Abstract
This study examined the impact of prison-initiated methadone maintenance at 12-months post-release. Males with pre-incarceration heroin dependence (n=204) were randomly assigned to: 1) Counseling Only: counseling in prison, with passive referral to treatment upon release; 2) Counseling+Transfer: counseling in prison with transfer to methadone maintenance treatment upon release; and 3) Counseling+Methadone: counseling and methadone maintenance in prison, continued in the community upon release. The mean number of days in community-based drug abuse treatment were, respectively, Counseling Only 23.1, Counseling+Transfer 91.3, and Counseling+Methadone 166.0, p <.01; all pairwise comparisons were statistically significant (all ps < .01). Counseling+Methadone participants were also significantly less likely than participants in each of the other two groups to be opioid-positive or cocaine-positive according to urine drug testing. These results support the effectiveness of prison-initiated methadone for males in the United States. Further study is required to confirm the findings for women.
Keywords: Methadone maintenance, Prison, Substance abuse treatment
1. Introduction
Despite extensive evidence of methadone maintenance treatment’s effectiveness in community settings (Ball & Ross, 1991; Johnson et al., 2000; Joseph, Stancliff, & Langrod, 2000; Platt, Widman, Lidz, & Marlowe, 1998; Schwartz et al., 2006) and its widespread use in prisons throughout the world [European Monitoring Centre for Drugs and Drug Addiction (EMCDDA); 2002; Jurgens, 2004; McSweeney, Turnbull, & Hough, 2002], methadone maintenance treatment has rarely been used with individuals who are exiting correctional institutions in the United States. In the jail setting, initiating heroin-dependent individuals on methadone maintenance and maintaining arrestees already enrolled in drug treatment programs has been found effective through years of practice in New York City (Dole et al., 1969; Magura, Rosenblum, Lewis, & Joseph, 1993; Tomasino, Swanson, Nolan, & Shuman, 2001). Initiating prisoners who are not currently heroin dependent or are not receiving methadone treatment but who have a history of severe heroin addiction prior to incarceration on maintenance treatment prior to release is a promising intervention that warrants research to determine its effectiveness. Such research is urgently needed because relapse to heroin addiction typically occurs within one month of release (Kinlock, Battjes, & Schwartz, 2002; Maddux & Desmond, 1981; Nurco, Hanlon, & Kinlock, 1991), the opportunity to engage newly released individuals in treatment is greatly diminished upon re-addiction (Inciardi, McBride, & Surratt, 1998; Smith-Rohrberg, Bruce, & Altice, 2004), and the life-threatening adverse consequences associated with heroin addiction, such as overdose (Binswanger et al., 2007; Bird & Hutchinson, 2003; Farrell & Marsden, 2008; Stewart, Henderson, Hobbs, Ridout, & Knuiman, 2004), human immunodeficiency virus [(HIV; Centers for Disease Control (CDC; 2006); Chitwood, Comerford, & Weatherby, 1998]; and hepatitis B and C infections (Edlin, 2002; Mark, Woody, Juday, & Kleber, 2001) are substantial.
In contrast to the United States, a number of other countries have routinely offered methadone maintenance treatment in prisons and jails (Kerr & Jurgens, 2004). Perhaps the most rigorously evaluated of these prison-based methadone maintenance programs has been the one initiated in a pre-release facility in 1986 by the New South Wales Department of Correction for inmates with a pre-incarceration history of heroin addiction (Gorta, 1992). A randomized controlled trial of this methadone program as compared to wait list for the program in prison showed that heroin use was lower among treated participants during a four month in-prison follow-up (Dolan et al., 2003). A four-year follow-up of the study cohort found that retention in treatment was associated with decreases in mortality, re-incarceration, and hepatitis C infection (Dolan et al., 2005).
The present study is, to our knowledge, the first randomized clinical trial in the United States to examine the efficacy of prison- (as opposed to jail-) initiated methadone treatment (Kinlock, Schwartz, & Gordon, 2005). It was conducted to assess the extent to which initiating methadone in prison prior to release with continued treatment in the community would be more efficacious than initiating methadone treatment in the community or simply providing counseling in prison with a passive referral to treatment upon release. Short-term results at 1- and 3-months (Kinlock et al., 2007; Kinlock, Gordon, Schwartz, & O’Grady, 2008) post-release and longer-term findings at 6-months post-release (Gordon, Kinlock, Schwartz, & O’Grady, 2008) showed that prison-initiated and community-initiated methadone treatment were more effective than counseling only in terms of heroin use and treatment entry. While these findings are encouraging, considerable evidence exists indicating that continuous enrollment for at least 12 months is needed to produce long-term behavioral change in methadone maintenance treatment (Greenfield & Fountain, 2000; Joe, Simpson, & Broome, 1999; MacGowan et al., 1996; Moolchan & Hoffman, 1994). The present report, representing the main outcome paper, provides more comprehensive, longer-term findings at 12-months post-release.
2. Methods
Study methods were described in detail elsewhere (Kinlock et al., 2007). In brief, all participants met criteria for methadone treatment in the year prior to incarceration, received an individual counseling intake and a physical examination and were scheduled to receive, within treatment condition, 12 weekly sessions of drug abuse education in prison. Immediately prior to release, all participants were scheduled to meet with the study’s counselor individually to discuss plans for release. Counseling Only participants were advised by treatment staff at release to seek drug abuse treatment in the community in any of the publicly funded programs in Baltimore according to standard admission procedures. Counseling+Transfer participants were informed by treatment staff at release to report to the program’s community-based facility within 10 days to begin methadone at 5 mg with increases of 5 mg every eighth day to a target minimum dose of 60 mg. Participants in the Counseling+Methadone condition began methadone at 5 mg and increased 5 mg every eighth day during incarceration to a target dose of 60 mg. They were advised upon release to report to the program’s community-based facility within 10 days for continuing care. These low initial doses and slow dose increases were utilized because participants were not tolerant to opioids at the time of dose induction.
