Abstract
The study's aim was to examine factors that may influence health information managers in the adoption of electronic health records. The Technology Acceptance Model (TAM) served as theoretical foundation for this quantitative study. Hospital health information managers in Arkansas were queried as to the constructs of perceived usefulness, perceived ease of use, and behavior intention. The study population comprised 94 health information managers with a return rate of 74.5 percent. One manager was identified to represent each hospital. In each of the construct areas, the results showed a difference between health information managers that had adopted components of EHRs versus those that had not. This study may serve to guide the educational process of both health information managers that have yet to implement EHRs as well as the EHR vendor community.
Key words: health information, TAM, change management
Introduction
Recent healthcare reform efforts have placed additional emphasis on the need for electronic health records (EHRs) as a way to provide a more efficient exchange of health information. Anecdotal evidence has shown that a number of health information directors have not fully embraced the idea of implementing EHRs in their facility. The purpose of this study is to evaluate factors that may influence health information directors in hospitals to adopt EHR technology.
Background
Within a healthcare facility, a number of workers serve on a team to render the best care possible to each patient. The health information manager is the team member that may serve as a change agent to aid in the implementation of EHRs.1–2 In order for EHR implementation to occur, the health information manager must be willing to take on this leadership role.
Change Management and the Nature of Change
While change is a naturally occurring phenomenon in our daily lives, it is often approached with skepticism and fear. Most people tend to cling to the routine and known within their lives and shy away from the new and unfamiliar. They may feel personally threatened by impending change.3–4 The field of information technology (IT) is particularly known for ever-changing innovations, as is the field of medicine. It is no wonder that change is evident yet often feared in the area of health information technology. In the face of inevitable change, a leader of change emerges to direct the organization through the transformation process. One study defines the concept of change management as “the process by which an organization gets to its future state, its vision.”5 This definition gives a positive spin to the notion of change.
Studies have examined the notion of acceptance of many different forms of technology. Examples of these include online shopping and banking technology and even patients' access to health information on the Internet. These studies looked at processes viewed as optional for the end user. When studying the implementation of electronic health records, however, the end user is expected to utilize the technology. It is viewed as mandatory and not optional. The end users of health information technology in a hospital would be required to make use of the technology or lose their job. Very little research appears to have been conducted in the area of mandatory implementation and usage of any technology, and health information technology in particular.
A review of literature in this area suggests that several barriers exist in the implementation of electronic health records. These barriers seem to focus on process barriers, such as interoperability and cost issues. Resistance to change is a natural phenomenon, and strong leadership is needed to aid in the implementation of such technology.6 There appears to be a gap in the literature regarding the human aspects of implementation of electronic health records.
Theoretical Model
This study utilized the Technology Acceptance Model (TAM) to evaluate the factors that cause end users to embrace or reject information technology.7 This model appears to be particularly applicable in the health information technology field because it focuses on two specific variables believed to influence the use of information technology. Perceived usefulness is the factor that indicates the degree that the person believes the information system will assist them in the performance of their job.8–9 Perceived ease of use is the second factor, which is used to indicate how difficult the person believes the proposed system would be to use.10–11
These constructs are based in the theory of reasoned action, which noted that a person's behavioral intention is determined by the person's attitude as well as a subjective norm as estimated by regression.12
While the TAM has been utilized in a number of studies dealing with a wide array of information technologies, a review of the literature shows very few studies in the healthcare field and even fewer related to health information technology. No studies were found to investigate health information managers and their role in the implementation of electronic health record systems.
Research Questions
The research questions addressed in this study are as follows:
Is there a difference in the perceived usefulness of EHRs between health information managers that have adopted EHRs and those that have not adopted EHRs?
Is there a difference in the perceived ease of use of EHRs between health information managers that have adopted EHRs and those that have not adopted EHRs?
Is there a difference in behavioral intention between health information managers that have made the decision to adopt EHRs and those that have not adopted EHRs?
Methods
Population
Hospitals listed as members of the Arkansas Hospital Association were used as the study population. Within each hospital listed, one health information manager was identified to receive the study survey. This encompassed a total of 94 healthcare facilities/managers within the state.
