Abstract
Background:
The outcomes of informal caregivers of survivors of critical illness likely depend on patient characteristics, which may change over time. To date, few studies have examined patient-specific predictors of post-ICU informal caregiver burden, and none has tested whether predictors vary after hospital discharge.
Methods:
We designed a prospective, longitudinal observational study, enrolling 48 patient-caregiver dyads from four ICUs in a university hospital. Informal caregiver depression symptoms were measured with the Center for Epidemiologic Studies Depression scale. Lifestyle disruption was measured with the Activity Restriction Scale. Linear regression models were built to test for patient- and caregiver-specific predictors of depression symptoms and lifestyle disruption 2, 6, and 12 months after ICU admission.
Results:
Patients had a mean (SD) age of 52.5 (19.7) years, 67% were men, median (interquartile range) Acute Physiology and Chronic Health Evaluation score was 52 (38.5, 65). The caregivers had a mean (SD) age of 52.8 (12.8) years, 91.2% were women, and 48% were spouses. Predictors of caregiver depression symptoms were patient gender (men) at 2 and 12 months and tracheostomy at 12 months. Predictors of lifestyle disruption were patient education (more common among high school graduates) and patient gender (men) at 2 months, and tracheostomy, functional dependency, and patient gender (men) at 12 months.
Conclusions:
The determinants of post-ICU informal caregiver burden likely depend on characteristics of the patient as well as the caregiver and may vary over time. Further research is necessary to better understand the longitudinal determinants of burden in order to develop more effective caregiver interventions.
Informal caregivers are an important source of support for our health care system. An estimated 46 million informal caregivers provide support for adults in the United States.1 As a result they are at risk for burden, which can be manifested as depression, physical health problems, employment reduction, and even increased mortality.1-4
Although caregiver burden is traditionally studied among outpatients with chronic illness, informal caregivers are often at the bedside when a loved one is hospitalized. Therefore, an important opportunity exists to study informal caregivers in the context of acute illness. Recent studies have shown that post-ICU informal caregivers also suffer from depression symptoms, reduced employment, and disruption of their lifestyle.5-8
There are two important limitations in the existing literature of post-ICU informal caregivers. First, the studies tend to focus on caregiver-specific predictors of burden rather than patient-specific ones.5-7 In addition, most studies are cross-sectional and do not consider whether predictors of burden change over time as changes occur in a patient’s condition or as caregivers adapt or fatigue.5-8 Therefore, we designed a study from the Quality of Life after Prolonged Mechanical Ventilation(QOL-MV) data set in order to analyze both patient-specific and caregiver-specific predictors of burden, and to test whether these predictors change over time. Second, because of a lack of consensus about the definition of functional dependency in the literature,9,10 we tested three different levels of dependency in order to examine the relative importance of dependency as a predictor of burden. Although caregiver outcomes from this cohort have been previously reported, these studies did not evaluate the variability of predictors of burden over time.7,11 Our primary hypothesis was that predictors of caregiver burden change over time as changes occur in a patient’s condition or in a caregiver’s appraisal of their role.
Materials and Methods
Study Design
This prospective cohort study was designed to examine the 1-year, longitudinal outcomes of survivors of critical illness and their informal caregivers. A detailed description was previously reported.12 Briefly, the QOL-MV cohort included patients admitted to four ICUs at a tertiary-care teaching hospital in Pittsburgh, Pennsylvania over a 26-month period beginning in June 1997. Patients and their caregivers were eligible if mechanical ventilation in an ICU was required for at least 48 h. Patients were excluded if they were hospitalized following solid-organ transplantation, younger than 18 years of age, chronically ventilator dependent prior to hospital admission, or intubated more than 24 h prior to transfer from an outside hospital. Outcome data were collected 2, 6, and 12 months after the initiation of mechanical ventilation. The protocol was approved by the University of Pittsburgh Institutional Review Board.
Patient Data Collection and Measurements
Baseline patient data were obtained by interviews with proxies and from medical records and consisted of sociodemographics, ICU admission diagnosis, Acute Physiology and Chronic Health Evaluation (APACHE) III score,13 and the Charlson comorbidity score.14 Functional status was assessed using two scales; the Activities of Daily Living (ADL) scale,15 ranging from 0 to 6, and the Instrumental Activities of Daily Living (IADL) scale, ranging from 0 to 8.
