Abstract
OBJECTIVES
Psychological and behavioral therapies are increasingly employed for symptom management in patients with irritable bowel syndrome (IBS). The aim of this study was to compare two delivery modes for a comprehensive self-management intervention, primarily by telephone versus entirely in-person, and compare each to usual care.
METHODS
Adults with IBS were recruited through community advertisement. Subjects (N = 188) were randomly assigned to three groups: one in which all 9-weekly comprehensive self-management sessions were delivered in-person (CSM-IP), one in which 6 of the 9 session were conducted by the telephone (CSM-T/IP), and one in which subjects received usual care (UC). Primary outcome measures were a GI symptom score based on six symptoms from a daily diary and disease-specific quality of life. These and other outcomes were assessed at baseline and at 3, 6 and 12 months post randomization. Mixed model analyses tested for differences between the three groups in each outcome variable at the three follow-up occasions, controlling for baseline level of each outcome.
RESULTS
Both GI symptom score and QOL showed significantly greater improvement in the two CSM groups than in the UC group (P < 0.001), with the magnitude of this difference being quite similar for the three follow-up time points. The two CSM groups experienced a very similar degree of improvement, and there were no statistically significant differences between the two.
CONCLUSIONS
A comprehensive self-management program is efficacious whether delivered primarily by telephone or totally in-person, and there is no evidence that replacing six of the in-person sessions by telephone sessions reduces the efficacy of the intervention.
Introduction
There is increasing evidence that psychological treatments including cognitive behavioral therapy (CBT) are effective strategies for the management of patients with irritable bowel syndrome (IBS) (1). The use of CBT is based on the hypothesis that IBS symptoms are due, at least in part, to dysfunctional cognitions about visceral sensations (2, 3). CBT has been compared to standard medical care using both an individual presentation (4, 5) and small groups (6). When compared to education alone, CBT was shown to decrease gastrointestinal (GI) symptoms to a greater degree (7). In a study using group therapy, the psychoeducation support group was as effective as the cognitive therapy group in reducing GI symptoms, and both were more effective than daily stress monitoring (6). In Great Britain, a nurse-delivered CBT plus mebeverine intervention when compared to mebeverine alone was found to produce greater reductions in symptom severity and that the response could be sustained for 12 months (8).
In prior work our team combined CBT with education, relaxation training, and diet management into an 8-session comprehensive self-management (CSM) program for patients with IBS (5). When compared to usual care, this full 8-session CSM delivered by an advanced practice nurse resulted in improvements in GI symptoms and quality of life (QOL) that were sustained at 12 months post- intervention (5). One problem noted in this study was that the need for weekly travel to the intervention site imposed a burden on patients.
Alternatives to face-to-face approaches for the effective delivery of therapist-intensive interventions are prompted by concerns over travel time, clinical availability, and disruptions in patients’ daily activities. Telephone, web-based, and video-conferencing may all yield benefits in terms of access and convenience (9, 10). Previous research has demonstrated the feasibility of using the telephone to delivery interventions for depression (11–14), anxiety disorders (9, 15), cancer- symptom management (16, 17) and smoking cessation (18, 19). In most cases cognitive behavioral interventions delivered by telephone or a combination of telephone and in-person sessions were as effective as those relying exclusively on in-person groups (15), and more effective than usual care (13, 17, 20), attention control (14), or care management approach (12). However, in one study, cancer-symptom management by telephone did not differ from usual care (16).
The goal of the current study was to modify the previously tested CSM intervention for delivery by telephone, and compare the efficacy of CSM delivered mainly by telephone (CSM-T/IP) to in-person delivery (CSM-IP) and to Usual Care. We hypothesized that those in the CSM-IP and CSM-T/IP groups would demonstrate decreased GI symptoms and enhanced QOL compared to those in the UC group, and that outcomes in the CSM-T/IP group would be comparable to the CSM-IP group.
METHODS
A three-arm randomized controlled trial design (CSM-IP, CSM-T/IP, and UC) was used with a 12-month longitudinal follow-up. All three groups completed interviews, questionnaires, and kept a symptom diary for primary and secondary outcomes at each of four assessment periods (baseline, three, six and twelve month post-randomization).
Recruitment and Eligibility
Recruitment
Volunteers with IBS were recruited through community advertisements and a single mailing to patients in a university-based gastroenterology practice.
Study eligibility
To be included, men and women had to be at least 18 years of age, have a prior diagnosis of IBS made by a health care provider, and had to report current IBS symptoms (Rome-II criteria). Participants were excluded if they had a history of co-existing GI pathology (e.g., inflammatory bowel disease, celiac disease) or surgery (e.g., bowel resection), renal, or reproductive pathology (e.g., endometriosis, prostate cancer). Participants with certain other comorbidities or medication use were also excluded, based on the guiding principle of whether the disorder or medications could confound the measurement of the symptoms of IBS or compromise the subject’s ability to complete the study. Subjects were excluded for conditions such as severe fibromyalgia, type 1 or 2 diabetes mellitus, infectious diseases (e.g., hepatitis B or C, HIV), symptoms of dementia, untreated sleep apnea/hypopnea, severe cardiovascular disease, severe depression, and current substance abuse. Examples of medications that lead to exclusion included the regular use of antibiotics, anticholinergics, cholestyramine, narcotics, colchicine, docusate, enema preparations, iron supplements, or laxatives. Human subjects institutional review approval was obtained prior to enrolling participants (May 2002) and renewed yearly thereafter. This study was registered with clinicaltrials.gov through the U.S. National Institutes of Health.
Baseline Assessment
Baseline assessment was a 6-step process over 6 to 9 weeks. In Step 1 subjects were assessed for eligibility at the initial telephone screening. Step 2 was an in-person session where written consent was obtained, a health interview was conducted by a research nurse, and questionnaires were completed. Step 3 was the assessment of a 4-week symptom diary completed each evening to determine if the subjects had both abdominal pain/discomfort and diarrhea or constipation at least 25% of the days. Step 4 was a computerized mental health assessment done over the telephone sometime during the 4 weeks of the diary. The fifth step was a review by a gastroenterologist of all baseline data to determine whether the diagnosis of IBS was appropriate and there were no red flags that indicated a need for further assessment. Finally, subjects who were eligible to be randomized were asked if they wished to continue with the study.
Randomization
Subjects were randomized to one of the three treatment arms. A computerized adaptive randomization procedure (21) was used to ensure the three groups remain balanced with respect to age, sex, predominant stool consistency (loose stools, hard stools), and severity of abdominal pain (mild vs. moderate to severe) at baseline. Randomization started on April 2003 and ended on January 2007.
Treatment Phase
The intervention was delivered in nine individual one-hour sessions by two research nurses who were trained as psychiatric nurse practitioners. Because of potential unexpected delays we allowed up to 13 weeks to complete the nine sessions. Participants in the individualized CSM-IP group were seen at the study research office for all nine sessions. Those in the CSM-T/IP group had their first two sessions in the study office in order to build rapport and teach breathing exercises. Sessions 3 through 8 were conducted by telephone, and the last session (termination) was at the study research office. An IBS Workbook was used so that participants could read the content for the week prior to the session.
