Abstract
Objective
The purpose of this study was to compare clinical and radiological outcomes of percutaneous endoscopic lumbar discectomy (PELD) and open lumbar microdiscectomy (OLM) for recurrent disc herniation.
Methods
Fifty-four patients, who underwent surgery, either PELD (25 patients) or repeated OLM (29 patients), due to recurrent disc herniation at L4-5 level, were divided into two groups according to the surgical methods. Excluded were patients with sequestrated disc, calcified disc, severe neurological deficit, or instability. Clinical outcomes were assessed using Visual Analogue Scale (VAS) score and Oswestry Disability Index (ODI). Radiological variables were assessed using plain radiography and/or magnetic resonance imaging.
Results
Mean operating time and hospital stay were significantly shorter in PELD group (45.8 minutes and 0.9 day, respectively) than OLM group (73.8 minutes and 3.8 days, respectively) (p < 0.001). Complications occurred in 4% in PELD group and 10.3% in OLM group in the perioperative period. At a mean follow-up duration of 34.2 months, the mean improvements of back pain, leg pain, and functional improvement were 4.0, 5.5, and 40.9% for PELD group and 2.3, 5.1, and 45.0% for OLM group, respectively. Second recurrence occurred in 4% after PELD and 10.3% after OLM. Disc height did not change after PELD, but significantly decreased after OLM (p = 0.0001). Neither sagittal rotation angle nor volume of multifidus muscle changed significantly in both groups.
Conclusion
Both PELD and repeated OLM showed favorable outcomes for recurrent disc herniation, but PELD had advantages in terms of shorter operating time, hospital stay, and disc height preservation.
Keywords: Reherniation, Discectomy, Lumbar spine
INTRODUCTION
Recurrent disc herniation, considered as the major cause of surgical failure after open lumbar microdiscectomy (OLM), has been reported in 5-18% of patients after the procedure2,7,15,32-34). Repeated OLM is the most commonly recommended surgical option for recurrent lumbar disc herniation, when not accompanied by definite radiological instability8,10,33,34). Though repeated OLM shows comparable results to those of primary OLM, major concerns are approach-related complications due to scar tissue and segmental instability by further damages to vertebral motion segment including facet joint6,7,27,35). Considering minimally invasive spinal surgery, microendoscopic discectomy seems to face similar problems with repeated OLM for recurrent disc herniation, since via posterior approach, surgeons are always interfered by scar tissue to reach recurrent disc fragment despite the advantage of operating on virgin paraspinal muscle14,17,30).
Given that posterolateral transforaminal approach through unscarred tissue can prevent nerve injury and can prevent further damages to the posterior spinal and paraspinal structure1), percutaneous endoscopic lumbar discectomy (PELD) has advantages especially for recurrent disc herniation. Though PELD showed favorable outcomes for lumbar disc herniation including recurrent disc herniation1,12,13,18-22,36), studies comparing surgical outcomes of PELD with repeated OLM for recurrent disc herniation have been rare. In the present study, we compared clinical and radiological outcomes of PELD and repeated OLM for recurrent disc herniation.
MATERIALS AND METHODS
Patient population
Fifty-four patients, who underwent surgical discectomy between December 2004 and May 2006, due to recurrent disc herniation after primary OLM at L4-5 level, were retrospectively selected. There were 38 men and 16 women and mean age of the patients was 45 years (range 26-67 years). The mean follow-up period was 34.2 months (range 25-41 months). Inclusion criteria were as follows: 1) a previous episode of OLM at L4-5 level resulting from lumbar disc herniation, 2) recurrent radicular pain after a pain-free interval longer than 4 weeks, 3) recurrent disc herniation at the same level and the same side, verified by radiological studies, [i.e., the presence of abnormal epidural tissue that did not enhance after contrast injection, as well as epidural fibrosis showing enhancement with gadolinium on T1-weighted magnetic resonance imaging (MRI)], and 4) failure of extensive conservative treatment for more than 6 weeks4). Excluded were patients with sequestrated disc, calcified disc, severe neurological deficit, and/or instability. The patients were divided into two groups according to the surgical methods. Group I included patients who underwent PELD for recurrent disc herniation and Group II included patients who underwent repeated OLM for recurrent disc herniation. Seven spine surgeons were involved in the present study and the selection of surgical method was mainly up to each surgeon's preference and familiarity. Four of seven surgeons performed PELD for recurrent disc herniation and all the four surgeons had a clinical experience of PELD more than 50 cases before the beginning of the present study. Three surgeons performed repeated OLM for recurrent disc herniation.