Informal Caregiver Data Collection and Measurements
The primary caregiver outcomes of interest were depression symptoms and lifestyle disruption. Improvement or worsening of scores in these domains was interpreted as caregiver adaption or fatigue, respectively. Depression symptoms were measured using the Center for Epidemiologic Studies Depression (CES-D) scale,17 a 20-item instrument that has very good reliability (α coefficients, 0.85-0.91) and validity (using Raskin as a criterion, sensitivity was 99%).18 A score ≥ 16 indicates a risk for suffering from clinical depression. The internal consistency of this instrument was very good in this cohort of caregivers (Cronbach α, 0.92-0.93). Lifestyle disruption was evaluated using the Activity Restriction Scale (ARS), an 11-item instrument designed to measure changes in caregiver activities due to caring for the patient.19 Caregivers were asked to report the degree of restriction they were experiencing in 11 categories (eg, caring for self, caring for others, eating habits, and so forth) resulting in a score ranging from 11 to 44. This instrument was modified for the QOL-MV study. The internal consistency was very good (Cronbach α, 0.89-0.90).
Statistical Analysis
Continuous variables are reported as mean (SD) for normally distributed variables, and as median (interquartile range [IQR]) for variables with a skewed distribution. Categorical variables are reported as proportions. Predictors of depression symptoms and lifestyle disruption were determined by building two linear regression models for each time point using CES-D and ARS as the respective dependent variables. Independent variables were included in the model if associated with caregiver instrument scores in univariate analysis at a significance level of P < .20. The patient-specific variables considered for inclusion were age, gender, level of education ( < 12th grade vs ≥ 12th grade), pre-ICU and post-ICU functional status (dependent vs independent), Charlson comorbidity score, APACHE III score, duration of mechanical ventilation, hospital length of stay (LOS), ICU LOS, tracheostomy, and location of residence (home vs institution). Caregiver-specific independent variables tested for inclusion in the multivariable models included gender, age, relationship (spouse vs other), and level of education ( < 12th grade vs ≥ 12th grade). Colinearity was tested for in the final multivariable regression models by using the variance inflation factor. We tested for changes over time in patient and caregiver outcomes using the analysis of variance statistic for continuous variables and the Χ2 statistic for categorical variables. The CES-D and ARS values were square-root transformed to normalize their distributions. In order to determine the effect of varying levels of functional dependency on caregiver outcomes, three different levels of functional dependency were tested in separate regression models: ADL > 0 or IADL > 0; ADL > 0 or IADL > 1; ADL > 0 or IADL > 2. Statistical analyses were performed using Stata (Version 8; StataCorp; College Station, TX).
Results
Patient Outcomes
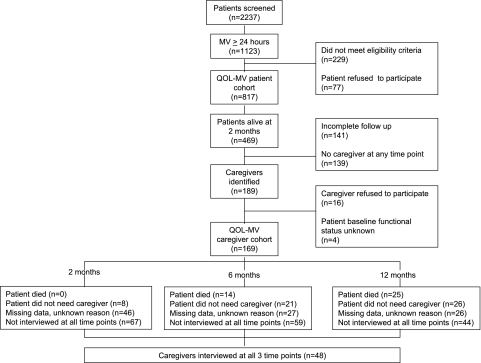
At 2 months after the initiation of mechanical ventilation, the patient mortality rate for the entire QOL-MV cohort was 42.6% (Fig 1). Among the 48 patients enrolled in the caregiver cohort study, 32 (66.7%) were men, their mean (SD) age was 52.5 (19.7) years, they had a median (IQR) APACHE III score of 52 (38.5, 65), and 17 (35.4%) had a tracheostomy (Table 1). Over the 1-year follow-up period, the proportion of functionally dependent survivors (ADL > 0 or IADL > 2) decreased (43 [89.6%], 34 [70.8%], 35 [72.9%], P = .08), and the respective proportion of patients living at home increased (28 [58.3%], 39 [83.0%], 41 [85.4%], P < .01) at 2, 6, and 12 months, respectively.
Figure 1.
Flow diagram of patient and caregiver enrollment. MV = mechanical ventilation; QOL-MV = Quality of Life after Mechanical Ventilation.
Table 1.
