Abstract
Objective
Recently, motion preservation has come to the forefront of emerging technologies in spine surgery. This is the important background information of the emergence of cervical arthroplasty as an alternative to arthrodesis that offers the promise of restoring normal spinal movement and reduces a kinematic strain on adjacent segments. The study was designed to evaluate early surgical outcome and radiological effects of Bryan® cervical disc prosthesis.
Methods
The authors retrospectively reviewed radiographic and clinical outcomes in 52 patients who received the Bryan® Cervical Disc prosthesis, for whom follow-up data were available. Static and dynamic radiographs were measured by computer to determine the angles formed by the endplates of the natural disc preoperatively, those formed by the shells of the implanted prosthesis, the angle of functional spine unit (FSU), and the C2-7 Cobb angle. The range of motion (ROM) was also determined radiographically, whereas clinical outcomes were assessed using Odom's criteria, visual analogue pain scale (VAS) and neck disability index (NDI).
Results
A total of 71 Bryan® disc were placed in 52 patients. A single-level procedure was performed in 36 patients, a two-level procedure in 13 patients, and a three-level procedure in 3. Radiographic and clinical assessments were made preoperatively. Mean follow-up duration was 29.2 months, ranging from 6 to 36 months. All of the patients were satisfied with the surgical results by Odom's criteria, and showed significant improvement by VAS and NDI score (p < 0.05). The postoperative ROM of the implanted level was preserved without significant difference from preoperative ROM of the operated level (p < 0.05). 97% of patients with a preoperative lordotic sagittal orientation of the FSU were able to maintain lordosis. The overall sagittal alignment of the cervical spine was preserved in 88.5% of cases at the final follow up. Interestingly, preoperatively kyphotic FSU resulted in lordotic FSU in 70% of patients during the late follow up, and preoperatively kyphotic overall cervical alignment resulted in lordosis in 66.6% of the patients postoperatively.
Conclusion
Arthroplasty using the Bryan® disc seemed to be safe and provided encouraging clinical and radiologic outcome in our study. Although the early results are promising, this is a relatively new approach, therefore long-term follow up studies are required to prove its efficacy and its ability to prevent adjacent segment disease.
Keywords: Arthroplasty, Cervical disc, Artificial disc, Bryan®
INTRODUCTION
The procedure of cervical anterior inter-body fusion has been initiated more than 50 years before. Until recently, it has been known as the representative surgical modality for the treatment of degenerative cervical pathologies3-5,18). Its surgical outcomes have been reported to be relatively good according to many studies. On the other hand, however, socioeconomic loss due to the postoperative long-term use of orthosis, an impairment of the cervical movement due to inter-body fusion, the severe degenerative changes of adjacent vertebral body and inter-vertebral disc, the occurrence of secondary pathological conditions have also been reported to be the problems2,8-10,12,13). Particularly in cases where degenerative cervical pathologies were present in the multiple segments, a severe degree of the sequelae occurred. According to some studies, among patients who underwent interbody fusion for the treatment of lesions occurring in the adjacent segments, 2.9% underwent revision surgery within a year. Within ten years, 25.6% of these patients would undergo revision surgery for the management of recurrence13).
In recent years, attempts have been made to compensate these disadvantages using surgical methods that can maintain the segment of cervical motion and remove the pathological conditions. The representative surgical methods include anterior microforaminotomy and various types of artificial disc surgery. Anterior microforaminotomy is a method that removes the part of uncinate process, affecting no cervical movement, and thereby decompresses the neural foramen while preserving a major part of the inter-vertebral disc14). Artificial disc surgery is a type of artificial joint procedure that replaces the lesions with a movable artificial disc after removing all the inter-vertebral discs and the pathological conditions1,7,11). Artificial disc surgery was designed to maintain the articular movement, to avoid the disadvantages of inter-body fusion, to achieve a prompt recovery and to help patients return to the daily lives or work as soon as possible. The objectives of this surgery are to maintain the height of disc, to remove all the pathological conditions compressing the nerve, to maintain the movable joint and to maintain the normal status of adjacent segments.