Clinical evaluation
Before and after surgery, pain was measured by the 10-point Visual Analogue Scale (VAS) scoring (0-10) and function was assessed by the Oswestry Disability Index (ODI) in percent (0-100%)9). Complications were categorized using the classification scheme described by Carreon et al.3), dividing them into major and minor complications. Major complications were considered to have caused a negative effect on a patient's recovery, whereas minor complications were not considered to have affected recovery significantly. Pre- and postoperative data were assessed using clinical charts and operative reports. All patients visited the outpatient department in June 2008 and a trained nurse collected follow-up clinical data.
Radiological evaluation
The follow-up plain radiographs of standing lateral and flexion-extension lateral view were performed in all 54 patients at 1, 6, and 12 months after surgery to assess spinal stability. Plain radiographs and MRI were performed in 51 patients (23 in Group I and 28 in Group II) in June 2008 to assess disc height, sagittal rotation angle (SRA), and volume of multifidus muscle at the diseased side.
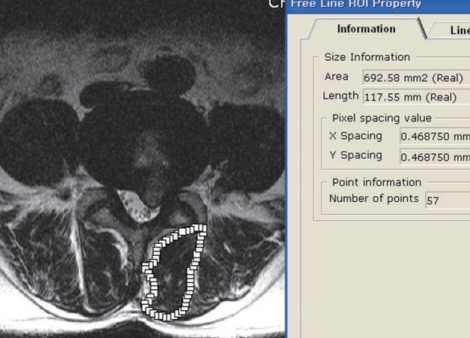
Radiographic criteria for instability were as follows; 1) sagittal plane displacement greater than 4.5 mm or 15 percent of the anteroposterior diameter of the vertebral body on standing lateral radiography, 2) relative sagittal angulation greater than 22 degrees on standing lateral radiography, 3) sagittal plane translation greater than 4.5 mm or 15 percent of the anteroposterior diameter of the vertebral body on dynamic radiography, or 4) sagittal plane rotation greater than 20 degrees on dynamic radiography11). The disc height was measured on the plain standing lateral radiography according to modified Mochida's method21,24). Disc height was calculated by the following equation : (disc height/vertebral height) × 100. Sagittal rotation angle was measured on the flexion-extension lateral radiographs. Volume of multifidus muscle at the diseased side was measured on T2-weighted axial MRI. The MRI scans were performed using Magnetom Symphony Ultragradient 1.5 tesla MRI system (Siemens, Erlangen, Germany) with a slice thickness of 4 mm. Axial T2-weighted images were obtained under the following scan setting; repetition time (TR) 3,700 msec and echo time (TE) 120 msec. Axial scans were aligned parallel to the vertebral end-plate. The MRI scan measurements were taken using a software PiView system (Infinitt Co., Ltd., Seoul, Korea). After enlarging the axial slice of the lumbar spine, the cursor identified the area of the multifidus muscle, which the software calculated automatically (Fig. 1).
Fig. 1.
The volume of multifidus muscle was measured on axial T2-weighted magnetic resonance imaging scan using a software system. After enlarging the axial slice of the lumbar spine, the cursor identified the area of the multifidus muscle, which the software calculated automatically.
Statistical analysis
Statistical analyses were performed using SPSS statistic software (Version 14.0K). Paired sample t-test and Wilcoxon signed rank test were used to compare the differences of pre- and postoperative parameters on clinical and radiological outcomes in each group. Then independent t-test, Mann-Whitney U test, Chi-square test, and Fisher's exact test were used to compare the differences of clinical and radiological outcomes between the two groups. A p value of less than 0.05 was considered significant.