Study Design
A survey link was e-mailed to each health information manager in the population. This introductory e-mail included a definition of electronic health records, as noted in an Institute of Medicine report, so that all respondents would be utilizing the same baseline definition of the technology.13 The survey was administered through SurveyMonkey (www.surveymonkey.com), an Internet-based survey hosting service.
The questions of the survey were constructed to measure perceived usefulness, perceived ease of use, and behavioral intention as potential factors as viewed by the health information manager in implementing EHRs. A Likert scale ranging from strongly disagree to strongly agree for each construct was used as a measurement tool. Seven demographic questions were also included on the survey. Table 1 lists statements used to measure perceived usefulness. Table 2 lists statements used to measure perceived ease of use. Table 3 lists the statements used to measure behavioral intention. Demographic questions assessed areas including the age of the respondent, the size and type of hospital, the respondent's professional credential status and years of experience, the respondent's level of education, and whether or not the facility had already implemented any components of EHRs. The survey was constructed from instruments that had previously been used and tested for reliability. Once survey data was received, it was downloaded directly from SurveyMonkey to SPSS 16.0 for analysis.
Table 1.
Statements Addressing Perceived Usefulness
| Construct | Statement |
| Perceived Usefulness | Using EHRs in my job would enable me to accomplish tasks more quickly. |
| Using EHRs would improve my job performance. | |
| Using EHRs would make it easier to do my job. | |
| EHRs are useful in my job. | |
| Using EHRs in my job would increase my productivity. |
Table 2.
Statements Addressing Perceived Ease of Use
| Construct | Statement |
| Perceived Ease of Use | I believe that interaction with an EHR would be clear and understandable. |
| I believe navigation of an EHR would be easy. | |
| Learning to operate an EHR would be easy for me. | |
| It would be easy for me to become skillful at using an EHR system. |
Table 3.
Statements Addressing Behavioral Intention
| Construct | Statement |
| Behavioral Intention | I am willing to use an EHR for my work. |
| I do not mind spending some time to learn how to use this system for my work. |
Results
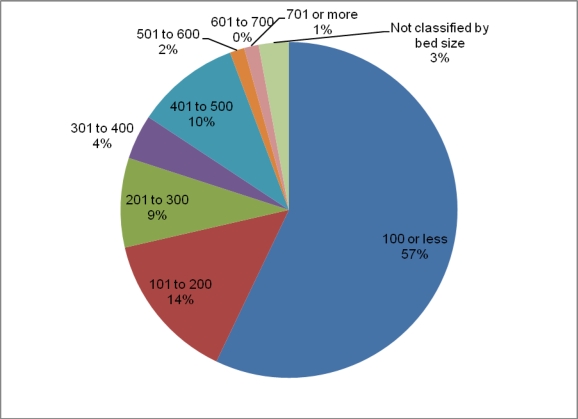
A total of 94 surveys were distributed, and 70 were received for a response rate of 74.5 percent. No surveys were returned incomplete. No data items were missing. The demographic items assessed characteristics of the healthcare facility as well as characteristics of the individual completing the survey. The items used to evaluate the facility include the size and type of facility. Percentages for each of these variables are shown in Figure 1 and Figure 2.
Figure 1.
Distribution of Facility (Bed) Size
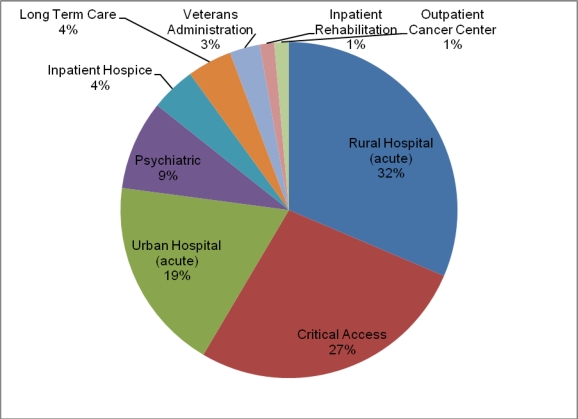
Figure 2.
