Abstract
OBJECTIVES:
To evaluate the impact of a neonatal resuscitation course on the theoretical knowledge and practical skills of birthing room personnel, and to evaluate the performance of skills at different times after the course.
DESIGN:
A program evaluation using a before and after cohort study.
SETTING:
Seven level II perinatal centres in the central-east region of Ontario.
PARTICIPANTS:
Seven hundred thirty-seven individuals (medical staff, nurses and respiratory technologists) who worked in birthing rooms.
INTERVENTION:
During an eight-month period, a course in neonatal resuscitation was presented at the perinatal centres. A cohort of 108 (15%) participants received testing before and after the course; the theoretical knowledge and practical performance of 62 of these participants were retested after six and 12 months.
RESULTS:
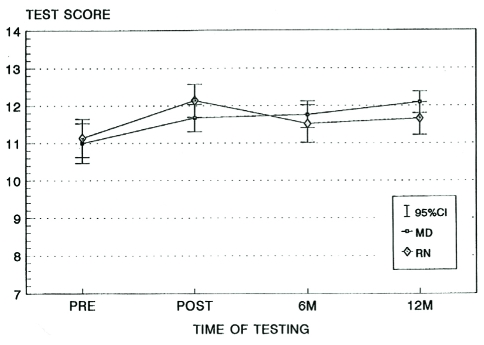
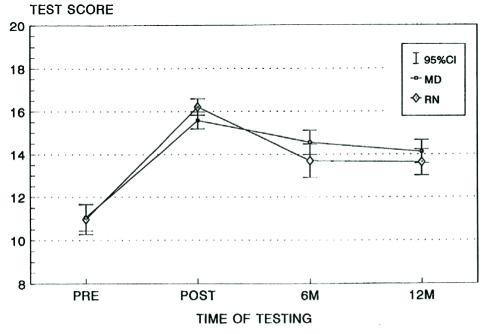
A significant improvement in both theoretical knowledge and practical skills was seen immediately after the course. Throughout the study, no difference was observed in the performance of nursing staff compared with that of medical staff, nor among the institutions involved. No significant difference in the decline of either theoretical knowledge or practical skills was seen among those who scored well in the original pre-test compared with those who scored poorly.
CONCLUSIONS:
Neonatal resuscitation should be an integral part of continuing education for all personnel involved in obstetrical care because it improves both tested knowledge and performance. Practical skills appear to decline faster than theoretical knowledge. Inservice instruction is required, at least, every six months.
Keywords: Neonatal resuscitation, Skill retention
Abstract
OBJECTIFS :
Évaluer les répercussions d’un cours de réanimation néonatale sur les connaissances théoriques et les compétences pratiques du personnel de la salle d’accouchement, ainsi que la performance de ces compétences à diverses intervalles après le cours.
MÉTHODOLOGIE :
Évaluation d’un programme au moyen d’une étude de cohorte avant et après le cours
ÉTABLISSEMENT :
Sept centres périnatals de niveau II de la région centre-est de l’Ontario
PARTICIPANTS :
Sept cent trente-sept individus (personnel médical, infirmières et inhalothérapeutes) qui travaillaient dans des salles d’accouchement
INTERVENTION :
Pendant une période de huit mois, un cours sur la réanimation néonatale a été donné dans les centres périnatals. Une cohorte de 108 (15 %) participants a été évaluée avant et après le cours. Les connaissances théoriques et la performance pratique de 62 de ces participants ont été réévaluées six et douze mois après le cours.
RÉSULTATS :
Une amélioration notable tant des connaissances théoriques que des compétences pratiques s’observait immédiatement après le cours. Pendant l’étude, on n’a remarqué de différence ni dans la performance du personnel infirmier par rapport à celle du personnel médical ni entre les établissements en cause. Par ailleurs, on n’a observé aucune différence marquée dans la diminution des connaissances théoriques ou des compétences pratiques chez ceux qui ont obtenu des bons résultats dans la préévaluation originale par rapport à ceux dont les résultats étaient mauvais.
CONCLUSIONS :
La réanimation néonatale devrait faire partie intégrante de la formation continue de tout le personnel en obstétrique parce qu’elle améliore à la fois les connaissances évaluées et la performance. Les compétences pratiques semblent diminuer plus rapidement que les connaissances théoriques. Des ateliers interactifs sont nécessaires au moins tous les six mois au sein du service.