Surgical techniques
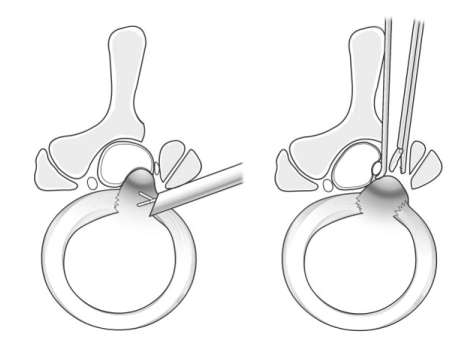
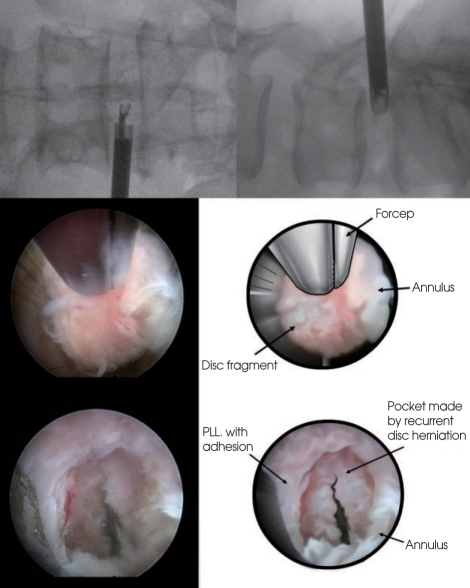
In both groups, all operations followed a standard pattern suggested by the senior author (Fig. 2). In PELD group, the procedure was performed under local anesthesia in the prone position on a radiolucent table in all patients. Before beginning of the treatment, patients were informed with all steps of the procedure. Patients communicated with the surgeon during the entire procedure. The skin entry point was usually about 10-12 cm from the midline. After infiltration of the entry point with local anesthetics, an 18-gauge spinal needle was introduced under the guidance of a fluoroscopic image. The final target point of the spinal needle was the medial pedicular line on the anteroposterior image and the posterior vertebral line on the lateral image. Then an epidurogram was performed using contrast media to confirm the location of the exiting root and the traversing root. After insertion of the spinal needle into the disc, the nucleus pulposus was stained blue with 1 mL of indigo carmine. The next steps were as follows : 1) a guide wire was inserted through the spinal needle, 2) the spinal needle was removed, 3) a small skin incision was made at the entry site, 4) a tapered cannulated obturator was inserted along the guide wire, 5) after touching the annulus, the obturator was inserted into the disc with hammering, and 6) finally, a bevel-ended, oval-shaped working cannula was inserted into the disc along the obturator and then the obturator was removed. Then an endoscope was inserted through the cannula. The blue-stained disc was removed using small forceps and a side firing Holmium yttrium-aluminum-garnet (Ho : YAG) laser using the 'in and out' techniqueworking from the central portion to the lateral portion of the disc space on the anteroposterior image. Targeted fragmentectomy was performed in all cases. After herniated fragment was all removed, the endoscope was removed, and a sterile dressing was applied with a 1-point suture (Fig. 3)18,19).
Fig. 2.
Schematic drawing showing percutaneous endoscopic lumbar discectomy (left) and repeated open lumbar microdiscectomy (right) for recurrent disc herniation.
Fig. 3.
Upper : Intraoperative fluoroscopic images taken after insertion of endoscopic cannula. Middle : Recurrent disc herniation was removed with forceps under endoscopic view. Lower : Endoscopic view taken after successful removal of recurrent disc herniation.
In OLM group, the procedure was performed under general anesthesia in the prone position on a radiolucent Wilson frame and Jackson table in all patients. After a 2-3 cm skin incision was made, paravertebral muscles were dissected. The operating field was exposed using Casper speculum (Aesculap). Under microscopic view, scar was removed from the lamina with curettes to clearly identify the previous laminotomy edges, with great care not to violate the dura mater. In all cases, a high-speed drill was used to thin the medial facet lateral to the previous laminotomy, and then a few millimeters of new bone were removed. After clear delineation of nerve root, discectomy was performed with careful retraction of nerve root. After thorough decompression of nerve root was achieved, closure was performed in a conventional way34).
RESULTS
Group I (PELD) included 25 patients and Group II (repeated OLM) included 29 patients. There was no significant intergroup difference in sex ratio (male : female, 16 : 9 in Group I and 22 : 7 in Group II, p = 0.38), mean age at the time of operation (42.0 ± 11.4 in Group I and 47.7 ± 12.2 in Group II, p = 0.08), and mean follow-up periods (34.0 ± 4.4 in Group I and 34.3 ± 4.6 in Group II, p = 0.76).
