state of childhood asthma, United States, 1980–2005. CDC Advance Data No 381. From Vital and Health Statistics. 2006 [PubMed] [Google Scholar]
- 2.Expert panel report 3: Guidelines for the Diagnosis and Management of Asthma. National Institutes of Health Pub. # 08-5846; Bethesda, MD: 2007. National Asthma Education and Prevention Program. Available at http://www.nhlbi.nih.gov/guidelines/asthma/asthmafullrpt.pdf. [Google Scholar]
- 3.Lieu TA, Quesenberry CP, Capra AM, et al. Outpatient management practices associated with reduced risk of pediatric asthma hospitalization and emergency department visits. Pediatrics. 1997;100:334–341. doi: 10.1542/peds.100.3.334. [DOI] [PubMed] [Google Scholar]
- 4.Donahue JG, Weiss ST, Livingston JM, et al. Inhaled steroids and the risk of hospitalization for asthma. JAMA. 1997;277:887–891. [PubMed] [Google Scholar]
- 5.The Childhood Asthma Management Program Research Group. Long-term effects of budesonide or nedocromil in children with asthma. N Engl J Med. 2000;343:1054–1063. doi: 10.1056/NEJM200010123431501. [DOI] [PubMed] [Google Scholar]
- 6.Adams RJ, Fuhlbrigge A, Finkelstein JA, et al. Impact of inhaled antiinflammatory therapy on hospitalization and emergency department visits for children with asthma. Pediatrics. 2001;107:706–711. doi: 10.1542/peds.107.4.706. [DOI] [PubMed] [Google Scholar]
- 7.Leickly FE, Wade SL, Crain E, Kruszon-Moran D, Wright EC, Evans R. Self-reported adherence, management behavior, and barriers to care after an emergency department visit by inner city children with asthma. Pediatrics. 1998;101(5) doi: 10.1542/peds.101.5.e8. URL: http://www.pediatrics.org/cgi/content/full/101/5/e8. [DOI] [PubMed]
- 8.Smith S, Jaffe D, Fisher E, et al. Improving follow-up for children with asthma after an acute emergency department visit. J Pediatr. 2004;145:772–7. doi: 10.1016/j.jpeds.2004.08.029. [DOI] [PubMed] [Google Scholar]
- 9.Zorc JJ, Scarfone RJ, Li Y, et al. Scheduled follow-up after a pediatric emergency department visit for asthma. Pediatrics. 2003;111(3):495–502. doi: 10.1542/peds.111.3.495. [DOI] [PubMed] [Google Scholar]
- 10.Smith SR, Jaffe DM, Highstein G, et al. Asthma coaching in the emergency department. Acad Emerg Med. 2006;13(8):835–9. doi: 10.1197/j.aem.2006.03.565. [DOI] [PubMed] [Google Scholar]
- 11.Crain EF, Kercsmar C, Weiss KB, Mitchell H, Lynn H. Reported difficulties in access to quality care for children with asthma in the inner city. Arch Pediatr Adolesc Med. 1998;152:333–339. doi: 10.1001/archpedi.152.4.333. [DOI] [PubMed] [Google Scholar]
- 12.Baren JM, Boudreaux ED, Brenner BE, et al. Randomized controlled trial of emergency department interventions to improve primary care follow-up for patients with acute asthma. Chest. 2006;129:257–265. doi: 10.1378/chest.129.2.257. [DOI] [PubMed] [Google Scholar]
- 13.Gorelick MH, Meurer JR, Walsh-Kelly CM, et al. Emergency Department Allies: A controlled trial of two emergency department-based follow-up interventions to improve asthma outcomes in children. Pediatrics. 2006;117:S127–S134. doi: 10.1542/peds.2005-2000J. [DOI] [PubMed] [Google Scholar]
- 14.Mansour ME, Lanphear BP, DeWitt TG. Barriers to asthma care in urban children: Parent perspectives. Pediatrics. 2000;106:512–519. doi: 10.1542/peds.106.3.512. [DOI] [PubMed] [Google Scholar]
- 15.Zorc JJ, Scarfone RJ, Li Y. Predicting follow-up after an emergency department visit for asthma. J Asthma. 2005;42:571–6. doi: 10.1080/02770900500215947. [DOI] [PubMed] [Google Scholar]
- 16.Zorc JJ, MD, Pawlowski NA, Allen J, et al. Validation of an instrument to measure asthma control in children. J Asthma. 2006;43:753–8. doi: 10.1080/02770900601031615. [DOI] [PubMed] [Google Scholar]
- 17.Bukstein DA, McGrath MM, Buchner DA, Landgraf J, Goss TF. Evaluation of a short form for measuring health-related quality of life among pediatric asthma patients. J Allergy Clin Immunol. 2000;105:245–251. doi: 10.1016/s0091-6749(00)90072-1. [DOI] [PubMed] [Google Scholar]
- 18.Smith SR, Highstein GR, Jaffe DM, Fisher EB, Strunk RC. Parental impressions of the benefits (pros) and barriers (cons) of follow-up care after an acute emergency visit for children with asthma. Pediatrics. 2002;110:323–30. doi: 10.1542/peds.110.2.323. [DOI] [PubMed] [Google Scholar]
- 19.Sockrider MM, Abramson S, Brooks E, et al. Delivering tailored asthma family education in a pediatric emergency department setting: A pilot study. Pediatrics. 2006;117:S135–44. doi: 10.1542/peds.2005-2000K. [DOI] [PubMed] [Google Scholar]
- 20.Lehman HK, Lillis KA, Shaha SH, Augustine M, Ballow M. Initiation of maintenance antiinflammatory medication in asthmatic children in a pediatric emergency department. Pediatrics. 2006;118:2394–401. doi: 10.1542/peds.2006-0871. [DOI] [PubMed] [Google Scholar]
- 21.Teach SJ, Crain EF, Quint DM, Hylan ML, Joseph JG. Improved asthma outcomes in a high-morbidity pediatric population: Results of an emergency department-based randomized clinical trial. Arch Ped Adolesc Med. 2006;160:535–41. doi: 10.1001/archpedi.160.5.535. [DOI] [PubMed] [Google Scholar]