CSM-IP and CSM-T/IP Protocol
The intervention received by the CSM-IP and CSM-T/IP groups covered four themes: education, diet, relaxation, and cognitive-behavioral strategies (Table 1). Initially, IBS was defined for participants and reassurance was given that IBS is not life threatening. Signs and symptoms that are would require consulting a health care provider were reviewed. The participants completed a Food Frequency questionnaire (22, 23) that was reviewed by a registered dietician to identify problems in the diet. This information was used to tailor the instructions on healthy eating strategies. Participants were taught to recognize foods that were associated with their symptoms (e.g., coffee, fatty foods, raw vegetables) as well as situations when select foods were not tolerated (e.g., a time of high work stress) (24, 25). Homework included keeping a food diary to identify when they ate, what they ate, and what was happening in their environment. Relaxation training included abdominal breathing, progressive muscle relaxation (26), and mini-relaxations (27). Homework included abdominal breathing at least three times a day (e.g., before each meal), use of the relaxation audio recordings three times a week, and daily mini-relaxation using tension as a cue. Specific cognitive behavioral strategies were selected based on individualized assessment. These included examining alternative thinking, cognitive distortions, assertiveness and social skills training, and social support. Homework included writing down their automatic thoughts and identifying and using alternative thoughts (28, 29). After each session the research nurse recorded the percentage of homework completed in the session notes.
Table 1.
Overview of Study Sessions.
| CSM- IP | CSM- T/IP | No. | Session Topics |
|---|---|---|---|
| FtF | FtF | 1 | Overview, Introduction to 3 primary strategies, and explanation of self-management. |
| FtF | FtF | 2 | Diet and review of abdominal breathing |
| FtF | T | 3 | Alternative thinking and passive progressive muscle relaxation |
| FtF | T | 4 | Cognitive distortions, diet, and personalized goals |
| FtF | T | 5 | Fiber, fluids, and active progressive relaxation |
| FtF | T | 6 | Sleep patterns, sleep hygiene, and mini-relaxers |
| FtF | T | 7 | Pain management and sexual dysfunction |
| FtF | T | 8 | Eating out, travel, summary, and yearly plan |
| FtF | FtF | 9 | Evaluation of plan and termination |
CONSORT, Consolidated Standards of Reporting Trials; CSM-IP, comprehensive self-management— in person; CSM-T/IP, comprehensive self-management —telephone.
Usual Care Protocol
Participants in the UC group were notified that they would not receive either of the active intervention, but should continue with whatever treatment was recommended or provided by their health care provider. They were told that they would be contacted in two months from the first the follow-up visit. At the end of the study they were sent the study Workbook.
Follow-up Phase
Participants in all three groups were re-assessed for the primary and secondary outcomes (questionnaires and 4-week diary) at three, six, and twelve months post-randomization. The three month follow-up was designed to be shortly after the last treatment session. Follow-up data collection was done by a research nurse who was blinded to the group assignment.
Measures
Primary Outcomes
IBS Symptom score
Every day subjects rated 26 symptoms on a scale of 0 (not present), 1 (mild), 2 (moderate), 3 (severe) or 4 (very severe). Of these, six were GI symptoms related to IBS: abdominal pain or discomfort, bloating, constipation, diarrhea, intestinal gas, and urgency. An IBS symptom score was computed by first determining the severity of the worst IBS symptom on each day to get an IBS severity for that day, then collapsing across the diary days for each subject to determine the percentage of days with moderate to very severe GI symptoms (30, 31).
Quality of Life
The IBS-Quality of Life (IBSQOL) questionnaire is a 42-item questionnaire with nine scales: sleep, emotional, mental health beliefs, energy, physical functioning, diet, social role, physical role, and sexual relations (32). Example questions are “How often did your IBS make you feel fed up or frustrated” e.g., 1 (always), 2 (often), 3 (sometimes), 4 (seldom) to 5 (never); or “My IBS affected my ability to succeed at work/main activity” e.g., 1 (strongly agree) to 5 (strongly disagree). The scales are transformed to a standard 0 to 100 scale. A total score was computed by averaging all but two of the scales (eating/diet and sexual relations). The eating/diet scale was omitted because participants in the CSM groups were encouraged to avoid foods that cause problems for them. The sexual relations scale was omitted because it was missing for a large fraction of the sample had not been sexually active in the previous 4 weeks. Extensive and acceptable validity and reliability tests have been conducted (32). Internal consistency (Cronbach’s alpha) for the scales ranged from α = 0.73 to 0.93 for this study.
Secondary Outcomes
Psychological distress
The Brief Symptoms Index (BSI) includes 53 symptoms that are collapsed into 9 subscales: depression, hostility, somatization, interpersonal sensitivity, psychoticism, obsessive-compulsive, anxiety, phobic anxiety, paranoid ideation, and a mean score of all items (Global Severity Index). The subject is asked to consider the last 7 days then rate each symptom from 0 (not at all) to 4 (extremely) distressing. However, for the follow-up assessments the BSI-18 was used, which includes 3 subscales anxiety, depression, and somatization. This BSI is based on the Symptom Checklist-90-Revised (SCL-90R), which has been normed on men and women and adolescents in non-patient and adult psychiatric outpatient and inpatient samples. Internal consistency of the subscale scores are reported to range from α = .77 to .90 and test-retest reliability (one week interval) was .78 to .90 (33). For this study the internal consistency was α = .88 for Global Severity Index, α = .80 for Anxiety, α = .85 for Depression, α = .69 for Somatization at Baseline.
Cognitive beliefs
The Cognitive Scale for Functional Bowel Disorders (CSFBD) describes 25 cognitive beliefs related to functional bowel disorders (34). The items are rated from 1 (strongly disagree) to 7 (strongly agree). A typical item is, “I often worry that there might not be a bathroom available when I need it.” The CSFBD has high concurrent criterion validity, acceptable convergent validity, and high content validity and face validity with minimal social desirability contamination (34). The internal consistency for this study was α = .937. The summary score was the mean of all items.
Work Productivity and Activity
The Work Productivity and Activity Impairment Questionnaire (WPAI) has been adapted for persons with IBS (35). It includes 9 questions related to the impact of IBS on work and other regular activities. Construct validity is acceptable when tested against known measures in employed individuals affected by a health problem. The test-retest (1-day) ranged from r = .71 to .95 for the items (35). For this analysis two scales will be used, the Overall Work Productivity Loss (missed work and work impairment due to IBS) and the Daily Activity Impairment scales (impairment while working due to IBS).