We performed a surgery mainly using Bryan® (Medtronic Sofamor Danek, Memphis, USA), of various types of artificial disc that have been frequently used, in patients with degenerative cervical pathologies and then attempted to examine the treatment outcomes.
MATERIALS AND METHODS
Of 368 patients with degenerative cervical pathologies who were surgically treated by us at our institution during a period ranging from September of 2000 to March of 2008, 52 patients (71 discs) who underwent artificial disc surgery were enrolled in the current study. Preoperatively, a plain radiography, C-spine 3-D computed topography (CT) and magnetic resonance imaging (MRI) were performed. Six months later, postoperatively follow-up 3-D CT was performed. In some cases, a fluoroscopy was performed to confirm a cervical range of motion (ROM) postoperatively. Preoperative clinical symptoms mainly included unilateral radiculopathy. There were three cases of the compression of spinal cord.
Surgical indications included patients with degenerative cervical pathologies between the levels ranging from the inter-vertebral disc of C3-4 to that of C6-7 whose symptoms could not be improved using the conservative treatment and who concurrently had radiculopathy or the compression of spinal cord. However, patients with a severe pathology of posterior column, vertebral instability, tumor, pathological conditions due to trauma or infections were all excluded from the current analysis. Surgical outcomes were determined based on Odom's criteria, visual analogue pain scale (VAS), and neck disability index (NDI). For the radiological assessment pre- and postoperatively, shell angle, a cervical ROM based on the shell angle, functional spine unit (FSU) and Cobb angle were measured for a comparison (Fig. 1).
Fig. 1.
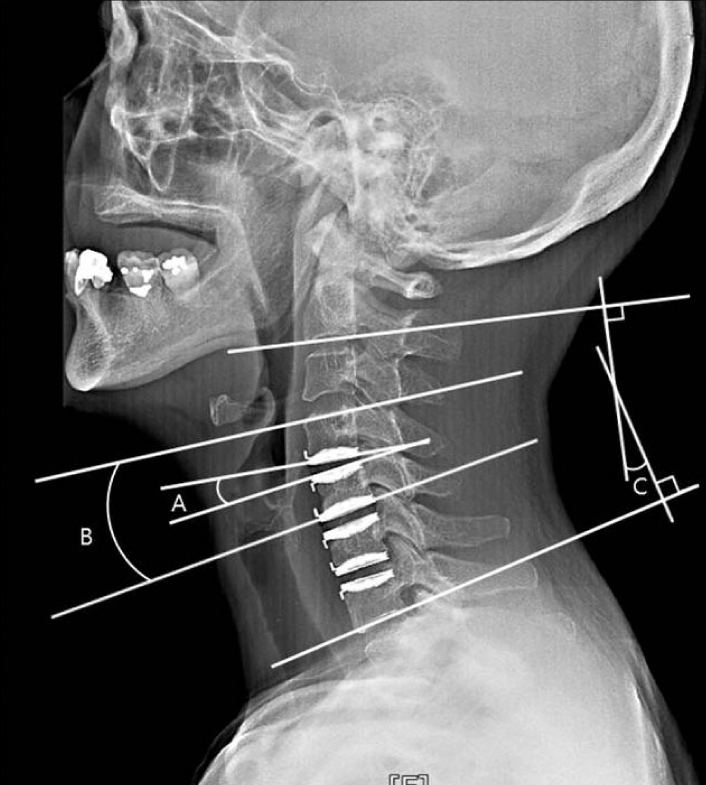
C-spine lateral film showing postoperative state of patient who underwent 3 level cervical arthroplasty for radiculopathy due to muli-level disc herniation. Implant level was measured by shell angles (A), and the adjacent levels were measured by disc space angles, measured on endplates. The functional spine unit (B) and overall cervical (C2-7) alignment (C) were measured by Cobb's method.