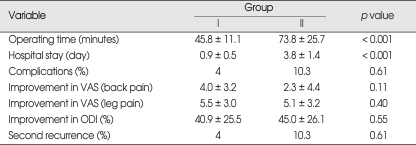
Clinical outcomes
Mean operating time was significantly shorter in Group I (45.8 ± 11.1 minutes) compared with Group II (73.8 ± 25.7 minutes) (p < 0.001). Mean hospital stay was significantly shorter in Group I (0.9 ± 0.5 days) compared with Group II (3.8 ± 1.4 days) (p < 0.001). Complications occurred in one patient (4%) in Group I and three patients (10.3%) in Group II during the perioperative period (p = 0.61). One patient in Group I complaint of persistent leg pain after PELD due to residual disc fragment and underwent subsequent OLM one week thereafter. Dural tear occurred in two patients in Group II, which was successfully managed with primary suture. Major complication occurred in one patient in Group II; the patient complaint of voiding difficulty and dysesthesia on perineal area immediately after surgery, which were persistent at the final follow-up.
In Group I, the mean VAS score for back pain was 7.0 ± 2.8 before surgery and improved to 2.9 ± 2.4 after surgery (p < 0.001). The mean VAS score for leg pain was 8.4 ± 1.7 before surgery and improved to 2.9 ± 2.5 after surgery (p < 0.001). The mean ODI score was 61.6 ± 22.1% before surgery and improved to 20.7 ± 15.9% after surgery (p < 0.001). In Group II, the mean VAS score for back pain was 5.4 ± 3.7 before surgery and improved to 3.1 ± 2.5 after surgery (p = 0.009). The mean VAS score for leg pain was 8.6 ± 1.7 before surgery and improved to 3.5 ± 3.1 after surgery (p < 0.001). The mean ODI score was 63.1 ± 22.3% before surgery and improved to 18.2 ± 15.4% after surgery (p < 0.001). Mean improvements of VAS score for back pain, leg pain, and ODI scores (i.e., the differences in scores between preoperative and last follow-up) were 4.0 ± 3.2, 5.5 ± 3.0, 40.9 ± 25.5% respectively in Group I, and 2.3 ± 4.4, 5.1 ± 3.2, 45.0 ± 26.1% respectively in Group II. There was no significant intergroup difference in improvement of VAS and ODI scores (Table 1). Second recurrence occurred in one patient (4%) in Group I and three patients (10.3%) in Group II (p = 0.61). One patient in each group underwent instrumented mini-open TLIF for second recurrence. Two other patients in Group II with second recurrence were managed with conservative treatment.
Table 1.
Summary of clinical outcomes who underwent PELD (Group I) and OLM (Group II)*
*Mean values are presented ± standard deviations. ODI : Oswestry Disability Index, OLM : open lumbar microdiscectomy, PELD : percutaneous endoscopic lumbar discectomy, VAS : visual analogue scale
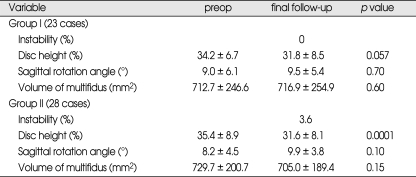
Radiological outcomes
At the last follow-up, no patient in Group I showed instability on plain standing and dynamic plain radiograph. One patient (3.6%) in Group II showed newly developed instability (sagittal plane translation 6 mm) at the index level on dynamic plain radiographs. In Group I, mean disc height was 34.2 ± 6.7% before surgery and decreased to 31.8 ± 8.5% after surgery, which was not statistically significant (p = 0.057). The mean SRA was 9.0 ± 6.1° before surgery and changed to 9.5 ± 5.4° after surgery (p = 0.70). The mean volume of multifidus muscle at diseased side was 712.7 ± 246.6 mm2 before surgery and 716.9 ± 254.9 mm2 after surgery (p = 0.60). In Group II, the mean disc height was 35.4 ± 8.9% before surgery and significantly decreased to 31.6 ± 8.1% after surgery (p = 0.0001) (Fig. 4). The mean SRA was 8.2 ± 4.5° before surgery and changed to 9.9 ± 3.8° after surgery (p = 0.10). The mean volume of multifidus muscle at diseased side was 729.7 ± 200.7 mm2 before surgery and 705.0 ± 189.4 mm2 after surgery (p = 0.15) (Table 2). Therefore, among the radiological variables, disc height at index level showed significant intergroup difference. The intraobserver reliability concerning radiological measurement was 0.95.