Quality Control, Blinding, and Safety Measures
Quality control and safety measures included the use of a standardized protocol manual and standardized training. The two advanced practice nurses who delivered the intervention were aware of the group assignment and provided both interventions. A third nurse collected the follow-up data and was blinded to the participant’s group assignment. Weekly staff meetings were held to review the study implementation. The CSM sessions were audio recorded to assess adherence to the intervention protocol. Three randomly selected recordings per participant were reviewed using a checklist for compliance with the protocol. Our Data Safety Monitoring Board met prior to the onset of the study and yearly until the study was completed.
Sample Size Determination
The goal of the study was to finish with 180 subjects with analyzable follow-up data. With that sample size there would be 81% power if the change in QOL or IBS symptom score was 0.5 SD higher in the two CSM than in the usual care group, or 93% power if the change in QOL or IBS symptom score was 0.6 SD higher. These power calculations are based on ANOVA at one time point, but actual analyses use data from three time points and control for baseline, hence power will be somewhat higher. Our earlier study showed a difference of about 0.7 SD between CSM and usual care.
Analysis
The two primary outcome variables (IBS symptom score and QOL) were analyzed separately. For each, data from the three follow-up time points were analyzed together using a mixed model, with subject as a random effect and treatment group (three levels, CSM-IP, CSM-T/IP, UC) and measurement time (three levels, 3-mo., 6-mo., 12-mo) as fixed factors. Analyses controlled for covariates that might be related to the outcomes: baseline levels of the outcome variable as well as QOL and psychological distress at baseline. The main effect for group was used to test whether the three treatment groups differ with respect to GI symptoms at follow-up. Whenever this overall main effect was significant, univariate ANOVAs were done at each follow-up time point and appropriate contrasts were used to test all pairwise comparisons (CSM-T/IP versus Usual Care, CSM-IP versus Unusual Care, and CSM-T/IP versus CSM-IP). Similar analysis were done for secondary outcomes.
Two binary symptom improvement variables were created, defined as a 50% decrease from baseline in the IBS symptom score (% of days with at least moderate symptom) and a 50% decrease in abdominal pain/discomfort score. Logistic regression was used to estimate the odds ratios for probability of improvement in each CSM group relative to Usual Care, controlling for baseline. These analyses will allow comparison of our results to those reported in two recent meta-analyses (1, 36) which reviewed a number of studies using psychological interventions for IBS where 50% improvement in symptoms was used as the primary outcome. Some pain researchers would regard a 50% criterion as excessively stringent and prefer 30% threshold for clinical significance (37), however the 50% threshold is what has been reported in the IBS literature.
An intent-to-treat approach was used in this study. That is, every effort was made to collect follow-up data on every subject who was randomized, regardless of how many intervention sessions were attended, and all subjects on whom follow-up data were available were included in the analysis.
RESULTS
Participant Flow and Follow-Up
Table 2 is the consolidated standards of reporting trials (CONSORT) diagram showing numbers of subjects screened, randomized, and followed. One hundred and eighty eight subjects were randomized and only 12 of these (6%) failed to provide any follow-up data. Eighty-seven percent of subjects assigned to CSM received at least seven out of nine sessions. Homework was assigned between treatment sessions and 90% of CSM-T/IP subjects and 91% of CSM-IP subjects meet our expectations for homework completion, i.e., at least 75% of assigned work was completed on at least 75% of the sessions.
Table 2.
Study CONSORT Table
| Assessed for Eligibility | N = 771 | ||
|---|---|---|---|
| Excluded | N = 583 | ||
| Reasons: | |||
| Not met inclusion criteria | n = 328 | ||
| Chose not to participate | n = 255 | ||
| ↓ | |||
| Randomized | N=188 | ||
| UC | CSM-T/IP | CSM-IP | |
| Randomized | N = 62 | N = 64 | N = 62 |
| ↓ | |||
| Received full intervention (7+ sessions) | NA | N = 55 | N = 54 |
| Received partial intervention | NA | N = 7 | N = 5 |
| Reasons: | |||
| Too busy | n = 1 | n = 3 | |
| Unable to contact | n = 4 | n = 2 | |
| Health problems | n = 2 | ||
| Received no intervention | NA | N = 2 | N = 3 |
| Reasons: | |||
| Too busy | n = 1 | n = 2 | |
| Unable to contact | n = 1 | n = 1 | |
| Health problems | |||
| ↓ | |||
| Complete follow-up | N = 52 | N = 52 | N = 49 |
| Partial follow-up | N = 8 | N = 6 | N = 9 |
| Reasons: | |||
| Too busy | n = 5 | n = 2 | n = 6 |
| Unable to contact | n = 3 | n = 4 | n = 2 |
| Health problems | n = 0 | n = 0 | n = 1 |
| No follow-up | N = 2 | N = 6 | N = 4 |
| Reasons: | |||
| Too busy | n = 1 | n = 3 | n = 2 |
| Unable to contact | n = 1 | n = 2 | n = 1 |
| Health problems | n = 0 | n = 1 | n = 1 |
| Analyzed | N = 60 | N = 58 | N = 58 |
Demographics and baseline clinical characteristics are given in Table 3. Subjects in this sample were mainly female, white and relatively well educated. Seventy-five percent of the sample was working, 11% were retired, 20% were not working when they enrolled in the study, and 5% were stay-at-home parents. Over half of those participants who were working gave job titles that were classified as professional. Overall, participants reported having typical IBS symptoms for 10 years (SD 14) prior to their diagnosis: 31% started in childhood (4 to < 17.99 yrs), 62% started between 18 – 49 years, and 8% reported that their symptoms started at 50 years or older. Half of the subjects were diagnosed by a gastroenterologist and the rest by a primary care provider (i.e., family practice physician, internist, nurse practitioner, physician’s assistant, or other). Average age of first IBS diagnosis was 27 years (SD 14). Neither demographic or IBS characteristics differed statistically among groups. Twelve participants in this study did not provide any follow-up date. The participants who had no follow-up data (6%) or partial follow-up data (13%) did not differ on demographic variables or IBS characteristics from those participants that had complete data (86%).
Table 3.
Baseline Demographics and Clinical Characteristics
| Variable | UC n = 60 | CSM-T/IP n = 58 | CSM-IP n = 58 | P values |
|---|---|---|---|---|
| Demographics | ||||
| Age, Mean (SD) | 43 (14) | 45 (14) | 44 (14) | .744 |
| Gender – Female, % (n)b | 85% (51) | 88% (51) | 86% (50) | .897 |
| Race, White, % (n) b | 92% (55) | 86% (50) | 95% (55) | .263 |
| Married or Partnered b | 47% (28) | 43% (25) | 47% (27) | .908 |
| Education, Bachelors or above b | 57% (34) | 72% (42) | 60% (40) | .164 |
| Income, > $65,000/yr b,d | 57% (34) | 49% (28) | 54% (31) | .705 |
| Professional Job b,c | 68% (30) | 76% (31) | 75% (30) | .692 |
| Predominant Bowel Pattern d | ||||
| Normal | 3% (02) | 5% (03) | 7% (04) | .507 |
| Constipation | 18% (11) | 26% (15) | 22% (13) | |
| Diarrhea | 52% (31) | 48% (28) | 59% (34) | |
| Alternating | 27% (16) | 21% (12) | 12% (07) | |
Note. CSM-T/IP = Comprehensive Self-Management-Telephone. CSM-IP = Comprehensive Self-Management-In-Person.