Surgery was performed under general anesthesia, for which anterior cervical discectomy was used. The patients were recommended to maintain a normal status of neck in a supine position. Through the conventional methods, the disc was exposed and its part was dissected. Under the guidance of C-arm fluoroscopy, the longitudinal center of the adjacent vertebral body was examined. Based on this, drilling and milling machine were inserted in a sequential manner. The remaining articular plate and some part of the inter-vertebral body were removed. Under the guidance of microscopy, the pathological conditions of vertebral body or inter-vertebral disc were confirmed and then removed. Posterior longitudinal ligament (PLL) was also removed. This was followed by the insertion of artificial disc. The exact position of Bryan® artificial disc was confirmed by C-arm.
RESULTS
Clinical outcome
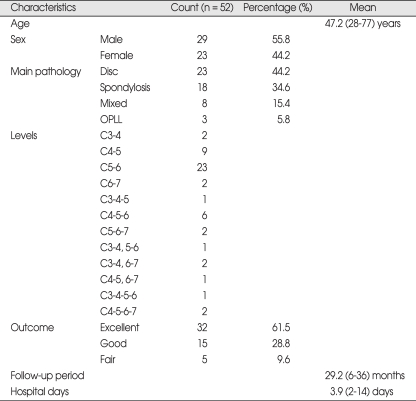
A follow-up observation period ranged between six and 36 months postoperatively (mean value : 29.2 months). In a number of 52 patients, 71 cases of artificial disc replacement were performed. Of these patients, 23 were female patients and 29 were male patients. In these patients, mean age was 47.2 years (28-77 years). Major lesions include 23 patients (44.2%) of herniation of cervical disc, 18 patients (34.6%) of cervical spondylosis, three patients (5.8%) of ossification of posterior longitudinal ligament (OPLL) and eight mixed (15.4%). The number of patients who underwent surgery for one, two and three segments was 36 (69.2%), 13 (25%) and 3 (5.8%), respectively. The areas where surgery was performed include C5-6, C4-5, C6-7 and C3-4 in a decreasing order of the frequency. Surgeries which were concomitantly performed include seven cases (13.5%) of inter-body fusion and eight cases (15.4%) of anterior microforaminotomy. There were no patients who developed the complications associated with the surgery. There were no cases in which a blood transfusion was needed. Surgical outcomes include 32 excellent cases (61.5%), 15 good cases (28.8%) and 5 fair cases (9.6%) (Table 1). Preoperative VAS and NDI scores were significantly improved postoperatively (p < 0.05) (Fig. 2).
Table 1.
Clinical analysis of 52 patients with cervical degenerative pathologies, who underwent cervical artificial disc surgery
OPLL : ossification of posterior longitudinal ligament
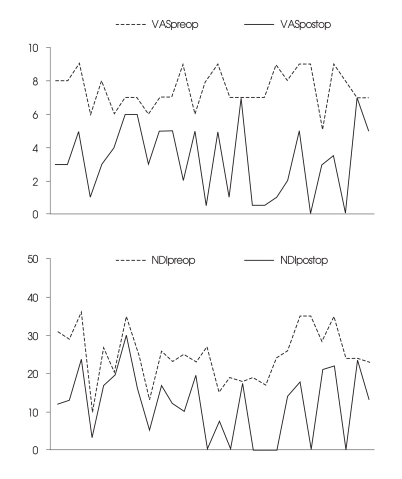
Fig. 2.
Pre- and postoperative visual analogue pain scale (VAS), neck disability index (NDI) score. Both VAS and NDI scores were significantly improved postoperatively.
Radiological outcome
52 total cases
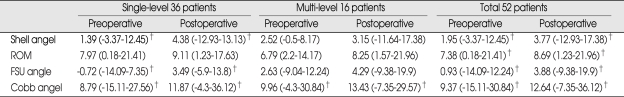
Preoperatively, the mean shell angle was 1.95 degree; a mean cervical ROM based on the shell angle was 7.38 degree; mean FSU angle was 0.93 degree; and mean Cobb angle was 9.37 degree. Postoperatively, these measurements were increased to 3.77 degree, 8.69 degree, 3.88 degree and 12.64 degree respectively. The pre- and postoperative difference of all these parameters showed a statistical significance (p < 0.05) (Table 2).
Table 2.
