Abstract
A 47-year-old man presented with a subarachnoid hemorrhage (SAH) and right cerebellar hematoma was referred for evaluation. Cerebral angiography revealed a distal anterior inferior cerebellar artery (AICA) aneurysm associated with an arteriovenous malformation (AVM). Successful obliteration and complete removal of the aneurysm and AVM were obtained using transcortical approach under the guidance of neuronavigation system. The association of a peripheral AICA aneurysm and a cerebellar AVM by the same artery is unique. The reported cases of conventional surgery for this disease complex are not common and their results are variable. Less invasive surgery using image-guided neuronavigation system would be helpful and feasible for a peripheral aneurysm combining an AVM of the posterior fossa in selective cases.
Keywords: Aneurysm, Anterior inferior cerebellar artery, Arteriovenous malformation, Neuronavigation
INTRODUCTION
Distal anterior inferior cerebellar artery (AICA) aneurysms are very rare3,8). Aneurysms associated with an arteriovenous malformation (AVM) fed by the same arterial trunk reportedly account for only 2.8 to 9.3% of all cerebral AVMs4,13). Cases of peripheral AICA aneurysms associated with an AVM are also very rare, and most cases of the combination of the two malformations have been treated using various surgical approaches, depending on their location and neurovascular intimacy with the brain stem1,6-8,10,11,14,16). In this paper, the authors report the usefulness of a cerebellar transcortical approach performed with the assistance of imageguided neuronavigation in order to verify the exact location of the aneurysm accompanied by an AVM and to simultaneously remove them using a less invasive procedure.
CASE REPORT
A 47-year-old man was transferred to our hospital with a history of sudden headache and dizziness. Computed tomographic scan showed an subarachnoid hemorrhage (SAH) and hematoma in the right cerebellum (Fig. 1). Brain magnetic resonance imaging revealed a tangled signal void in the peripheral portion of the right cerebellar hematoma (Fig. 2). Angiography revealed a 7-mm sized saccular aneurysm of the right distal AICA and a 12-mm sized AVM nidus located distally from the aneurysm and fed by the same artery with a single draining vein (Fig. 3). Due to the distal location of the AICA aneurysm, which was a strong indication of the source of the SAH and cerebellar hematoma, in addition to its favorable dome-to-neck ratio, endovascular coil embolization was performed but failed because the aneurysm was too distal from the vertebrobasilar trunk. Microcatheter navigation was also too difficult to perform due to the acute angulation between the AICA and basilar artery. Several gentle trials of navigation through the AICA were carried out using both microwire-guided and flow-directed microcatheters but caused a significant vasospasm in the proximal AICA and basilar artery (Fig. 4), followed by an unstable fluctuation in blood pressure. Because the AICA in our patient supplied not only the territory of the AICA, but also the territory of the ipsilateral posterior inferior cerebellar artery (PICA), saying the AICA-PICA common trunk, serious damage could occur even with subtle complication in the proximal AICA during endovascular therapy. Thus, any further manipulation involving an endovascular approach was abandoned, and the patient was scheduled to undergo a subsequent neck clipping and nidus resection with a craniotomy. Surgical clipping of the distal AICA aneurysm and AVM resection were performed via a unilateral retrosigmoid suboccipital approach. A modified three-quarter position was used, and several fiducial markers were attached to the surface of the parieto-occipital scalp in order to verify the exact location of the cerebellar hematoma that overlaid both the aneurysm and AVM. A right-sided lateral retrosigmoid suboccipital bone flap was made, and the dura was opened. The AICA proximal to the aneurysm and its lowest part were found using a navigation wand following the partial removal of the cerebellar hematoma (Fig. 5). The AICA was then followed to the periphery until the neck of aneurysm was exposed with minimal brain retraction. After applying a temporary clip to the AICA, less than 10 minutes in each three temporary placements of clip, and performing a careful neck dissection, the neck of the aneurysm was clipped with a straight clip. A portion of the AVM nidus medial to the clipped aneurysm was exposed and removed following circumferential dissection and careful coagulation. Finally, the draining vein was closed after the total removal of the nidus. The postoperative course was uneventful, and postoperative angiography showed neither aneurysm nor AVM nidus (Fig. 6). The patient was discharged after a short hospital stay, and he is doing well during the 25-month follow-up.