Participants were assessed five times during the course of the study; at baseline (study entry), and at 1-, 3-, 6-, and 12-months post-release. Baseline assessments included the Addiction Severity Index (ASI; McLellan et al., 1992), which assesses problem severity in seven areas: alcohol use, drug use, medical, psychiatric, family/social, employment, and legal functioning. Post-release assessments at each follow-up point involved drug abuse treatment record review; a urine drug test for opioids and cocaine; and a confidential, semi-structured interview addressing substance abuse treatment and incarceration history, heroin use, cocaine use, and criminal activity (Hanlon, Nurco, Kinlock, & Duszynski, 1990; Nurco, 1998). Participants were paid $20 for each post-release assessment that they completed. The study was approved by the Friends Research Institute’s Institutional Review Board.
2.1. Outcome Measures
The three primary outcome measures examined at the twelve-month follow-up period were: 1) the number of days enrolled in drug abuse treatment in the community; and urine test results for 2) opioids; and 3) cocaine. The secondary outcome measures were: the frequency, or number of days in the past 365 days [adjusted for days at risk in the community], that the participant reported: 4) using heroin; 5) using cocaine; and 6) committing crime. Two additional secondary outcome measures were examined: 7) arrested (yes v. no) during the 12-month post-release follow-up period; and 8) number of days employed during the past 30 days at the end of the study (12-months post-release). Data on drug abuse treatment status were obtained from treatment program records and participant self-report. Urine samples were tested using the enzyme-multiplied immunoassay technique for opioids (excluding methadone) and cocaine, with cutoff calibration concentrations of 300 μg/mL for morphine and benzoylecgonine. Data on the frequency of heroin days, cocaine days, and crime days were obtained using the ASI and the above-mentioned supplemental questionnaire. Arrest data were obtained from records maintained by the Maryland Department of Public Safety and Correctional Services. Data on the number of days employed were obtained from the ASI.
2.2. Statistical Analysis
The targeted number of participants was 240. A power analysis for the Poisson regression analysis indicated that 80 prisoners in each group would be needed to detect a “small-to-medium” effect size (f2 = .058) with 90% power in an intent-to-treat analysis. Results of a subsequent power analysis conducted for the Poisson regression analysis for the final sample size of 204, the number of participants enrolled in the trial, found that this sample size still provided 90% power to detect a “small-to-medium” (f2 = .070) effect. Poisson regression analysis (McCullough & Nelder, 1989) was used to compare the three treatment conditions on the number of days enrolled in drug abuse treatment in the community, the number of days used heroin, the number of days used cocaine, the number of days committed crime, and the number of days employed because these variables represented counts. Logistic regression analysis (Agresti, 1990; Hosmer & Lemeshow, 1989) was used to compare the three treatment conditions on the relative number of opioid-positive and cocaine-positive urine samples as well as the relative number of participants arrested. In each of the regression analyses, a small set of control variables was included because of the relatively small sample size. Behavioral variables that had predicted responsiveness to treatment in prior research with drug-involved offenders were included, such as age at first crime (Hanlon, Nurco, Bateman, & O’Grady, 1998; Hiller, Knight, & Simpson, 1999; Kinlock, Battjes, & Schwartz, 2005), having a history of prior cocaine use (Magura, Nwakese, & Demsky, 1998; Rowan-Szal, Chatham, & Simpson, 2000), and completed prison treatment (Butzin, Martin, & Inciardi, 2002; Prendergast & Wexler, 2004). Control variables in each regression analysis included age, age at first crime, prior cocaine use (the number of self-reported days of cocaine use in the 30 days in the community before the index incarceration), completed prison treatment as part of the current intervention (yes v. no), and length of baseline (index) incarceration. For the analysis of each outcome variable, the predictor variable of primary interest, treatment condition, and the control variables were entered simultaneously. Pairwise comparisons between the different treatment conditions were conducted following the detection of a significant treatment condition effect. All analyses were conducted on an intent-to-treat basis.
3. Results
3.1. Participant Characteristics
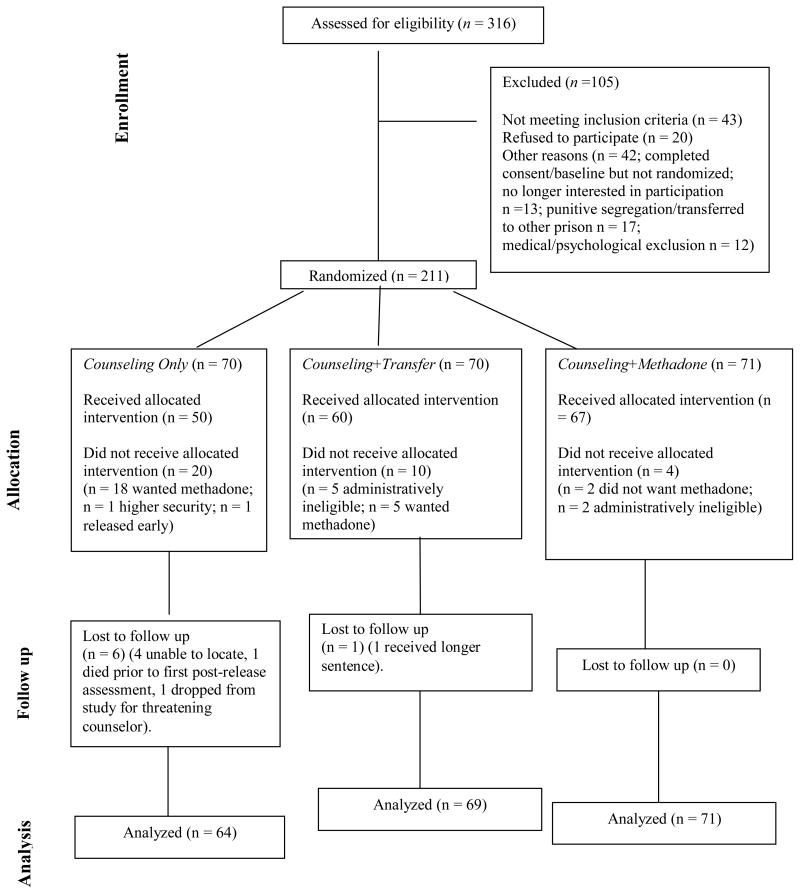
Data on twelve-month outcomes were obtained on 204, or 96.7% of the 211 randomized participants; 64 of 70 (91.4%) in the Counseling Only condition, 69 of 70 (98.6%) in the Counseling+Transfer condition, and 71 of 71 (100.0%) in the Counseling+Methadone condition (Figure 1). The 204 participants were, on average, 40.3 (SD = 7.1) years of age; 69.6% were African American, 24.0% were Caucasian, and 6.4% were other ethnicity; 70.6 % had one or more prior substance abuse treatment episodes; whereas 23.0% had one or more previous episodes of methadone maintenance treatment (Table 1). The 204 participants were, on average, 18.5 (SD = 5.0) years of age at first heroin use; the mean number of days used heroin in the 30 days before their index incarceration was 27.2 (SD = 5.0). At study entry, participants had a mean duration of incarceration of 604.5 days (SD = 589.1 days). There was only one statistically significant difference (p < .05) between treatment conditions on the above variables, namely, length of baseline incarceration (p = .01), wherein the Counseling+Methadone group was incarcerated for a longer period of time than the Counseling Only group.