Radiologic outcome analysis according to pre- and postoperative shell angle, range of motion (ROM) using shell angle on dynamic radiography, functional spine unit (FSU) angle, Cobb angle in patients underwent Bryan® artificial disc surgery. In single-level patients, preoperative shell angle, ROM, FSU angle, and Cobb angle were all improved postoperatively. But, only Cobb angle was improved significantly in multi-level operated patients
†p value less than 0.05 using Student t-test. FSU : functional spine unit, ROM : range of motion
Cases in which a surgery was performed for one segment
Preoperatively, the mean shell angle was 1.39 degree, ROM was 7.97, FSU angle -0.72 and Cobb angle 8.79. Postoperatively, these measurements were increased to 4.38, 9.11, 3.49 and 11.87 in the corresponding order. Of these, only ROM did not reach a statistical significance (p > 0.05) (Table 2). The number of cases showing kyphosis in the segment of operation was 7/36 (19.4%). The number of cases in which there was a kyphosis in the overall cervical area was 7/36 (19.4%). The number of cases in which a kyphosis was corrected postoperatively in the corresponding segment was 5/6 (71.4%). The number of cases in which a kyphosis present in the overall area of cervix was corrected was 5/7 (71.4%). The number of cases in which a kyphosis was developed in the corresponding segment was 2/29 (6.9%). The number of cases in which a kyphosis occurred in the overall area of cervical spine was 1/29 (3.5%).
Cases in which a surgery was performed for more than two segments
Preoperatively, the shell angle was 2.52 degrees, ROM was 6.79, FSU angle 2.63 and Cobb angle 9.96. These measurements were postoperatively increased to 3.15, 8.25, 4.29 and 13.43. But, of these parameters, only the difference of Cobb angle was statistically significant (p < 0.05) (Table 2). The number of cases in which there was a kyphosis in the surgical segment was 3/35 (8.6%). The number of cases in which a kyphosis occurred in the overall area of cervix was 2/16 (12.5%). 2 cases (67%) in which a kyphosis present in the corresponding segment and 1 case (50%) showing kyphosis in overall cervical area were corrected following the surgery. The number of cases in which a kyphosis occurred in the corresponding segment was 5/32 (15.6%). The number of cases in which a kyphosis occurred in the overall area of cervix was 2/14 (14.3%).
DISCUSSION
Cervical anterior inter-body fusion is a standard surgical treatment regimen for the cervical lesions. Despite a higher degree of the satisfactory treatment outcomes, degenerative changes in the adjacent segments to the surgical ones appear in a time-dependent manner following the surgery. The concept that degenerative changes occur with the increased loading on the adjacent inter-vertebral disc because of the cervical inter-body fusion has been widely accepted13,16,20). Although the inter-body fusion is beneficial for the lesion segments, it has a detrimental effect on the remaining movable segments. Due to a loss of the movement, as described here, patients intermittently complain of the cervical stiffness, the functional restriction and the functional degeneration of inter-vertebral disc in the adjacent segments. These changes are seen in 3% of patients, which are expected to rise up to 25% on postoperative ten years.
To overcome these disadvantages, the artificial disc surgery has been designed. Many studies have reported good treatment outcomes. According to a European report about a short-term surgical outcome which was assessed after a 1-year postoperative period, the proportion of patients who showed excellent, good and fair surgical treatment outcomes exceeded 90%. A cervical movement has been reported to be maintained in 88% of cases in which a surgery was performed for one segment and 86% of those in which a surgery was performed for more than two segments11).
Goffin et al.11) conducted a multi-center study, based on which these authors reported that good treatment outcomes were achieved in 90% of cases in which a surgery was performed for one segment after a 6-month period, 86% after a 12-month period and 90% after a 24-month period. According to these authors, good treatment outcomes were also achieved in 82% of cases in which a surgery was performed for two segments after a 6-month period and 96% after a 12-month period. There were no cases in which the abnormal findings or the dislocation of artificial disc occurred following the use of artificial disc. After a 1-year period, ROM of flexion and extension per segment has been reported to be 7.9 degree in cases in which a surgery was performed for one segment and 7.4 degree in those in which it was performed for two segments.
