Abstract
Cerebellar hemorrhage is an unusual complication of supratentorial neurosurgery. To the best of our knowledge, only three case reports have described the occurrence of cerebellar hemorrhage after burr hole drainage for the treatment of chronic subdural hematoma (SDH). We present the case of a patient with this rare postoperative complication of cerebellar hemorrhage after burr hole drainage of a chronic SDH. Although burr hole drainage for the treatment of chronic SDH is rare complication, it is necessary to be aware of the possibility of cerebellar hemorrhage after supratentorial surgery, even with limited surgery such as burr hole drainage of a chronic SDH.
Keywords: Cerebral hemorrhage, Subdural hematoma, Craniotomy, Complication, Supratentorial
INTRODUCTION
Cerebellar hemorrhage is an unusual but increasingly recognized complication of supratentorial neurosurgery4,7). Most cases describe this remote cerebellar hemorrhage in relation to craniotomy for cerebral tumor resection, aneurysm surgery, intracranial hematoma decompression and temporal lobe resection requiring brain retraction and removal of CSF at the time of surgery.
To our knowledge, only three reported cases have previously described the occurrence of cerebellar hemorrhage after burr hole drainage of a chronic subdural hematoma (SDH)3,6,14). Several preoperative and medical risk factors may predispose patients to cerebellar hemorrhage after supratentorial surgery. However, the etiology of this complication remains unclear. We report a case of cerebellar hemorrhage after burr hole drainage of a chronic SDH and review the reported cases to discuss possible etiologic mechanisms.
CASE REPORT
A 53-year-old woman who was previously healthy complained of right leg weakness lasting for one week. There had been no prior head trauma. Due to a gradually developing gait disorder, magnetic resonance imaging of the brain was performed, and the results showed a chronic bifrontal subdural hematoma (Fig. 1). She had been taking metformin under the diagnosis of diabetes mellitus for 3 years. There was no history of arterial hypertension or hemorrhagic diathesis. Preoperative coagulation parameters (prothrombin time, partial thromboplastin time, anti-thrombin III, bleeding time, platelet count) were normal. Surgery was performed under general anesthesia with the patient in the supine position, without head rotation. Frontal burr holes were drilled on each side. The hematoma was slowly decompressed, and the subdural space was gently irrigated with warm isotonic saline to evacuate the hematoma. Irrigation was continued until clear fluid returned. At the end of the operation, a subdural frontal closed drainage system without negative pressure was placed on each side. The procedure was completed without any obvious complications. The patient's perioperative blood pressure remained within normal range. The patient developed a strong headache, dizziness, nausea and vomiting after being transported to the neurosurgical intensive care unit. Computed tomography (CT) scan taken 6 hours after the operation demonstrated adequate drainage of the subdural hematomas, and it also revealed a new hemorrhage within the left cerebellar hemisphere (Fig. 2). The total drainage from the subdural space was 100 mL on the right side and 120 mL on the left side. Because the fluid in the connecting catheter was clean and pulsated with the patient's heart beat, the drainage system was clamped. On the second day after the operation, the patient immediately developed a severe headache upon transient opening of the drainage system, which was removed 3 days after the surgery. The patient improved gradually with bed rest and hydration. CT scan performed 14 days after the operation showed resolution of the cerebellar hemorrhage (Fig. 3). There was no abnormal finding on conventional angiography (Fig. 4). The patient was discharged 3 weeks after surgery with the recovery of leg weakness.
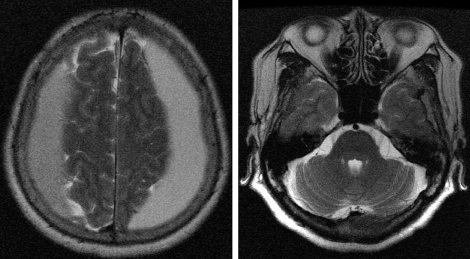
Fig. 1.
Preoperative T2-weighted axial magnetic resonance images of the brain show a bifrontal subdural hematoma without abnormal findings in the posterior fossa.
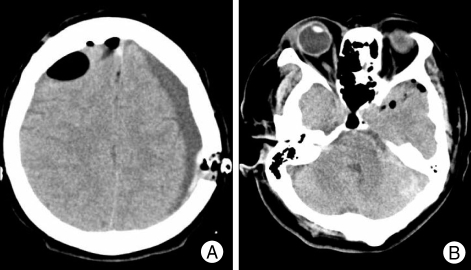
Fig. 2.
Postoperative computed tomography images obtained 6 hours after surgery show resolution of the subdural hematoma (A) and left-sided cerebellar hemorrhage (B).