Fig. 4.
A : A plain radiograph taken 31 months after repeated open lumbar microdiscectomy for recurrent disc herniation at L4-5 level showing decrease of disc height at L4-5 level (left : preoperation, right : postoperation). B : A plain radiograph taken 34 months after percutaneous endoscopic lumbar discectomy for recurrent disc herniation at L4-5 level showing preserved disc height at L4-5 level (left : preoperation, right : postoperation).
Table 2.
Summary of radiological outcomes who underwent PELD (Group I) and OLM (Group II)*
*Mean values are presented ± standard deviations. OLM : open lumbar microdiscectomy, PELD : percutaneous endoscopic lumbar discectomy
DISCUSSION
As a form of minimally invasive surgery, PELD has several advantages over conventional OLM; it is usually performed under local anesthesia, normal paraspinal structures are preserved during the procedure, and the postoperative pain is quite minimal which usually enables early discharge18). For recurrent disc herniation after primary OLM, it would be theoretically an advantage not going through the old scar tissue and not requiring general anesthesia13). Ahn et al.1) reported a retrospective study of 43 consecutive patients who underwent PELD for recurrent disc herniation. At a mean follow-up duration of 31 months, the mean VAS score significantly decreased and 81.4% of the patients showed excellent or good outcomes based on Macnab criteria. Hoogland et al.13) performed a prospective cohort evaluation of 262 consecutive patients who underwent PELD for recurrent disc herniation. At 2-year follow-up, both back pain and leg pain significantly improved, and 85.71% of the patients rated the result of surgery as excellent or good. In the present study, clinical outcomes of PELD were compared with those of repeated OLM. PELD yielded comparable outcomes to repeated OLM in terms of improvement in back pain, leg pain, and functional status. Repeated muscle dissection and further removal of posterior structures, such as lamina, and medial facet joint, during repeated OLM have been suggested to increase the risk of postoperative back pain1,27,35). The prevalence of facet joint mediated chronic low back pain was reported even 32% in postsurgical group who underwent lumbar laminectomy23). Theoretically, PELD was supposed to be superior in terms of postoperative back pain, because normal paraspinal structures are preserved during the procedure. However, in the present study, there was no significant difference in improvement of back pain after surgery between the two groups. To determine the inter-group difference between PELD and OLM on postoperative back pain, further long-term follow-up studies are mandatory. As with PELD for primary lumbar disc herniation21), PELD for recurrent disc herniation also had advantages over repeated OLM in that it was performed under local anesthesia in all patients and required significantly shorter operating time and hospital stay.
The major concern for repeated OLM for recurrent disc herniation was approach related complications. Scar tissue usually makes repeated OLM more difficult, and increases the risk of dural tear and/or nerve root injury1,6,7,27,35). The incidence of dural tear during repeated OLM was reported up to 20% of the patients5,25). Dural tear during lumbar disc surgery was suggested being associated with long-term clinical sequelae and poorer clinical outcomes29). Considering PELD for recurrent disc herniation, Ahn et al.1) reported no case of dural tear of 43 consecutive patients and Hoogland et al.13) also reported no definite dural leakage after surgery of 262 consecutive patients. In the present study, dural tear occurred in two patients (6.9%) in repeated OLM group, whereas there was no dural tear in PELD group. Nerve root injury during repeated OLM sometimes results in long-term clinical sequelae and poor clinical outcome. According to the report by Choi et al.4), permanent foot drop developed in one (2.9%) of 35 patients after repeated OLM. Considering PELD for recurrent disc herniation, Ahn et al.1) reported one patient (2.3%) with transient dysesthesia and Hoogland et al.13) reported three patients (1.1%) with nerve root irritation. However, there was no patient with permanent nerve root injury in both series. In the present study, persistent voiding disturbance along with dysesthesia developed after surgery in one patient (3.4%) in repeated OLM group, whereas there was no case of nerve root injury in PELD group.
Though there have been numerous reports on recurrent disc herniation after OLM7,8,10,32-34), few authors stated concerns about the second recurrence after repeated OLM for recurrent disc herniation. Considering PELD, Hoogland et al.13) reported 11 cases (4.62%) of second recurrence after PELD for recurrent disc herniation. In the present study, second recurrence rate was 10.3% in repeated OLM group and 4% in PELD group and the difference was statistically not significant. In those patients, spinal arthrodesis (instrumented mini-open TLIF) was a preferred surgical treatment when not responding to conservative treatment.