Anderson et al.1) conducted a follow-up study in 73 patients who underwent surgery using Bryan® artificial disc for one segment and then could be followed up during a minimum period of 2 years, based on which these authors noted that there were 45 cases of excellent treatment outcomes, seven cases of good treatment outcomes, 13 cases of fair treatment outcomes and eight cases of poor treatment outcomes. Based on the functional assessment of surgical outcomes on SF-36 scale, the surgical outcomes were greatly improved after a 3-month period following the surgery. Besides, this was reported to be maintained for 24 months. Mean range of the motion per each segment was 8 degrees. In one case, due to an insufficient extent of the surgery, the displacement of artificial disc was observed.
Duggal et al.7) performed surgery using 30 Bryan® artificial discs in 26 patients and then conducted a follow-up study during a mean period of 12.3 months. According to these authors, NDI was significantly improved. Besides, from a biomechanical perspective, the exercise and loading which was increased in the adjacent segment seen following the interbody fusion were reported to disappear following the artificial disc surgery6).
The other study, Park et al.17) performed surgery using 21 Mobi-C® artificial discs and then compared with 32 Solis®-cage interbody fusion. They suggest that clinical results, such as NDI and upper extremity VAS score, were similar in both groups that underwent arthroplasty or fusion. Postoperative recovery time was, however, shorter in the arthroplasty group, which may be related to absence of postoperative orthosis and iliac graft donor site pain. But, the patients underwent surgery for one segment.
Complications have been reported to include the hematoma formed in the anterior region to the vertebrae, the remaining presence of lesions, epidural hematoma, damages to the larynx or esophagus, the transient or permanent paralysis of vocal cord and the transient displacement of artificial disc11). Some authors have reported that the bone fusion occurred due to spontaneous ossification following the artificial disc surgery15,18). Pickett et al.18) conducted 96 cases of artificial disc surgery in 74 patients and then reported that the complications occurred at an incidence of 6.2%. Of these, there were two cases of bone fusion due to the spontaneous ossification. Leung et al.15) reported these phenomena in 17.8% of patients who underwent artificial disc surgery. According to these authors, the male patients and old age were risk factors. In this study, however, there were no cases in which bone fusion occurred due to spontaneous ossification following the artificial disc surgery.
Treatment goals of the artificial disc surgery for cervical spine are to remove the nerve compression showing the symptoms through a cervical decompression without a loss of the movement. Through the artificial disc surgery, pain alleviation, nerve decompression, the prevention of degenerative changes of adjacent segments, the preservation of movement, the maintenance of the height of inter-vertebral disc, the decreased morbidity due to the surgery and a prompt recovery of the function could be expected. Indications include the following : 1) Cases in which no instability or hypermobility were present despite a lack of the abnormality in cervical alignment; 2) Cases in which there were no findings that are suggestive of osteoporosis. By contrast, contraindications include the following19) : 1) Cases in which there was a past surgical history or cervical pain was the only symptomatic presentation; 2) Severe anatomical deformity; 3) Cases in which there was a radiological instability (the displacement of > 2mm and the flexion deformity of > 11 degree); 4) Osteoporosis; 5) Metastatic cancer; 6) Osteomalacia; 7) The pathological conditions of posterior joint; 8) The presence of severe spinal abnormality due to osteophyte; 9) Chronic infections; 10) Tumors; 11) Systemic or metabolic diseases; and 12) Metal allergy.
In the current study, the shell angle was significantly increased postoperatively as compared with preoperatively (p < 0.05). There was no significant difference in the ROM of the corresponding segments based on the shell angle between preoperatively and postoperatively (p > 0.05). In the adjacent segments to the surgical sites, the ROM which was decreased postoperatively in the early stage achieved a greater extent of the recovery on postoperative month 6 (p < 0.05). Following the surgery, both FSU angle and Cobb angle were found to increase (p < 0.05). Radiological findings which were shown preoperatively and postoperatively were all improved in cases in which a surgery was performed for one segment. In cases in which a surgery was performed for more than two segments, however, there was no significant difference following the surgery except Cobb angle.