Although regionalization is the optimal way to deliver perinatal care to high risk mothers and infants, it is essential that the peripheral hospitals’ capabilities be constantly maintained in the areas of resuscitation, stabilization and transportion of infants whose mothers had either not been identified previously as being high risk or whose condition had been too unstable to permit a transfer before delivery (1). A national survey of Canadian hospitals conducted in 1986, however, showed that there was a significant need for inservice education in neonatal resuscitation (2). In 1989, the Canadian Institute of Child Health published guidelines that outlined the criteria for the identification of high risk newborns and gave practical guidance about resuscitation (3). These guidelines supported the use of the Textbook of Neonatal Resuscitation, which was produced for the American Academy of Pediatrics (AAP) in 1987 (4) and endorsed by the Canadian Paediatric Society in 1989. Although these two valuable textbooks provide excellent learning opportunities, there remains a need for coordinated instruction in neonatal resuscitation so that individuals can function as members of a team that works within the framework presented in the text. Even regular experience with cardiopulmonary resuscitation does not seem to help individuals retain knowledge and skill (5–7). More importantly, the authors of the textbooks mentioned above and other authors (5,8) have shown that an individual’s perception of skills is frequently at variance with his or her tested ability.
Proven knowledge and ability in neonatal resuscitation by health care personnel working in birthing suites is becoming mandatory in some Canadian hospitals. The question remains as to how frequently individuals should be tested with regard to the maintenance of competence in this area. Many authors have shown a fall off in adult cardiopulmonary resuscitation skills in both medical and nursing staff within six months of training (6,9–11), and Fossel and his co-workers (12) demonstrated a decline in skills by medical students even after a two-to three-week period. Programs in neonatal resuscitation seem to affect changes in preparedness and equipment (13), and performance (8). Only Fossel et al (12), however, evaluated the impact of a neonatal resuscitation education program with regard to the retention of knowledge and skill, but the study was limited to nursing personnel. The present study evaluates whether knowledge and skills are gained and retained after a neonatal resuscitation course.
DATA AND METHODS
During eight months, a course in neonatal resuscitation was given at seven level II perinatal centres within the central-east region of Ontario. The course was open to all personnel (medical, nursing and respiratory technologists) who worked in the centres’ obstetrical units. The course included central lectures given by a neonatologist. The content of the lecture was based on published material that is widely accepted (3,4,14), and dealt with the patho-physiology of asphyxia neonatorum, the initial evaluation and management of an infant at risk, and the preparation and use of equipment and medications required. The effectiveness of properly applied bag and mask ventilation was emphasized over endotracheal intubation. Following the lecture, all participants were divided into groups of no more than 10 individuals for a practical demonstration using mannequins that were equipped with electronic indicators of correct ventilation and chest compression techniques (Armstrong Medical Industries Canada Inc, Canada). For the practical sessions, the nursing staff and respiratory technologists were instructed by a nurse professor and the physicians by a neonatologist. Questions were invited in an informal setting. Although attendance at the course was voluntary, some centres boosted attendance by making payments to registered nurses and respiratory technologists who attended the course on off-duty days. The course was repeated on as many occasions as required during a one-week period to allow maximum attendance. Some centres chose to have the lecture and practical sessions given consecutively to small numbers of personnel (10 to 20 individuals) over several days. Other centres chose one or two large lecture presentations followed by many practical sessions over several days. Before undertaking the course, the institutions coded all participants and assigned 20% of them to undergo written and practical pretesting by the investigators. Institutions were requested only to assign staff for pre- and post-testing who were likely to remain in the birthing unit for the duration of the study.