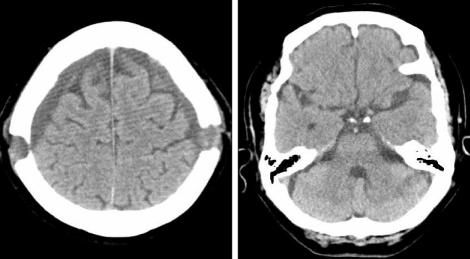
Fig. 3.
Postoperative computed tomography images taken on postoperative day 14 show resolution of the cerebellar hemorrhage.
Fig. 4.
The normal structure of posterior circulation is seen in arterial phase (A) and venous phase (B) of conventional cerebral angiography.
DISCUSSION
Postoperative hemorrhage is a feared complication of neurosurgery. Much effort is focused on minimizing the risk of postoperative hemorrhage through careful hemostasis intraoperatively and tight control of coagulation parameters perioperatively. Previous studies reported that the incidence of postoperative hematoma was 0.8% after 4,992 craniotomies5), including burr hole trephination, and 1.1% after 6,668 neurosurgical procedures of any kind10). Hemorrhage remote from the site of surgery is an increasingly recognized complication of neurosurgery. Infratentorial surgery can lead to supratentorial hemorrhage and vice versa13). Remote cerebellar hemorrhage is a rare complication of neurosurgery. Approximately, 60 cases of craniotomy complicated by cerebellar hemorrhage have been documented9).
We performed a PubMed search using the key words "hemorrhage", "remote hemorrhage", "cerebellar hemorrhage", "subdural hematoma", and/or "burr hole craniotomy". The characteristics of our case and 3 cases of remote cerebellar hemorrhage after burr hole trephination for chronic SDH are summarized in Table 1. These cases were not related to high blood pressure, underlying vascular malformation or neoplasm, though postoperative hypertension may have been transient and gone unnoticed. Although cases 1 and case 2 were treated with temporary external ventricular drainage for acute hydrocephalus, the prognosis was generally good. The patient in case 3 had a low platelet count and died due to massive cerebellar hemorrhage after the third evacuation for the treatment of SDH. Our case seemed to be associated with overdrainage of CSF during perioperative period. The patient was fully recovered following bed rest and hydration.
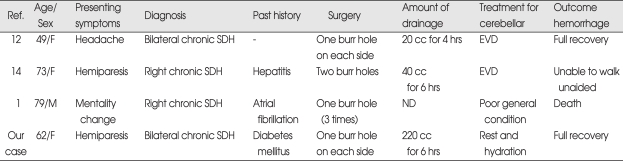
Table 1.
Patient characteristics with cerebellar hemorrahge after burr hole evacuation of chronic subdural hematoma
EVD : extraventricular drainage, ND : not described , Ref. : references, SDH : subdural hematoma
The mechanism of remote cerebellar hemorrhage is unknown, but it is suspected to be multifactorial. The previously proposed mechanisms include intracranial hypotension through removal of the supratentorial mass8), altered coagulation profile, postoperative hypertension15), excessive head rotation coupled with hyperextension leading to obstruction of the ipsilateral jugular vein12), overdrainage of CSF via removal leading to a shift in the intracranial contents with resultant tearing, compression or an increase in the transmural pressure of cerebellar draining veins or cerebellar parenchymal vessels16). It has been considered that stretching of the cerebellum and cerebellar veins, which can occur during surgery that requires brain retraction or excessive CSF loss, may cause transient occlusion of the vermian veins increasing the venous pressure resulting in venous hemorrhage1). Postoperative repositioning of patients with intraand extradural drains maylead to negative intracranial pressure causing a suction effect on the brain and cerebellum. The transtentorial pressure gradient precipitates damage to the draining cerebellar venous system2). Expansion of the CSF spaces, depending on the size of the resection cavity or the size of the drained subdural fluid compartment reduces intracranial pressure and may furthermore cause increased mobility of the intracranial structures.
In our case, a relatively large amount of fluid was drained for 6 hours, and the patient immediately developed a severe headache and vomiting when the drainage system was reopened. The fact that normal angiograms followed this complication suggests that it is not arterial in origin. Further, the thin-walled veins should be more susceptible to indirect injury. Continuous drainage could lead to negative intracranial pressure causing a suction effect on the brain and cerebellum, which seems to be associated with rupture of the small supracerebellar veins and capillary bed with venous bleeding11).
CONCLUSION
We report a case of cerebellar hemorrhage after burr hole drainage of chronic SDH. Although a rare complication, it is necessary to be aware of the possibility of cerebellar hemorrhage after supratentorial surgery, even with limited surgery such as burr hole drainage of a chronic SDH. Cerebellar hemorrhage should be considered when neurological deterioration occurs after evacuation of chronic SDH.