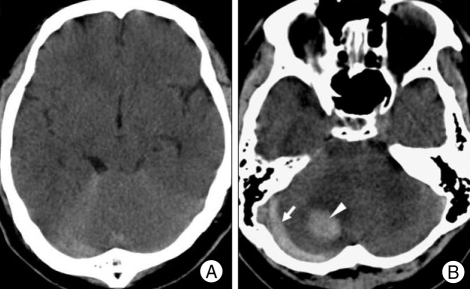
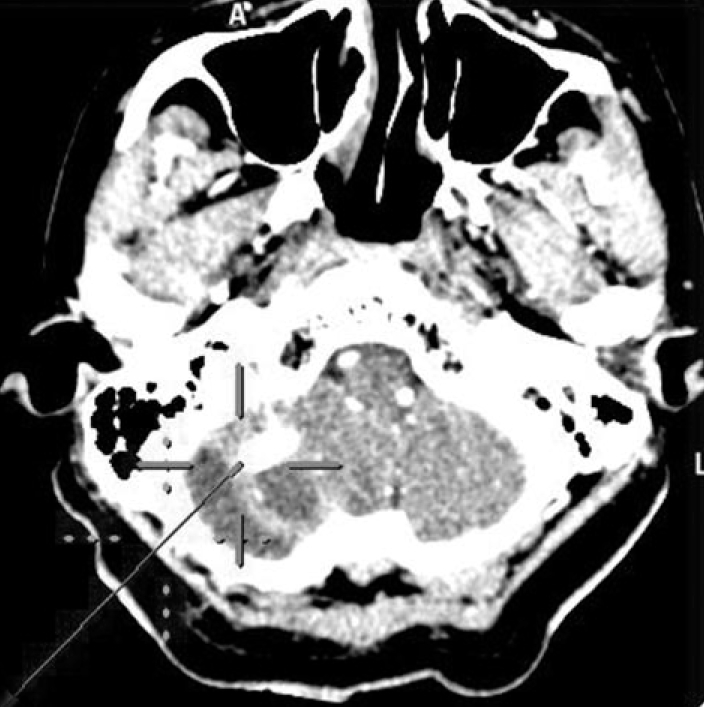
Fig. 1.
Computed tomography at admission showing a subarachnoid hemorrhage under the falcotentorium (A), subdural (arrow) and subcortical (arrowhead) hematoma in the right cerebellum (B).
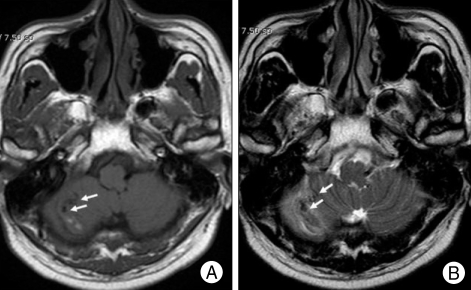
Fig. 2.
Axial T1-weighted (A) and T2-weighted (B) magnetic resonance image showing tangled signal voids (arrows) near the right cerebellar hematoma.
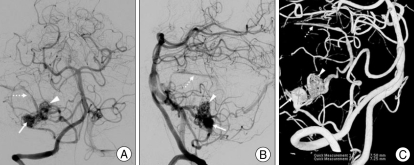
Fig. 3.
Right vertebral angiogram anteroposterior (A) and lateral (B) image revealing a distal anterior inferior cerebellar artery (AICA) aneurysm (arrow) associated with an arteriovenous malformation (AVM) nidus (arrowhead) with a draining vein (broken arrow) into the sigmoid sinus that was located distal to the AICA aneurysm. Note the clear relationship between a flow-related AICA aneurysm and cerebellar AVM shown by the reconstruction image of 3D rotational angiogram (C).
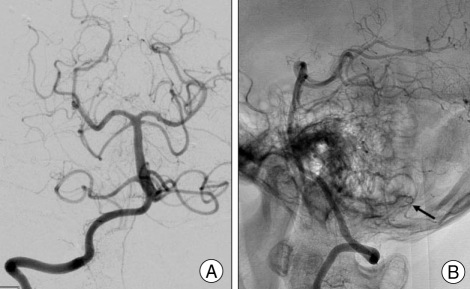
Fig. 4.

Right vertebral angiogram during the endovascular neurointervention showing a severe vasospasm (arrows) in the proximal part of the anterior inferior cerebellar artery due to the heavy tension caused by microcatheter manipulations.
Fig. 5.
The photograph obtained during the image-guided neurosurgery showing the target entry to the vascular pathology in the right cerebellum pointed out by a navigation wand (dotted cross to the skull and cross to the malformation).
Fig. 6.
Postoperative right vertebral angiogram anteroposterior (A) view and lateral (B) none-subtracted view showing neither distal anterior inferior cerebellar aneurysm nor an associated arteriovenous malformation. Arrow in (B) indicates a surgical clip.