Of patients who underwent surgery for one segment, 19.4% who showed a kyphosis in the corresponding segments were found to have a corrected kyphosis at a frequency of 71.4%. In 17.3% of patients who had a kyphosis in the overall area of cervix, a corrected kyphosis was seen at a frequency of 66.7%. The proportion of cases in which a kyphosis which was absent preoperatively occurred postoperatively was 7%. In patients who were surgically treated for more than two segments, however, two of patients showed a kyphosis in the corresponding segments and one who showed a kyphosis in the overall area of the cervix did not feature a corrected kyphosis postoperatively. There was one patient who presented with a kyphosis although it did not occur preoperatively. Cases in which a kyphosis occurred include the insertion angle of artificial disc, an excessive manipulation during the milling process for the implantation of artificial disc and the severity of the preoperative presence of kyphosis. Insertion angle for artificial disc is important and it is also associated with the articular plate and a partial removal of adjacent vertebral spines. There are no specific methods for maintaining an optimal level of the angle. The insertion angle can be affected by the location of segments where lesions are present, the overall shape of cervical region, the patient posture during surgery, the degree of relaxation of cervical muscles, the scope of skin incision and the relative location. Particularly in cases in which a surgery is performed for multiple adjacent segments, by establishing an optimal level of the insertion angle, a preoperative planning is essential for the prevention of an excessive manipulation.
On radiological assessment, the findings are observed to be closer to those of kyphosis immediately after surgery. In most cases, however, from postoperative week 6, this had a tendency to be improved. Rather than the relationship with the biomechanical characteristics of artificial disc, the time-dependent alleviation of pain and muscle stiffness would be a more responsible factor. Based on clinical and radiological findings, surgical segments were mostly found to preserve the degree of movement to such an extent as preoperative status or higher. Pain which was seen preoperatively was markedly reduced. There were no cases featuring the displacement or dislocation of the inserted artificial disc. In two cases, however, the direction to which the artificial disc was initially inserted was deviated. But this did not affect the clinical outcomes.
Most cases of the degenerative cervical pathologies are present in more than one segment. Therefore, the functional loss due to the bone fusion for multiple segments can be problematic. In recent studies, the artificial disc surgery for two segments has been accredited as a feasible, safe procedure. In our series, we performed artificial disc surgery for more than two segments in 16 patients. We also performed artificial disc surgery for three segments in three patients. All of these cases showed good clinical results. Radiological outcomes also showed that the ROM was maintained and the alignment of overall cervical area was improved as compared with preoperatively. Although the effects of artificial disc surgery for three segments could not been clarified in patients with degenerative cervical pathologies, based on our clinical experience, the effectiveness of artificial disc surgery for multiple segments would be accredited in the near future.
CONCLUSION
Limitations of the current study include the following. The current study was conducted in a limited scope of the radiological assessment which was restricted to the sagittal plane. Radiological changes were not compared with those of clinical symptoms. A long-term follow-up study would be essential for an accurate assessment. In the current study, however, the artificial disc surgery using Bryan® showed safe, satisfying results from both clinical and radiological perspectives. These results indicate that novel methods of surgical treatment have been of increasing interest in patients with degenerative cervical pathologies.