In terms of postoperative spinal stability, discectomy via transforaminal route has advantages over that via posterior route, since via transforaminal appraoch, discectomy can be performed while preserving paravertebral and posterior spinal structures such as, lamina, facet, ligaments and muscles, as mentioned above1). According to the comparative study using cadavers by Osman et al.26), after transforaminal decompression, there was no flexibility change, and minimal anatomic damage to the spine was noted. However, significant increase in extension and axial rotation flexibility were noted after the posterior decompression. In the present study, one patient (3.4%) showed newly developed instability (sagittal plane translation 6 mm on dynamic radiography) after repeated OLM, whereas no patients showed instability after PELD at the final follow-up. However, the mean SRA did not change significantly after surgery in both groups. In the present study, the mean disc height did not change significantly after PELD, whereas, the mean disc height significantly decreased after repeated OLM. These findings were nearly similar with those in primary lumbar disc herniation. The mean degree of disc space and foraminal narrowing was significantly higher after OLM than after PELD21). Larger amount of disc removal and violation of posterior spinal structures during OLM were suggested as the causes of these differences, which was usually the case with recurrent disc herniations. Posterior lumbar surgical procedures have high chance of damage to dorsal rami, which frequently results in denervation atrophy of multifidus muscle28,31). Kahanovitz et al.16) performed long-term strength assessment of postoperative discectomy patients and reported that every strength parameter tested except male isokinetic flexion strength showed at least a 30% decrease at 1-year after surgery, when compared with normal values. They recommended the specific isometric, isokinetic, and endurance rehabilitation programs for the postoperative discectomy patient. There-fore, the atrophy and weakness of paraspinal muscles were suggested as one of the possible predisposing factors for further instability and dysfunction4). PELD was considered to have an advantage for recurrent disc herniation in terms of paraspinal muscle atrophy, since repeated OLM had a higher change of re-damaging paraspinal muscles and innervating dorsal rami. However, there was no significant difference in the mean changes of multifidus muscle volume after surgery between the two groups. It was supposed that the influences of second surgeries on the volume of paraspi-nal muscles were not significant, regardless of type of surgery, because denervation atrophy of paraspinal muscles had already significantly progressed after first surgery in both groups.
The retrospective study design and relatively small number of patients should be considered when interpreting the results of the present study. Further randomized controlled trials are needed.
CONCLUSION
Both PELD and repeated OLM showed favorable clinical and radiological outcomes for recurrent disc herniation. Compared with repeated OLM, PELD had several advantages; 1) the procedure was performed under local anesthesia, 2) the operating time and hospital stay were significantly shorter, 3) there were no approach-related complications, such as dural tear and/or permanent nerve root injury, and 4) the disc height was preserved after the procedure.
Acknowledgements
This study was supported by a grant from the Wooridul Spine Foundation.