P-value for age was based on Oneway Analysis of Variance.
P-value based on Pearson’s Chi Square.
Based on US job classification system; only 125 currently had a job.
Based on Rome II definition.(42)
Primary and Secondary Outcomes
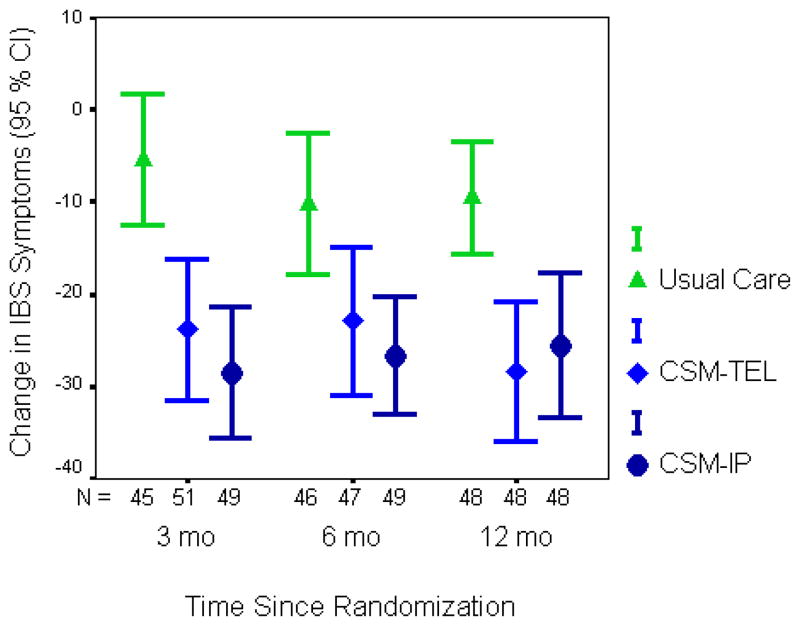
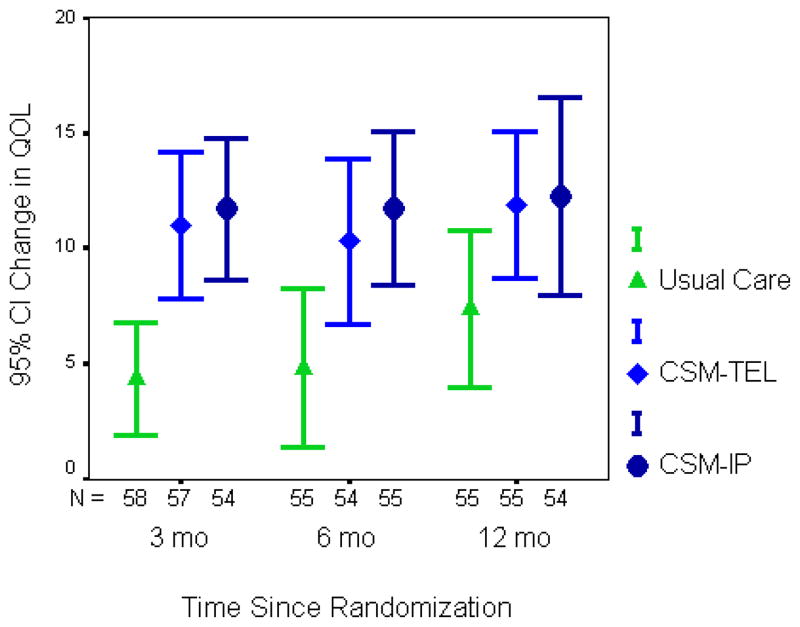
Table 4 shows the baseline means and change scores of the primary and secondary outcome variables in the three treatment groups. The two CSM groups show a large improvement from baseline to 3 months in the primary outcomes which persists at 6 months and 12 months. Note that for the QOL an increase indicates improvement, while for the other variables a decrease (minus value) indicates improvement. There was no significant difference in the amount of improvement in CSM-T/IP compared to CSM-IP. Figure 1, 2, and 3 further illustrates these results for the two primary outcome variables.
Table 4.
Baseline and Change Scores on the Primary and Secondary Outcome Variables by Treatment Group
| Mean (SD) | Mean (SD) Change from Baseline | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Baseline | N | 3-Months | N | 6-Months | N | 12-Months | Pa | |
| Primary Outcomes | |||||||||
| IBS Symptom Score | |||||||||
| UC | 53 | 64.9 (26.7) | 45 | −5.4 (23.4) | 46 | −10.3 (25.7) | 48 | −9.5 (21.0) | <.001 |
| CSM-T/IP | 54 | 69.9 (24.3) | 51 | −23.8 (27.0) | 47 | −22.9 (27.4) | 48 | −28.4 (26.0) | |
| CSM-IP | 53 | 76.0 (22.1) | 49 | −28.5 (24.9) | 49 | −26.6 (22.1) | 48 | −25.6 (27.0) | |
| Pair-wise p values b | .001, <.001, .516 | .027, .007, .610 | <.001, .006, .471 | ||||||
| IBS-QOL Total | |||||||||
| UC | 60 | 66.3 (15.9) | 58 | 4.4 (9.2) | 55 | 4.8 (12.6) | 55 | 7.4 (12.6) | <.001 |
| CSM-T/IP | 58 | 70.7 (14.9) | 57 | 11.0 (11.9) | 54 | 10.3 (13.1) | 55 | 11.90 (11.8) | |
| CSM-IP | 58 | 68.4 (12.9) | 54 | 11.7 (11.2) | 55 | 11.7 (12.3) | 54 | 12.2 (15.6) | |
| Pair-wise p values b | <.001, <.001, .970 | .005, .003, .881 | .010, .029, .677 | ||||||
| Secondary Outcomes | |||||||||
| Psychological distress - BSI | |||||||||
| UC | 60 | 0.50 (0.46) | 58 | 0.20 (0.39) | 55 | 0.17 (0.42) | 56 | 0.13 (0.40) | <.001 |
| CSM-T/IP | 58 | 0.52 (0.41) | 57 | −0.07 (0.35) | 54 | −0.06 (0.38) | 55 | −0.08 (0.42) | |
| CSM-IP | 58 | 0.52 (0.40) | 55 | −0.03 (0.40) | 54 | 0.03 (0.42) | 54 | 0.05 (0.45) | |
| Pair-wise p values b | <.001, .001, .553 | .003, .123, .073 | .009, .457 .061 | ||||||
| CSFBD | |||||||||
| UC | 60 | 4.52 (1.09) | 58 | −0.28 (0.53) | 55 | −0.42 (0.67) | 55 | −0.46 (0.78) | <.001 |
| CSM-T/IP | 58 | 4.36 (1.01) | 56 | −0.83 (0.80) | 54 | −0.75 (0.90) | 55 | −1.01 (0.89) | |
| CSM-IP | 58 | 4.71 (0.99) | 53 | −1.13 (0.74) | 53 | −1.04 (0.69) | 54 | −1.11 (0.79) | |
| Pair-wise p values b | <.001,<.001, .046 | 0.016, <.001, .101 | <.001,<.001, .829 | ||||||
| WPAI – Work Loss | |||||||||
| UC | 45 | 24.6 (20.7) | 35 | 4.1 (19.0) | 38 | −2.7 (20.6) | 34 | −3.2 (21.4) | .008 |
| CSM-T/IP | 41 | 25.7 (17.5) | 35 | −10.5 (17.6) | 30 | −10.8(16.7) | 34 | −12.4 (17.9) | |
| CSM-IP | 37 | 28.4 (24.8) | 30 | −11.9 (30.5) | 30 | −12.9 (28.1) | 32 | −12.9 (31.8) | |
| Pair-wise p values b | .009, .039, .660 | .052, .140, .660 | .074, .303, .467 | ||||||
| WPAI – Activity | |||||||||
| UC | 59 | 34.1 (22.9) | 56 | −1.1 (24.1) | 54 | −5.4 (17.7) | 55 | −6.2 (26.1) | <.001 |
| CSM-T/IP | 57 | 29.6 (20.8) | 56 | −13.2 (24.4) | 53 | −11.9 (22.8) | 52 | −13.3 (20.7) | |
| CSM−IP | 58 | 30.5 (21.8) | 54 | −14.6 (25.4) | 53 | −12.8 (24.4) | 53 | −14.5 (30.2) | |