References
- 1.Brisman MH, Bederson JB, Sen CN, Germano IM, Moore F, Post KD. Intracerebral hemorrhage occurring remote from the craniotomy site. Neurosurgery. 1996;39:1114–1121. doi: 10.1097/00006123-199612000-00009. discussion 1121-1122. [DOI] [PubMed] [Google Scholar]
- 2.Honegger J, Zentner J, Spreer J, Carmona H, Schulze-Bonhage A. Cerebellar hemorrhage arising posteratively as a complication of supratentorial surgery : a retrospective study. J Neurosurg. 2002;96:248–254. doi: 10.3171/jns.2002.96.2.0248. [DOI] [PubMed] [Google Scholar]
- 3.Hyam JA, Turner J, Peterson D. Cerebellar haemorrhage after repeated burr hole evacuation for chronic subdural haematoma. J Clin Neurosci. 2007;14:83–86. doi: 10.1016/j.jocn.2005.12.048. [DOI] [PubMed] [Google Scholar]
- 4.Jang JW, Joo SP, Kim JH, Kim SH. Remote cerebellar hemorrhage after supratentorial aneurysmal surgery : report of six cases. J Korean Neurosurg Soc. 2006;39:370–373. [Google Scholar]
- 5.Kalfas IH, Little JR. Postoperative hemorrhage : a survey of 4992 in intracranial procedure. Neurosurgery. 1988;23:343–347. doi: 10.1227/00006123-198809000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan SS, Lauryssen C. Cerebellar haemorrahge after evacuation of an acute supratentorial susbdural haematoma. Br J Neurosurg. 1999;13:329–331. doi: 10.1080/02688699943790. [DOI] [PubMed] [Google Scholar]
- 7.Kim SS, Kim CH, Cheong JH, Kim JM. Massive intracranial hemorrhage following drainage of subdural hygroma. J Korean Neurosurg Soc. 2007;41:261–263. [Google Scholar]
- 8.König A, Laas R, Herrmann HD. Cerebellar hemorrhage as a complication after supratentorial craniotomy. Acta Neurochir (Wien) 1987;88:104–108. doi: 10.1007/BF01404145. [DOI] [PubMed] [Google Scholar]
- 9.Marquardt G, Setzer M, Schick U, Seifert V. Cerebellar hemorrhage after supratentorial craniotomy. Surg Neurol. 2002;57:241–251. doi: 10.1016/s0090-3019(02)00642-0. discussion 251-252. [DOI] [PubMed] [Google Scholar]
- 10.Palmer JD, Sparrow OC, Iannotti F. Post-operative hematoma : a 5-year survey ad identification of avoidable risk factors. Neurosurgery. 1994;35:1061–1064. doi: 10.1227/00006123-199412000-00007. discussion 1064-1065. [DOI] [PubMed] [Google Scholar]
- 11.Papanastassiou V, Kerr R, Adams C. Contralateral cerebellar hemorrhage infarction after pterional craniotomy report of five cases ad review of the literature. Neurosurgery. 1996;39:841–851. doi: 10.1097/00006123-199610000-00040. discussion 851-852. [DOI] [PubMed] [Google Scholar]
- 12.Toczek MT, Morrel MJ, Silverberg GA, Lowe GM. Cerebellar hemorrhage complicating temporal lobectomy, report of four cases. J Neurosurg. 1996;85:718–722. doi: 10.3171/jns.1996.85.4.0718. [DOI] [PubMed] [Google Scholar]
- 13.Tondon A, Mahapatra AK. Supratentorial intracranial haemorrhage following infratentorial surgery. J Clin Neurosci. 2004;11:762–765. doi: 10.1016/j.jocn.2003.10.029. [DOI] [PubMed] [Google Scholar]
- 14.Vogels RL, Verstegen MJ, van Furth WR. Cerebellar haemorrhage after non-traumatic evacuation of supratentorial chronic subdural haematoma : report of two cases. Acta Neurochir (Wien) 2006;148:993–996. doi: 10.1007/s00701-006-0800-y. [DOI] [PubMed] [Google Scholar]
- 15.Yasargil MG, Yonekawa Y. Results of microsurgical extra-intracranial arterial bypass in the treatment of cerebral ischemia. Neurosurgery. 1977;1:22–24. doi: 10.1227/00006123-197707000-00005. [DOI] [PubMed] [Google Scholar]
- 16.Yoshida S, Yonekawa Y, Yamashita K, Ihara I, Morooka Y. Cerebellar hemorrhage after supratentorial craniotomy, report of three cases. Neurol Med Chir (Tokyo) 1990;30:738–743. doi: 10.2176/nmc.30.738. [DOI] [PubMed] [Google Scholar]