Distribution of Facility Type
Examination of the demographic characteristics of the facilities shows that 71.4 percent of the respondents represent smaller facilities, with 200 beds or less. This is expected and is in keeping with the rural nature of the state of Arkansas. The U.S. Census Bureau reports 51.3 persons per square mile according to 2000 census data, compared to 79.6 persons per square mile in the entire United States.14 The fact that most respondents represent smaller facilities is further evidenced by the fact that the majority (58.6 percent) of the respondent directors work in critical access or rural hospitals, both characteristic of smaller facilities.
Cross tabulation for the facility (bed) size and adoption of EHR components is shown in Table 4. For each category of facility size, more facilities had begun to use EHR components than those that had not. The largest percentage of those that were not using EHR components is in the category of 100 beds or less. All of the facilities with over 300 beds as well as those that are not classified by bed size indicated that EHR components have been adopted.
Table 4.
Cross Tabulation of Facility (Bed) Size and Adoption of EHR Components
| Adopted EHR Components | |||
| Facility (Bed) Size | Yes | No | Total |
| 100 or less | 18 (45%) | 22 (55%) | 40 (100%) |
| 101–200 | 8 (80%) | 2 (20%) | 10 (100%) |
| 201–300 | 5 (83%) | 1 (17%) | 6 (100%) |
| 301–400 | 3 (100%) | 0 (0%) | 3 (100%) |
| 401–500 | 7 (100%) | 0 (0%) | 7 (100%) |
| 501–600 | 1 (100%) | 0 (0%) | 1 (100%) |
| 601–700 | 0 (0%) | 0 (0%) | 0 (0%) |
| 701 or more | 1 (100%) | 0 (0%) | 1 (100%) |
| Not classified by bed size | 2 (100%) | 0 (0%) | 2 (100%) |
| Total | 45 (64%) | 25 (36%) | 70 (100%) |
Table 5 shows the cross tabulation for the type of facility and those that have adopted EHR components. Within the 64 percent of facilities that reported adoption of EHR components, 100 percent of respondents from inpatient hospice facilities, the outpatient cancer center, urban acute hospitals, and Veterans Administration hospitals had adopted some components of EHRs.
Table 5.
Cross Tabulation of Facility Type and Adoption of EHR Components
| Adopted EHR Components | |||
| Facility Classification | Yes | No | Total |
| Critical Access | 8 (42%) | 11 (58%) | 19 (100%) |
| Inpatient Hospice | 3 (100%) | 0 (0%) | 3 (100%) |
| Long Term Care | 0 (0%) | 3 (100%) | 3 (100%) |
| Outpatient Cancer Center | 1 (100%) | 0 (0%) | 1 (100%) |
| Psychiatric | 1 (17%) | 5 (83%) | 6 (100%) |
| Rural Acute Hospital | 17 (77%) | 5 (23%) | 22 (100%) |
| Urban Acute Hospital | 13 (100%) | 0 (0%) | 13 (100%) |
| Veterans Administration Hospital | 2 (100%) | 0 (0%) | 2 (100%) |
| Inpatient Rehabilitation | 0 (0%) | 1 (100%) | 1 (100%) |
| Total | 45 (64%) | 25 (36%) | 70 (100%) |
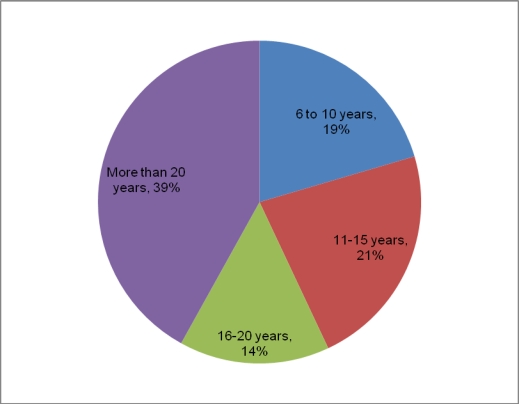
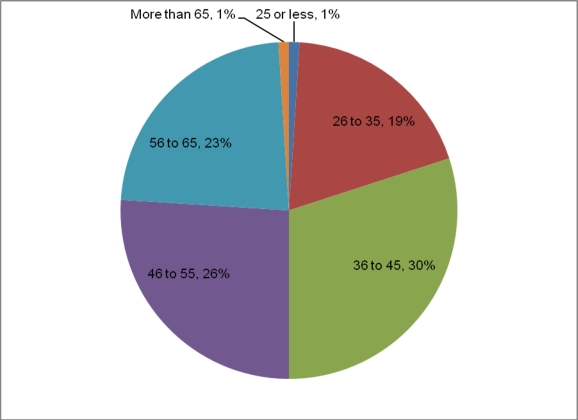
The remainder of the demographic items focused on the health information manager. These include the number of years of experience in the health information management field, the age of the respondent, and professional credentials held. Percentages for each of these variables are shown in Figure 3, Figure 4, and Figure 5. The majority of the health information managers that responded (74.3 percent) had more than 10 years of experience, with 38.6 percent having more than 20 years of experience. The reported ages of respondents are as expected for a population made up of management-level professionals in the field of health information: 20 percent indicated an age of 35 or less and 80 percent were 36 or older.