| Pair-wise p values b | <.001,<.001, .920 | .004, .009, .800 | .005, .006, .972 | ||||||
Note. CSM-T/IP = Comprehensive Self-Management-Telephone. CSM-IP = Comprehensive Self-Management-In-Person. IBS Symptom Score = diary symptom severity was summarized across all days for each person as the percent of days on which symptoms were at least moderate. IBSQOL was rated on a 1 to 5 or 1 to 6 Likert scale e.g., emotional scale ‘1’ always, ‘2’ often ‘3’ sometimes, ‘4’ seldom, ‘5’ never. BSI-53 was rated from ‘0’ not at all, ‘1’ a little bit, ‘2’ moderately, ‘3’ quite a bit and ‘4’ extremely. CSFBD = Cognitive Scale for Functional Bowel Disorders. CSFBD was rated from ‘1’ strongly disagree to ‘4’ neutral to ‘7’strongly agree. WPAI – Work loss = Work Productivity and Activity Impairment questionnaire – Overall Work Productivity Loss. WPAI – Activity = Work Productivity and Activity Impairment questionnaire – Daily Activity Impairment. These items are rated from “0” IBS has not effect to “10” IBS completely prevents me from working or completely prevented my participation in usual daily activities.
P-value from Mixed methods for testing the null hypothesis that the mean is the same in all three treatment groups at all three time points, adjusting for the baseline value of the variable.
Pair-wise comparisons: CSM-T/IP vs. UC; CSM-IP vs. UC; CSM-T/IP vs. CSM-IP.
Figure 1.
Graph of mean (95% CI) for change in IBS symptoms from the daily diary across the three follow-up assessments by the CSM-IP, CSM-T/IP and UC groups. Number of subjects in each analysis is beneath the figure for each time period.
Figure 2.
Graph of mean (95% CI) for change in QOL across the three follow-up assessments by the CSM-IP, CSM-T/IP and UC groups. Number of subjects in each analysis is beneath the figure for each time period.
Results are similar for most secondary outcomes, with both CSM groups being better than Usual Care and the CSM groups not differing from each other. However, for psychological distress there is a trend towards better outcomes in the CSM-T/IP than in CSM-IP while for CSFBD there is a trend towards better outcomes in CSM-IP than in CSM-T/IP. Note also that the treatment differences for psychological distress are due to the worsening of symptoms in the Usual Care group more than the improvement in the intervention groups. The intervention effect was stronger for the WPAI measure of interference with daily activities than on the WPAI measure of interference with work, partially due to the smaller sample of people who were employed at both baseline and follow-up.
These results are based on models with only main effects. Additional analyses tested for interaction effects. The interaction between follow-up time and treatment group was not significant for any outcome, though it was nearly significant (p = .088) for CSFBD. Overall, these results indicate that the treatment effect seen at 3 months persists at 6 and 12 months with little diminution.
Several ancillary analyses were conducted in an effort to determine which particular GI symptoms were most affected by CSM. Table 5 presents the baseline means and change scores of the individual GI symptoms that were included in the IBS Symptom score. The two CSM groups show a large improvement in abdominal pain/discomfort and intestinal gas which persists through 12 months. The changes in bloating, constipation, diarrhea, and urgency were greater in CSM than UC but not significantly different in the mixed model test.
Table 5.