—Patient and Caregiver Characteristics
| Characteristic | Patients | Caregivers |
| No. | 48 | 48 |
| Age, mean (SD), y | 52.5 (19.7) | 52.8 (12.8) |
| Male, n (%) | 32 (66.7) | 9 (18.8) |
| Race, n (%) | ||
| White | 43 (89.6) | 44 (91.7) |
| Black | 50 (10.4) | 40 (8.3) |
| Education ≥ 12th grade, No. (%) | 35 (72.9) | 42 (87.5) |
| Relationship, No. (%) | ||
| Spouse | … | 23 (47.9) |
| Other family | … | 18 (37.5) |
| Not family | … | 7 (14.6) |
| Charlson comorbidity score, median (IQR) | 2 (0, 3) | … |
| Pre-ICU ADL (range 0-6), median (IQR) | 0 (0, 1.5) | … |
| Pre-ICU IADL (range 0-8), median (IQR) | 2 (0, 4) | … |
| Disease category, No. (%) | … | |
| Medical | 33 (68.8) | … |
| Surgical | 3 (6.3) | … |
| Trauma | 10 (20.8) | … |
| Tracheostomy, No. (%) | 17 (35.4) | … |
| APACHE III, median (IQR) | 52 (38.5, 65) | … |
| MV duration, median (IQR), d | 10 (5, 16.5) | … |
| ICU LOS, median (IQR), d | 13 (7, 19.5) | … |
| Hospital LOS, median (IQR), d | 19 (13.5, 31) | … |
ADL = activities of daily living; APACHE = Acute Physiologic and Chronic Health Evaluation; IADL = Instrumental Activities of Daily Living; IQR = interquartile range; LOS = length of stay; MV = mechanical ventilation.
Caregiver Outcomes
The caregivers were mostly women (81.2%) and had a mean (SD) age of 52.8 (12.8) years (Table 1). The majority of caregivers were spouses (47.9%), 37.5% were other family members, and 14.6% were not family members. The proportion at risk for depression (ie, caregivers with a high number of depression symptoms as indicated by a CES-D score ≥ 16) was greater than 30% at 2 months and remained high at all three time points. In addition, the caregivers reported moderate or great restriction in more than three activities at 2 months and there was no significant change in their mean activity restriction score over the 12-month period (Table 2).
Table 2.
—Caregiver Outcomes at 2, 6, and 12 Months After the Initiation of Mechanical Ventilation
| Time Point | P Value | |||
| 2 mo | 6 mo | 12 mo | ||
| No. | 48 | 48 | 48 | … |
| Depression symptoms | ||||
| CES-D, mean (SD) | 13.4 (12.4) | 12.3 (12.0) | 11.8 (12.1) | 0.94 |
| CES-D ≥ 16, n (%) | 18 (37.5) | 14 (29.2) | 14 (29.2) | 0.63 |
| Lifestyle disruption | ||||
| ARS, mean (SD) | 22.3 (8.7) | 19.7 (8.1) | 19.4 (8.0) | 0.84 |
| Mean (SD) number of activities that were moderately or greatly restricted | 3.4 (3.4) | 2.9 (3.1) | 2.5 (3.2) | 0.86 |
ARS = Activity Restriction Scale; CES-D = Center for Epidemiologic Studies Depression scale.
Univariate Analyses
Significant univariate predictors of the CES-D score at each time point were as follows: at 2 months, patient gender (men), caregiver gender (women), and post-ICU functional dependency; at 6 months, patient gender (men), increased Charlson comorbidity score, caregiver gender (women), and residence in an institution; and at 12 months, patient gender (men), caregiver gender (women), tracheostomy, residence in an institution, patient education < 12th grade, and post-ICU functional dependency.
Significant univariate predictors of the ARS score at each time point were as follows: at 2 months, patient gender (men), patient education ≥ 12th grade, younger patient, and relationship (spouse); at 6 months, post-ICU functional dependency, older caregiver, and caregiver gender (women); and at 12 months, caregiver gender (women), patient gender (men), post-ICU functional dependency, longer duration of mechanical ventilation, longer ICU LOS, tracheostomy, and relationship (spouse).
Multivariable Analyses
In the multivariable regression model on CES-D, patient gender (men) was a significant predictor at 2 months, and patient gender (men) and tracheostomy were significant at 12 months. No variables were significant at 6 months (Table 3). In the multivariable regression model on ARS, patient gender (men) and patient education ≥ 12th grade were significant predictors at 2 months, and patient gender (men), tracheostomy, and post-ICU functional dependency were significant at 12 months. There were no significant variables at 6 months (Table 3).