References
- 1.Ahn Y, Lee SH, Park WM, Lee HY, Shin SW, Kang HY. Percutaneous endoscopic lumbar discectomy for recurrent disc herniation : surgical technique, outcome, and prognostic factors of 43 consecutive cases. Spine. 2004;29:E326–E332. doi: 10.1097/01.brs.0000134591.32462.98. [DOI] [PubMed] [Google Scholar]
- 2.Carragee EJ, Spinnickie AO, Alamin TF, Paragioudakis S. A prospective controlled study of limited versus subtotal posterior discectomy : short-term outcomes in patients with herniated lumbar intervertebral discs and large posterior annular defect. Spine. 2006;31:653–657. doi: 10.1097/01.brs.0000203714.76250.68. [DOI] [PubMed] [Google Scholar]
- 3.Carreon LY, Puno RM, Dimar JR, 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003;85:2089–2092. doi: 10.2106/00004623-200311000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Choi G, Raiturker PP, Kim MJ, Chung DJ, Chae YS, Lee SH. The effect of early isolated lumbar extension exercise program for patients with herniated disc undergoing lumbar discectomy. Neurosurgery. 2005;57:764–772. doi: 10.1093/neurosurgery/57.4.764. discussion 764-772. [DOI] [PubMed] [Google Scholar]
- 5.Choi KB, Lee DY, Lee SH. Contralateral reherniation after open lumbar microdiscectomy; a comparison with ipsilateral reherniation. J Korean Neurosurg Soc. 2008;44:320–326. doi: 10.3340/jkns.2008.44.5.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cinotti G, Gumina S, Giannicola G, Postacchini F. Contralateral recurrent lumbar disc herniation : results of discectomy compared with those in primary herniation. Spine. 1999;24:800–806. doi: 10.1097/00007632-199904150-00012. [DOI] [PubMed] [Google Scholar]
- 7.Cinotti G, Roysam GS, Eisenstein SM, Postacchini F. Ipsilateral recurrent lumbar disc herniation. A prospective, controlled study. J Bone Joint Surg Br. 1998;80:825–832. doi: 10.1302/0301-620x.80b5.8540. [DOI] [PubMed] [Google Scholar]
- 8.Dai LY, Zhou Q, Yao WF, Shen L. Recurrent lumbar disc herniation after discectomy : outcome of repeated discectomy. Surg Neurol. 2005;64:226–231. doi: 10.1016/j.surneu.2004.11.003. discussion 231. [DOI] [PubMed] [Google Scholar]
- 9.Fairbank JC, Couper J, Davies JB, O'Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 10.Fu TS, Lai PL, Tsai TT, Niu CC, Chen LH, Chen WJ. Long-term results of disc excision for recurrent lumbar disc herniation with or without posterolateral fusion. Spine. 2005;30:2830–2834. doi: 10.1097/01.brs.0000190393.15369.94. [DOI] [PubMed] [Google Scholar]
- 11.Herkowitz HN, Garfin SR, Balderston RA, Eismont FJ, Bell GR, Wiesel SW. Rothman-Simeone The Spine. ed 4. Philadelphia: W.B. Saunders Company; 1999. pp. 1089–1093. [Google Scholar]
- 12.Hoogland T, Schubert M, Miklitz B, Ramirez A. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain : a prospective randomized study in 280 consecutive cases. Spine. 2006;24:E890–E897. doi: 10.1097/01.brs.0000245955.22358.3a. [DOI] [PubMed] [Google Scholar]
- 13.Hoogland T, van den Brekel-Dijkstra K, Schubert M, Miklitz B. Endoscopic transforaminal discectomy for recurrent lumbar disc herniation : a prospective, cohort evaluation of 262 consecutive cases. Spine. 2008;33:973–978. doi: 10.1097/BRS.0b013e31816c8ade. [DOI] [PubMed] [Google Scholar]
- 14.Isaacs RE, Podichetty V, Fessler RG. Microendoscopic discectomy for recurrent disc herniation. Neurosurg Focus. 2003;15:E11. doi: 10.3171/foc.2003.15.3.11. [DOI] [PubMed] [Google Scholar]
- 15.Javedan S, Sonntag VK. Lumbar disc herniation : microsurgical approach. Neurosurgery. 2003;52:160–162. doi: 10.1097/00006123-200301000-00021. discussion 162-164. [DOI] [PubMed] [Google Scholar]
- 16.Kahanovitz N, Viola K, Gallagher M. Long-term strength assessment of postoperative diskectomy patients. Spine. 1989;14:402–403. doi: 10.1097/00007632-198904000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Le H, Sandhu FA, Fessler RG. Clinical outcomes after minimal-access surgery for recurrent lumbar disc herniation. Neurosurg Focus. 2003;15:E12. doi: 10.3171/foc.2003.15.3.12. [DOI] [PubMed] [Google Scholar]