Baseline and Change Scores on the Specific IBS Symptom Variables by Treatment Group
| Variable | Baseline | N | 3-Months | N | 6-Months | N | 12-Months | P value |
|---|---|---|---|---|---|---|---|---|
| Abdominal pain/discomfort | ||||||||
| UC | 35.2 (26.3) | 39 | −0.9 (22.8) | 40 | −1.9 ( 25.8) | 41 | −5.2 (16.6) | <.001 |
| CSM-T/IP | 35.1 (26.5) | 40 | −19.3 (27.2) | 36 | −20.4 (28.3) | 37 | −24.7 (24.6) | |
| CSM-IP | 45.3 (24.4) | 45 | −23.5 (23.0) | 44 | −20.8 (22.9) | 43 | −18.3 (27.0) | |
| Pair-wise p values b | .001, <.001, .631 | .003, .005, .708 | <.001, .026, .107 | |||||
| Bloating | ||||||||
| UC | 36.3 (29.7) | 36 | −7.3 (22.7) | 36 | −12.32 (24.2) | 38 | −10.89 (25.9) | .162 |
| CSM-T/IP | 41.3 (35.3) | 34 | −24.2 (31.6) | 31 | −23.92 (32.4) | 32 | −29.73 (25.9) | |
| CSM-IP | 37.2 (29.8) | 38 | −17.7 (27.9) | 38 | −12.65 (30.3) | 37 | −15.50 (29.4) | |
| Pair-wise p values b | .059, .092, .771 | .371, .932, .321 | .024, .522, .092 | |||||
| Constipation | ||||||||
| UC | 20.0 (23.0) | 24 | −11.2 (19.3) | 24 | −11.5 (21.7) | 26 | −10.7 (21.1) | .059 |
| CSM-T/IP | 22.0 (25.2) | 29 | −22.8 (24.8) | 26 | −21.8 (29.4) | 28 | −21.0 (32.5) | |
| CSM-IP | 25.4 (26.3) | 30 | −17.3 (19.4) | 29 | −12.6 (19.3) | 29 | −13.5 (21.5) | |
| Pair-wise p values b | .037, .270, .278 | .130, .896, .142 | .210,.928, .226 | |||||
| Diarrhea | ||||||||
| UC | 14.57 (18.81) | 22 | −4.20 (20.07) | 22 | −9.26 (17.46) | 24 | −10.19 (16.57) | .624 |
| CSM-T/IP | 17.23 (22.84) | 21 | −10.15 (23.93) | 19 | −11.38 (31.82) | 20 | −20.95 (21.92) | |
| CSM-IP | 15.36 (20.30) | 21 | −12.26 (18.18) | 22 | −15.08 (18.11) | 18 | −14.69 (18.25) | |
| Pair-wise p values b | .860, .165, .233 | .244, .917, .256 | .317, .938, .360 | |||||
| Intestinal gas | ||||||||
| UC | 41.84 (29.00) | 38 | −7.03 (26.75) | 39 | −9.61 (30.32) | 40 | −9.39 (27.58) | .006 |
| CSM-T/IP | 38.50 (32.11) | 40 | −20.44 (28.55) | 38 | −20.40 (28.44) | 39 | −23.58 (28.13) | |
| CSM-IP | 51.92 (29.33) | 45 | −25.71 (29.06) | 45 | −23.44 (26.65) | 44 | −24.22 (27.11) | |
| Pair-wise p values b | .009, .002, .713 | .049, .059, .876 | .009, .028, .633 | |||||
| Urgency | ||||||||
| UC | 20.03 (23.72) | 27 | −5.27 (18.99) | 29 | −7.07 (21.62) | 26 | −15.58 (22.68) | .143 |
| CSM-T/IP | 20.15 (23.33) | 26 | −12.46 (21.46) | 24 | −15.93 (23.95) | 23 | −25.84 (21.54) | |
| CSM-IP | 21.26 (23.76) | 24 | −19.20 (27.55) | 26 | −20.57 (17.04) | 25 | −17.82 (26.18) | |
| Pair-wise p values b | .255, .051, .393 | .204, .066, .584 | .075, .919, .097 | |||||
Note. CSM-T/IP = Comprehensive Self-Management-Telephone. CSM-IP = Comprehensive Self-Management-In-Person.
Symptom severity is reported as the percent of days with moderate or higher severity. Analyses for each symptom were restricted to only those subjects who rate that symptom as moderate or higher severity on at least 10 % of days at baseline.
P-value from Mixed methods for testing the null hypothesis that the mean is the same in all three treatment groups at all three time points, adjusting for the baseline value of the variable.
Pair-wise comparisons: CSM-T/IP vs. UC; CSM-IP vs. UC; CSM-T/IP vs. CSM-IP.
Table 6 presents the percent of subjects with at least 50% improvement in the IBS symptom score and abdominal pain/discomfort score, and odds ratios of CSM-T/IP and CSM-IP relative to UC. The odds ratios were all large, greater than 2.3, and almost all are statistically significant.
Table 6.
Percent of Subjects with 50% Improvement in IBS Symptom Score and Abdominal Pain/Discomfort.
| IBS Symptoms Score | Abdominal Pain/Discomfort | |||||||
|---|---|---|---|---|---|---|---|---|
| Follow-up | N | Improved N (%) | Odds Ratio (95% CI) | p-value | N | Improved N (%) | Odds Ratio (95% CI) | p-value |
| 3 Months | ||||||||
| UC | 45 | 7 (16%) | 1.00 | 45 | 9 (20%) | 1.00 | ||
| CSM-T/IP | 51 | 20 (39%) | 3.56 (1.33, 9.55) | .012 | 51 | 22 (43%) | 3.05 (1.22, 7.64) | .017 |
| CSM-IP | 49 | 21 (43%) | 4.27 (1.57, 11.62) | .004 | 49 | 31 (63%) | 6.81 (2.67, 17.38) | <.001 |
| 6 Months | ||||||||
| UC | 46 | 10 (22%) | 1.00 | 46 | 15 (33%) | 1.00 | ||
| CSM-T/IP | 47 | 17 (36%) | 2.42 (0.93, 6.34) | .071 | 47 | 25 (53%) | 2.35 (1.01, 5.46) | .046 |
| CSM-IP | 49 | 18 (37%) | 2.82 (1.07, 7.44) | .037 | 49 | 30 (61%) | 3.37 (1.43, 7.96) | .006 |
| 12 Months | ||||||||
| UC | 48 | 11 (23%) | 1.00 | 48 | 13 (27%) | 1.00 | ||
| CSM-T/IP | 48 | 19 (40%) | 2.67 (1.05, 6.78) | .039 | 48 | 30 (62%) | 4.51 (1.89, 10.75) | .001 |
| CSM-IP | 48 | 19 (40%) | 3.00 (1.16, 7.78) | .024 | 48 | 27 (56%) | 3.76 (1.57, 9.00) | .003 |
Note. The outcome score is defined as the fraction of days on which this abdominal pain is at least moderate. “Improvement” is defined as this score decreasing by at least 50%. CSM-T/IP = Comprehensive Self-Management Telephone. CSM-IP = Comprehensive Self-Management In-person.
OR’s and p-values are based on a logistic regression that controls for baseline value of the outcome score.
Adverse events include one participant who experienced suicidal thoughts, which lead to her withdrawing from the study.
DISCUSSION
The results in this trial demonstrate that comprehensive self-management (CSM) therapy is effective, whether delivered primarily by telephone or delivered entirely in-person. Both approaches were more effective in decreasing GI symptoms and increasing QOL than usual care. The magnitude of the treatment effect was virtually the same for the two delivery modalities. Moreover, these improvements persisted through the 12 months post-randomization follow-up (i.e., 9 months post intervention). The GI symptoms most strongly impacted by the intervention were abdominal pain/discomfort and intestinal gas. This is interesting in light of an earlier report (38) showing that these two symptoms were most strongly associated with reduced QOL.
There was also a strong effect of CSM on cognitive beliefs and work loss and impact on daily activities. Given the large financial impact of IBS due to lost productivity, this finding has important implications for potential societal cost-savings from CBT (39, 40). Further research using more extensive measures of productivity loss and health care costs would be useful in evaluating the cost effectiveness of CSM therapy. It should be noted that the CSM-T/IP delivery mode was not designed to be cheaper to deliver than CSM-IP in terms of therapist time, since all sessions were approximately 60 minutes in length whether delivered by telephone or in-person. The main benefit of CSM-T/IP over CSM-IP was the decreased travel time to the therapist’s office.
The CSM intervention is multi-faceted, consisting of education and reassurance, nutritional counseling, relaxation strategies, and cognitive restructuring (5). While all participants received all components, the therapists observed that individuals differed in which components they found most helpful. The use of a workbook allowed participants to continue using strategies that they found helpful after the end of treatment sessions.