DISCUSSION
Aneurysms of the peripheral AICA are quite rare, with an incidence of 0.0003-0.5%3). They tend to occur predominantly in the meatal segment or dorsolateral branch of the AICA2), and their occurrence in association with a high-flow lesion, such as an AVM or cerebellar hemagioblastoma, has scarcely been reported1,6-11,14,16). The association of a distal AICA aneurysm with an AVM fed by the same artery has been described in only 11 cases elsewhere1,6-8,10,11,14,16).
The clinical presentation of distal cerebral aneurysms usually includes sudden-onset SAH or the gradual onset of cerebellopontine angle signs, less frequently, including facial nerve paresis and hearing disturbance, depending on their location. With the exception of post-traumatic or mycotic aneurysms, the pathogenesis of distal cerebral aneurysms remains unclear; however, it is known that increased blood flow through a blood vessel causes a certain hemodynamic burden to the vessel wall and in turn stimulates the formation of an aneurysm on that vessel. The association of a cerebral aneurysm of the feeding artery with an AVM, especially infratentorial AVMs, is a well-known phenomenon15,17,18). Increased blood flow in the common trunk and a distal AVM may stimulate the formation of a flow-related aneurysm. Surgical treatment should be directed towards the pathology responsible for the hemorrhage and asymptomatic vascular malformation. The treatment of either an aneurysm or AVM alone may cause the remaining lesion to bleed due to hemodynamic changes11,15). Some authors have recommended that the symptomatic lesion, if determined, should be treated first and that simultaneous exclusion of both the aneurysm and the malformation can be undertaken whenever it is possible to safely do so during the same operation without unreasonably increasing the risk of the procedure5).
The surgical management of AICA aneurysms is complex due to their location and close relationship to the brain stem and lower cranial nerves. The reported complication rate reaches almost 60% with various surgical approaches, even in the hands of experts in the field of microvascular surgery8). Most of the surgical series in the literature used a retrosigmoid approach or some form of skull-based surgery, especially when the AICA aneurysm was located in the anterolateral portion of the brain stem1,2,7,8,10,11,14,16). The retrosigmoid suboccipital approach is typically recommended for the treatment of distal aneurysms and their associated AVMs because the petrous surface of the cerebellar hemisphere provides an appropriate surgical corridor8,11,16). In our case, the authors used a distinguished cerebellar transcortical approach and used a novel neuronavigation system to achieve an accurate trajectory in accordance with the removal of the pre-existing cerebellar clot. With this method, a peripheral aneurysm and its parent artery, the AICA, were exposed easily after the partial removal of the hematoma without brain retraction. The usefulness of recent advances in neuronavigation technology in the management of skull base tumors and of vascular lesions has been recently presented12,19). To the best of the authors' knowledge, this is the first report to describe the usage of an image-guided neuronavigation system when performing aneurysm clipping and resection of an associated AVM via a transcortical approach. Blind removal of a cerebellar hematoma can cause the peripheral aneurysm that was hidden behind the clot to rupture prematurely. Image-guided neurosurgery with the use of a neuronavigation system may effectively minimize the unpredictable risks associated with blind removal and could be used to tailor the surgical corridor when properly applied to the patient.
CONCLUSION
The authors present a case of ruptured distal AICA aneurysm associated with an AVM. This phenomenal peripheral aneurysm was believed to be a flow-related aneurysm, and both the aneurysm and AVM were totally excluded from the cerebellar circulation via a transcortical approach under the guidance of a neuronavigation system. The effectiveness and feasibility of the use of advanced neuronavigation technology for peripheral cerebrovascular lesions should be the focus of future investigations in a larger series of cases.