Figure 1.
Consort Diagram of Recruitment
Table 1.
Sample Characteristics (N = 204)
| Categorical Variables n (%) | Counseling Only (n = 64) | Counseling+Transfer (n = 69) | Counseling+Methadone (n = 71) |
|---|---|---|---|
| Race | |||
| African American | 41 (64.1) | 51 (73.9) | 50 (70.4) |
| Caucasian | 21 (32.8) | 13 (18.8) | 15 (21.1) |
| Other | 2 (3.1) | 5 (7.2) | 6 (8.5) |
| Prior drug treatment | 44 (68.8) | 48 (69.6) | 52 (73.2) |
| Prior methadone treatment | 15 (23.4) | 17 (24.6) | 15 (21.1) |
| Continuous Variables Mean (SD) | |||
| Age | 40.7 (7.5) | 40.3 (6.7) | 39.9 (7.0) |
| Age first heroin use | 19.1 (5.3) | 18.5 (4.8) | 18.0 (4.8) |
| Heroin use daysa | 27.1 (7.8) | 27.8 (6.1) | 26.7 (8.9) |
| Lifetime incarcerated, yrs | 7.3 (5.1) | 6.1 (4.2) | 7.5 (5.4) |
| Length of Current Incarcerationb,c months | 464.8 (487.7) | 569.5 (577.4) | 764.5 (650.7) |
Past 30 days in the community prior to the current incarceration.
Calculated from current incarceration until release from prison.
Counseling Only v. Counseling+Methadone, p < .05.
3.2 Primary Outcomes
3.2.1. Community Treatment Duration
Results of treatment duration over the 12-month post-release follow-up period are shown in Table 2. The three treatment conditions were significantly different. The mean number of days that participants in each condition were enrolled in community based treatment were, respectively, Counseling Only 23.1 (SD = 72.5), Counseling+Transfer 91.3 (SD = 144.6), and Counseling+Methadone 166.0 (SD = 166.4). All pairwise comparisons were statistically significant (all ps < .01). Notably, none of the Counseling Only (25% entered treatment) participants were in treatment for 365 days, while 17.3 % of Counseling+Transfer (53.6% entered treatment) and 36.7 % of Counseling+Methadone (70.4% entered treatment) participants were in treatment for one year. As expected, failure to complete study-provided prison treatment was significantly associated with shorter duration of treatment in the community (p = .0001).
Table 2.
Results of Poisson Regression Analyses of Days Retained in Treatment
| χ2 | p | SE | |
|---|---|---|---|
| Condition | |||
| CO vs. C+T | 9.848 | .002 | 3.599 |
| CO vs. C+M | 27.314 | .0001 | .345 |
| C+M vs. C+T | 11.791 | .001 | .196 |
| Age | 3.371 | .066 | .013 |
| Age First Crime | 1.936 | .164 | .018 |
| Cocaine Days Baseline | 1.552 | .213 | .007 |
| Completed Prison Treatment | 16.651 | .0001 | .344 |
| Incarceration Days Baseline | .046 | .830 | .000 |
Overall model: [χ 2 = 13465.7; p = .0001]
χ 2 is the Wald test.
SE = the standard error.
3.2.2. Urine Opioid Drug Test Results
Urine samples were not obtained on 89 of the 204 participants because of incarceration, hospitalization, being located out of the Baltimore area and interviewed by telephone, or being interviewed more than two months after their due date for the scheduled interview. Results of urine opioid testing at the 12-month post-release follow-up period are shown in Table 3. There were significant differences in the percentage of participants in each condition who tested positive for opioids at 12-months post-release [χ2 (df = 2) = 12.7; p = .002]. The percentage of participants in each condition who were opioid-positive were, Counseling Only, 65.6% (n = 32), Counseling+Transfer, 48.7%, (n = 39) and Counseling+Methadone, 25.0 % (n = 44). Regarding pairwise differences, the Counseling Only group (p = .001) and Counseling+Transfer group (p = .008) were significantly more likely to be opioid-positive than the Counseling+Methadone group. There were no significant differences between the Counseling Only group and the Counseling+Transfer group. None of the other predictor variables were statistically significant.