The written test consisted of a 55-item, multiple choice examination that covered 13 facets of the lecture. The practical test consisted of a performance check list. Participants were given the scenario of a term infant born apnoeic through clear liquor amnii, and they were expected to dry and position the infant correctly, select a proper-sized mask, and initiate bag and mask ventilation. After 30 s, they were informed that the infant’s heart rate remained less than 80 beats/min, and while one examiner took over ventilation, they were requested to institute chest compressions. The choice of appropriate equipment, and the correct use of the equipment were scored on a scale of 0 to 2, where an incorrect choice was scored as 0, a correct choice received a score of 1, a persistently wrong application received a score of 0, an occasionally correct application was scored as 1 and a consistently correct application received a score of 2. The electronically operated lights on the mannequin were used to determine the scores. The doll is designed so that the lights are activated on preset limits when optimal chest compressions and ventilatory parameters are met. Both observers scored participants independently, and the average score was recorded. These same participants underwent the identical testing procedures immediately after the completion of the course, and then after six-and 12-month intervals. These follow-up tests were observed and scored by the same two individuals. Each participant was tested in private, and scores were reported to the participants immediately after testing.
Ethics
Permission to offer the course was obtained from the relevant departmental chiefs of each institution and also, where possible, from each institutions’ perinatal committee. Attendance at the course was voluntary. Codes assigned to the individuals to be tested were used throughout the study and assured anonymity. Nursing and respiratory technologists were given letter codes, and medical staff were given number codes to allow identification of the two groups. Upon completion of the course, a certificate of attendance, but not a certificate of competence, was issued.
Statistics
The results were analyzed using repeated measures analysis of variance and expressed as means, with 95% CIs. Only those individuals who completed the initial pre- and post-testing, as well as the six-and 12-month reviews were included in the final analyses.
RESULTS
In all, 737 health care professionals attended the initial course offered at each institution.
Fifty-nine lectures were given and 78 practical sessions were supervised. Only 62 individuals completed the course and were available for the full pre- and post-testing procedures at both six and 12 months. This total consisted of 34 physicians, and 28 nurses and allied health professionals. Twenty per cent of the total participants were chosen by each institution to undergo post-testing. Although these individuals were chosen at random, the institutions were allowed to reject those chosen if it was known that the individual was unlikely to be working in a birthing area at the time of the post-testing, and six and 12 months later. Thus, only 15% (108 of 737) of the participants were available at the initial post-test, and despite these precautions, only 62 individuals were available to complete all of the post-testing scheduled, and their results were used for the final analysis. The professional background of the tested group was virtually identical to the make-up of the initial cohort. Figures 1 and 2 show the combined performances of all participants in the written tests (Figure 1) and the practical testing (Figure 2). There were no significant differences in the performances at any stage between medical and nursing and/or allied health professional personnel in either factual knowledge (Figure 3) or practical scores (Figure 4). Those individuals who initially scored poorly in the written pretest improved their scores after the course, but not to such a degree as those whose factual knowledge was greater initially (Figure 5). The course allowed everyone’s practical performance to improve to a similar degree, irrespective of participants’ initial skills (Figure 6).
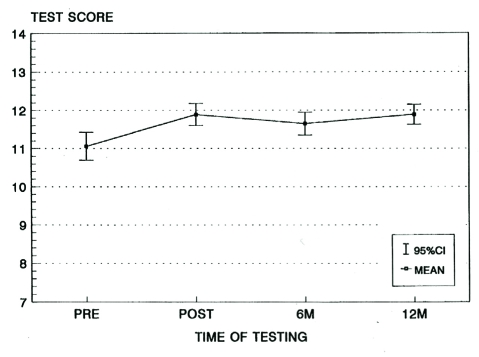
Figure 1.
The scores of all candidates in the written test, both before (pre) and after (post) the initial neonatal resuscitation teaching session, and six months (6M) and 12 months (12M) after the initial teaching session
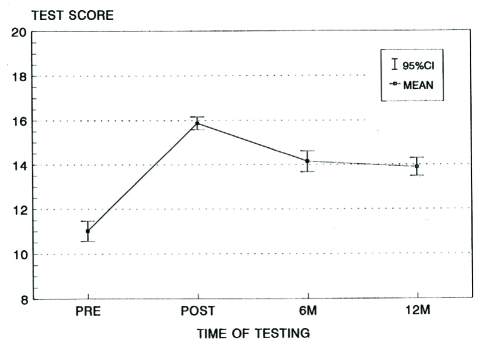
Figure 2.
The scores of all candidates in the practical test, both before (pre) and after (post) the initial neonatal resuscitation teaching session, and six months (6M) and 12 months (12M) after the initial teaching session
Figure 3.