Figure 3.
Distribution of Health Information Managers' Years of Experience
Figure 4.
Distribution of Health Information Managers' Age
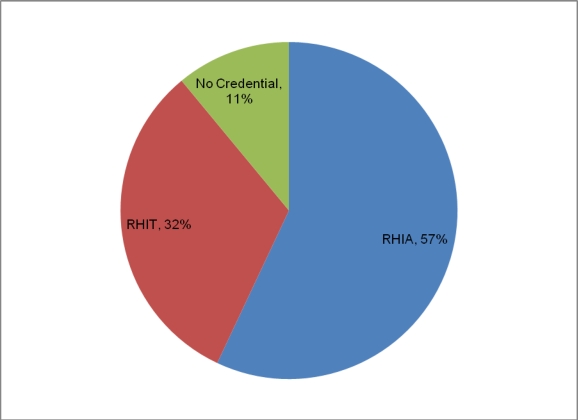
Figure 5.
Distribution of Health Information Managers' Professional Credentials
The Registered Health Information Administrator (RHIA) credential was held by 57.1 percent of respondents, while 31.4 percent had obtained the Registered Health Information Technician (RHIT) credential. A total of 11.4 percent of respondents did not have a professional credential. However, some reported that they were in progress of obtaining a credential.
Table 6 illustrates the cross tabulation of years of experience and adoption of EHR components. The only category in which more health information managers had not adopted components of EHRs than those that had was the group with less than six years of experience. The highest rates of EHR component adoption were in the two categories with the most experience.
Table 6.
Cross Tabulation of Respondents' Years of Experience and Adoption of EHR Components
| Adopted EHR Components | |||
| Years of Experience | Yes | No | Total |
| 0–5 years | 2 (40%) | 3 (60%) | 5 (100%) |
| 6–10 years | 7 (54%) | 6 (46%) | 13 (100%) |
| 11–15 years | 8 (53%) | 7 (47%) | 15 (100%) |
| 16–20 years | 8 (80%) | 2 (20%) | 10 (100%) |
| More than 20 years | 20 (74%) | 7 (26%) | 27 (100%) |
| Total | 45 (64%) | 25 (36%) | 70 (100%) |
Table 7 details the statistics for perceived usefulness. The nonparametric Mann-Whitney U and Wilcoxon W tests were chosen for use in this study as the values were assessing preferences rather than a specific numerical amount. Also, assumptions necessary for parametric tests were not met. The p-values of all the constructs of perceived usefulness were less than .05. The p-value of PU1 (accomplish tasks more quickly) was .000. The p-val ue of PU2 (improve job performance) was .009. The p-value of PU3 (easier to do job) was .000. The p-value of PU4 (useful) was .000, and the p-value of PU5 (will increase productivity) was .003. With all of these falling below .05, the null hypothesis was rejected. There is a difference in perceived usefulness of EHRs between health information managers that have adopted them versus those that have not them.
Table 7.