Table 3.
—Results From Multivariable Regression Analyses on Caregiver CES-D and ARS Scores at 2, 6, and 12 Months After the Initiation of Mechanical Ventilation
| Independent Variables by Time Point | CES-D | ARS | ||
| Coefficient (SE) | P Value | Coefficient(SE) | P Value | |
| 2 mo | ||||
| Patient education ≥ 12th grade | … | … | 7.09 (2.50) | < .01 |
| Male patient | −1.66 (0.51) | < .01 | −7.29 (2.35) | < .01 |
| 6 mo | ||||
| No significant variables | … | … | … | … |
| 12 mo | ||||
| Tracheostomy | 1.26 (0.49) | .01 | 0.56 (0.23) | .02 |
| Male patient | −1.02 (0.50) | .05 | −0.73 (0.23) | < .01 |
| Functional dependencya | … | … | 0.73 (0.34) | .03 |
ADL = Activities of Daily Living; IADL = Instrumental ADL. See Table 2 for expansion of other abbreviations.
ADL > 0 or IADL > 0.
Functional Dependency Analyses
As a secondary aim of this study, multiple levels of functional dependency were tested in the univariate and multivariate regression analyses. Our findings indicate that the level of dependency was not an important factor in determining caregiver outcomes. In the multivariate analyses, functional dependency (defined as either ADL > 0 or IADL > 0; or ADL > 0 or IADL > 1) was only significantly associated with the ARS score at the 12-month time point. There was no significant association between functional dependency and caregiver CES-D score at any time point.
Tracheostomy Subgroup
Because tracheostomy was significantly associated with depression symptoms and lifestyle disruption, we compared the characteristics between patients with and without a tracheostomy. There were no significant differences identified between their respective mean ages (48.9 vs 54.4 years, P = .35), APACHE III scores (52.9 vs 46.8, P = .52), or number of Charlson comorbidities (1.9 vs 2.1, P = .81). Patients with a tracheostomy had a longer mean duration of mechanical ventilation (20.3 vs 7.6 days, P < .01) and longer hospital LOS (30.2 vs 20.2 days, P = .01).
Discussion
This study is the first to focus on time-varying predictors of post-ICU informal caregiver burden over a 1-year period. We identified variation in predictors of both lifestyle disruption and depression symptoms. Importantly, functional dependency was not a predictor of depression symptoms at any time point and did not predict lifestyle disruption at either 2 or 6 months after initiation of mechanical ventilation. These findings provide evidence for the need to broaden the focus of patient-specific interventions beyond the management of functional dependency.
Time-varying risk factors might be explained by either changes in a patient’s condition or changes in a caregiver’s appraisal of their role. From the caregiver perspective, changes in burden can be explained as either a result of adaptation20 or fatigue21 over time. Applying these models to our findings, it appears that patient-education level was a marker for caregiver adaptation, whereas the presence of a tracheostomy and functional dependency were associated with fatigue. Although these variables have not been previously reported as significant predictors of post-ICU caregiver burden, tracheostomy has been associated with burden in the context of chronic respiratory failure. Rossi Ferrario et al22 reported that tracheostomy predicted a medium degree of caregiver strain, which persisted for 14 months following the procedure. The reason for this association between tracheostomy and caregiver burden is not clear. In our study, tracheostomy was not a surrogate marker for severity of patient illness. Some studies have found that caregivers of tracheostomy patients receive inadequate information and therefore might benefit from more instruction in tracheostomy care.23 Our finding of an association between higher education level of the patient with greater caregiver lifestyle disruption is inconsistent with existing health-care literature demonstrating higher education level associated with lower risk for disability.24 The reason for this apparent discrepancy requires further investigation.
Other patient-specific risk factors have been investigated in cross-sectional studies of post-ICU caregiver outcomes. Cameron et al5 found that patient depression symptoms were a predictor of caregiver depression symptoms at a median of 2 years after hospital discharge. Notably, similar to our findings, functional status was not identified as a predictor of caregiver depression symptoms in other ICU survivor cohorts,5,6 and was not associated with psychosocial burden in the contexts of stroke, dementia, and Parkinson disease.25 Given our limited knowledge of patient-specific risk factors, future investigations of caregiver burden should consider other known manifestations of post-ICU patient impairment, such as cognitive problems,26 respiratory symptoms,27 posttraumatic stress symptoms,28 and depression.29 Other medical care issues particular to the post-ICU condition that could be considered in future studies include the management of newly diagnosed conditions (eg, renal failure, diabetes mellitus), polypharmacy, and the use of medical devices (eg, intravenous catheters).