One challenge with delivering CSM by telephone became apparent early on in the study: some participants were multitasking while on the telephone with the therapist. The study protocol was quickly changed so that prior to the first phone therapy session, the therapist discussed with the participant the importance of being in a quiet place without distractions during the telephone session, and helped the subject problem-solve about how to arrange that.
Several studies have shown the efficacy of CBT delivered in-person for IBS (1, 5–7). Recently studies have investigated alternative delivery modes for CBT in IBS. An earlier study by our group (5) found a workbook plus one in-person session to be less effective overall than eight in-person CBT sessions. Lackner (41) found that four CBT sessions in combination with a self-help book were as effective as ten sessions of in-person CBT. Delivery of CBT by trained clinic nurses was also effective (8). Although telephone delivery of psychotherapy has been studied for depression and anxiety (9, 10), this is the first study of a CBT-based intervention for IBS delivered primarily by telephone.
As in any psychological intervention study, it was not possible to blind subjects as to treatment assignment. It is possible that some of the observed treatment effect could be due to the placebo effect. But the fact that treatment differences persisted nine months after the end of treatment implies long-term changes in behaviors, habits, attitudes, or beliefs among subjects in the CSM intervention groups.
It should be noted that the CSM-T/IP intervention was not entirely by telephone. The first two sessions were in-person, in order to build a therapeutic relationship with the therapist and teach breathing exercises before starting the telephone sessions. The final session was also in-person, in order to provide a transition to self care. We feel that these three in-person sessions were important to the success of the CSM-T/IP intervention. An intervention that was totally conducted by telephone might not be as effective. Anecdotally, the research staff noted that quite a few subjects volunteered a preference for mode of delivery of CSM, with some having a preference for CSM-T/IP because of the reduced travel time, while others indicated a preference for CSM-IP due to the personal interaction. Since this study found both versions to be effective with no evidence that one is better than the other, a flexible delivery model could be the best approach, with patients allowed a choice in delivery mode for sessions 3 through 8.
In conclusion, this report has shown that the mulitifaceted CSM intervention delivered primarily over the phone by psychiatric nurse practitioners is an effective option for treating IBS. Further investigation is warranted into how best to incorporate such an intervention into clinical practices.
Study Highlights
-
WHAT IS CURRENT KNOWLEDGE
Irritable Bowel Syndrome is common but treatments are limited.
Psychological interventions can be an alternative to multiple medications.
-
WHAT IS NEW HERE
Nutrition and cognitive behavioral therapy is effective in decreasing the distress caused by IBS.
Therapy is effective whether delivered by telephone or in-person.
Acknowledgments
Supported by grants from the NINR, NIH (R01 NR004142 and P30 NR04001). We would like to thank our research nurses, Pam Barney and Pam Weisman, who skillfully conducted the intervention sessions; Heeyoung Lee, PhD who knew where every piece of data was and knew that is was entered correctly; to the rest of the staff who helped us reach this point; and with gratitude to the patients who volunteered to participate.
Abbreviations
- BSI
Brief Symptoms Index
- CBT
cognitive behavioral therapy
- CSFBD
Cognitive Scale for Functional Bowel Disorders
- CSM
comprehensive self-management
- IBS
Irritable Bowel Syndrome
- QOL
quality of life
- WPAI
Work Productivity and Activity Impairment Questionnaire
References
- 1.Lackner JM, Mesmer C, Morley S, et al. Psychological treatments for irritable bowel syndrome: a systematic review and meta-analysis. J Consult Clin Psychol. 2004;72:1100–13. doi: 10.1037/0022-006X.72.6.1100. [DOI] [PubMed] [Google Scholar]
- 2.Boyce P, Gilchrist J, Talley N, et al. Cognitive-behaviour therapy as a treatment for irritable bowel syndrome: a pilot study. Aust N Z J Psychiatry. 2000;34:300–309. doi: 10.1080/j.1440-1614.2000.00731.x. [DOI] [PubMed] [Google Scholar]
- 3.Lackner JM, Jaccard J, Krasner SS, et al. How does cognitive behavior therapy for irritable bowel syndrome work? A mediational analysis of a randomized clinical trial. Gastroenterology. 2007;133:433–44. doi: 10.1053/j.gastro.2007.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Payne A, Blanchard EB. A controlled comparison of cognitive therapy and self-help support groups in the treatment of irritable bowel syndrome. J Consult Clin Psychol. 1995;63:779–86. doi: 10.1037//0022-006x.63.5.779. [DOI] [PubMed] [Google Scholar]
- 5.Heitkemper M, Jarrett M, Levy R, et al. Self-management for women with irritable bowel syndrome. Clin Gastroenterol Hepatol. 2004;2:585–596. doi: 10.1016/s1542-3565(04)00242-3. [DOI] [PubMed] [Google Scholar]
- 6.Blanchard EB, Lackner JM, Sanders K, et al. A controlled evaluation of group cognitive therapy in the treatment of irritable bowel syndrome. Behav Res Ther. 2007;45:633–48. doi: 10.1016/j.brat.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 7.Drossman DA, Toner BB, Whitehead WE, et al. Cognitive-behavioral therapy versus education and desipramine versus placebo for moderate to severe functional bowel disorders. Gastroenterology. 2003;125:19–31. doi: 10.1016/s0016-5085(03)00669-3. [DOI] [PubMed] [Google Scholar]
- 8.Kennedy TM, Chalder T, McCrone P, et al. Cognitive behavioural therapy in addition to antispasmodic therapy for irritable bowel syndrome in primary care: randomised controlled trial. Health Technol Assess. 2006;10:iii–iv. ix–x, 1–67. doi: 10.3310/hta10190. [DOI] [PubMed] [Google Scholar]
- 9.Bee PE, Bower P, Lovell K, et al. Psychotherapy mediated by remote communication technologies: a meta-analytic review. BMC Psychiatry. 2008;8:60. doi: 10.1186/1471-244X-8-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leach LS, Christensen H. A systematic review of telephone-based interventions for mental disorders. J Telemed Telecare. 2006;12:122–129. doi: 10.1258/135763306776738558. [DOI] [PubMed] [Google Scholar]
- 11.Ludman EJ, Simon GE, Grothaus LC, et al. A pilot study of telephone care management and structured disease self-management groups for chronic depression. Psychiatr Serv. 2007;58:1065–72. doi: 10.1176/ps.2007.58.8.1065. [DOI] [PubMed] [Google Scholar]