Table 3.
Results of Logistic Regression Analyses at 12-Months Post-Release Urine Tests
| Opioidsa |
Cocaineb |
|||
|---|---|---|---|---|
| OR | 95%CI | OR | 95%CI | |
| Condition | ||||
| CO vs. C+T | .572 | .200–1.638 | .479 | .149–1.539 |
| CO vs. C+M | 7.074*** | 2.301–21.744 | 7.066*** | 2.198–22.716 |
| C+M vs. C+T | 4.046** | 1.446–11.318 | 3.384* | 1.250–9.161 |
| Age | .987 | .922–1.056 | 1.048 | .981–1.119 |
| Age First Crime | 1.011 | .931–1.097 | .940 | .867–1.019 |
| Cocaine Days Baseline | .987 | .957–1.017 | .995 | .965–1.026 |
| Completed Prison Treatment | 1.703 | .651–4.452 | .503 | .187–1.355 |
| Incarceration Days Baseline | 1.001 | 1.000-.1.001 | 1.001 | 1.000–1.002 |
OR = odds ratio.
CO = Counseling Only; C+T = Counseling+Transfer; C+M = Counseling+Methadone.
Omnibus Test χ2 = 18.90; p = .009
Omnibus Test χ2 = 17.23; p = .016
p < .05;
p < .01;
p < .001.
Note. Number of urinalyses obtained: CO, n = 32; C+T, n = 39; C+M, n = 44.
3.2.3. Urine Cocaine Drug Test Results
Results of urine cocaine testing at the 12-month post-release follow-up period are shown in Table 3. There were significant differences in the percentage of participants in each condition who tested positive for cocaine at 12-months post-release. Regarding pairwise comparisons, the Counseling Only (71.9%) and Counseling+Transfer (66.6%) were more likely to be cocaine -positive at 12-months post-release compared to the Counseling+Methadone (43.2%) group, ps < .001 and < .05 respectively, while the former two groups were not significantly different from each other. None of the other predictor variables were statistically significant.
3.3. Secondary Outcomes
3.3.1. Heroin use days
The reported number of days of heroin use in the past 365 days post-release was significantly predicted by the set of six predictor variables (p < .0001). Although not statistically significant, the pattern of results regarding treatment condition was in the predicted direction with Counseling Only (M = 167.1; SD = 132.7) reporting more days of use compared to Counseling+Transfer (M = 120.7; SD = 114.8) and Counseling+Methadone (M = 106.2; SD = 133.5). However, none of the other predictor variables were significant.
3.3.2. Cocaine use days
Reported cocaine use in the past 365 days post-release was significantly predicted by the set of six predictor variables (p < .0001). As might be expected, higher levels of self-reported cocaine use in the 30 days prior to the current incarceration was related to reporting having used cocaine more frequently at 12 months post-release (p = .0001). Although not statistically significant, the pattern of results regarding treatment condition was in the predicted direction with Counseling Only (M = 76.9; SD = 83.4) reporting more days of use compared to Counseling+Transfer (M = 53.2; SD = 82.5) and Counseling Methadone (M = 37.2; SD = 60.1). None of the other predictor variables were significant.
3.3.3. Criminal Activity
The reported number of days of criminal activity in the past 365 days post-release was significantly predicted by the set of six predictor variables (p < .0001). Although not statistically significant, the pattern of results regarding treatment condition was in the predicted direction with Counseling Only (M = 106.7; SD = 128.7) reporting more days of criminal activity compared to Counseling+Transfer (M = 65.2; SD = 96.2) and Counseling+Methadone (M =81.8; SD = 109.5). Also, none of the other predictor variables were significant.
3.3.4. Arrests
Results of logistic regression analyses regarding any arrests during the post-release follow-up period indicated there were no significant differences between conditions. The percentage of participants in each treatment condition who were arrested during the 12-month post-release follow-up period were, respectively, Counseling Only, 50.8%; Counseling+Transfer, 59.1%, and Counseling+Methadone, 52.9%. The only significant control variable was age (p = .025), indicating that older participants were less likely to be arrested during the 12-months post-release.
3.3.5. Employment
The reported number of days employed during the past 30 days was significantly predicted by the set of six predictor variables (p < .0001). However, treatment condition was not significant, nor was any other predictor variable. The mean (SD) of days employed in the last 30 days reported by participants in each condition were, respectively, Counseling Only, 12.0 (10.3); Counseling+Transfer, 10.3 (10.9); and Counseling + Methadone, 8.5 (10.5).
4.0. Serious Adverse Events
There were 51 serious adverse events (SAEs). Forty-three were hospitalizations (9 in the Counseling Only, 14 in the Counseling+Transfer, and 20 in the Counseling+Methadone condition). Only two of the SAEs (brief hospitalizations for constipation—one each in the Counseling+Transfer and Counseling+Methadone groups)—were considered possibly-related to study participation. There were eight deaths. Of these, six occurred to Counseling Only participants [four opioid overdoses—two involving heroin, one involving illicitly obtained methadone (the participant was not enrolled in a methadone program at the time of his death), and one involving fentanyl] and two deaths from cardiovascular disease. One Counseling+Transfer participant died from AIDS and one Counseling+Methadone participant died of cardiovascular disease. Neither of the latter two participants was enrolled in methadone treatment at the time of death.
5. Discussion
The present study is the first randomized clinical trial evaluating the effectiveness of methadone maintenance treatment provided to U.S. prisoners with pre-incarceration histories of heroin addiction. Perhaps the most striking and promising finding involves the differences between treatment conditions with regard to the number of days participants spent in community-based drug abuse treatment. Results showed that prison-initiated methadone maintenance treatment was associated with greater duration of treatment in the community during the 12 months post-prison release compared to counseling in prison with passive referral at release or counseling in prison with initiation of methadone treatment admission upon release. Compared to Counseling Only participants, participants who received methadone in prison spent seven times as many days in drug abuse treatment during the year following release.