Knowing the complexity of caregiver burden, it is not surprising that the development of interventions has proved to be difficult. A 2-month, multicomponent intervention for the caregivers of ICU survivors provided emotional support (discussion, reassurance), and instrumental support (care coordination, education). The intervention showed trends toward improved outcomes, but the trends were not statistically significant.30 One study of a multicomponent intervention of Alzheimer’s caregivers had medium to large effect sizes, achieved by tailoring the intervention to the patient- and caregiver-risk profiles.31 The interventions tested included skills training, telephone support, computer-aided communication, education, counseling, and support groups. Although such interventions seem reasonable as measures to relieve burden, in the traditional caregiver literature patient functional and behavioral disability only explain a small portion of the variance in morbidity associated with caregiving. Therefore burden might be better explained by less tangible factors, such as caregiver perception of patient suffering.32 Although the findings of our study will not directly lead to effective interventions, they do emphasize the importance of conducting new research of post-ICU informal caregiver outcomes to better identify the determinants of burden from both the patient and caregiver perspectives in a longitudinal fashion. Enrollment of more caregivers in outcome studies of ICU survivors could facilitate development of this knowledge base.
This study has several limitations. The secondary analysis of a small cohort from an observational, longitudinal study limits the statistical significance of our findings. In particular, type one error may result in false-positive findings, unmeasured variables such as caregiver experience may confound the results, and missing data in longitudinal analyses may introduce bias. However, this is the first study to address the variability of predictors of burden over a 1-year period in a cohort of patient caregiver dyads of survivors of critical illness. Confounding is an inherent problem in outcome studies of this type as it is not feasible to randomize subjects to the exposures of interest (ie, critical illness and caregiving).
It has been more than 10 years since this study completed enrollment. Although many changes have occurred in the practice of medicine, shorter patient hospitalizations have probably resulted in greater burden on informal caregivers. The cohort of patients in this caregiver study represents a small subgroup with relatively better outcomes, when compared with the entire QOL-MV cohort. The cohort of caregivers, therefore, cannot be considered representative of all post-ICU informal caregivers. Moreover, our findings in this post hoc analysis are meant to be hypothesis generating and should not be used for making clinical decisions. The generalizability of our findings of lifestyle disruption is limited because the Activity Restriction Scale has not been previously used to measure the outcomes of post-ICU informal caregivers. By contrast, the CES-D, a widely accepted caregiver outcome used in other caregiver disciplines, allows our findings to be compared with other studies. The CES-D score only indicates the degree to which depression symptoms are present; the diagnosis of depression requires further evaluation.
Conclusion
Informal caregiver burden is common following critical illness. The predictors of burden depend on complex, poorly defined interactions between patient and informal caregiver characteristics, which may vary over time. Interventions focusing on patient functional dependency may not improve caregiver outcomes. More research is needed to better understand the predictors of burden over time in order to develop intervention strategies.
Acknowledgments
Author contributions: Dr Van Pelt: contributed to developing the primary hypothesis, collating the screened data from the existing database, performing the initial and follow-up statistical analyses, and writing the manuscript.
Dr Schulz: contributed to developing the primary hypothesis, performing the follow-up statistical analyses, and writing the manuscript.
Dr Chelluri: contributed to developing the primary hypothesis, creating the original database from which these data were extracted, performing the follow-up statistical analyses, and writing the manuscript.
Dr Pinsky: contributed to developing the primary hypothesis, creating the original database from which these data were extracted, performing the initial and follow-up statistical analyses, and writing the manuscript.
Financial/nonfinancial disclosures: The authors have reported to CHEST that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Other contributions: This work was performed at the University of Pittsburgh School of Medicine.