- 18.Lee DY, Ahn Y, Lee SH. Percutaneous endoscopic lumbar discectomy for adolescent lumbar disc herniation : surgical outcomes in 46 consecutive patients. Mt Sinai J Med. 2006;73:864–870. [PubMed] [Google Scholar]
- 19.Lee DY, Lee SH. Learning curve for percutaneous endoscopic lumbar discectomy. Neurol Med Chir (Tokyo) 2008;48:383–388. doi: 10.2176/nmc.48.383. discussion 388-389. [DOI] [PubMed] [Google Scholar]
- 20.Lee S, Kim SK, Lee SH, Kim WJ, Choi WC, Choi G, et al. Percutaneous endoscopic lumbar discectomy for migrated disc herniation : classification of disc migration and surgical approaches. Eur Spine J. 2007;16:431–437. doi: 10.1007/s00586-006-0219-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee SH, Chung SE, Ahn Y, Kim TH, Park JY, Shin SW. Comparative radiologic evaluation of percutaneous endoscopic lumbar discectomy and open microdiscectomy : a matched cohort analysis. Mt Sinai J Med. 2006;73:795–801. [PubMed] [Google Scholar]
- 22.Lee SH, Kang BU, Ahn Y, Choi G, Choi YG, Ahn KU, et al. Operative failure of percutaneous endoscopic lumbar discectomy : a radiological analysis of 55 cases. Spine. 2006;31:E285–E290. [PubMed] [Google Scholar]
- 23.Manchikanti L, Pampati V, Baha AG, Fellows B, Damron KS, Barnhill RC. Contribution of facet joints to chronic low back pain in postlumbar laminectomy syndrome : a controlled comparative prevalence evaluation. Pain Physician. 2001;4:175–180. [PubMed] [Google Scholar]
- 24.Mochida J, Nishimura K, Nomura T. Appropriate procedure of posterior herniotomy and percutaneous nucleotomy in lumbar disc herniation. Rinsho Seikei Geka. 1994;29:423–430. [Google Scholar]
- 25.Morgan-Hough CVJ, Jones PW, Eisenstein SM. Primary and revision lumbar discectomy. J Bone Joint Surg Br. 2003;85:871–874. [PubMed] [Google Scholar]
- 26.Osman SG, Nibu K, Panjabi MM, Marsolais EB, Chaudhary R. Transforaminal and posterior decompression of the lumbar spine. A comparative study of stability and intervertebral foraminal area. Spine. 1997;22:1690–1695. doi: 10.1097/00007632-199708010-00002. [DOI] [PubMed] [Google Scholar]
- 27.Ozgen S, Naderi S, Ozek MM, Pamir MN. Findings and outcome of revision lumbar disc surgery. J Spinal Disord. 1999;12:287–292. [PubMed] [Google Scholar]
- 28.Panjabi MM. Clinical spinal instability and low back pain. J Electromyogr Kinesiol. 2003;13:371–379. doi: 10.1016/s1050-6411(03)00044-0. [DOI] [PubMed] [Google Scholar]
- 29.Saxler G, Kramer J, Barden B, Kurt A, Pfortner J, Bernsmann K. The long-term clinical sequelae of incidental durotomy in lumbar disc surgery. Spine. 2005;30:2298–2302. doi: 10.1097/01.brs.0000182131.44670.f7. [DOI] [PubMed] [Google Scholar]
- 30.Shin DA, Kim KN, Shin HC, Yoon do H. The efficacy of microendoscopic discectomy in reducing iatrogenic muscle injury. J Neurosurg Spine. 2008;8:39–43. doi: 10.3171/SPI-08/01/039. [DOI] [PubMed] [Google Scholar]
- 31.Sihvonen T, Herno A, Paljarvi L, Airaksinen O, Partanen J, Tapaninaho A. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine. 1993;18:575–581. doi: 10.1097/00007632-199304000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Silvers HR, Lewis PJ, Asch HL, Clabeaux DE. Lumbar diskectomy for recurrent disk herniation. J Spinal Disord. 1994;7:408–419. [PubMed] [Google Scholar]
- 33.Suk KS, Lee HM, Moon SH, Kim NH. Recurrent lumbar disc herniation : results of operative management. Spine. 2001;26:672–676. doi: 10.1097/00007632-200103150-00024. [DOI] [PubMed] [Google Scholar]
- 34.Swartz KR, Trost GR. Recurrent lumbar disc herniation. Neurosug Focus. 2003;15:E10. doi: 10.3171/foc.2003.15.3.10. [DOI] [PubMed] [Google Scholar]
- 35.Vishteh AG, Dickman CA. Anterior lumbar microdiscectomy and interbody fusion for the treatment of recurrent disc herniation. Neurosurgery. 2001;48:334–337. discussion 338. [PubMed] [Google Scholar]
- 36.Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation : surgical technique, outcome, and complications in 307 consecutive cases. Spine. 2002;27:722–731. doi: 10.1097/00007632-200204010-00009. [DOI] [PubMed] [Google Scholar]