Perceived Usefulness Test Statistics
| PU1 | PU2 | PU3 | PU4 | PU5 | |
| Mann-Whitney U | 107.000 | 158.000 | 101.000 | 115.000 | 143.000 |
| Wilcoxon W | 162.000 | 213.000 | 156.000 | 170.000 | 198.000 |
| Z | −3.78 | −2.595 | −3.724 | −3.495 | −2.947 |
| Asymp. Sig. (2-tailed) | .000 | .009 | .000 | .000 | .003 |
| Grouping Variable: Have Adopted EHRs | |||||
Statistics for perceived ease of use are found in Table 8. The p-values of each of the constructs for perceived ease of use were below .05. The p-values for PEOU1 (interaction with EHR would be clear and understandable), PEOU2 (easy to navigate), PEOU3 (easy to learn), and PEOU4 (easy to become skillful) were all .000. With this value being below .05, the null hypothesis was rejected. There is a difference in the perceived ease of use of EHRs between health information managers that have adopted them versus those that have not adopted them.
Table 8.
Perceived Ease of Use Test Statistics
| PEOU1 | PEOU2 | PEOU3 | PEOU4 | |
| Mann-Whitney U | 84.000 | 79.500 | 80.000 | 80.000 |
| Wilcoxon W | 139.000 | 134.500 | 135.000 | 135.000 |
| Z | −3.882 | −3.951 | −4.029 | −4.112 |
| Asymp. Sig. (2-tailed) | .000 | .000 | .000 | .000 |
| Grouping Variable: Have Adopted EHRs | ||||
Table 9 contains statistics for the behavioral intention construct. The p-values for both BI1 (willing to use) and BI2 (willing to spend time to learn) were .000. This is less than .05, so the null hypothesis was rejected. There is a difference in behavioral intention between health information managers who have made the decision to adopt EHRs versus those that have not adopted EHRs.
Table 9.
Behavioral Intention Test Statistics
| BI1 | BI2 | |
| Mann-Whitney U | 110.000 | 110.000 |
| Wilcoxon W | 165.000 | 165.000 |
| Z | −3.842 | −3.842 |
| Asymp. Sig. (2-tailed) | .000 | .000 |
| Grouping Variable: Have Adopted EHRs | ||
Discussion
The population of the study appeared to reflect the rural nature of the state. Many of the facilities were small, with 71.4 percent having 200 beds or less. A total of 58.5 percent were either a rural acute care hospital or a critical access hospital. Only two hospitals were classified as having more than 500 beds. It was believed that, due to the small and rural nature of the hospitals in the state, there would be a small number that had adopted EHR components. It was not surprising that 55 percent of the facilities with 100 beds or less had not adopted any EHR components. Conversely, 100 percent of hospitals with 300 beds or more had adopted some EHR components.
The demographic picture of the health information managers revealed that the largest category (38.6 percent) had 20 or more years of experience and the smallest category (7.1 percent) had five or fewer years of experience. This finding is expected as the population surveyed was health information department managers, who would tend to have more experience to be able to supervise a department. Another finding that fits with this picture is the fact that 80 percent reported to be 36 or older. This is also consistent with the fact that a department manager would usually require some years to earn experience before moving into an administrative position.
The first research question was “Is there a difference in the perceived usefulness of EHRs between health information managers that have adopted EHRs and those that have not adopted EHRs?” Within the area of perceived usefulness, it was evident that respondents that had adopted EHR components felt that EHRs would be beneficial in their work. Results indicated that EHRs would enable them to accomplish tasks more quickly as well as improve their job performance. The health information managers surveyed felt EHRs would make it easier to do their job and would also increase their productivity. This addresses the first research question in that there is a difference in the perceived usefulness of EHRs between health information managers that have adopted EHRs and those that have not adopted EHRs.
The second research question was “Is there a difference in perceived ease of use of EHRs between health information managers that have adopted EHRs and those that have not adopted EHRs?” The responses indicated a difference of perceived ease of use between those that had adopted EHRs and those that had not. Health information managers felt EHRs would be clear and understandable and easy to navigate. They further felt learning to operate an EHR and becoming skillful with an EHR would be easy.
The third research question was, “Is there a difference in behavioral intention between health information managers that have made the decision to adopt EHRs and those that have not adopted EHRs?” In the category of behavioral intention, survey respondents indicated that they would be willing to use an EHR and would be willing to spend time to learn such a system. Perhaps this is a result of managers' becoming more comfortable with the use of computers in general. Many use electronic functions such as banking applications or online shopping.