Abbreviations
- ADL
activities of daily living
- APACHE
Acute Physiology and Chronic Health Evaluation
- ARS
Activity Restriction Scale
- CES-D
Center for Epidemiologic Studies Depression scale
- IADL
instrumental activities of daily living
- IQR
interquartile range
- LOS
length of stay
- MV
mechanical ventilation
- QOL-MV
Quality of Life After Prolonged Mechanical Ventilation
Footnotes
Funding/Support: This study was funded by the National Institute on Aging [Grants AG11970, AG024827, AG13305, AG015321, AG20677, AG19180], the National Institute on Nursing Research [Grant NR08272], the National Institute of Mental Health [Grant MH071944], the National Center on Minority Health and Health Disparities [Grant MD000207], the National Heart, Lung, and Blood Institute [Grants HL07820, HL076852, HL076858], and the National Science Foundation [Grant EEEC-0540865].
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal.org/site/misc/reprints.xhtml).
References
- 1.The Johnson and Johnson Caregiver Initiative. Family Caregiving in America: Facts at a Glance. http://www.strengthforcaring.com/util/press/facts/facts-at-a-glance.html . Accessed August 15, 2008.
- 2.Beach SR, Schulz R, Yee JL, Jackson S. Negative and positive health effects of caring for a disabled spouse: longitudinal findings from the caregiver health effects study. Psychol Aging. 2000;15(2):259–271. doi: 10.1037//0882-7974.15.2.259. [DOI] [PubMed] [Google Scholar]
- 3.Dennis M, O’Rourke S, Lewis S, Sharpe M, Warlow C. A quantitative study of the emotional outcome of people caring for stroke survivors. Stroke. 1998;29(9):1867–1872. doi: 10.1161/01.str.29.9.1867. [DOI] [PubMed] [Google Scholar]
- 4.Schulz R, Beach SR. Caregiving as a risk factor for mortality: the Caregiver Health Effects Study. JAMA. 1999;282(23):2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 5.Cameron JI, Herridge MS, Tansey CM, McAndrews MP, Cheung AM. Well-being in informal caregivers of survivors of acute respiratory distress syndrome. Crit Care Med. 2006;34(1):81–86. doi: 10.1097/01.ccm.0000190428.71765.31. [DOI] [PubMed] [Google Scholar]
- 6.Douglas SL, Daly BJ. Caregivers of long-term ventilator patients: physical and psychological outcomes. Chest. 2003;123(4):1073–1081. doi: 10.1378/chest.123.4.1073. [DOI] [PubMed] [Google Scholar]
- 7.Im K, Belle SH, Schulz R, Mendelsohn AB, Chelluri L QOL-MV Investigators. Prevalence and outcomes of caregiving after prolonged ( ≥ 48 hours) mechanical ventilation in the ICU. Chest. 2004;125(2):597–606. doi: 10.1378/chest.125.2.597. [DOI] [PubMed] [Google Scholar]
- 8.Azoulay E, Pochard F, Kentish-Barnes N, et al. FAMIREA Study Group. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171(9):987–994. doi: 10.1164/rccm.200409-1295OC. [DOI] [PubMed] [Google Scholar]
- 9.Wu JH, Haan MN, Liang J, Ghosh D, Gonzalez HM, Herman WH. Diabetes as a predictor of change in functional status among older Mexican Americans: a population-based cohort study. Diabetes Care. 2003;26(2):314–319. doi: 10.2337/diacare.26.2.314. [DOI] [PubMed] [Google Scholar]
- 10.Covinsky KE, Goldman L, Cook EF, et al. The impact of serious illness on patients’ families. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risk of Treatment. JAMA. 1994;272(23):1839–1844. doi: 10.1001/jama.272.23.1839. [DOI] [PubMed] [Google Scholar]
- 11.Van Pelt DC, Milbrandt EB, Qin L, et al. Informal caregiver burden among survivors of prolonged mechanical ventilation. Am J Respir Crit Care Med. 2007;175(2):167–173. doi: 10.1164/rccm.200604-493OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Quality of Life After Mechanized Ventilation in the Elderly Study Investigators. 2-month mortality and functional status of critically ill adult patients receiving prolonged mechanical ventilation. Chest. 2002;121(2):549–558. doi: 10.1378/chest.121.2.549. [DOI] [PubMed] [Google Scholar]
- 13.Knaus WA, Wagner DP, Draper EA, et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100(6):1619–1636. doi: 10.1378/chest.100.6.1619. [DOI] [PubMed] [Google Scholar]