References
- 1.Akyüz M, Tuncer R. Multiple anterior inferior cerebellar artery aneurysms associated with an arteriovenous malformation : case report. Surg Neurol. 2005;64(Suppl 2):S106–S108. doi: 10.1016/j.surneu.2005.07.037. [DOI] [PubMed] [Google Scholar]
- 2.Andaluz N, Pensak ML, Zuccarello M. Multiple, peripheral aneurysms of the anterior inferior cerebellar artery. Acta Neurochir (Wien) 2005;147:419–422. doi: 10.1007/s00701-004-0453-7. discussion 422. [DOI] [PubMed] [Google Scholar]
- 3.Banczerowski P, Sipos L, Vajda J. Aneurysms of the internal auditory artery. Our experience and review of the literature. Acta Neurochir (Wien) 1996;138:1157–1162. doi: 10.1007/BF01809744. [DOI] [PubMed] [Google Scholar]
- 4.Cronqvist S, Troupp H. Intracranial arteriovenous malformation and arterial aneurysm on the same patient. Acta Neurol Scand. 1996;42:307–316. doi: 10.1111/j.1600-0404.1966.tb01185.x. [DOI] [PubMed] [Google Scholar]
- 5.Cunha e Sa MJ, Stein BM, Solomon RA, McCormick PC. The treatment of associated intracranial aneurysm and arteriovenous malformation. J Neurosurg. 1992;77:853–859. doi: 10.3171/jns.1992.77.6.0853. [DOI] [PubMed] [Google Scholar]
- 6.Drake CG, Friedman AH, Peerless SJ. Posterior fossa arteriovenous malformation. J Neurosurg. 1986;64:1–10. doi: 10.3171/jns.1986.64.1.0001. [DOI] [PubMed] [Google Scholar]
- 7.Gacs G, Vinuela F, Fox AZ, Drake CG. Peripheral aneurysm of the cerebellar arteries. Review of 16 cases. J Neurosurg. 1983;58:63–68. doi: 10.3171/jns.1983.58.1.0063. [DOI] [PubMed] [Google Scholar]
- 8.Gonzalez LF, Alexander MJ, McDougall CG, Spetzler RF. Anteroinferior cerebellar artery aneurysms : surgical approaches and outcomesa review of 34 cases. Neurosurgery. 2004;55:1025–1035. doi: 10.1227/01.neu.0000141083.00866.82. [DOI] [PubMed] [Google Scholar]
- 9.Guzman R, Grady MS. An intracranial aneurysm on the feeding artery of a cerebellar hemangioblastoma. J Neurosurg. 1999;91:136–138. doi: 10.3171/jns.1999.91.1.0136. [DOI] [PubMed] [Google Scholar]
- 10.Kikuchi K, Kamisato N, Sasanuma J, Watanabe K, Kowada M. [Trigeminal neuralgia associated with posterior fossa arteriovenous malformation and aneurysm fed by the same artery. Case report] Neurol Med Chir (Tokyo) 1990;30:918–921. doi: 10.2176/nmc.30.918. [DOI] [PubMed] [Google Scholar]
- 11.Menovsky T, André Grotenhuis J, Bartels RH. Aneurysm of the anterior inferior cerebellar artery associated with high-flow lesion : report of two cases and review of literature. J Clin Neurosci. 2002;9:207–211. doi: 10.1054/jocn.2001.0945. [DOI] [PubMed] [Google Scholar]
- 12.Redekop G, TerBrugge K, Montanera W, Willinsky R. Arterial aneurysms associated with cerebral arteriovenous malformation : classification, incidence, and their risk of hemorrhage. J Neurosurg. 1998;89:539–546. doi: 10.3171/jns.1998.89.4.0539. [DOI] [PubMed] [Google Scholar]
- 13.Rohde V, Spangenberg P, Mayfrank L, Reinges M, Gilsbach JM, Coenen VA. Advanced neuronavigation in skull base tumors and vascular lesions. Minim Invasive Neurosurg. 2005;43:13–18. doi: 10.1055/s-2004-830179. [DOI] [PubMed] [Google Scholar]
- 14.Suzuki J, Onuma T. Intracranial aneurysms associated with arteriovenous malformation. J Neurosurg. 1979;50:742–749. doi: 10.3171/jns.1979.50.6.0742. [DOI] [PubMed] [Google Scholar]
- 15.Tarlov E. Subarachnoid hemorrhage. Prim Care. 1979;6:791–803. [PubMed] [Google Scholar]
- 16.Thompson RC, Steinberg GK, Levy RP, Marks MP. The management of patients with arteriovenous malformation and associated intracranial aneurysms. Neurosurgery. 1998;43:202–211. doi: 10.1097/00006123-199808000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Vincetelli F, Caruso G, Licastro G, Rabehanta P. Association between an aneurysm of the anterior inferior cerebellar artery and an arteriovenous malformation fed by the same artery. J Neurosurg Sci. 1998;42:41–45. [PubMed] [Google Scholar]
- 18.Westphal M, Grzyska U. Clinical significance of pedicle aneurysm on feeding vessels, especially those located in infratentorial arteriovenous malformations. J Neurosurg. 2000;92:995–1001. doi: 10.3171/jns.2000.92.6.0995. [DOI] [PubMed] [Google Scholar]
- 19.Willems PW, van Walsum T, Woerdeman PA, van de Kraats EB, de Kort GA, Niessen WJ, et al. Image-guided vascular neurosurgery based on three-dimensional rotational angiography Technical note. J Neurosurg. 2007;106:501–506. doi: 10.3171/jns.2007.106.3.501. [DOI] [PubMed] [Google Scholar]