Changes in performance in the written test between nursing (including allied health professionals) and medical personnel, both before (pre) and after (post) the initial neonatal resuscitation teaching session, and six months (6M) and 12 months (12M) after the initial teaching session. MD Medical doctor; RN Registered nurse
Figure 4.
Changes in performance in the practical test between nursing (including allied health professionals) and medical personnel, both before (pre) and after (post) the initial neonatal resuscitation teaching session, and six months (6M) and 12 months (12M) after the initial teaching session. MD Medical doctor; RN Registered nurse
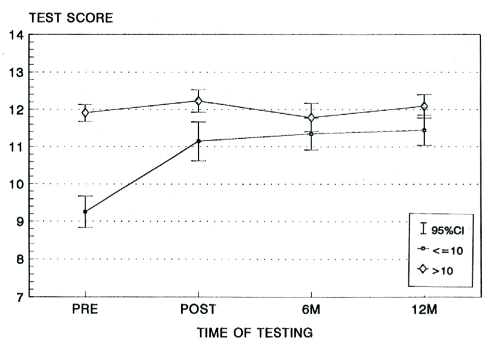
Figure 5.
Written test scores between those who initially scored well (a score above 10) compared with those who initially scored poorly (a score of 10 or less), both before (pre) and after (post) the initial neonatal resuscitation teaching session, and six months (6M) and 12 months (12M) after the initial teaching session
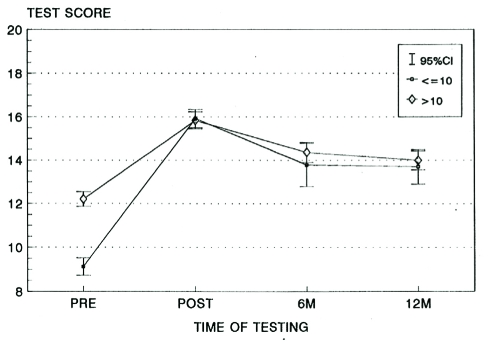
Figure 6.
Practical test scores between those who initially scored well (a score above 10) compared with those who initially scored poorly (a score of 10 or less), both before (pre) and after (post) the initial neonatal resuscitation teaching session, and six months (6M) and 12 months (12M) after the initial teaching session
Figure 1 shows that factual knowledge was improved and maintained after the course for a one-year period. Practical ability, however, began to fall off significantly after six months but was still maintained at a significantly greater degree, even after one year (Figure 2).
DISCUSSION
A limitation of this study is that the examiners were obviously aware that the individuals undergoing the initial practical, pre-test had not taken the course. It may have been possible to video all of the performances and have a third party assess the results after viewing the videos in random order. However, this option was considered impractical, and the error was limited by scoring only factual events and using the coloured, lighted codes on the mannequins to assess correct positioning and the effectiveness of resuscitation techniques. Appointments for the post-testing sessions were necessary; therefore, participants may have reviewed lecture notes beforehand. It was impossible to control for such an occurrence. Although follow-up scores were withheld, the relatively better performance at the 12-month testing may have been because of poor scores at the six-month testing sessions and review and/or practice that may have been undertaken for subsequent testing.
A similar education program offered to 190 nurses by Dunn et al (8) showed similar results, with knowledge but not skill performance being maintained at six months. That practical skills fall off quicker than knowledge of neonatal resuscitation is hardly surprising. It is easy to reread lecture notes, but practice can only be achieved by attending neonatal resuscitations or practice sessions. Only 8% of newborns require active resuscitation, so unless health care professionals work in perinatal centres for high risk deliveries, they may only participate in resuscitations once or twice per year, which is hardly frequently enough to maintain competence. Walker and Balvert (15) proposed a practical program to help maintain neonatal resuscitation skills. Their approach, coupled with the increasing use of the American Heart Association and the AAP Textbook of Neonatal Resuscitation (4) seems an ideal way to teach and maintain standards of neonatal resuscitation. Adherence to standards for neonatal resuscitation can and have been assessed, and have been shown to improve professional performance (16). The content of the present study’s educational initiative was similar but not identical to the Neonatal Resuscitation Program endorsed by the AAP and the Canadian Paediatric Society. The Neonatal Resuscitation Program has recently undergone revision and will need to be validated. Once this has been achieved, its impact on patient outcomes should be investigated in large scale, multicentre trials.