- 14.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 15.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged, the index of adl: a standardized measure of biological and psychosocial function. JAMA. 1963;185(12):914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 16.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9(3):179–186. [PubMed] [Google Scholar]
- 17.Radloff L. The Center for Epidemiological Studies-depression scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- 18.McDowell I, Newell C, editors. Measuring Health: A Guide to Rating Scales and Questionnaires. 2nd ed. New York: Oxford University Press; 1996. pp. 254–259. [Google Scholar]
- 19.Williamson GM, Schulz R. Pain, activity restriction, and symptoms of depression among community-residing elderly adults. J Gerontol. 1992;47(6):367–372. doi: 10.1093/geronj/47.6.p367. [DOI] [PubMed] [Google Scholar]
- 20.Whitlatch CJ, Feinberg LF, Sebesta DS. Depression and health in family caregivers: adaptation over time. J Aging Health. 1997;9(2):222–243. doi: 10.1177/089826439700900205. [DOI] [PubMed] [Google Scholar]
- 21.Townsend A, Noelker L, Deimling G, Bass D. Longitudinal impact of interhousehold caregiving on adult children’s mental health. Psychol Aging. 1989;4(4):393–401. doi: 10.1037//0882-7974.4.4.393. [DOI] [PubMed] [Google Scholar]
- 22.Rossi Ferrario S, Zotti AM, Zaccaria S, Donner CF. Caregiver strain associated with tracheostomy in chronic respiratory failure. Chest. 2001;119(5):1498–1502. doi: 10.1378/chest.119.5.1498. [DOI] [PubMed] [Google Scholar]
- 23.Krouse HJ, Rudy SF, Vallerand AH, et al. Impact of tracheostomy or laryngectomy on spousal and caregiver relationships. ORL Head Neck Nurs. 2004;22(1):10–25. [PubMed] [Google Scholar]
- 24.Schoeni RF, Martin LG, Andreski PM, Freedman VA. Persistent and growing socioeconomic disparities in disability among the elderly: 1982-2002. Am J Public Health. 2005;95(11):2065–2070. doi: 10.2105/AJPH.2004.048744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thommessen B, Aarsland D, Braekhus A, Oksengaard AR, Engedal K, Laake K. The psychosocial burden on spouses of the elderly with stroke, dementia and Parkinson’s disease. Int J Geriatr Psychiatry. 2002;17(1):78–84. doi: 10.1002/gps.524. [DOI] [PubMed] [Google Scholar]
- 26.Hopkins RO, Weaver LK, Collingridge D, Parkinson RB, Chan KJ, Orme JF., Jr Two-year cognitive, emotional, and quality-of-life outcomes in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2005;171(4):340–347. doi: 10.1164/rccm.200406-763OC. [DOI] [PubMed] [Google Scholar]
- 27.Weinert CR, Gross CR, Kangas JR, Bury CL, Marinelli WA. Health-related quality of life after acute lung injury. Am J Respir Crit Care Med. 1997;156(4, pt 1):1120–1128. doi: 10.1164/ajrccm.156.4.9611047. [DOI] [PubMed] [Google Scholar]
- 28.Davydow DS, Gifford JM, Desai SV, et al. Posttraumatic stress disorder in general intensive care unit survivors: a systematic review. Gen Hosp Psychiatry. 2008;30(5):421–434. doi: 10.1016/j.genhosppsych.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Weinert C. Epidemiology and treatment of psychiatric conditions that develop after critical illness. Curr Opin Crit Care. 2005;11(4):376–380. doi: 10.1097/01.ccx.0000168529.23078.64. [DOI] [PubMed] [Google Scholar]
- 30.Douglas SL, Daly BJ, Kelley CG, O’Toole E, Montenegro H. Impact of a disease management program upon caregivers of chronically critically ill patients. Chest. 2005;128(6):3925–3936. doi: 10.1378/chest.128.6.3925. [DOI] [PubMed] [Google Scholar]
- 31.Belle SH, Burgio L, Burns R, et al. Resources for Enhancing Alzheimer’s Caregiver Health (REACH) II Investigators. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: a randomized, controlled trial. Ann Intern Med. 2006;145(10):727–738. doi: 10.7326/0003-4819-145-10-200611210-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schulz R, Martire LM, Klinger JN. Evidence-based caregiver interventions in geriatric psychiatry. Psychiatr Clin North Am. 2005;28(4):1007–1038. doi: 10.1016/j.psc.2005.09.003. [DOI] [PubMed] [Google Scholar]