Furthermore, none of the Counseling Only participants spent the entire post-release year in treatment compared to approximately 37% of Counseling+Methadone participants. The present results extend those found on the present sample at 6-months post-release (Gordon et al., 2008) and also support and extend the findings of Doleet al. (1969). These findings at 12-months post-release may have significant public health and public policy implications because greater treatment retention for heroin-dependent individuals has been found to be related to reduced heroin use (Anglin, 1988; Hser, Hoffman, Grella, & Anglin, 2001; Leukefeld, Tims, & Farabee, 2002).
Regarding urine opioid drug test results, Counseling Only participants were significantly more likely than Counseling+Methadone participants to test positive for opioids at 12-months post-release. At 12-months post-release, there was also a difference between methadone initiated in prison and upon release, with the former condition having the superior outcome. While differences at 1- and 6- months post-release regarding the present sample also indicated that Counseling Only participants were over twice as likely to be opioid-positive according to urine drug testing than Counseling+Methadone participants (see Gordon et al., 2008; Kinlock et al., 2007), these 12-month results differ from those reported at earlier follow-up points which showed no differences between the Counseling+Methadone and Counseling+Transfer conditions. These findings appear encouraging given that reductions in heroin use have been found to be related to fewer adverse health (CDC, 2006; Edlin, 2002; Mark et al., 2001; Weatherburn & Lind, 1999) and criminogenic consequences (Chaiken & Chaiken, 1990; Kinlock, O’Grady, & Hanlon, 2003). However, enthusiasm for this finding is tempered somewhat by the number of respondents on which urine samples at 12-months post-release were not obtained.
In view of the fact that methadone treatment has been shown to be more effective in treating opioid use than cocaine use (Platt et al., 1998; Schwartz et al., 2006), it seems encouraging that cocaine use as assessed by urine testing differed among the three treatment groups at 12-months post-release. The observation that the Counseling+Methadone group were significantly less likely to be cocaine-positive by at 12-months post-release than either the Counseling Only and Counseling+Transfer groups is consistent with the finding that longer-term methadone treatment duration, in some instances, has been found to be associated with reduced cocaine use in addition to reduced heroin use (Platt et al., 1998). Furthermore, the 12-month follow-up point was the only period among the four post-release assessment points that showed a significant difference by condition in the proportion of cocaine-positive urine samples (Gordon et al., 2008; Kinlock et al., 2007, 2008). Perhaps the longer duration of treatment on the part of the Counseling+Methadone participants contributed to this finding. However, as noted above with regard to the results on opioid-positive urine testing, these results appear more tentative than conclusive because of the number of missing values at 12-months post-release.
In contrast to findings regarding urine testing, the three treatment conditions did not significantly differ with regard to self-reported measures of heroin use, cocaine use, or criminal activity during the 12-month post-release period, although the pattern of results were in the predicted direction. Such findings were not observed at six-month post-release, which indicated that the number of days reported by the Counseling+Methadone participants on all three measures was significantly lower than those reported by the Counseling Only participants (Gordon et al., 2008). Concerning self-reported criminal activity, consistent with the present results, Magura et al. (1993) found no significant differences between KEEP participants and a comparison group of untreated inmates with regard to the mean number of days engaged in property crime at follow-up, an average of 6.5 months post-release. Furthermore, in the present study, there were no significant differences by treatment condition with regard to two additional secondary outcomes that were not examined previously: the percentage of participants arrested over the 12-month period or on the number of days employed at the end of that 12-month period. The present findings regarding arrests were similar to those of two prior studies involving prison-initiated opioid agonist maintenance. The initial evaluation of the New South Wales program (Hume & Gorta, 1989) found no significant differences between inmates who had received methadone maintenance in prison and a comparison group in terms of being charged in court or reconvicted at follow-up, an average of 12.9 months following release. A small-scale study of opioid agonist maintenance examining Levo-alpha-acetylmethadol (LAAM) prior to prison release found no significant differences with regard to being arrested between participants who received LAAM and a control group at nine-months post-release (Kinlock, Battjes, & Schwartz, 2005).
However, these findings are in contrast to the pilot study conducted in New York by Dole et al. (1969). The latter found that only 3 of 12 prisoners who started on methadone prior to release were convicted of new crimes during an 11.5 month follow-up as compared to 15 of 16 prisoners randomly assigned to a control condition.
Previous research indicates that drug dependent prisoners are at high risk of overdose death following release to the community (Binswanger et al., 2007; Bird & Hutchinson, 2003; Farrell & Marsden, 2008; Stewart et al., 2004). Dolan et al. (2005) found that 17 of 382 participants died from overdose during the 4 year follow-up period while not enrolled in methadone treatment while none of the participants died while enrolled in treatment. In the present study, there were no overdose deaths in either the Counseling+Methadone and Counseling+Transfer conditions, while four such deaths occurred to Counseling Only participants during the 12-month follow-up period at 1, 3, 6, and 12 months post-release. Because only one of these deaths occurred during active participant enrollment, and out-of-treatment participants who wanted treatment were given referrals, recruitment in that study condition was not discontinued.
Participants in the present study were not tolerant to opioids at the time of methadone initiation. Thus, induction started at a low dose and proceeded slowly. Dole et al. (1969) also reported starting pre-release jail inmates (who were presumably non-tolerant also) at a lower methadone dose than customary (10 mg) with a slow dose increase. Because the first two participants in the present study reported excessive drowsiness at 10 mg, the protocol was changed to begin at 5 mg. This dose induction schedule was well tolerated although constipation was a fairly frequent side effect during induction and the maintenance phase.