- 12.Simon GE, Ludman EJ, Tutty S, et al. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trial. JAMA. 2004;292:935–42. doi: 10.1001/jama.292.8.935. [DOI] [PubMed] [Google Scholar]
- 13.Wang PS, Simon GE, Avorn J, et al. Telephone screening, outreach, and care management for depressed workers and impact on clinical and work productivity outcomes: a randomized controlled trial. JAMA. 2007;298:1401–11. doi: 10.1001/jama.298.12.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mohr DC, Hart SL, Julian L, et al. Telephone-administered psychotherapy for depression. Arch Gen Psychiatry. 2005;62:1007–14. doi: 10.1001/archpsyc.62.9.1007. [DOI] [PubMed] [Google Scholar]
- 15.Hecker JE, Losee MC, Roberson-Nay R, et al. Mastery of Your Anxiety and Panic and brief therapist contact in the treatment of panic disorder. Journal of Anxiety Disorders. 2004;18:111–126. doi: 10.1016/S0887-6185(02)00241-4. [DOI] [PubMed] [Google Scholar]
- 16.Sandgren AK, McCaul KD, King B, et al. Telephone therapy for patients with breast cancer. Oncology Nursing Forum. 2000;27:683–688. [PubMed] [Google Scholar]
- 17.Sherwood P, Given BA, Given CW, et al. A cognitive behavioral intervention for symptom management in patients with advanced cancer. Oncol Nurs Forum. 2005;32:1190–8. doi: 10.1188/05.ONF.1190-1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ershoff DH, Quinn VP, Boyd NR, et al. The Kaiser Permanente prenatal smoking-cessation trial: When more isn’t better, what is enough? American Journal of Preventive Medicine. 1999;17:161–168. doi: 10.1016/s0749-3797(99)00071-9. [DOI] [PubMed] [Google Scholar]
- 19.Strecher VJ, Marcus A, Bishop K, et al. A Randomized Controlled Trial of Multiple Tailored Messages for Smoking Cessation Among Callers to the Cancer Information Service. J Health Commun: Routledge. 2005;10(Suppl 1):105–118. doi: 10.1080/10810730500263810. [DOI] [PubMed] [Google Scholar]
- 20.Ludman EJ, Simon GE, Tutty S, et al. A randomized trial of telephone psychotherapy and pharmacotherapy for depression: continuation and durability of effects. J Consult Clin Psychol. 2007;75:257–66. doi: 10.1037/0022-006X.75.2.257. [DOI] [PubMed] [Google Scholar]
- 21.Pocock SJ, Simon R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics. 1975;31:103–15. [PubMed] [Google Scholar]
- 22.Parr CL, Veierod MB, Laake P, et al. Test-retest reproducibility of a food frequency questionnaire (FFQ) and estimated effects on disease risk in the Norwegian Women and Cancer Study (NOWAC) Nutr J. 2006;5:4. doi: 10.1186/1475-2891-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kristal AR, Feng Z, Coates RJ, et al. Associations of Race/Ethnicity, Education, and Dietary Intervention with the Validity and Reliability of a Food Frequency Questionnaire: The Women’s Health Trial Feasibility Study in Minority Populations. Am J Epidemiol. 1997;146:856–869. doi: 10.1093/oxfordjournals.aje.a009203. [DOI] [PubMed] [Google Scholar]
- 24.Blanchard EB, Schwarz SP, Suls JM, et al. Two controlled evaluations of multicomponent psychological treatment of irritable bowel syndrome. Behav Res Ther. 1992;30:175–189. doi: 10.1016/0005-7967(92)90141-3. [DOI] [PubMed] [Google Scholar]
- 25.Stefanini GF, Saggioro A, Alvisi V, et al. Oral cromolyn sodium in comparison with elimination diet in the irritable bowel syndrome, diarrheic type. Multicenter study of 428 patients. Scand J Gastroenterol. 1995;30:535–541. doi: 10.3109/00365529509089786. [DOI] [PubMed] [Google Scholar]
- 26.Jacobson E. You must relax; a practical method of reducing the strains of modern living. New York: McGraw-Hill; 1934. [Google Scholar]
- 27.Benson H. The relaxation response. New York: Morrow; 1975. [Google Scholar]
- 28.Beck AT. Cognitive therapy of depression. New York: Guilford Press; 1979. [Google Scholar]
- 29.Toner BB. Cognitive-behavioral treatment of irritable bowel syndrome : the brain-gut connection. New York: Guilford Press; 2000. [Google Scholar]
- 30.Levy RL, Cain KC, Jarrett M, et al. The relationship between daily life stress and gastrointestinal symptoms in women with irritable bowel syndrome. J Behav Med. 1997;20:177–193. doi: 10.1023/a:1025582728271. [DOI] [PubMed] [Google Scholar]
- 31.Jarrett M, Heitkemper M, Cain KC, et al. The relationship between psychological distress and gastrointestinal symptoms in women with irritable bowel syndrome. Nurs Res. 1998;47:154–161. doi: 10.1097/00006199-199805000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Hahn BA, Kirchdoerfer LJ, Fullerton S, et al. Evaluation of a new quality of life questionnaire for patients with irritable bowel syndrome. Aliment Pharmacol Ther. 1997;11:547–552. doi: 10.1046/j.1365-2036.1997.00168.x. [DOI] [PubMed] [Google Scholar]
- 33.Derogatis L. SCL-90R: Administration, Scoring and Procedures Manual. Minneapolis: NCS Pearson, Inc; 1994. [Google Scholar]
- 34.Toner BB, Stuckless N, Ali A, et al. The development of a cognitive scale for functional bowel disorders. Psychosom Med. 1998;60:492–497. doi: 10.1097/00006842-199807000-00017. [DOI] [PubMed] [Google Scholar]
- 35.Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4:353–65. doi: 10.2165/00019053-199304050-00006. [DOI] [PubMed] [Google Scholar]
- 36.Zijdenbos IL, de Wit NJ, van der Heijden GJ, et al. Psychological treatments for the management of irritable bowel syndrome. Cochrane Database Syst Rev. 2009 January 21;1:CD006442. doi: 10.1002/14651858.CD006442.pub2. [DOI] [PubMed] [Google Scholar]
- 37.Farrar JT, Young JP, LaMoreaux L, et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 38.Cain KC, Headstrom P, Jarrett ME, et al. Abdominal pain impacts quality of life in women with irritable bowel syndrome. Am J Gastroenterol. 2006;101:124–32. doi: 10.1111/j.1572-0241.2006.00404.x. [DOI] [PubMed] [Google Scholar]
- 39.Cash B, Sullivan S, Barghout V. Total costs of IBS: employer and managed care perspective. Am J Manag Care. 2005;11:S7–16. [PubMed] [Google Scholar]
- 40.Leong SA, Barghout V, Birnbaum HG, et al. The economic consequences of irritable bowel syndrome: a US employer perspective. Arch Intern Med. 2003;163:929–935. doi: 10.1001/archinte.163.8.929. [DOI] [PubMed] [Google Scholar]
- 41.Lackner JM, Jaccard J, Krasner SS, et al. Self-administered cognitive behavior therapy for moderate to severe irritable bowel syndrome: clinical efficacy, tolerability, feasibility. Clin Gastroenterol Hepatol. 2008;6:899–906. doi: 10.1016/j.cgh.2008.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Drossman D, Corazziari E, Talley N, et al. Rome II: The functional gastrointestinal disorders. 2. McLean: Degnon Associates; 2000. [Google Scholar]