Implications for Practice and Further Research
While it is widely accepted that electronic health records are inevitable for the future of healthcare, the challenge comes in empowering a change leader within each facility to direct the effort for implementation. If health information managers understand the EHR system to be used, including how it could improve their job and that it would be relatively easy to use, they will be more likely to take the role of change leader and aid in the implementation of the system. The same is true when considering behavioral intention factors as related to EHR technology. Health information managers seem more likely to adopt EHR technology if their attitude reflects the belief that they would be willing to use the EHR system. Health information managers also appear more likely to adopt EHR technology if they are willing to spend time to learn the EHR system.
The TAM appears to be upheld with the results of the study. These results shed some light on factors that have proven significant for adoption of EHRs by health information managers. Perhaps educational tools could be developed to guide facilities through the implementation process and minimize resistance to change. Vendors may also possibly benefit from the results as the constructs of the study point to reasons that health information managers would want to utilize EHRs.
While this study gives some insight as to the thought process of health information managers when adopting EHR technology, it focused on only one state. Expanding the study to encompass the entire United States could serve to offer additional information and further support the theoretical model. Another area recommended for further study includes physician offices as well as other healthcare providers. One overall goal of the Office of the National Coordinator for Health Information Technology is to provide for consumer-centric healthcare.15 With consumers receiving care at a wide variety of settings, health information managers at these settings could have critical input into the consumers' overall EHR use, and therefore their attitudes related to EHRs could be investigated in future studies.
Notes
- 1.Amatayakul M, Work M. Best Practices in Electronic Health Records. Chicago, IL: AHIMA; 2006. [Google Scholar]
- 2.Fenton S.H, Amatayakul M, Work M. “The HIM Impact of EHRs: Newly Released Study Links HIM Professionals and Successful EHR Implementations.”. Journal of AHIMA. 2006;77(9):36–40. [PubMed] [Google Scholar]
- 3.Folaran J. “The Human Side of Change Leadership.”. Quality Progress. 2005;38(4):39–43. [Google Scholar]
- 4.Glandon G.L, Smaltz D.H, Slovensky D.J. Austin and Boxerman's Information Systems for Healthcare Management. Arlington, VA: AUPHA Press; 2008. [Google Scholar]
- 5.Lorenzi N.M, Riley R.T. “Managing Change: An Overview.”. Journal of the American Medical Informatics Association. 2000;7:116–24. doi: 10.1136/jamia.2000.0070116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Poon E.G, Blumenthal D, Jaggi T, Honour M.M, Bates D.W, Kaushal R. “Overcoming Barriers to Adopting and Implementing Computerized Order Entry Systems in U.S. Hospitals.”. Health Affairs. 2004;23:184–90. doi: 10.1377/hlthaff.23.4.184. [DOI] [PubMed] [Google Scholar]
- 7.Davis F.D. “Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology.”. MIS Quarterly. 1989;13(3):319–40. [Google Scholar]
- 8.Davis F.D. “Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology.”. MIS Quarterly. 1989;13(3):319–40. [Google Scholar]
- 9.Davis F.D, Bagozzi R.P, Warshaw P.R. “User Acceptance of Computer Technology: A Comparison of Two Theoretical Models.”. Management Science. 1989;35(8):982–1003. [Google Scholar]
- 10.Davis, F.D., “Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology.”
- 11.Davis, F.D., R. P. Bagozzi, and P. R. Warshaw. “User Acceptance of Computer Technology: A Comparison of Two Theoretical Models.”
- 12.Ajzen I, Fishbein M. Understanding Attitudes and Predicting Social Behavior. Englewood Cliffs, NJ: Prentice-Hall; 1980. [Google Scholar]
- 13.Tang P.C. Key Capabilities of an Electronic Health Record System. Letter Report by Committee on Data Standards for Patient Safety to Institute of Medicine. Washington, DC: National Academy of Science; 2003. [Google Scholar]
- 14.U.S. Census Bureau. “Arkansas Quick Facts.” 2006. Available at http://quickfacts.census.gov/qfd/states/05000.html (accessed October 19, 2008).
- 15.U.S. Department of Health and Human Services. “The Office of the National Coordinator for Health Information Technology.” Available at http://healthit.hhs.gov/portal/server.pt?open=512&objID=1200&parentname=CommunityPage&parentid=18&mode=2&in_hi_userid=10741&cached=true (accessed August 28, 2009).