This study has several limitations. A more precise comparison of the effects of treatment condition on opioid and cocaine drug testing results was not possible because such data were not obtained on all 204 participants because of incarceration, hospitalization, being located out of the Baltimore area and interviewed by telephone, or being interviewed more than 2 months after their due date.
The results may not be generalizable to female prisoners or to prison inmates from other geographic locations because the sample exclusively involved male prisoners from Baltimore. However, methadone treatment is effective in both men and women (Greenfield et al., 2007; Peles & Adelson, 2006; Platt et al., 1998) and has been shown to be effective in studies throughout the world (Gossop, 2006; Michels, Stover, & Gerlach., 2007; Pang et al., 2007; Peles & Adelson, 2006; Platt et al., 1998). The results regarding arrest may not be generalizable to other cities, which may have markedly different arrest rates and/or policing strategies than Baltimore. Furthermore, the comparison of the present findings regarding post-release arrest with previous studies of the effects of prison-initiated opioid agonist maintenance, cited above, need to be interpreted with caution because of differences in the type of criminal justice sanction (e.g., arrest, conviction, being charged in court), nationality and ethnicity of participants, and type of opioid agonist administered.
Despite these limitations, this study confirms and extends the findings of Dole et al. (1969), Dolan et al. (2003, 2005) and of the longstanding methadone program in the New York City jail (Magura et al., 1993; Tomasino et al., 2001). These studies and experiences in other countries throughout the world indicate that is quite feasible and effective to provide opioid agonist therapy to inmates with heroin addiction histories. The World Health Organization has listed methadone as an essential medication and has strongly recommended that methadone treatment in prison should be available in countries where methadone treatment is available in the community in order to significantly reduce the likelihood of adverse health and criminogenic consequences (Herget, 2005). Results suggest that the current intervention may be able to meet an urgent public health need in ensuring a continuum of drug abuse treatment spanning the institution and the community.
Acknowledgments
This study was funded by the National Institute on Drug Abuse (NIDA), Grant R01 DA 16237 (PI: Timothy W. Kinlock, Ph.D). Limited portions of this manuscript were presented at the American Society of Criminology annual meeting in November, 2007 and the College on Problems of Drug Dependence Annual Meeting in June, 2008. The views expressed in this article are those of the authors and do not necessarily represent the opinion of the National Institute on Drug Abuse or the National Institutes of Health. We wish to thank Redonna K. Chandler, Ph.D., Chief, Services Research Branch, Division of Epidemiology, Services, and Prevention Research at NIDA as well as Akiva Liberman, Ph.D., also of the Division of Epidemiology, Services, and Prevention Research at NIDA. The authors would also like to thank the Maryland Department of Public Safety and Correctional Services, specifically Gregory Warren, former Director of Substance Abuse Treatment Services; and the staff of the Metropolitan Transition Center, particularly Gary Hornbaker, Warden; Kendall Gifford, Case Management Manager, and Andrew Stritch, Audit Coordinator; the research participants, the staff of Man Alive Research, specifically Karen Reese, Director, Gary Sweeney, Program Manager and Robin Ingram, Project Nurse. In addition, we would like to thank the project staff at the Social Research Center; Kathryn Couvillion, Bernard Fowlkes, Donnette Randolph, and Melissa Harris for their efforts related to this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agresti A. Categorical data analysis. New York: Wiley; 1990. [Google Scholar]
- Anglin MD. The efficacy of civil commitment in treating narcotic addiction. National Institute on Drug Abuse Research Monograph. 1988;86:8–34. [PubMed] [Google Scholar]
- Ball JC, Ross A. The effectiveness of methadone maintenance treatment: patients, programs, services, and outcomes. New York, NY: Springer; 1991. [Google Scholar]
- Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, Koepsell TD. Release from prison a high risk of death for former inmates. New England Journal of Medicine. 2007;356:157–165. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird SM, Hutchinson SJ. Male drugs-related deaths in the fortnight after release from prison, Scotland, 1996–99. Addiction. 2003;98:185–190. doi: 10.1046/j.1360-0443.2003.00264.x. [DOI] [PubMed] [Google Scholar]
- Butzin CA, Martin SS, Inciardi JA. Evaluating component effects of a prison-based treatment continuum. Journal of Substance Abuse Treatment. 2002;22:63–99. doi: 10.1016/s0740-5472(01)00216-1. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control. Epidemiology of HIV/AIDS-United States, 1981. Morbidity and Mortality Weekly Reports. 2006;55:589–592. [Google Scholar]
- Chaiken JM, Chaiken MR. Drugs and predatory crime. In: Tonry M, Wilson JQ, editors. Drugs and crime: crime and justice: A Review of Research. Vol. 13. Chicago: University of Chicago Press; 1990. pp. 203–219. [Google Scholar]
- Chitwood D, Comerford M, Weatherby N. The initiation and use of heroin in the age of crack. In: Inciardi JA, Harrison LD, editors. Heroin in the age of crack-cocaine. Thousand Oaks, CA: Sage; 1998. pp. 51–76. [Google Scholar]