References
- 1.Anderson PA, Sasso RC, Rouleau JP, Carlson CS, Goffin J. The Bryan Cervical Disc : wear properties and early clinical results. Spine J. 2004;4:303S–309S. doi: 10.1016/j.spinee.2004.07.026. [DOI] [PubMed] [Google Scholar]
- 2.Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993;75:1298–1307. doi: 10.2106/00004623-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Clements D, O'Leary PF. Anterior cervical discectomy and fusion. Spine. 1990;15:1023–1025. doi: 10.1097/00007632-199015100-00008. [DOI] [PubMed] [Google Scholar]
- 4.Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15:602–617. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 5.Cloward RB. The treatment of ruptured lumbar intervertebral disc by vertebral body fusion : III. Method of use of banked bone. Ann Surg. 1952;136:987–992. doi: 10.1097/00000658-195212000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DiAngelo DJ, Roberston JT, Metcalf NH, McVay BJ, Davis RC. Biomechanical testing of an artificial cervical joint and an anterior cervical plate. J Spinal Disord Tech. 2003;16:314–323. doi: 10.1097/00024720-200308000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Duggal N, Pickett GE, Mitsis DK, Keller JL. Early clinical and biomechanical results following cervical arthroplasty. Neurosurg Focus. 2004;17:E9. doi: 10.3171/foc.2004.17.3.9. [DOI] [PubMed] [Google Scholar]
- 8.Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine. 2002;27:2431–2434. doi: 10.1097/00007632-200211150-00003. [DOI] [PubMed] [Google Scholar]
- 9.Fuller DA, Kirkpatrick JS, Emery SE, Wilber RG, Davy DT. A kinematic study of the cervical spine before and after segmental arthrodesis. Spine. 1998;23:1649–1656. doi: 10.1097/00007632-199808010-00006. [DOI] [PubMed] [Google Scholar]
- 10.Goffin J, Geusens E, Vantomme N, Quintens E, Waerzeqqers Y, Depreitere B, et al. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech. 2004;17:79–85. doi: 10.1097/00024720-200404000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Goffin J, Van Calenbergh F, van Loon J, Casey A, Kehr P, Liebig K, et al. Intermediate follow-up after treatment of degenerative disc disease with the Bryan Cervical Disc Prosthesis : single-level and bi-level. Spine (Phila Pa 1976) 2003;28:2673–2678. doi: 10.1097/01.BRS.0000099392.90849.AA. [DOI] [PubMed] [Google Scholar]
- 12.Goffin J, van Loon J, Van Calenbergh F, Plets C. Long-term results after anterior cervical fusion and osteosynthetic stabilization for fractures and/or dislocations of the cervical spine. J Spinal Disord. 1995;8:500–508. discussion 499. [PubMed] [Google Scholar]
- 13.Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999;81:519–528. doi: 10.2106/00004623-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Jho HD, Kim WK, Kim MH. Anterior microforaminotomy for treatment of cervical radiculopathy : part 1 disc-preserving "functional cervical disc surgery". Neurosurgery. 2002;51:S46–S53. [PubMed] [Google Scholar]
- 15.Leung C, Casey AT, Goffin J, Kehr P, Liebig K, Lind B, et al. Clinical significance of heterotopic ossification in cervical disc replacement : a prospective multicenter clinical trial. Neurosurgery. 2005;57:759–763. doi: 10.1093/neurosurgery/57.4.759. [DOI] [PubMed] [Google Scholar]
- 16.Matsunaga S, Kabayama S, Yamamoto T, Yone K, Sakou T, Nakanishi K. Strain on intervertebral discs after anterior cervical decompression and fusion. Spine. 1999;24:670–675. doi: 10.1097/00007632-199904010-00011. [DOI] [PubMed] [Google Scholar]
- 17.Park JH, Roh KH, Cho JY, Ra YS, Rhim SC, Noh SW. Comparative analysis of cervical arthroplasty using mobi-C(r) and anterior cervical discectomy and fusion using the solis(r)-Cage. J Korean Neurosurg Soc. 2008;44:217–221. doi: 10.3340/jkns.2008.44.4.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pickett GE, Sekhon LH, Sears WR, Duggal N. Complications with cervical arthroplasty. J Neurosurg Spine. 2006;4:98–105. doi: 10.3171/spi.2006.4.2.98. [DOI] [PubMed] [Google Scholar]
- 19.Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40A:607–624. [PubMed] [Google Scholar]
- 20.Wigfield C, Gill S, Nelson R, Langdon I, Metcalf N, Robertson J. Influence of an artificial cervical joint compared with fusion on adjacent-level motion in the treatment of degenerative cervical disc disease. J Neurosurg. 2002;96:17–21. doi: 10.3171/spi.2002.96.1.0017. [DOI] [PubMed] [Google Scholar]