We wholeheartedly endorse Dunn and her co-workers’ (8) statement that “every nursery and intrapartum unit should have newborn mannequins, space and dedicated practice time to facilitate skills maintenance”. No effort was made to control for each participant’s personal involvement with neonatal resuscitation procedures during the period of this study nor for the participants’ perceived skill in this technique. To maintain competence, it would appear that both nurses and physicians, as well as paramedical support staff, require regular inservices at least every six months.
Acknowledgments
This work was supported by a grant from the Ontario Easter Seal Society.
REFERENCES
- 1.McManus F, Rang M, Chance G, Whittake J. Is cerebral palsy a preventable disease? Obstet Gynecol. 1977;50:71–7. [PubMed] [Google Scholar]
- 2.Chance G, Hanvey L. Neonatal resuscitation in Canadian hospitals. CMAJ. 1987;136:601–6. [PMC free article] [PubMed] [Google Scholar]
- 3.National Guidelines for Neonatal Resuscitation. Ottawa: Canadian Institute of Child Health; 1994. [Google Scholar]
- 4.Bloom RJ, Cropley C. Textbook of Neonatal Resuscitation Dallas: American Heart Association and American Academy of Pediatrics. 1994. [Google Scholar]
- 5.Moser DK, Coleman S. Recommendations for improving cardiopulmonary skills retention. Heart Lung. 1992;21:372–80. [PubMed] [Google Scholar]
- 6.Curry L, Gass D. Effects of training cardiopulmonary resuscitation on competence and patient outcome. CMAJ. 1987;137:491–6. [PMC free article] [PubMed] [Google Scholar]
- 7.Yakel ME. Retention of cardiopulmonary resuscitation skills among nursing personnel: What makes the difference? Heart Lung. 1989;18:520–5. [PubMed] [Google Scholar]
- 8.Dunn S, Niday P, Watters NE, McGrath P, Alcock D. The provision and evaluation of a neonatal resuscitation program. J Contin Educ Nurs. 1992;23:118–26. doi: 10.3928/0022-0124-19920501-08. [DOI] [PubMed] [Google Scholar]
- 9.Glendon AI, Blaylock S, McKenna SP, Hunt K. Cardiopulmonary resuscitation skill decay: Current research and findings. Br Health Safety Soc Newsl. 1986;12:14–8. [Google Scholar]
- 10.Kaye W, Mancini ME, Rallis SF, et al. Can better basic and advanced cardiac life support improve outcome from cardiac arrest. Crit Care Med. 1985;13:916–20. doi: 10.1097/00003246-198511000-00015. [DOI] [PubMed] [Google Scholar]
- 11.McKenna SP, Glendon AL. Occupational first aid learning: Decay in cardiopulmonary resuscitation skills. J Occup Psychol. 1985;58:109–17. [Google Scholar]
- 12.Fossel M, Kiskaddon RT, Sternbach GL. Retention of cardiopulmonary resuscitation skills by medical students. J Med Educ. 1983;58:568–75. doi: 10.1097/00001888-198307000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Singhal N, McMillan DD, Lockyer JM. Attitudinal and resource changes after a neonatal resuscitation training program. Neonatal Network. 1990;9:35–9. [PubMed] [Google Scholar]
- 14.Guidelines for cardiopulmonary resuscitation and emergency cardiac care. Recommendations of the 1992 National Conference. Emergency Cardiac Care Committee and Subcommittees, American Heart Association. Part VII: Neonatal Resuscitation JAMA 19922682276–81. [PubMed] [Google Scholar]
- 15.Walker DE, Balvert L. A practical program to maintain neonatal resuscitation skills. CMAJ. 1994;151:299–304. [PMC free article] [PubMed] [Google Scholar]
- 16.McCulloch KM, Vidyasagar D. Assessing adherence to standards for neonatal resuscitation taught throughout the perinatal area; A quality assurance activity. Pediatr Clin North Am. 1993;40:431–38. doi: 10.1016/s0031-3955(16)38519-4. [DOI] [PubMed] [Google Scholar]