- Dolan KA, Shearer J, MacDonald M, Mattick RP, Hall W, Wodak AD. A randomized controlled trial of methadone maintenance treatment versus wait list control in an Australian prison system. Drug and Alcohol Dependence. 2003;72:59–65. doi: 10.1016/s0376-8716(03)00187-x. [DOI] [PubMed] [Google Scholar]
- Dolan KA, Shearer J, White B, Zhou J, Kaldor J, Wodak A. Four-year follow-up of imprisoned male heroin users and methadone treatment: mortality, re-incarceration, and hepatitis C infection. Addiction. 2005;100(6):820–828. doi: 10.1111/j.1360-0443.2005.01050.x. [DOI] [PubMed] [Google Scholar]
- Dole V, Robinson J, Orraga J, Towns E, Searcy P, Caine E. Methadone treatment of randomly selected criminal addicts. New England Journal of Medicine. 1969;280:1372–1375. doi: 10.1056/NEJM196906192802502. [DOI] [PubMed] [Google Scholar]
- Edlin BR. Prevention and treatment of hepatitis C in injection drug users. Hepatology. 2002;36:S210–S219. doi: 10.1053/jhep.2002.36809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) EMCDDA annual report. Brussels: Author; 2002. [Google Scholar]
- Farrell M, Marsden J. Acute risk of drug-related death among newly released prisoners in England and Wales. Addiction. 2008;103:251–255. doi: 10.1111/j.1360-0443.2007.02081.x. [DOI] [PubMed] [Google Scholar]
- Gordon MS, Kinlock TW, Schwartz RP, O’Grady KE. A randomized clinical trial of methadone maintenance for prisoners: findings at 6-months post-release. Addiction. 2008;103:1333–1342. doi: 10.1111/j.1360-0443.2008.002238.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorta A. Research Publication No. 25. New South Wales Department of Corrective Services; 1992. Nov, Monitoring the New South Wales methadone program: 1986–1991. [Google Scholar]
- Gossop M. Treating drug misuse problems: evidence of effectiveness. London: National Treatment Agency for Substance Misuse; 2006. [Google Scholar]
- Greenfield L, Fountain D. Influence of time in treatment and follow-up duration on methadone treatment outcomes. Journal of Psychopathology and Behavioral Assessment. 2000;22:353–364. [Google Scholar]
- Greenfield SF, Brooks AJ, Gordon SM, Green CA, Kropp F, McHugh RK, Lincoln M, Hien D, Miele GM. Substance abuse treatment entry, retention, and outcome in women: a review of the literature. Drug and Alcohol Dependence. 2007;86:1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanlon TE, Nurco DN, Bateman RW, O’Grady KE. The response of drug abuser parolees to a combination of treatment and intensive supervision. The Prison Journal. 1998;78:31–44. [Google Scholar]
- Hanlon TE, Nurco DN, Kinlock TW, Duszynski KR. Trends in criminal activity and drug use over an addiction career. American Journal of Drug and Alcohol Abuse. 1990;16:223–228. doi: 10.3109/00952999009001585. [DOI] [PubMed] [Google Scholar]
- Herget G. Methadone and buprenorphine added to the WHO list of essential medicines. HIV AIDS Policy Law Review. 2005;10:23–24. [PubMed] [Google Scholar]
- Hiller ML, Knight K, Simpson DD. Risk factors that predict dropout from corrections-based treatment for drug abuse. The Prison Journal. 1999;79:411–30. [Google Scholar]
- Hosmer D, Lemeshow S. Applied logistic regression. New York: Wiley; 1989. [Google Scholar]
- Hser YI, Hoffman V, Grella CE, Anglin MD. A 33-year follow-up of narcotics addicts. Archives of General Psychiatry. 2001;58:503–508. doi: 10.1001/archpsyc.58.5.503. [DOI] [PubMed] [Google Scholar]
- Hume S, Gorta A. Evaluation of the NSW Department of Corrective Services Prison Methadone Program. Sydney: Research and Statistics Division, New South Wales Department of Corrective Services; 1989. The effects of the NSW prison methadone program on criminal recidivism and retention in methadone treatment. Study No. 7. [Google Scholar]
- Inciardi JA, McBride D, Surratt H. The heroin street addict: profiling a national population. In: Inciardi JA, Harrison LD, editors. Heroin in the age of crack-cocaine. Thousand Oaks, CA: Sage; 1998. pp. 31–50. [Google Scholar]
- Joe GW, Simpson DD, Broome KM. Retention and patient engagement models for different treatment modalities in DATOS. Drug and Alcohol Dependence. 1999;57:113–125. doi: 10.1016/s0376-8716(99)00088-5. [DOI] [PubMed] [Google Scholar]
- Johnson RE, Chutuape MA, Strain EC, Walsh SL, Stitzer ML, Bigelow GE. A comparison of levomethadyl acetate, buprenorphine, and methadone for opioid dependence. New England Journal of Medicine. 2000;343:1290–1297. doi: 10.1056/NEJM200011023431802. [DOI] [PubMed] [Google Scholar]
- Joseph H, Stancliff S, Langrod J. Methadone Maintenance Treatment (MMT): a review of historical and clinical issues. Mount Sinai Journal of Medicine. 2000;67:347–364. [PubMed] [Google Scholar]
- Jurgens R. Is the world finally waking up to HIV/AIDS in prisons? Infectious Disease in Corrections Report. 2004 September;7(9) [Google Scholar]
- Kerr T, Jurgens R. Methadone maintenance therapy in prisons: reviewing the evidence. Montreal: Canadian HIV/AIDS Legal Network; 2004. [Google Scholar]
- Kinlock TW, Battjes RJ, Schwartz RP. A novel opioid maintenance program for prisoners: preliminary findings. Journal of Substance Abuse Treatment. 2002;22:141–147. doi: 10.1016/s0740-5472(02)00226-x. [DOI] [PubMed] [Google Scholar]
- Kinlock TW, Battjes RJ, Schwartz RP. A novel opioid maintenance treatment program for prisoners: report of post-release outcomes. American Journal of Drug and Alcohol Abuse. 2005;31:433–454. doi: 10.1081/ada-200056804. [DOI] [PubMed] [Google Scholar]
- Kinlock TW, Gordon MS, Schwartz RP, O’Grady KE. A study of methadone maintenance for male prisoners: 3-month post-release outcomes. Criminal Justice and Behavior. 2008;35:34–47. doi: 10.1177/0093854807309111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinlock TW, Gordon MS, Schwartz RP, O’Grady KE, Fitzgerald T, Wilson M. A randomized clinical trial of methadone maintenance for prisoners: results at 1-month post-release. Drug and Alcohol Dependence. 2007;91:220–227. doi: 10.1016/j.drugalcdep.2007.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinlock TW, O’Grady KE, Hanlon TE. Prediction of the criminal activity of incarcerated drug-abusing offenders. Journal of Drug Issues. 2003;33:897–920. [Google Scholar]
- Kinlock TW, Schwartz RP, Gordon MS. The significance of interagency collaboration in developing opioid agonist programs for inmates. Corrections Compendium. 2005;30:6–9. 28–30. [Google Scholar]
- Leukefeld CG, Tims FM, Farabee D. Treatment of drug offenders: policies and issues. New York, NY: Springer; 2002. [Google Scholar]
- MacGowan RJ, Swanson NM, Brackbill RM, Rugg DL, Barker T, Molde S. Retention in methadone maintenance treatment programs, Connecticut and Massachusetts, 1990–1993. Journal of Psychoactive Drugs. 1996;28:259–265. doi: 10.1080/02791072.1996.10472487. [DOI] [PubMed] [Google Scholar]
- Maddux JF, Desmond DP. Careers of opioid users. New York, NY: Praeger; 1981. [Google Scholar]
- Magura S, Nwakeze P, Demsky S. Pre- and in-treatment predictors of retention in methadone treatment using survival analysis. Addiction. 1998;93:51–61. doi: 10.1046/j.1360-0443.1998.931516.x. [DOI] [PubMed] [Google Scholar]
- Magura S, Rosenblum A, Lewis C, Joseph H. The effectiveness of in-jail methadone maintenance. Journal of Drug Issues. 1993;23:75–99. [Google Scholar]
- Mark TL, Woody GE, Juday T, Kleber HD. The economic costs of heroin addiction in the United States. Drug Alcohol Dependence. 2001;61(2):195–206. doi: 10.1016/s0376-8716(00)00162-9. [DOI] [PubMed] [Google Scholar]
- McCullough P, Nelder JA. Generalized Linear Models. 2. London: Chapman and Hall; 1989. [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, Argeriou M. The fifth edition of the Addiction Severity Index: historical critique and normative data. Journal of Substance Abuse Treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- McSweeney T, Turnbull PJ, Hough M. Review of criminal justice interventions for drug use in other countries. London: Criminal Policy Research Unit; 2002. [Google Scholar]
- Michels II, Stover H, Gerlach R. Substitution treatment for opioid addicts in Germany. Harm Reduction Journal. 2007;2:4–5. doi: 10.1186/1477-7517-4-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moolchan ET, Hoffman JA. Phases of treatment: a practical approach to methadone maintenance treatment. International Journal on Addiction. 1994;29:135–160. doi: 10.3109/10826089409047374. [DOI] [PubMed] [Google Scholar]
- Nurco DN. A long-term program of research on drug use and crime. Substance Use and Misuse. 1998;33:1817–1837. doi: 10.3109/10826089809059323. [DOI] [PubMed] [Google Scholar]
- Nurco DN, Hanlon TE, Kinlock TW. Recent research on the relationship between illicit drug use and crime. Behavioral Sciences and the Law. 1991;9:221–242. [Google Scholar]
- Pang L, Hao Y, Mi G, Wang C, Luo W, Rou K, Li J, Wu Z. Effectiveness of first eight methadone maintenance treatment clinics in China. AIDS. 2007;21(Suppl 8):S103–S107. doi: 10.1097/01.aids.0000304704.71917.64. [DOI] [PubMed] [Google Scholar]
- Peles E, Adelson M. Gender differences and pregnant women in a methadone maintenance treatment (MMT) clinic. Journal of Addictive Diseases. 2006;25:39–45. doi: 10.1300/J069v25n02_06. [DOI] [PubMed] [Google Scholar]
- Platt JJ, Widman M, Lidz V, Marlowe D. Methadone maintenance treatment: its development and effectiveness after 30 years. In: Inciardi JA, Harrison LD, editors. Heroin in the age of crack-cocaine. Thousand Oaks, CA: Sage; 1998. pp. 160–187. [Google Scholar]
- Prendergast ML, Wexler HK. Correctional substance abuse treatment programs in California: A historical perspective. The Prison Journal. 2004;84:61–80. [Google Scholar]
- Rowan-Szal GA, Chatham LR, Simpson DD. Importance of identifying cocaine and alcohol-dependent methadone clients. American Journal of Addiction. 2000;9:38–50. doi: 10.1080/10550490050172218. [DOI] [PubMed] [Google Scholar]
- Schwartz RP, Highfield DA, Jaffe JH, Brady JV, Butler CA, Rouse CO, Callaman JM, O’Grady KE, Battjes RJ. A randomized controlled trial of interim methadone maintenance. Archives of General Psychiatry. 2006;63:102–109. doi: 10.1001/archpsyc.63.1.102. [DOI] [PubMed] [Google Scholar]
- Smith-Rohrberg D, Bruce RD, Altice FL. Research note-review of corrections-based therapy for opiate-dependent patients: implications for buprenorphine treatment among correctional populations. Journal of Drug Issues. 2004;34:451–480. [Google Scholar]
- Stewart LM, Henderson CJ, Hobbs MS, Ridout SC, Knuiman WW. Risk of death in prisoners after release from jail. Australian and New Zealand Journal of Public Health. 2004;28(1):32–36. doi: 10.1111/j.1467-842x.2004.tb00629.x. [DOI] [PubMed] [Google Scholar]
- Tomasino V, Swanson AJ, Nolan J, Shuman H. The Key Extended Entry Program (KEEP): a methadone treatment program for opiate-dependent inmates. Mount Sinai Journal of Medicine. 2001;68:14–20. [PubMed] [Google Scholar]
- Weatherburn D, Lind B. Heroin harm minimization: do we really have to choose between law enforcement and treatment? New South Wales Crime and Justice Bulletin. 1999;46:1–11. [Google Scholar]